PCP in adults Presentation Treatment and Prophylaxis Prof



- Slides: 26
PCP in adults: Presentation , Treatment and Prophylaxis Prof. David W. Denning Professor of Infectious Diseases in Global Health The University of Manchester, UK

Presentation in adults
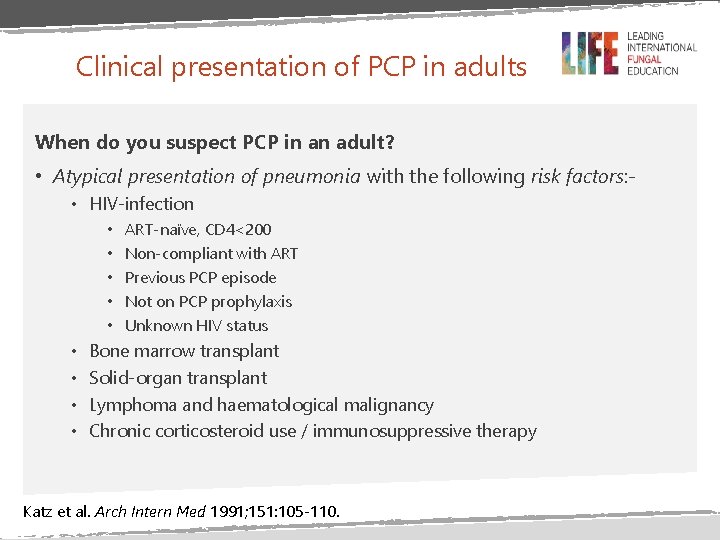
Clinical presentation of PCP in adults When do you suspect PCP in an adult? • Atypical presentation of pneumonia with the following risk factors: • HIV-infection • • • ART-naïve, CD 4<200 Non-compliant with ART Previous PCP episode Not on PCP prophylaxis Unknown HIV status Bone marrow transplant Solid-organ transplant Lymphoma and haematological malignancy Chronic corticosteroid use / immunosuppressive therapy Katz et al. Arch Intern Med 1991; 151: 105 -110.
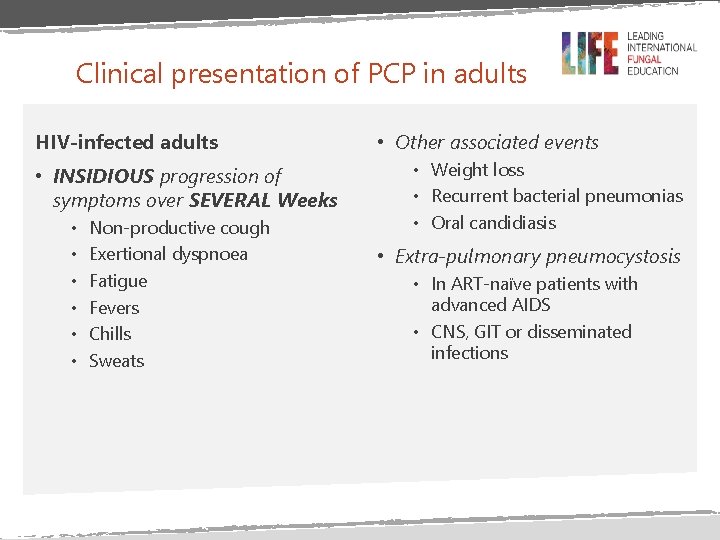
Clinical presentation of PCP in adults HIV-infected adults • INSIDIOUS progression of symptoms over SEVERAL Weeks • • • Non-productive cough Exertional dyspnoea Fatigue Fevers Chills Sweats • Other associated events • Weight loss • Recurrent bacterial pneumonias • Oral candidiasis • Extra-pulmonary pneumocystosis • In ART-naïve patients with advanced AIDS • CNS, GIT or disseminated infections
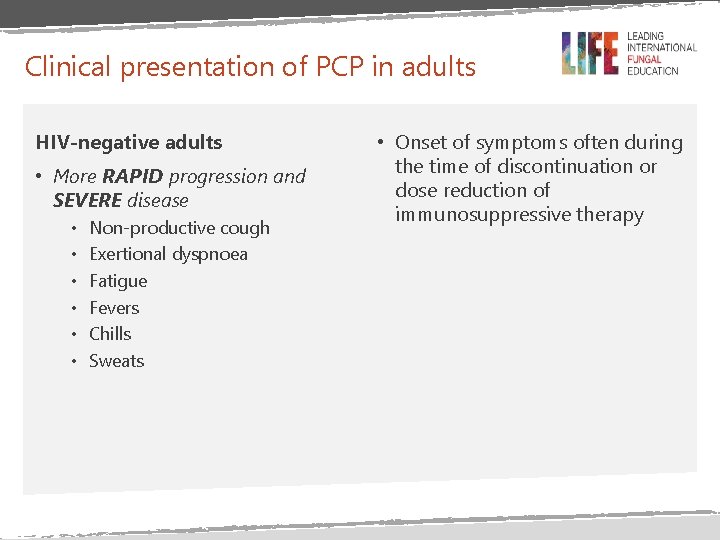
Clinical presentation of PCP in adults HIV-negative adults • More RAPID progression and SEVERE disease • • • Non-productive cough Exertional dyspnoea Fatigue Fevers Chills Sweats • Onset of symptoms often during the time of discontinuation or dose reduction of immunosuppressive therapy
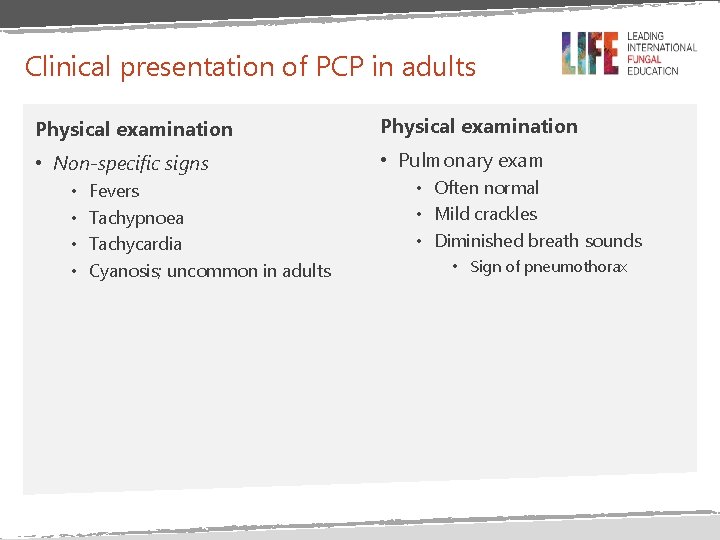
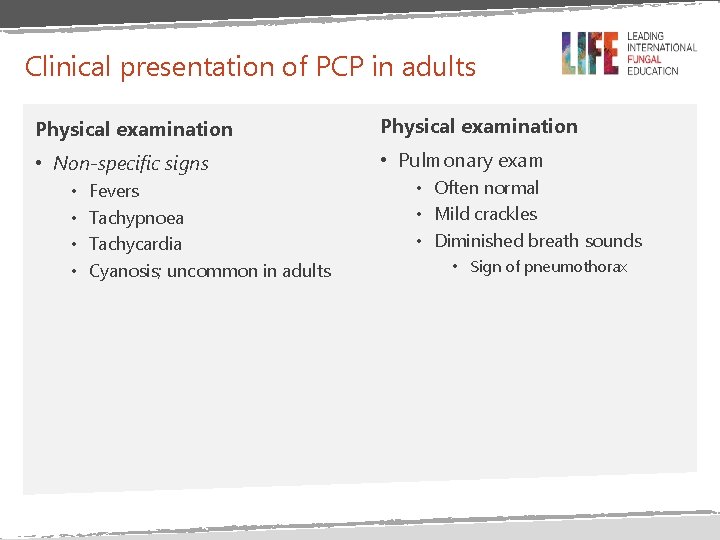
Clinical presentation of PCP in adults Physical examination • Non-specific signs • Pulmonary exam • • Fevers Tachypnoea Tachycardia Cyanosis; uncommon in adults • Often normal • Mild crackles • Diminished breath sounds • Sign of pneumothorax
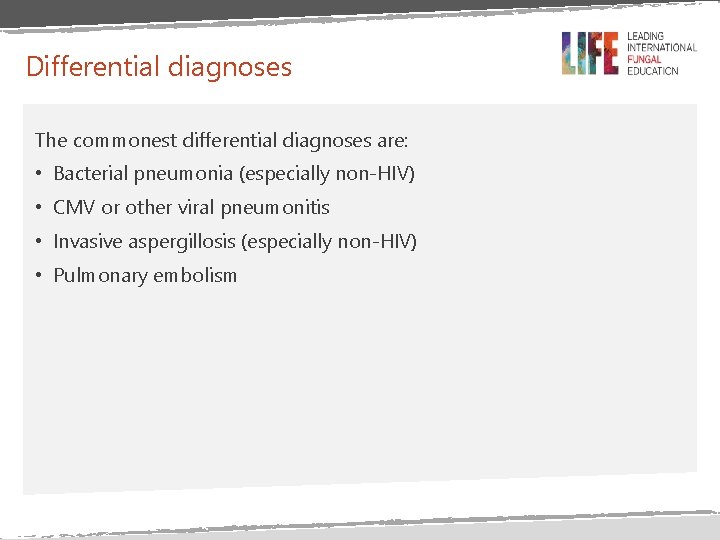
Differential diagnoses The commonest differential diagnoses are: • Bacterial pneumonia (especially non-HIV) • CMV or other viral pneumonitis • Invasive aspergillosis (especially non-HIV) • Pulmonary embolism
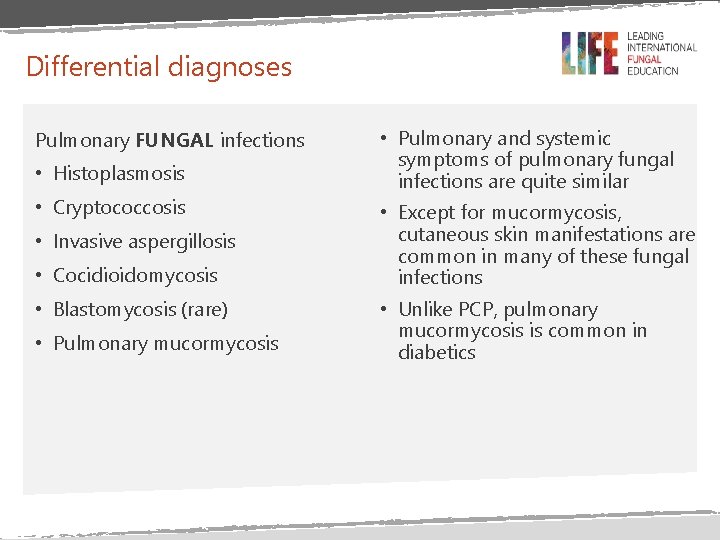
Differential diagnoses Pulmonary FUNGAL infections • Histoplasmosis • Cryptococcosis • Invasive aspergillosis • Cocidioidomycosis • Blastomycosis (rare) • Pulmonary mucormycosis • Pulmonary and systemic symptoms of pulmonary fungal infections are quite similar • Except for mucormycosis, cutaneous skin manifestations are common in many of these fungal infections • Unlike PCP, pulmonary mucormycosis is common in diabetics
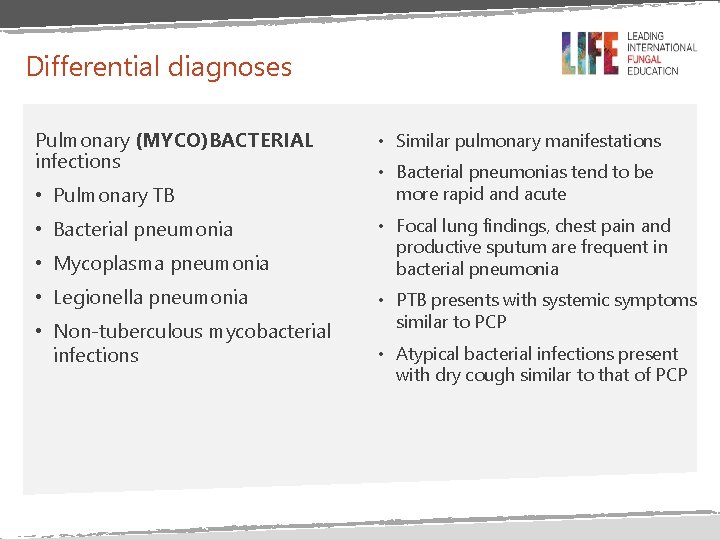
Differential diagnoses Pulmonary (MYCO)BACTERIAL infections • Pulmonary TB • Bacterial pneumonia • Mycoplasma pneumonia • Legionella pneumonia • Non-tuberculous mycobacterial infections • Similar pulmonary manifestations • Bacterial pneumonias tend to be more rapid and acute • Focal lung findings, chest pain and productive sputum are frequent in bacterial pneumonia • PTB presents with systemic symptoms similar to PCP • Atypical bacterial infections present with dry cough similar to that of PCP
Differential diagnoses Pulmonary VIRAL infections • Cytomegalovirus pneumonitis • Influenza • Other viral pneumonias • CMV pneumonitis is usually associated with a non-productive cough and minimal findings on lung examination and is more common in HIV-negative patients • Influenza has signs and symptoms similar to PCP and does not respond to empirical antibiotic therapy
Differential diagnoses Pulmonary OTHER conditions • Pulmonary Kaposi's sarcoma • Acute respiratory distress syndrome • Pulmonary embolus • Sarcoidosis • Non-infectious interstitial lung diseases • Lymphoid interstitial pneumonitis • Pulmonary symptoms similar to those of PCP are common in this conditions • Unlike PCP, these conditions are often associated with pleural effusion
PCP versus other conditions In PCP: Hypoxia or exercise-induced hypoxia (reduced O 2 saturation) is worse than the chest X-ray would suggest.

Treatment
Treatment considerations • Severity of the disease • Based on blood gas analysis or • Room air partial pressure of oxygen (p. O 2) • Toxicities of the agents • Adjunctive therapy • Moderate-severe PCP
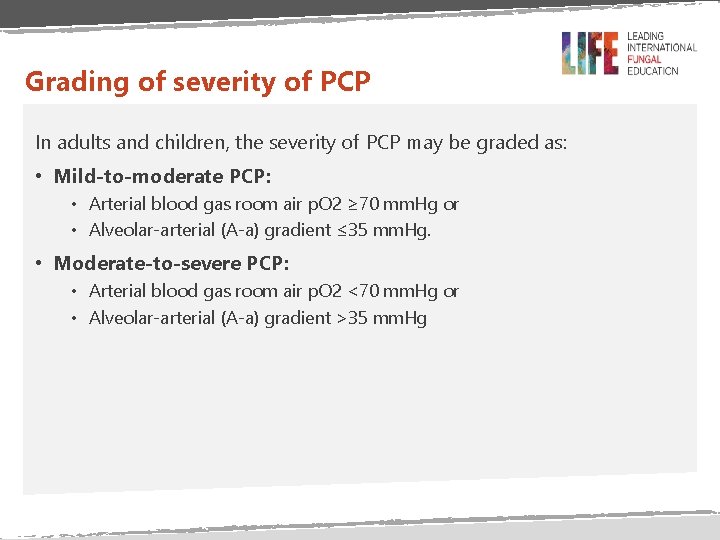
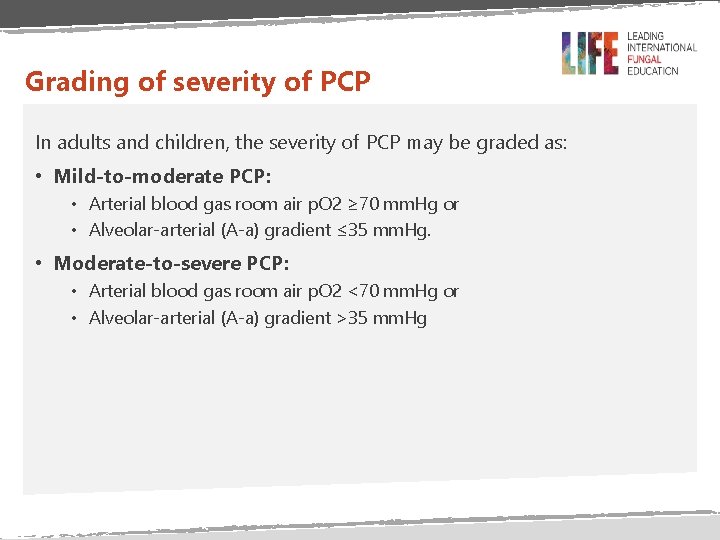
Grading of severity of PCP In adults and children, the severity of PCP may be graded as: • Mild-to-moderate PCP: • Arterial blood gas room air p. O 2 ≥ 70 mm. Hg or • Alveolar-arterial (A-a) gradient ≤ 35 mm. Hg. • Moderate-to-severe PCP: • Arterial blood gas room air p. O 2 <70 mm. Hg or • Alveolar-arterial (A-a) gradient >35 mm. Hg
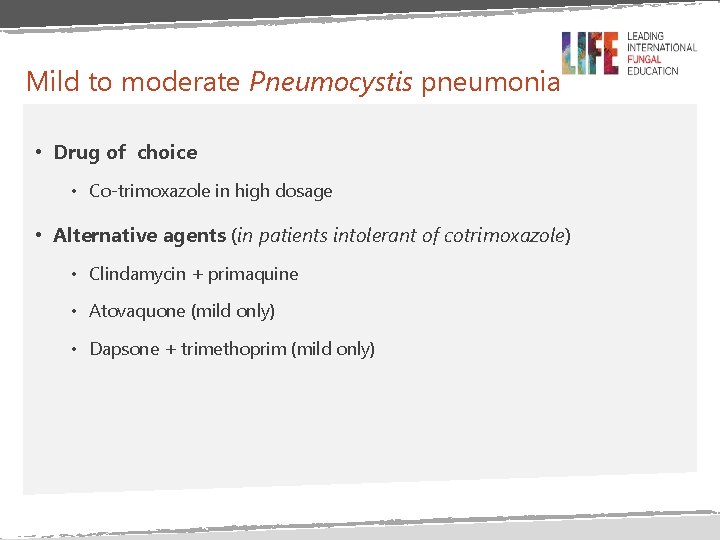
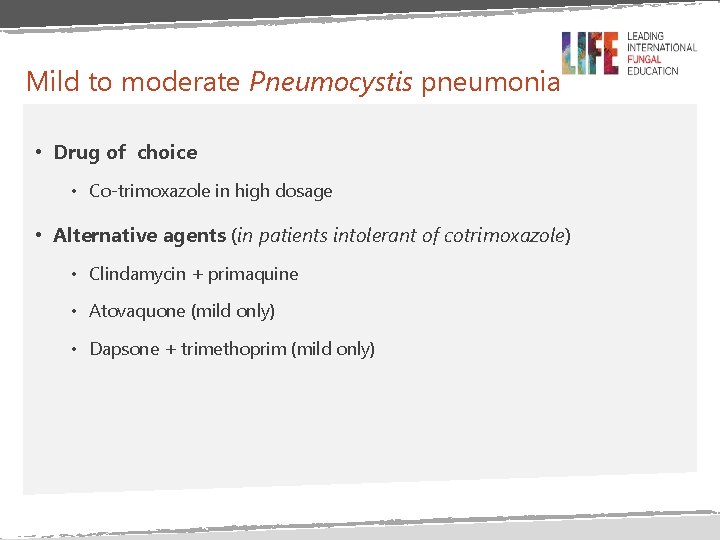
Mild to moderate Pneumocystis pneumonia • Drug of choice • Co-trimoxazole in high dosage • Alternative agents (in patients intolerant of cotrimoxazole) • Clindamycin + primaquine • Atovaquone (mild only) • Dapsone + trimethoprim (mild only)
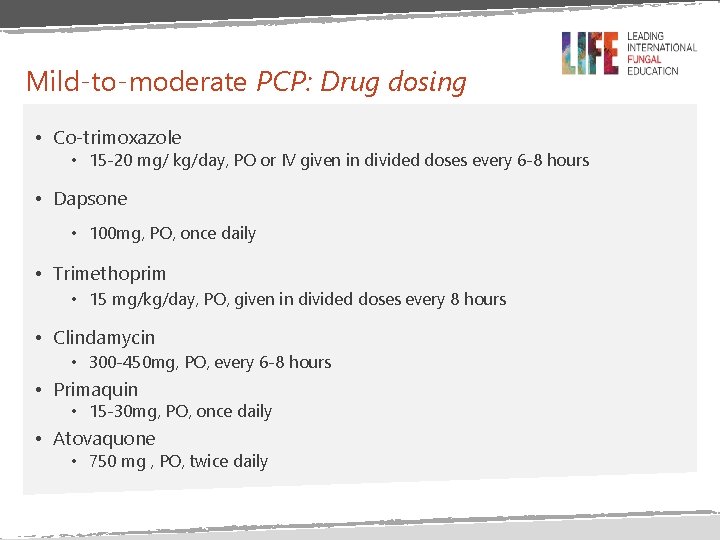
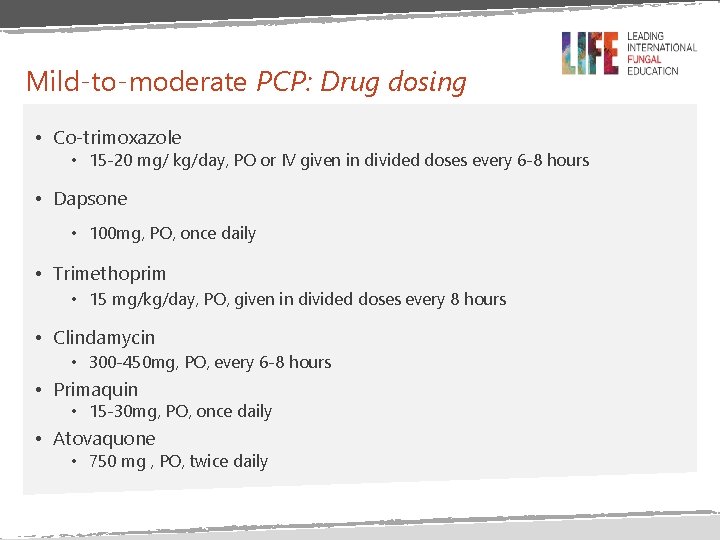
Mild-to-moderate PCP: Drug dosing • Co-trimoxazole • 15 -20 mg/ kg/day, PO or IV given in divided doses every 6 -8 hours • Dapsone • 100 mg, PO, once daily • Trimethoprim • 15 mg/kg/day, PO, given in divided doses every 8 hours • Clindamycin • 300 -450 mg, PO, every 6 -8 hours • Primaquin • 15 -30 mg, PO, once daily • Atovaquone • 750 mg , PO, twice daily
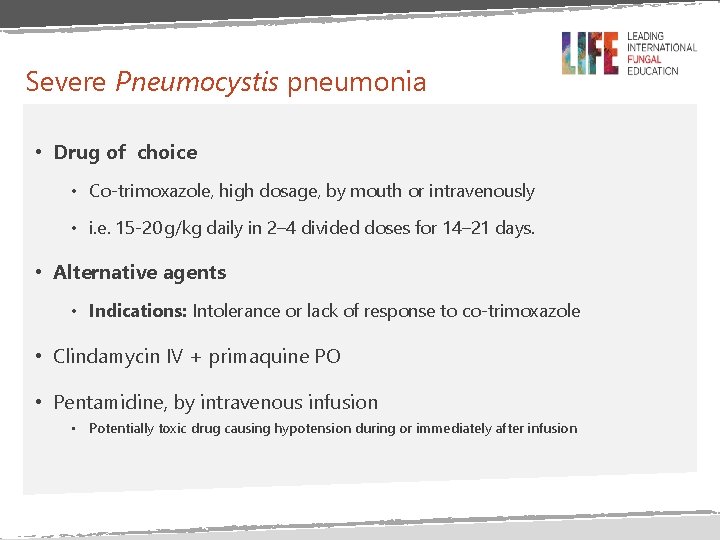
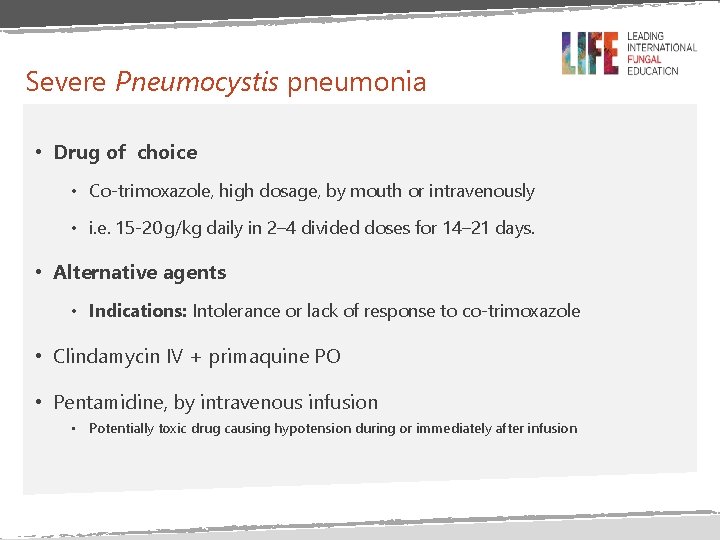
Severe Pneumocystis pneumonia • Drug of choice • Co-trimoxazole, high dosage, by mouth or intravenously • i. e. 15 -20 g/kg daily in 2– 4 divided doses for 14– 21 days. • Alternative agents • Indications: Intolerance or lack of response to co-trimoxazole • Clindamycin IV + primaquine PO • Pentamidine, by intravenous infusion • Potentially toxic drug causing hypotension during or immediately after infusion
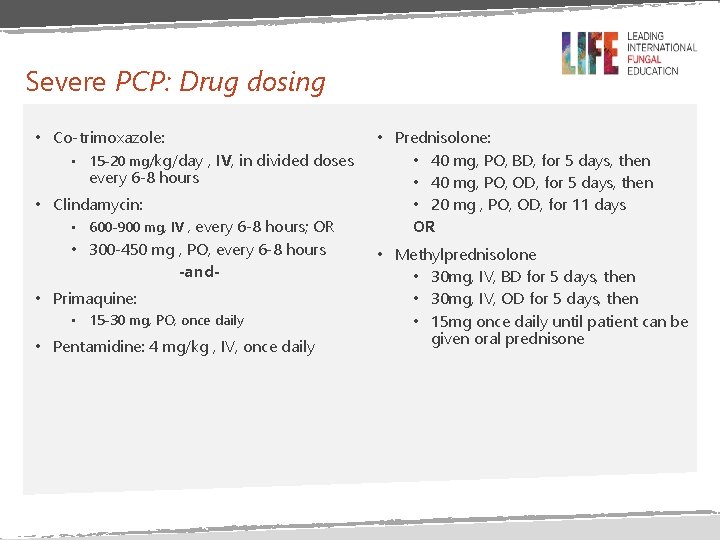
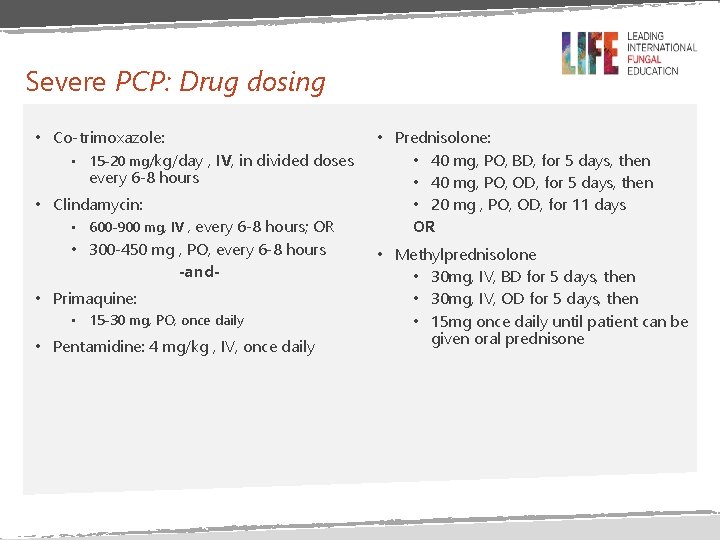
Severe PCP: Drug dosing • Co-trimoxazole: • 15 -20 mg/kg/day , IV, in divided doses every 6 -8 hours • Clindamycin: • 600 -900 mg, IV , every 6 -8 hours; OR • 300 -450 mg , PO, every 6 -8 hours -and • Primaquine: • 15 -30 mg, PO, once daily • Pentamidine: 4 mg/kg , IV, once daily • Prednisolone: • 40 mg, PO, BD, for 5 days, then • 40 mg, PO, OD, for 5 days, then • 20 mg , PO, OD, for 11 days OR • Methylprednisolone • 30 mg, IV, BD for 5 days, then • 30 mg, IV, OD for 5 days, then • 15 mg once daily until patient can be given oral prednisone
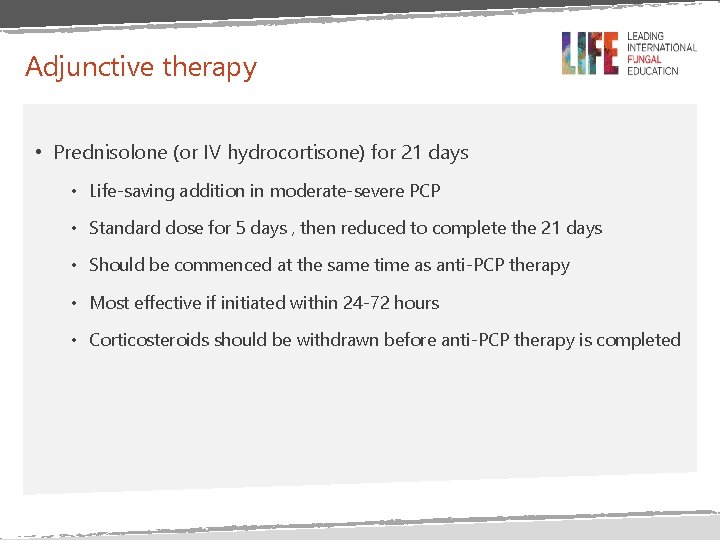
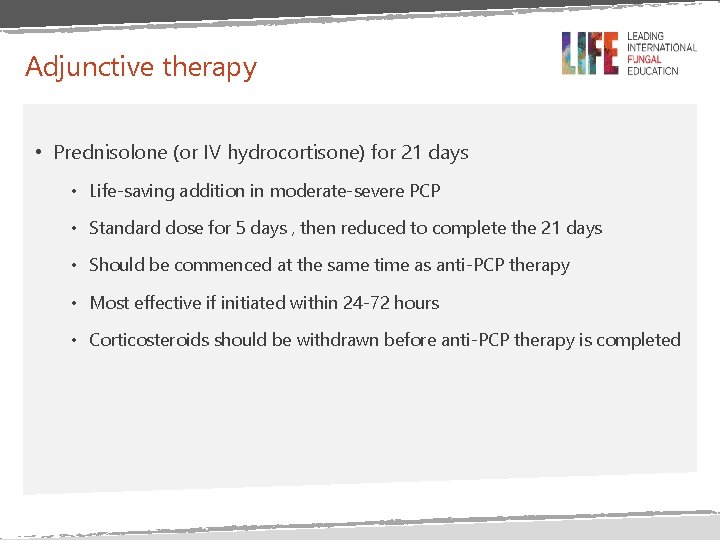
Adjunctive therapy • Prednisolone (or IV hydrocortisone) for 21 days • Life-saving addition in moderate-severe PCP • Standard dose for 5 days , then reduced to complete the 21 days • Should be commenced at the same time as anti-PCP therapy • Most effective if initiated within 24 -72 hours • Corticosteroids should be withdrawn before anti-PCP therapy is completed
PCP prophylaxis
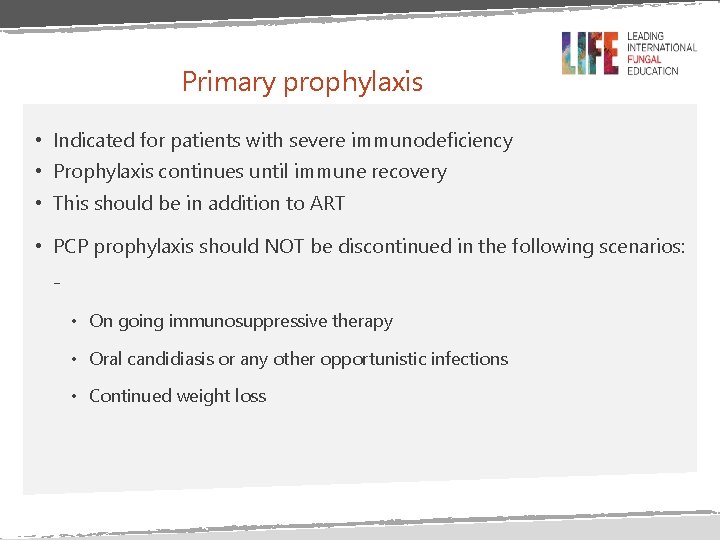
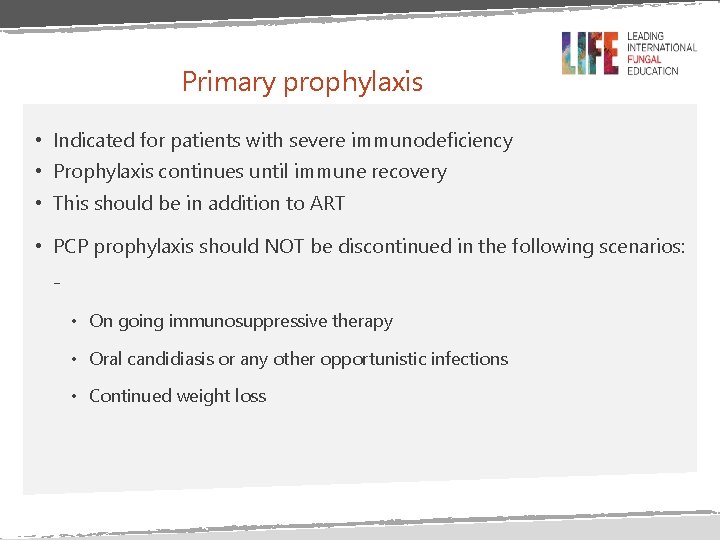
Primary prophylaxis • Indicated for patients with severe immunodeficiency • Prophylaxis continues until immune recovery • This should be in addition to ART • PCP prophylaxis should NOT be discontinued in the following scenarios: • On going immunosuppressive therapy • Oral candidiasis or any other opportunistic infections • Continued weight loss
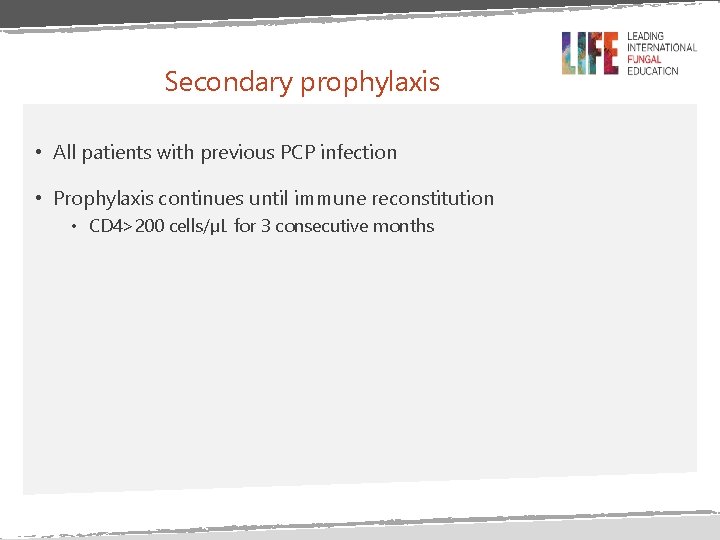
Secondary prophylaxis • All patients with previous PCP infection • Prophylaxis continues until immune reconstitution • CD 4>200 cells/µL for 3 consecutive months
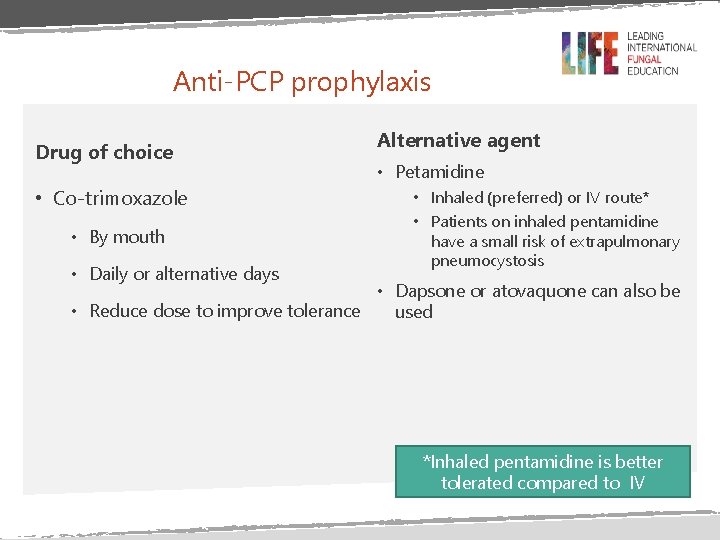
Anti-PCP prophylaxis Drug of choice • Co-trimoxazole • By mouth • Daily or alternative days Alternative agent • Petamidine • Inhaled (preferred) or IV route* • Patients on inhaled pentamidine have a small risk of extrapulmonary pneumocystosis • Dapsone or atovaquone can also be • Reduce dose to improve tolerance used *Inhaled pentamidine is better tolerated compared to IV
Summary • Pneumocystis jirovecii pneumonia (PCP) is the most common AIDSdefining opportunistic infection associated with significant morbidity and mortality • The clinical manifestation tend to be insidious in HIV-infected patients but rapidly progressive and severe in HIV-negative patients • Cotrimoxazole is the drug of choice for primary and secondary prophylaxis, and treatment of PCP • Alternative agents are used in case of lack of response to cotrimoxazole or intolerance to it

END