Pattern Recognition For Muscle Diseases With Case Examples

- Slides: 63
Pattern Recognition For Muscle Diseases, With Case Examples KUMC Neurology/Neurosurgery Grand Rounds April 7 th 2017 Richard J. Barohn, M. D. Chair, Department of Neurology Gertrude and Dewey Ziegler Professor of Neurology University Distinguished Professor Vice Chancellor for Research President, Research Istitute University of Kansas Medical Center Kansas City, KS 1
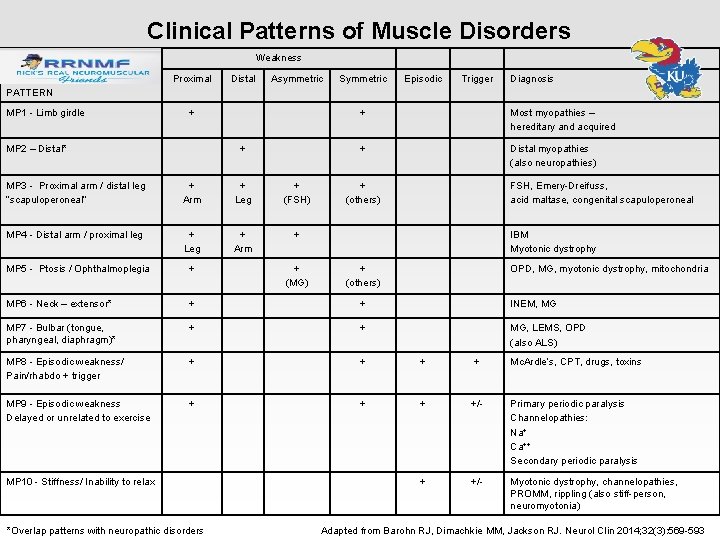
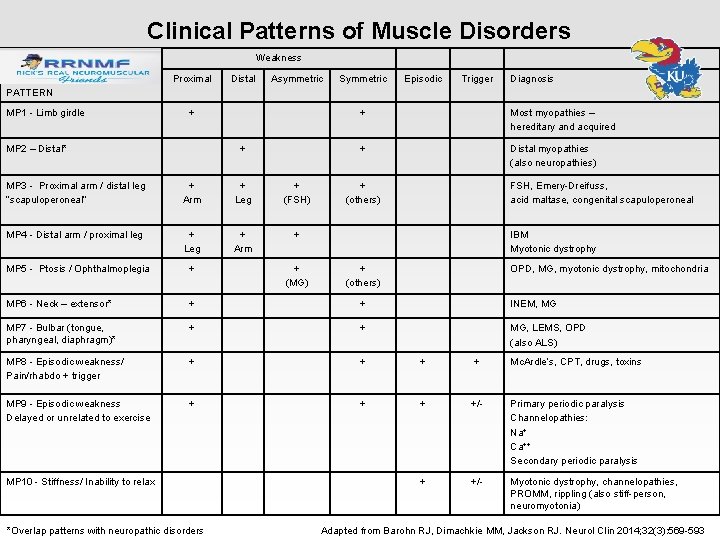
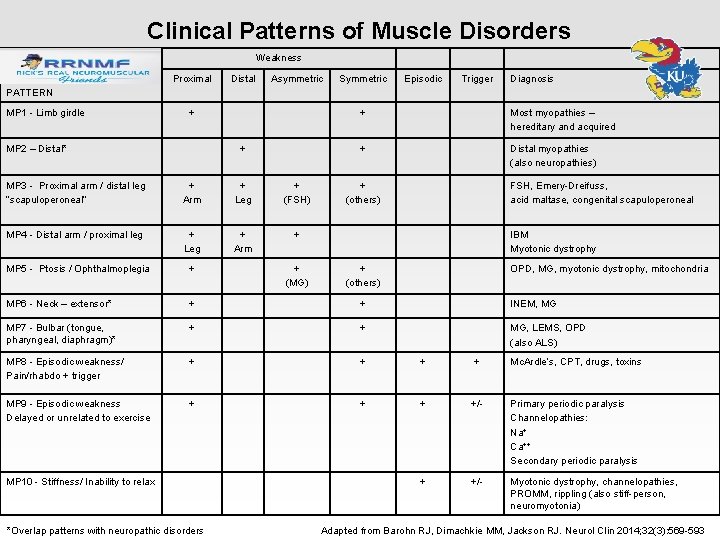
Clinical Patterns of Muscle Disorders Weakness Proximal Distal Asymmetric Symmetric Episodic Trigger Diagnosis PATTERN MP 1 - Limb girdle + MP 2 – Distal* + MP 3 - Proximal arm / distal leg “scapuloperoneal” + Arm + Leg + (FSH) MP 4 - Distal arm / proximal leg + Leg + Arm + Most myopathies – hereditary and acquired + Distal myopathies (also neuropathies) + (others) FSH, Emery-Dreifuss, acid maltase, congenital scapuloperoneal IBM Myotonic dystrophy MP 5 - Ptosis / Ophthalmoplegia + MP 6 - Neck – extensor* + + INEM, MG MP 7 - Bulbar (tongue, pharyngeal, diaphragm)* + + MG, LEMS, OPD (also ALS) MP 8 - Episodic weakness/ Pain/rhabdo + trigger + + Mc. Ardle’s, CPT, drugs, toxins MP 9 - Episodic weakness Delayed or unrelated to exercise + +/- Primary periodic paralysis Channelopathies: Na+ Ca++ Secondary periodic paralysis + +/- Myotonic dystrophy, channelopathies, PROMM, rippling (also stiff-person, neuromyotonia) MP 10 - Stiffness/ Inability to relax + (MG) + + (others) OPD, MG, myotonic dystrophy, mitochondria *Overlap patterns with neuropathic disorders Adapted from Barohn RJ, Dimachkie MM, Jackson RJ. Neurol Clin 2014; 32(3): 569 -593
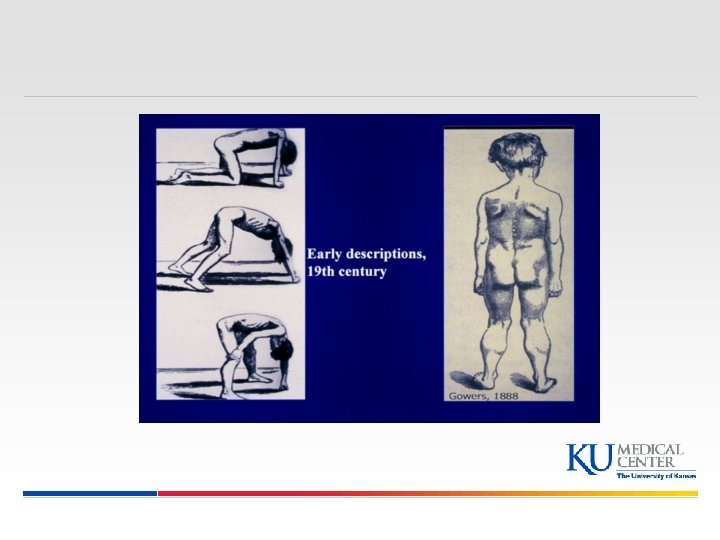
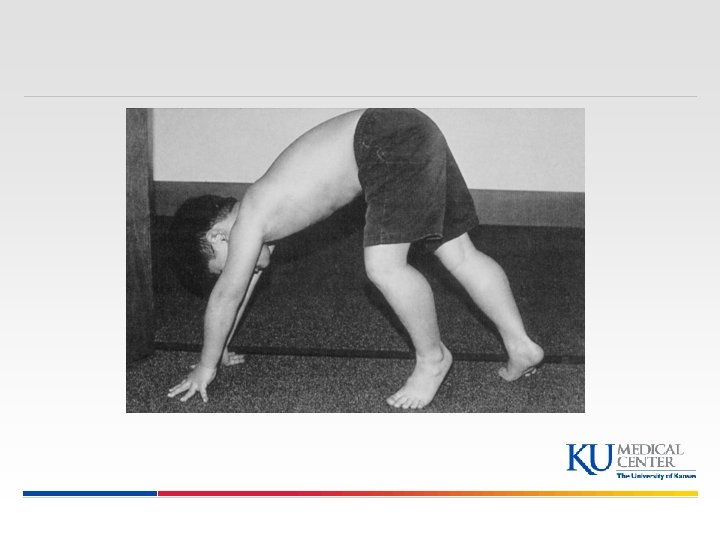
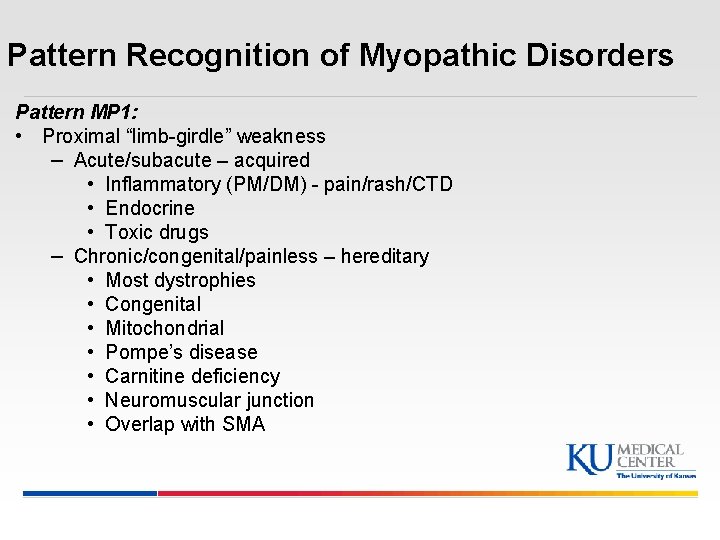
Pattern Recognition of Myopathic Disorders Pattern MP 1: • Proximal “limb-girdle” weakness – Acute/subacute – acquired • Inflammatory (PM/DM) - pain/rash/CTD • Endocrine • Toxic drugs – Chronic/congenital/painless – hereditary • Most dystrophies • Congenital • Mitochondrial • Pompe’s disease • Carnitine deficiency • Neuromuscular junction • Overlap with SMA
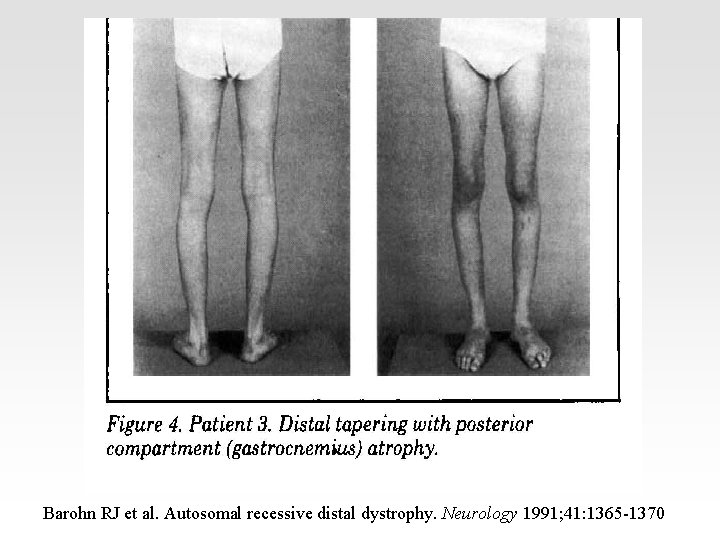
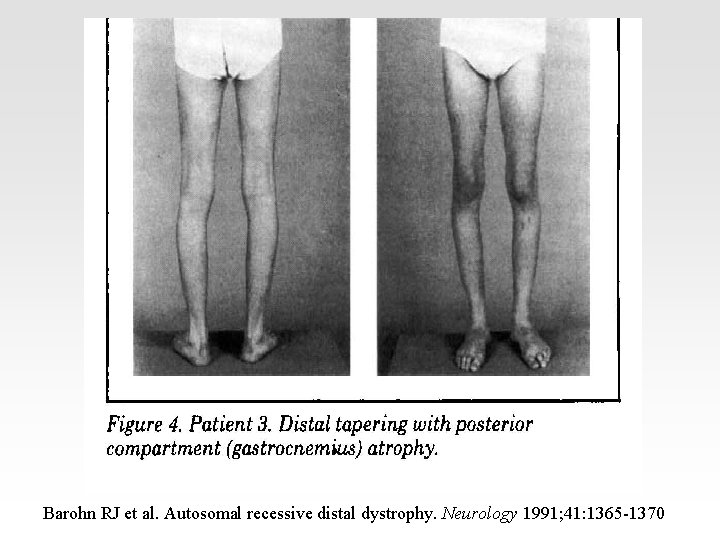
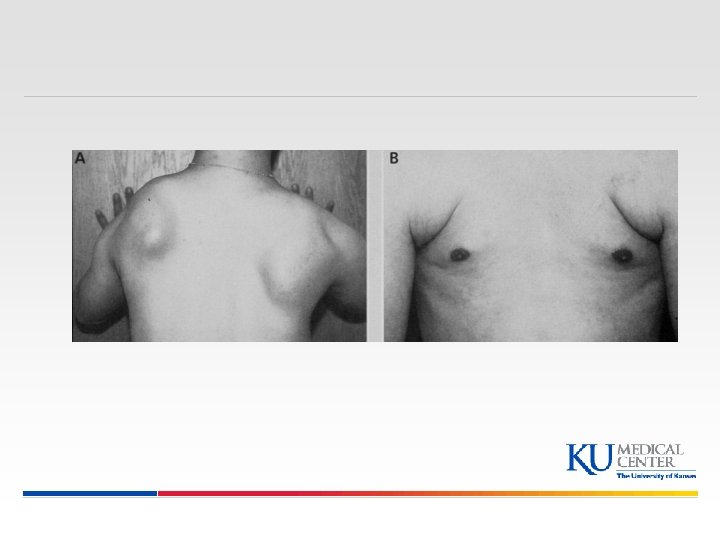
Barohn RJ et al. Autosomal recessive distal dystrophy. Neurology 1991; 41: 1365 -1370
Pattern Recognition of Myopathic Disorders Pattern MP 2: § Distal weakness Distal muscular dystrophies: • Late adult onset, AD: Welander (TIA 1); Markesbery (2 asp); Udd (titin) • Early adult onset, AR: Nonaka (GNE myopathy); Miyoshi (dysferlin); Laing (myosin) § Myofibrillar (Desmin) myopathy § IBM with paget disease (VCP) § Myotonic dystrophy § Congenital myopathies § Other: NMJ disease - MG, congenital MG § Overlap with CMT/hereditary motor neuropathy Dimachkie MM, Barohn RJ. Neurol Clin. 2014; 32(3): 817 -42
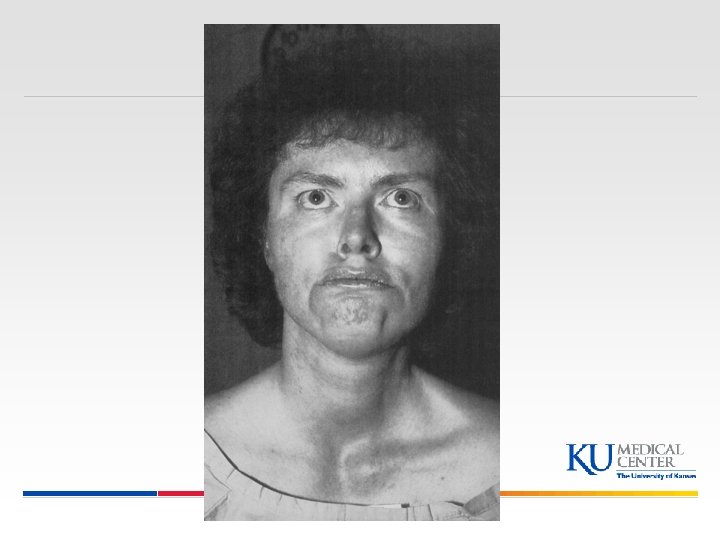
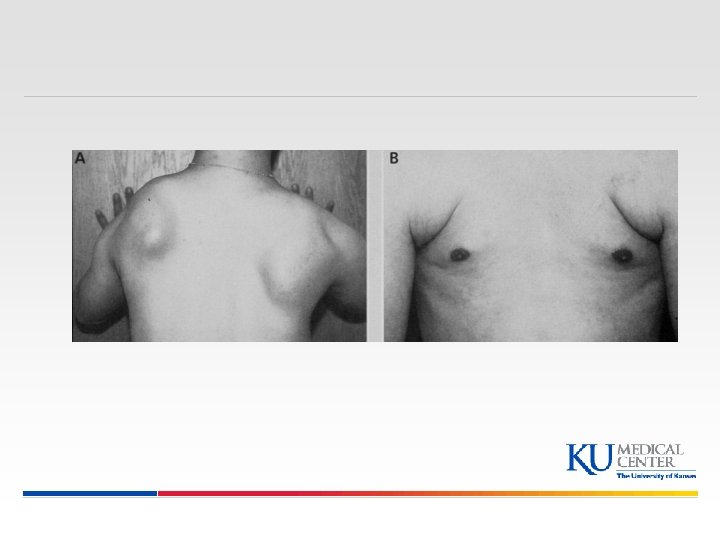
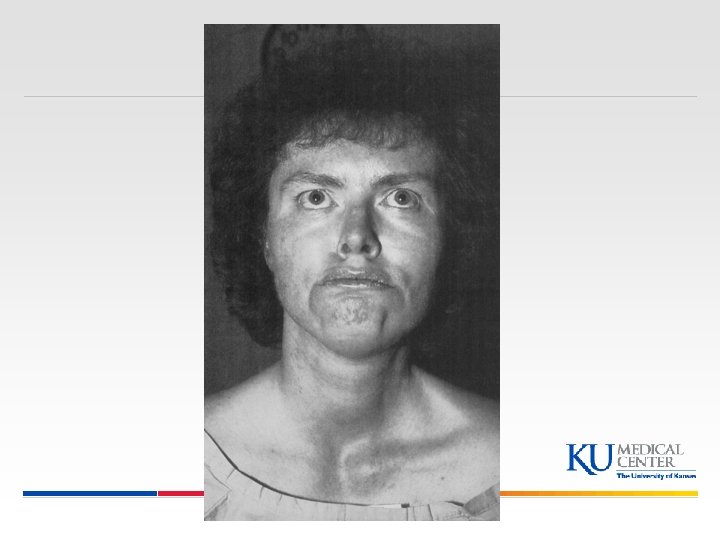
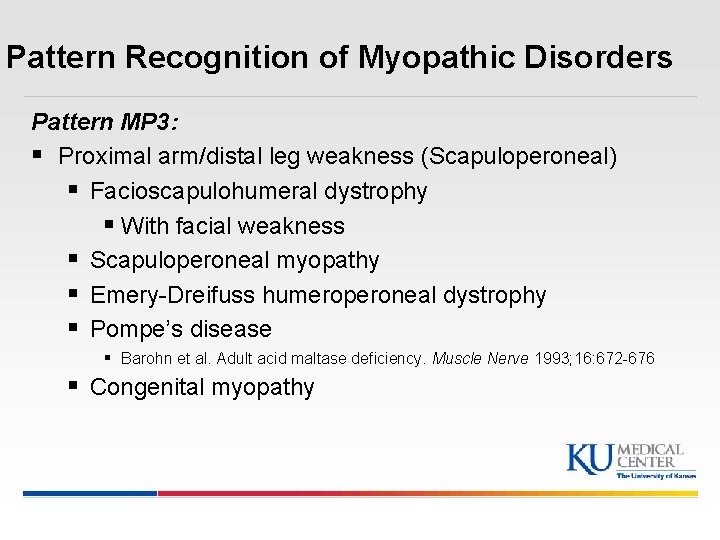
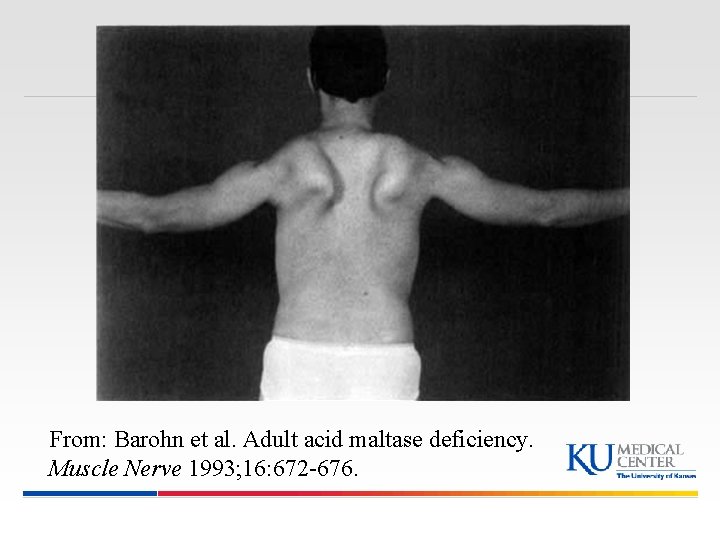
Pattern Recognition of Myopathic Disorders Pattern MP 3: § Proximal arm/distal leg weakness (Scapuloperoneal) § Facioscapulohumeral dystrophy § With facial weakness § Scapuloperoneal myopathy § Emery-Dreifuss humeroperoneal dystrophy § Pompe’s disease § Barohn et al. Adult acid maltase deficiency. Muscle Nerve 1993; 16: 672 -676 § Congenital myopathy
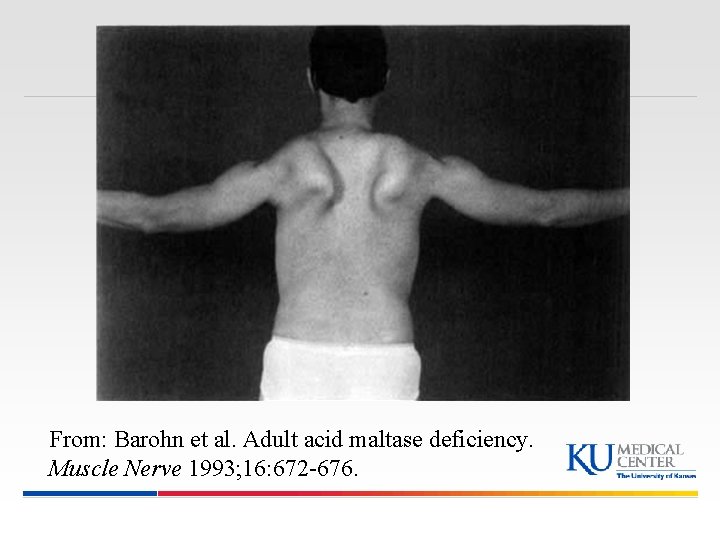
From: Barohn et al. Adult acid maltase deficiency. Muscle Nerve 1993; 16: 672 -676.
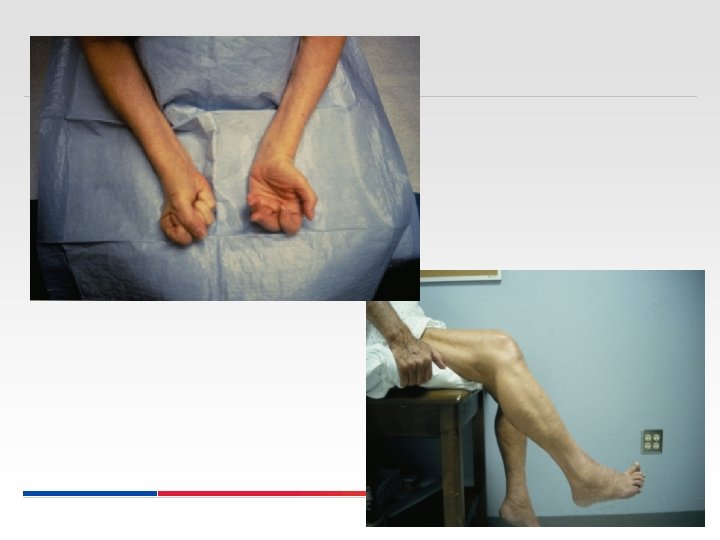
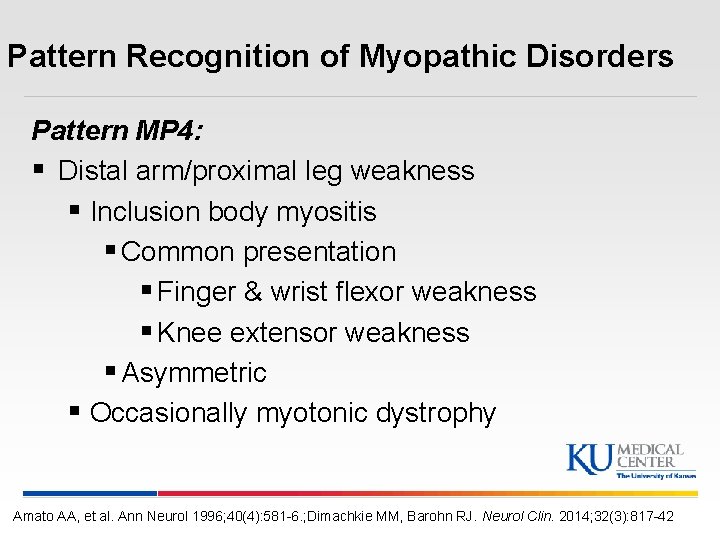
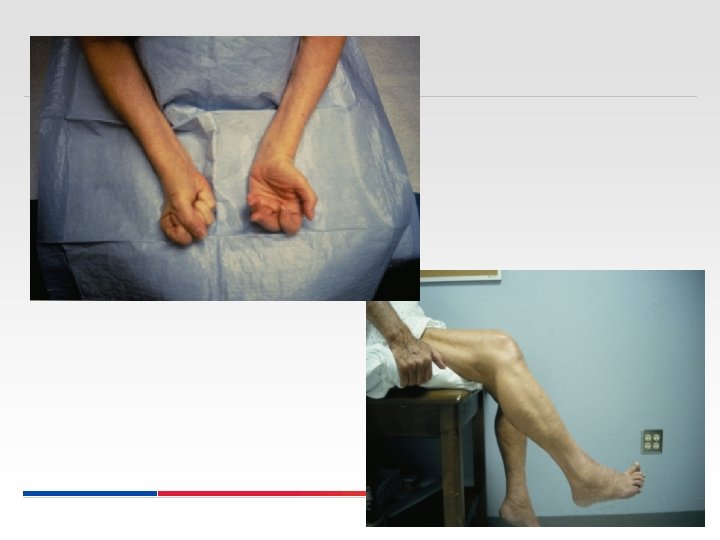
Pattern Recognition of Myopathic Disorders Pattern MP 4: § Distal arm/proximal leg weakness § Inclusion body myositis § Common presentation § Finger & wrist flexor weakness § Knee extensor weakness § Asymmetric § Occasionally myotonic dystrophy Amato AA, et al. Ann Neurol 1996; 40(4): 581 -6. ; Dimachkie MM, Barohn RJ. Neurol Clin. 2014; 32(3): 817 -42
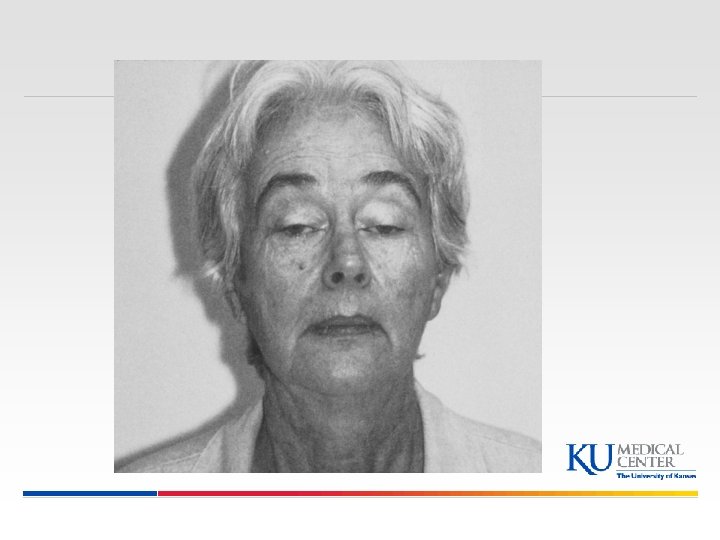
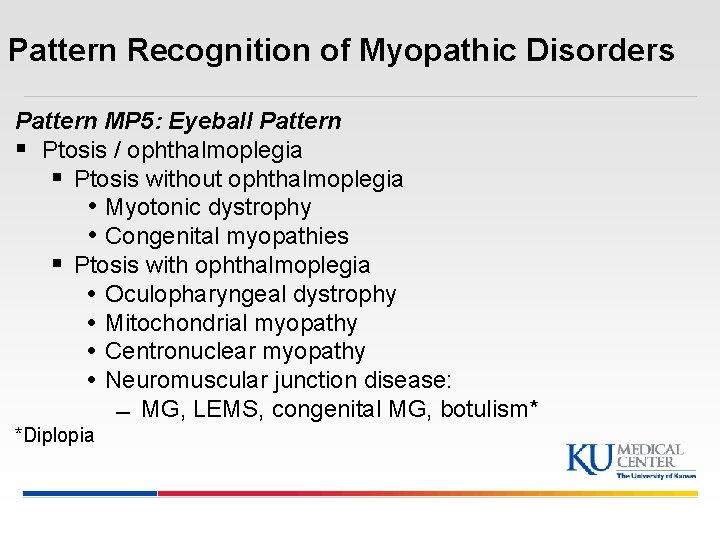
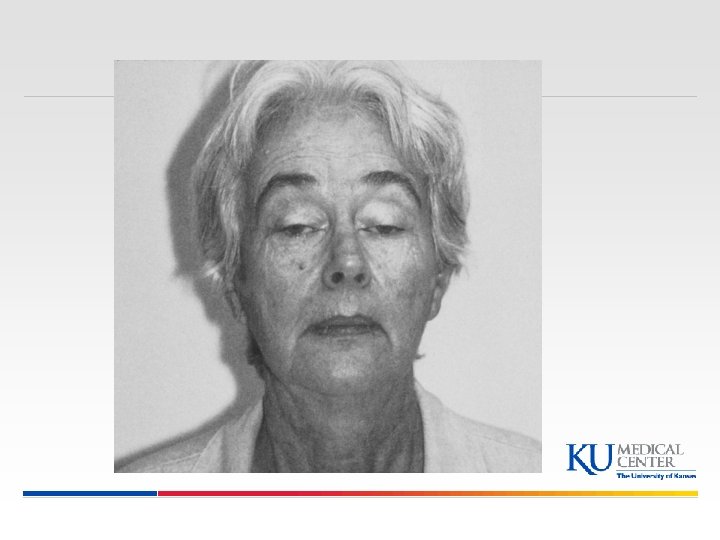
Pattern Recognition of Myopathic Disorders Pattern MP 5: Eyeball Pattern § Ptosis / ophthalmoplegia § Ptosis without ophthalmoplegia • Myotonic dystrophy • Congenital myopathies § Ptosis with ophthalmoplegia • Oculopharyngeal dystrophy • Mitochondrial myopathy • Centronuclear myopathy • Neuromuscular junction disease: MG, LEMS, congenital MG, botulism* *Diplopia
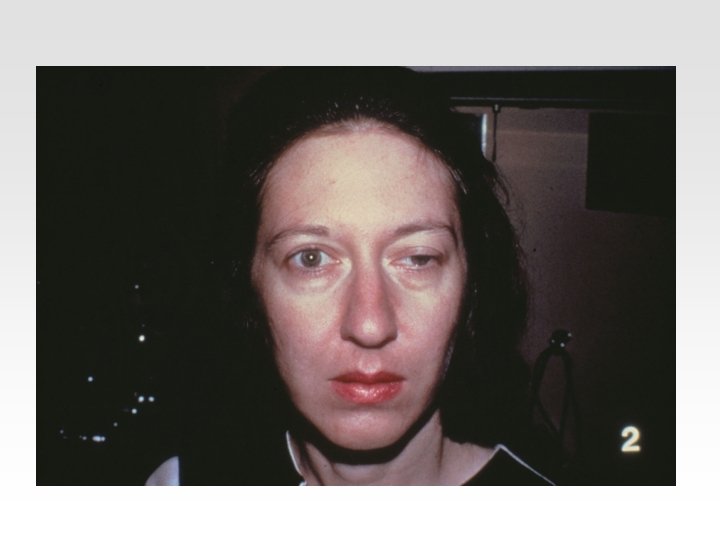
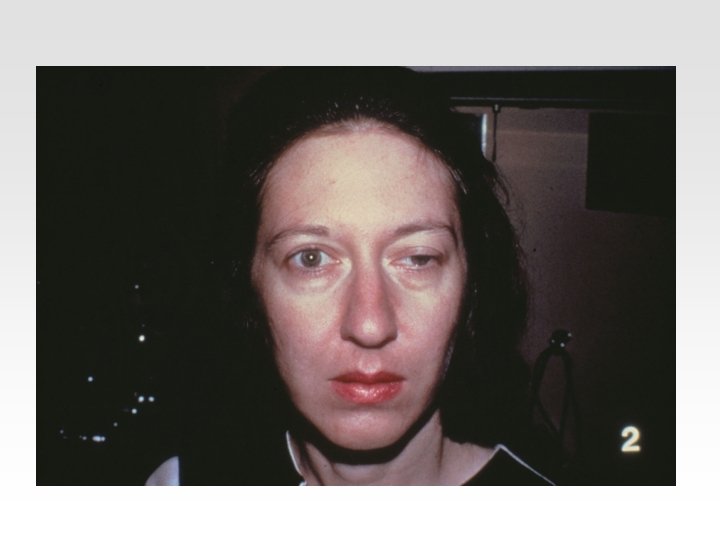
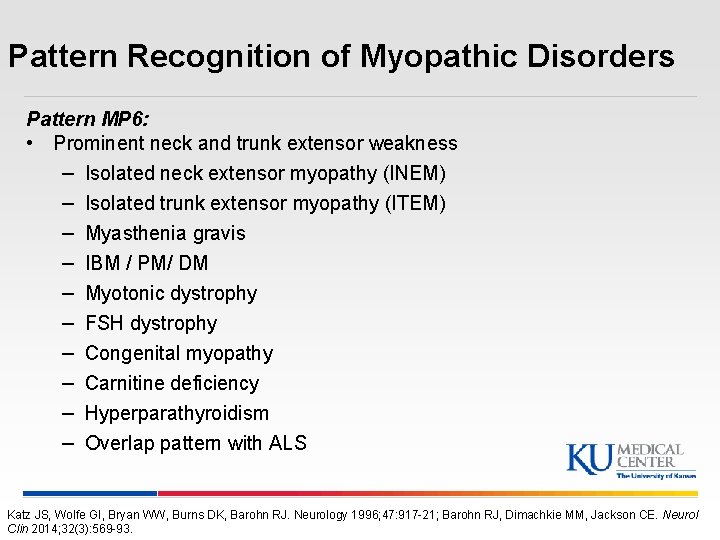
Pattern Recognition of Myopathic Disorders Pattern MP 6: • Prominent neck and trunk extensor weakness – – – – – Isolated neck extensor myopathy (INEM) Isolated trunk extensor myopathy (ITEM) Myasthenia gravis IBM / PM/ DM Myotonic dystrophy FSH dystrophy Congenital myopathy Carnitine deficiency Hyperparathyroidism Overlap pattern with ALS Katz JS, Wolfe GI, Bryan WW, Burns DK, Barohn RJ. Neurology 1996; 47: 917 -21; Barohn RJ, Dimachkie MM, Jackson CE. Neurol Clin 2014; 32(3): 569 -93.

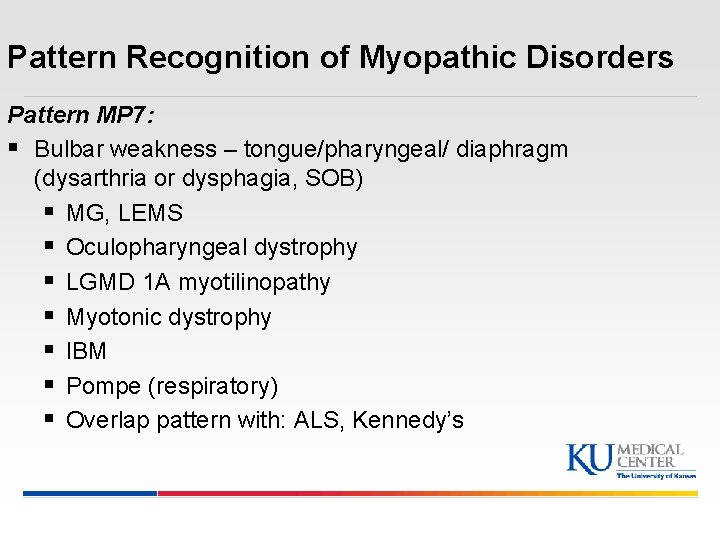
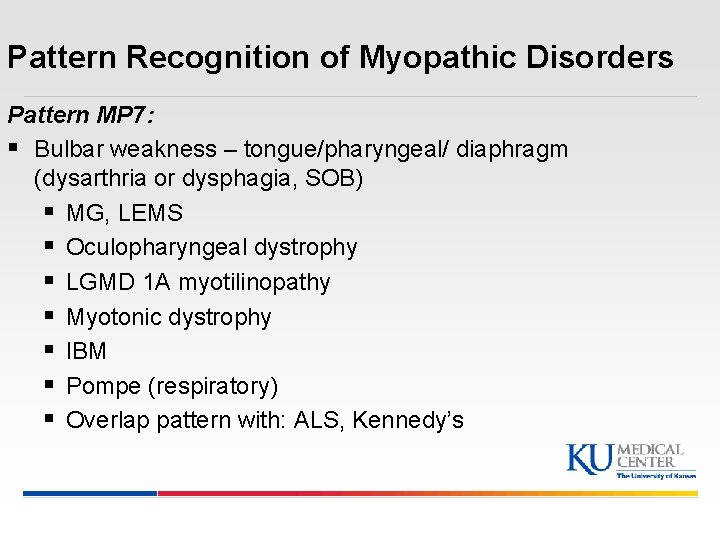
Pattern Recognition of Myopathic Disorders Pattern MP 7: § Bulbar weakness – tongue/pharyngeal/ diaphragm (dysarthria or dysphagia, SOB) § MG, LEMS § Oculopharyngeal dystrophy § LGMD 1 A myotilinopathy § Myotonic dystrophy § IBM § Pompe (respiratory) § Overlap pattern with: ALS, Kennedy’s
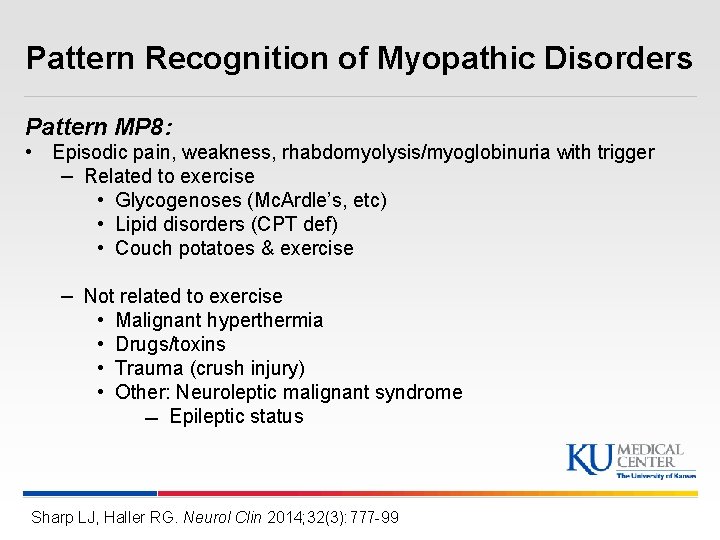
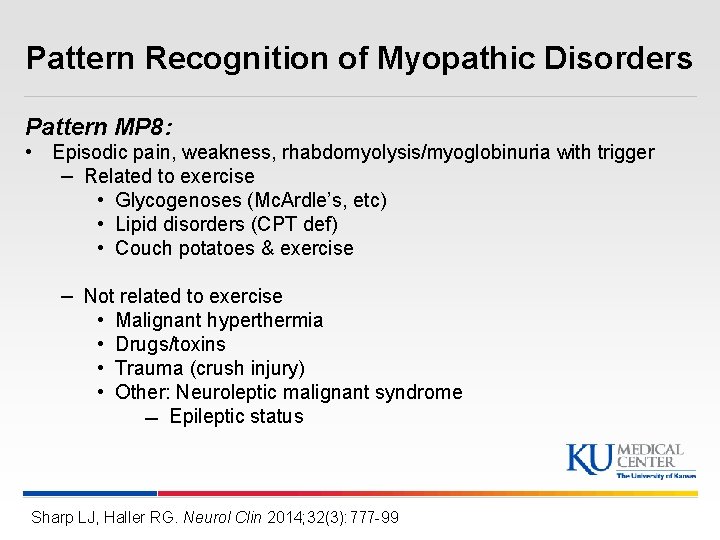
Pattern Recognition of Myopathic Disorders Pattern MP 8: • Episodic pain, weakness, rhabdomyolysis/myoglobinuria with trigger – Related to exercise • Glycogenoses (Mc. Ardle’s, etc) • Lipid disorders (CPT def) • Couch potatoes & exercise – Not related to exercise • Malignant hyperthermia • Drugs/toxins • Trauma (crush injury) • Other: Neuroleptic malignant syndrome Epileptic status Sharp LJ, Haller RG. Neurol Clin 2014; 32(3): 777 -99
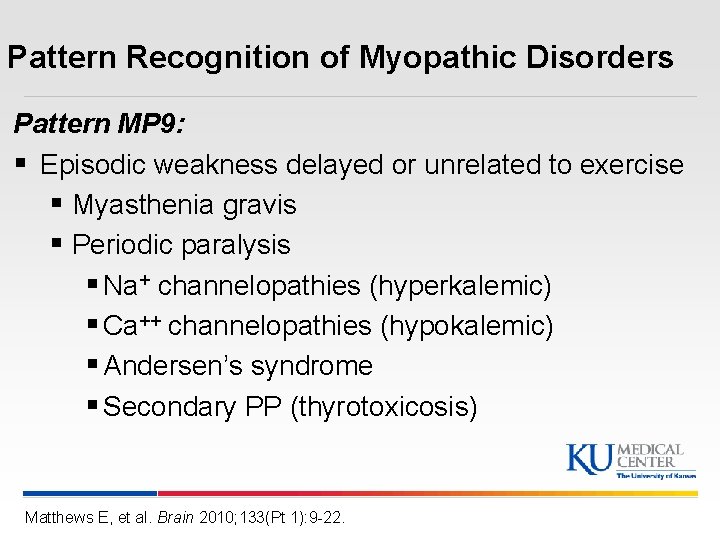
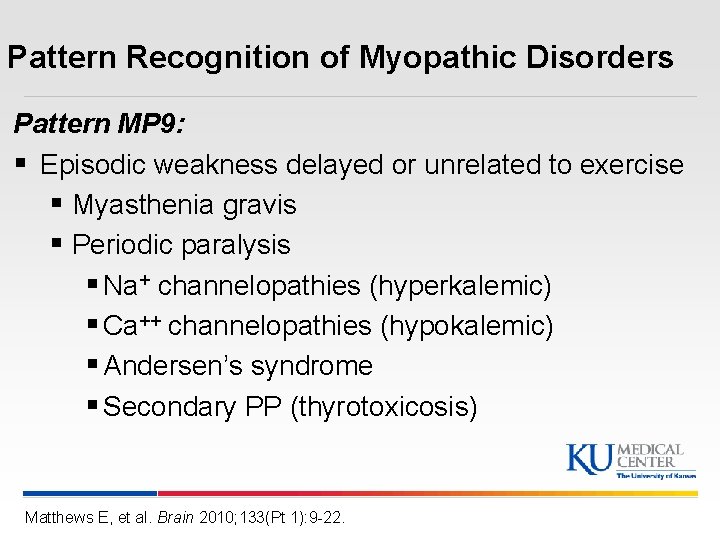
Pattern Recognition of Myopathic Disorders Pattern MP 9: § Episodic weakness delayed or unrelated to exercise § Myasthenia gravis § Periodic paralysis § Na+ channelopathies (hyperkalemic) § Ca++ channelopathies (hypokalemic) § Andersen’s syndrome § Secondary PP (thyrotoxicosis) Matthews E, et al. Brain 2010; 133(Pt 1): 9 -22.
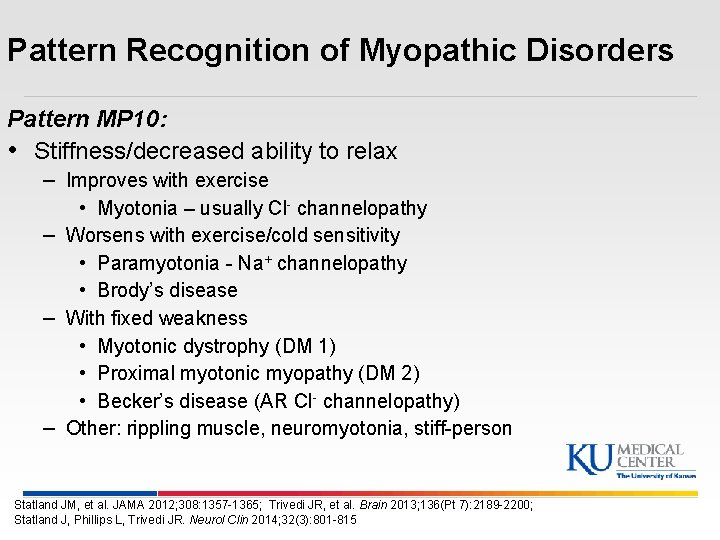
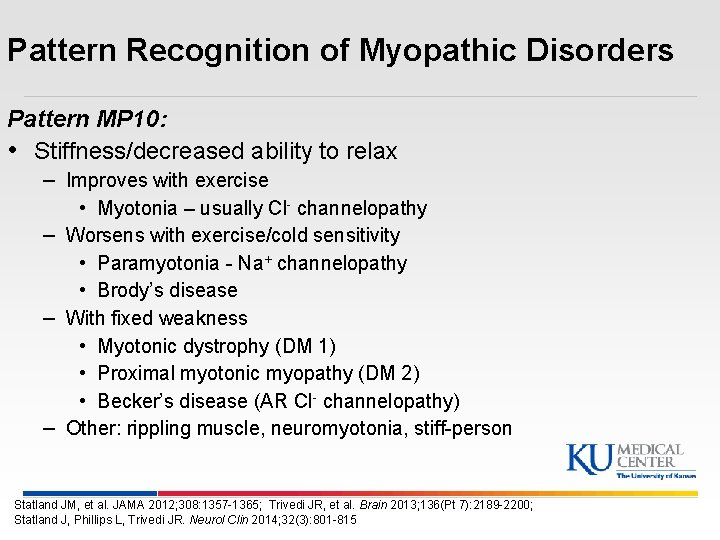
Pattern Recognition of Myopathic Disorders Pattern MP 10: • Stiffness/decreased ability to relax – Improves with exercise • Myotonia – usually Cl- channelopathy – Worsens with exercise/cold sensitivity • Paramyotonia - Na+ channelopathy • Brody’s disease – With fixed weakness • Myotonic dystrophy (DM 1) • Proximal myotonic myopathy (DM 2) • Becker’s disease (AR Cl- channelopathy) – Other: rippling muscle, neuromyotonia, stiff-person Statland JM, et al. JAMA 2012; 308: 1357 -1365; Trivedi JR, et al. Brain 2013; 136(Pt 7): 2189 -2200; Statland J, Phillips L, Trivedi JR. Neurol Clin 2014; 32(3): 801 -815
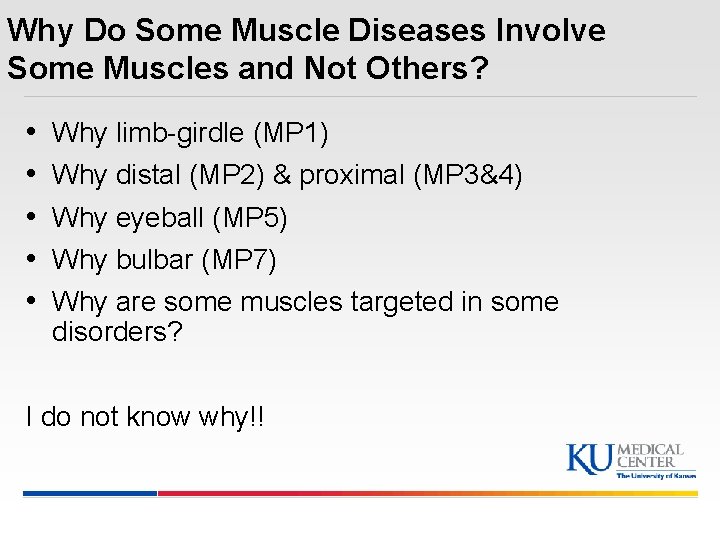
Why Do Some Muscle Diseases Involve Some Muscles and Not Others? • • • Why limb-girdle (MP 1) Why distal (MP 2) & proximal (MP 3&4) Why eyeball (MP 5) Why bulbar (MP 7) Why are some muscles targeted in some disorders? I do not know why!!
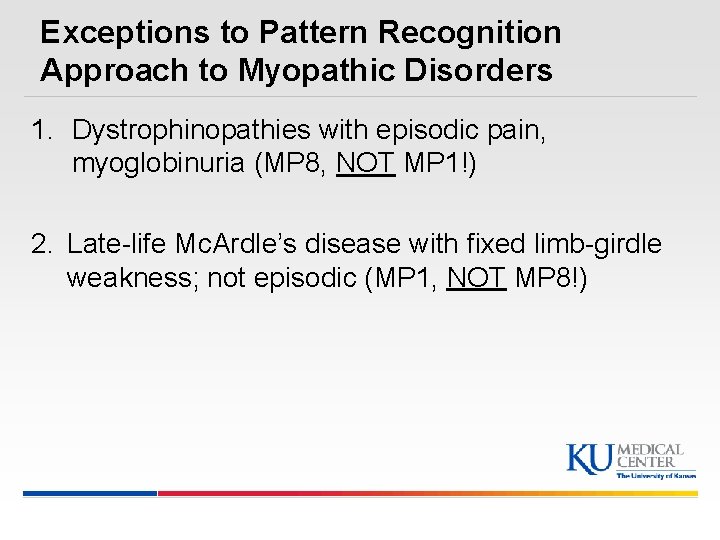
Exceptions to Pattern Recognition Approach to Myopathic Disorders 1. Dystrophinopathies with episodic pain, myoglobinuria (MP 8, NOT MP 1!) 2. Late-life Mc. Ardle’s disease with fixed limb-girdle weakness; not episodic (MP 1, NOT MP 8!)
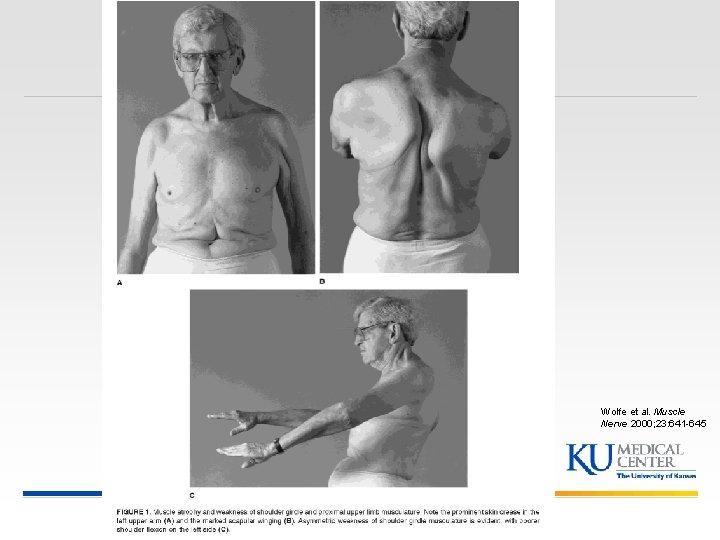
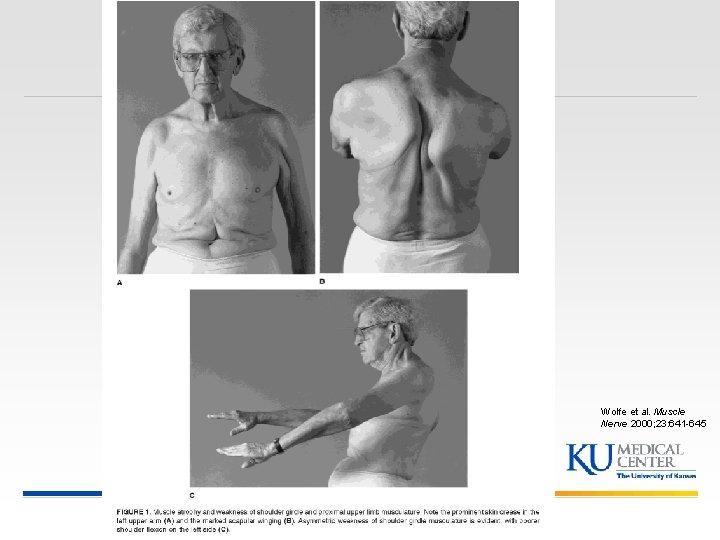
Wolfe et al. Muscle Nerve 2000; 23: 641 -645
Laboratory Evaluation of Myopathic Disorders § Serum creatine kinase § Others: AST, ALT, LDH, Aldolase § Electrolytes, thyroid functions § Serum antibodies § Needle EMG § NCS exercise tests § Muscle biopsy: open vs. needle § Molecular genetic studies § Ischemic forearm test § Urine for myoglobin § Muscle imaging
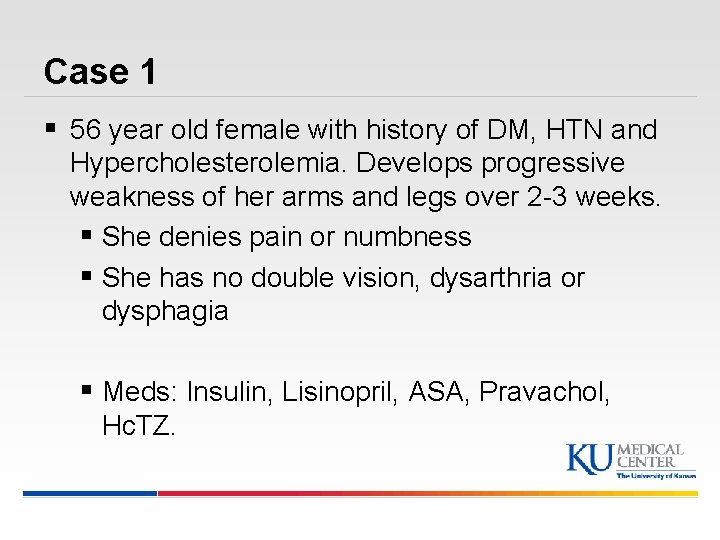
Case 1 § 56 year old female with history of DM, HTN and Hypercholesterolemia. Develops progressive weakness of her arms and legs over 2 -3 weeks. § She denies pain or numbness § She has no double vision, dysarthria or dysphagia § Meds: Insulin, Lisinopril, ASA, Pravachol, Hc. TZ.
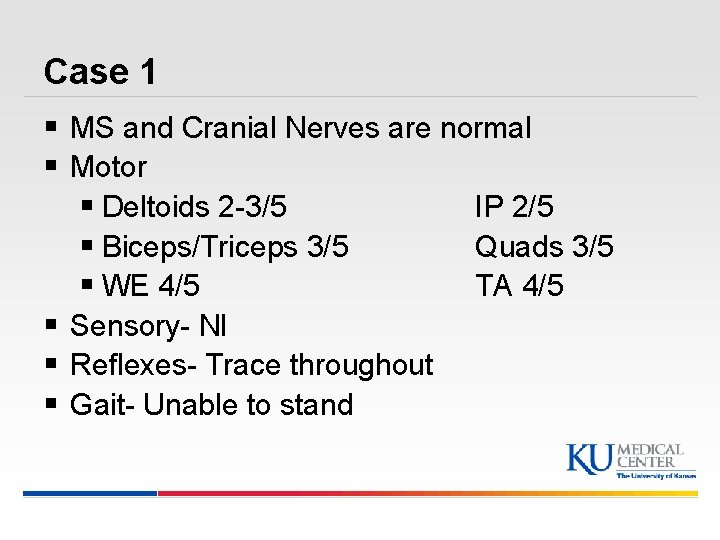
Case 1 § MS and Cranial Nerves are normal § Motor § Deltoids 2 -3/5 IP 2/5 § Biceps/Triceps 3/5 Quads 3/5 § WE 4/5 TA 4/5 § Sensory- Nl § Reflexes- Trace throughout § Gait- Unable to stand
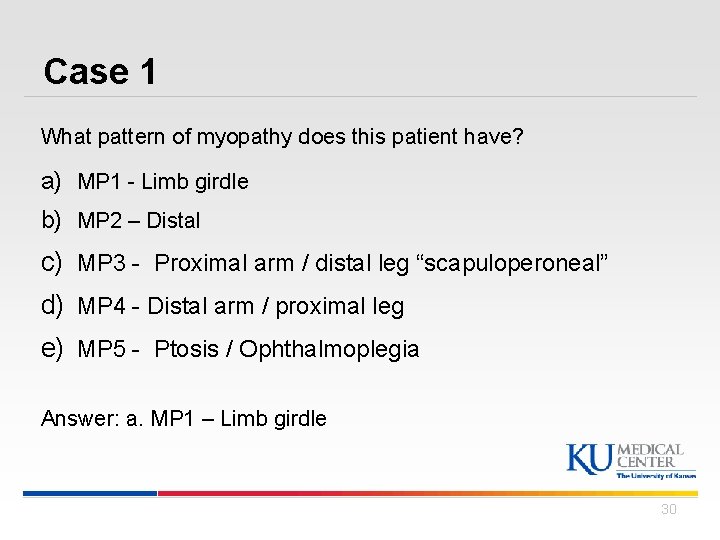
Case 1 What pattern of myopathy does this patient have? a) MP 1 - Limb girdle b) MP 2 – Distal c) MP 3 - Proximal arm / distal leg “scapuloperoneal” d) MP 4 - Distal arm / proximal leg e) MP 5 - Ptosis / Ophthalmoplegia Answer: a. MP 1 – Limb girdle 30
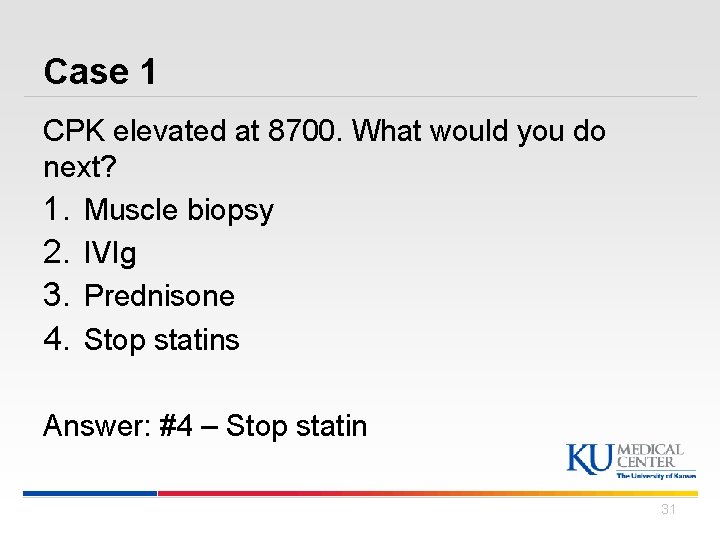
Case 1 CPK elevated at 8700. What would you do next? 1. Muscle biopsy 2. IVIg 3. Prednisone 4. Stop statins Answer: #4 – Stop statin 31
Case 1 § Statin is stopped and she is sent to SNF § 8 weeks later she has not gotten stronger and her CPK is still 4800 § Now what would you order? 1. Muscle Biopsy 2. Jo-1 Antibody and other muscle specific antibodies 3. HMGCR Antibody 4. Muscle MRI Answer: #3 – HMGCR Antibody
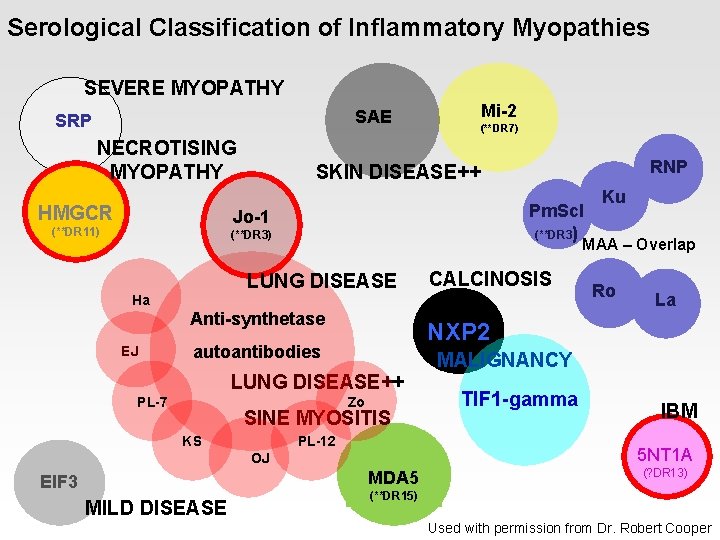
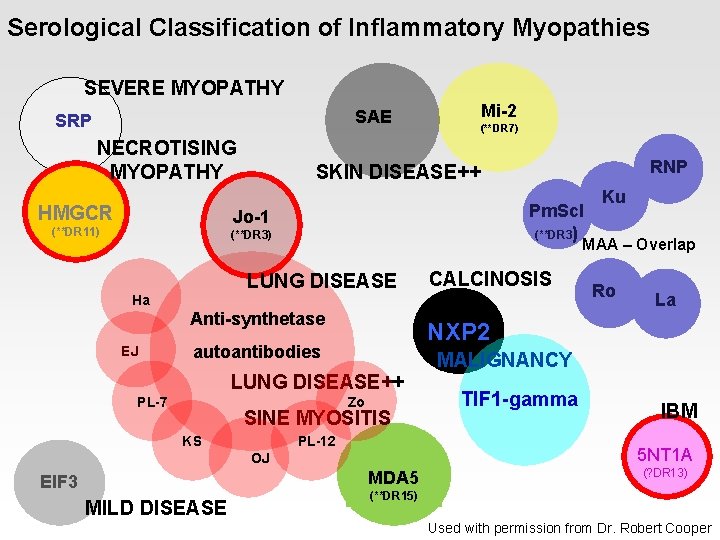
Serological Classification of Inflammatory Myopathies SEVERE MYOPATHY Mi-2 SAE SRP NECROTISING MYOPATHY HMGCR (**DR 7) Pm. Scl (**DR 3) Jo-1 (**DR 11) (**DR 3) Anti-synthetase EJ Zo SINE MYOSITIS PL-12 MDA 5 MILD DISEASE La TIF 1 -gamma IBM 5 NT 1 A OJ EIF 3 Ro MALIGNANCY LUNG DISEASE++ KS CALCINOSIS NXP 2 autoantibodies PL-7 Ku MAA – Overlap LUNG DISEASE Ha RNP SKIN DISEASE++ (? DR 13) (**DR 15) Used with permission from Dr. Robert Cooper
Case 1 § MSA- Normal § HMGCR Antibodies markedly elevated § Would you do muscle biopsy now? § Diagnosis? § Treatment?
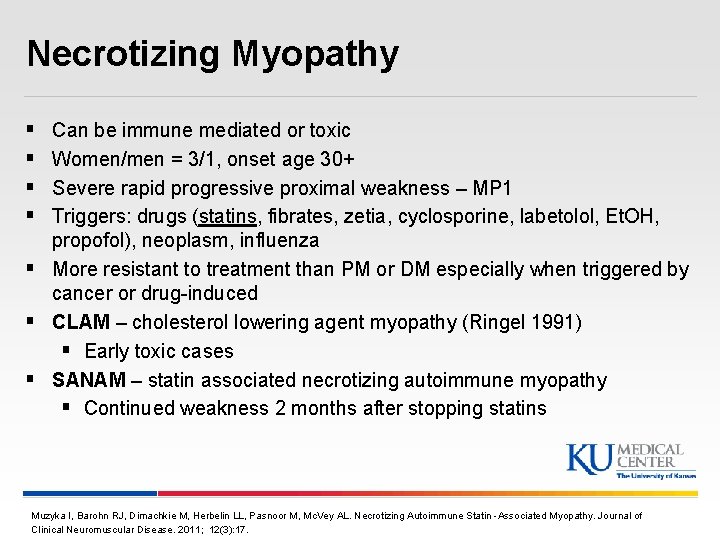
Necrotizing Myopathy § § Can be immune mediated or toxic Women/men = 3/1, onset age 30+ Severe rapid progressive proximal weakness – MP 1 Triggers: drugs (statins, fibrates, zetia, cyclosporine, labetolol, Et. OH, propofol), neoplasm, influenza § More resistant to treatment than PM or DM especially when triggered by cancer or drug-induced § CLAM – cholesterol lowering agent myopathy (Ringel 1991) § Early toxic cases § SANAM – statin associated necrotizing autoimmune myopathy § Continued weakness 2 months after stopping statins Muzyka I, Barohn RJ, Dimachkie M, Herbelin LL, Pasnoor M, Mc. Vey AL. Necrotizing Autoimmune Statin -Associated Myopathy. Journal of Clinical Neuromuscular Disease. 2011; 12(3): 17.
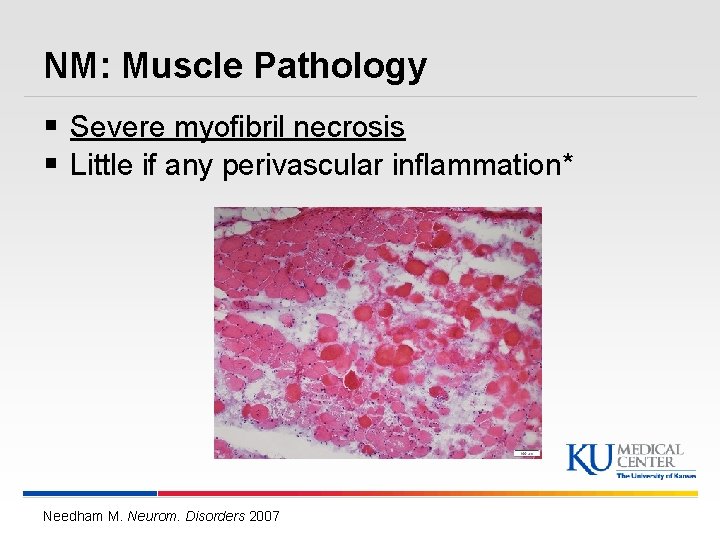
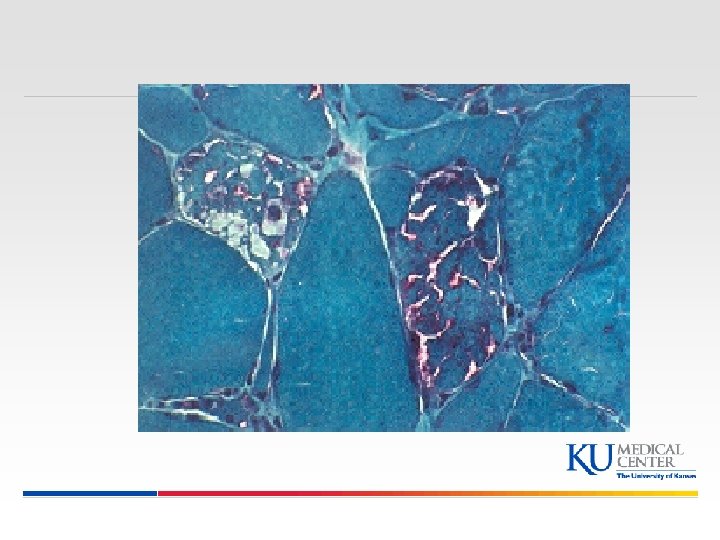
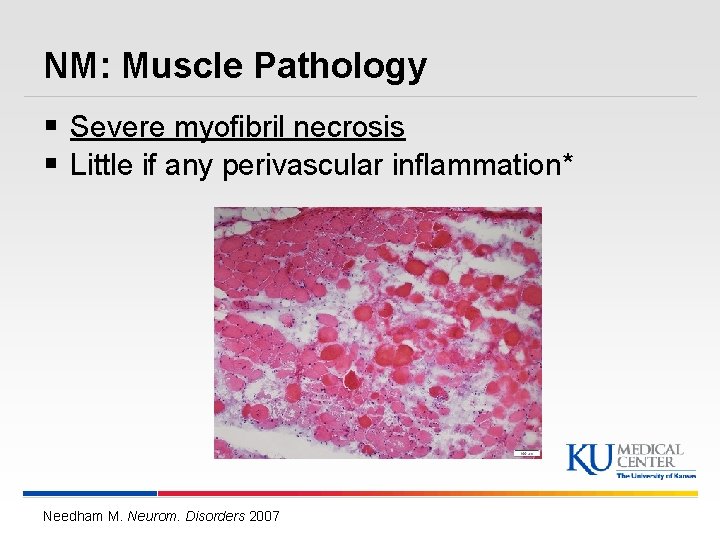
NM: Muscle Pathology § Severe myofibril necrosis § Little if any perivascular inflammation* Needham M. Neurom. Disorders 2007
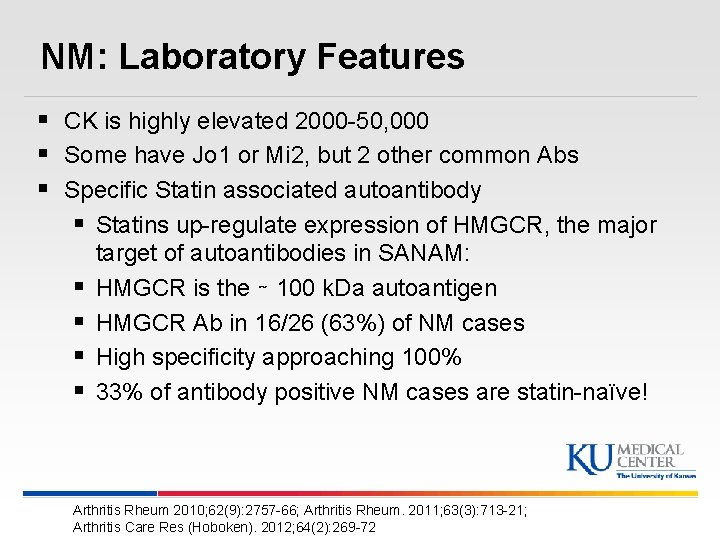
NM: Laboratory Features § CK is highly elevated 2000 -50, 000 § Some have Jo 1 or Mi 2, but 2 other common Abs § Specific Statin associated autoantibody § Statins up-regulate expression of HMGCR, the major § § target of autoantibodies in SANAM: HMGCR is the ∼ 100 k. Da autoantigen HMGCR Ab in 16/26 (63%) of NM cases High specificity approaching 100% 33% of antibody positive NM cases are statin-naïve! Arthritis Rheum 2010; 62(9): 2757 -66; Arthritis Rheum. 2011; 63(3): 713 -21; Arthritis Care Res (Hoboken). 2012; 64(2): 269 -72
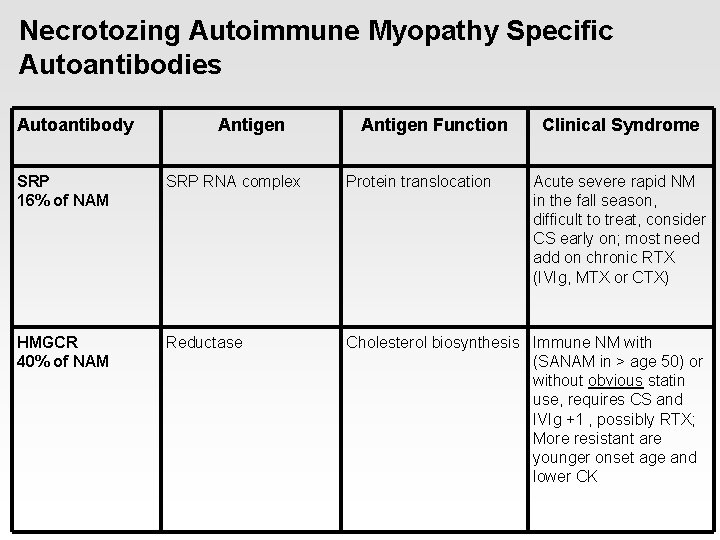
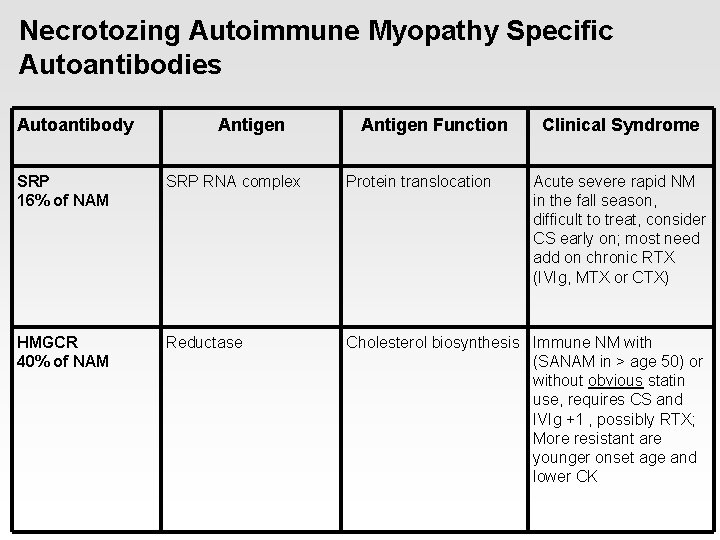
Necrotozing Autoimmune Myopathy Specific Autoantibodies Autoantibody Antigen Function Clinical Syndrome SRP 16% of NAM SRP RNA complex Protein translocation Acute severe rapid NM in the fall season, difficult to treat, consider CS early on; most need add on chronic RTX (IVIg, MTX or CTX) HMGCR 40% of NAM Reductase Cholesterol biosynthesis Immune NM with (SANAM in > age 50) or without obvious statin use, requires CS and IVIg +1 , possibly RTX; More resistant are younger onset age and lower CK
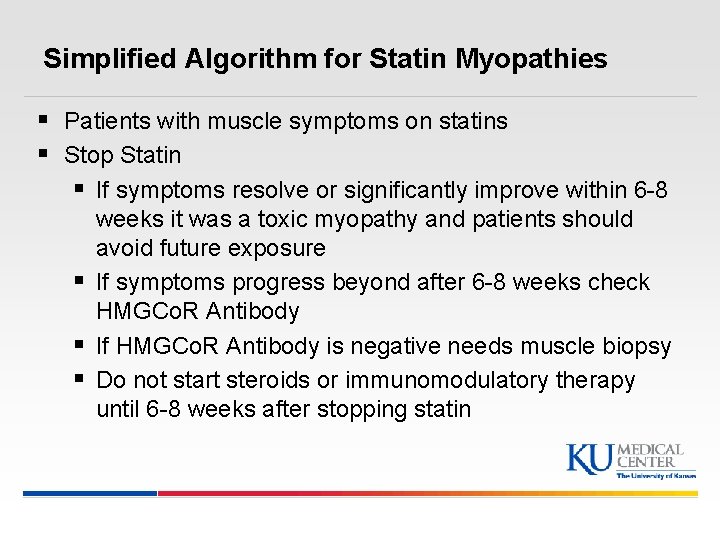
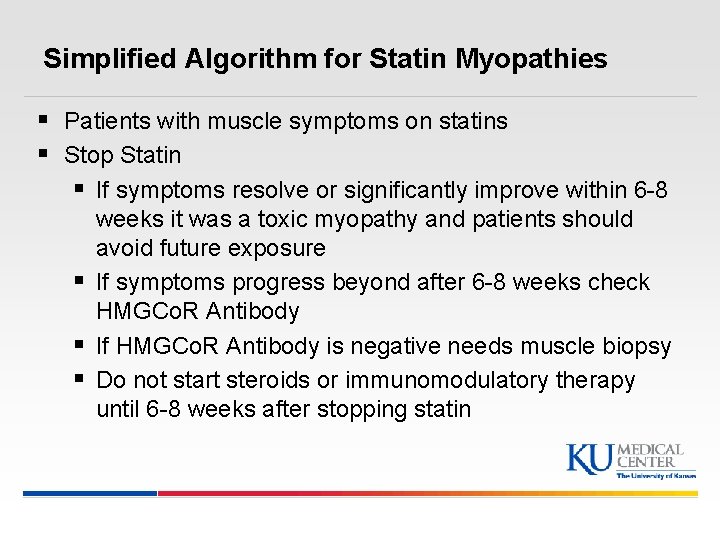
Simplified Algorithm for Statin Myopathies § Patients with muscle symptoms on statins § Stop Statin § If symptoms resolve or significantly improve within 6 -8 weeks it was a toxic myopathy and patients should avoid future exposure § If symptoms progress beyond after 6 -8 weeks check HMGCo. R Antibody § If HMGCo. R Antibody is negative needs muscle biopsy § Do not start steroids or immunomodulatory therapy until 6 -8 weeks after stopping statin
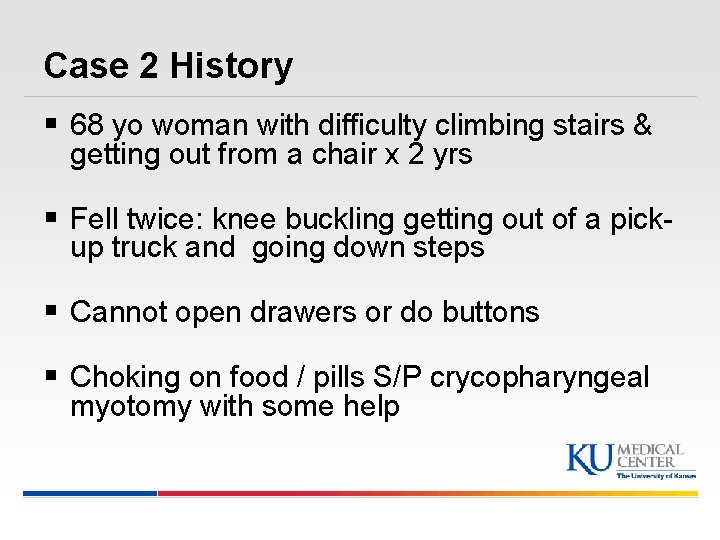
Case 2 History § 68 yo woman with difficulty climbing stairs & getting out from a chair x 2 yrs § Fell twice: knee buckling getting out of a pickup truck and going down steps § Cannot open drawers or do buttons § Choking on food / pills S/P crycopharyngeal myotomy with some help
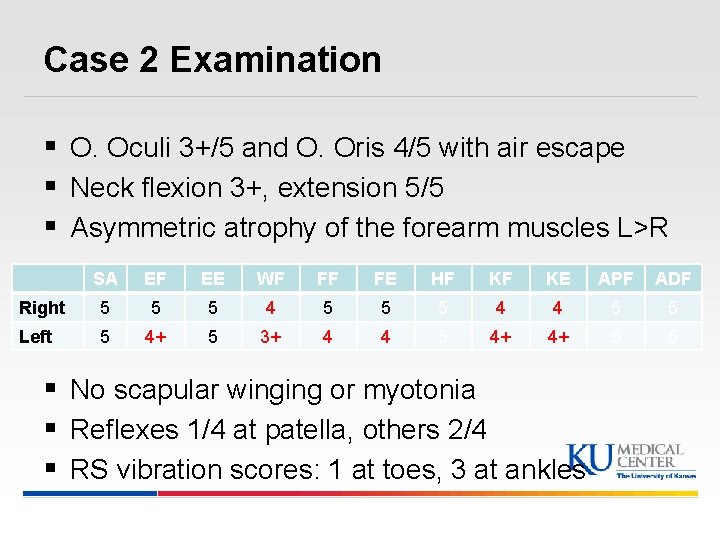
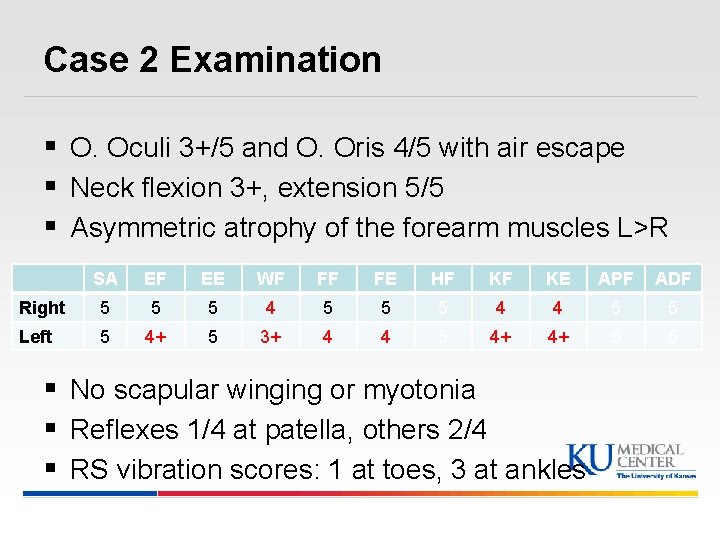
Case 2 Examination § O. Oculi 3+/5 and O. Oris 4/5 with air escape § Neck flexion 3+, extension 5/5 § Asymmetric atrophy of the forearm muscles L>R SA EF EE WF FF FE HF KF KE APF ADF Right 5 5 5 4 4 5 5 Left 5 4+ 5 3+ 4 4 5 4+ 4+ 5 5 § No scapular winging or myotonia § Reflexes 1/4 at patella, others 2/4 § RS vibration scores: 1 at toes, 3 at ankles
Case 2 Question #1 What pattern of myopathy does this patient have? a) MP 1 - Limb girdle b) MP 2 – Distal c) MP 3 - Proximal arm / distal leg “scapuloperoneal” d) MP 4 - Distal arm / proximal leg e) MP 5 - Ptosis / Ophthalmoplegia Answer: d. MP 4 - Distal arm / proximal leg
Case 2 Question #2 What test should you consider? a) Creatine kinase b) EMG/NCS c) Muscle biopsy d) All of the above Answer: d. All of the above
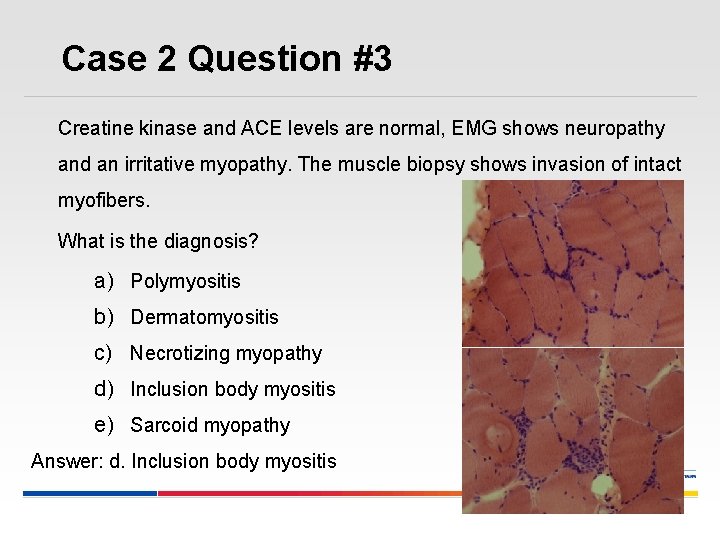
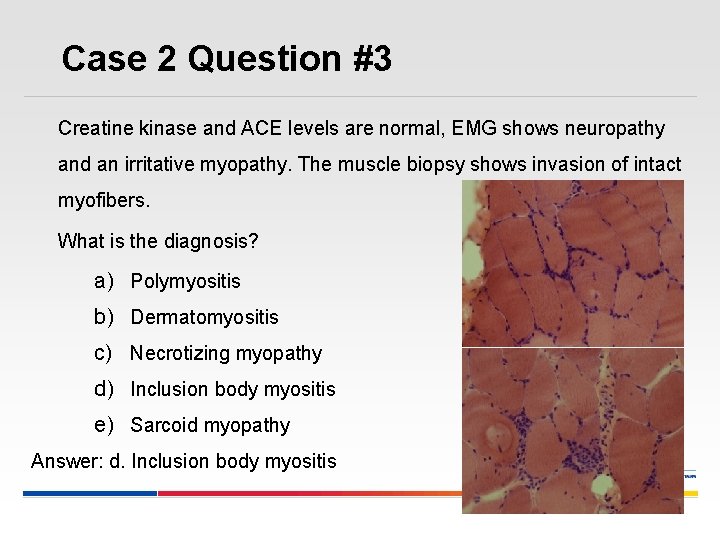
Case 2 Question #3 Creatine kinase and ACE levels are normal, EMG shows neuropathy and an irritative myopathy. The muscle biopsy shows invasion of intact myofibers. What is the diagnosis? a) Polymyositis b) Dermatomyositis c) Necrotizing myopathy d) Inclusion body myositis e) Sarcoid myopathy Answer: d. Inclusion body myositis
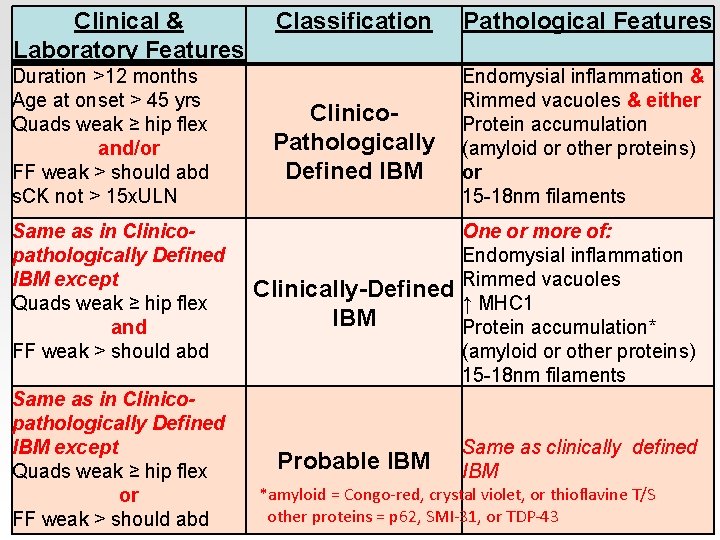
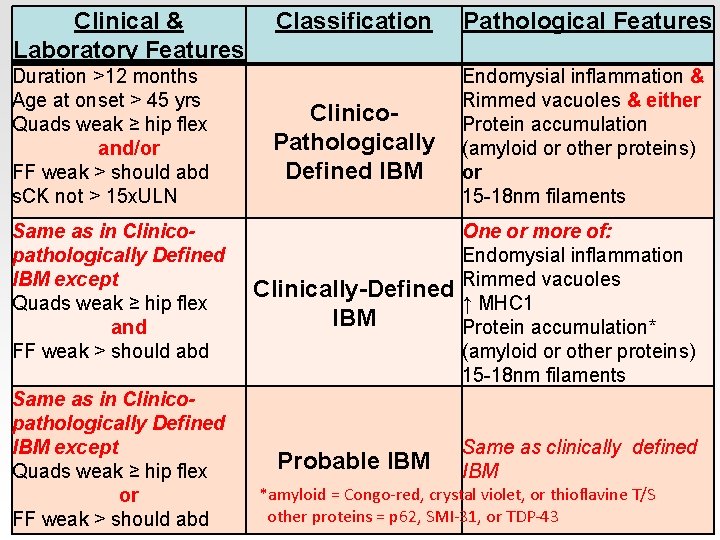
Clinical & Laboratory Features Classification Pathological Features Endomysial inflammation & 2011 -13 IBM diagnostic criteria Duration >12 months Age at onset > 45 yrs Quads weak ≥ hip flex and/or FF weak > should abd s. CK not > 15 x. ULN Same as in Clinicopathologically Defined IBM except Quads weak ≥ hip flex and FF weak > should abd Same as in Clinicopathologically Defined IBM except Quads weak ≥ hip flex or FF weak > should abd Clinico. Pathologically Defined IBM Rimmed vacuoles & either Protein accumulation (amyloid or other proteins) or 15 -18 nm filaments Clinically-Defined IBM One or more of: Endomysial inflammation Rimmed vacuoles ↑ MHC 1 Protein accumulation* (amyloid or other proteins) 15 -18 nm filaments Probable IBM Same as clinically defined IBM *amyloid = Congo-red, crystal violet, or thioflavine T/S other proteins = p 62, SMI-31, or TDP-43
Case 2 Question #4 What should this patient with ENMC 2011 Clinically-Defined IBM do? a) Follow up with Neuromuscular specialist familiar with IBM b) Mild to moderate intensity exercise c) Seek research studies to participate in d) All of the above Answer: d. All of the above
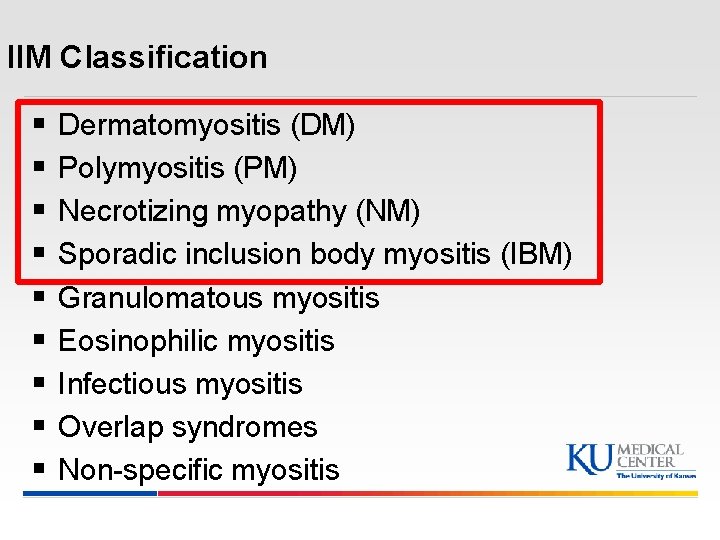
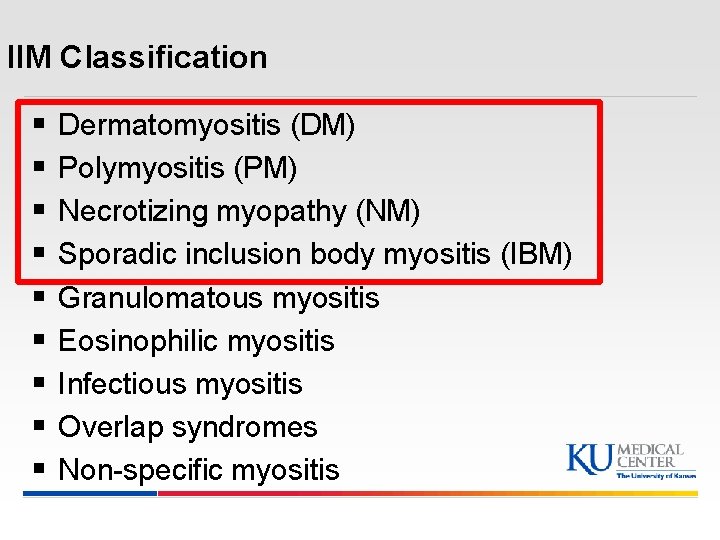
IIM Classification § § § § § Dermatomyositis (DM) Polymyositis (PM) Necrotizing myopathy (NM) Sporadic inclusion body myositis (IBM) Granulomatous myositis Eosinophilic myositis Infectious myositis Overlap syndromes Non-specific myositis
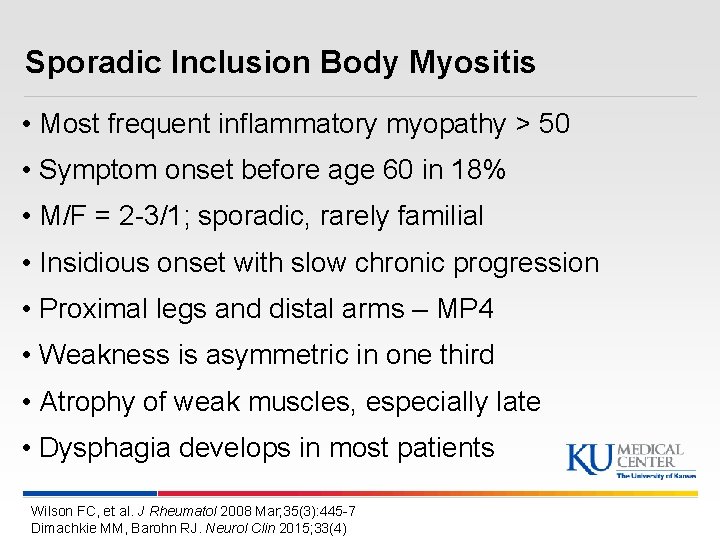
Sporadic Inclusion Body Myositis • Most frequent inflammatory myopathy > 50 • Symptom onset before age 60 in 18% • M/F = 2 -3/1; sporadic, rarely familial • Insidious onset with slow chronic progression • Proximal legs and distal arms – MP 4 • Weakness is asymmetric in one third • Atrophy of weak muscles, especially late • Dysphagia develops in most patients Wilson FC, et al. J Rheumatol 2008 Mar; 35(3): 445 -7 Dimachkie MM, Barohn RJ. Neurol Clin 2015; 33(4)
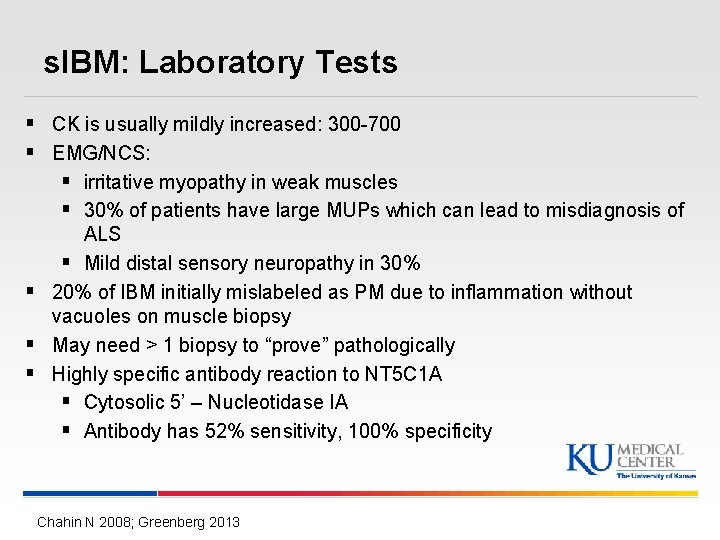
s. IBM: Laboratory Tests § CK is usually mildly increased: 300 -700 § EMG/NCS: § irritative myopathy in weak muscles § 30% of patients have large MUPs which can lead to misdiagnosis of ALS § Mild distal sensory neuropathy in 30% § 20% of IBM initially mislabeled as PM due to inflammation without vacuoles on muscle biopsy § May need > 1 biopsy to “prove” pathologically § Highly specific antibody reaction to NT 5 C 1 A § Cytosolic 5’ – Nucleotidase IA § Antibody has 52% sensitivity, 100% specificity Chahin N 2008; Greenberg 2013
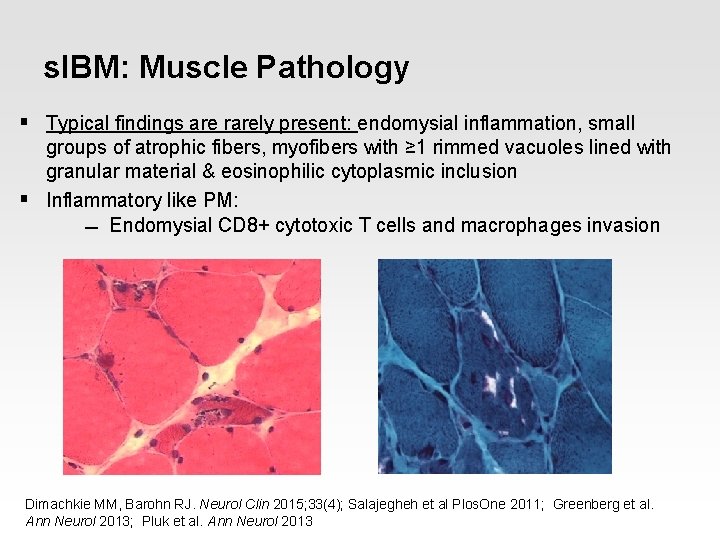
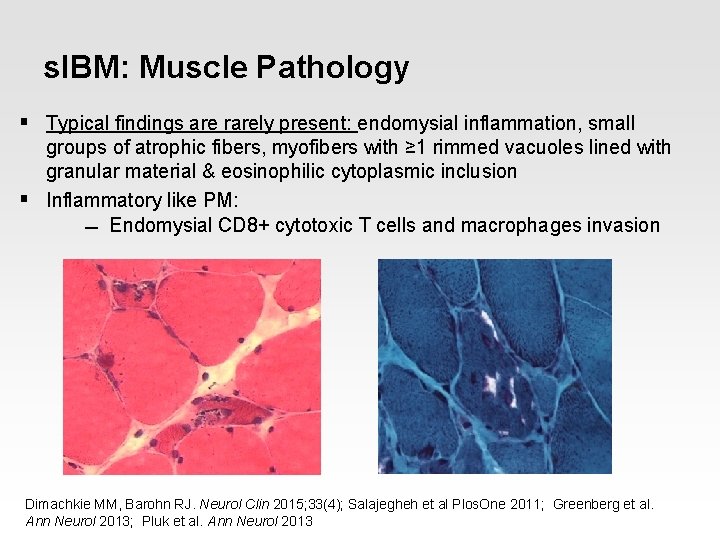
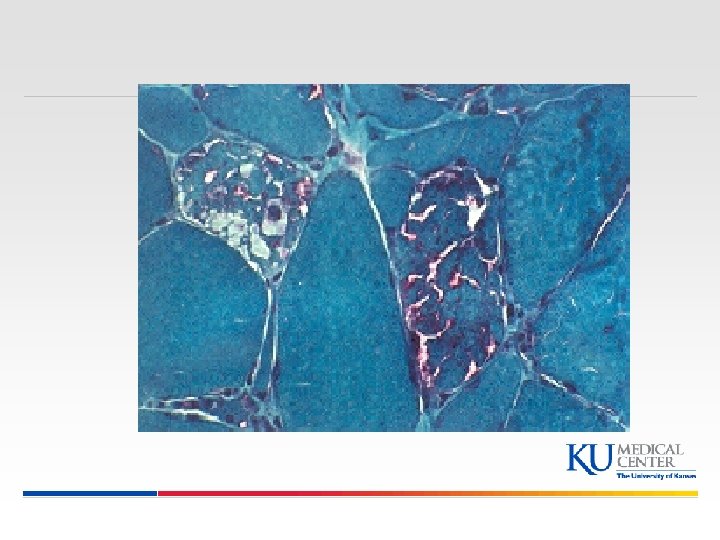
s. IBM: Muscle Pathology § Typical findings are rarely present: endomysial inflammation, small groups of atrophic fibers, myofibers with ≥ 1 rimmed vacuoles lined with granular material & eosinophilic cytoplasmic inclusion § Inflammatory like PM: Endomysial CD 8+ cytotoxic T cells and macrophages invasion Dimachkie MM, Barohn RJ. Neurol Clin 2015; 33(4); Salajegheh et al Plos. One 2011; Greenberg et al. Ann Neurol 2013; Pluk et al. Ann Neurol 2013
Sporadic Inclusion Body Myositis Prognosis • Relentless progression • 65% of patients by 5 years required a cane or support for ambulation • 60% of patients by 10 years required a wheelchair • No Rx at this time Dalakas & Sekul 1993
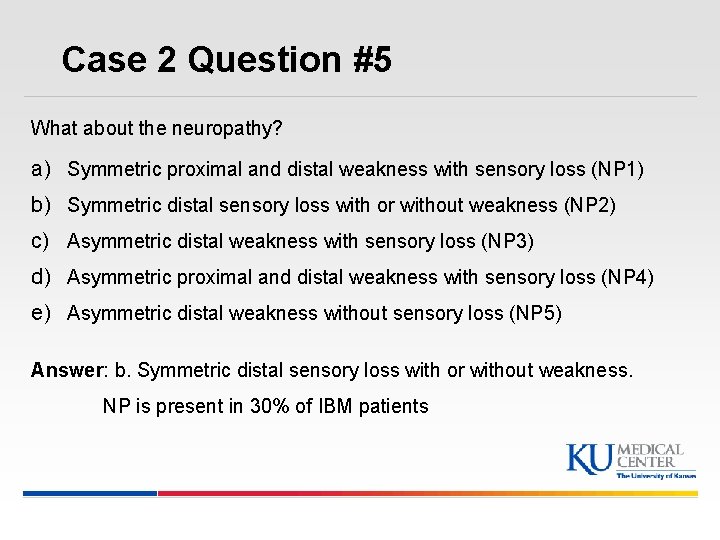
Case 2 Question #5 What about the neuropathy? a) Symmetric proximal and distal weakness with sensory loss (NP 1) b) Symmetric distal sensory loss with or without weakness (NP 2) c) Asymmetric distal weakness with sensory loss (NP 3) d) Asymmetric proximal and distal weakness with sensory loss (NP 4) e) Asymmetric distal weakness without sensory loss (NP 5) Answer: b. Symmetric distal sensory loss with or without weakness. NP is present in 30% of IBM patients
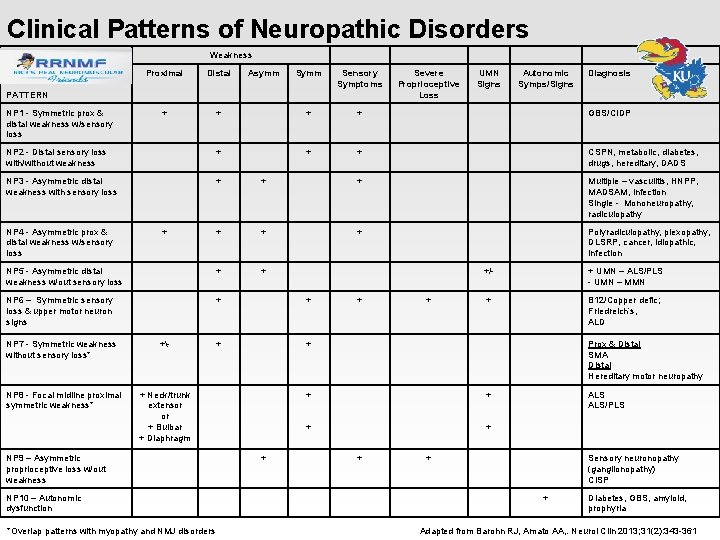
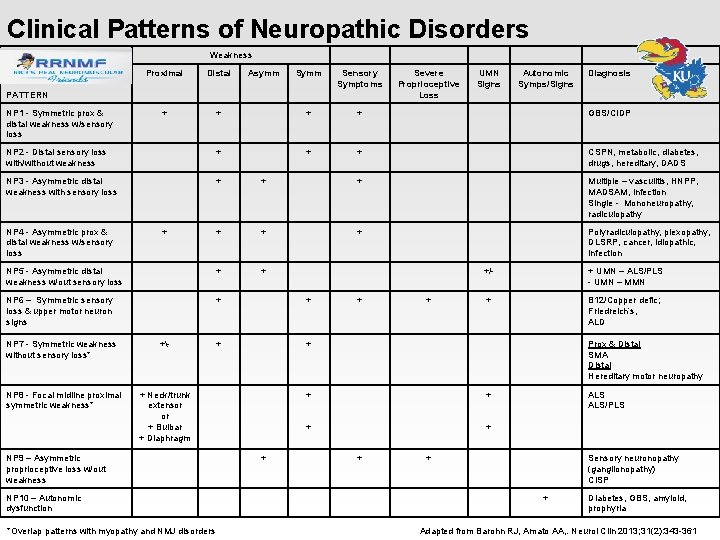
Clinical Patterns of Neuropathic Disorders Weakness Proximal Distal + Asymm Sensory Symptoms + + + GBS/CIDP NP 2 - Distal sensory loss with/without weakness + + + CSPN, metabolic, diabetes, drugs, hereditary, DADS NP 3 - Asymmetric distal weakness with sensory loss + + + Multiple – vasculitis, HNPP, MADSAM, infection Single - Mononeuropathy, radiculopathy + + + Polyradiculopathy, plexopathy, DLSRP, cancer, idiopathic, infection NP 5 - Asymmetric distal weakness w/out sensory loss + + NP 6 – Symmetric sensory loss & upper motor neuron signs + + PATTERN NP 1 - Symmetric prox & distal weakness w/sensory loss NP 4 - Asymmetric prox & distal weakness w/sensory loss + NP 7 - Symmetric weakness without sensory loss* +- NP 8 - Focal midline proximal symmetric weakness* + Neck/trunk extensor or + Bulbar + Diaphragm NP 9 – Asymmetric proprioceptive loss w/out weakness NP 10 – Autonomic dysfunction + + Severe Proprioceptive Loss + UMN Signs Autonomic Symps/Signs Diagnosis +/- + UMN – ALS/PLS - UMN – MMN + B 12/Copper defic; Friedreich’s, ALD Prox & Distal SMA Distal Hereditary motor neuropathy + + + ALS/PLS + Sensory neuronopathy (ganglionopathy) CISP + Diabetes, GBS, amyloid, prophyria *Overlap patterns with myopathy and NMJ disorders Adapted from Barohn RJ, Amato AA, . Neurol Clin 2013; 31(2): 343 -361
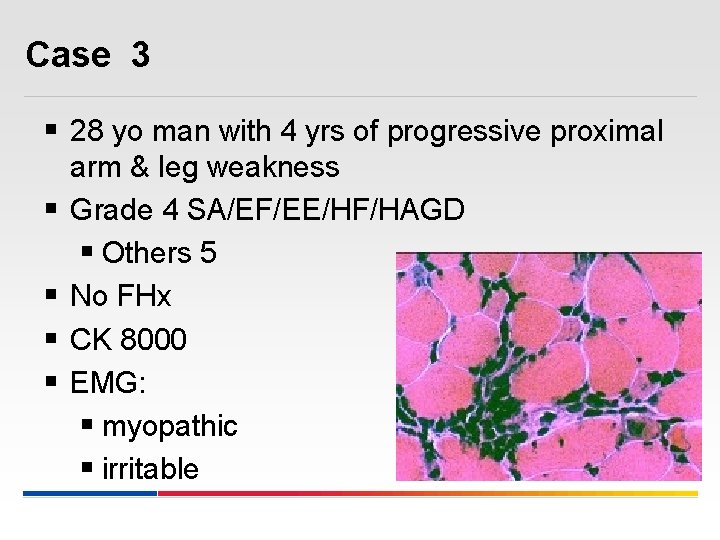
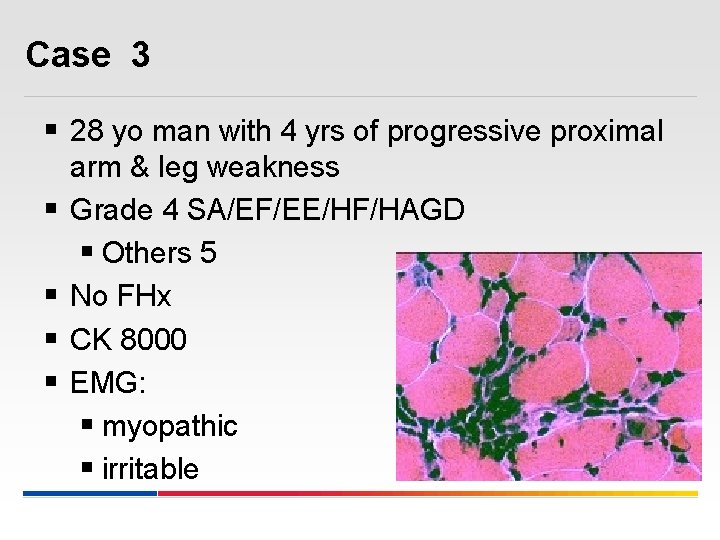
Case 3 § 28 yo man with 4 yrs of progressive proximal § § arm & leg weakness Grade 4 SA/EF/EE/HF/HAGD § Others 5 No FHx CK 8000 EMG: § myopathic § irritable
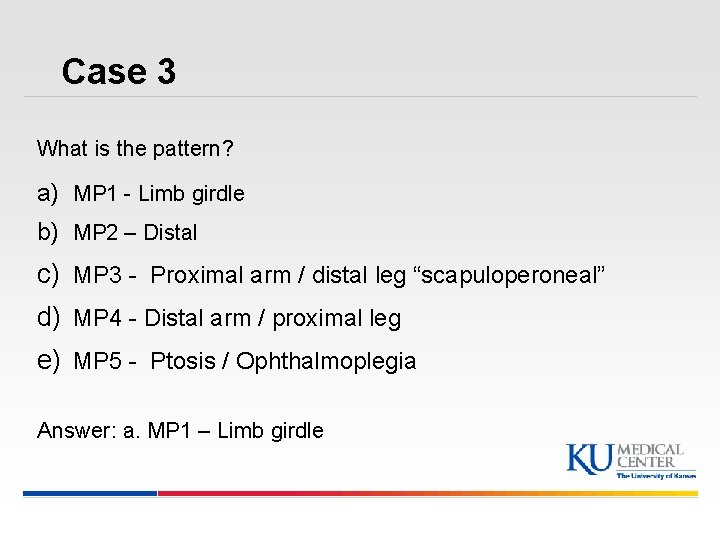
Case 3 What is the pattern? a) MP 1 - Limb girdle b) MP 2 – Distal c) MP 3 - Proximal arm / distal leg “scapuloperoneal” d) MP 4 - Distal arm / proximal leg e) MP 5 - Ptosis / Ophthalmoplegia Answer: a. MP 1 – Limb girdle
Case 3 § Diagnosed with PM § Treated with high dose prednisone § Patient reports subjective improvement § No clear objective improvement § Methotrexate added without clear benefit
Case 3 What would you do next? 1. Stop Methotrexate and add Cyclophosphamide 2. Begin IVIg 3. Begin ACTHAR Gel 4. Re-look at muscle biopsy 57
Case 3 § Frozen muscle from his initial bx is immunostained for dysferlin: § No dysferlin staining § Diagnosis = Limb-Girdle MD Type 2 B § Immunosuppressive meds discontinued
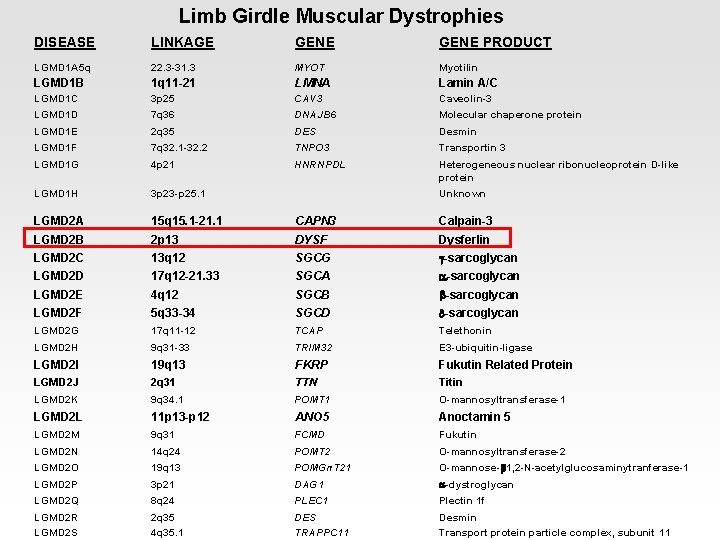
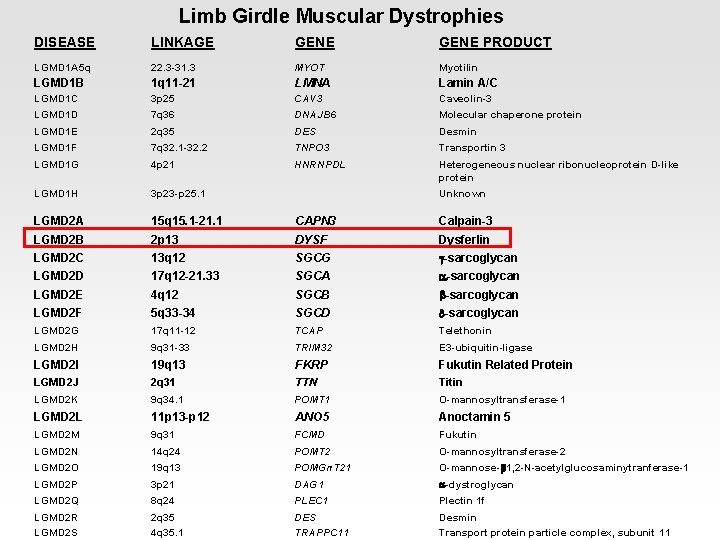
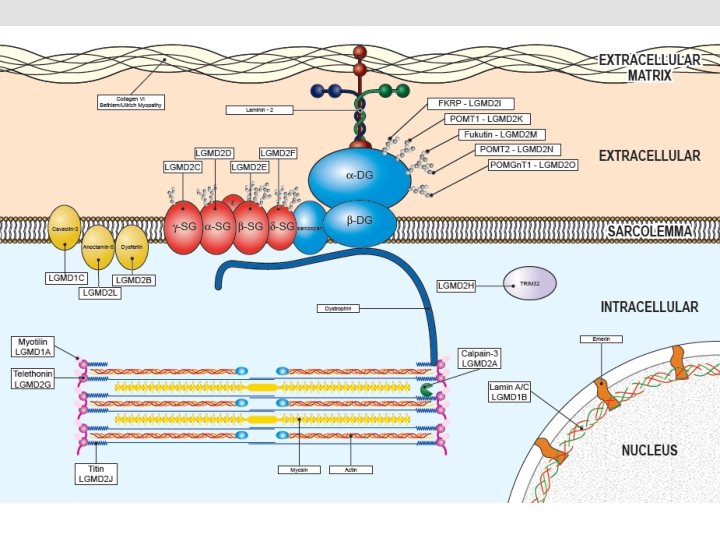
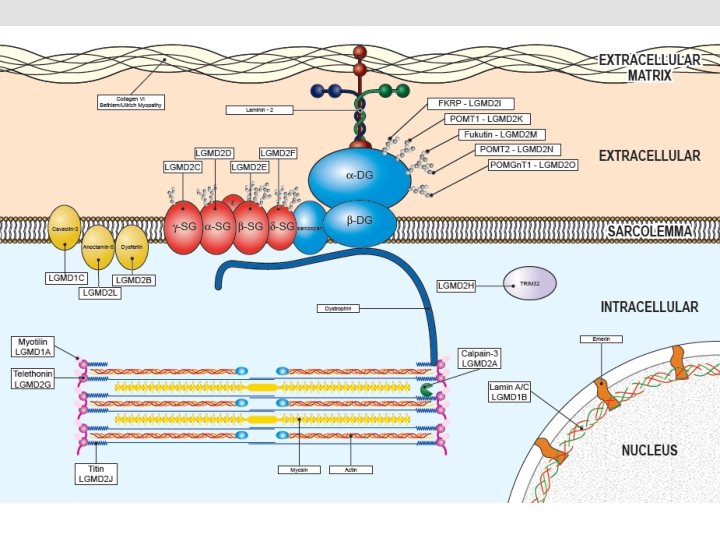
Limb Girdle Muscular Dystrophies DISEASE LINKAGE GENE PRODUCT LGMD 1 A 5 q 22. 3 -31. 3 MYOT Myotilin LGMD 1 B 1 q 11 -21 LMNA Lamin A/C LGMD 1 C 3 p 25 CAV 3 Caveolin-3 LGMD 1 D 7 q 36 DNAJB 6 Molecular chaperone protein LGMD 1 E 2 q 35 DES Desmin LGMD 1 F 7 q 32. 1 -32. 2 TNPO 3 Transportin 3 LGMD 1 G 4 p 21 HNRNPDL Heterogeneous nuclear ribonucleoprotein D-like protein LGMD 1 H 3 p 23 -p 25. 1 LGMD 2 A 15 q 15. 1 -21. 1 CAPN 3 Calpain-3 LGMD 2 B 2 p 13 DYSF Dysferlin LGMD 2 C 13 q 12 SGCG g-sarcoglycan LGMD 2 D 17 q 12 -21. 33 SGCA a-sarcoglycan LGMD 2 E 4 q 12 SGCB b-sarcoglycan LGMD 2 F 5 q 33 -34 SGCD d-sarcoglycan LGMD 2 G 17 q 11 -12 TCAP Telethonin LGMD 2 H 9 q 31 -33 TRIM 32 E 3 -ubiquitin-ligase LGMD 2 I 19 q 13 FKRP Fukutin Related Protein LGMD 2 J 2 q 31 TTN Titin LGMD 2 K 9 q 34. 1 POMT 1 O-mannosyltransferase-1 LGMD 2 L 11 p 13 -p 12 ANO 5 Anoctamin 5 LGMD 2 M 9 q 31 FCMD Fukutin LGMD 2 N 14 q 24 POMT 2 O-mannosyltransferase-2 LGMD 2 O 19 q 13 POMGn. T 21 O-mannose-b 1, 2 -N-acetylglucosaminytranferase-1 LGMD 2 P 3 p 21 DAG 1 a-dystroglycan LGMD 2 Q 8 q 24 PLEC 1 Plectin 1 f LGMD 2 R LGMD 2 S 2 q 35 4 q 35. 1 DES TRAPPC 11 Desmin Transport protein particle complex, subunit 11 Unknown
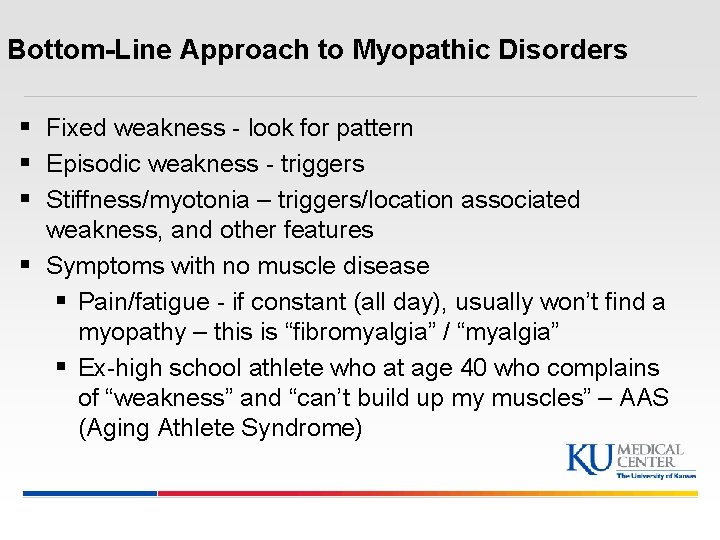
Bottom-Line Approach to Myopathic Disorders § Fixed weakness - look for pattern § Episodic weakness - triggers § Stiffness/myotonia – triggers/location associated weakness, and other features § Symptoms with no muscle disease § Pain/fatigue - if constant (all day), usually won’t find a myopathy – this is “fibromyalgia” / “myalgia” § Ex-high school athlete who at age 40 who complains of “weakness” and “can’t build up my muscles” – AAS (Aging Athlete Syndrome)
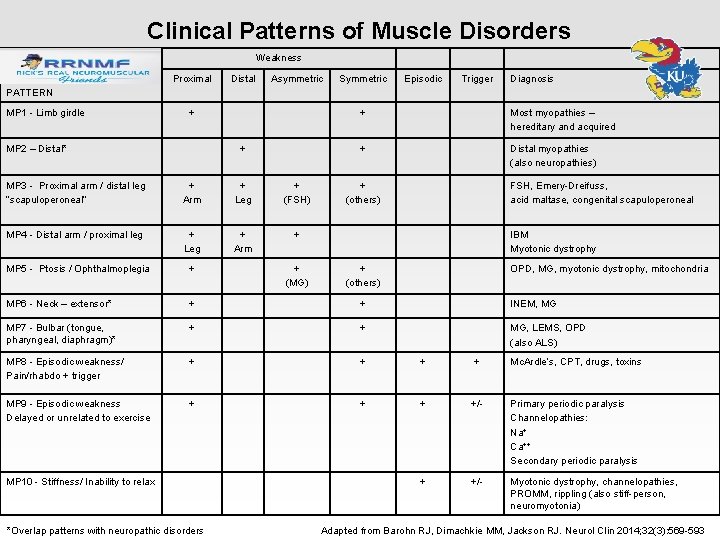
Clinical Patterns of Muscle Disorders Weakness Proximal Distal Asymmetric Symmetric Episodic Trigger Diagnosis PATTERN MP 1 - Limb girdle + MP 2 – Distal* + MP 3 - Proximal arm / distal leg “scapuloperoneal” + Arm + Leg + (FSH) MP 4 - Distal arm / proximal leg + Leg + Arm + Most myopathies – hereditary and acquired + Distal myopathies (also neuropathies) + (others) FSH, Emery-Dreifuss, acid maltase, congenital scapuloperoneal IBM Myotonic dystrophy MP 5 - Ptosis / Ophthalmoplegia + MP 6 - Neck – extensor* + + INEM, MG MP 7 - Bulbar (tongue, pharyngeal, diaphragm)* + + MG, LEMS, OPD (also ALS) MP 8 - Episodic weakness/ Pain/rhabdo + trigger + + Mc. Ardle’s, CPT, drugs, toxins MP 9 - Episodic weakness Delayed or unrelated to exercise + +/- Primary periodic paralysis Channelopathies: Na+ Ca++ Secondary periodic paralysis + +/- Myotonic dystrophy, channelopathies, PROMM, rippling (also stiff-person, neuromyotonia) MP 10 - Stiffness/ Inability to relax + (MG) + + (others) OPD, MG, myotonic dystrophy, mitochondria *Overlap patterns with neuropathic disorders Adapted from Barohn RJ, Dimachkie MM, Jackson RJ. Neurol Clin 2014; 32(3): 569 -593
www. rrnmf. com > 1500 Neuromuscular Health Care Professionals