Patients Are Care Managers Date presenter Chronic Care


- Slides: 48
Patients Are Care Managers Date presenter
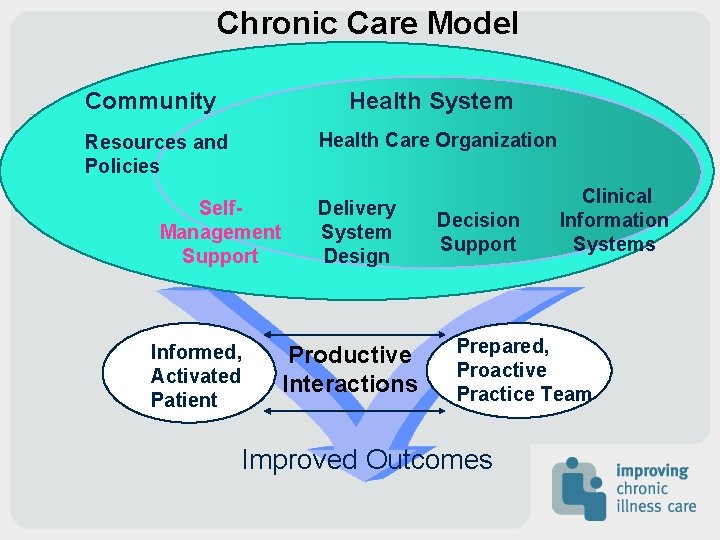
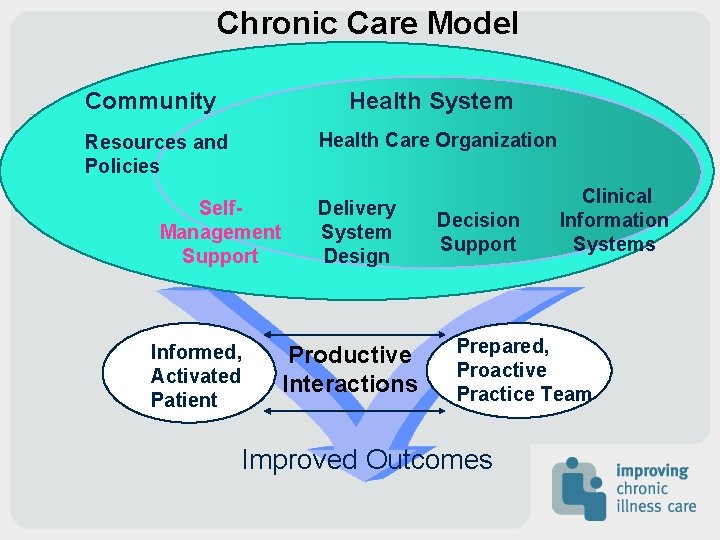
Chronic Care Model Community Health System Health Care Organization Resources and Policies Self. Management Support Informed, Activated Patient Delivery System Design Productive Interactions Decision Support Clinical Information Systems Prepared, Proactive Practice Team Improved Outcomes
Self-Management Support • Emphasize the patient’s central role in managing their illness • Assess patient’s beliefs, behavior and knowledge. • Advise patients by providing specific information about health risks and benefits of change.
Self-management support, cont. • Assist patients with problem-solving by identifying personal barriers, strategies, and social/environmental support. • Arrange a specific follow-up plan.
What is self-management? “The individual’s ability to manage the symptoms, treatment, physical and social consequences and lifestyle changes inherent in living with a chronic condition. ” Barlow et al, Patient Educ Couns 2002; 48: 177
What is self-management support? Making and refining the health care system to facilitate patient selfmanagement. This includes at the level of patient-provider, patienthealth care team, patient-health care system and the community. Glasgow et al, in submission
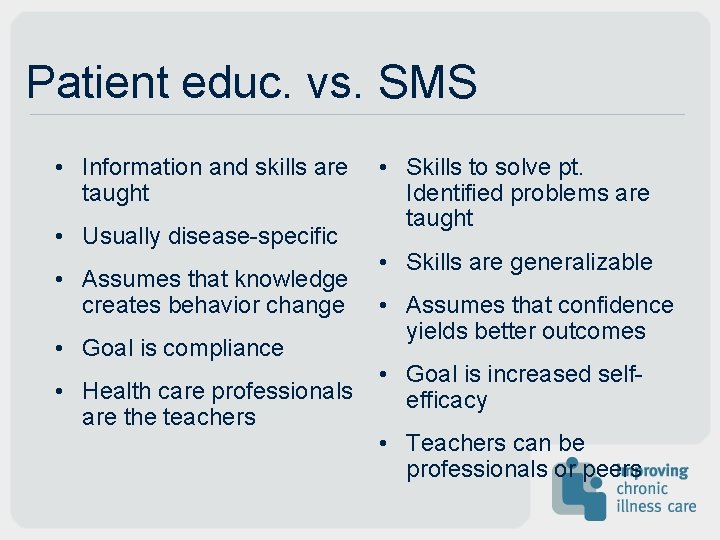
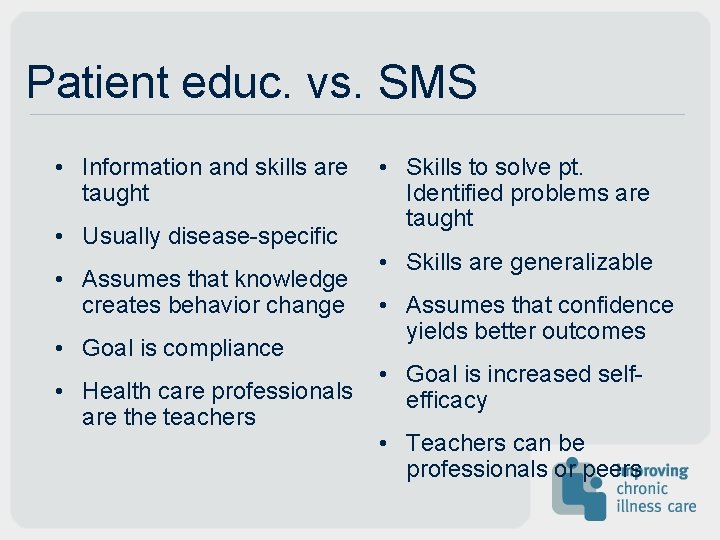
Patient educ. vs. SMS • Information and skills are taught • Usually disease-specific • Assumes that knowledge creates behavior change • Goal is compliance • Health care professionals are the teachers • Skills to solve pt. Identified problems are taught • Skills are generalizable • Assumes that confidence yields better outcomes • Goal is increased selfefficacy • Teachers can be professionals or peers
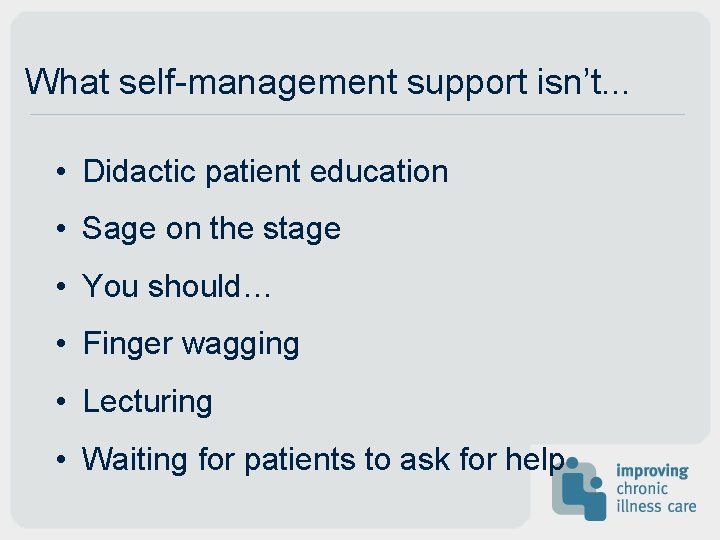
What self-management support isn’t. . . • Didactic patient education • Sage on the stage • You should… • Finger wagging • Lecturing • Waiting for patients to ask for help
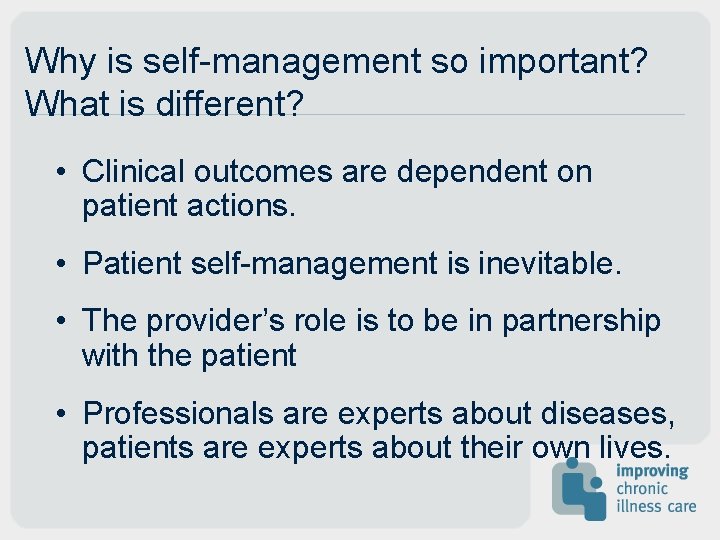
Why is self-management so important? What is different? • Clinical outcomes are dependent on patient actions. • Patient self-management is inevitable. • The provider’s role is to be in partnership with the patient • Professionals are experts about diseases, patients are experts about their own lives.
Self-Management Tasks in Chronic Illness • To take care of the illness • To carry out normal activities • To manage emotional changes Based on work by Corbin and Straus
Emphasizing the patient role
Collaborative care “If physicians view themselves as experts whose job is to get patients to behave in ways that reflect that expertise, both will continue to be frustrated…Once physicians recognize patients as experts on their own lives, they can add their medical expertise to what patients know about themselves to create a plan that will help patients achieve their goals. ” Funnell & Anderson JAMA 2000; 284: 1709
How to emphasize the patient’s role • Simple messages from the primary care provider: “Diabetes is a serious condition. There are things you can do to live better with diabetes and things the medical team can do to assist you. We are going to work together on this. ” • Consistent approach • Culturally and linguistically appropriate
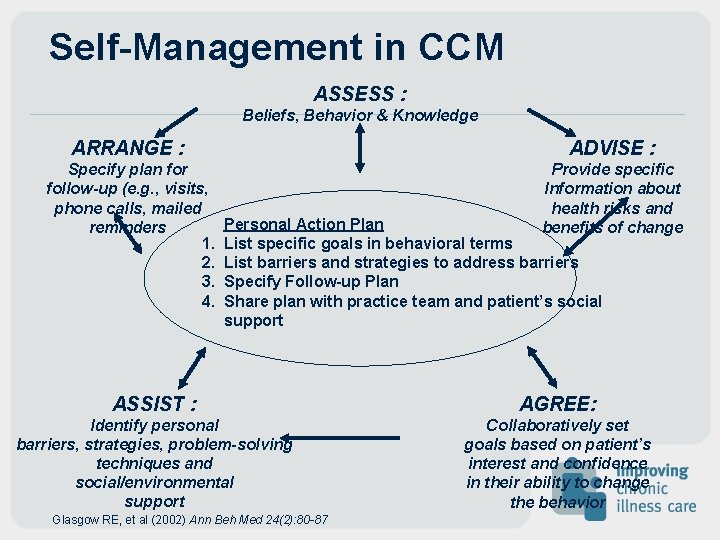
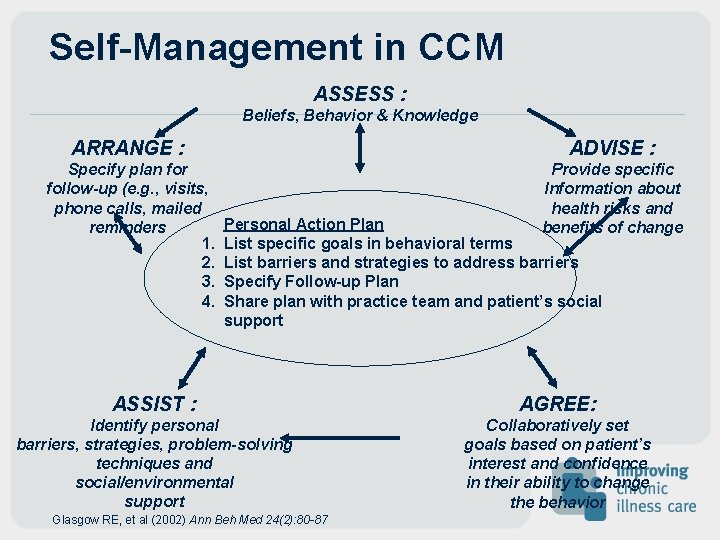
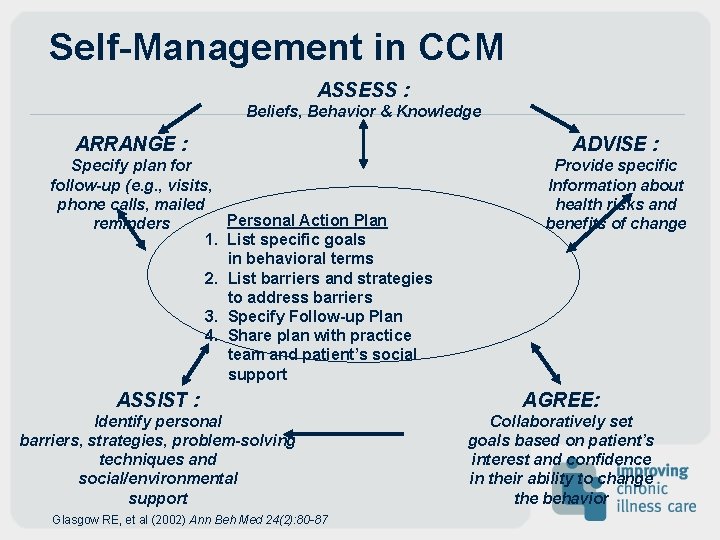
Self-Management in CCM ASSESS : Beliefs, Behavior & Knowledge ARRANGE : ADVISE : Specify plan for follow-up (e. g. , visits, phone calls, mailed reminders 1. 2. 3. 4. Provide specific Information about health risks and benefits of change Personal Action Plan List specific goals in behavioral terms List barriers and strategies to address barriers Specify Follow-up Plan Share plan with practice team and patient’s social support ASSIST : AGREE: Identify personal barriers, strategies, problem-solving techniques and social/environmental support Collaboratively set goals based on patient’s interest and confidence in their ability to change the behavior Glasgow RE, et al (2002) Ann Beh Med 24(2): 80 -87
ASSESS Risk factors, Beliefs, Behavior and Knowledge
Standardizing Assessment • Knowledge • Skills • Confidence • Supports • Barriers • Risk Factors
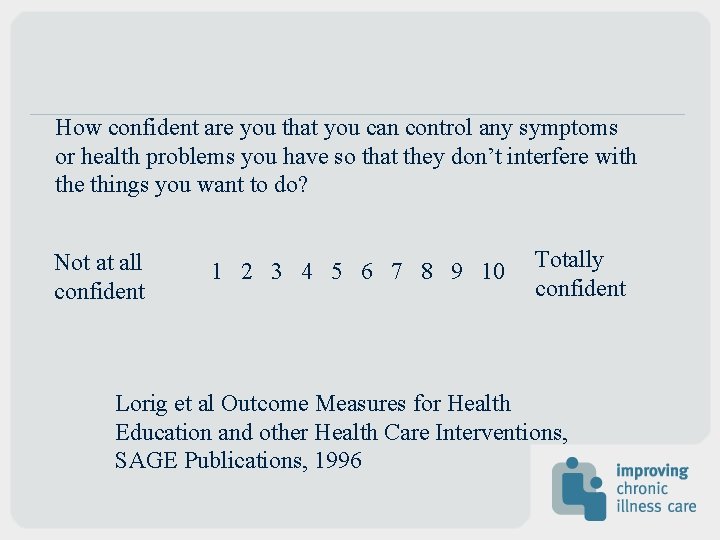
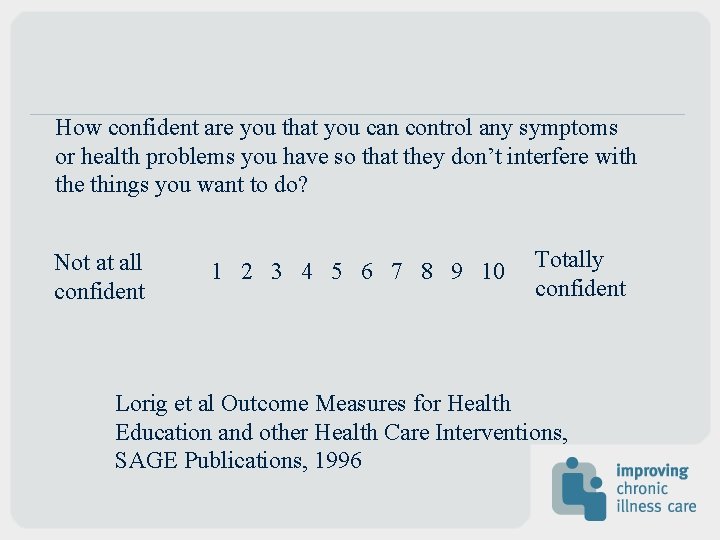
How confident are you that you can control any symptoms or health problems you have so that they don’t interfere with the things you want to do? Not at all confident 1 2 3 4 5 6 7 8 9 10 Totally confident Lorig et al Outcome Measures for Health Education and other Health Care Interventions, SAGE Publications, 1996
Tips on assessing patients • Use brief standardized assessments • Provide feedback to patient and care team • Assess patient’s view of progress and how choices relate to goals
ADVISE Provide specific personalized information about health risks and benefits of change
Tips on providing advice • Make the source of advice clear (medical knowledge or from similar patients) • Personalize lab values, health status and how choices affect outcomes • Provide patient-determined level of information to make decisions
Tips on providing advice (cont. ) • Tailor information to person and their environment • Listen more than you talk • Have a key message for each condition or symptom
AGREE Collaboratively select goals and treatment methods based on patient’s interest and confidence in their ability to change the behavior
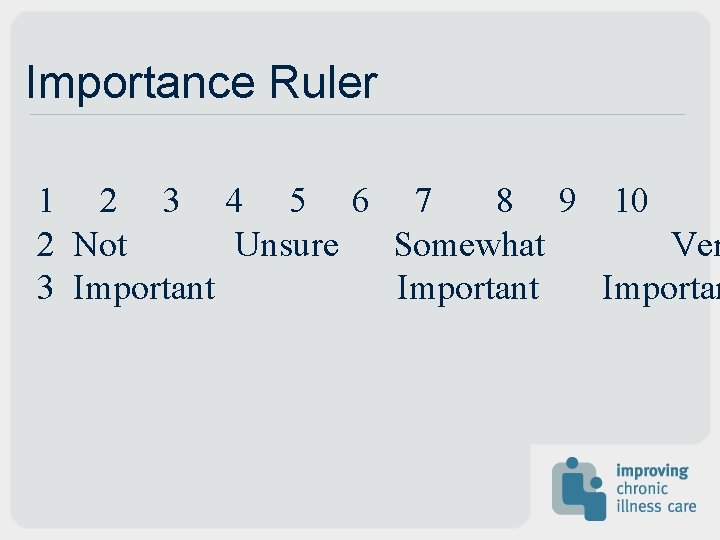
Importance Ruler 1 2 3 4 5 6 7 8 9 10 2 Not Unsure Somewhat Ver 3 Important Importan
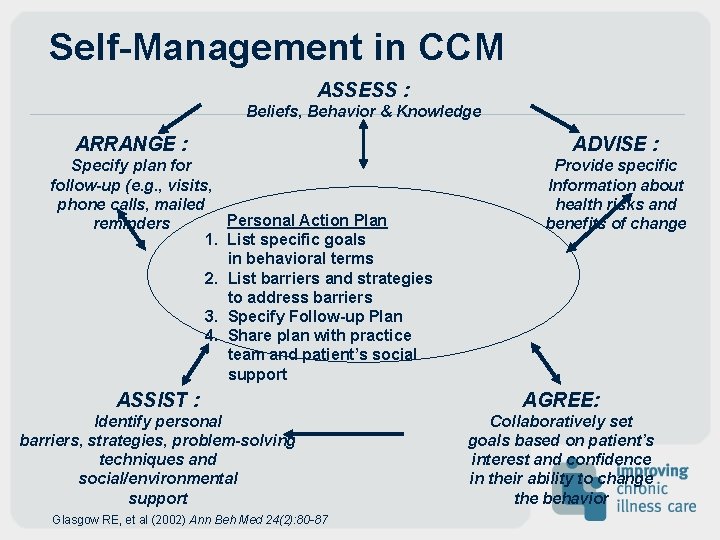
Self-Management in CCM ASSESS : Beliefs, Behavior & Knowledge ARRANGE : Specify plan for follow-up (e. g. , visits, phone calls, mailed Personal Action Plan reminders 1. List specific goals in behavioral terms 2. List barriers and strategies to address barriers 3. Specify Follow-up Plan 4. Share plan with practice team and patient’s social support ADVISE : Provide specific Information about health risks and benefits of change ASSIST : AGREE: Identify personal barriers, strategies, problem-solving techniques and social/environmental support Collaboratively set goals based on patient’s interest and confidence in their ability to change the behavior Glasgow RE, et al (2002) Ann Beh Med 24(2): 80 -87
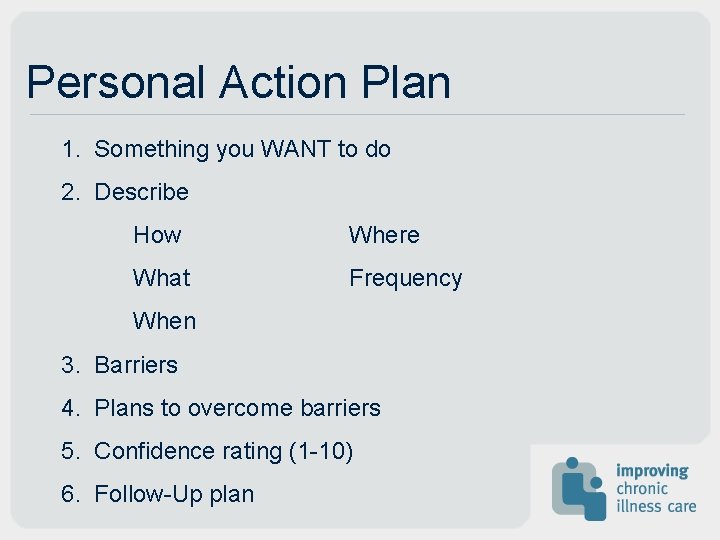
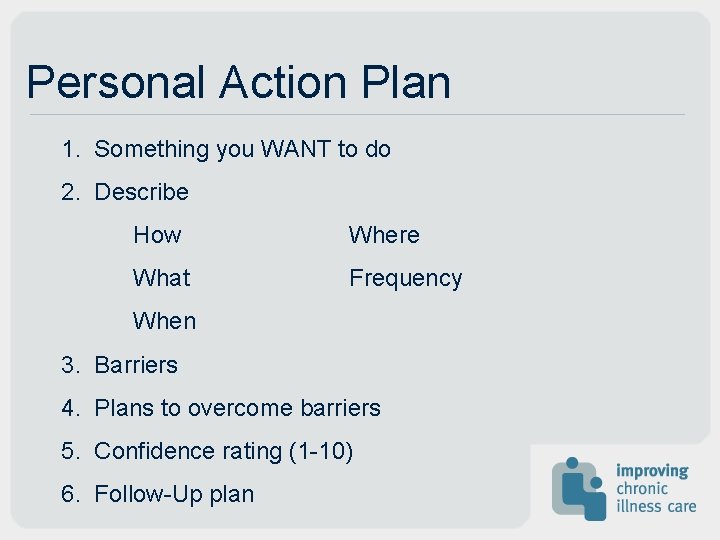
Personal Action Plan 1. Something you WANT to do 2. Describe How Where What Frequency When 3. Barriers 4. Plans to overcome barriers 5. Confidence rating (1 -10) 6. Follow-Up plan
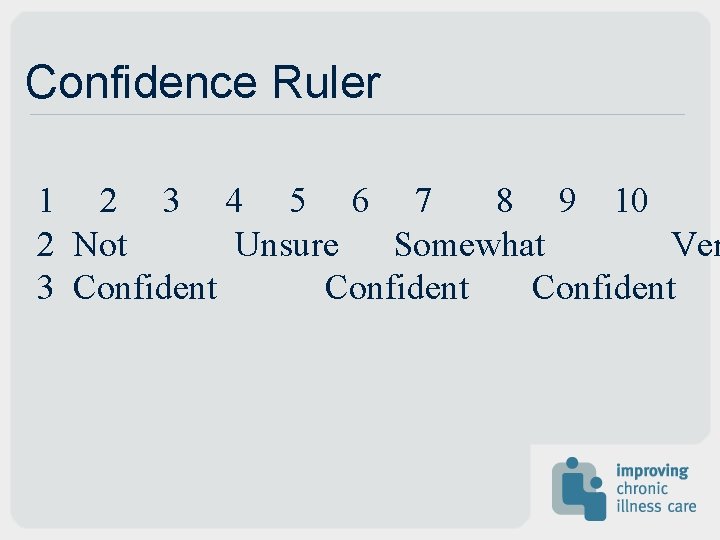
Confidence Ruler 1 2 3 4 5 6 7 8 9 10 2 Not Unsure Somewhat Ver 3 Confident
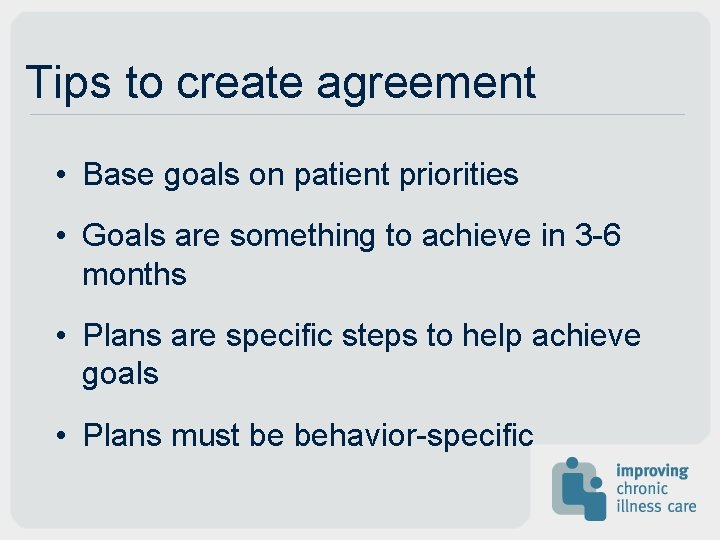
Tips to create agreement • Base goals on patient priorities • Goals are something to achieve in 3 -6 months • Plans are specific steps to help achieve goals • Plans must be behavior-specific
ASSIST Using behavior change techniques (selfhelp, counseling, etc. ) aid the patient in achieving agreed-upon goals by acquiring skills, confidence, and developing social/environmental supports.
Problem Solving 1. Identify the problem. 2. List all possible solutions. 3. Pick one. 4. Try it for 2 weeks. 5. If it doesn’t work, try another. 6. If that doesn’t work, find a resource for ideas. 7. If that doesn’t work, accept that the problem may not be solvable now.
Examples of Effective Interventions • CDSMP (Lorig) • Open Airways (Clark) • Office Practice (Glasgow) • Patient Empowerment (Anderson) • Diabetes Prevention (DPP study group)
Chronic Disease Self. Management Program • develop and studied by Kate Lorig and colleagues at Stanford • lay-leaders, 6 sessions, 2 1/2 hours each • addresses multiple conditions • includes planning and problem solving, skill acquisition • “Everything you wish patients knew” • outcomes: improved health behaviors and health status, fewer hospitalizations some sustained for 2 yrs (Lorig, Med Care 1999; 37: 5, 2002; 39: 1217)
Open Airways • developed by Clark and colleagues in Michigan • for children with asthma • 6 sessions, 1 hour each • information, emotional support, monitoring, problem solving, physical activity planning • reduced asthma episodes, decreased symptoms, improved self-efficacy (Evans, Hlth Ed Q 1987; 14: 267 -279)
Individual Office Practice • developed by Glasgow and colleagues • prior to visit: mailed reminder of self-monitoring • waiting room: self-care form • exam room: feedback on changes, check on goal, elicit current self-care concern • physical exam: message • follow-up: negotiate goals, develop plan, anticipate barriers, plan for support • outcomes: decr. serum cholesterol, alt. dietary habits, impr. satisfaction (Glasgow, Pt Ed & Couns 1997; 32: 175 -184)
Diabetes Prevention Program • Had IGT • 7% wt loss, 150 minutes exercise/wk • Diet, exercise, behavior modification 1: 1 for 24 weeks • Flexible support, culturally sensitive, individualized • Group and individual follow-up • After nearly 3 years, diabetes incidence decreased by 58% • More successful in those over 60 NEJM 2002; 346: 393 -403
Patient Empowerment • developed by Anderson and colleagues at University of Michigan • emphasis on whole patient • patient generates options • build on patient strengths • failures are learning experiences • diabetes outcomes: reduced Hb. A 1 c, improved selfefficacy (Anderson, Diabetes Care 1995; 18: 943 -949)
Techniques • Motivational Interviewing • Problem Solving • Peer Support • Empowerment • Skill Acquisition • Modeling • Reinterpreting symptoms
Thoughts on reading level • Developed to put school children into ability groups for educational purposes • Adults can read above their level on topics that interest them • Families and friends are often willing to read to their loved ones • Patients are very sensitive about being talked down to. Source: Kate Lorig, RN, Dr. PH
ARRANGE Schedule follow-up contacts to provide ongoing assistance and support to adjust the plan as needed, including referral to more intensive treatment

Tips for follow-up • Try a wide variety of methods, whichever patient prefers (in person, phone, email) • Make sure follow-up happens, patient trust can be destroyed by missed followup • Use outreach and community opportunities

Opportunities for SMS • Before the Encounter • During the Encounter • After the Encounter
Opportunities for SMS Before the Encounter • Pre-visit contact (phone, mail or e-mail) • Waiting room assessment • Patient education material • Posters • Pamphlets on “Talking to Your Provider” • Community outreach
Opportunities for SMS During the Encounter • Review assessments • Feedback on achievements vs. goals • Identifies priorities for visit • 5 “A”s Counseling • Targeted patient education materials • Referral for more SMS
Opportunities for SMS After the Encounter • Referrals (Health Education, etc) • Further 5 “A”s counseling • Phone calls follow-up • Mailed patient education • Peer support • Newsletters • Follow-up visits • e-mail/Internet sites
What about effectiveness? • The effects of behavioral interventions cannot be compared to drug trials. • Generally 5 -15% will make clinically significant behavior change • When viewed at the level of a population, this does benefit the health of the population. • A more relevant outcome than behavior change may be improved self-efficacy, which translates into better quality of life and decreased utilization.
Who can do this? • Natural helpers • Trained peers • Health educators • Nurses • Physicians • Any caring person. . .
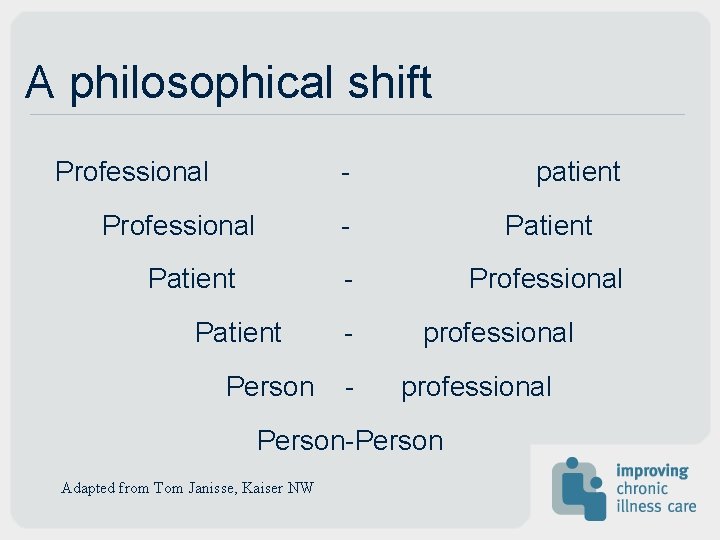
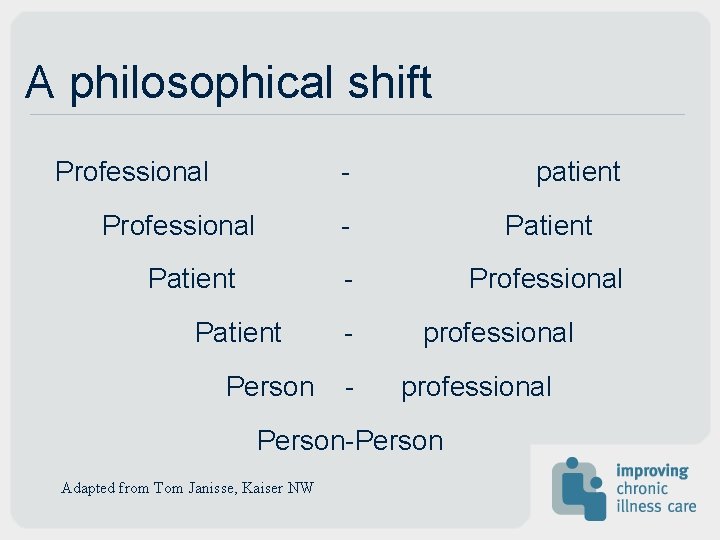
A philosophical shift Professional - Professional Patient Person patient - Professional - professional Person-Person Adapted from Tom Janisse, Kaiser NW
Web resources • www. bayerinstitute. com provides provider training in “Choices and Changes” • www. motivationalinterview. org has books, videos and training • www. stanford. edu/group/perc home of Chronic Disease Self-Management Program
Contact us: • www. improvingchroniccare. org thanks