PatientDelivered Partner Therapy for STD Evidence and Prospects
- Slides: 15
Patient-Delivered Partner Therapy for STD: Evidence and Prospects for Implementation National STD Conference 2004 Matthew Hogben, CDC Matthew R Golden, U Washington and PHSKC Patricia Kissinger, Tulane U Janet S St. Lawrence, CDC
Questions • Why consider dispensing medications or prescriptions to patients to give to their sex partners? • What do we know about the prevalence of PDPT? • What do we know about how well it works? – Using which measures of effectiveness?
Why consider PDPT • The standard of care is self-referral, which does not capture all partners • Meta-analyses suggest DIS-assisted notification is more effective than self-referral – But STD morbidity is too high for universal DISassisted referral – 89% of syphilis cases, but only 17% of GC and 12% of CT cases were interviewed in high morbidity areas* • PDPT is a possible alternative or complementary strategy *Golden, Hogben et al. (2003). Sex Transm Dis
PDPT Prevalence • Vague status of PDPT means data have been sparse – or vice versa – Legal (more civil than criminal) – Professional opinions surrounding physical evaluations of patients • A recent national survey has yielded more information
Survey Sample* • Five AMA specialties diagnosing 85% of STD in the USA • 4233 respondents (70% response rate) • 71% male, 76% White, 46 years old • 87% in private settings, 69% primary care offices • In the past year: ** – 54% had diagnosed GC – 73% had diagnosed CT *St. Lawrence, Montano, et al (2002). Am J Public Health. **Mc. Cree, Liddon, et al (2003). Sex Transm Inf.
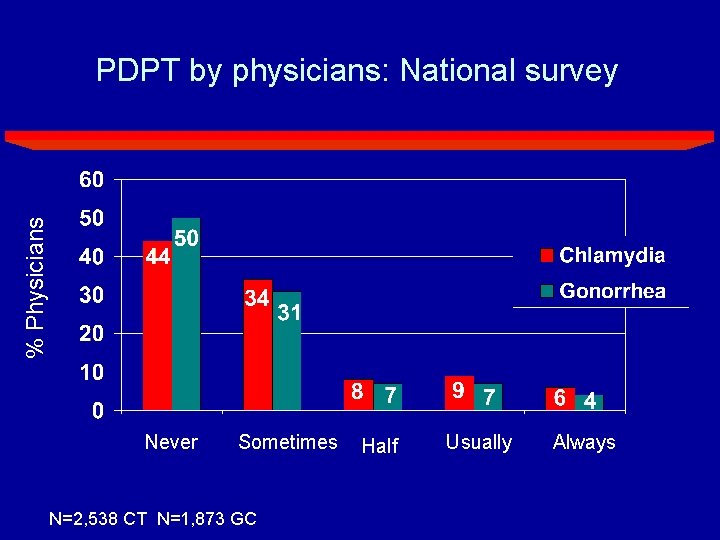
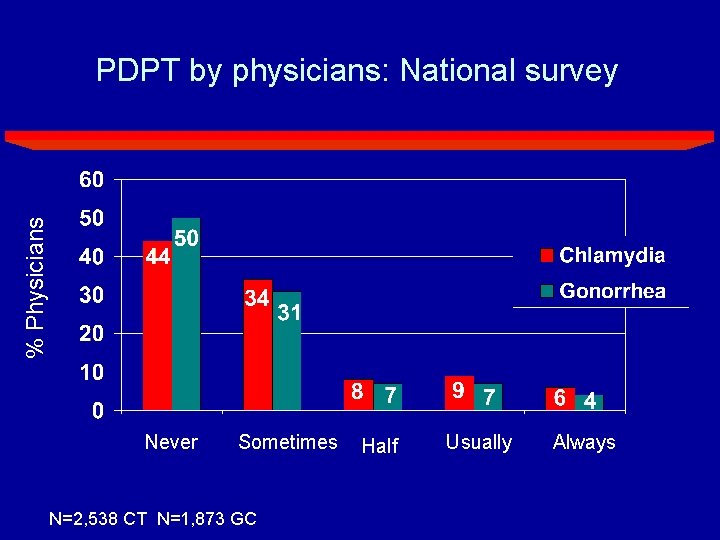
% Physicians PDPT by physicians: National survey Never Sometimes N=2, 538 CT N=1, 873 GC Half Usually Always
Correlates of PDPT • PDPT practice was most common among: – Ob/gyns and family/general practitioners (least common among ER physicians) – Physicians with higher proportions of female patients • Also correlated with forms of “provider referral. ” – Collecting partner information and contacting partners – Collecting partner information and sending it to HD • Less common in circumstances where STD is most prevalent – Negatively correlated with proportion of Black or African American patients – Least common in Southern US (Federal quadrant)
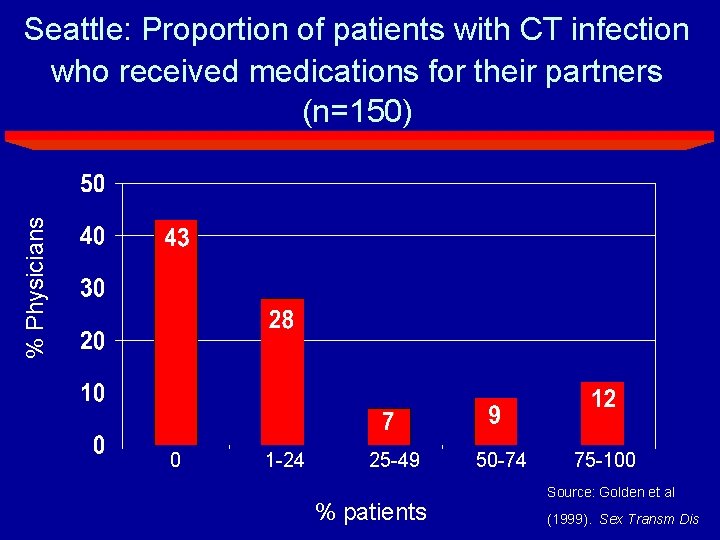
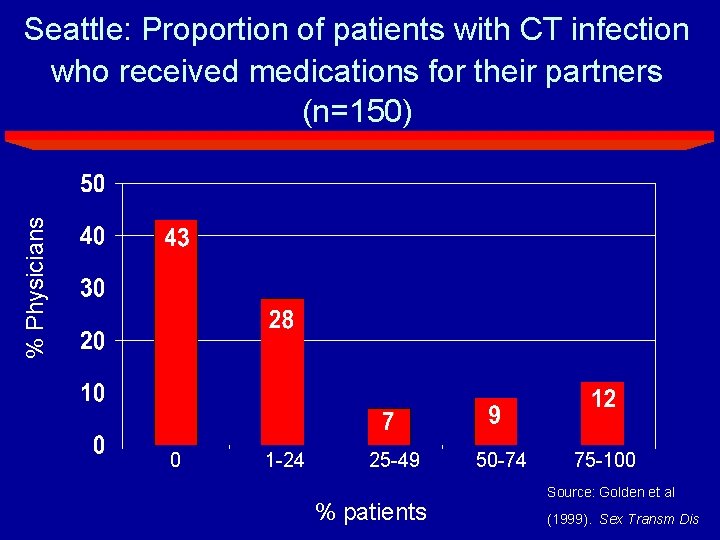
% Physicians Seattle: Proportion of patients with CT infection who received medications for their partners (n=150) 0 1 -24 25 -49 % patients 50 -74 75 -100 Source: Golden et al (1999). Sex Transm Dis
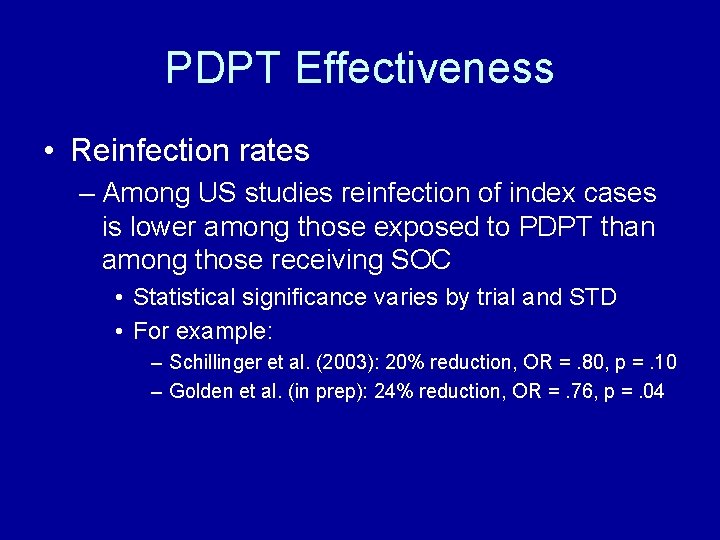
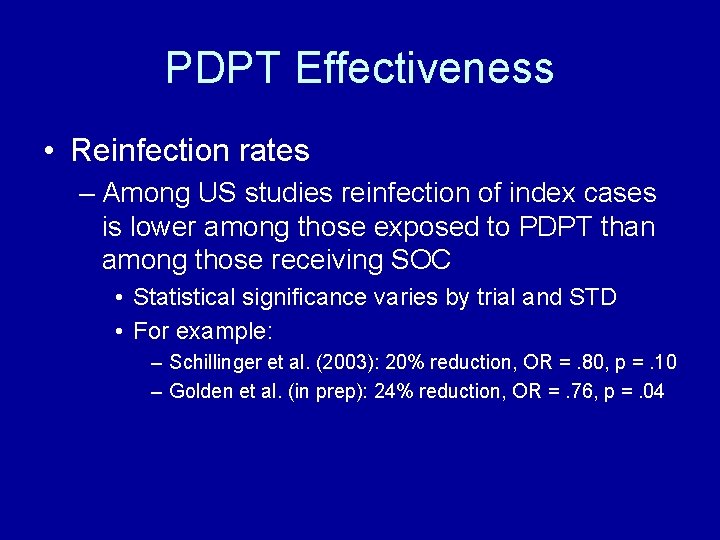
PDPT Effectiveness • Reinfection rates – Among US studies reinfection of index cases is lower among those exposed to PDPT than among those receiving SOC • Statistical significance varies by trial and STD • For example: – Schillinger et al. (2003): 20% reduction, OR =. 80, p =. 10 – Golden et al. (in prep): 24% reduction, OR =. 76, p =. 04
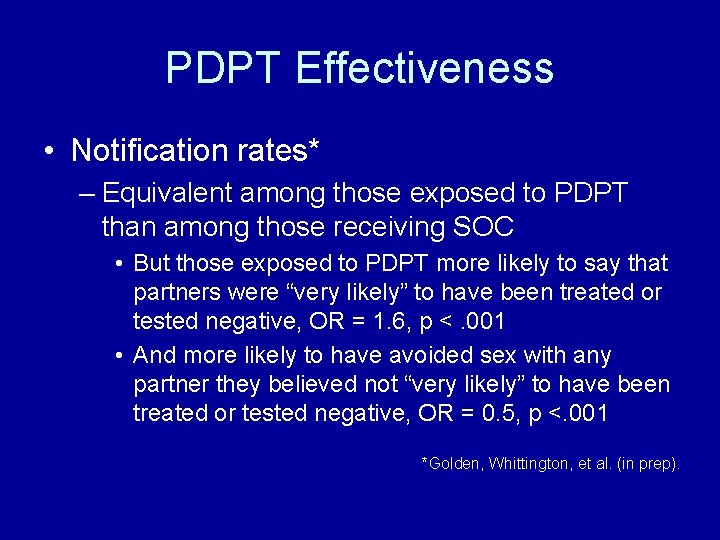
PDPT Effectiveness • Notification rates* – Equivalent among those exposed to PDPT than among those receiving SOC • But those exposed to PDPT more likely to say that partners were “very likely” to have been treated or tested negative, OR = 1. 6, p <. 001 • And more likely to have avoided sex with any partner they believed not “very likely” to have been treated or tested negative, OR = 0. 5, p <. 001 *Golden, Whittington, et al. (in prep).
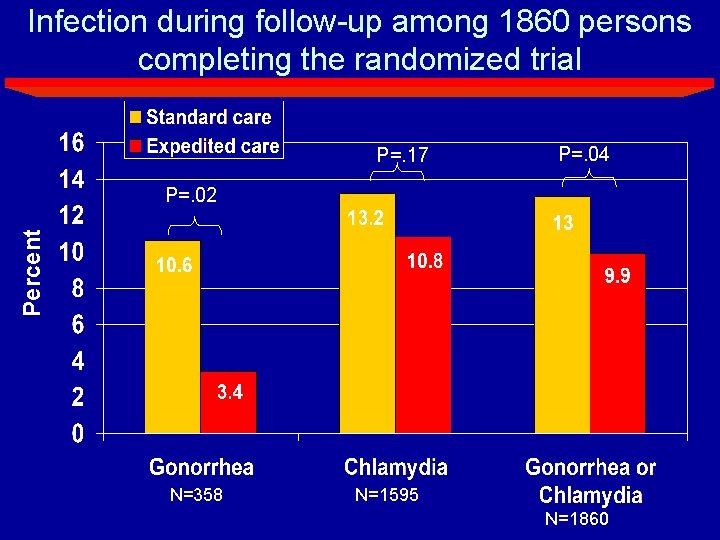
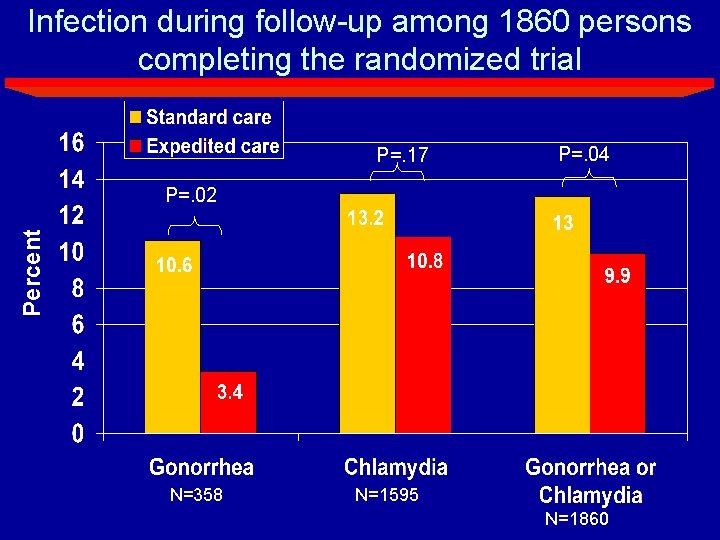
Infection during follow-up among 1860 persons completing the randomized trial P=. 17 P=. 04 Percent P=. 02 N=358 N=1595 N=1860
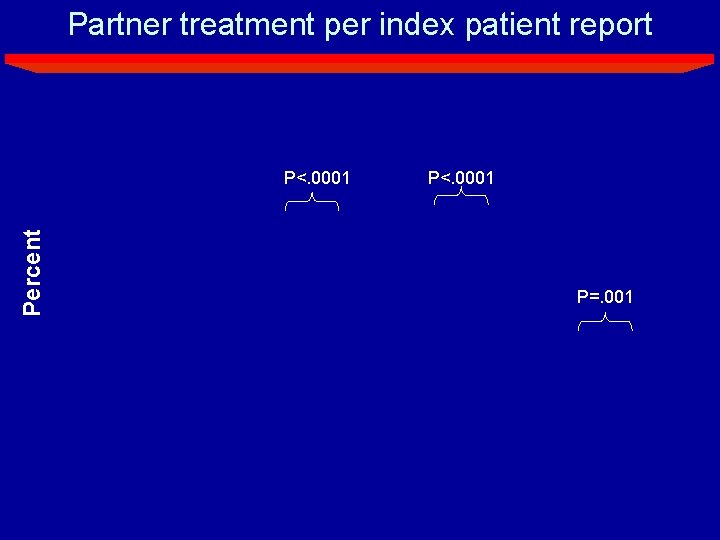
Partner treatment per index patient report Percent P<. 0001 P=. 001
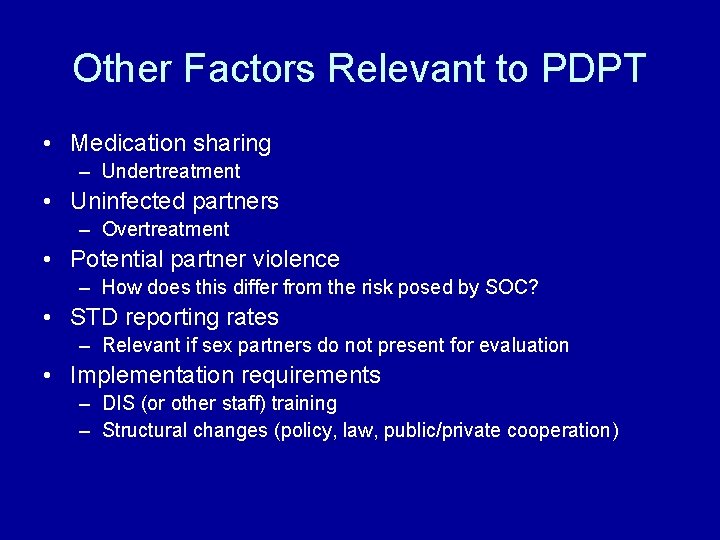
Other Factors Relevant to PDPT • Medication sharing – Undertreatment • Uninfected partners – Overtreatment • Potential partner violence – How does this differ from the risk posed by SOC? • STD reporting rates – Relevant if sex partners do not present for evaluation • Implementation requirements – DIS (or other staff) training – Structural changes (policy, law, public/private cooperation)
More Work to be Done • Using existing data – Meta-analysis will help establish • A more robust mean effect • Moderating effects on an overall mean – Descriptive multi-level modeling • Allows structural and individual influences and correlates to be assessed together • With whom does PDPT work best? • In conjunction with which other partner management strategies?
Reference list • References available as a handout. If you have relevant material, feel free to send it to Matthew Hogben at mhogben@cdc. gov. That includes references and ideas. – – – – – Golden MR, Hogben M et al. Sex Transm Dis 2003; 30: 490 -496 Golden MR, Whittington WLH et al. Sex Transm Dis 2001; 28: 658665. Kissinger P, Brown R et al. Sex Transm Inf 1998; 74: 331 -333. Klausner JD, Chaw JK. Sex Transm Dis 2003; 30: 509 -511. Macke B, Maher J. Am J Prev Med 1999; 17: 230 -242. Mc. Cree DH, Liddon NC et al. Sex Transm Inf 2003; 79: 254 -256. Oxman AD, Scott EAF et al. Can J Public Health 1994; 85 (supp 1): S 41 -S 47. Schillinger JA, Kissinger P et al. Sex Transm Dis 2003; 30: 49 -56. St. Lawrence, Montano et al. Amer J Public Health 2002; 92: 17841788.