PatientCentered Care Unit 7 Shared DecisionMaking Lecture a









- Slides: 21
Patient-Centered Care Unit 7: Shared Decision-Making Lecture a – Introduction This material (Comp 25 Unit 7) was developed by Columbia University, funded by the Department of Health and Human Services, Office of the National Coordinator for Health Information Technology under Award Number 90 WT 0006. This work is licensed under the Creative Commons Attribution-Non. Commercial-Share. Alike 4. 0 International License. To view a copy of this license, visit http: //creativecommons. org/licenses/by-nc-sa/4. 0/.

Shared Decision-Making Learning Objectives • Objective 1: Describe shared decisionmaking (Lecture a) • Objective 2: Explain the use of decision aids and how they facilitate shared decision-making (Lecture b) • Objective 3: Debate alternative strategies to implement decision aids within workflows (Lecture b) 2

What is shared decision-making? • Shared decision-making (SDM) is a collaborative process that allows patients and their providers to make health care decisions together, taking into account the best scientific evidence available, as well as the patient’s values and preferences – (Informed Medical Decisions Foundation) 3

When is SDM most appropriate? • Significant clinical uncertainty, ambiguity, or simply, the absence of evidence • “Equipoise”: when evidence for benefits and harms are closely balanced • In the context of clinical practice guidelines – When USPSTF (U. S. Preventive Services Task Force) recommendation is Grade C, the balance of benefits and harms at the population level is close and the net benefit is small 4
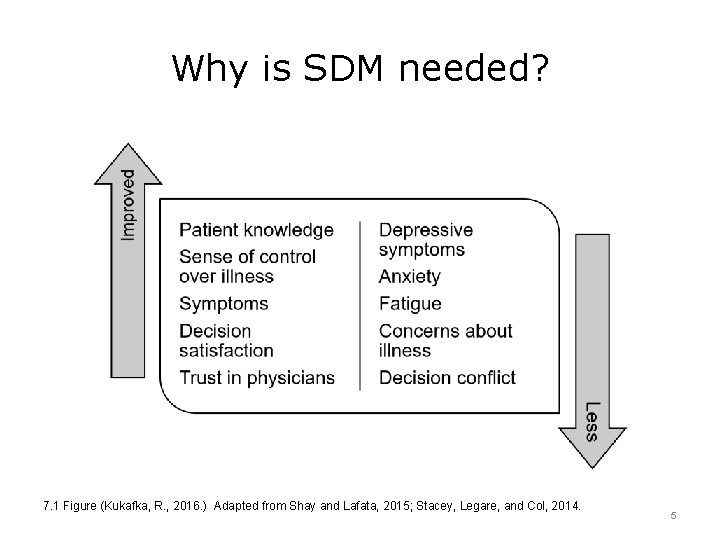
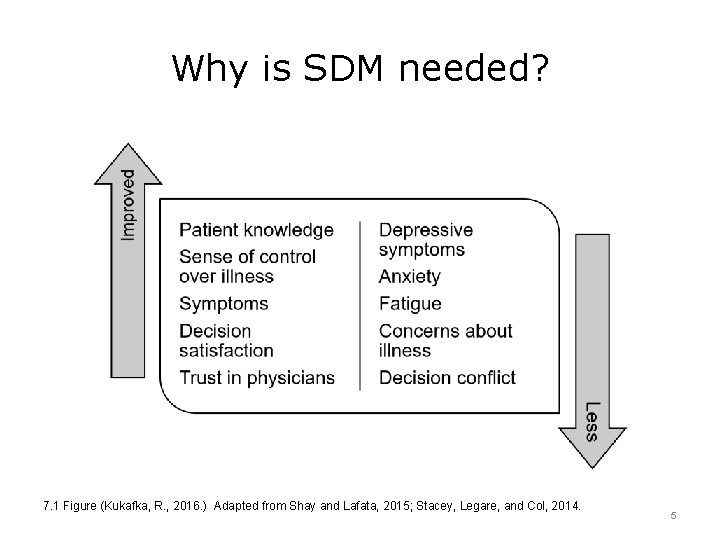
Why is SDM needed? 7. 1 Figure (Kukafka, R. , 2016. ) Adapted from Shay and Lafata, 2015; Stacey, Legare, and Col, 2014. 5

SDM is essential to quality health care • Good quality care requires that tests and procedures be medically appropriate and performed safely, but also reflects care that is desired by the patient • Preconditions for health care delivery emphasize SDM as mediator / moderator of health care quality • Helps providers implement evidence in a manner that reflects patients’ preferences • (Floyd, Fowler, Levin, and Sepucha, 2011) 6
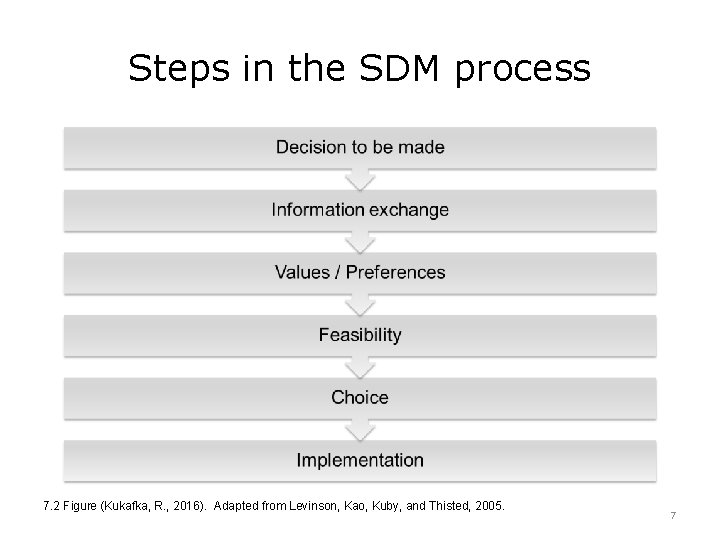
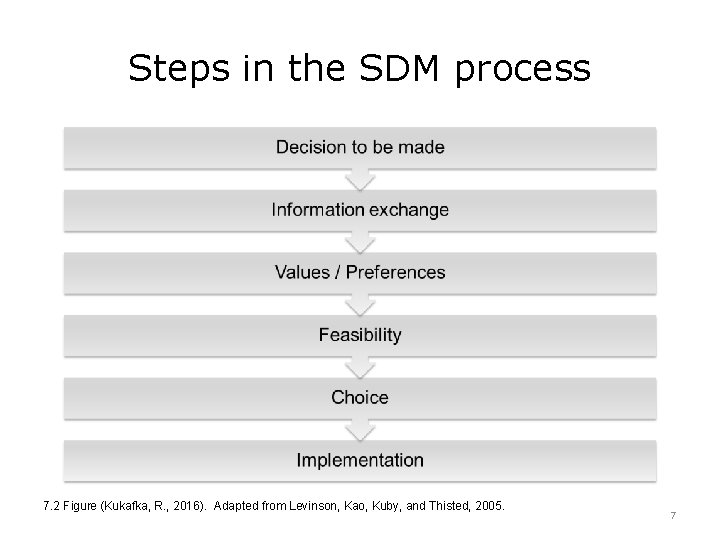
Steps in the SDM process 7. 2 Figure (Kukafka, R. , 2016). Adapted from Levinson, Kao, Kuby, and Thisted, 2005. 7
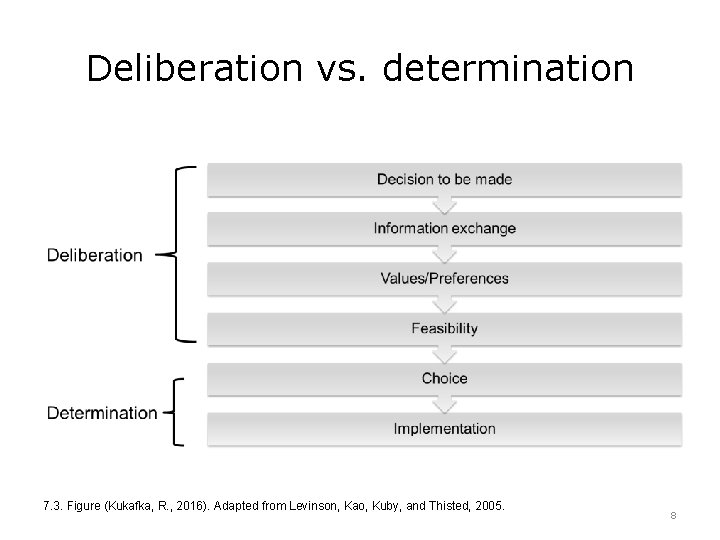
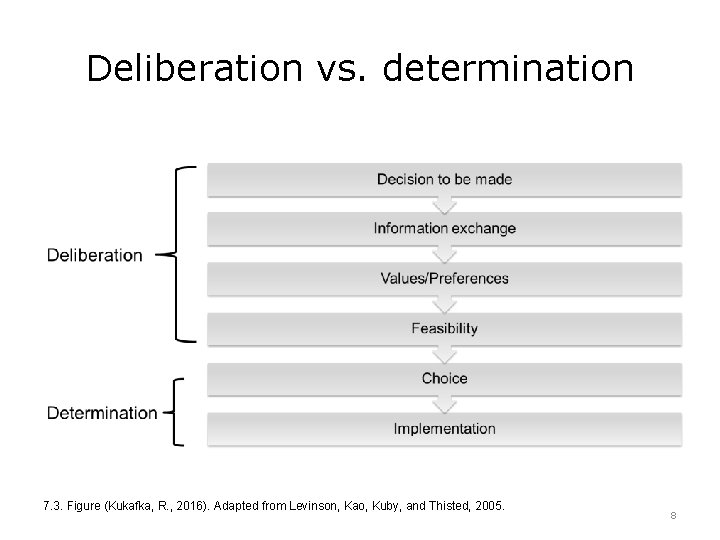
Deliberation vs. determination 7. 3. Figure (Kukafka, R. , 2016). Adapted from Levinson, Kao, Kuby, and Thisted, 2005. 8

Do patients want to engage in SDM? • In a national study of 3000 participants: – 96% of the respondents preferred to be offered choices about their care and asked for their preferences – 52% wanted to defer their decisions to their clinicians but still wanted to engage in deliberation about choice • Some patients may opt to defer their decision to providers, but they still want to be offered choices about their care and asked about their preferences • (Levinson, Kao, Kuby, and Thisted, 2005) 9
Misconceptions about SDM • Misconception #1: providers are already doing SDM – Physicians' inferences about patient values and preferences are often inaccurate, even among physicians with more clinical experience and longer patient-physician relationships – Therefore, engaging a patient in discussion of values and preferences is essential to avoid a “misdiagnosis” of patient preferences – (Mulley and Trimble, 2012; Street and Haidet, 2011) 10

Misconceptions about SDM (Cont’d – 1) • Misconception #2: SDM will increase health inequalities by excluding disadvantaged patients – Systematic review and meta-analysis of randomized controlled trials and observational studies do not confirm – Rather, disadvantaged groups may benefit from SDM more than groups of higher education and / or literacy – (Durand, Carpenter, Dolan, et al, 2014) 11
Misconceptions about SDM (Cont’d – 2) • Misconception #3: SDM takes too long – There is little evidence that SDM takes longer and actually there is conflicting evidence that use of a decision aid and SDM increases consultation times – One study found consultation increased by six minutes, another study found eight minute decrease – Therefore, there is no evidence that SDM systematically increases visits when compared with visits that do not include SDM – (O’Connor, Bennett, Stacey, et al, 2001; Bekker, Hewison, and Thorton, 2004; Green, Peterson, Baker, et al, 2005) 12
Misconceptions about SDM (Cont’d – 3) • Misconception #4: patient education will lead to SDM – Patients may not recognize feel that they have “expertise” to bring to the clinical encounter – It is important to consider not only patient knowledge, but also how much power and influence they feel they have in the decisionmaking process – (Joseph-Williams, Edwards, and Elwyn, 2014) 13

Interprofessional Shared Decision. Making (IP-SDM) Model • Addresses three levels within the health care system: – Micro-level (individual): patient’s health problem – – that requires a decision Meso-level (team/organization): health care teams within an organization Macro-level: broader policies and social contexts To see a visual of the IP-SDM model, please go to: https: //decisionaid. ohri. ca/docs/develop/IPSDM-Model. pdf (Stacey, Legare, and Pouliot, et al, 2010) 14
SBM is slow to become part of the clinical encounter • While the pendulum is swinging to more patient-centered health care and involvement of patients in decision-making, evidence shows that shared decision-making is slow to becoming part of the clinical consultation • Providers can learn to engage patients in shared decision-making as patients would prefer to have a more active role in decisionmaking 15
Unit 7: Shared Decision-Making, Summary – Lecture a, Introduction • Shared decision-making is a collaborative process that allows patients and their providers to make health care decisions together, taking into account the best scientific evidence available, as well as the patient’s values and preferences • Shared decision-making is important for health care quality, but should be used when appropriate • There is a process for shared decision-making, which includes deliberation and determination • There are some misconceptions about shared decision -making and there is slow adoption, but in general, patients would like to engage in decision-making 16

Shared Decision-Making References – Lecture a References Bekker, H. L. , Hewison, J. , & Thorton, J. G. (2004). Applying decision analysis to facilitate informed decision making about prenatal diagnosis for Down Syndrome: a randomised controlled trial. Prenat Diagn, 24, 4, 265 -275. Durand, M. -A. , Carpenter, L. , Dolan, H. , Bravo, P. , Mann, M. , Bunn, F. , & Elwyn, G. (2014). Do interventions designed to support shared decision-making reduce health inequalities? a systematic review and meta-analysis. PLo. S ONE, 9, 4), e 94670. Fowler Jr. , F. J. , Levin, C. A. , and Sepucha, K. R. (2011). The voice of patients: informing and involving patients to improve the quality of medical decisions. Health Aff, 30, 4699 -4706. Green, M. J. , Peterson, S. K, Baker, M. W. , Friedman, L. C. , Harper, G. R. , Rubinstein, W. S. , Peters, J. A. , & Mauger, D. T. (2005). Use of an educational computer program before genetic counseling for breast cancer susceptibility: effects on duration and content of counseling sessions. Genet Med, 7, 4, 221 -229. Informed Medical Decisions Foundation. Definition of shared decision-making. Available at www. informedmedicaldecisions. org/what-is-shared-decision-making/ Joseph-Williams, N. , Edwards, A. , & Elwyn, G. (2014). Power imbalance prevents shared decision making. BMJ, 348. 17
Shared Decision-Making References – Lecture a (Cont’d – 1) References Lee, C. N. , Dominik, R. , Levin, C. A. , Barry, M. J. , Cosenza, C. , O’Connor, A. M. , Mulley Jr. , A. G. , & Sepucha, K. R. (2010). Development of instruments to measure the quality of breast cancer treatment decisions. Health Expect, 13, 3, 258 -272. Levinson, W. , Kao, A. , Kuby, A. , & Thisted, R. A. (2005). Not all patients want to participate in decision making: a national study of public preferences. Journal of General Internal Medicine, 20, 6, 531– 535. Mulley, A. G. , Trimble, C. , & Elwyn, G. (2012). Stop the silent misdiagnosis: patients' preferences matter. BMJ, 345, e 6572. O’Connor, A. M. , Bennett, C. L. , Stacey, D. , Barry, M. , Col, N. F. , Eden, K. B. , Entwistle, V. A. , Fiset, V. , Holmes-Rovner, M. , Khangura, S. , Llewellyn-Thomas, H. , & Rovner, D. (2009). Cochrane Database Syst Rev, 8, 3. Legare, F. , Stacey, D, & IP Team. (2010) IP-SDM Model. Available at: https: //decisionaid. ohri. ca/docs/develop/IP-SDM-Model. pdf Rao, J. K. , Anderson, L. A. , Inui, T. S. , & Frankel, R. M. (2007). Communication interventions make a difference in conversations between physicians and patients: a systematic review of the evidence. Med Care, 45, 4, 340 -349. 18

Shared Decision-Making References – Lecture a (Cont’d – 2) References Shay, L. A. , & Lafata, J. E. (2015). Where is the evidence? A systematic review of shared decision-making and patient outcomes. Medical Decision Making, 35, 1, 114 -131. Stacey, D. , Legare, F. , Col, N. F. , Bennett, C. L. , Barry, M. J. , Eden, K. B. , Holmes-Rovner, M. , Llewellyn-Thomas, H. , Lyddiatt, A. , Thomson, R. , Trevena, L. , & Wu, J. H. (2014). Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. Stacey, D. , Legare, F. , Pouliot S. , Kryworuchko, J. , Dunn, S. (2010). Shared decision making models to inform an interprofessional perspective on decision making: a theory analysis. Patient Educ Couns, 80, 2, 164 -172. Street, R. & Jr, Haidet, P. (2011). How well do doctors know their patients? factors affecting physician understanding of patients' health beliefs. Journal of General Internal Medicine, 26, 21– 27. Weston, W. W. (2001). Informed and shared decision-making: the crux of patientcentered care. CMAJ, 165, 438 -439. 19
Shared Decision-Making References – Lecture a (Cont’d – 3) Charts, Tables, Figures 7. 1 Figure: Kukafka, R. (2016). Why is SDM needed? Used with permission. 7. 2 Figure: Kukafka, R. (2016). Steps in the SDM process. Used with permission. 7. 3 Figure: Kukafka, R. (2016). Deliberation vs. determination. Used with permission. 20
Unit 7: Shared Decision-Making, Lecture a – Introduction This material was developed by Columbia University, funded by the Department of Health and Human Services, Office of the National Coordinator for Health Information Technology under Award Number 90 WT 0006. 21