Patient Priorities Care Moving from diseasebased to patient
Patient Priorities Care: Moving from disease-based to patient priorities-aligned decisionmaking Mary Tinetti, MD, Professor of Medicine and Chief of Geriatrics, Yale School of Medicine Caroline Blaum, MD, MS, Director, Division of Geriatric Medicine and Palliative Care, NYU School of Medicine Mary Tinetti: @Goals. Drive. Care Caroline Blaum: @CBlaum. MD PPC: @Pt. Priorities Patient. Priorities. Care. org @Pt. Priorities © Mary Tinetti 2017

What is Patient Priorities Care? Moves decision-making & conversation from: Ø From: You need (fill in treatment) for your (fill in disease) Ø To: “Knowing all your conditions, your overall health, and your health outcome goals and care preferences, I suggest we try (fill in treatment option). © Mary Tinetti 2017
Patient Priorities Care • Is Not: • A new care model or treatment • Not limited to any care setting, disease, or health status • Is: • Approach to helping patients & clinicians make decisions aligned with what matters most to each patient © Mary Tinetti 2017

Patient Priorities Care • Member of health team helps patients identify their health priorities • Clinicians align their care with achieving these health priorities • Health priorities = each patient’s specific health outcome goals given their specific care preferences © Mary Tinetti 2017

What are health outcome goals? Health & life outcomes most desired Ø“SMART” goals (e. g. Babysit grandson 3 times/week; walk 2 blocks to poker game Ø Distinct from behavioral goals such as stop smoking or disease goals such as A 1 c or BP) © Mary Tinetti 2017
• …babysit my grandchildren each day to help my daughter while she works Examples • …be able to work outside in of Health garden and push a wheel Outcome barrel – fatigue makes this difficult Goals • …do ceramics again and walk ½ mile with my husband everyday—tiredness makes this difficult © Mary Tinetti 2017
What are care preferences**? • Health care utilization (e. g. # visits, hospitalizations; diagnostics) • Medication management (e. g. , complexity; adverse effects; costs) • Self-management tasks (e. g. , diet; monitor weights, bp, glucose) • Procedures (time, discomfort, anxiety, complications; time to recover) ** What patients are able to do and feels helps them achieve goals Boyd, Montori © Mary Tinetti 2017

Examples of care preferences: Helpful and doable © Mary Tinetti 2017 I go for blood work every month; it is not bothersome I walk & do the exercises that PT taught me every day CPAP helps Omeprazol e helps my reflux
Examples of care preference s: Not help or unable © Mary Tinetti 2017 • My medications are causing my muscle pain and makes it hard to walk and be active • I get hypoglycemic, I get weak and shaky. I’m taking too much of something • Ropinirole gives me hallucinations; doesn’t control my restless leg

Patient priorities decision-making & care is important because… • Care for many older adults with multiple conditions ØOf uncertain benefit (lack of evidence) ØBurdensome ØUnintentional harm ØFrustrating for clinicians • Individuals vary in health priorities in face of tradeoffs © Mary Tinetti 2017
To illustrate, Mr. A, an 83 -year-old man with fatigue, decreased appetite, weakness • Previous M. I. He thinks… • Diabetes • his medications are causing a lot of his symptoms • Hypertension • Heart failure (EF 28%) • Osteoporosis • Depression © Mary Tinetti 2017 • too much of his time involved in his health care
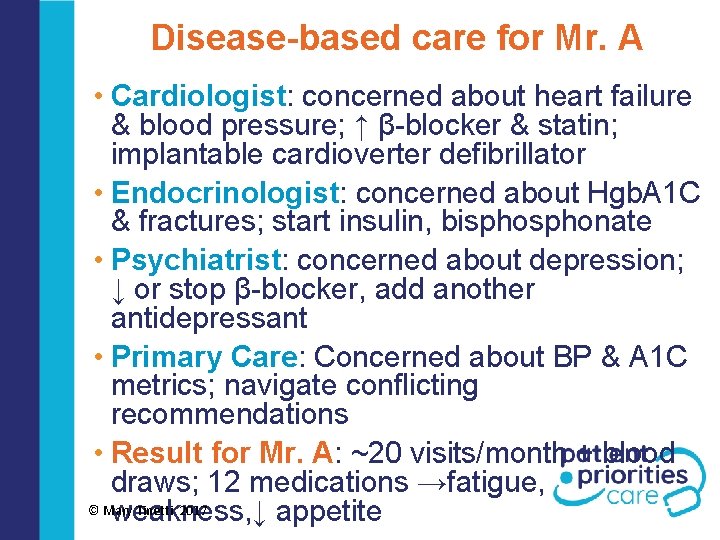
Disease-based care for Mr. A • Cardiologist: concerned about heart failure & blood pressure; ↑ β-blocker & statin; implantable cardioverter defibrillator • Endocrinologist: concerned about Hgb. A 1 C & fractures; start insulin, bisphonate • Psychiatrist: concerned about depression; ↓ or stop β-blocker, add another antidepressant • Primary Care: Concerned about BP & A 1 C metrics; navigate conflicting recommendations • Result for Mr. A: ~20 visits/month + blood draws; 12 medications →fatigue, © Mary Tinetti 2017 weakness, ↓ appetite

As Mr. A’s story shows…… • Care for older adults with multiple conditions : ØOf uncertain benefit (lack of evidence) ØNot focused on what matters most ØBurdensome; conflicting ØUnintentional harm ØFrustrating for patients & clinicians © Mary Tinetti 2017
Care may be of uncertain benefit • Few older adult with multiple conditions and functional limitations in RCTs • Persons with multiple conditions may have less benefit from treatments than RCTs With multiple conditions: what outcome defines benefit? © Mary Tinetti 2017

Care is not always aligned with what matters most … • Patients vary in their health outcome goals when faced with tradeoffs • Maintain function even if don’t life as long: 42% • Relief of symptoms like pain, dyspnea, fatigue: 32% • Stay alive even if less functional: 27% Fried TR • Patients vary in their care preferences / treatment burden tolerance (willing & able to do to achieve outcomes) Montori, Boyd © Mary Tinetti 2017

Care may be burdensome “ Caring for my chronic conditions is more burdensome than the conditions” (Montori; Boyd) © Mary Tinetti 2017
Care may be unintentionally harmful • 1 in 3 older adults receives a guidelinerecommended drug to help one condition that may worsen another one (Tinetti, 2014) • Older adults with multiple conditions face many tradeoffs and are at risk of adverse medication effects © Mary Tinetti 2017

Care can be frustrating for clinicians • Conflicting recommendations from colleagues who focus on a different disease • Patients don’t do what we want • Clinician thinks patient not adherent • Patient thinks “I cant do this” or “this won’t help me do what’s important” • Conflicts & frustration arise because different priorities (unspoken) © Mary Tinetti 2017

How can we work together to make Mr. A’s care… • Less burdensome & frustrating, and better focused on what matters most to him and his family? • Less expensive and fragmented for health systems and society? • Less frustrating for the clinicians who care for people like Mr. A? © Mary Tinetti 2017
Answer: Patient Priorities Care © Mary Tinetti 2017

A bridge between: Disease-based decision-making & and care © Mary Tinetti 2017 Decision-making & care based on what matters most to patients
For whom is patient priorities care most helpful? • Appropriate for everyone • Multiple conditions and multiple clinicians • Getting conflicting recommendations • Feeling burdened by care • Uncertain benefit of guideline-based care © Mary Tinetti 2017

The number of people in each of the above 3 groups may vary depending on the population and the specific comorbidities or advanced disease. The model is intended to demonstrate that there is a substantial group of older adults (uncertain) for whom guideline-driven care or advanced disease care is of uncertain benefit or not appropriate. Blaum, et al JAGS 2018. © Mary Tinetti 2017

Can Patient Priorities Care be implemente d in practice? 2015 -2018 © Mary Tinetti 2017
Patient Priorities Care: Pilot • Process: • Activate & train patients & clinicians • Address workflow, practice change, decision-making • Locations: 10 primary care providers & 5 cardiologists in central CT. • Evaluation: Patient, clinician, health system outcomes: PPC vs. usual care © Mary Tinetti 2017
Progress building Patient Priorities Care: • Feasible process for helping patients identify their SMART health outcome goals and care preferences • Workflow for incorporating patient priorities care into clinical practice • Identified challenges faced in aligning care with patient’s goals & preferences • Main challenge: Translating goals & preferences into care decisions © Mary Tinetti 2017

Develop & Implement (Translating prototype into practice): © Mary Tinetti 2017 What does health system need to do? What do patients need to do? What do clinicians need to do?
What patients need to know & do © Mary Tinetti 2017 Know: • Their health priorities: • Health outcomes most important in face of tradeoffs • What willing and able to do (healthcare preferences) • Do: • Active partner in decisions with their clinicians • Do what say they willing and able to do
Specific Ask (One thing) • Specific ask (One Thing): If we could change one thing about my health or healthcare, it would be: My arthritis pain in my hands so that I can: cook and cut up things easier, it is hard • I want to be less tired so that I can: walk more with my husband have more energy in the mornings © Mary Tinetti 2017
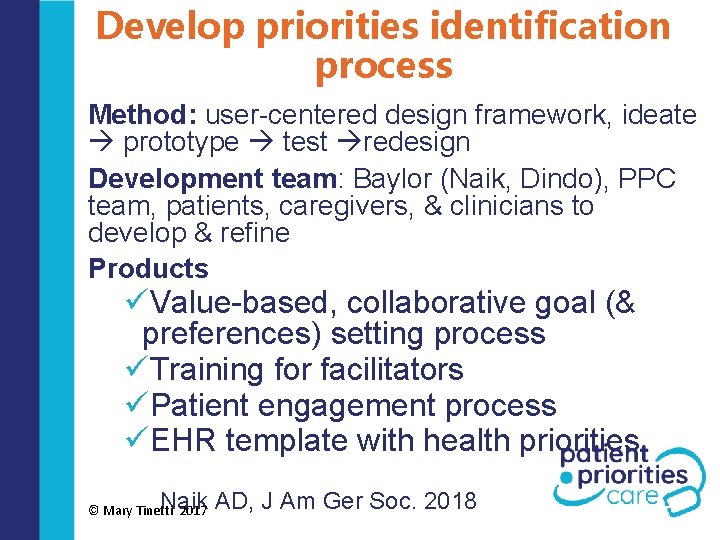
Develop priorities identification process Method: user-centered design framework, ideate prototype test redesign Development team: Baylor (Naik, Dindo), PPC team, patients, caregivers, & clinicians to develop & refine Products üValue-based, collaborative goal (& preferences) setting process üTraining for facilitators üPatient engagement process üEHR template with health priorities Naik AD, J Am Ger Soc. 2018 © Mary Tinetti 2017

Patient priorities identified Member of care team help patients: • Clarify Values • Set SMART Goals • Identify healthcare preferences • Engage actively in their healthcare © Mary Tinetti 2017
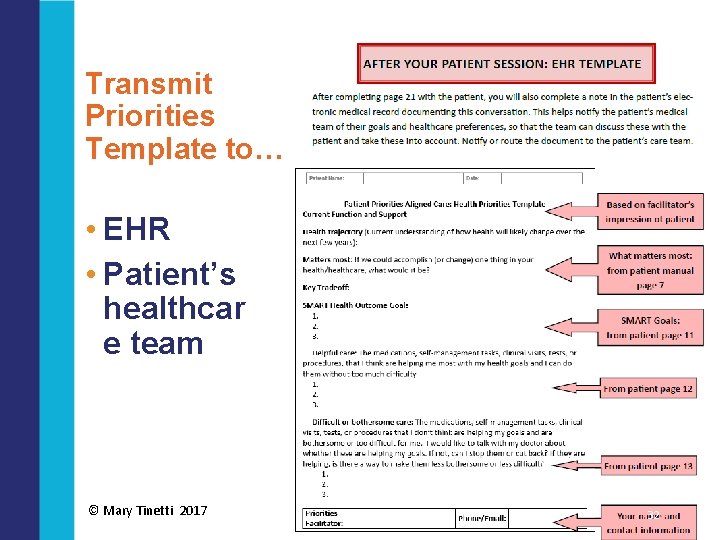
Transmit Priorities Template to… • EHR • Patient’s healthcar e team © Mary Tinetti 2017 32

• Know: Patients’ outcome goals & healthcare preferences What clinicians • Do: • Engage patient, caregiver, & need to other clinicians in decision know & making aligned with do priorities • Stop, start, or continue care aligned with patients' goals & preferences, health trajectory © Mary Tinetti 2017
How do clinicians align care with patient priorities? : Methods Ø Participant observation ØCoaching huddles; emergent learning Ø PPC team, training experts (ACP, Baylor), clinicians Ø 21 huddles (36 patients discussed) ØIdentify key challenges & strategies Tinetti ME et al. submitted © Mary Tinetti 2017
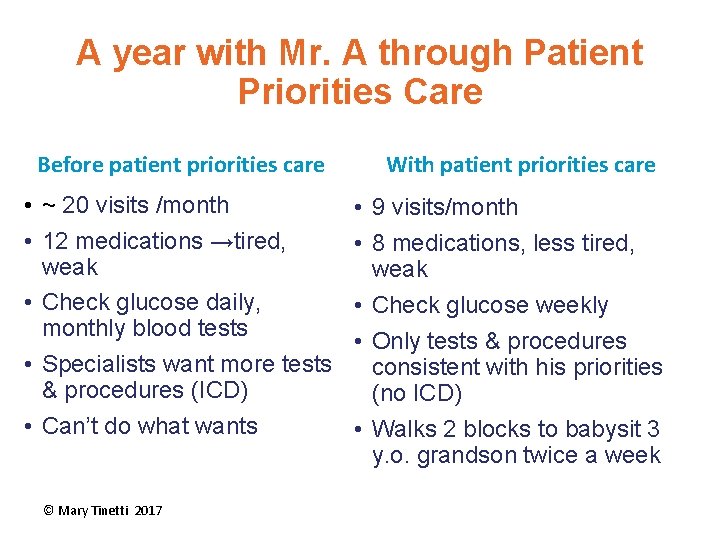
A year with Mr. A through Patient Priorities Care Before patient priorities care • ~ 20 visits /month • 12 medications →tired, weak • Check glucose daily, monthly blood tests • Specialists want more tests & procedures (ICD) • Can’t do what wants © Mary Tinetti 2017 With patient priorities care • 9 visits/month • 8 medications, less tired, weak • Check glucose weekly • Only tests & procedures consistent with his priorities (no ICD) • Walks 2 blocks to babysit 3 y. o. grandson twice a week

How to align decisions & care with priorities? Key Challenges… © Mary Tinetti 2017
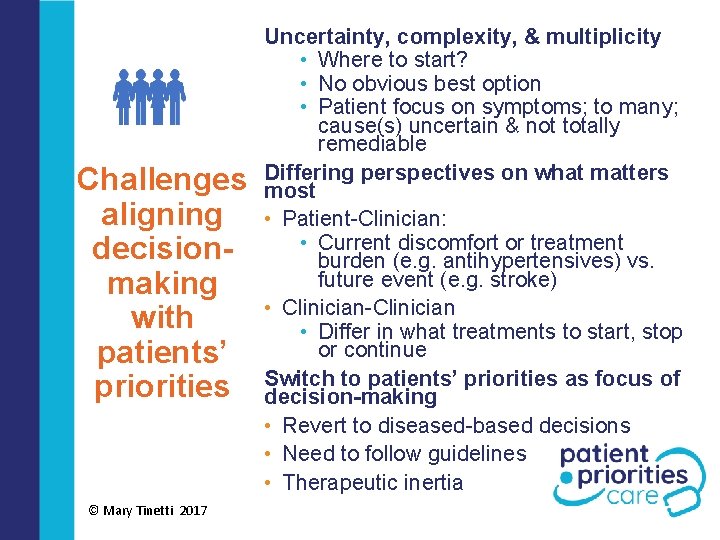
Challenges aligning decisionmaking with patients’ priorities © Mary Tinetti 2017 Uncertainty, complexity, & multiplicity • Where to start? • No obvious best option • Patient focus on symptoms; to many; cause(s) uncertain & not totally remediable Differing perspectives on what matters most • Patient-Clinician: • Current discomfort or treatment burden (e. g. antihypertensives) vs. future event (e. g. stroke) • Clinician-Clinician • Differ in what treatments to start, stop or continue Switch to patients’ priorities as focus of decision-making • Revert to diseased-based decisions • Need to follow guidelines • Therapeutic inertia

Other Challenges • Disconnect between goal (outcome desired) and preferences (what able/willing to do) • Unrealistic or unachievable goals • Care preferences vague and not actionable • Acute decision not addressed in patient’s priorities © Mary Tinetti 2017

How to align decisions & care with priorities? Strategies that emerged… © Mary Tinetti 2017
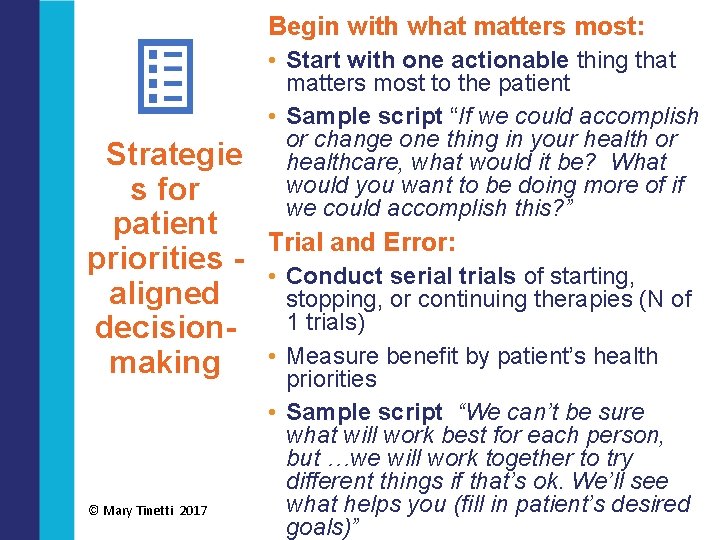
Begin with what matters most: • Start with one actionable thing that matters most to the patient • Sample script “If we could accomplish or change one thing in your health or healthcare, what would it be? What would you want to be doing more of if we could accomplish this? ” Strategie s for patient Trial and Error: priorities - • Conduct serial trials of starting, aligned stopping, or continuing therapies (N of 1 trials) decisionbenefit by patient’s health making • Measure priorities © Mary Tinetti 2017 • Sample script “We can’t be sure what will work best for each person, but …we will work together to try different things if that’s ok. We’ll see what helps you (fill in patient’s desired goals)”
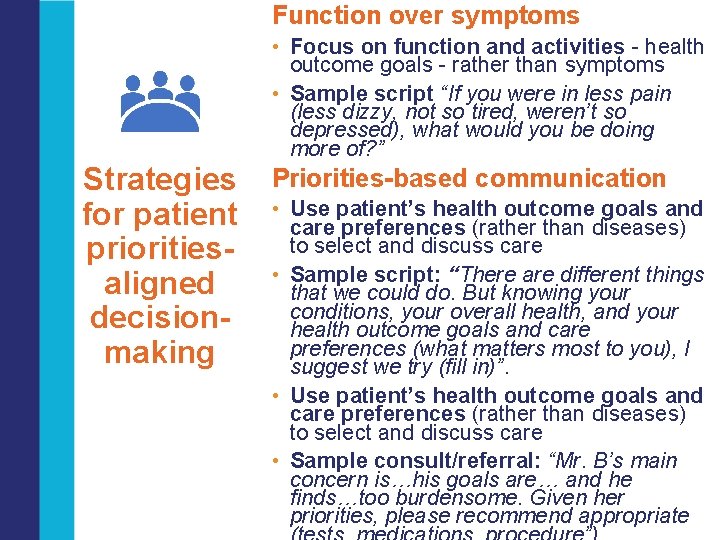
Function over symptoms • Focus on function and activities - health outcome goals - rather than symptoms • Sample script “If you were in less pain (less dizzy, not so tired, weren’t so depressed), what would you be doing more of? ” Strategies for patient prioritiesaligned decisionmaking Priorities-based communication • Use patient’s health outcome goals and care preferences (rather than diseases) to select and discuss care • Sample script: “There are different things that we could do. But knowing your conditions, your overall health, and your health outcome goals and care preferences (what matters most to you), I suggest we try (fill in)”. • Use patient’s health outcome goals and care preferences (rather than diseases) to select and discuss care • Sample consult/referral: “Mr. B’s main concern is…his goals are… and he finds…too burdensome. Given her priorities, please recommend appropriate
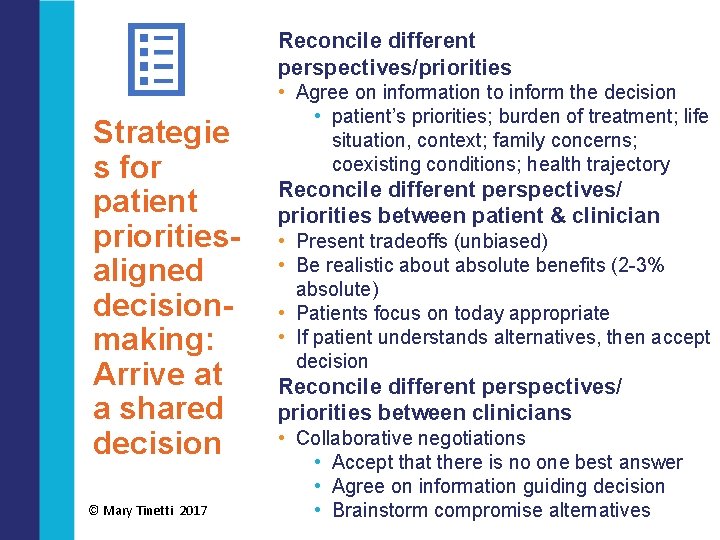
Reconcile different perspectives/priorities Strategie s for patient prioritiesaligned decisionmaking: Arrive at a shared decision © Mary Tinetti 2017 • Agree on information to inform the decision • patient’s priorities; burden of treatment; life situation, context; family concerns; coexisting conditions; health trajectory Reconcile different perspectives/ priorities between patient & clinician • Present tradeoffs (unbiased) • Be realistic about absolute benefits (2 -3% absolute) • Patients focus on today appropriate • If patient understands alternatives, then accept decision Reconcile different perspectives/ priorities between clinicians • Collaborative negotiations • Accept that there is no one best answer • Agree on information guiding decision • Brainstorm compromise alternatives

Feedback from pilot participants What do patients think? “… I don't always know the wisest thing to focus on. Helps to discuss things to make up your mind. It also gives you options about what you can do to make your life and health better. ” What do clinicians think? “…because I know what matters to her more than my goal to preserve her kidney function, I didn’t just increase her Lisinopril or something else I may have done. . . ” “ This helps my relationship but I still get measured on BP, BMI, A 1 C…” © Mary Tinetti 2017
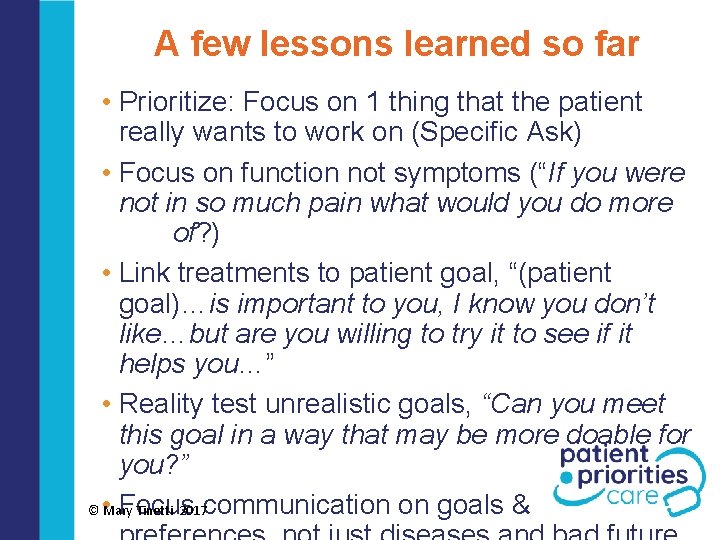
A few lessons learned so far • Prioritize: Focus on 1 thing that the patient really wants to work on (Specific Ask) • Focus on function not symptoms (“If you were not in so much pain what would you do more of? ) • Link treatments to patient goal, “(patient goal)…is important to you, I know you don’t like…but are you willing to try it to see if it helps you…” • Reality test unrealistic goals, “Can you meet this goal in a way that may be more doable for you? ” Focus © • Mary Tinetti 2017 communication on goals &
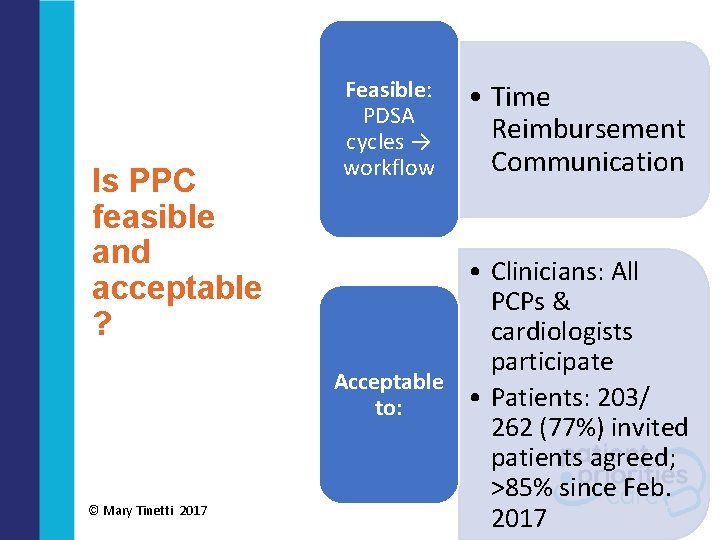
Is PPC feasible and acceptable ? © Mary Tinetti 2017 Feasible: PDSA cycles → workflow • Time Reimbursement Communication • Clinicians: All PCPs & cardiologists participate Acceptable • Patients: 203/ to: 262 (77%) invited patients agreed; >85% since Feb. 2017

Products to support Patient Priorities Care • Online curriculum to prepare health systems, clinicians, patients (with ACP) – in development • Training & point-of-care materials for patients & priorities facilitators • Decisional and communication tools (tips & scripts) for clinicians • AGS/ACP/ACC multiple chronic conditions (how to) action steps – in development • Future: patient priorities app; mentorship program *All current products available at Patient. Prioirities. Care. org © Mary Tinetti 2017

Patient. Priorities. Care. org: check back soon & often © Mary Tinetti 2017
- Slides: 47