PATIENT PRESENTATION By Kara Le Clair Social History
PATIENT PRESENTATION By Kara Le. Clair
Social History Initials: ER Age: 38 Gender: M Pt lives at home alone, Remote heroin use Tobacco use of ½ ppd No reported ETOH Employed DNR/DNI
Anthropometrics Ht: 5’ 9” Wt: 206 lbs (dry wt) � 179 lbs at admission BMI: overweight – � this is more than likely not accurate as pt suffers from anasarca and ascites IBW: 172 lbs %IBW: 120% UBW: 200 lbs %UBW: 103%
Medical history Hepatitis C Liver cirrhosis Hyperkalemia Ascites Upper extremity DVT Anasarca Upper GI bleed Heaptorenal syndrome Thrombocytopenia
Diagnosis End Stage Renal Disease � Kidney is unable to excrete waste product, maintain fluid and electrolytes and hormone balance Liver Cirrhosis Common with Hepatitis C (causes inflammation) � Chronic liver damage � Leads to scarring and liver failure � Result of Hepatorenal syndrome Renal failure occurs as result of severe liver disease � No underlying kidney problems � May require dialysis �

Physical Signs Ascites Very cachexic Bitemporal wasting Sallow skin Weaping wounds on LE Pt. is verbal but mumbles and can be difficult to understand Braden Scale: 15 - at risk
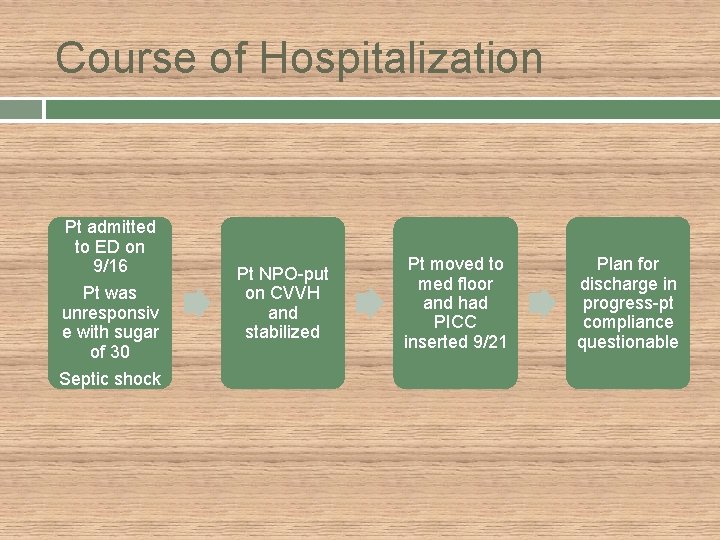
Course of Hospitalization Pt admitted to ED on 9/16 Pt was unresponsiv e with sugar of 30 Septic shock Pt NPO-put on CVVH and stabilized Pt moved to med floor and had PICC inserted 9/21 Plan for discharge in progress-pt compliance questionable
CVVH Continuous Veno-Venous Hemofiltration Intended for short-term ICU use Used for pts with low BP who are too sick for regular dialysis Dialysis catheter with two lines used � One line carries blood out of body, to CVVH machine where fluid waste is removed � Fluid and electrolytes are replace and blood returns via catheter
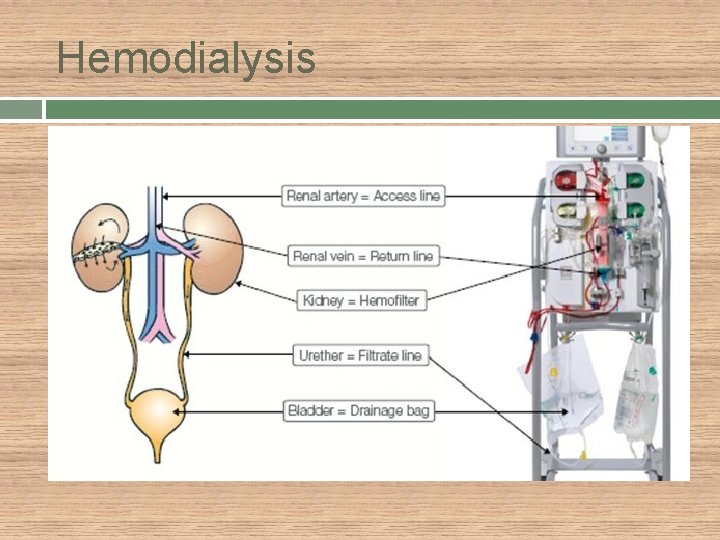
Hemodialysis

Medical Nutrition Therapy Dialysis requires higher protein intake Total energy needs should be high enough to spare protein Fluid, potassium, phosphorus and sodium should be restricted
Nutrition Education Pt. was provided with a packet of highlighted materials, printed from the AND website, providing a fair amount of information on what foods to eat/avoid with dialysis treatment. Pt was aware that he should not be eating high potassium foods and requested information on what he should and should not be eating. When pt was interviewed he had left his fruit salad on his tray because he remembered the nurse saying he should not eat melons.
Diet Order Present Diet Order: High calorie, high protein, 2 gm Na restriction, enlive supplement Previous Diet Order: Pt was NPO x 6 upon admission

Medications Heparin: anticoagulant Methadone: analglesic, narcotic, opioid Midodrine HCL: vasopressor/antihypotensive Protonil: pronton pump inhibitor-antiulcer, antigerd, antisecretory Sandostatin: oroctreotide- antidiarrheal (in HIV) Albumin (human): treatement for hypoalbuminia Lactulose: laxative Ventolin: albuterol- bronchodilator Zofran: ondansetron- antiemetic, antinauseant Multivitamin: pt malnourished d/t NPO x 6 while in ED Folic acid: B complex vitamin, antianemic Thiamine Calcium Glucose: phosphate binder Mg Sulfate: should improve pt levels, may be r/t kidney disease or general malnutrition/illness Potassium Phosphate
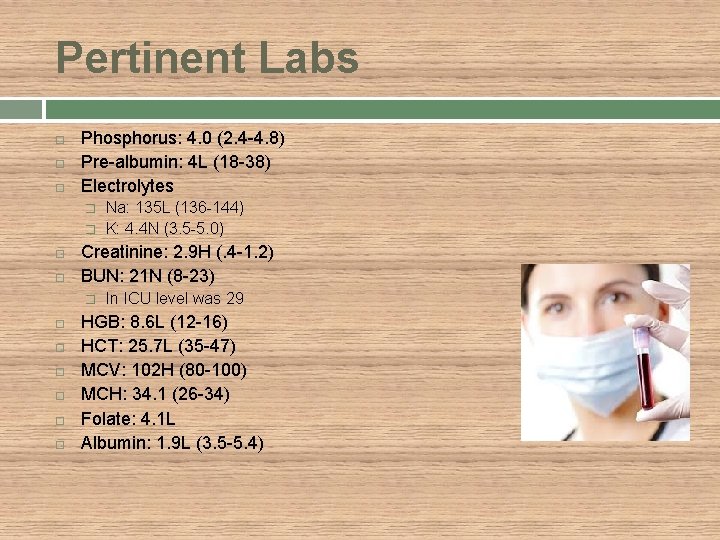
Pertinent Labs Phosphorus: 4. 0 (2. 4 -4. 8) Pre-albumin: 4 L (18 -38) Electrolytes � � Creatinine: 2. 9 H (. 4 -1. 2) BUN: 21 N (8 -23) � Na: 135 L (136 -144) K: 4. 4 N (3. 5 -5. 0) In ICU level was 29 HGB: 8. 6 L (12 -16) HCT: 25. 7 L (35 -47) MCV: 102 H (80 -100) MCH: 34. 1 (26 -34) Folate: 4. 1 L Albumin: 1. 9 L (3. 5 -5. 4)

PES Statement Pt has malnutrition r/t early satiety from cirrhosis as evidenced by decreased body weight of 15% in past 3 months, low albumin, reported poor appetite, N/V, muscle wasting.
Monitor/Evaluation Food/Nutrition Related Outcomes � Pt will consume more small frequent meals throughout the day and consume at at least 75% of each meal. Pt will consume 75% of an Enlive can TID. Anthropometric Measurement Outcomes � Pt weight should be monitored daily for water retention. Ascites should be monitored closely-pt has distended abdomen. Biochemical Data, Medical Tests, and Procedure � Monitor phosphorus, pre-albumin, electrolytes, MCV, HGB, HCT and folate. � Ideally, pt will reach a stable enough state where he will not require dialysis long-term.
Monitor/Evaluation Nutrition-Focused Physical Findings � Pt’s malnutrition will improve, wounds will heal with proper protein intake and care, edema and ascites will decrease and be stable, allowing the pt’s appetite to improve. Nutrition Education Outcomes � Pt will be able to state 3 foods high in potassium. � Pt. will be able to state 3 fruits/vegetables low in potassium. � Pt. will list 4 high protein foods he will include in his diet.
Coordination of Care Plans are being made for pt discharge Advised that pt enter rehab center for aid in wound healing Pt wants to return home despite inability to change dressings himself Concern for infection Methadone dispensing
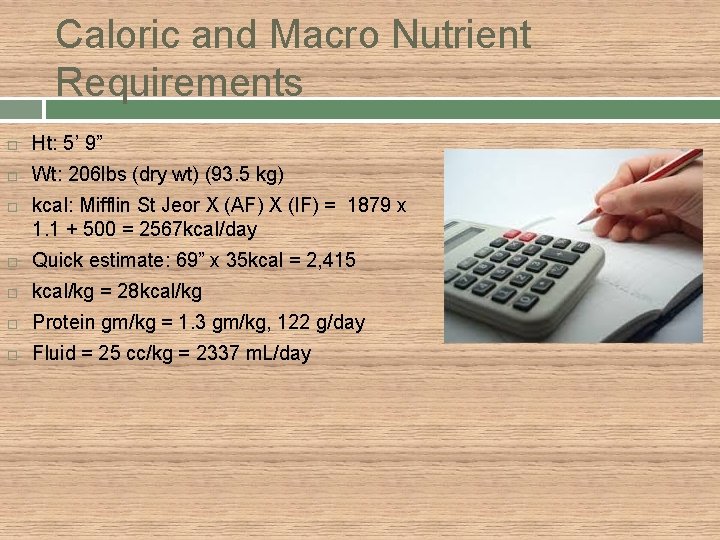
Caloric and Macro Nutrient Requirements Ht: 5’ 9” Wt: 206 lbs (dry wt) (93. 5 kg) kcal: Mifflin St Jeor X (AF) X (IF) = 1879 x 1. 1 + 500 = 2567 kcal/day Quick estimate: 69” x 35 kcal = 2, 415 kcal/kg = 28 kcal/kg Protein gm/kg = 1. 3 gm/kg, 122 g/day Fluid = 25 cc/kg = 2337 m. L/day
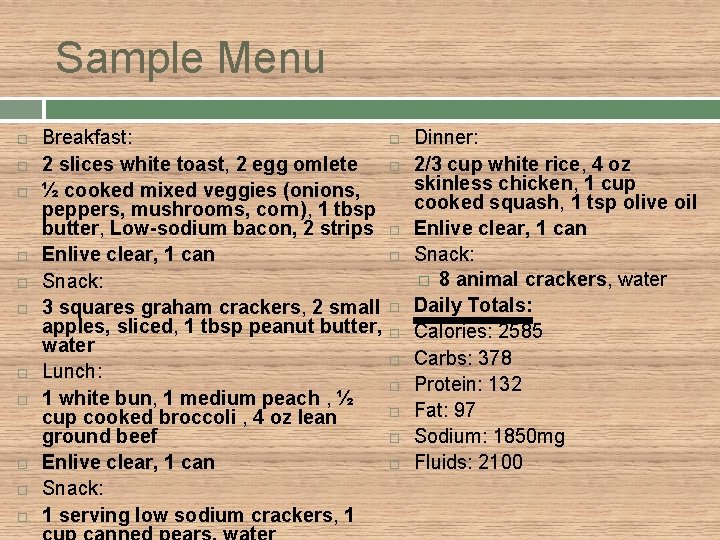
Sample Menu Breakfast: 2 slices white toast, 2 egg omlete ½ cooked mixed veggies (onions, peppers, mushrooms, corn), 1 tbsp butter, Low-sodium bacon, 2 strips Enlive clear, 1 can Snack: 3 squares graham crackers, 2 small apples, sliced, 1 tbsp peanut butter, water Lunch: 1 white bun, 1 medium peach , ½ cup cooked broccoli , 4 oz lean ground beef Enlive clear, 1 can Snack: 1 serving low sodium crackers, 1 Dinner: 2/3 cup white rice, 4 oz skinless chicken, 1 cup cooked squash, 1 tsp olive oil Enlive clear, 1 can Snack: � 8 animal crackers, water Daily Totals: Calories: 2585 Carbs: 378 Protein: 132 Fat: 97 Sodium: 1850 mg Fluids: 2100
References Guidelines for Estimating Fluid Needs. East Hartford: Riverside Health and Rehabilitation Center, 2014. Mahan, L. Kathleen. , Sylvia Escott-Stump, Janice L. Raymond, and Marie V. Krause's Food & the Nutrition Care Process. St. Louis, MO: Elsevier/Saunders, 2012. Print. http: www. myfitnesspal. com Pronsky, Zaneta M. , and Jeanne P. Crowe. Food Medication Interactions. Birchrunville, Penn. : Food-Medication Interactions, 2010. Print. *All images obtained from Google search engine
Questions
- Slides: 22