Patient Management with LDL Particle Number and Traditional

Patient Management with LDL Particle Number and Traditional Lipid Values William Cromwell, MD FAHA, FNLA
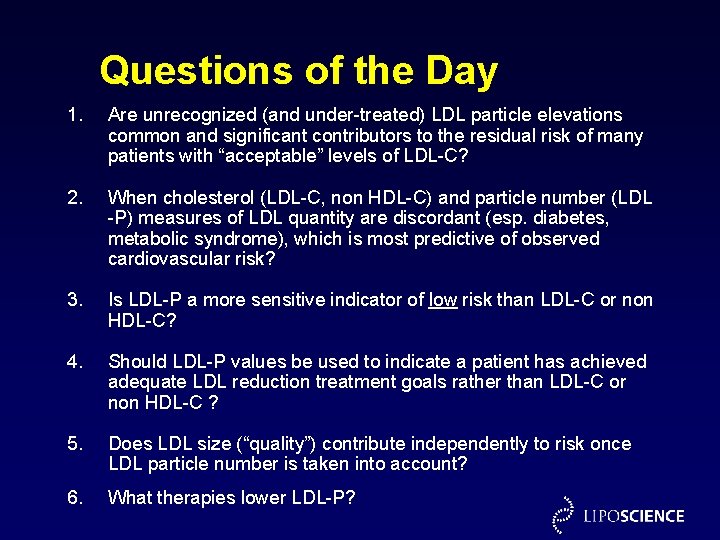
Questions of the Day 1. Are unrecognized (and under-treated) LDL particle elevations common and significant contributors to the residual risk of many patients with “acceptable” levels of LDL-C? 2. When cholesterol (LDL-C, non HDL-C) and particle number (LDL -P) measures of LDL quantity are discordant (esp. diabetes, metabolic syndrome), which is most predictive of observed cardiovascular risk? 3. Is LDL-P a more sensitive indicator of low risk than LDL-C or non HDL-C? 4. Should LDL-P values be used to indicate a patient has achieved adequate LDL reduction treatment goals rather than LDL-C or non HDL-C ? 5. Does LDL size (“quality”) contribute independently to risk once LDL particle number is taken into account? 6. What therapies lower LDL-P?
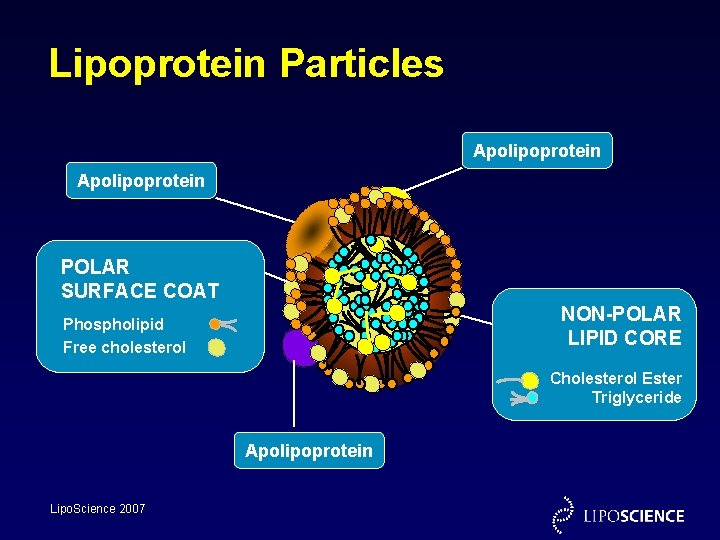
Lipoprotein Particles Apolipoprotein POLAR SURFACE COAT NON-POLAR LIPID CORE Phospholipid Free cholesterol Cholesterol Ester Triglyceride Apolipoprotein Lipo. Science 2007
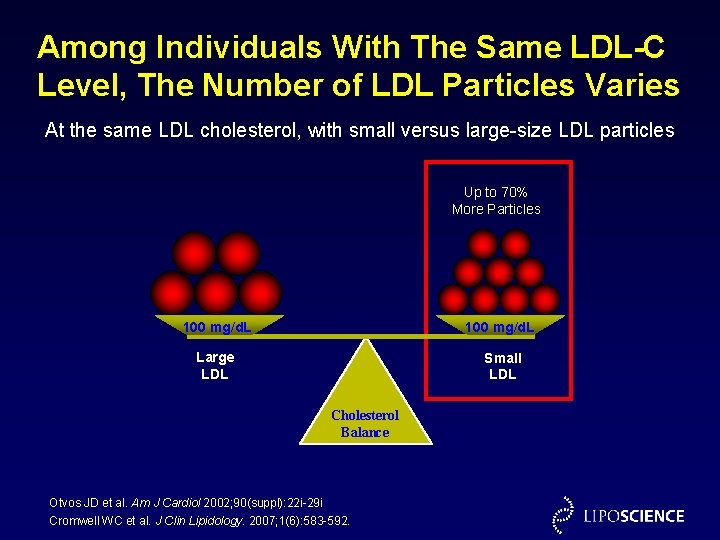
Among Individuals With The Same LDL-C Level, The Number of LDL Particles Varies At the same LDL cholesterol, with small versus large-size LDL particles Up to 70% More Particles 100 mg/d. L Large LDL Small LDL Cholesterol Balance Otvos JD et al. Am J Cardiol 2002; 90(suppl): 22 i-29 i Cromwell WC et al. J Clin Lipidology. 2007; 1(6): 583 -592.
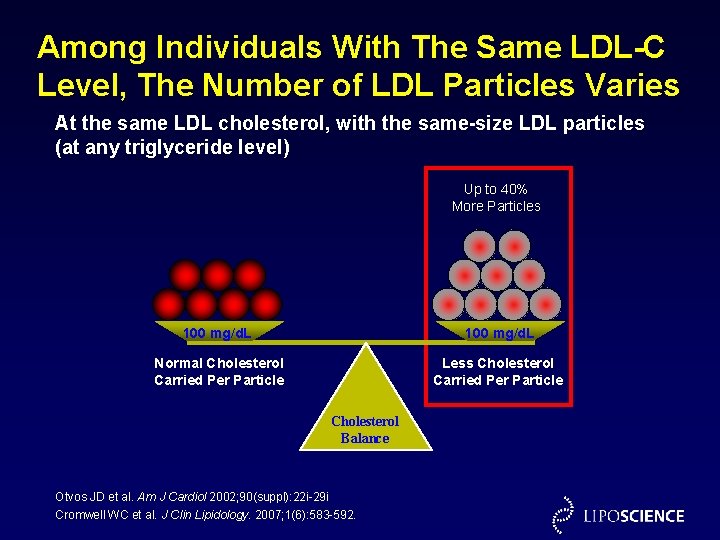
Among Individuals With The Same LDL-C Level, The Number of LDL Particles Varies At the same LDL cholesterol, with the same-size LDL particles (at any triglyceride level) Up to 40% More Particles 100 mg/d. L Normal Cholesterol Carried Per Particle Less Cholesterol Carried Per Particle Cholesterol Balance Otvos JD et al. Am J Cardiol 2002; 90(suppl): 22 i-29 i Cromwell WC et al. J Clin Lipidology. 2007; 1(6): 583 -592.
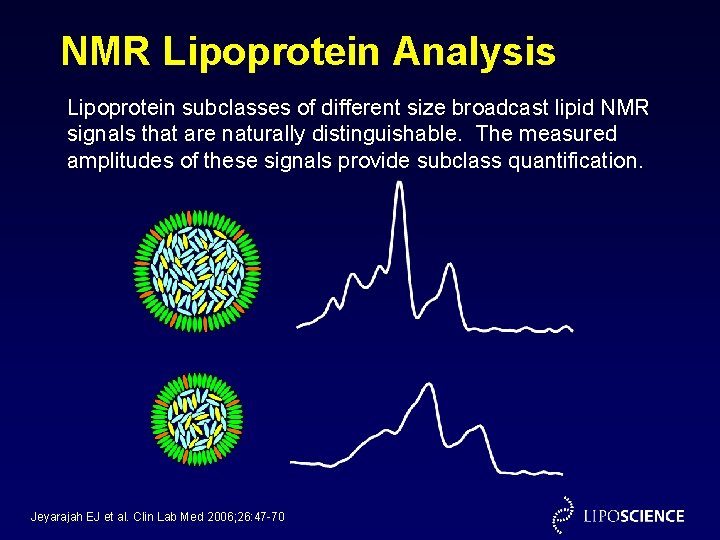
NMR Lipoprotein Analysis Lipoprotein subclasses of different size broadcast lipid NMR signals that are naturally distinguishable. The measured amplitudes of these signals provide subclass quantification. Jeyarajah EJ et al. Clin Lab Med 2006; 26: 47 -70
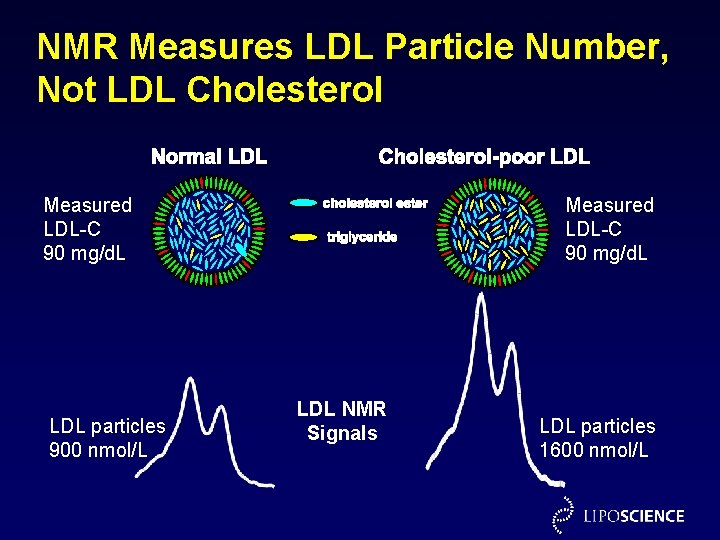
NMR Measures LDL Particle Number, Not LDL Cholesterol Measured LDL-C 90 mg/d. L LDL particles 900 nmol/L Measured LDL-C 90 mg/d. L LDL NMR Signals LDL particles 1600 nmol/L

Relations of LDL Particles and LDL Cholesterol to Levels of HDL Cholesterol and Triglycerides LDL Particles (nmol/L) LDL Particles LDL Cholesterol HDL Cholesterol (mg/d. L) Cromwell WC and Otvos JD. Curr Athero Reports 2004; 6: 381 -387 LDL Particles LDL Cholesterol Triglycerides (mg/d. L) LDL Cholesterol (mg/d. L) Framingham Offspring Study
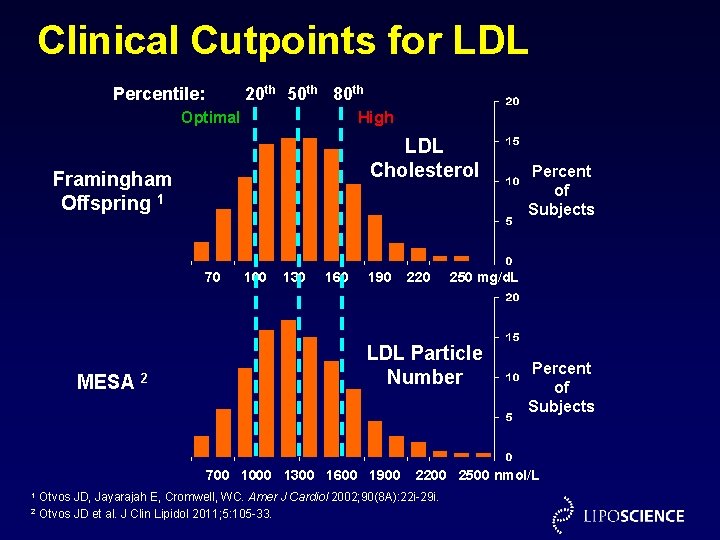
Clinical Cutpoints for LDL Percentile: 20 th 50 th 80 th Optimal High LDL Cholesterol Framingham Offspring 1 70 MESA 2 100 130 160 190 2 250 mg/d. L LDL Particle Number 700 1000 1300 1600 1900 1 220 Percent of Subjects 2200 2500 nmol/L Otvos JD, Jayarajah E, Cromwell, WC. Amer J Cardiol 2002; 90(8 A): 22 i-29 i. Otvos JD et al. J Clin Lipidol 2011; 5: 105 -33.
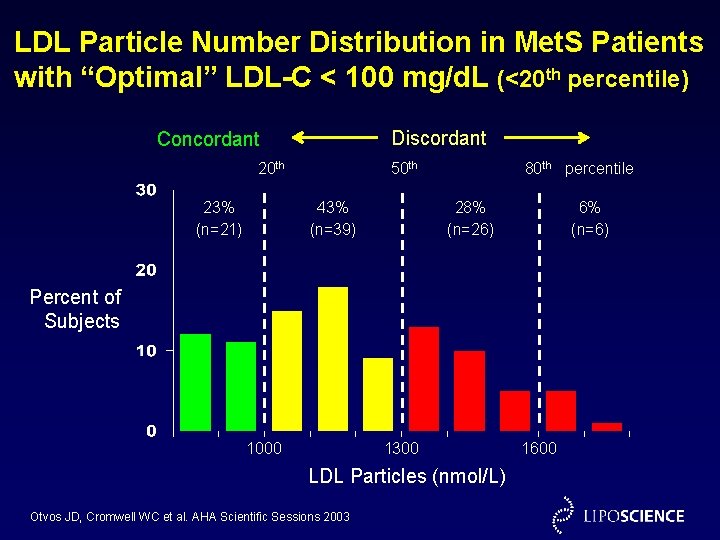
LDL Particle Number Distribution in Met. S Patients with “Optimal” LDL-C < 100 mg/d. L (<20 th percentile) Discordant Concordant 20 th 23% (n=21) 50 th 43% (n=39) 80 th percentile 28% (n=26) 6% (n=6) Percent of Subjects 1000 1300 LDL Particles (nmol/L) Otvos JD, Cromwell WC et al. AHA Scientific Sessions 2003 1600
LDL Particle Number is Highly Heterogeneous Among Patients with Type 2 Diabetes Mellitus at LDL Cholesterol Target Goal <100 mg/d. L W. C. Cromwell and J. D. Otvos American Journal of Cardiology 2006; 98: 1599 -1602
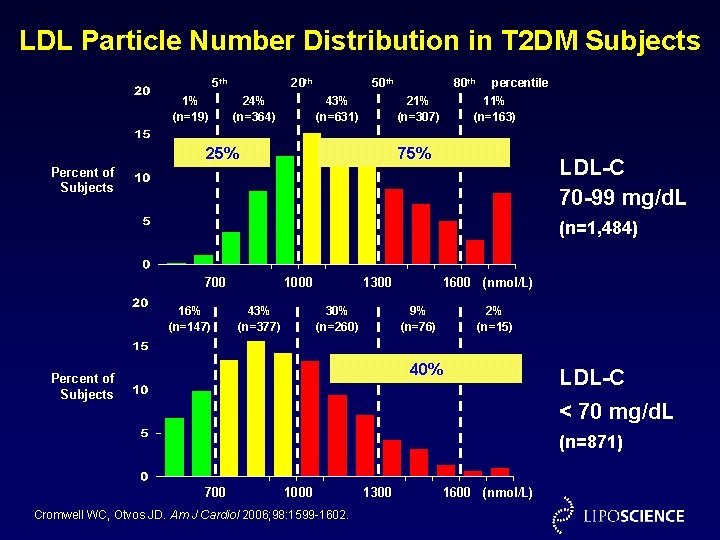
LDL Particle Number Distribution in T 2 DM Subjects 5 th 1% (n=19) 20 th 24% (n=364) 50 th 43% (n=631) 80 th 21% (n=307) 25% percentile 11% (n=163) 75% LDL-C 70 -99 mg/d. L Percent of Subjects (n=1, 484) 700 16% (n=147) 1000 43% (n=377) 1300 30% (n=260) 1600 (nmol/L) 9% (n=76) 2% (n=15) 40% Percent of Subjects LDL-C < 70 mg/d. L (n=871) 700 1000 Cromwell WC, Otvos JD. Am J Cardiol 2006; 98: 1599 -1602. 1300 1600 (nmol/L)
Relations of LDL Particle Number with CHD Outcomes
Alternate Measures of LDL Quantity are Not Equivalent The cholesterol in LDL (LDL-C) does not equate to the number of LDL particles (LDL-P) because the cholesterol content per LDL particle is highly variable. Concordance and discordance refer to when LDL-C and LDL-P levels agree or disagree. – When LDL-C and LDL-P are concordant (ie. , equally high or low), either LDL measure is an equally good guide to LDL treatment decision-making. – When LDL-C and LDL-P are discordant (ie. , one is lower or higher than the other), which LDL measure should guide clinical decision-making?
Ann Intern Med 2008; 149: 816 -22. Principles for determining when a new test is a better reference measure than the current “standard” test: 1) Value of the new reference test is best examined in cases of disagreement (discordance) between the new and standard tests.
Ann Intern Med 2008; 149: 816 -22. Principles for determining when a new test is a better reference measure than the current “standard” test: 2) Clinical consequences of disagreements between new and standard test requires a fair “umpire” test. 3) Fair umpire tests include clinical events or disease progression.

Outcome Associations of LDL Particle Number (Apo. B) versus LDL Cholesterol (LDL-C) 1. Even in high TG patients, more than 90% of total plasma apo. B is associated with LDL particles, except in type III hyperlipidemia [1, 2] 2. LDL particle number (Apo. B) is a stronger indicator of CHD risk vs LDL-C in: • Prospective epidemiologic trials [3 -12] • In assessing residual risk on statin or fibrate therapy in intervention trials [1317]. 3. LDL particle number (Apo. B) is a stronger indicator of CHD risk vs non HDL-C in: • Prospective epidemiologic trials [8, 11, 18] • In assessing residual risk on statin or fibrate therapy in intervention trials [1315, ]. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. Atherosclerosis. 1991; 89: 109 -16. Clin Chem Acta. 1978; 82: 151 -60. Circulation. 1996; 94: 273 -8. Circulation. 1999; 99: 2517 -22. Lancet. 2001; 358: 2026 -33. Arterioscler Thromb Vasc Biol. 2002; 22: 1918 -23. AJC. 2005; 997 -1001. Diabetologica. 2006; 49: 937 -944. Arterioscler Thromb Vasc Biol. 2007; 27: 661 -670. JAMA. 2005; 294: 326 -33. J Lipid Res. 2007; 48: 2499 -2505. JAMA. 2007; 298: 776 -785. Circulation. 2000; 101: 477 -84. Circulation. 2002; 105: 1162 -9. Arterioscler Thromb Vasc Biol. 2000; 20: 2408 -2413. JACC. 1998; 32: 1648 -1656. Circulation. 2003; 107: 1733 -1737. Lancet. 2003; 361: 777 -780.
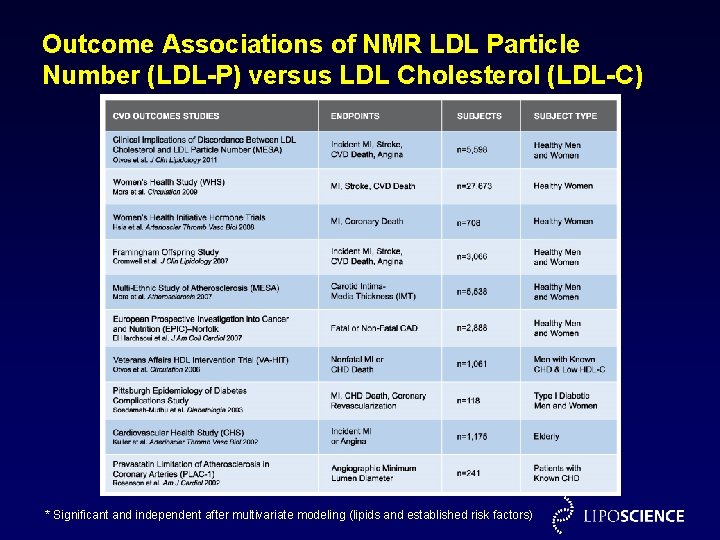
Outcome Associations of NMR LDL Particle Number (LDL-P) versus LDL Cholesterol (LDL-C) * Significant and independent after multivariate modeling (lipids and established risk factors)

Clinical Implications of Discordance Between Low-Density Lipoprotein Cholesterol and Particle Number James D. Otvos, Ph. D, Samia Mora, MD, MHS, Irina Shalaurova, MD, Philip Greenland, MD, Rachel H. Mackey, Ph. D, MPH, David C. Goff Jr. , MD, Ph. D Journal of Clinical Lipidology 2011; 5: 105 -113
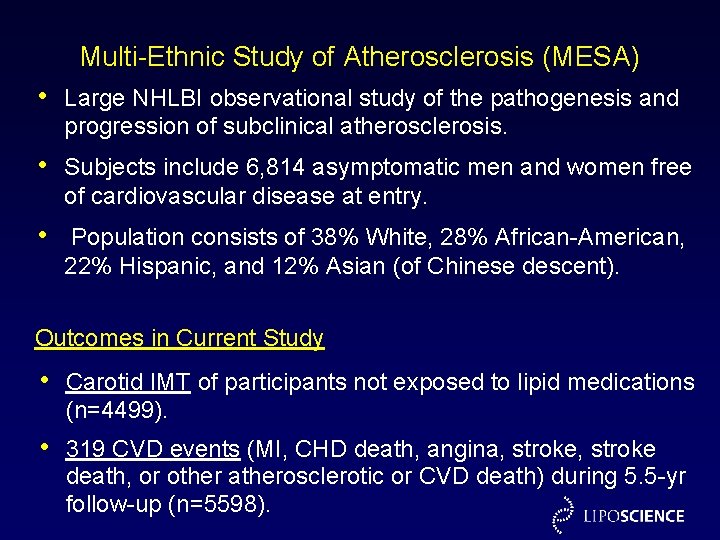
Multi-Ethnic Study of Atherosclerosis (MESA) • Large NHLBI observational study of the pathogenesis and progression of subclinical atherosclerosis. • Subjects include 6, 814 asymptomatic men and women free of cardiovascular disease at entry. • Population consists of 38% White, 28% African-American, 22% Hispanic, and 12% Asian (of Chinese descent). Outcomes in Current Study • Carotid IMT of participants not exposed to lipid medications (n=4499). • 319 CVD events (MI, CHD death, angina, stroke death, or other atherosclerotic or CVD death) during 5. 5 -yr follow-up (n=5598).

Study Design • LDL particle number (LDL-P) measured by NMR spectroscopy, calculated LDL cholesterol (LDL-C), and carotid intima-media thickness (IMT) were assessed at baseline. • Associations of LDL-C and LDL-P with CVD events (prospective) and carotid IMT (cross-sectional) were determined overall and in subgroups with concordant or discordant levels of these alternate LDL measures. • Discordance was defined as LDL-C and LDL-P levels differing by 12 percentile units, to give equal-sized concordant and discordant subgroups. Otvos et al. J Clin Lipidol 2011; 5: 105 -13
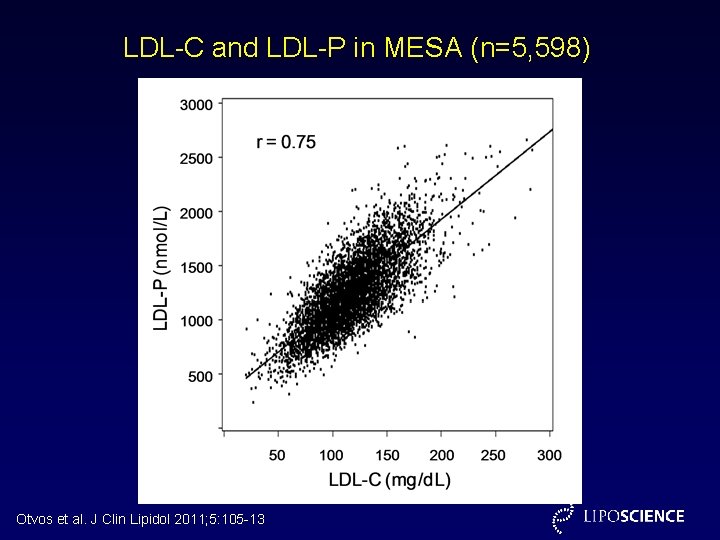
LDL-C and LDL-P in MESA (n=5, 598) Otvos et al. J Clin Lipidol 2011; 5: 105 -13
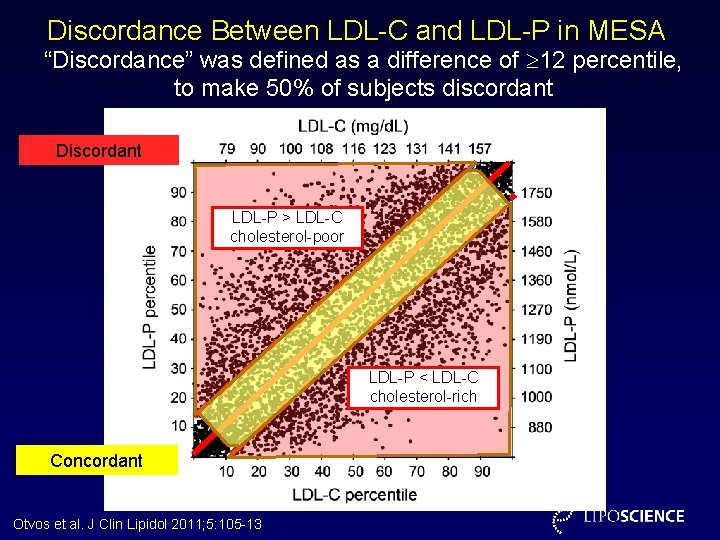
Discordance Between LDL-C and LDL-P in MESA “Discordance” was defined as a difference of 12 percentile, to make 50% of subjects discordant Discordant LDL-P > LDL-C cholesterol-poor LDL-P < LDL-C cholesterol-rich Concordant Otvos et al. J Clin Lipidol 2011; 5: 105 -13

LDL-P and LDL-C Discordance in MESA Relations with Incident CVD Events (n=319) LDL Size LDL-C Cumulative Incidence Met. Syn 0. 06 LDL-P > LDL-C Concordant LDL-P < LDL-C 0. 04 LDL-C underestimates LDL-attributable risk 54% 33% 16% 0. 02 20. 3 104 1372 20. 7 117 1249 21. 1 130 1117 nm mg/d. L nmol/L LDL-C overestimates LDL -attributable risk 0 1 2 3 4 Follow-up (years) Otvos et al. J Clin Lipidol 2011; 5: 105 -13 5 LDL-P
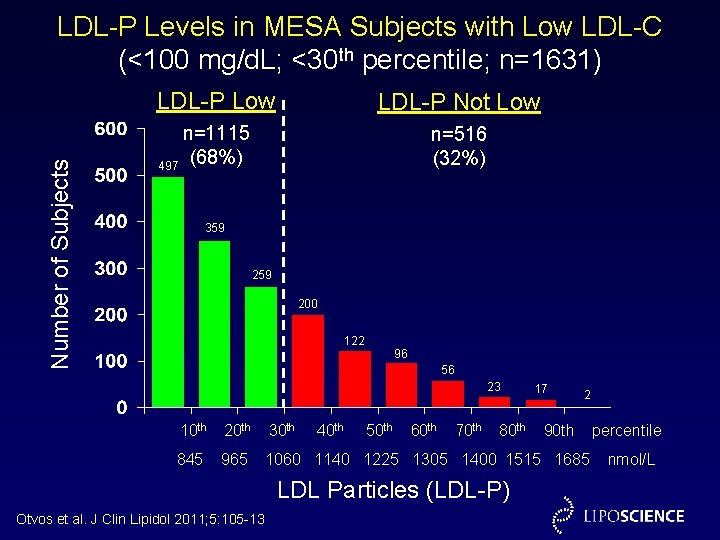
LDL-P Levels in MESA Subjects with Low LDL-C (<100 mg/d. L; <30 th percentile; n=1631) Number of Subjects LDL-P Low LDL-P Not Low n=1115 497 (68%) n=516 (32%) 359 200 122 96 56 23 40 th 50 th 60 th 70 th 80 th 17 2 10 th 20 th 30 th 845 965 1060 1140 1225 1305 1400 1515 1685 LDL Particles (LDL-P) Otvos et al. J Clin Lipidol 2011; 5: 105 -13 90 th percentile nmol/L

LDL-P and LDL-C Discordance in MESA CVD Event Rates in Subgroups with Low LDL Residual Risk Otvos et al. J Clin Lipidol 2011; 5: 105 -13
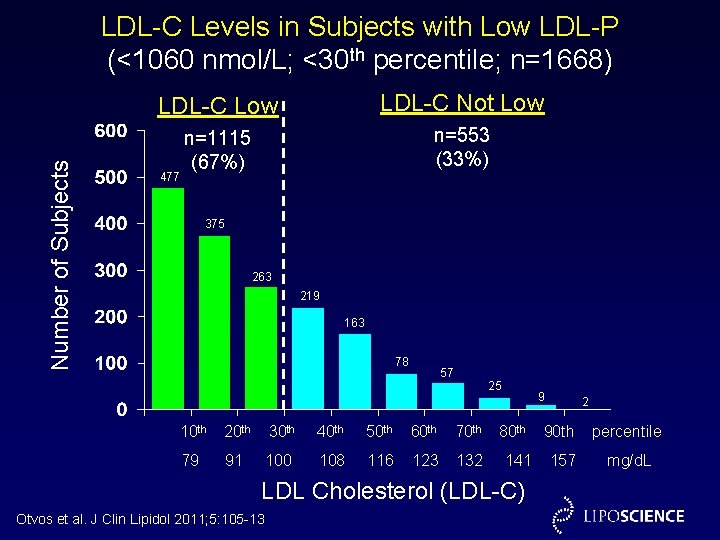
Number of Subjects LDL-C Levels in Subjects with Low LDL-P (<1060 nmol/L; <30 th percentile; n=1668) LDL-C Low LDL-C Not Low n=1115 (67%) n=553 (33%) 477 375 263 219 163 78 57 25 10 th 20 th 30 th 40 th 50 th 60 th 79 91 100 108 116 123 132 9 80 th 141 LDL Cholesterol (LDL-C) Otvos et al. J Clin Lipidol 2011; 5: 105 -13 2 90 th percentile 157 mg/d. L
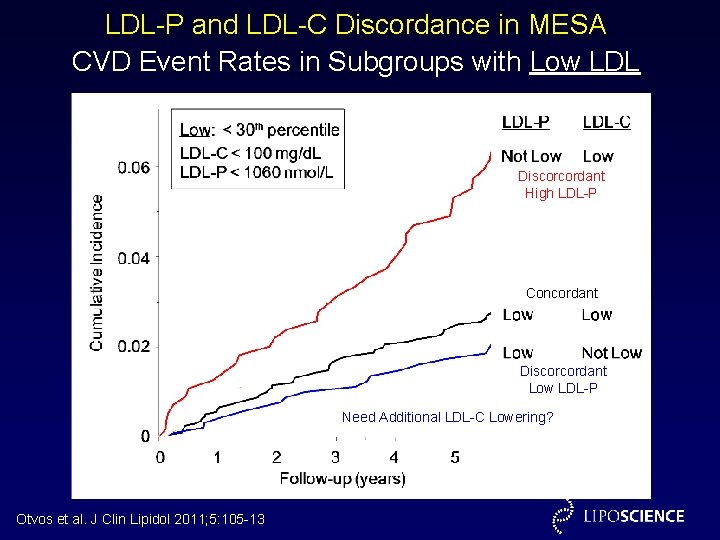
LDL-P and LDL-C Discordance in MESA CVD Event Rates in Subgroups with Low LDL Residual Risk Discorcordant High LDL-P Concordant Discorcordant Low LDL-P Need Additional LDL-C Lowering? Otvos et al. J Clin Lipidol 2011; 5: 105 -13
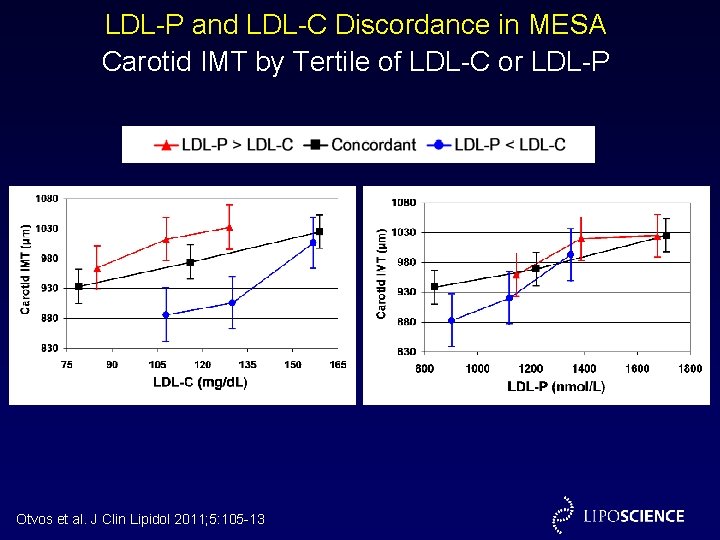
LDL-P and LDL-C Discordance in MESA Carotid IMT by Tertile of LDL-C or LDL-P Otvos et al. J Clin Lipidol 2011; 5: 105 -13
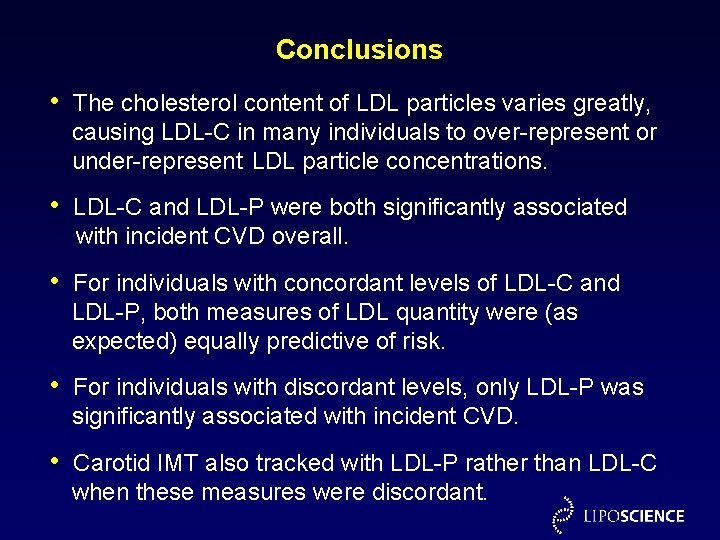
Conclusions • The cholesterol content of LDL particles varies greatly, causing LDL-C in many individuals to over-represent or under-represent LDL particle concentrations. • LDL-C and LDL-P were both significantly associated with incident CVD overall. • For individuals with concordant levels of LDL-C and LDL-P, both measures of LDL quantity were (as expected) equally predictive of risk. • For individuals with discordant levels, only LDL-P was significantly associated with incident CVD. • Carotid IMT also tracked with LDL-P rather than LDL-C when these measures were discordant.

CHD Event Associations of LDL-P versus LDL-C Framingham Offspring Study (n=3, 066) Cromwell WC et al. J Clin Lipidology 2007; 1(6): 583 -592.

Incident CHD Events at Low Levels of Alternative Measures of Atherogenic Lipoproteins Framingham Offspring Study* (n=3, 066) Quartile 1 * Adjusted for age and gender Cromwell WC et al. J Clin Lipidology. 2007; 1(6): 583 -592.
Recommendations from ADA/ACC Consensus Statement on Lipoprotein Management in Patients with Cardiometabolic Risk 1. “Measurement of LDL cholesterol (the cholesterol within LDL particles) has been the standard approach to approximate LDL levels. ” 2. “However, the cholesterol content of LDL particles varies from person to person and is influenced by metabolic abnormalities such as insulin resistance and hyperglycemia. ” 3. “Hence, measurement of LDL cholesterol may not accurately reflect the true burden of atherogenic LDL particles, especially in those with the typical lipoprotein abnormalities of cardio-metabolic risk. ” Brunzell et al. Diabetes Care. 2008. 31(4): 811 -822.
Recommendations from ADA/ACC Consensus Statement on Lipoprotein Management in Patients with Cardiometabolic Risk 4. “A more accurate way to capture the risk posed by LDL may be to measure the number of LDL particles directly using nuclear magnetic resonance (NMR). ” 5. “Measurements of apo. B or LDL particle number by NMR may more closely quantitate the atherogenic lipoprotein load. Some studies suggest that both are better indices of CVD risk than LDL cholesterol or non-HDL cholesterol and more reliable indexes of ontreatment residual CVD risk. ” 6. “Apo. B or LDL particle number also appear to be more discriminating measures of the adequacy of LDL lowering therapy than are LDL cholesterol or non-HDL cholesterol. ” Brunzell et al. Diabetes Care. 2008. 31(4): 811 -822.

Effect of LDL Lowering Therapies on LDL-C, Non-HDL-C, Apo B, and LDL-P Sniderman AD. J Clin Lipidology 2008; 2: 36 -42


2009 Position Statement from the AACC Lipoproteins and Vascular Diseases Division Working Group on Best Practices 1. “Any measure of LDL-C, including the b-quantification reference method, suffers from the fact that measurement of the cholesterol component of LDL does not consistently reflect the concentration of LDL particles in serum/plasma. ” 2. “Despite a high correlation, these markers are only modestly concordant, indicating that one cannot simply substitute for another in classifying patients into risk categories. ” Contois, et al. Clinical Chemistry 2009; 55: 407 -419.

2009 Position Statement from the AACC Lipoproteins and Vascular Diseases Division Working Group on Best Practices 3. “Importantly, on-treatment non HDL-C concentrations may not reflect residual risk associated with increased LDL particle number. ” 4. “We believe that the medical decision cutpoints should be set so that the apo. B and LDL-P cutpoints are equivalent to those for LDL-C in terms of population percentiles. ” Contois, et al. Clinical Chemistry 2009; 55: 407 -419.
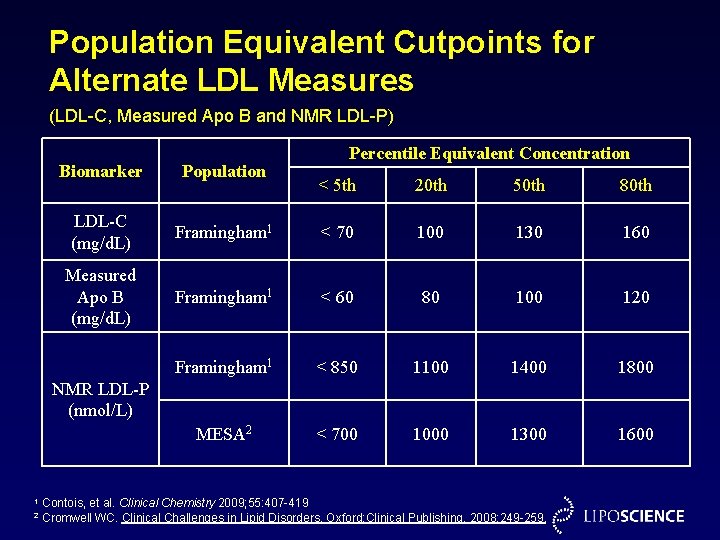
Population Equivalent Cutpoints for Alternate LDL Measures (LDL-C, Measured Apo B and NMR LDL-P) Biomarker Population LDL-C (mg/d. L) Measured Apo B (mg/d. L) Percentile Equivalent Concentration < 5 th 20 th 50 th 80 th Framingham 1 < 70 100 130 160 Framingham 1 < 60 80 100 120 Framingham 1 < 850 1100 1400 1800 MESA 2 < 700 1000 1300 1600 NMR LDL-P (nmol/L) 1 2 Contois, et al. Clinical Chemistry 2009; 55: 407 -419 Cromwell WC. Clinical Challenges in Lipid Disorders. Oxford: Clinical Publishing, 2008: 249 -259.
Relationship of LDL Particle Size with CHD Outcomes
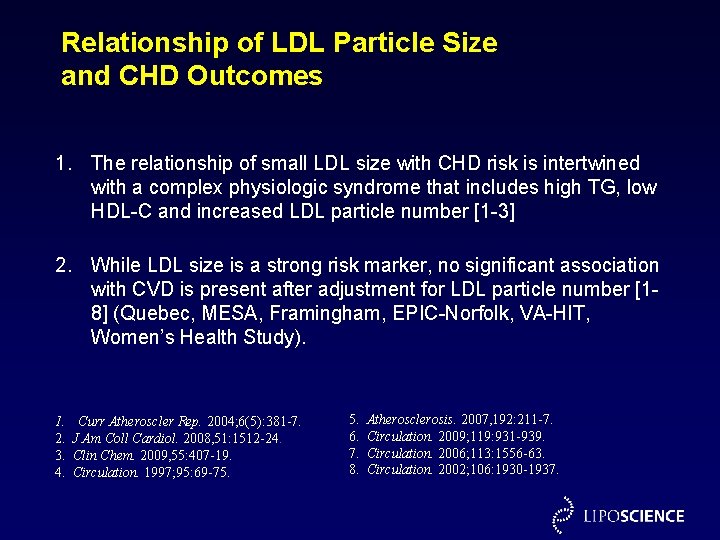
Relationship of LDL Particle Size and CHD Outcomes 1. The relationship of small LDL size with CHD risk is intertwined with a complex physiologic syndrome that includes high TG, low HDL-C and increased LDL particle number [1 -3] 2. While LDL size is a strong risk marker, no significant association with CVD is present after adjustment for LDL particle number [18] (Quebec, MESA, Framingham, EPIC-Norfolk, VA-HIT, Women’s Health Study). 1. 2. 3. 4. Curr Atheroscler Rep. 2004; 6(5): 381 -7. J Am Coll Cardiol. 2008, 51: 1512 -24. Clin Chem. 2009, 55: 407 -19. Circulation. 1997; 95: 69 -75. 5. 6. 7. 8. Atherosclerosis. 2007, 192: 211 -7. Circulation. 2009; 119: 931 -939. Circulation. 2006; 113: 1556 -63. Circulation. 2002; 106: 1930 -1937.
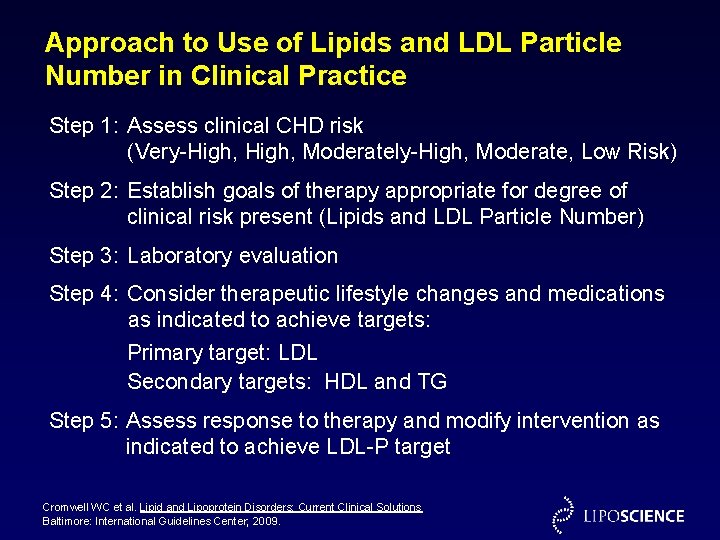
Approach to Use of Lipids and LDL Particle Number in Clinical Practice Step 1: Assess clinical CHD risk (Very-High, Moderately-High, Moderate, Low Risk) Step 2: Establish goals of therapy appropriate for degree of clinical risk present (Lipids and LDL Particle Number) Step 3: Laboratory evaluation Step 4: Consider therapeutic lifestyle changes and medications as indicated to achieve targets: Primary target: LDL Secondary targets: HDL and TG Step 5: Assess response to therapy and modify intervention as indicated to achieve LDL-P target Cromwell WC et al. Lipid and Lipoprotein Disorders: Current Clinical Solutions Baltimore: International Guidelines Center; 2009.

Assess Clinical Risk Cromwell WC et al. Lipid and Lipoprotein Disorders: Current Clinical Solutions Baltimore: International Guidelines Center; 2009.

Establish Goals of Therapy Risk Category LDL-C (mg/d. L) Non HDL-C (mg/d. L) Very High Risk < 100 (consider < 70) High Risk LDL Particle Number (Measured Apo B or NMR LDL-P) 1, 2, 3 HDL-C (mg/d. L) TG (mg/d. L) Measured Apo. B (mg/d. L) 1 NMR LDL-P (nmol/L) 2, 3 < 130 (consider < 100) < 80 * < 1000 * > 40 Male or > 50 Female < 150 < 100 (optional < 70) < 130 (optional < 100) < 80 < 1000 > 40 Male or > 50 Female < 150 Moderate High Risk < 130 (optional < 100) < 160 (optional < 130) < 100 (optional < 80) < 1300 ( optional < 1000) > 40 Male or > 50 Female < 150 Moderate Risk < 130 < 160 < 100 < 1300 > 40 Male or > 50 Female < 150 Low Risk < 160 < 190 < 120 < 1600 > 40 Male or > 50 Female < 150 1. Contois JH et al. Clin Chem. 2009; 55: 407 -419 2. Cromwell WC. In: Clinical Challenges in Lipid Disorders. Toth PP, Sica DA, editors. Oxford: Clinical Publishing; 2008. p. 249 -59. 3. Cromwell WC, Barringer TA. Curr Cardiol Reports 2009; 11(6): 468 -475 * More aggressive LDL lowering may be necessary based on clinical judgement.

Laboratory Evaluation 1. Fasting Lipid Profile, LDL Particle Number 2. Additional testing as indicated to evaluate secondary causes of dyslipoproteinemia • TSH • Fasting glucose • Hb. A 1 C • Bun • Creatinine • Urinalysis • Liver Function Tests 3. May consider additional laboratory studies to further assess risk or direct therapy • hs-CRP • Lp-PLA 2 • Lp(a) • Additional lipoprotein analysis (size, subclasses) Cromwell WC et al. Lipid and Lipoprotein Disorders: Current Clinical Solutions Baltimore: International Guidelines Center; 2009.
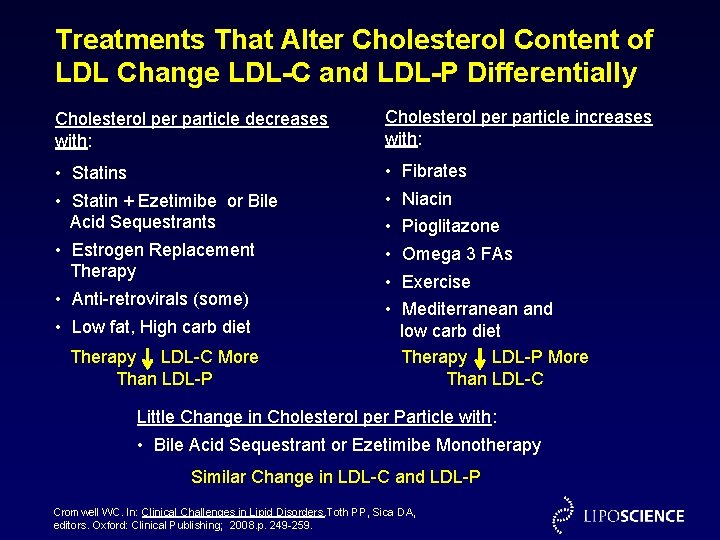
Treatments That Alter Cholesterol Content of LDL Change LDL-C and LDL-P Differentially Cholesterol per particle decreases with: Cholesterol per particle increases with: • Statins • Statin + Ezetimibe or Bile Acid Sequestrants • Estrogen Replacement Therapy • Anti-retrovirals (some) • Low fat, High carb diet • • • Therapy LDL-C More Than LDL-P Fibrates Niacin Pioglitazone Omega 3 FAs Exercise Mediterranean and low carb diet Therapy LDL-P More Than LDL-C Little Change in Cholesterol per Particle with: • Bile Acid Sequestrant or Ezetimibe Monotherapy Similar Change in LDL-C and LDL-P Cromwell WC. In: Clinical Challenges in Lipid Disorders. Toth PP, Sica DA, editors. Oxford: Clinical Publishing; 2008. p. 249 -259.

Pharmacologic Options for Reaching Lipid and LDL Particle Number Goals Cromwell WC, Barringer TA. Curr Cardiol Reports 2009; 11(6): 468 -475.
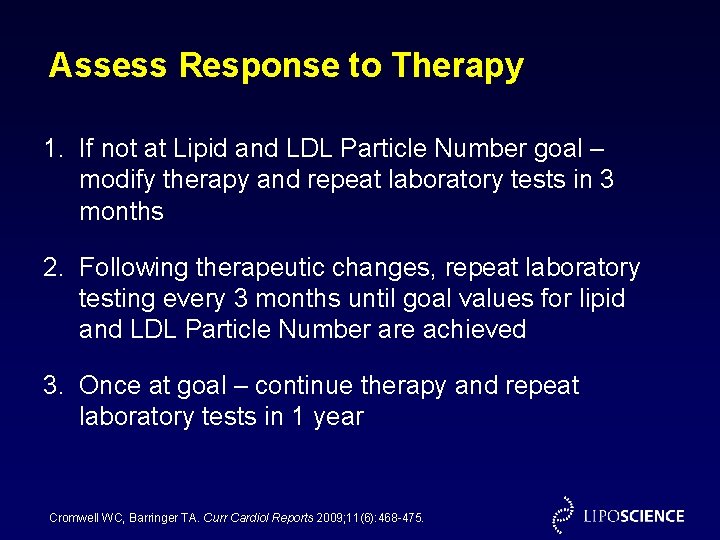
Assess Response to Therapy 1. If not at Lipid and LDL Particle Number goal – modify therapy and repeat laboratory tests in 3 months 2. Following therapeutic changes, repeat laboratory testing every 3 months until goal values for lipid and LDL Particle Number are achieved 3. Once at goal – continue therapy and repeat laboratory tests in 1 year Cromwell WC, Barringer TA. Curr Cardiol Reports 2009; 11(6): 468 -475.
Case ES Patient is a 55 year-old male who entered for evaluation of low HDL-C. Patient became aware of low HDL-C 10 years prior to office visit during routine laboratory screening showed HDL-C 30 mg/d. L. No specific therapy has been recommended for this condition to date. He has been intermittently physically active which he tolerates without symptoms. Patient follows no specific diet at presentation. He has no known history of CHD. No specific workup has been performed to date. Past Medical History: Non contributory Current Medications: None
Case ES Family History: Unremarkable Review of Systems: Unremarkable, Weight unchanged x 6 months PE: BP 115/72 Pulse 68 Wt 178 Ht 5’ 10” Waist 37” BMI 25. 5 Unremarkable
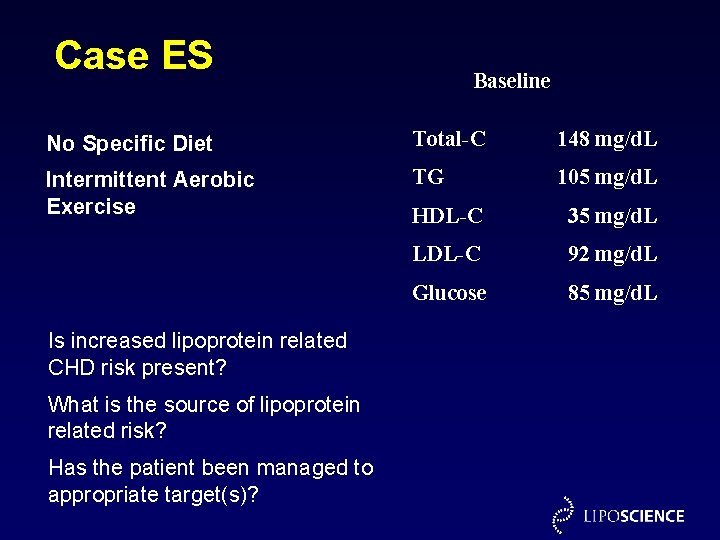
Case ES Baseline No Specific Diet Total-C 148 mg/d. L Intermittent Aerobic Exercise TG 105 mg/d. L Is increased lipoprotein related CHD risk present? What is the source of lipoprotein related risk? Has the patient been managed to appropriate target(s)? HDL-C 35 mg/d. L LDL-C 92 mg/d. L Glucose 85 mg/d. L
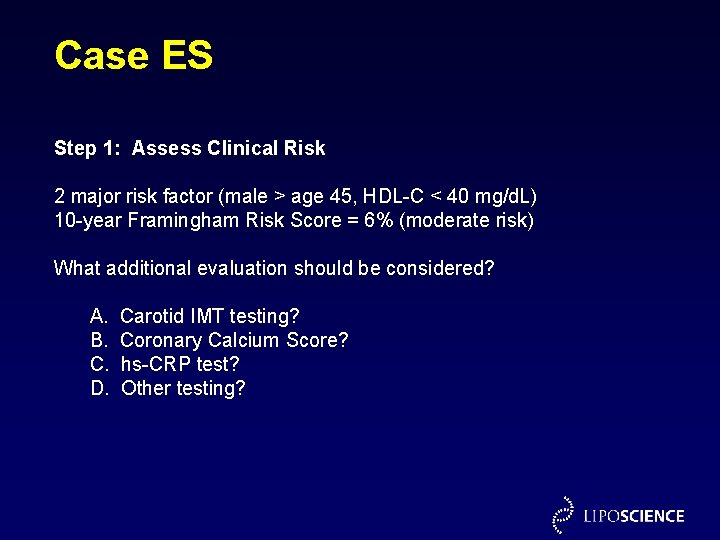
Case ES Step 1: Assess Clinical Risk 2 major risk factor (male > age 45, HDL-C < 40 mg/d. L) 10 -year Framingham Risk Score = 6% (moderate risk) What additional evaluation should be considered? A. B. C. D. Carotid IMT testing? Coronary Calcium Score? hs-CRP test? Other testing?
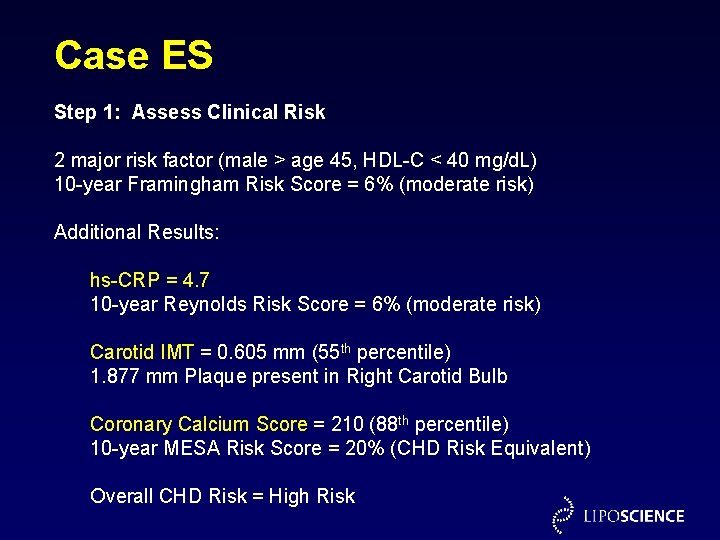
Case ES Step 1: Assess Clinical Risk 2 major risk factor (male > age 45, HDL-C < 40 mg/d. L) 10 -year Framingham Risk Score = 6% (moderate risk) Additional Results: hs-CRP = 4. 7 10 -year Reynolds Risk Score = 6% (moderate risk) Carotid IMT = 0. 605 mm (55 th percentile) 1. 877 mm Plaque present in Right Carotid Bulb Coronary Calcium Score = 210 (88 th percentile) 10 -year MESA Risk Score = 20% (CHD Risk Equivalent) Overall CHD Risk = High Risk
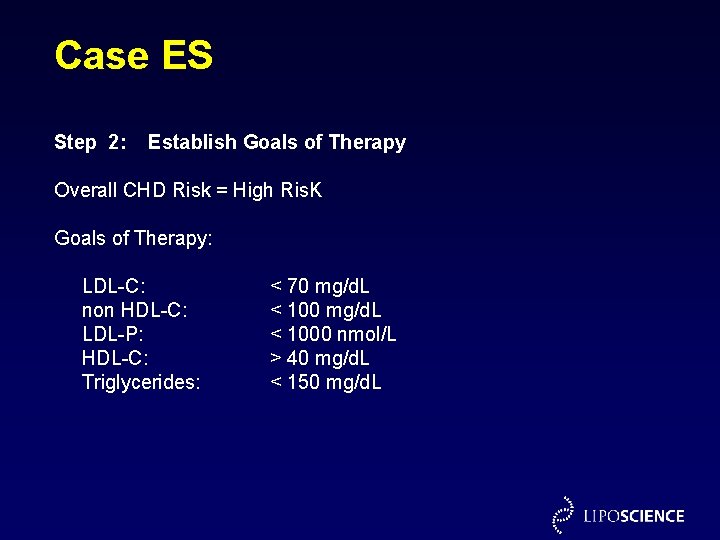
Case ES Step 2: Establish Goals of Therapy Overall CHD Risk = High Ris. K Goals of Therapy: LDL-C: non HDL-C: LDL-P: HDL-C: Triglycerides: < 70 mg/d. L < 1000 nmol/L > 40 mg/d. L < 150 mg/d. L
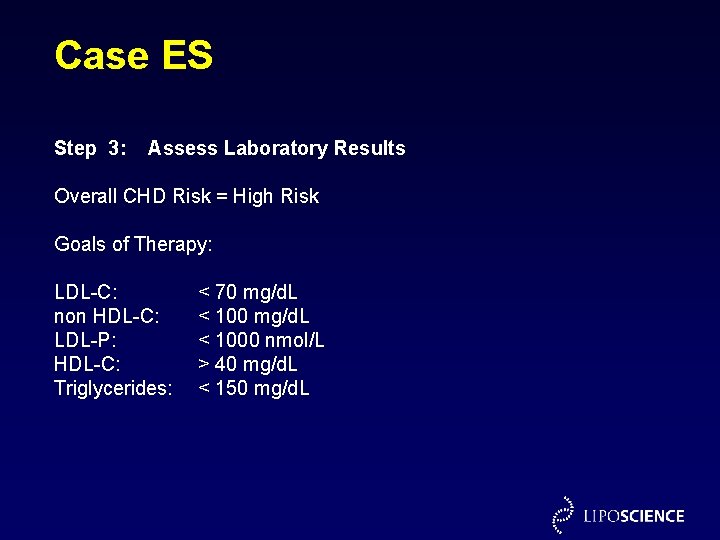
Case ES Step 3: Assess Laboratory Results Overall CHD Risk = High Risk Goals of Therapy: Results LDL-C: non HDL-C: LDL-P: HDL-C: Triglycerides: 92 mg/d. L 113 mg/d. L 1952 nmol/L (1675 small) 35 mg/d. L 105 mg/d. L < 70 mg/d. L < 1000 nmol/L > 40 mg/d. L < 150 mg/d. L
Case ES Step 4: Clinical Management Therapeutic Lifestyle Changes Mediterranean - American Diet Exercise 30 minutes, 5 days per week Pharmacologic Therapy Simvastatin 40 mg daily
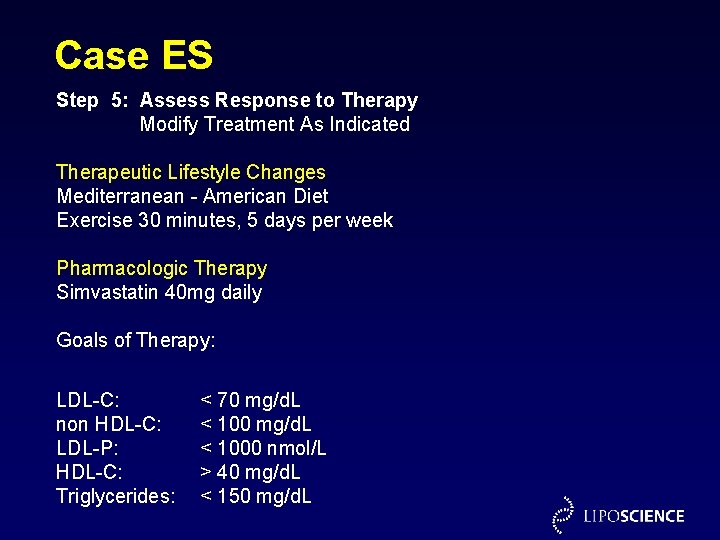
Case ES Step 5: Assess Response to Therapy Modify Treatment As Indicated Therapeutic Lifestyle Changes Mediterranean - American Diet Exercise 30 minutes, 5 days per week Pharmacologic Therapy Simvastatin 40 mg daily Goals of Therapy: 3 Months Later (wt. same) (Compliant with meds only) LDL-C: non HDL-C: LDL-P: HDL-C: Triglycerides: 79 mg/d. L 97 mg/d. L 1501 nmol/L (1175 small) 36 mg/d. L 90 mg/d. L < 70 mg/d. L < 1000 nmol/L > 40 mg/d. L < 150 mg/d. L
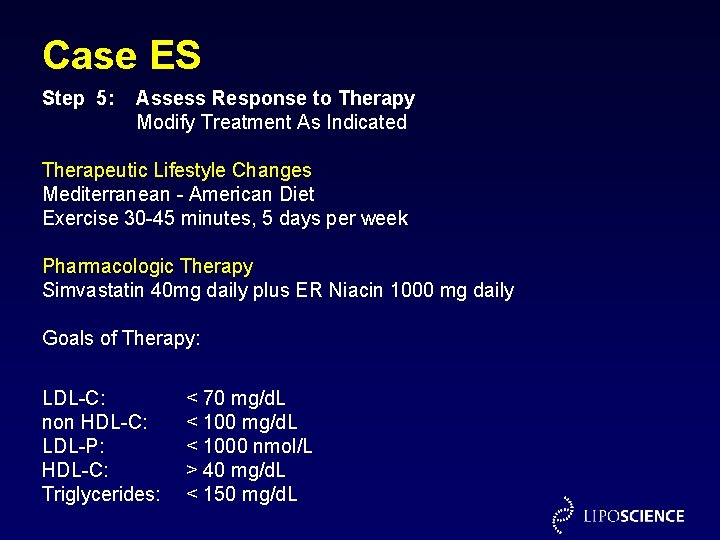
Case ES Step 5: Assess Response to Therapy Modify Treatment As Indicated Therapeutic Lifestyle Changes Mediterranean - American Diet Exercise 30 -45 minutes, 5 days per week Pharmacologic Therapy Simvastatin 40 mg daily plus ER Niacin 1000 mg daily Goals of Therapy: 3 Months Later (10# wt. loss) (Compliant with TLC & meds) LDL-C: non HDL-C: LDL-P: HDL-C: Triglycerides: 72 mg/d. L 86 mg/d. L 948 nmol/L (675 small) 42 mg/d. L 70 mg/d. L < 1000 nmol/L > 40 mg/d. L < 150 mg/d. L

Conclusions 1. Unrecognized (and under-treated) LDL particle elevations are common and a significant contributor to the residual risk of many patients with “acceptable” levels of LDL-C. 2. When LDL-C and LDL-P levels are discordant (esp. diabetes, metabolic syndrome), risk tracks with LDL-P, not LDL-C. 3. LDL-P values should be used to indicate a patient has achieved adequate LDL reduction, because LDL-P is a significant independent predictor of CHD end points. 4. LDL size (“quality”) does not contribute independently to risk once LDL particle number is taken into account. 5. LDL-P is a more sensitive indicator of low risk than LDL-C or non. HDL-C, and therefore a more discriminating LDL treatment target. 6. LDL-P may be lowered not only by statins, but by lifestyle change and combination drug therapy.
- Slides: 60