Patient Guide to Colon Cancer Surgery and Treatment

- Slides: 32
Patient Guide to Colon Cancer Surgery and Treatment
Table of Contents • • 2 Colon anatomy About colon cancer Characterizing your cancer Your treatment decision Oncotype DX® Your treatment profile My Colon Cancer Coach Resources
Where to Begin • Learn all you can about colon cancer • Find the best care that gives you confidence • Feel comfortable talking with your healthcare team • Understand your diagnosis and treatment plan • Keep track of how you are feeling • Stay involved in all treatment decisions 3
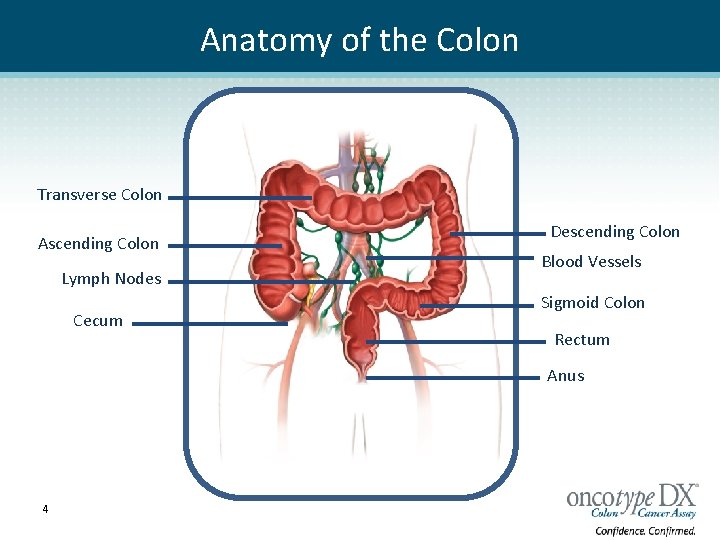
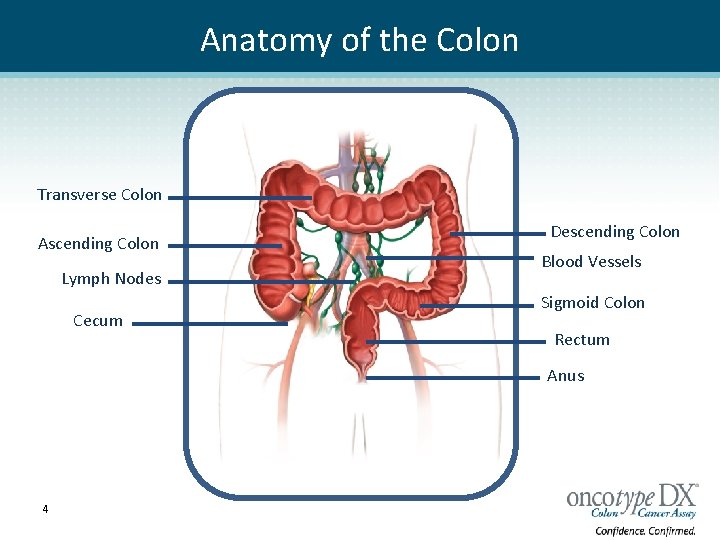
Anatomy of the Colon Transverse Colon Ascending Colon Lymph Nodes Cecum Descending Colon Blood Vessels Sigmoid Colon Rectum Anus 4
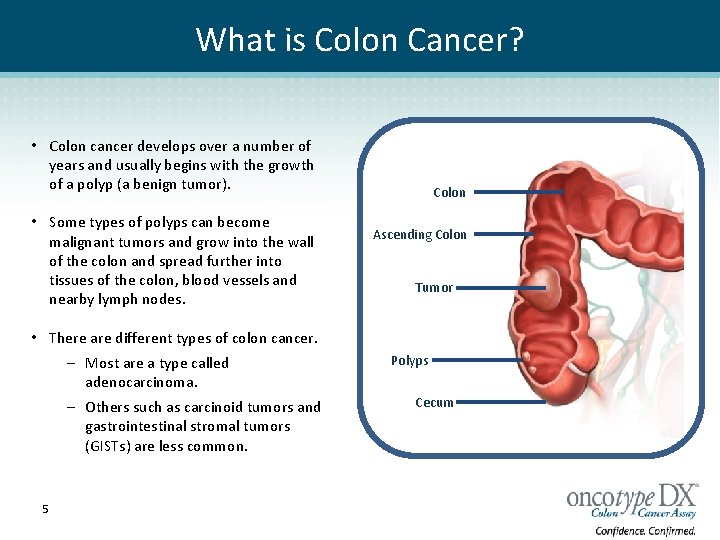
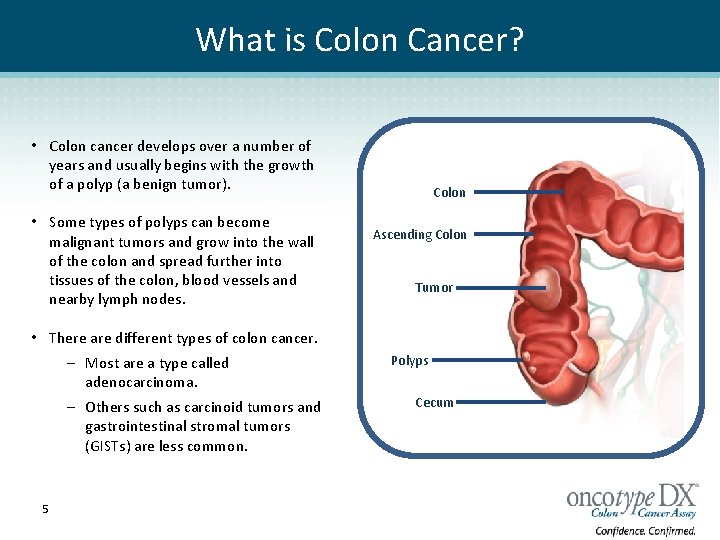
What is Colon Cancer? • Colon cancer develops over a number of years and usually begins with the growth of a polyp (a benign tumor). • Some types of polyps can become malignant tumors and grow into the wall of the colon and spread further into tissues of the colon, blood vessels and nearby lymph nodes. Colon Ascending Colon Tumor • There are different types of colon cancer. – Most are a type called adenocarcinoma. – Others such as carcinoid tumors and gastrointestinal stromal tumors (GISTs) are less common. 5 Polyps Cecum
What Causes Colon Cancer • Several known risk factors are associated with colon cancer. • Colon cancers results from changes in DNA (deoxyribonucleic acid) within the cells. • Changes (mutations) can be inherited or acquired during a person’s lifetime. • The majority of patients acquire mutations in their colon cells that results in malignant tumors over time. • A small percentage of colon cancer patients have inherited a susceptibility to colon cancer. 6
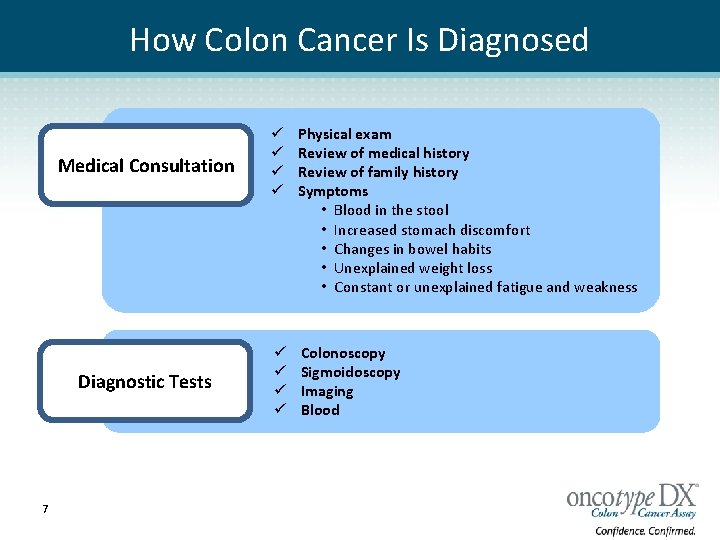
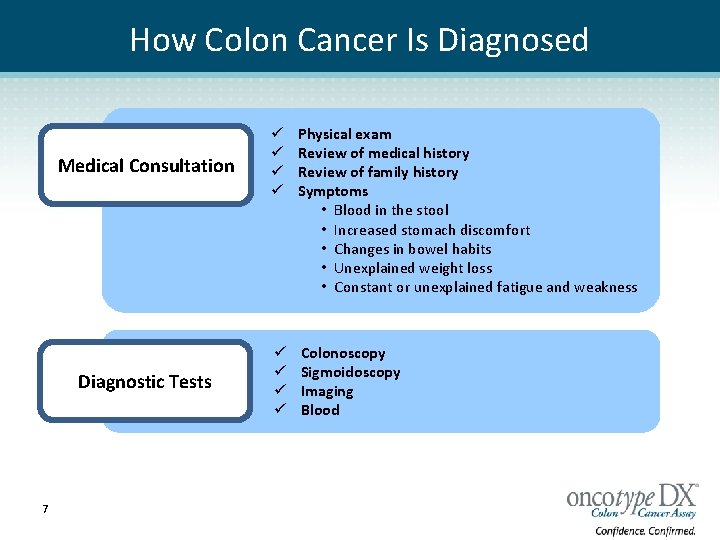
How Colon Cancer Is Diagnosed 7 Medical Consultation ü ü Physical exam Review of medical history Review of family history Symptoms • Blood in the stool • Increased stomach discomfort • Changes in bowel habits • Unexplained weight loss • Constant or unexplained fatigue and weakness Diagnostic Tests ü ü Colonoscopy Sigmoidoscopy Imaging Blood
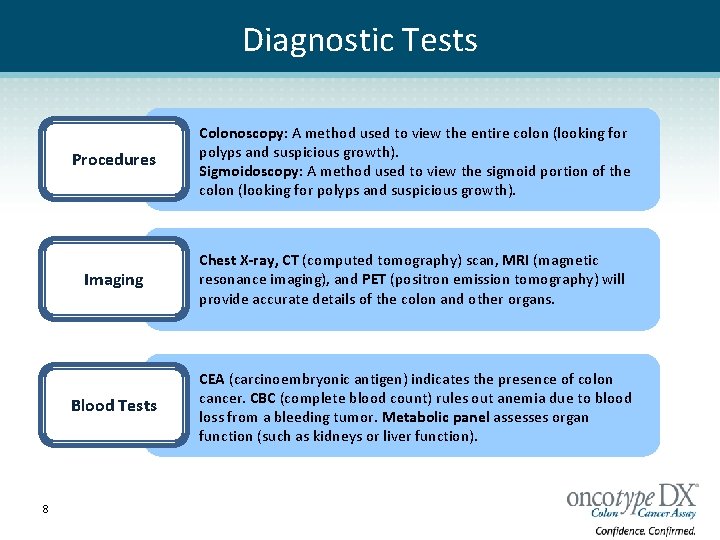
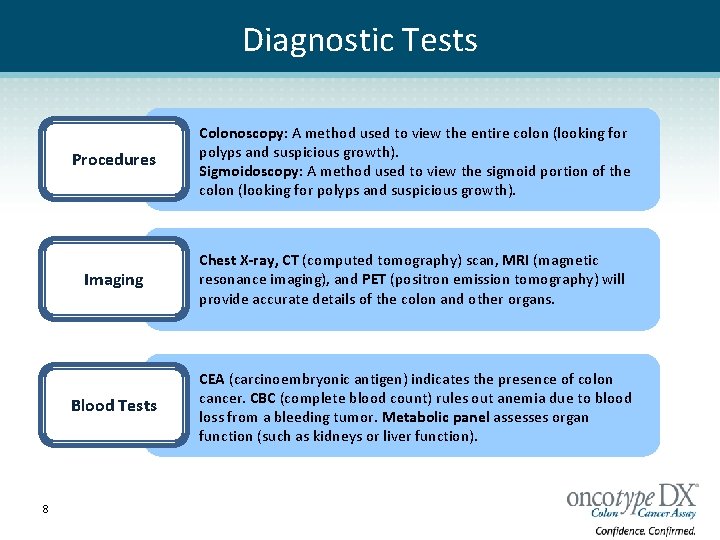
Diagnostic Tests 8 Procedures Colonoscopy: A method used to view the entire colon (looking for polyps and suspicious growth). Sigmoidoscopy: A method used to view the sigmoid portion of the colon (looking for polyps and suspicious growth). Imaging Chest X-ray, CT (computed tomography) scan, MRI (magnetic resonance imaging), and PET (positron emission tomography) will provide accurate details of the colon and other organs. Blood Tests CEA (carcinoembryonic antigen) indicates the presence of colon cancer. CBC (complete blood count) rules out anemia due to blood loss from a bleeding tumor. Metabolic panel assesses organ function (such as kidneys or liver function).
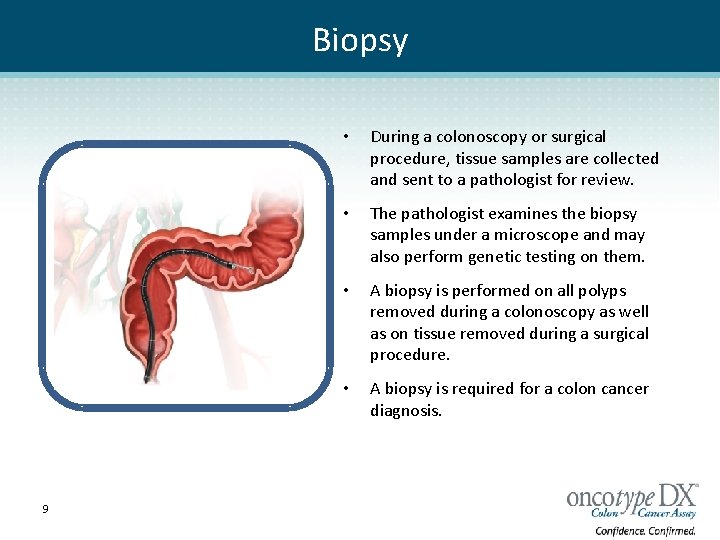
Biopsy 9 • During a colonoscopy or surgical procedure, tissue samples are collected and sent to a pathologist for review. • The pathologist examines the biopsy samples under a microscope and may also perform genetic testing on them. • A biopsy is performed on all polyps removed during a colonoscopy as well as on tissue removed during a surgical procedure. • A biopsy is required for a colon cancer diagnosis.
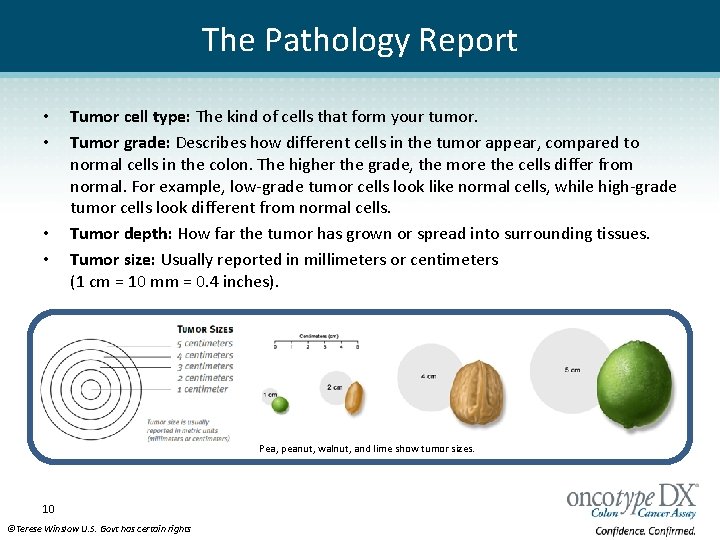
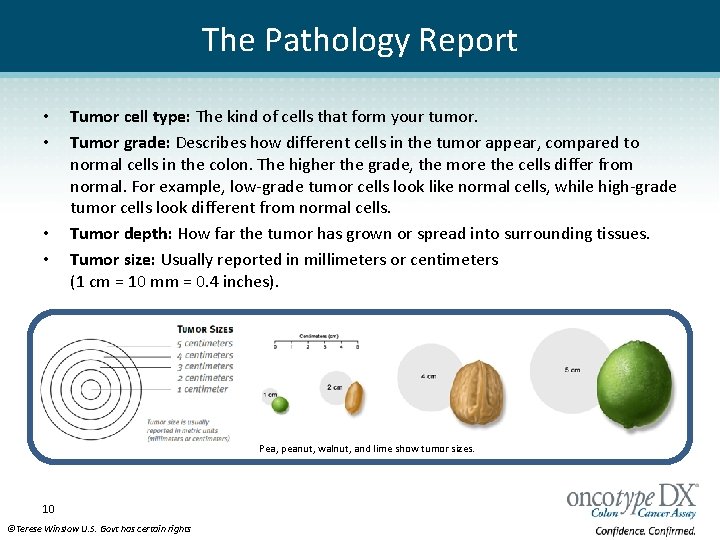
The Pathology Report • • Tumor cell type: The kind of cells that form your tumor. Tumor grade: Describes how different cells in the tumor appear, compared to normal cells in the colon. The higher the grade, the more the cells differ from normal. For example, low-grade tumor cells look like normal cells, while high-grade tumor cells look different from normal cells. Tumor depth: How far the tumor has grown or spread into surrounding tissues. Tumor size: Usually reported in millimeters or centimeters (1 cm = 10 mm = 0. 4 inches). Pea, peanut, walnut, and lime show tumor sizes. 10 ©Terese Winslow U. S. Govt has certain rights
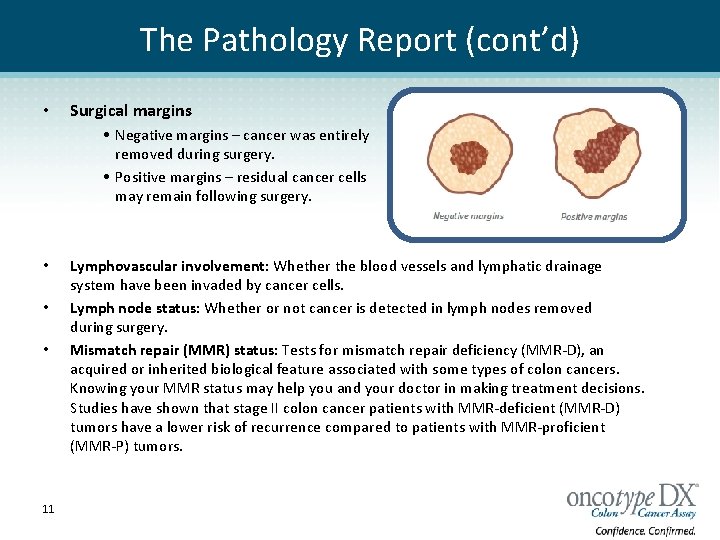
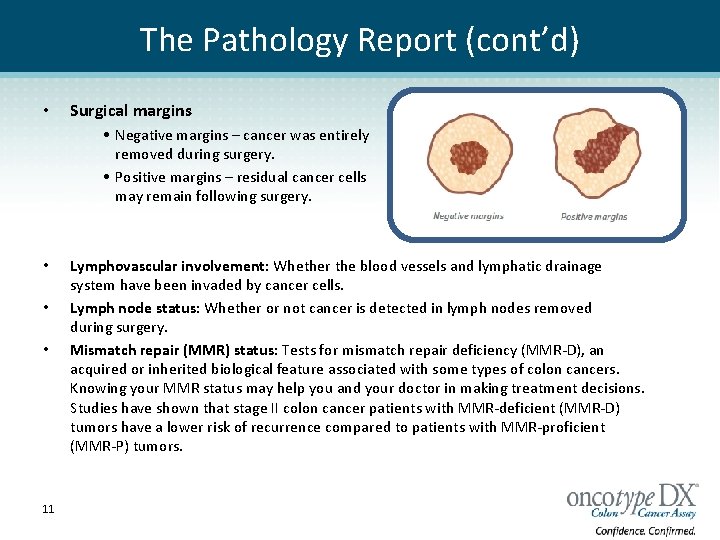
The Pathology Report (cont’d) • Surgical margins • Negative margins – cancer was entirely removed during surgery. • Positive margins – residual cancer cells may remain following surgery. • • • 11 Lymphovascular involvement: Whether the blood vessels and lymphatic drainage system have been invaded by cancer cells. Lymph node status: Whether or not cancer is detected in lymph nodes removed during surgery. Mismatch repair (MMR) status: Tests for mismatch repair deficiency (MMR-D), an acquired or inherited biological feature associated with some types of colon cancers. Knowing your MMR status may help you and your doctor in making treatment decisions. Studies have shown that stage II colon cancer patients with MMR-deficient (MMR-D) tumors have a lower risk of recurrence compared to patients with MMR-proficient (MMR-P) tumors.
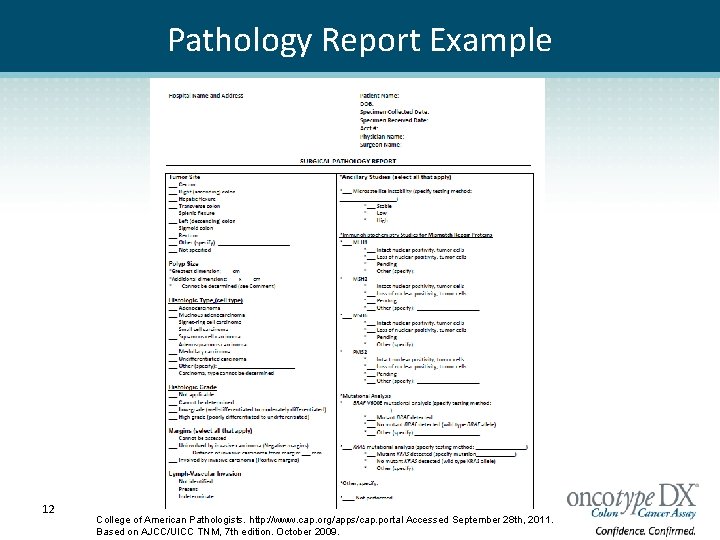
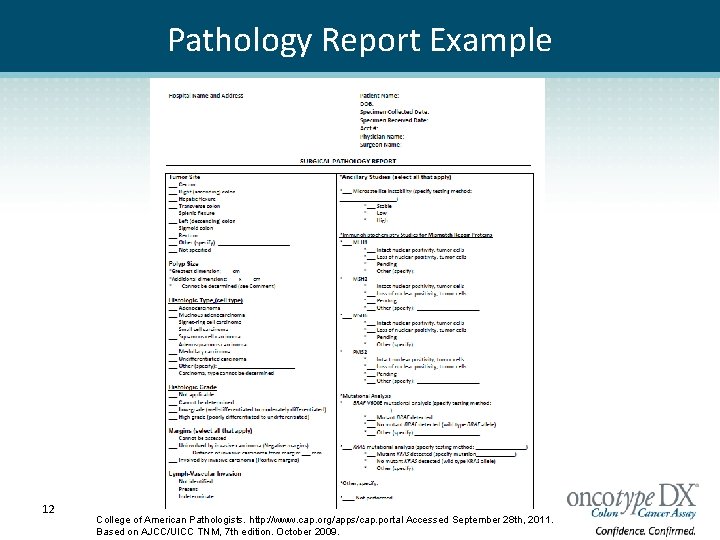
Pathology Report Example 12 College of American Pathologists. http: //www. cap. org/apps/cap. portal Accessed September 28 th, 2011. Based on AJCC/UICC TNM, 7 th edition. October 2009.
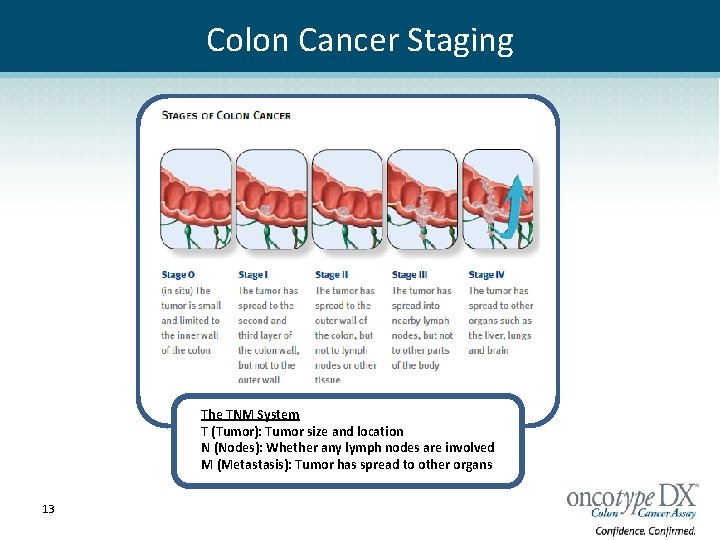
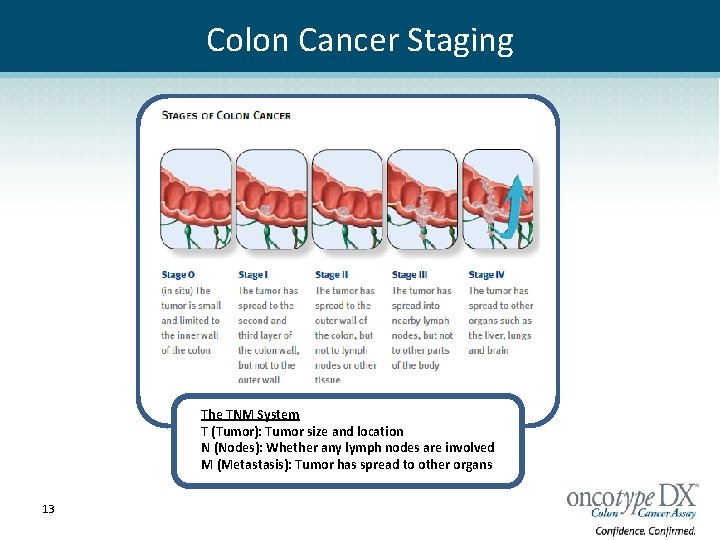
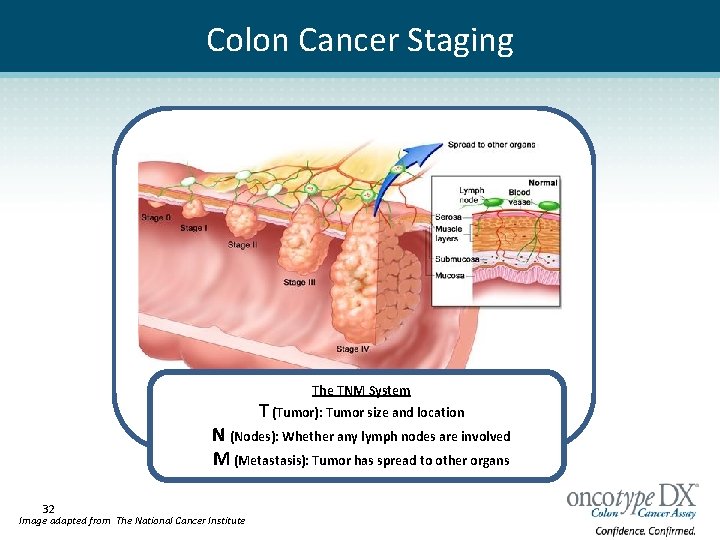
Colon Cancer Staging The TNM System T (Tumor): Tumor size and location N (Nodes): Whether any lymph nodes are involved M (Metastasis): Tumor has spread to other organs 13
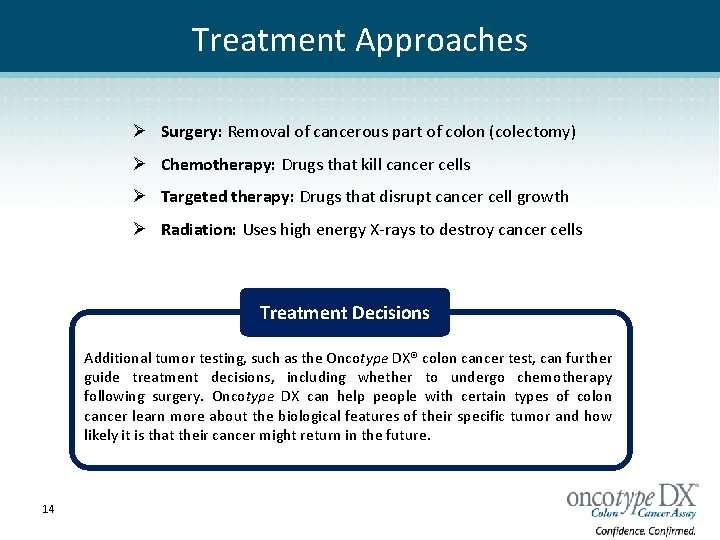
Treatment Approaches Ø Surgery: Removal of cancerous part of colon (colectomy) Ø Chemotherapy: Drugs that kill cancer cells Ø Targeted therapy: Drugs that disrupt cancer cell growth Ø Radiation: Uses high energy X-rays to destroy cancer cells Treatment Decisions Additional tumor testing, such as the Oncotype DX® colon cancer test, can further guide treatment decisions, including whether to undergo chemotherapy following surgery. Oncotype DX can help people with certain types of colon cancer learn more about the biological features of their specific tumor and how likely it is that their cancer might return in the future. 14
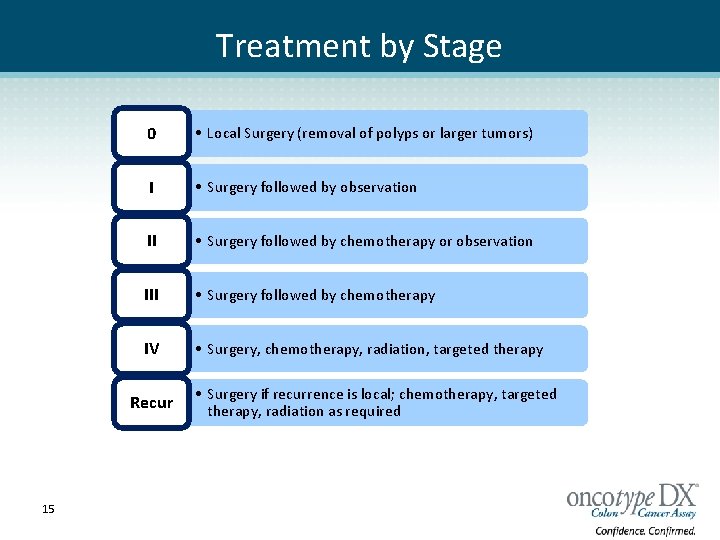
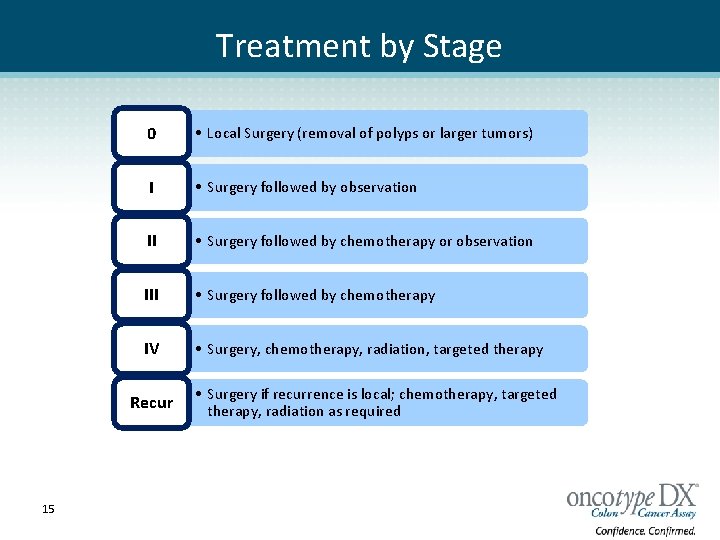
Treatment by Stage 0 • Local Surgery (removal of polyps or larger tumors) I • Surgery followed by observation II • Surgery followed by chemotherapy or observation III • Surgery followed by chemotherapy IV • Surgery, chemotherapy, radiation, targeted therapy Recur 15 • Surgery if recurrence is local; chemotherapy, targeted therapy, radiation as required
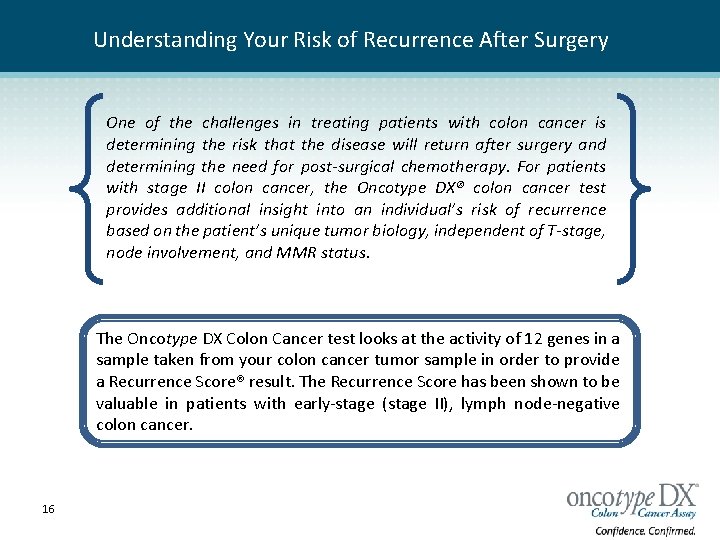
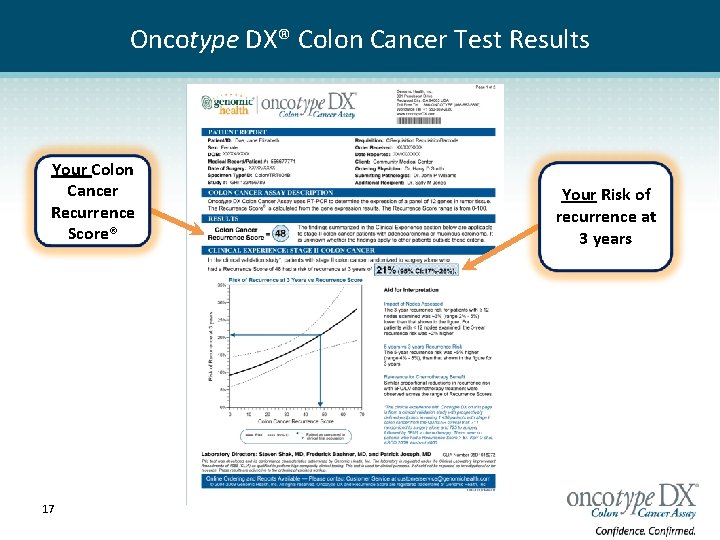
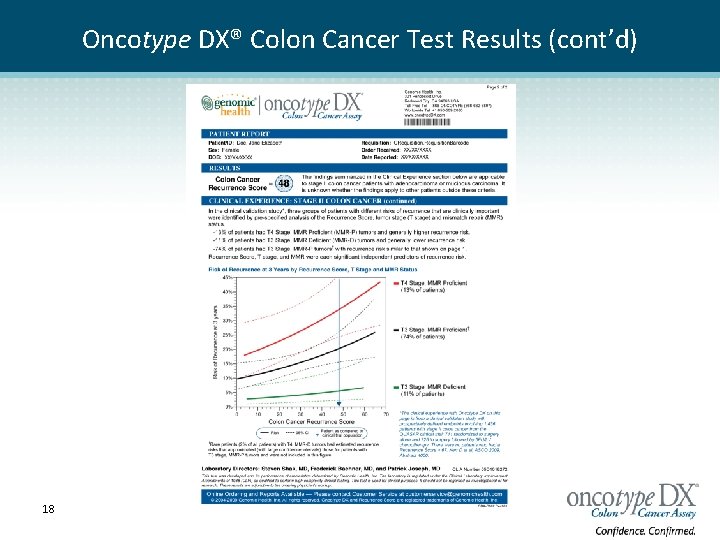
Understanding Your Risk of Recurrence After Surgery One of the challenges in treating patients with colon cancer is determining the risk that the disease will return after surgery and determining the need for post-surgical chemotherapy. For patients with stage II colon cancer, the Oncotype DX® colon cancer test provides additional insight into an individual’s risk of recurrence based on the patient’s unique tumor biology, independent of T-stage, node involvement, and MMR status. The Oncotype DX Colon Cancer test looks at the activity of 12 genes in a sample taken from your colon cancer tumor sample in order to provide a Recurrence Score® result. The Recurrence Score has been shown to be valuable in patients with early-stage (stage II), lymph node-negative colon cancer. 16
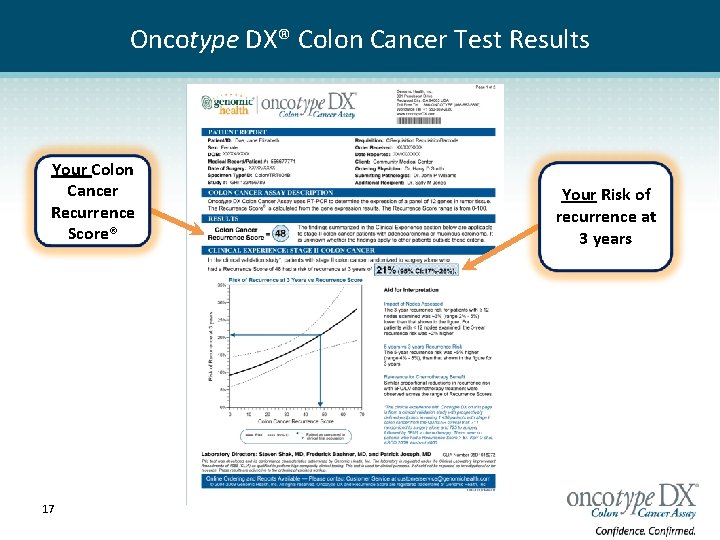
Oncotype DX® Colon Cancer Test Results Your Colon Cancer Recurrence Score® 17 Your Risk of recurrence at 3 years
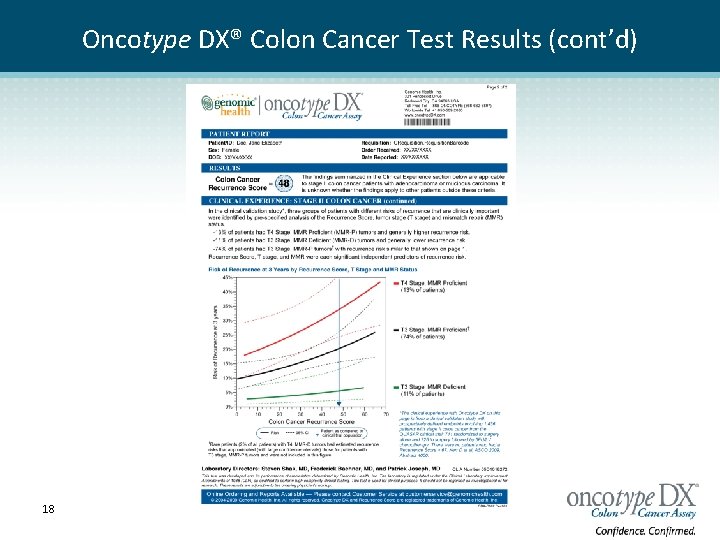
Oncotype DX® Colon Cancer Test Results (cont’d) 18
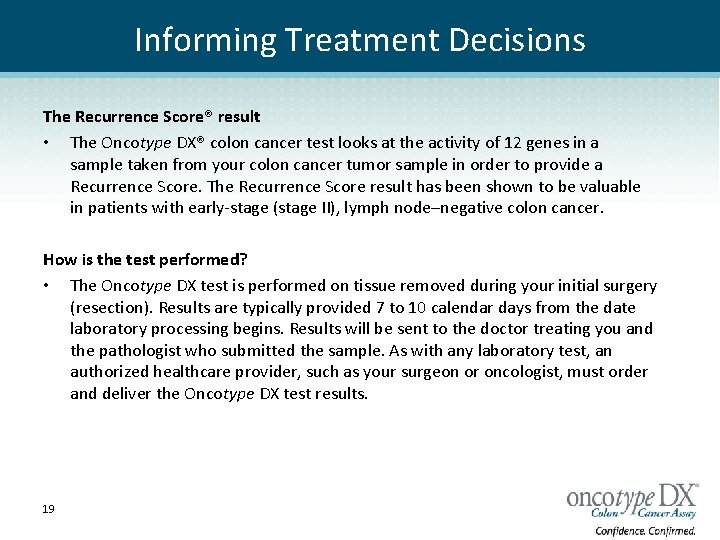
Informing Treatment Decisions The Recurrence Score® result • The Oncotype DX® colon cancer test looks at the activity of 12 genes in a sample taken from your colon cancer tumor sample in order to provide a Recurrence Score. The Recurrence Score result has been shown to be valuable in patients with early-stage (stage II), lymph node–negative colon cancer. How is the test performed? • The Oncotype DX test is performed on tissue removed during your initial surgery (resection). Results are typically provided 7 to 10 calendar days from the date laboratory processing begins. Results will be sent to the doctor treating you and the pathologist who submitted the sample. As with any laboratory test, an authorized healthcare provider, such as your surgeon or oncologist, must order and deliver the Oncotype DX test results. 19
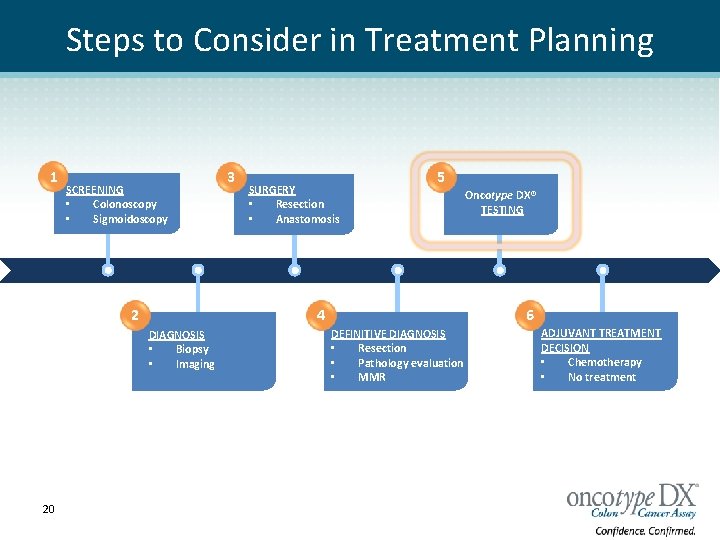
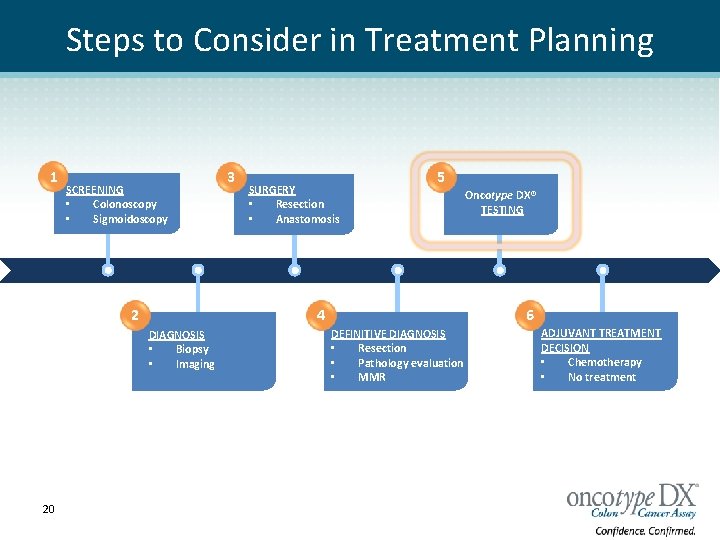
Steps to Consider in Treatment Planning 1 SCREENING • Colonoscopy • Sigmoidoscopy 2 SURGERY • Resection • Anastomosis 5 4 DIAGNOSIS • Biopsy • Imaging 20 3 Oncotype DX® TESTING 6 DEFINITIVE DIAGNOSIS • Resection • Pathology evaluation • MMR ADJUVANT TREATMENT DECISION • Chemotherapy • No treatment
Am I eligible for the test? • You may be a candidate for the Oncotype DX test if: q You have recently been diagnosed with stage II colon cancer, and your doctor are making treatment decisions regarding chemotherapy. • The decision whether or not to order the Oncotype DX test is one that you and your doctor should make together. 21
Does my insurance cover the Oncotype DX® test? • Genomic Health offers the Genomic Access Program (GAP), a comprehensive program designed to help you with the coverage process and provide financial assistance when necessary, based on eligibility. • Expanding payor coverage by both public and private payors. Please call 866 -ONCOTYPE (866 -662 -6897) for more information on insurance and financial aid questions. 22
What will I learn from the Oncotype DX® colon cancer test? • Your doctor will receive a report with the results of your Oncotype DX colon cancer test. The report contains your Recurrence Score® result, which is a number between 0 and 100. It provides a specific estimate of your risk of colon cancer recurrence within 3 years of surgery. • Individuals with a lower Recurrence Score have a lower risk of their colon cancer recurring. Individuals with a higher Recurrence Score have a higher risk of their colon cancer recurring. A Recurrence Score result, along with other information, can help you and your physician make a more informed, individualized treatment decision. • It is important to understand that having a lower Recurrence Score result does not mean that there is no chance that your colon cancer will return. Likewise, having a higher Recurrence Score does not mean that your colon cancer will definitely return. 23
Patient Ambassador: Dan Clementi, Oncotype DX® Colon Cancer Patient Click here to watch Dan’s story. http: //www. oncotypedx. com/en-US/Colon/Patient. Caregiver/Patient. Stories. aspx 24
My Colon Cancer Coach www. mycoloncancercoach. org Colon Cancer 101 Personalized Treatment Options Questions to Ask Your Doctor
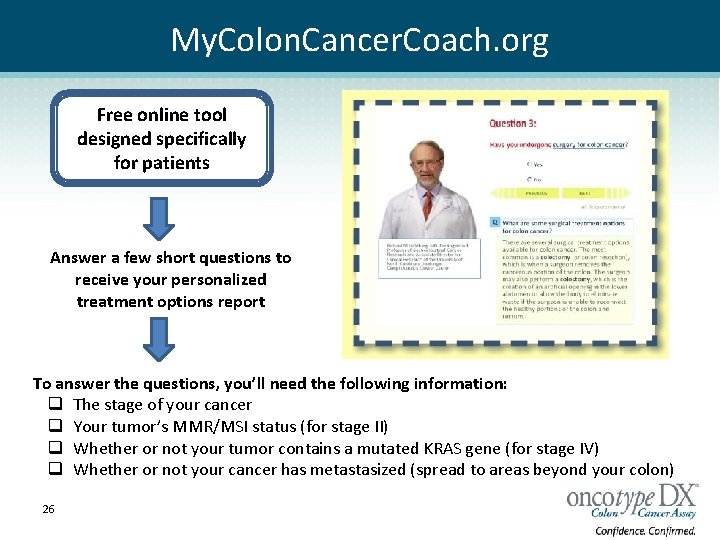
My. Colon. Cancer. Coach. org Free online tool designed specifically for patients Answer a few short questions to receive your personalized treatment options report To answer the questions, you’ll need the following information: q The stage of your cancer q Your tumor’s MMR/MSI status (for stage II) q Whether or not your tumor contains a mutated KRAS gene (for stage IV) q Whether or not your cancer has metastasized (spread to areas beyond your colon)) 26
A Report to Make Sense of Your Diagnosis E-mail Summary Printed Report 27
What to Ask Your Doctor q q q 28 How do I obtain a copy of my pathology report and testing information? How large and at what stage is my tumor? Is there a way to tell how quickly my cancer is growing or if it is invasive? How likely is my cancer to spread? Am I a candidate for the Oncotype DX® 1, 2 test, or other tumor specific tests? Am I going to need radiation or chemotherapy and if so, what can I expect during that period of time? Has my cancer metastasized? How quickly can I expect to recover? What is my risk of having the cancer come back (recurrence)? What can I do to help prevent the return of my cancer? How often do you recommend I be screened for recurrent cancer? Do you have any recommendations for support groups?

Resources www. cancercare. org www. cancer. org www. fightcolorectalcancer. org http: //cancersupportcommunity. org/ Patient www. cancer. gov www. mycoloncancercoach. org 29 www. ccalliance. org
Oncotype DX® Colon Cancer Assay Oncotype DX Colon Cancer Assay Make it part of the conversation, and make the informed, more individualized treatment decision. 30
BACK UP SLIDES 31
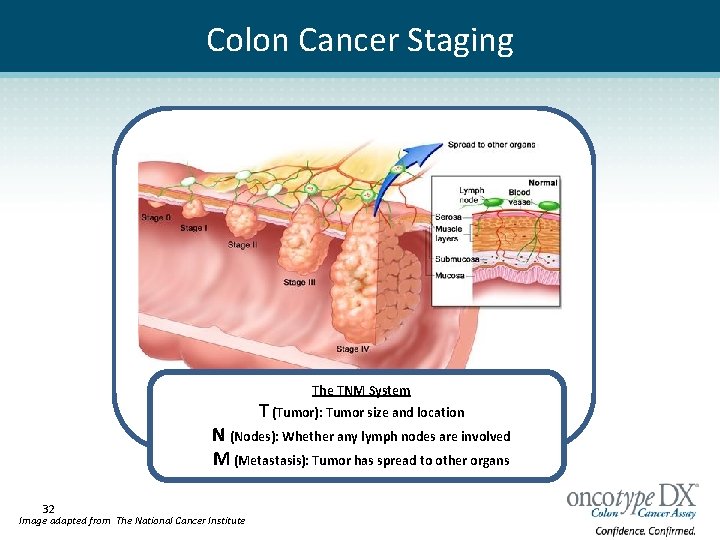
Colon Cancer Staging The TNM System T (Tumor): Tumor size and location N (Nodes): Whether any lymph nodes are involved M (Metastasis): Tumor has spread to other organs 32 Image adapted from The National Cancer Institute