Patient Care Services SelfLearning Packet Advanced Directive and









- Slides: 42

Patient Care Services Self-Learning Packet
Advanced Directive and POLST Patient Care Services Orientation
Advanced Directive & POLST • • An Advanced Directive is a Legal Document where the POLST is an order. Advanced Directive o o A document allowing a patient to direct who will make their health care decisions and state wishes for treatment if he/she is unable to decide for oneself in the future. Patients have a right to formulate an Advanced Directive and to have hospital staff and practitioners who provide care in the hospital to comply with the directives. • Advanced Directives are followed in hospitals where the POLST can be followed by all aspects of care including: Home Care, EMS & Nursing Homes • Practitioner Orders in Life Sustaining Treatment o For patients who have an advanced chronic progressive illnesses or life expectancy less than five years o Complements a patient’s advanced directive by converting the person’s wishes regarding lifesustaining treatment into a medical order which can accompany the patient in any health care setting, including pre and post-hospital care 2

Infection Prevention Patient Care Services Orientation
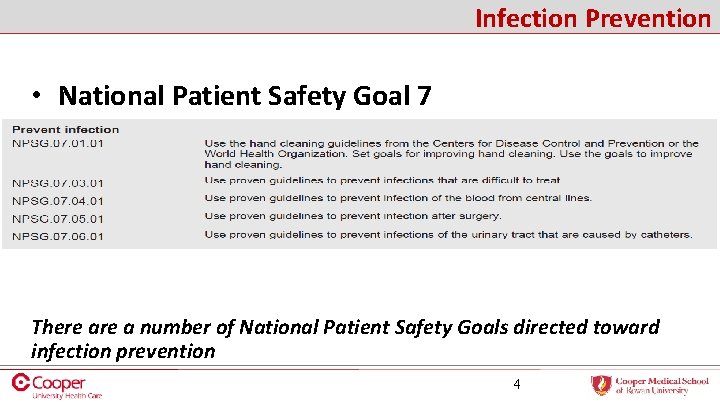
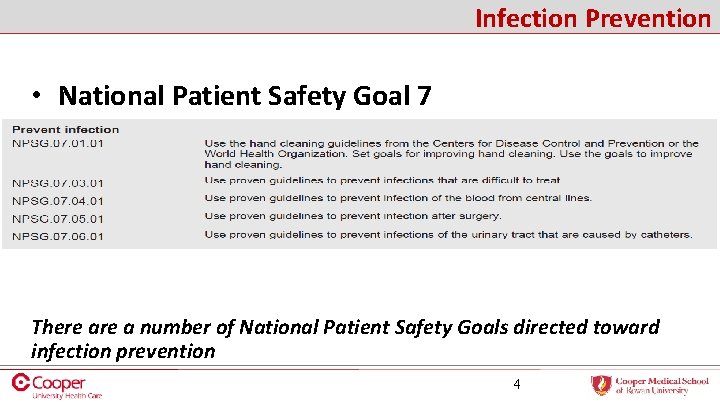
Infection Prevention • National Patient Safety Goal 7 There a number of National Patient Safety Goals directed toward infection prevention 4

Infection Prevention Hand Hygiene is the most important means of preventing and/or controlling infections – Perception of risk to the patient is sadly the least motivating in terms of Compliance with Hand Hygiene • Completing hand hygiene frequently and at key points of patient care significantly decreases the spread of infection – Surfaces are Contaminated with the Patient’s Organisms therefore Hand Hygiene must be performed after contact with Patient’s Environment. • The longer a patient is in a hospital the greater their risk is of 5 contracting an infection due to the increase in the number of contacts
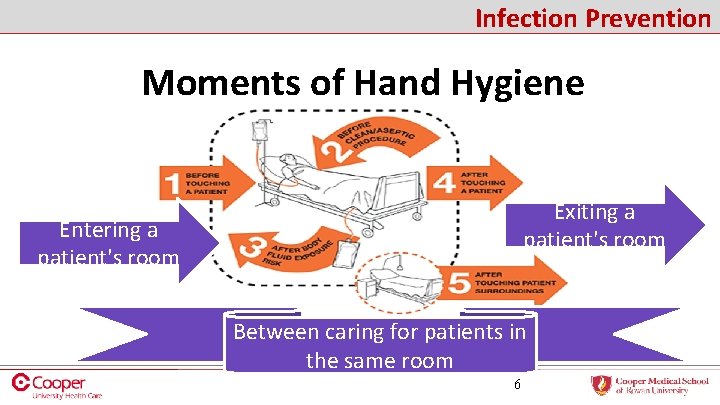
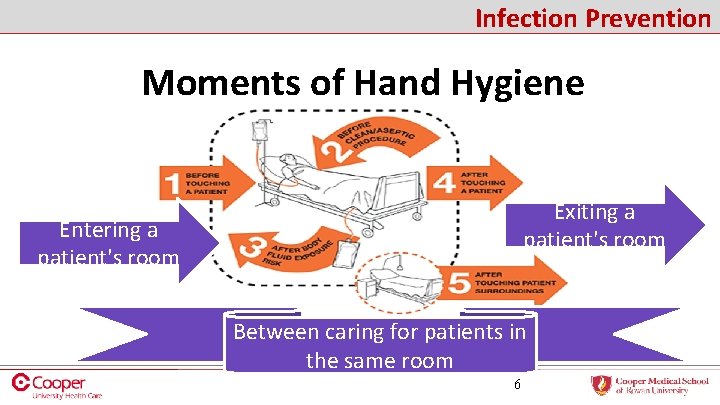
Infection Prevention Moments of Hand Hygiene Exiting a patient's room Entering a patient's room Between caring for patients in the same room 6
Moments of hand hygiene need to occur: • Before and after each patient contact • Before and after each glove use • Before and after contact with patient belongings • Before entering a patient room • After exiting a patient room 7
Infection Prevention • Important Hand Hygiene Facts o Pathogens can travel from patient to patient on the gloves/hands of healthcare workers. § Wash or gel before and after patient/belonging/equipment contact. o Materials can transfer to hands when removing gloves. § Wash or gel before and after glove use. § Germs are able to transfer to our hands from gloves, for this reason it is important to perform hand hygiene before and after glove use. 8
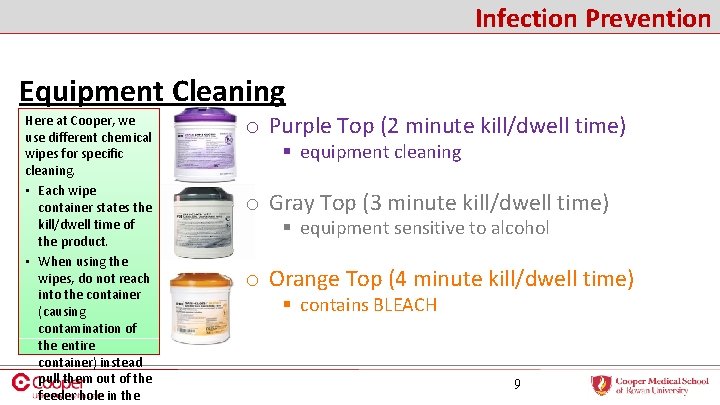
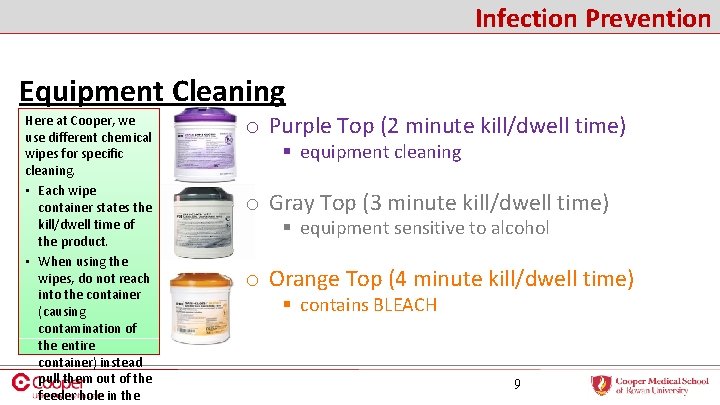
Infection Prevention Equipment Cleaning Here at Cooper, we use different chemical wipes for specific cleaning. • Each wipe container states the kill/dwell time of the product. • When using the wipes, do not reach into the container (causing contamination of the entire container) instead pull them out of the feeder hole in the o Purple Top (2 minute kill/dwell time) § equipment cleaning o Gray Top (3 minute kill/dwell time) § equipment sensitive to alcohol o Orange Top (4 minute kill/dwell time) § contains BLEACH 9

Infection Prevention • Hospital Associated Infections (HAIs) o What are HAIs? § Infections the patient would not have acquired if they were not in the hospital setting. o Hospital Associated Infections • • CAUTI – Catheter Associated Urinary Tract Infections CLABSI – Central Line Associated Blood Stream Infections VAP – Ventilator Associated Pneumonia SSI – Surgical Site Infections o How do HAIs affect the hospital if they are not contagious? § Patient Length of Stay is longer § Cooper does not get reimbursed for any care necessary to treat HAIs 10
Infection Prevention • How can you prevent HAIs? o CAUTI § Absence of catheter § Assess the need for Foley Catheters every shift § Initiate the Nurse-Driven Foley Removal Protocol when appropriate § Keep Foley bags off the floor, below the bladder and EMPTY § Secure tubing to the leg to prevent tension § Good Perineal care every shift and as needed 11
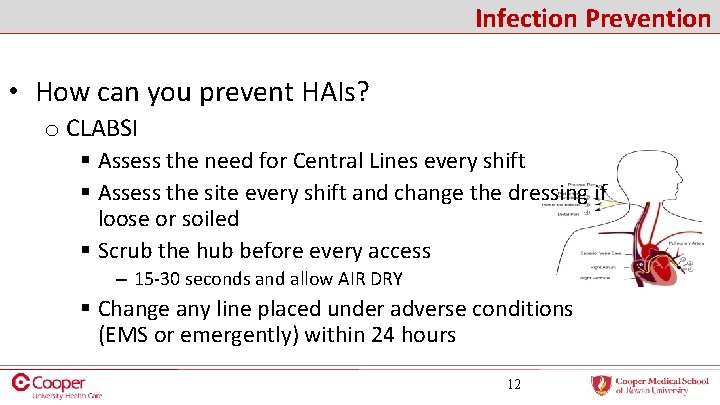
Infection Prevention • How can you prevent HAIs? o CLABSI § Assess the need for Central Lines every shift § Assess the site every shift and change the dressing if loose or soiled § Scrub the hub before every access – 15 -30 seconds and allow AIR DRY § Change any line placed under adverse conditions (EMS or emergently) within 24 hours 12
Infection Prevention • How can you prevent HAIs? o VAP § Head of bead positioned at 30 O § Oral care every 4 hours and as needed § Sedation Vacation o SSI § § Pre-op antibiotics Appropriate hair removal (no shaving) Glucose and temperature control Pre-op CHG bathing 13
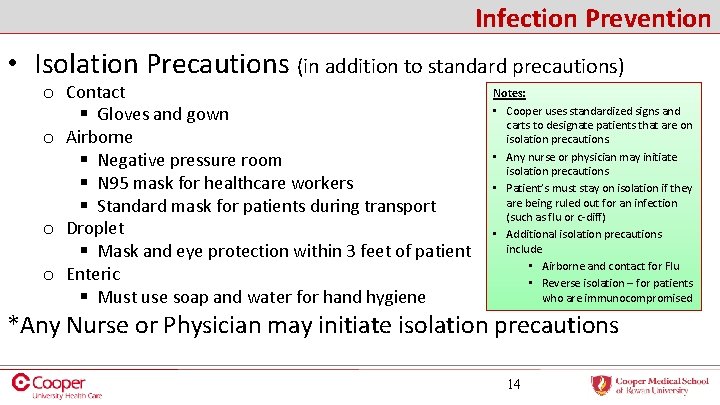
Infection Prevention • Isolation Precautions (in addition to standard precautions) o Contact § Gloves and gown o Airborne § Negative pressure room § N 95 mask for healthcare workers § Standard mask for patients during transport o Droplet § Mask and eye protection within 3 feet of patient o Enteric § Must use soap and water for hand hygiene Notes: • Cooper uses standardized signs and carts to designate patients that are on isolation precautions. • Any nurse or physician may initiate isolation precautions • Patient’s must stay on isolation if they are being ruled out for an infection (such as flu or c-diff) • Additional isolation precautions include • Airborne and contact for Flu • Reverse isolation – for patients who are immunocompromised *Any Nurse or Physician may initiate isolation precautions 14
Infection Prevention • Safe Injection Practices include using one syringe and one needle only one time on a patient. o One Syringe o One Time o One Needle • Become familiar with all Cooper Devices before use on patients. o IV catheters o Butterfly needles Example: Cooper’s butterfly needles retract with a push of a button and that button can be very sensitive. o Insulin Syringes o Safety needles 15
Infection Prevention • Patient Education o Information and materials are available on the Portal (English & Spanish) o Topics include § Preventing line infections § Preventing surgical site infections § Isolation Precautions…. . and more • Vaccine Information Sheets (VIS) are in the Infection Prevention Information Box and medication rooms. o Patients should receives the appropriate VIS when receiving any vaccine. 16
Patient Care Services Orientation
Pain • Joint Commission New and Revised Requirements o Involve patients in developing their treatment plans and setting realistic expectations and measurable goals o Promoting safe opioid use by identifying and monitoring high-risk patients o Facilitating clinician access to prescription drug monitoring program databases o Performance improvement activities focusing on pain assessment and management to increase the safety and quality for patients 18
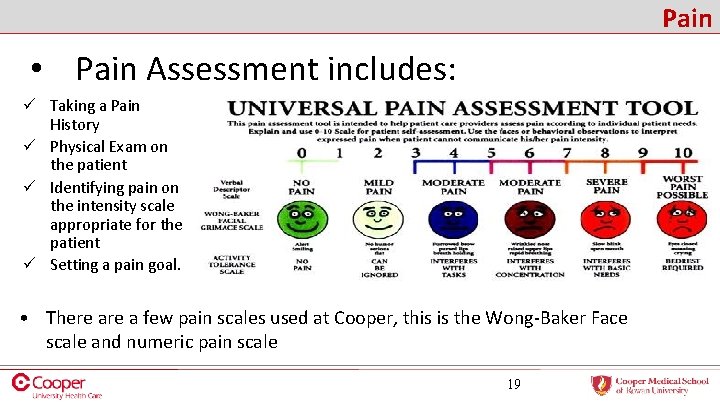
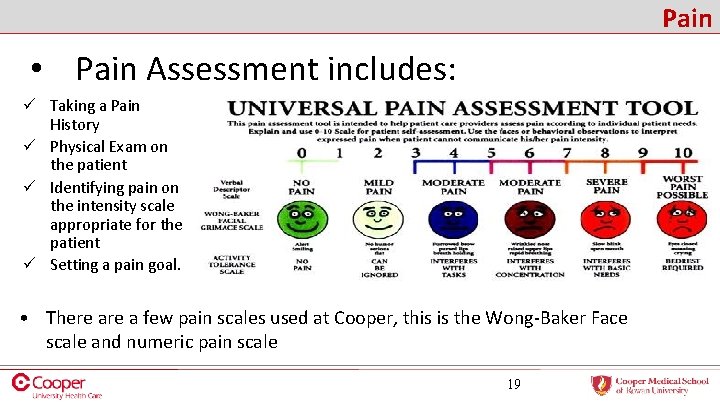
Pain • Pain Assessment includes: ü Taking a Pain History ü Physical Exam on the patient ü Identifying pain on the intensity scale appropriate for the patient ü Setting a pain goal. • There a few pain scales used at Cooper, this is the Wong-Baker Face scale and numeric pain scale 19
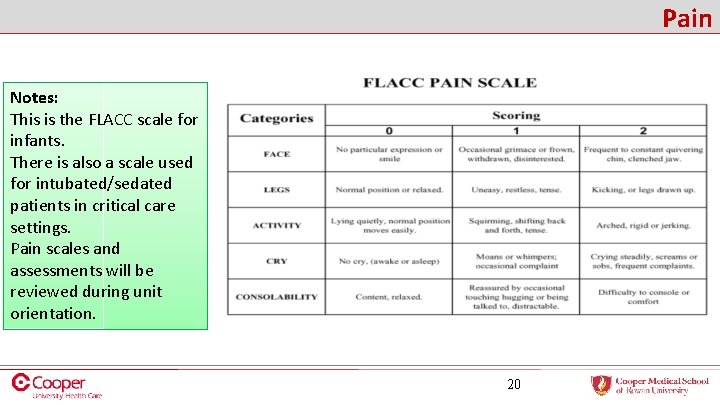
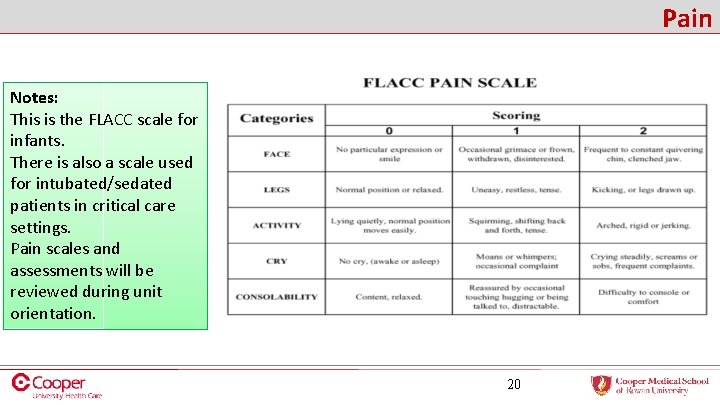
Pain Notes: This is the FLACC scale for infants. There is also a scale used for intubated/sedated patients in critical care settings. Pain scales and assessments will be reviewed during unit orientation. 20

Pain Key aspects of Pain Management • Pain assessment must be completed upon initial evaluation and in regular assessments • Reassessment must occur after each intervention (Medications 30 min post IV/60 min post PO/IM) • The absence of pain should be documented at regular intervals • Pain relief requires individualized treatment of pain • Healthcare providers, family and the patient must all work together to develop and implement a plan of pain relief • Effective pain relief is an important part of treatment • Communication of unrelieved pain is essential • Healthcare professionals shall respond quickly to reports of pain Please Review Policy – Pain Management 21
Pain education is not only for the patient. Staff and Family members also have a role in pain education. • Staff need to understand the expectations for pain management at Cooper and regularly document assessments, interventions and reassessments. • Staff should advocate for patients to receive the most appropriate pain management, which is not always more of the same medicine. • Patient and Family learning needs need to be evaluated and addressed. • Everyone should be aware of their role and responsibility regarding pain. • patients should not wait until pain is at an unacceptable level before notifying their nurse • The Care team, along with the patient and family, should set a pain goal that is acceptable and attainable for the patient in his/her situation • a post-op patient should not expect to be pain free post-op day 1 22

Pain Resources • Anesthesia Pain Management • Acute post-op complex pain management cases • Invasive techniques (epidurals/nerve blocks) • Physical Medicine and Rehabilitation (PM&R) • Physical Therapy Consults • Medication Management Consults • Palliative Care • Pain management in patients facing life threatening illnesses • Provides support for the patient and family 23

Performance Improvement Patient Care Services Orientation
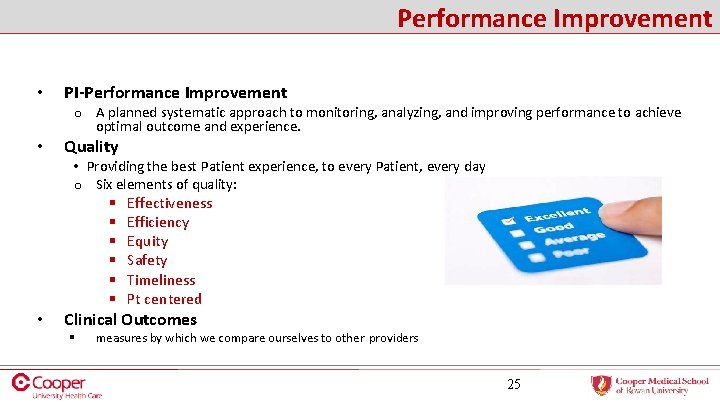
Performance Improvement • PI-Performance Improvement o A planned systematic approach to monitoring, analyzing, and improving performance to achieve optimal outcome and experience. • Quality • Providing the best Patient experience, to every Patient, every day o Six elements of quality: § Effectiveness § Efficiency § Equity § Safety § Timeliness § Pt centered • Clinical Outcomes § measures by which we compare ourselves to other providers 25
Performance Improvement • Core Measures are developed by the Joint Commission. • The first Core Measures were publicly reported in 2005 for AMI, HF and PNA • As hospitals become proficient at core measures, they retire old ones and add new ones, or modify existing ones • The Core Measures are the Foundation of how we deliver care using Evidencedbased practice • Cooper utilizes order sets, best practice alerts, and clinical documentation to improve quality in the organization. • Example of Current Core Measures o Stroke Core Measure (STK-1) § Venous Thromboembolism (VTE Prophylaxis) – Ischemic or hemorrhagic stroke patients to receive VTE prophylaxis the day of or the day after hospital admission 26
Performance Improvement • Value Based Purchasing o Participating hospitals are paid for inpatient acute care services based on the quality of care, not just quantity of services. Value based purchasing ensures that hospitals provide quality of care over quantity. 27
Performance Improvement • Outcomes Based Reimbursement o Patient Safety Indicators § CMS determines what Patient Safety Indicators to focus on based on National Standards and the cost to hospitals if these standards are not met. o Hospital Acquired Infections § Hospitals are financially penalized for patients who develop Hospital Acquired infections (such as CAUTI/CLABSI/VAP/SSI). § Hospitals do not receive reimbursement for care needed for a hospital acquired infection/problem. This is why it is so important to document wounds on admission, perform peri-care, follow removal bundles, follow antibiotic guidelines, etc. 28
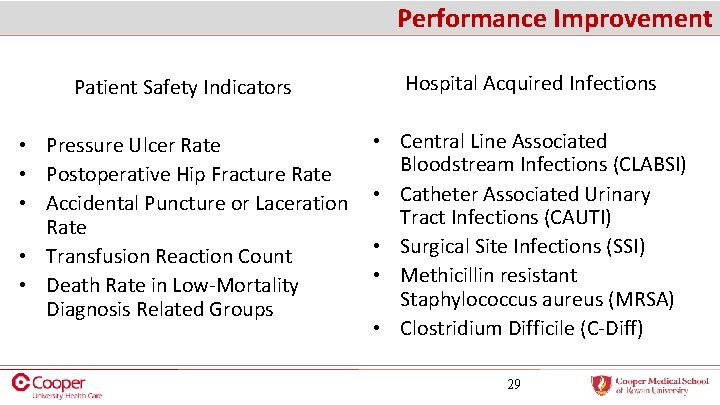
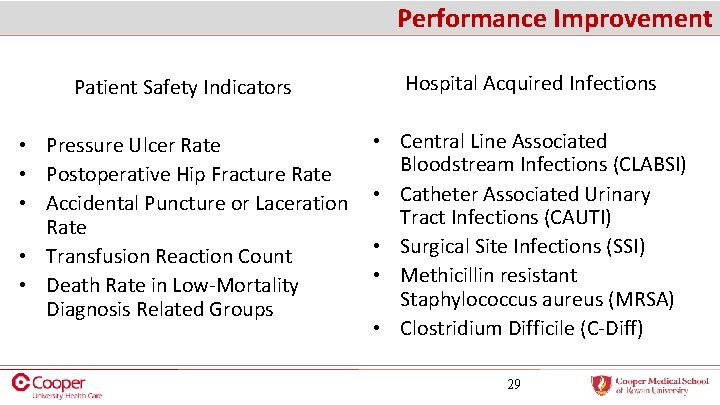
Performance Improvement Patient Safety Indicators Hospital Acquired Infections • Pressure Ulcer Rate • Postoperative Hip Fracture Rate • Accidental Puncture or Laceration Rate • Transfusion Reaction Count • Death Rate in Low-Mortality Diagnosis Related Groups • Central Line Associated Bloodstream Infections (CLABSI) • Catheter Associated Urinary Tract Infections (CAUTI) • Surgical Site Infections (SSI) • Methicillin resistant Staphylococcus aureus (MRSA) • Clostridium Difficile (C-Diff) 29
Performance Improvement Strategies to Keep Quality Affordable • • DMAIC process • Define, Measure, Analyze, Improve and Control. Six Sigma • Improvement teams use the DMAIC methodology to root out and eliminate the causes of defects Population Health: • Goal to keep pts out of ED by utilizing Health Coaches, APN’s, RN’s MA’s, primary care providers and community outreach to manage chronic conditions Clinical Documentation • RN’s trained in latest coding working with providers to clarify diagnoses and charting • Prevents the hospital from incurring penalties 30

Performance Improvement The entire organization has a role in quality. • What can you do? – – – Document accurately & timely Educate the pt and the family Minimize waste (time & resources) Keep the pt safe (from injury & infections) Participate in UBC, unit projects, LSS, staff mtgs, huddles & Nsg councils – Vaccinate and Immunize your pts and yourself – Use appropriate d/c instructions to prevent readmission. – Remember, if you didn’t document it, you didn’t do it!! 31
Transitional Care Patient Care Services Orientation
Transitional Care Social Work * Home Care * Health Coaches Main Department Number - (856)342 -3270 • AMION • Staff coverage is listed daily • Social Workers are on every unit • Home Care Coordinators cover multiple units • Individual contact information is provided • STAFFING • There is one social worker assigned to every in-patient unit • Home Care Coordinators cover multiple in-patient units • Referrals • Be Proactive - Early referrals allow for efficient & timely throughput
Transitional Care Social Work – Consult Required. Staffed 7 days a week • • • Crisis intervention Homelessness Abuse/Neglect (Child/Adult) ESRD (End Stage Renal Patients) ETOH/Substance Abuse In patient psychiatric Social Work coverage Facility Placement (long-term care, rehab, LTACH) Hospice (In-Patient/Scatter Bed) Some transportation Needs (for patients Social Work is following)
Transitional Care Home Care Coordinators – Consult Required. Staffed 7 days a week. • • Visiting Nurse Follow Up Home PT, OT, ST Home Infusions (TPN, IV Antibiotics) Wound Vacs Durable Medical Equipment (DME) Home Hospice Transportation Needs (for patients Home Care is following)

Transitional Care Transitional Health Care Coach • Health Care Coaches use a risk stratification tool to determine need and are staffed Monday thru Friday. • Health Care Coaches • provide community-based resources • Evaluate self-management goals • Coordinate follow-up appointments and transportation • Utilize Risk Stratification. Staffed Monday thru Friday • Follow patients while admitted • If appropriate, follow for 30 days post discharge • Linkage to community based resources • Determine post discharge self-management goals with the patients • Coordinate follow-up appointments & transportation
Wound Care Patient Care Services Orientation
Wound Care • • What is a Wound/Ostomy/Continence (WOC) Nurse Specialty of Nursing Advanced education/certification Acute/rehabilitative care for GI, GU, Skin system problems Direct/Assistive care: o Evaluation/Implementation/Planning • WOC nurses are able to provide direct or assistive care for the following: • Skin care prevention • Abdominal stomas • Complex wounds • Fistulas/Drains • Pressure injuries • Continence disorders 38
Wound Care Consulting WOCN Educators • • • Educate staff and physicians Provide consults and recommendations Review quality Always evaluate situation before consult Place consult in EPIC o Enterostomal Therapy. (Follow prompts) o Complete all requested information 39
Wound Care Questions • Daytime – Immediate o Linda Gazzerro- 1008445 o Elizabeth Sgrillo-1008716 • After 4: 30 pm- 856 -963 -3957. Leave message • Email- Days/Nights/Weekends. Gazzerro-Linda@Cooperhealth. edu 40 to WOCNs?
This completes the self-learning packet form Patient Care Services. You will be required to sign an attestation at Patient Care Service Orientation acknowledging receipt of the packet. Patient Care Service Orientation occurs on the Tuesday after Hospital Orientation. Questions or concerns feel free to contact Jennifer Harbourt (856) 968 -8522 or Christal Young (856) 968 -7829