PATIENT CARE NETWORK OF OKLAHOMA PCNOK Oklahoma Healthcare





- Slides: 17
PATIENT CARE NETWORK OF OKLAHOMA (PCNOK) Oklahoma Healthcare Authority ABD Care Coordination RFI Response August 17, 2015
2 Patient Care Network of Oklahoma • Care coordination network of 20 Federally Qualified Health Centers (FQHCs) • Serve over 160, 000 patients • Operate over 50 primary care sites in 77 counties • Patient Centered Medical Homes that currently target chronically ill and medically complex patients • Strategic investment in infrastructure including Electronic Health Records, Health Information Exchange (connectivity to My. Health), and data analytics and performance measurement (i. e. Sooner. Verse)
3 FQHCs in Oklahoma
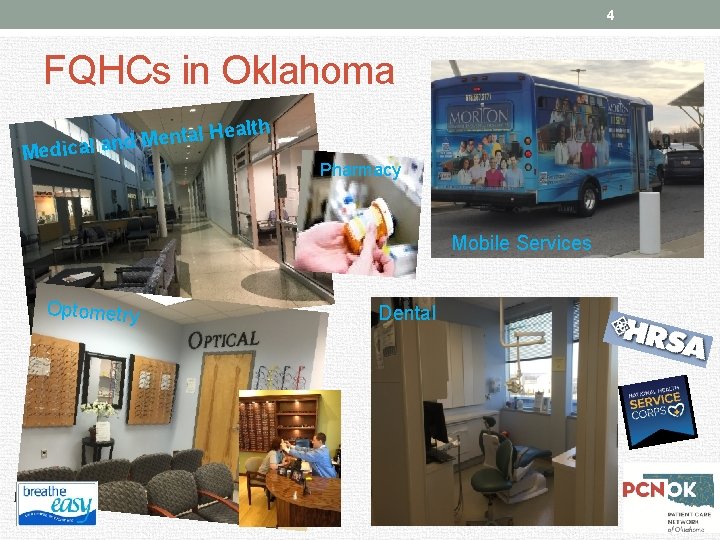
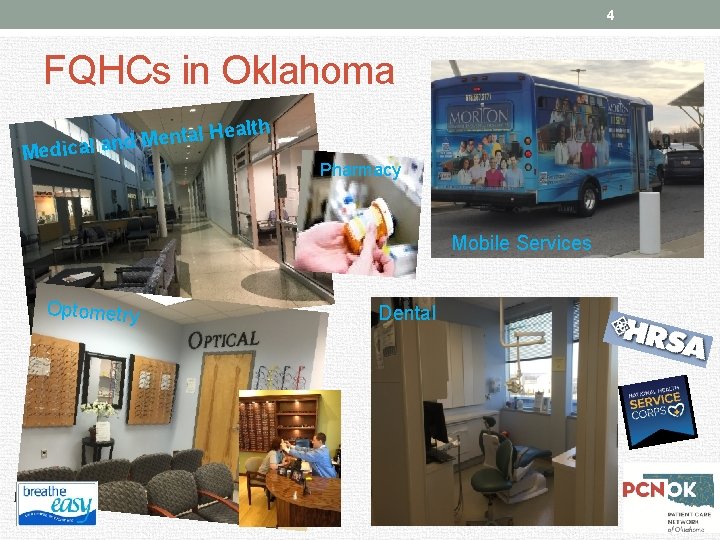
4 FQHCs in Oklahoma ealth H l a t n e M d Medical an Pharmacy Mobile Services Optometry Dental
5 FQHCs are Uniquely Positioned “Many FQHCs and CHCs are uniquely positioned to coordinate care for dual-eligible beneficiaries because they provide primary care, behavioral health services, and care management services, often at the same clinic site. ” The Medicare Payment Advisory Commission: June 2013 Report to the Congress: Medicare and the Health Care Delivery System
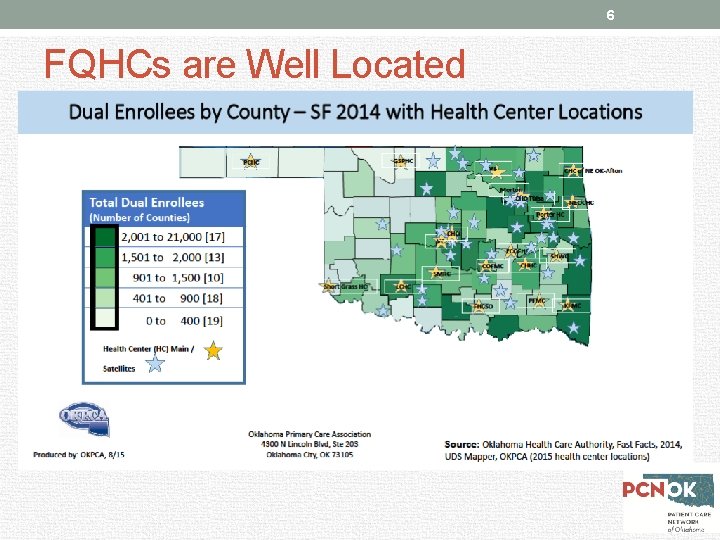
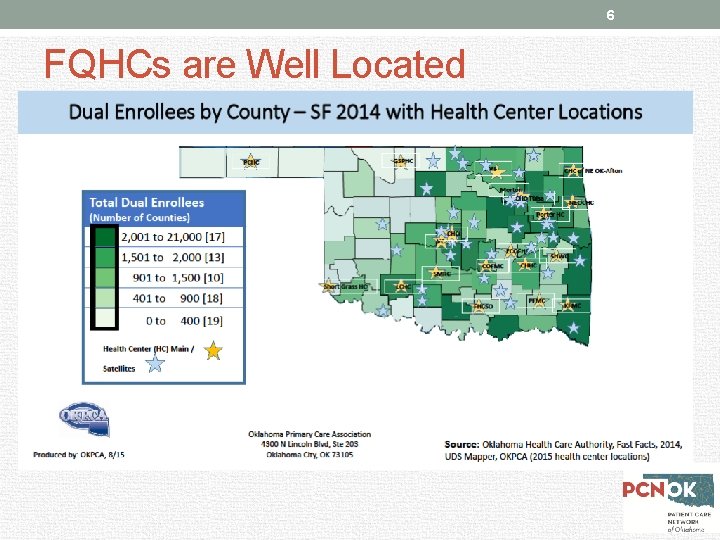
6 FQHCs are Well Located

7 Ultra-sound l He alth Ser vice dic Ora Car e s Pa y, a R s n tio a ic La M ed Ey Be h tie - X b, e Me En ab lin g al C are So cia l FQHCs: Comprehensive Services / Patient Centered Care e r ca nt Ed u av ior a ca l. H tio n ea lth

8 FQHC: Care Model for Complex Patients Integrated Delivery Model Data Driven Patient Centered Better Outcomes………AND Lower Costs
9 Proposed Model: Care Coordination led by Patient Centered Medical Homes • Develop an Accountable Care Organization structure that will manage the cost and quality outcomes of the target population through a managed fee-for-service payment mechanism • Employ a care coordination model that includes local, dedicated care managers to work with the highest complexity patients • Through investments from the State, establish a robust technology and data infrastructure for the creation of statewide care coordination and claims-based risk assessments and interventions

10 Proposed Model: Care Coordination led by Patient Centered Medical Homes
11 Best Practices for Complex Patients • High-contact, on the ground intensive care management • Focus on coordinating communication across provider care settings (i. e. hospitals, primary care, social service agencies) • Leverage community-based resources, including FQHCs • Many FQHCs are uniquely positioned to coordinate care for dual-eligible beneficiaries because they provide primary care, behavioral health services, and care management services, often at the same clinic site Source: The Medicare Payment Advisory Commission: June 2013 Report to the Congress: Medicare and the Health Care Delivery System

12 Proposed Model: Flexibility and Scalability • Builds upon existing community based, managed FFS pilots already underway in Oklahoma • Leverages existing infrastructure among FQHCs • Allows for flexibility and innovation over time • Risk sharing models could change as model matures • PCNOK can interact with a variety of payers • Model can expand to include patients beyond Duals • Includes proven best practices of approaches in other states that target Duals and other high-need patients

13 Financial Model Overview • Maintenance of the payment relationship between Sooner. Care and Medicare as payers; PCNOK FQHCs maintain all base, contracted services within the current covered benefits and services. • Tiered PBPM payment based on acuity to the PCNOK to cover the cost of the Care Management function. • “Shared Savings” payments paid to the PCNOK, and correspondingly shared to the Health Centers. • Quality measures that demonstrate no use of “care rationing” to achieve cost goals. • No impact on patient’s right to choose where to seek care or payment terms to providers outside of the PCNOK. • Alignment with State and Federal Regulations.
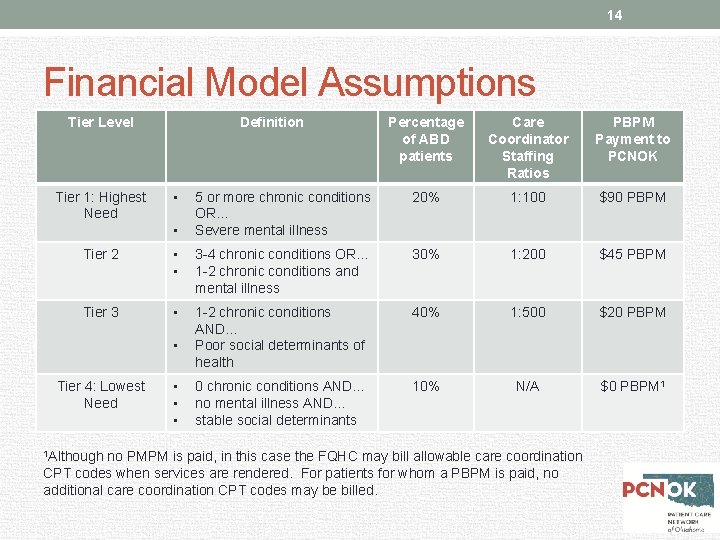
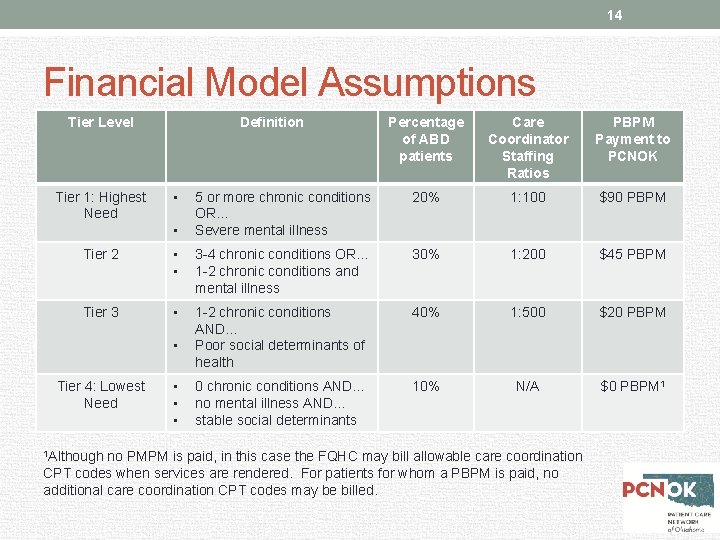
14 Financial Model Assumptions Tier Level Tier 1: Highest Need Definition • • Percentage of ABD patients Care Coordinator Staffing Ratios PBPM Payment to PCNOK 5 or more chronic conditions OR… Severe mental illness 20% 1: 100 $90 PBPM Tier 2 • • 3 -4 chronic conditions OR… 1 -2 chronic conditions and mental illness 30% 1: 200 $45 PBPM Tier 3 • 1 -2 chronic conditions AND… Poor social determinants of health 40% 1: 500 $20 PBPM 0 chronic conditions AND… no mental illness AND… stable social determinants 10% N/A $0 PBPM 1 • Tier 4: Lowest Need 1 Although • • • no PMPM is paid, in this case the FQHC may bill allowable care coordination CPT codes when services are rendered. For patients for whom a PBPM is paid, no additional care coordination CPT codes may be billed.
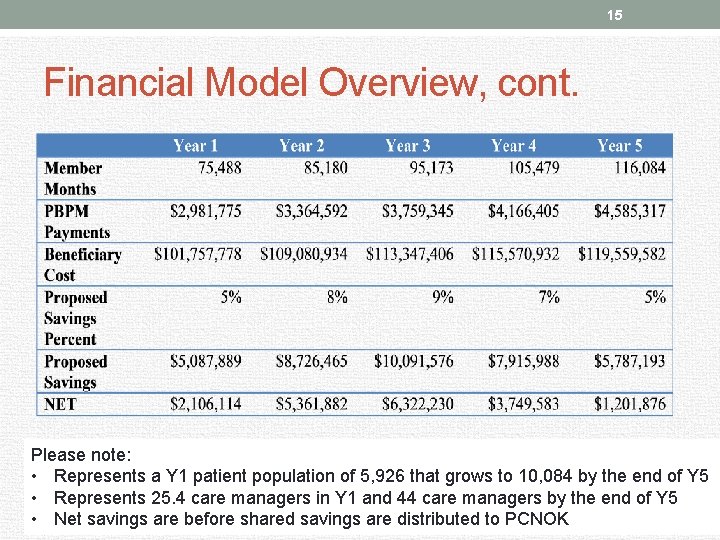
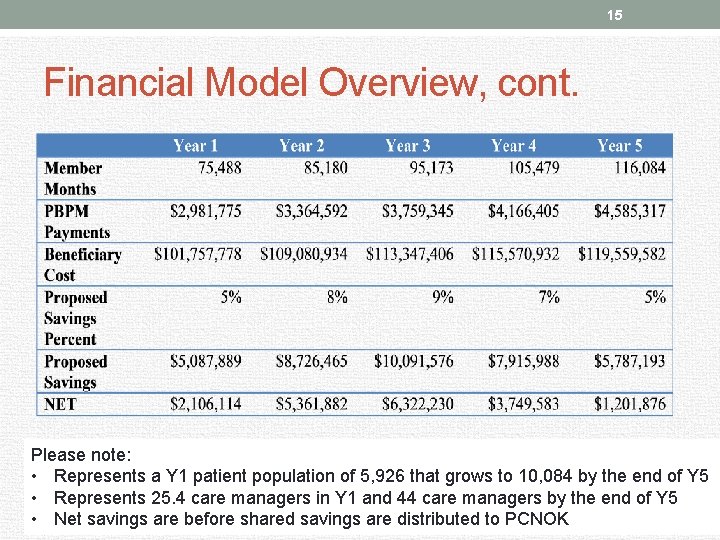
15 Financial Model Overview, cont. Please note: • Represents a Y 1 patient population of 5, 926 that grows to 10, 084 by the end of Y 5 • Represents 25. 4 care managers in Y 1 and 44 care managers by the end of Y 5 • Net savings are before shared savings are distributed to PCNOK
16 Efficient, Effective, Patient-Centered Hospital Admission Social Services Out Patient Care Specialty Care
17 QUESTIONS
 Pcnok
Pcnok Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Sports medicine definition
Sports medicine definition Primary care secondary care tertiary care
Primary care secondary care tertiary care Patient 2 patient
Patient 2 patient Oklahoma health care authority
Oklahoma health care authority Smartnet vs smartnet total care
Smartnet vs smartnet total care Uhccp com tnenroll
Uhccp com tnenroll Va sunshine healthcare network
Va sunshine healthcare network Xcel primary care frederick md
Xcel primary care frederick md Team nursing care delivery model
Team nursing care delivery model Primary nursing care model
Primary nursing care model Qsen standards
Qsen standards What is progressive patient care
What is progressive patient care The factors of care that patients can expect to receive
The factors of care that patients can expect to receive Nursing management
Nursing management Ocd nursing management
Ocd nursing management Chapter 55 care of the patient with an immune disorder
Chapter 55 care of the patient with an immune disorder