Patient and financial impact of implementing WHO recommendations

- Slides: 14

Patient and financial impact of implementing WHO recommendations for EID testing – expanding entry point testing and introduction of POC Jenna Mezhrahid CHAI Laboratory Services Team July 25 th, 2017 Paris, FRANCE 1
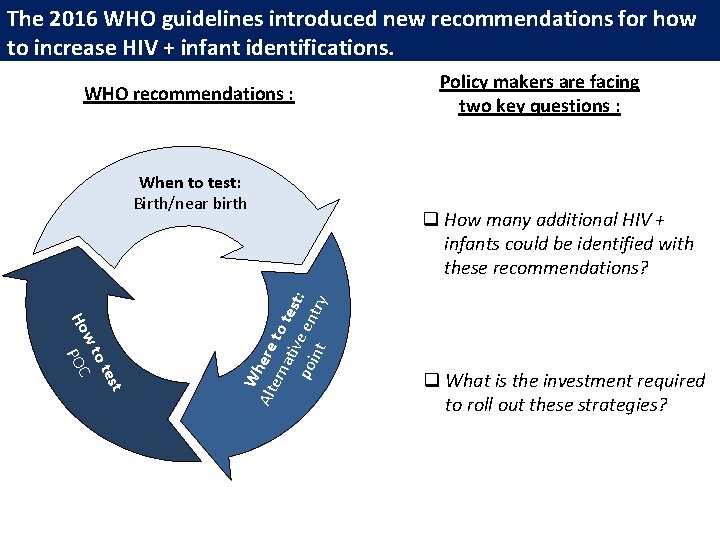
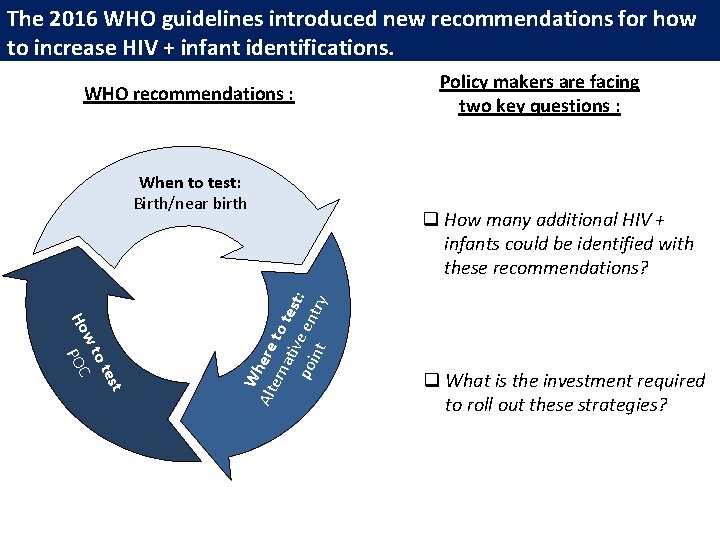
The 2016 WHO guidelines introduced new recommendations for how to increase HIV + infant identifications. WHO recommendations : est ot wt Ho POC W Alt here ern to ati tes po ve en t: int try When to test: Birth/near birth Policy makers are facing two key questions : q How many additional HIV + infants could be identified with these recommendations? q What is the investment required to roll out these strategies?
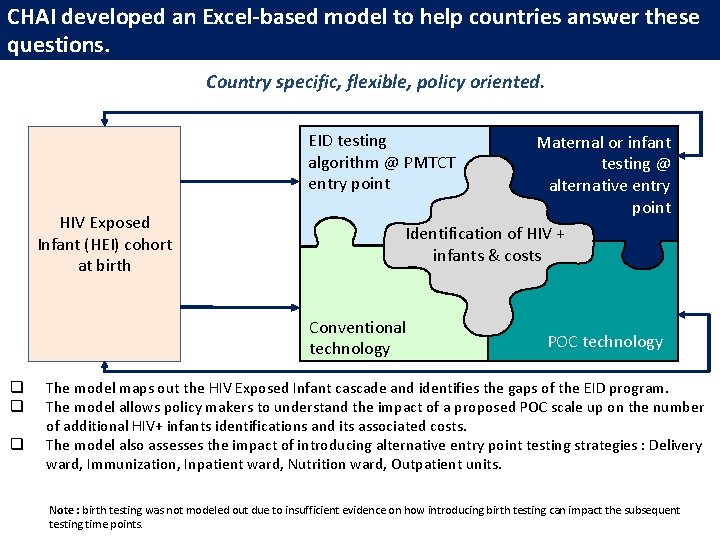
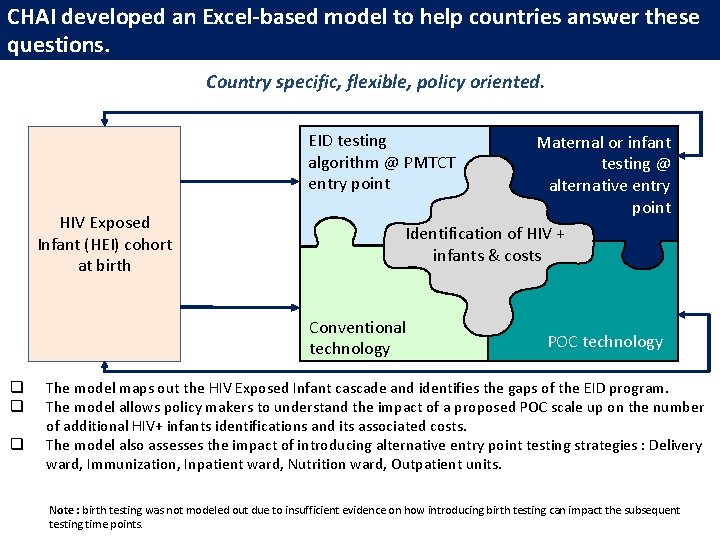
CHAI developed an Excel-based model to help countries answer these questions. Country specific, flexible, policy oriented. EID testing algorithm @ PMTCT entry point HIV Exposed Infant (HEI) cohort at birth Maternal or infant testing @ alternative entry point Identification of HIV + infants & costs Conventional technology q q q POC technology The model maps out the HIV Exposed Infant cascade and identifies the gaps of the EID program. The model allows policy makers to understand the impact of a proposed POC scale up on the number of additional HIV+ infants identifications and its associated costs. The model also assesses the impact of introducing alternative entry point testing strategies : Delivery ward, Immunization, Inpatient ward, Nutrition ward, Outpatient units. Note : birth testing was not modeled out due to insufficient evidence on how introducing birth testing can impact the subsequent testing time points.
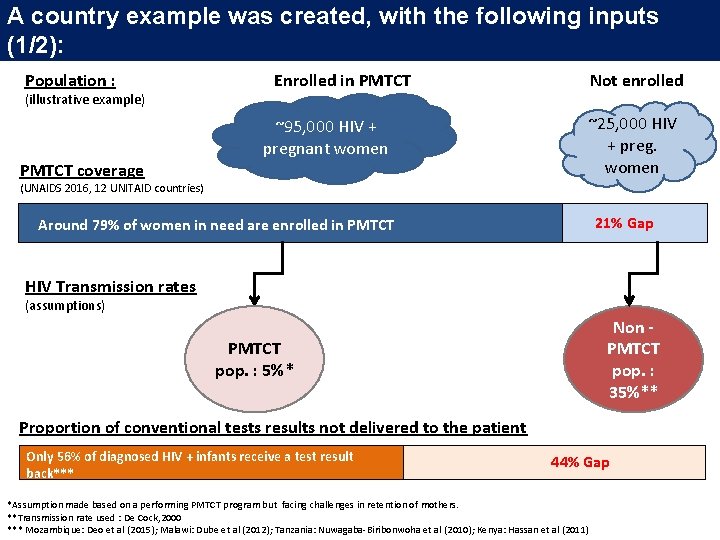
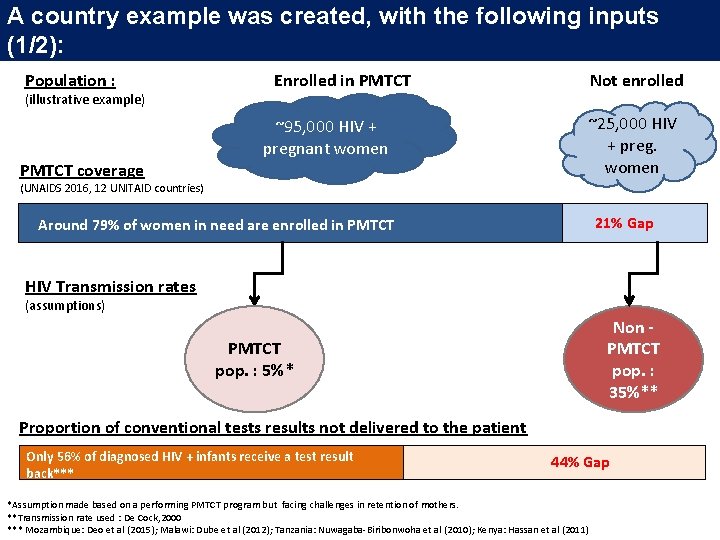
A country example was created, with the following inputs (1/2): Population : (illustrative example) Enrolled in PMTCT ~95, 000 HIV + pregnant women PMTCT coverage Not enrolled ~25, 000 HIV + preg. women (UNAIDS 2016, 12 UNITAID countries) 21% Gap Around 79% of women in need are enrolled in PMTCT HIV Transmission rates (assumptions) Non PMTCT pop. : 35%** PMTCT pop. : 5%* Proportion of conventional tests results not delivered to the patient Only 56% of diagnosed HIV + infants receive a test result back*** 44% Gap *Assumption made based on a performing PMTCT program but facing challenges in retention of mothers. **Transmission rate used : De Cock, 2000 *** Mozambique: Deo et al (2015); Malawi: Dube et al (2012); Tanzania: Nuwagaba-Biribonwoha et al (2010); Kenya: Hassan et al (2011)
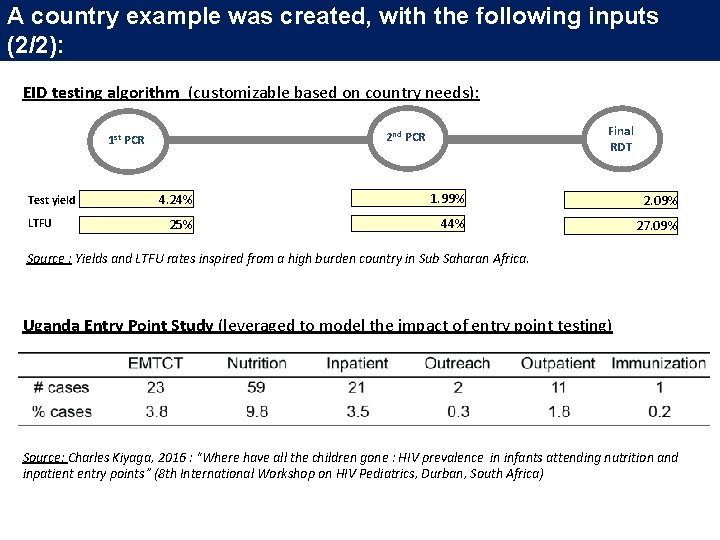
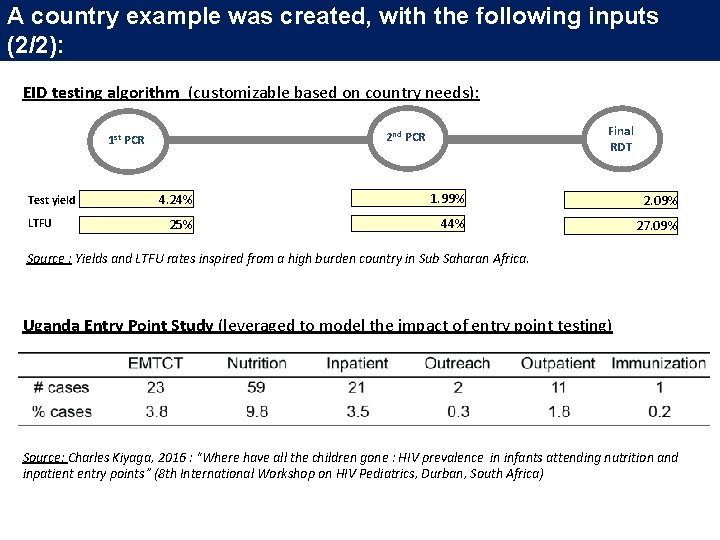
A country example was created, with the following inputs (2/2): EID testing algorithm (customizable based on country needs): Test yield LTFU Final RDT 2 nd PCR 1 st PCR 4. 24% 1. 99% 2. 09% 25% 44% 27. 09% Source : Yields and LTFU rates inspired from a high burden country in Sub Saharan Africa. Uganda Entry Point Study (leveraged to model the impact of entry point testing) Source: Charles Kiyaga, 2016 : “Where have all the children gone : HIV prevalence in infants attending nutrition and inpatient entry points” (8 th International Workshop on HIV Pediatrics, Durban, South Africa)
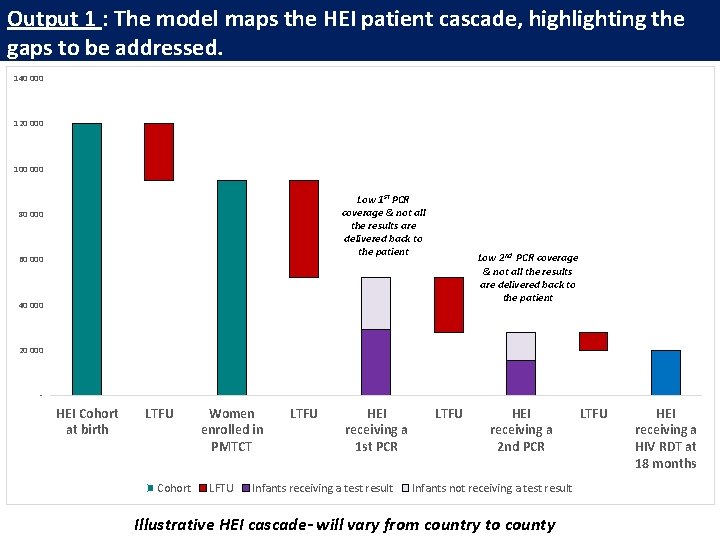
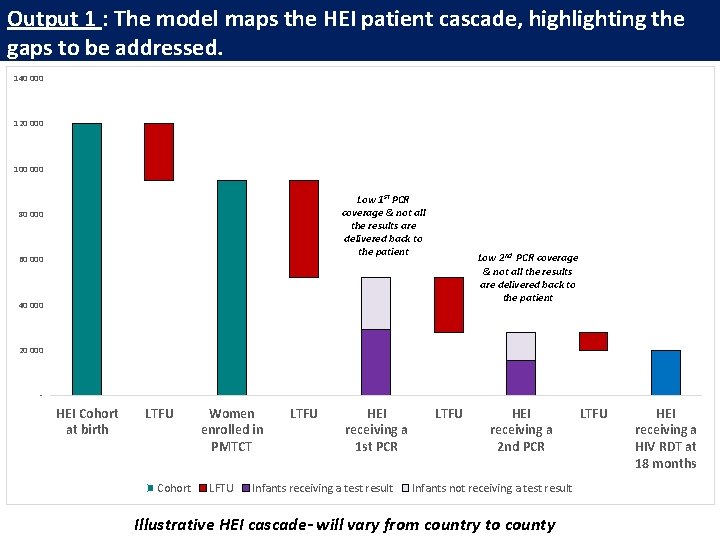
Output 1 : The model maps the HEI patient cascade, highlighting the gaps to be addressed. 140 000 120 000 100 000 Low 1 st PCR coverage & not all the results are delivered back to the patient 80 000 60 000 Low 2 nd PCR coverage & not all the results are delivered back to the patient 40 000 20 000 - HEI Cohort at birth LTFU Cohort Women enrolled in PMTCT LFTU LTFU HEI receiving a 1 st PCR Infants receiving a test result LTFU HEI receiving a 2 nd PCR Infants not receiving a test result Illustrative HEI cascade- will vary from country to county LTFU HEI receiving a HIV RDT at 18 months
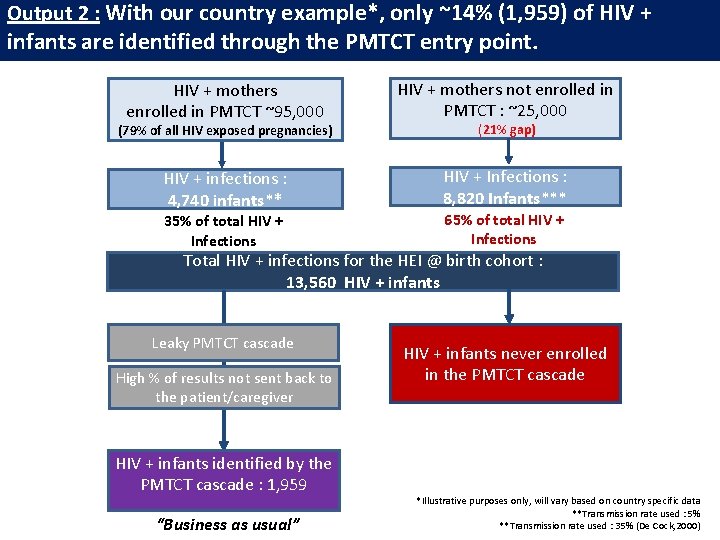
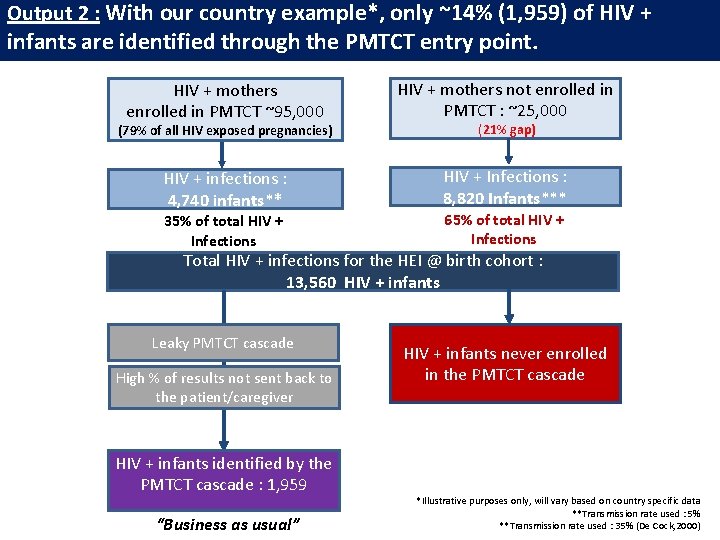
Output 2 : With our country example*, only ~14% (1, 959) of HIV + infants are identified through the PMTCT entry point. HIV + mothers enrolled in PMTCT ~95, 000 HIV + mothers not enrolled in PMTCT : ~25, 000 (79% of all HIV exposed pregnancies) (21% gap) HIV + infections : 4, 740 infants** HIV + Infections : 8, 820 Infants*** 35% of total HIV + Infections 65% of total HIV + Infections Total HIV + infections for the HEI @ birth cohort : 13, 560 HIV + infants Leaky PMTCT cascade High % of results not sent back to the patient/caregiver HIV + infants identified by the PMTCT cascade : 1, 959 “Business as usual” HIV + infants never enrolled in the PMTCT cascade *Illustrative purposes only, will vary based on country specific data **Transmission rate used : 5% **Transmission rate used : 35% (De Cock, 2000)
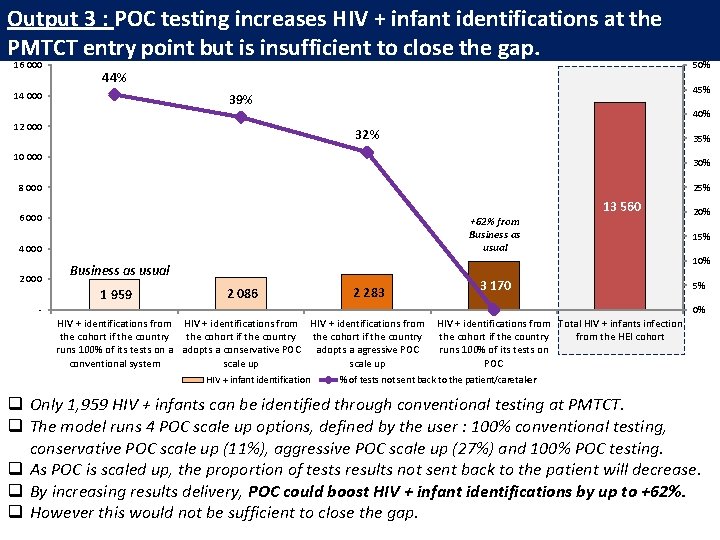
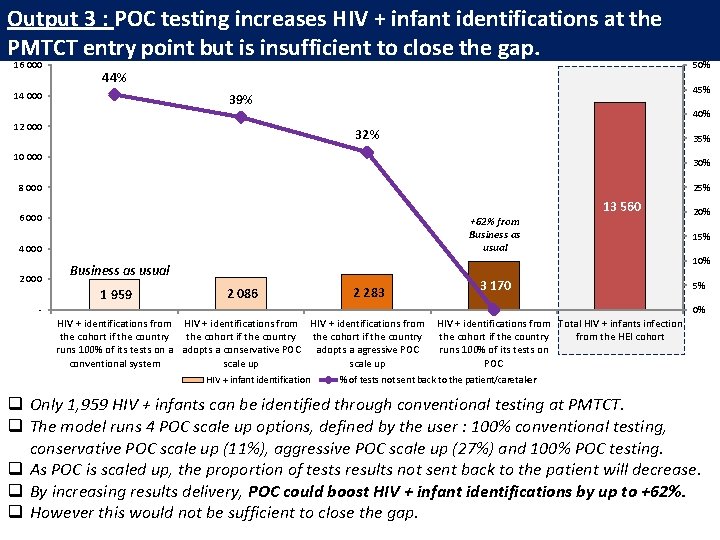
Output 3 : POC testing increases HIV + infant identifications at the PMTCT entry point but is insufficient to close the gap. 16 000 44% 14 000 45% 39% 12 000 40% 32% 35% 10 000 30% 8 000 25% 6 000 +62% from Business as usual 4 000 2 000 50% 20% 15% 10% Business as usual 1 959 13 560 2 086 2 283 3 170 - 5% 0% HIV + identifications from the cohort if the country runs 100% of its tests on a adopts a conservative POC adopts a agressive POC conventional system scale up HIV + infant identification HIV + identifications from Total HIV + infants infection the cohort if the country from the HEI cohort runs 100% of its tests on POC % of tests not sent back to the patient/caretaker q Only 1, 959 HIV + infants can be identified through conventional testing at PMTCT. q The model runs 4 POC scale up options, defined by the user : 100% conventional testing, conservative POC scale up (11%), aggressive POC scale up (27%) and 100% POC testing. q As POC is scaled up, the proportion of tests results not sent back to the patient will decrease. q By increasing results delivery, POC could boost HIV + infant identifications by up to +62%. q However this would not be sufficient to close the gap.
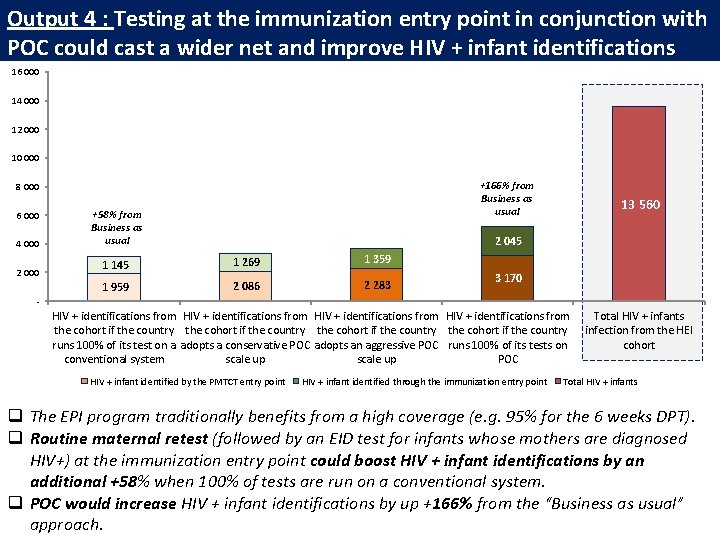
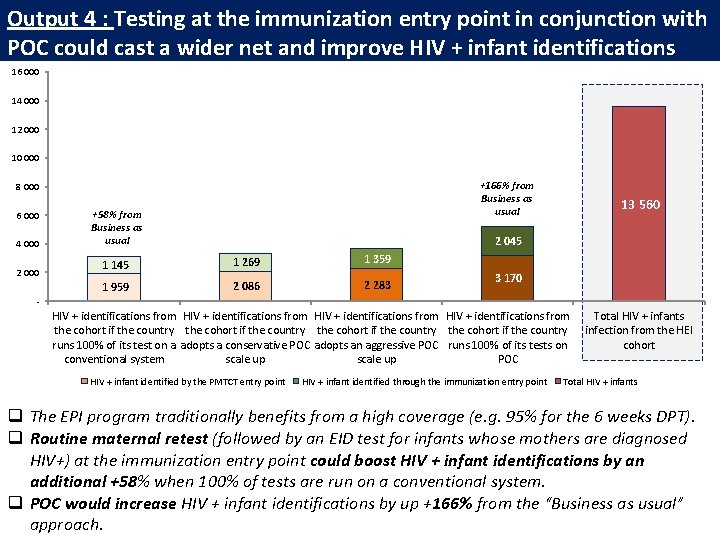
Output 4 : Testing at the immunization entry point in conjunction with POC could cast a wider net and improve HIV + infant identifications 16 000 14 000 12 000 10 000 +166% from Business as usual 8 000 6 000 4 000 2 000 +58% from Business as usual 13 560 2 045 1 145 1 269 1 359 1 959 2 086 2 283 3 170 - HIV + identifications from the cohort if the country runs 100% of its test on a adopts a conservative POC adopts an aggressive POC runs 100% of its tests on conventional system scale up POC HIV + infant identified by the PMTCT entry point HIV + infant identified through the immunization entry point Total HIV + infants infection from the HEI cohort Total HIV + infants q The EPI program traditionally benefits from a high coverage (e. g. 95% for the 6 weeks DPT). q Routine maternal retest (followed by an EID test for infants whose mothers are diagnosed HIV+) at the immunization entry point could boost HIV + infant identifications by an additional +58% when 100% of tests are run on a conventional system. q POC would increase HIV + infant identifications by up +166% from the “Business as usual” approach.
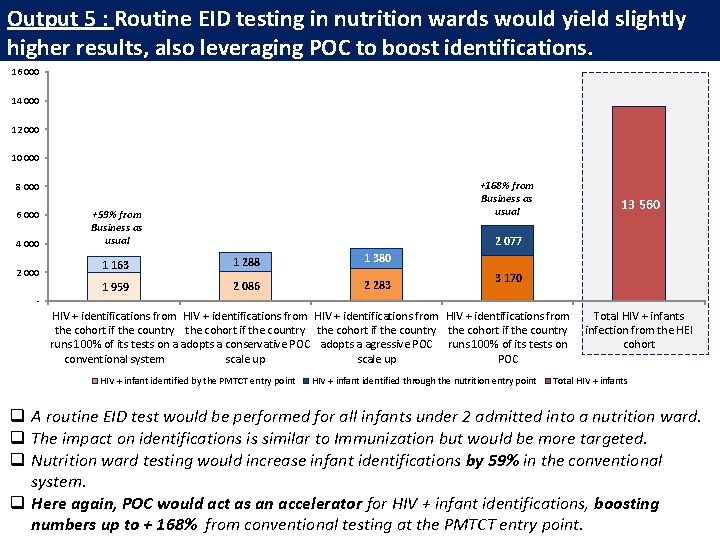
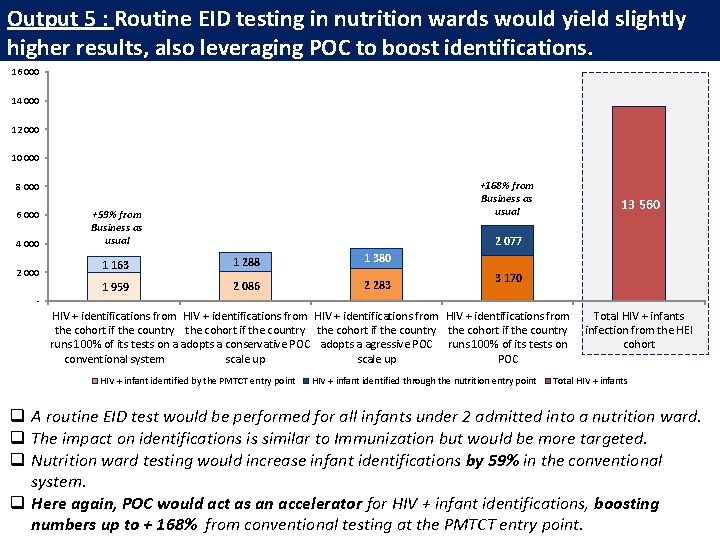
Output 5 : Routine EID testing in nutrition wards would yield slightly higher results, also leveraging POC to boost identifications. 16 000 14 000 12 000 10 000 +168% from Business as usual 8 000 6 000 4 000 2 000 +59% from Business as usual 13 560 2 077 1 163 1 288 1 380 1 959 2 086 2 283 3 170 - HIV + identifications from the cohort if the country runs 100% of its tests on a adopts a conservative POC adopts a agressive POC runs 100% of its tests on conventional system scale up POC HIV + infant identified by the PMTCT entry point HIV + infant identified through the nutrition entry point Total HIV + infants infection from the HEI cohort Total HIV + infants q A routine EID test would be performed for all infants under 2 admitted into a nutrition ward. q The impact on identifications is similar to Immunization but would be more targeted. q Nutrition ward testing would increase infant identifications by 59% in the conventional system. q Here again, POC would act as an accelerator for HIV + infant identifications, boosting numbers up to + 168% from conventional testing at the PMTCT entry point.
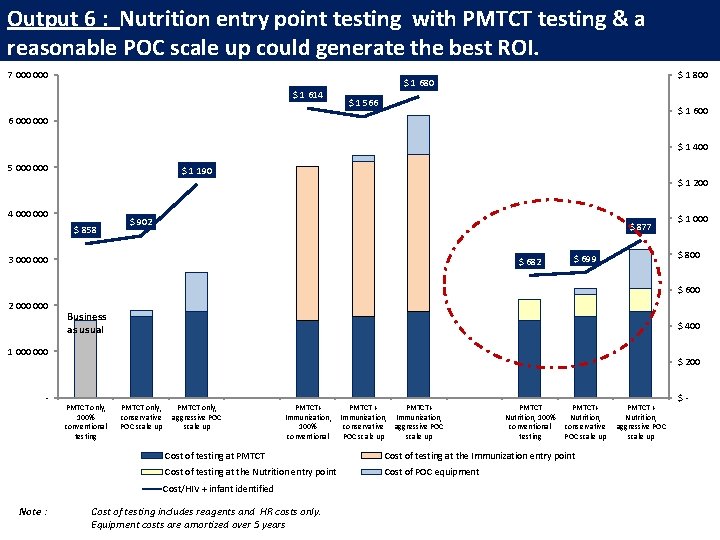
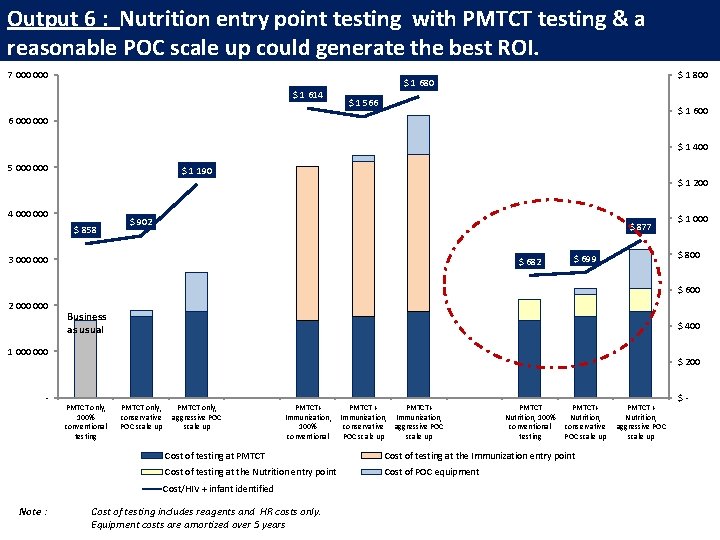
Output 6 : Nutrition entry point testing with PMTCT testing & a reasonable POC scale up could generate the best ROI. 7 000 $ 1 614 $ 1 800 $ 1 680 $ 1 566 $ 1 600 6 000 $ 1 400 5 000 $ 1 190 4 000 $ 858 $ 1 200 $ 902 $ 877 3 000 $ 682 $ 1 000 $ 800 $ 699 $ 600 2 000 Business as usual $ 400 1 000 - $ 200 PMTCT only, 100% conventional testing PMTCT only, conservative POC scale up PMTCT only, aggressive POC scale up PMTCT+ Immunization, 100% conventional PMTCT Nutrition, 100% conventional testing PMTCT+ Nutrition, conservative POC scale up Cost of testing at PMTCT Cost of testing at the Immunization entry point Cost of testing at the Nutrition entry point Cost of POC equipment Cost/HIV + infant identified Note : PMTCT + PMTCT+ Immunization, conservative aggressive POC scale up Cost of testing includes reagents and HR costs only. Equipment costs are amortized over 5 years PMTCT + Nutrition, aggressive POC scale up $-
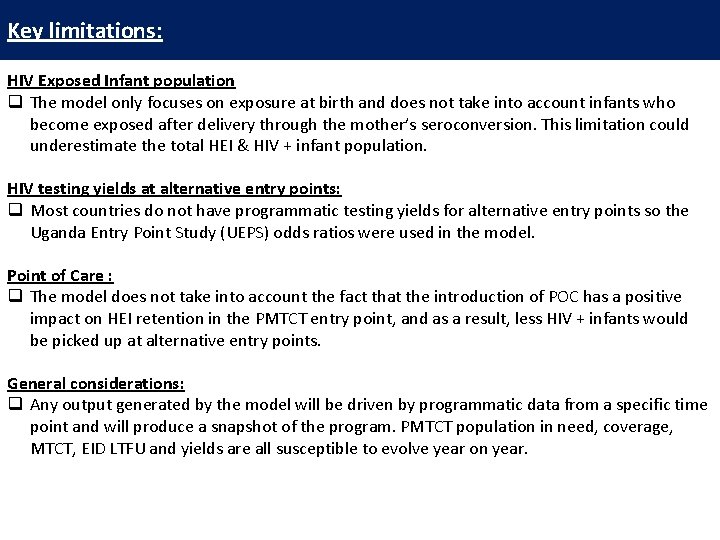
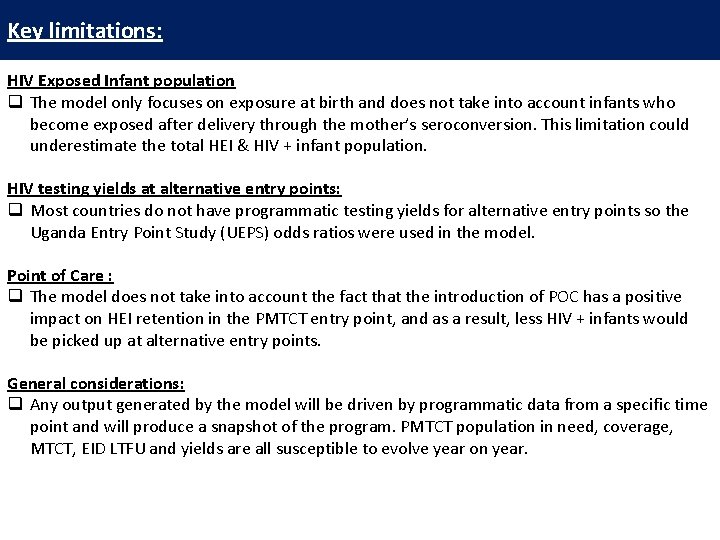
Key limitations: HIV Exposed Infant population q The model only focuses on exposure at birth and does not take into account infants who become exposed after delivery through the mother’s seroconversion. This limitation could underestimate the total HEI & HIV + infant population. HIV testing yields at alternative entry points: q Most countries do not have programmatic testing yields for alternative entry points so the Uganda Entry Point Study (UEPS) odds ratios were used in the model. Point of Care : q The model does not take into account the fact that the introduction of POC has a positive impact on HEI retention in the PMTCT entry point, and as a result, less HIV + infants would be picked up at alternative entry points. General considerations: q Any output generated by the model will be driven by programmatic data from a specific time point and will produce a snapshot of the program. PMTCT population in need, coverage, MTCT, EID LTFU and yields are all susceptible to evolve year on year.
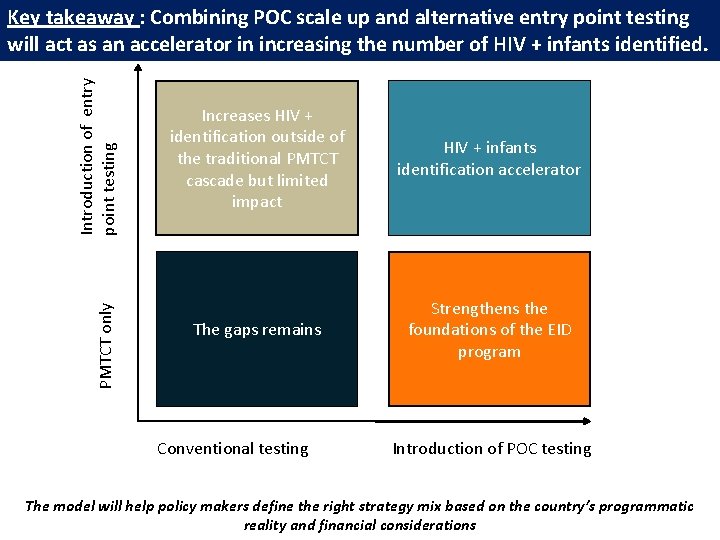
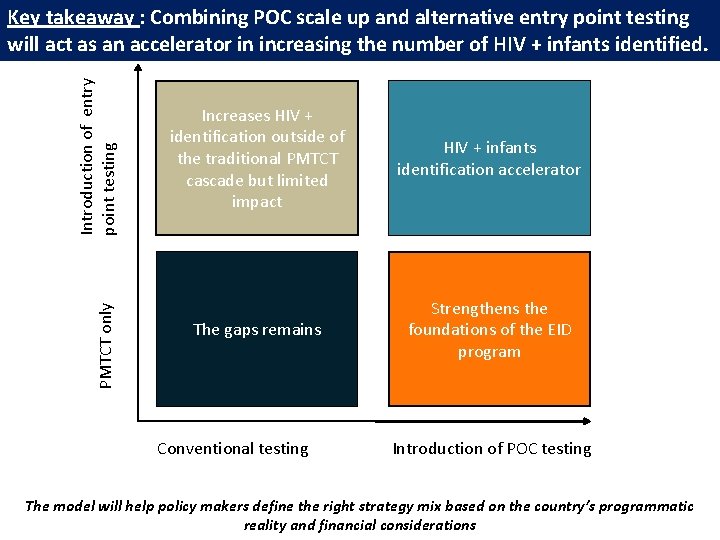
PMTCT only Introduction of entry point testing Key takeaway : Combining POC scale up and alternative entry point testing will act as an accelerator in increasing the number of HIV + infants identified. Increases HIV + identification outside of the traditional PMTCT cascade but limited impact HIV + infants identification accelerator The gaps remains Strengthens the foundations of the EID program Conventional testing Introduction of POC testing The model will help policy makers define the right strategy mix based on the country’s programmatic reality and financial considerations
Thank you ! For any questions : Jenna Mezhrahid jmezhrahid@clintonhealthaccess. org