Pathophysiology of respiratory system 2 Obstructive and restrictive
Pathophysiology of respiratory system 2 Obstructive and restrictive diseases
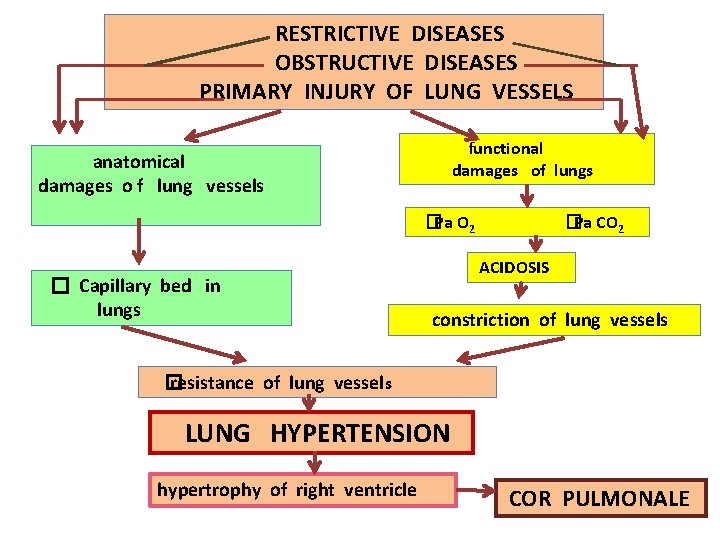
RESTRICTIVE DISEASES OBSTRUCTIVE DISEASES PRIMARY INJURY OF LUNG VESSELS functional damages of lungs anatomical damages o f lung vessels �Ра О 2 � Capillary bed in lungs �Ра СО 2 ACIDOSIS constriction of lung vessels � resistance of lung vessels LUNG HYPERTENSION hypertrophy of right ventricle COR PULMONALE
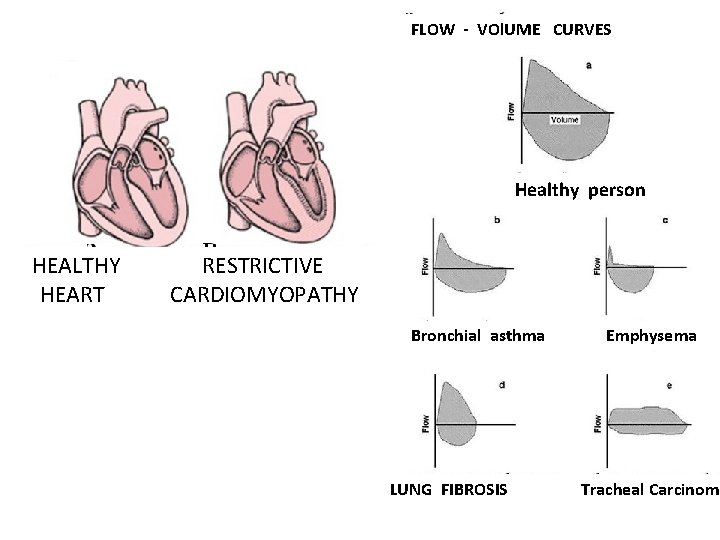
FLOW - VOl. UME CURVES Healthy person HEALTHY HEART RESTRICTIVE CARDIOMYOPATHY Bronchial asthma LUNG FIBROSIS Emphysema Tracheal Carcinoma
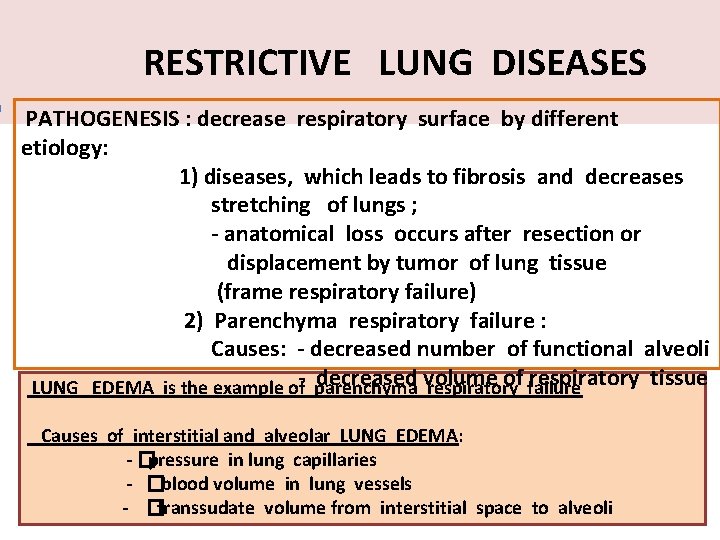
RESTRICTIVE LUNG DISEASES PATHOGENESIS : decrease respiratory surface by different etiology: 1) diseases, which leads to fibrosis and decreases stretching of lungs ; - anatomical loss occurs after resection or displacement by tumor of lung tissue (frame respiratory failure) 2) Parenchyma respiratory failure : Causes: - decreased number of functional alveoli decreased volume of failure respiratory tissue LUNG EDEMA is the example of- parenchyma respiratory Causes of interstitial and alveolar LUNG EDEMA: - �pressure in lung capillaries - �blood volume in lung vessels - �transsudate volume from interstitial space to alveoli
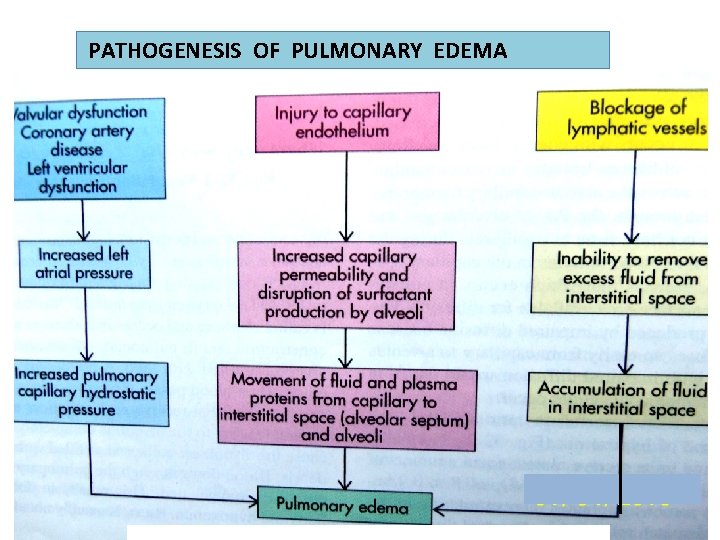
PATHOGENESIS OF PULMONARY EDEMA
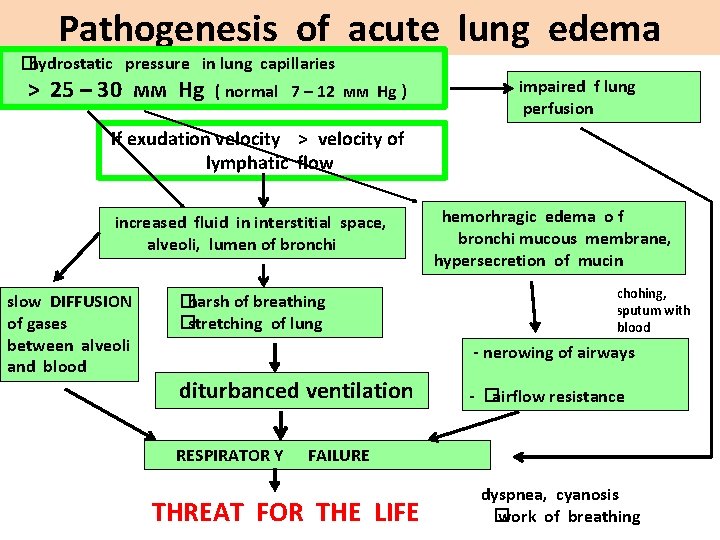
Pathogenesis of acute lung edema �hydrostatic pressure in lung capillaries > 25 – 30 мм Hg ( normal 7 – 12 мм Hg ) impaired f lung perfusion If exudation velocity > velocity of lymphatic flow increased fluid in interstitial space, alveoli, lumen of bronchi slow DIFFUSION of gases between alveoli and blood �harsh of breathing �stretching of lung hemorhragic edema o f bronchi mucous membrane, hypersecretion of mucin chohing, sputum with blood - nerowing of airways diturbanced ventilation RESPIRATOR Y - �airflow resistance FAILURE THREAT FOR THE LIFE dyspnea, cyanosis � work of breathing
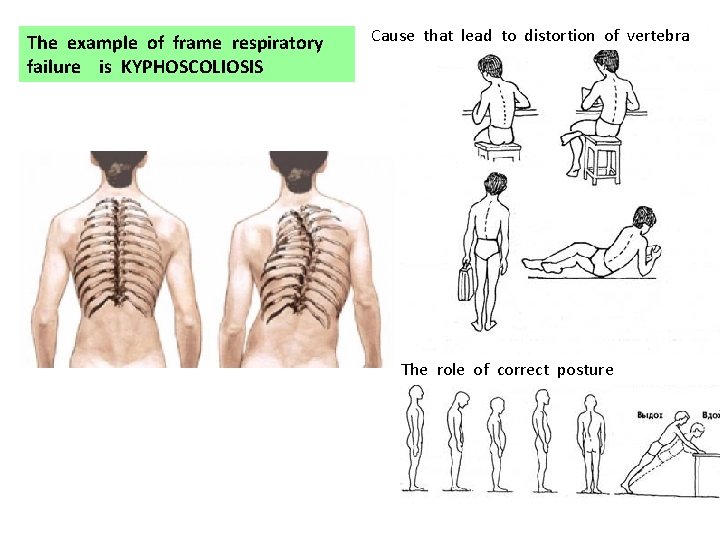
The example of frame respiratory failure is KYPHOSCOLIOSIS Cause that lead to distortion of vertebra The role of correct posture
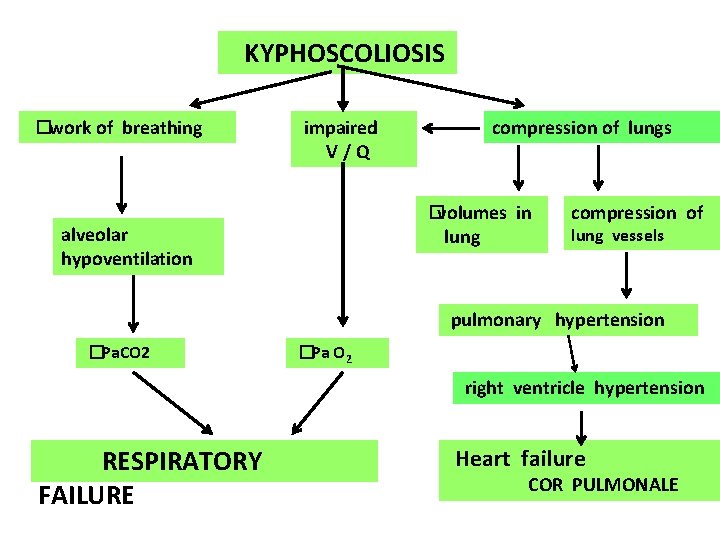
KYPHOSCOLIOSIS �work of breathing impaired V/Q compression of lungs �volumes in alveolar hypoventilation lung compression of lung vessels pulmonary hypertension �Ра. СО 2 �Ра О 2 right ventricle hypertension RESPIRATORY FAILURE Heart failure COR PULMONALE
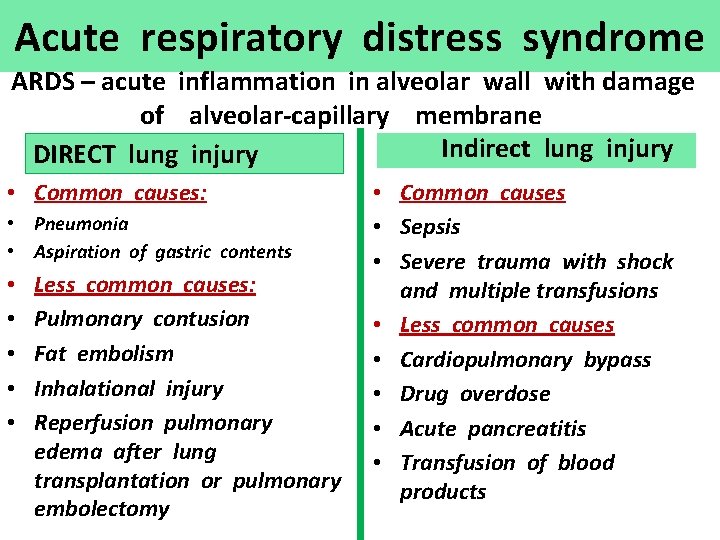
Acute respiratory distress syndrome ARDS – acute inflammation in alveolar wall with damage of alveolar-capillary membrane Indirect lung injury DIRECT lung injury • Common causes: • Pneumonia • Aspiration of gastric contents • • • Less common causes: Pulmonary contusion Fat embolism Inhalational injury Reperfusion pulmonary edema after lung transplantation or pulmonary embolectomy • Common causes • Sepsis • Severe trauma with shock and multiple transfusions • Less common causes • Cardiopulmonary bypass • Drug overdose • Acute pancreatitis • Transfusion of blood products

Acute respiratory distress syndrome (ARDS) Acute onset Cyanosis refractory to oxygen therapy Decreased lung compliance Diffuse infiltrates on chest radiograph Pulmonary – artery wedge pressure is > 13 mm Hg, but < 18 mm Hg Clinical manifestations: Rapid, shallow breathing, dyspnea, hyperventilation, respiratory - metabolic acidosis, Dyspnea, decreased compliance, increased work of breathing, hypoxemia Hypoxemia metabolic acidosis respiratory acidosis Hypotension decreased cardiac output death further hypoxemia
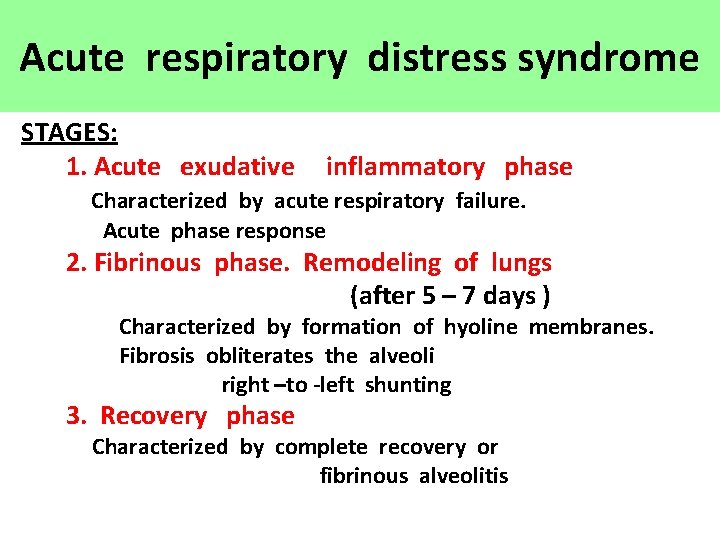
Acute respiratory distress syndrome STAGES: 1. Acute exudative inflammatory phase Characterized by acute respiratory failure. Acute phase response 2. Fibrinous phase. Remodeling of lungs (after 5 – 7 days ) Characterized by formation of hyoline membranes. Fibrosis obliterates the alveoli right –to -left shunting 3. Recovery phase Characterized by complete recovery or fibrinous alveolitis
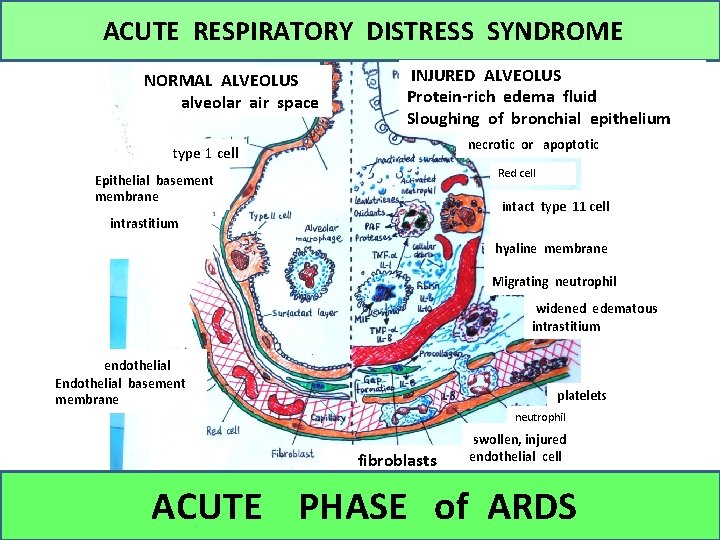
ACUTE RESPIRATORY DISTRESS SYNDROME NORMAL ALVEOLUS alveolar air space INJURED ALVEOLUS Protein-rich edema fluid Sloughing of bronchial epithelium necrotic or apoptotic type 1 cell Red cell Epithelial basement membrane intact type 11 cell intrastitium hyaline membrane Migrating neutrophil widened edematous intrastitium endothelial Endothelial basement membrane platelets neutrophil fibroblasts swollen, injured endothelial cell ACUTE PHASE of ARDS
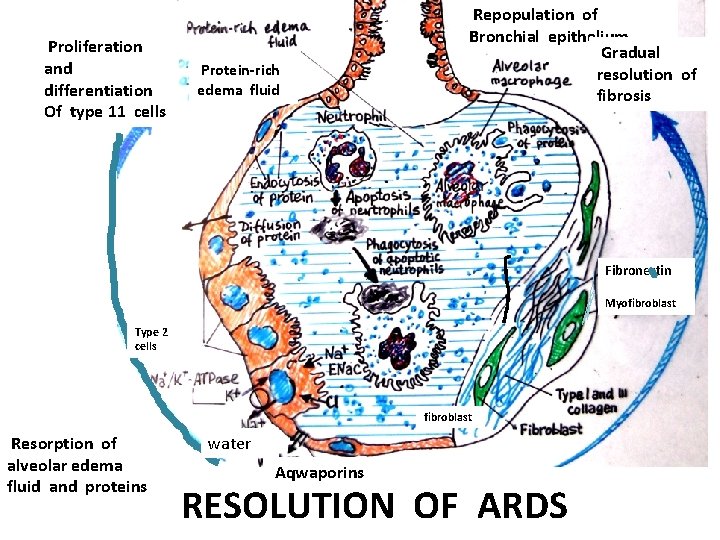
Proliferation and differentiation Of type 11 cells Protein-rich edema fluid Repopulation of Bronchial epithelium Gradual resolution of fibrosis Fibronectin Myofibroblast Type 2 cells fibroblast Resorption of alveolar edema fluid and proteins water Aqwaporins RESOLUTION OF ARDS
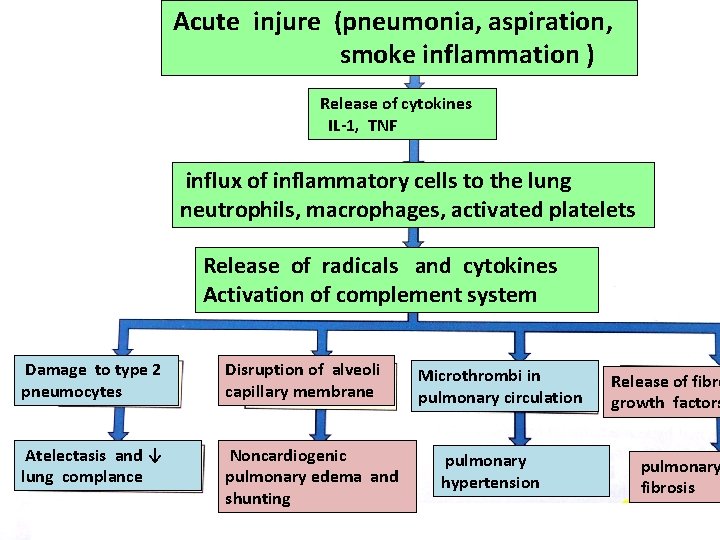
Acute injure (pneumonia, aspiration, smoke inflammation ) Release of cytokines IL-1, TNF influx of inflammatory cells to the lung neutrophils, macrophages, activated platelets Release of radicals and cytokines Activation of complement system Damage to type 2 pneumocytes Disruption of alveoli capillary membrane Atelectasis and ↓ lung complance Noncardiogenic pulmonary edema and shunting Microthrombi in pulmonary circulation pulmonary hypertension Release of fibro growth factors pulmonary fibrosis
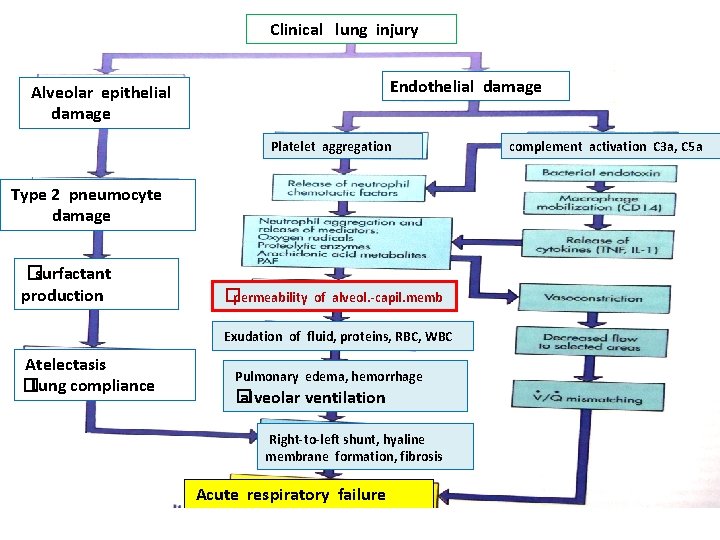
Clinical lung injury Endothelial damage Alveolar epithelial damage Platelet aggregation Type 2 pneumocyte damage �surfactant production �permeability of alveol. -capil. memb Exudation of fluid, proteins, RBC, WBC Atelectasis �Lung compliance Pulmonary edema, hemorrhage � alveolar ventilation Right-to-left shunt, hyaline membrane formation, fibrosis Acute respiratory failure complement activation C 3 a, C 5 a
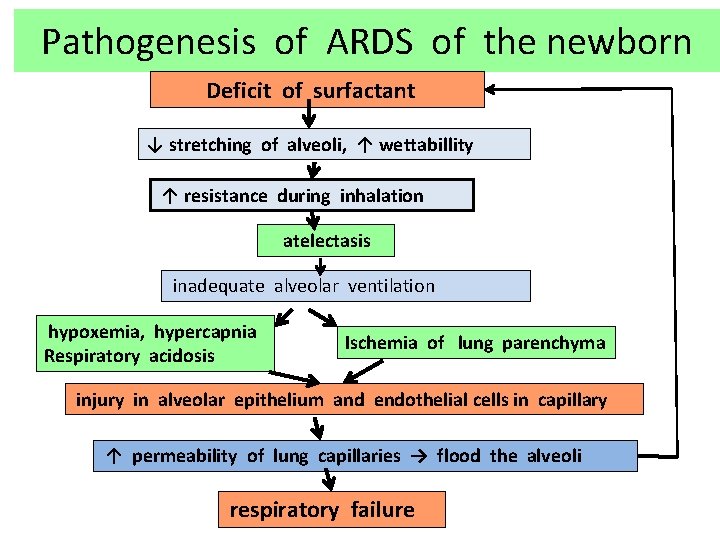
Pathogenesis of ARDS of the newborn Deficit of surfactant ↓ stretching of alveoli, ↑ wettabillity ↑ resistance during inhalation atelectasis inadequate alveolar ventilation hypoxemia, hypercapnia Respiratory acidosis Ischemia of lung parenchyma injury in alveolar epithelium and endothelial cells in capillary ↑ permeability of lung capillaries → flood the alveoli respiratory failure
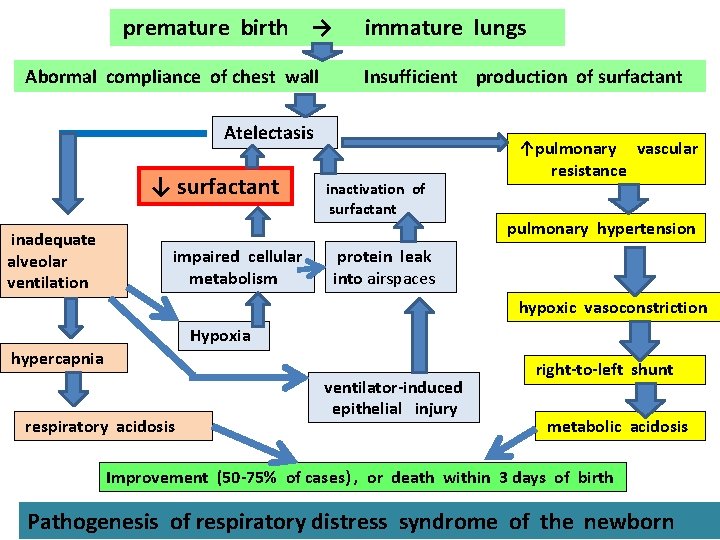
premature birth → Abormal compliance of chest wall immature lungs Insufficient production of surfactant Atelectasis ↓ surfactant inadequate alveolar ventilation impaired cellular metabolism inactivation of surfactant ↑pulmonary vascular resistance pulmonary hypertension protein leak into airspaces hypoxic vasoconstriction Hypoxia hypercapnia respiratory acidosis ventilator-induced epithelial injury right-to-left shunt metabolic acidosis Improvement (50 -75% of cases) , or death within 3 days of birth Pathogenesis of respiratory distress syndrome of the newborn
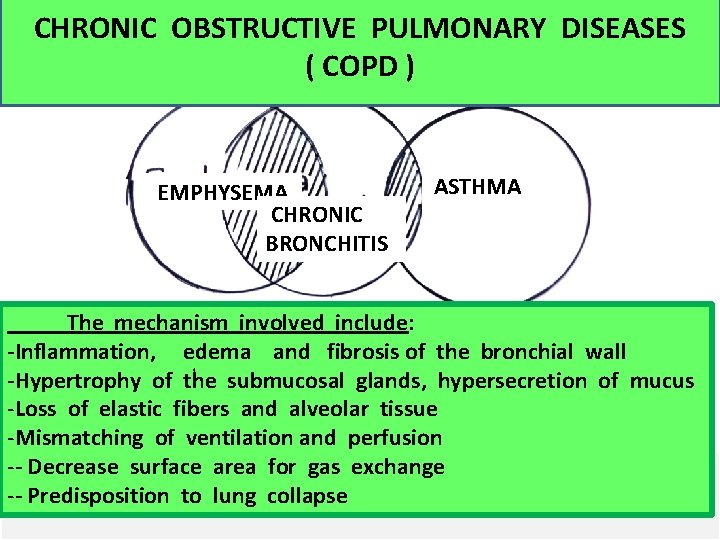
CHRONIC OBSTRUCTIVE PULMONARY DISEASES ( COPD ) EMPHYSEMA CHRONIC BRONCHITIS ASTHMA The mechanism involved include: -Inflammation, edema and fibrosis of the bronchial wall -Hypertrophy of the submucosal glands, hypersecretion of mucus -Loss of elastic fibers and alveolar tissue -Mismatching of ventilation and perfusion -- Decrease surface area for gas exchange -- Predisposition to lung collapse
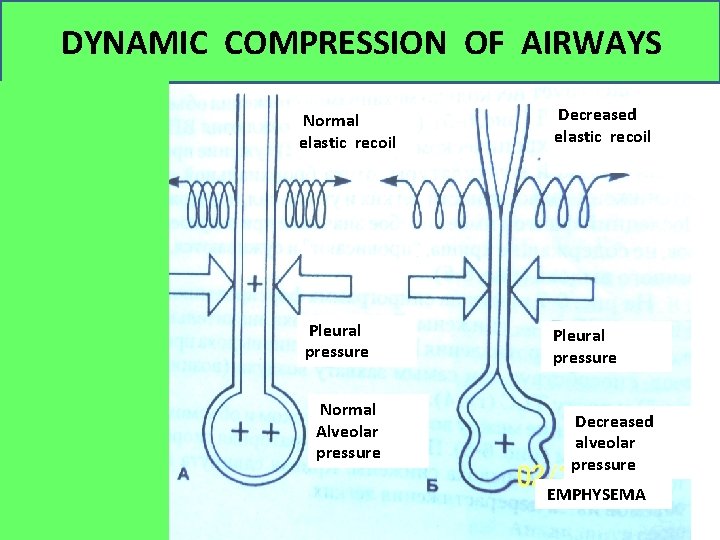
DYNAMIC COMPRESSION OF AIRWAYS Normal elastic recoil Pleural pressure Normal Alveolar pressure Decreased elastic recoil Pleural pressure Decreased alveolar pressure EMPHYSEMA
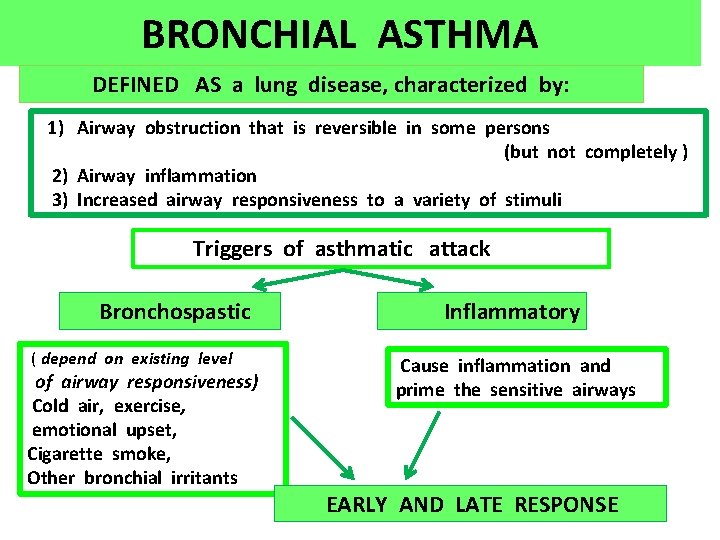
BRONCHIAL ASTHMA DEFINED AS a lung disease, characterized by: 1) Airway obstruction that is reversible in some persons (but not completely ) 2) Airway inflammation 3) Increased airway responsiveness to a variety of stimuli Triggers of asthmatic attack Bronchospastic ( depend on existing level of airway responsiveness) Cold air, exercise, emotional upset, Cigarette smoke, Other bronchial irritants Inflammatory Cause inflammation and prime the sensitive airways EARLY AND LATE RESPONSE
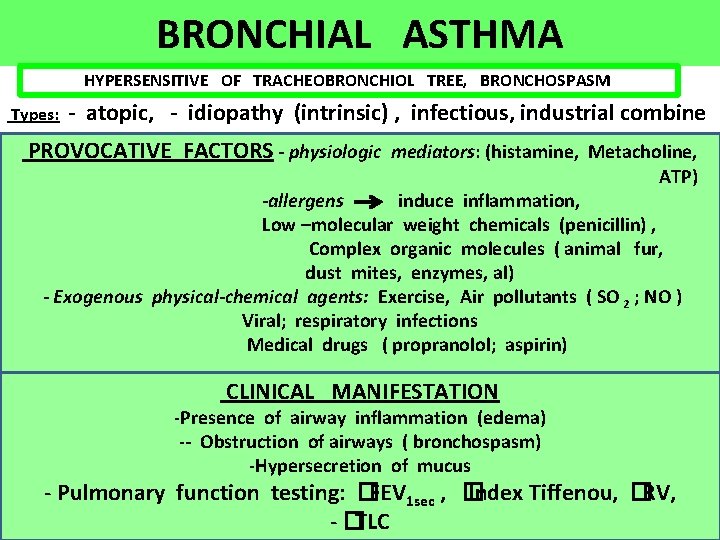
BRONCHIAL ASTHMA HYPERSENSITIVE OF TRACHEOBRONCHIOL TREE, BRONCHOSPASM Types: - atopic, - idiopathy (intrinsic) , infectious, industrial combine PROVOCATIVE FACTORS - physiologic mediators: (histamine, Metacholine, ATP) -allergens induce inflammation, Low –molecular weight chemicals (penicillin) , Complex organic molecules ( animal fur, dust mites, enzymes, al) - Exogenous physical-chemical agents: Exercise, Air pollutants ( SO 2 ; NO ) Viral; respiratory infections Medical drugs ( propranolol; aspirin) CLINICAL MANIFESTATION , -Presence of airway inflammation (edema) -- Obstruction of airways ( bronchospasm) -Hypersecretion of mucus - Pulmonary function testing: �FEV 1 sec , � Index Tiffenou, �RV, - �TLC
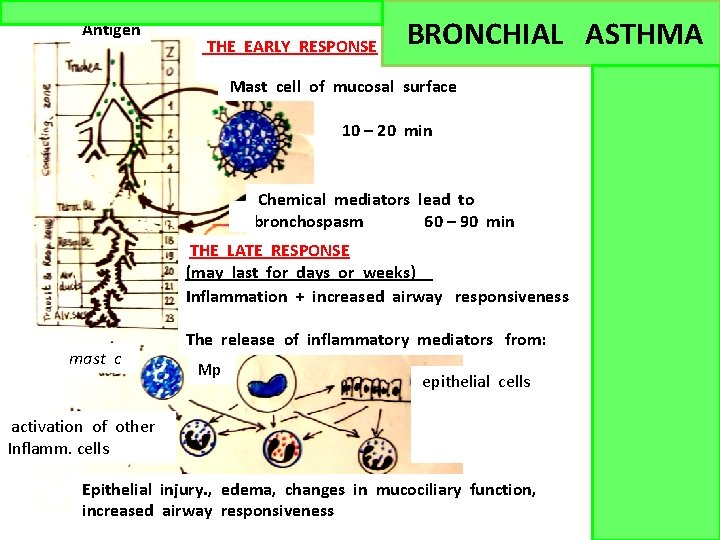
Antigen THE EARLY RESPONSE BRONCHIAL ASTHMA Mast cell of mucosal surface 10 – 20 min Chemical mediators lead to bronchospasm 60 – 90 min THE LATE RESPONSE (may last for days or weeks) Inflammation + increased airway responsiveness mast c The release of inflammatory mediators from: Mp epithelial cells activation of other Inflamm. cells Epithelial injury. , edema, changes in mucociliary function, increased airway responsiveness
ASTh. MATI Responses A - acute B - Late
- Slides: 23