PATHOPHYSIOLOGY OF NERVOUS SYSTEM DISEASES Mehtap KAAR KOAK





- Slides: 154
PATHOPHYSIOLOGY OF NERVOUS SYSTEM DISEASES Mehtap KAÇAR KOÇAK MD Ph. D Yeditepe University Medicine School 1
OVERWIEV l l l l l 1 - Alterations in Cognitive Networks 2 - Seizures and Epilepsy 3 - Cerebrovascular Diseases (Ischemic stroke) 4 - Dementias (Alzheimer’s Disease) 5 - Movement Disorders (Parkinson’s Disease) 6 - Motor Neuron Diseases (ALS) 7 - Demyelinating Diseases (Multiple Sclerosis) 8 - Neuromuscular Junction Diseases (Myasthenia Gravis) 9 - Meningitis (Acute Bacterial Meningitis) 10 - Stress 2
Alterations in Cognitive Networks l Full consciousness: awareness of self and the environment l. Arousal: state of awakeness l. Mediated by the reticular activating system l. Content of Thought: all cognitive functions l. Awareness of self, environment and affective states (moods) 3
Alterations in Arousal l Causes: l. Structural l. Divided by location above or below tentorial plate l. Metabolic l. Psychogenic 4
Alterations in Arousal l Pathological processes l. Infectious, vascular, neoplastic, traumatic, congenital, degenerative, polygenic l. Metabolic l. Hypoxia, electrolyte disturbances, hypoglycemia, drugs and toxins 5
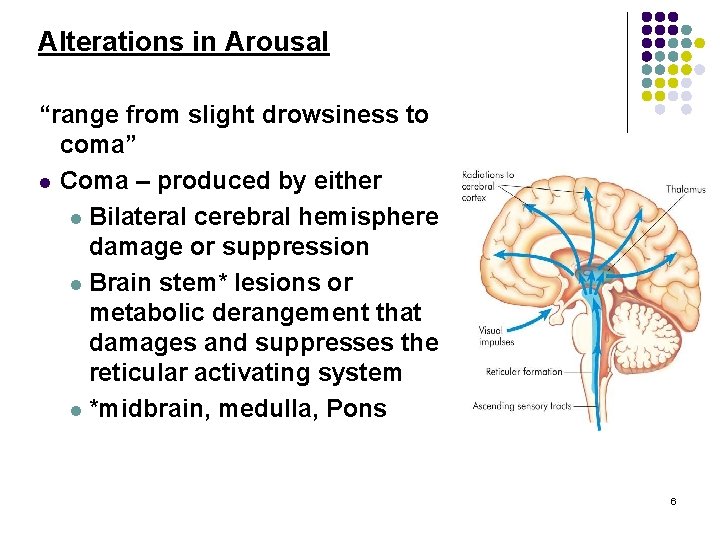
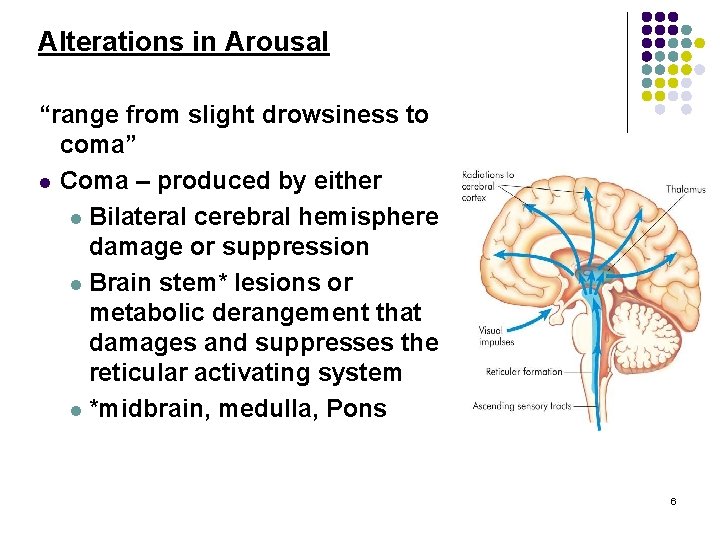
Alterations in Arousal “range from slight drowsiness to coma” l Coma – produced by either l Bilateral cerebral hemisphere damage or suppression l Brain stem* lesions or metabolic derangement that damages and suppresses the reticular activating system l *midbrain, medulla, Pons 6
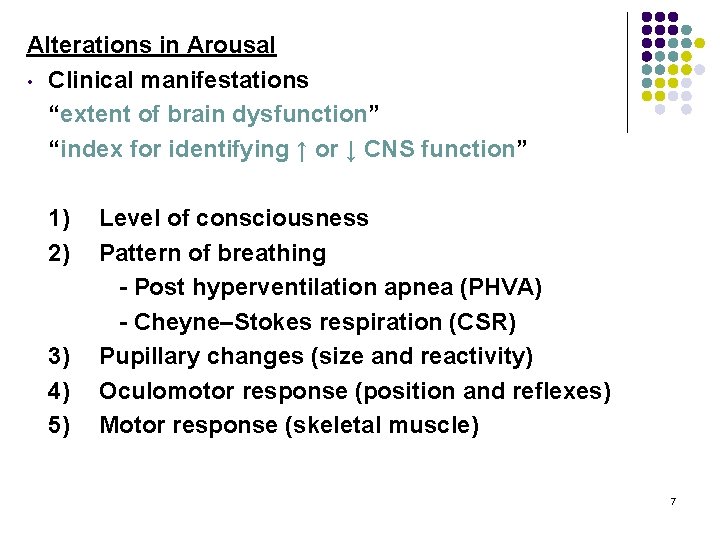
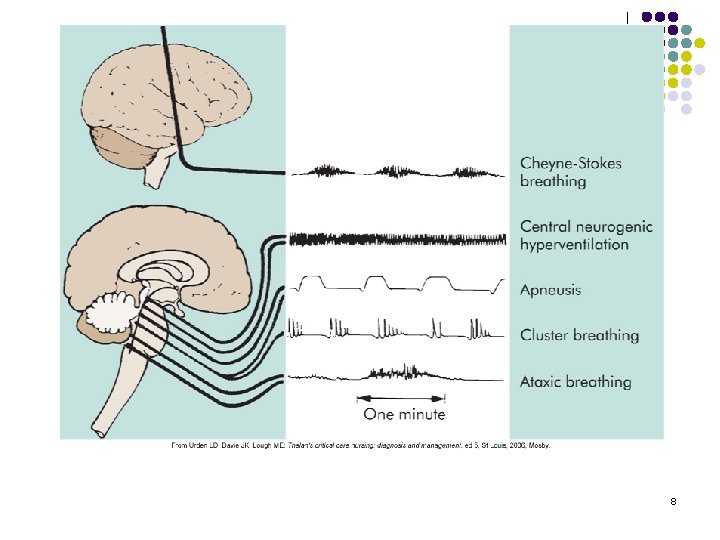
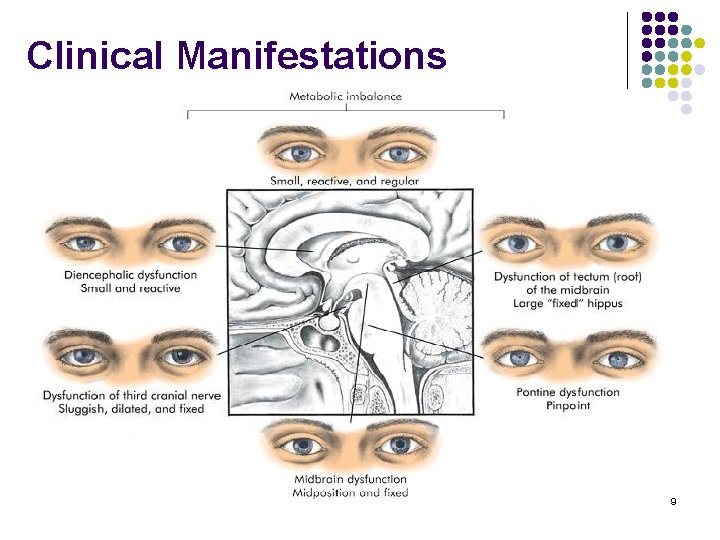
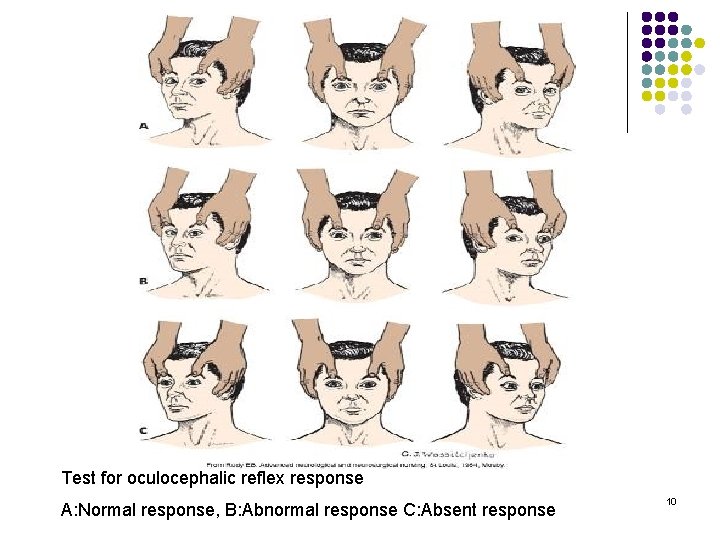
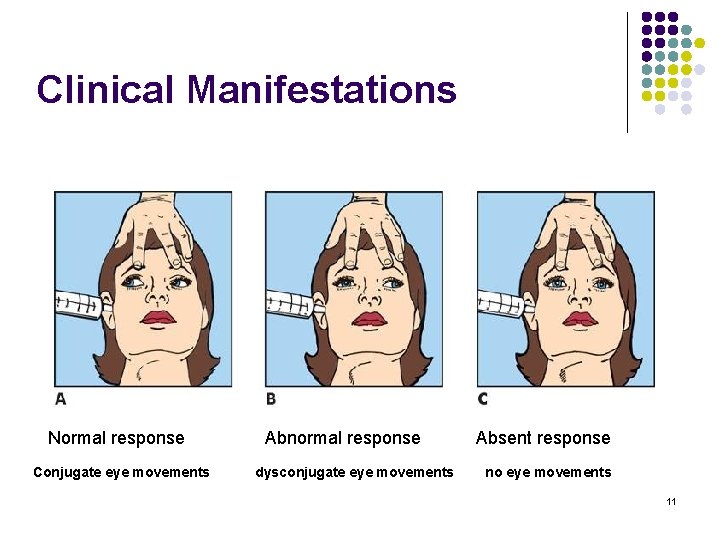
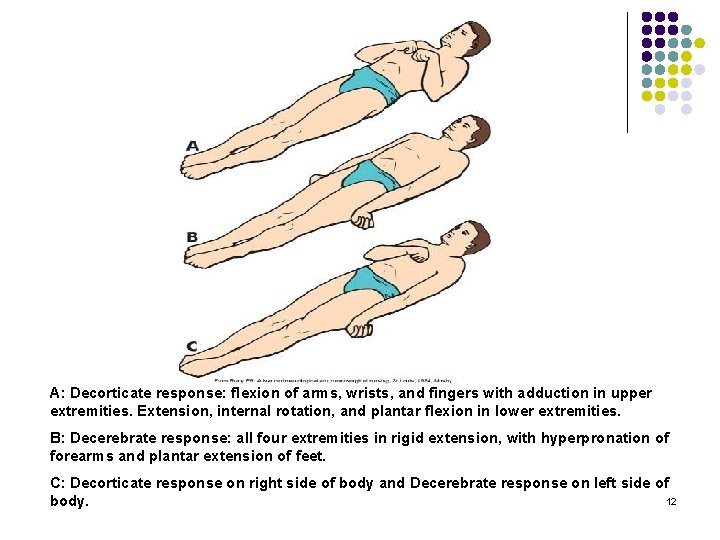
Alterations in Arousal • Clinical manifestations “extent of brain dysfunction” “index for identifying ↑ or ↓ CNS function” 1) 2) 3) 4) 5) Level of consciousness Pattern of breathing - Post hyperventilation apnea (PHVA) - Cheyne–Stokes respiration (CSR) Pupillary changes (size and reactivity) Oculomotor response (position and reflexes) Motor response (skeletal muscle) 7
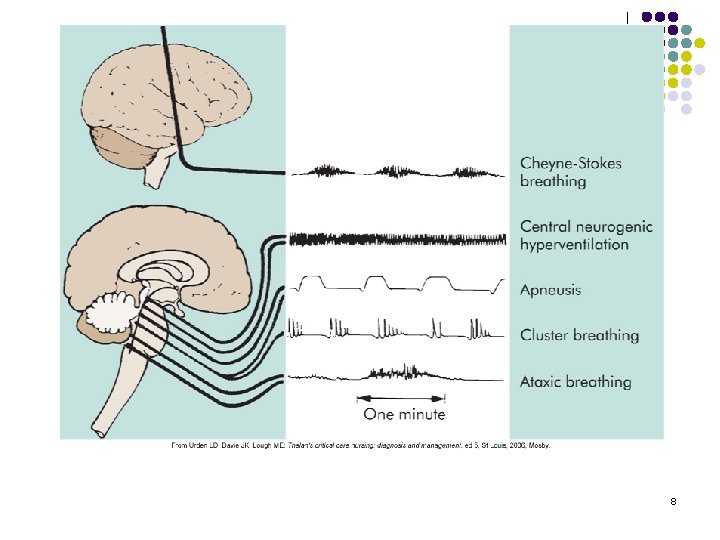
8
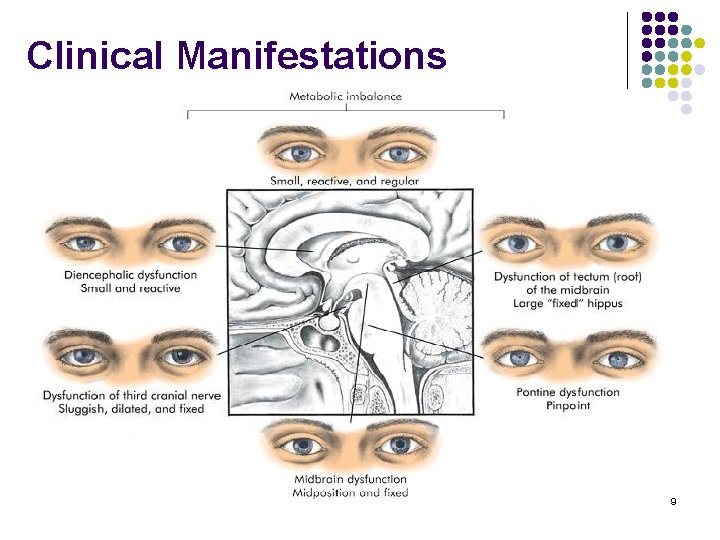
Clinical Manifestations 9
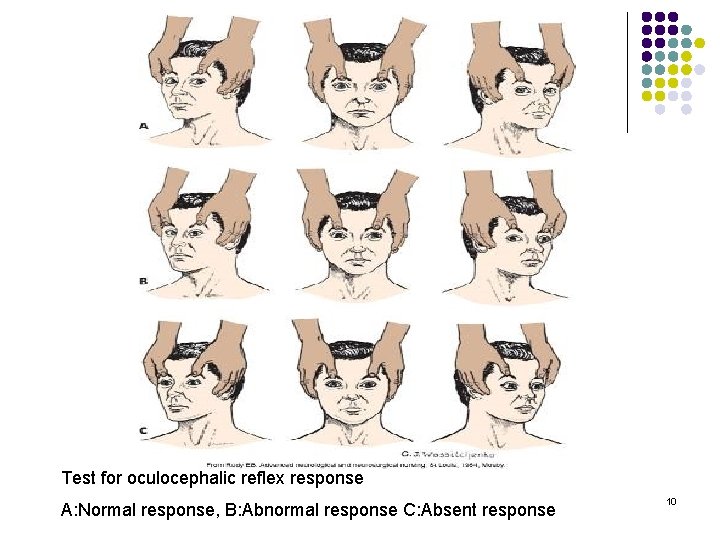
Test for oculocephalic reflex response A: Normal response, B: Abnormal response C: Absent response 10
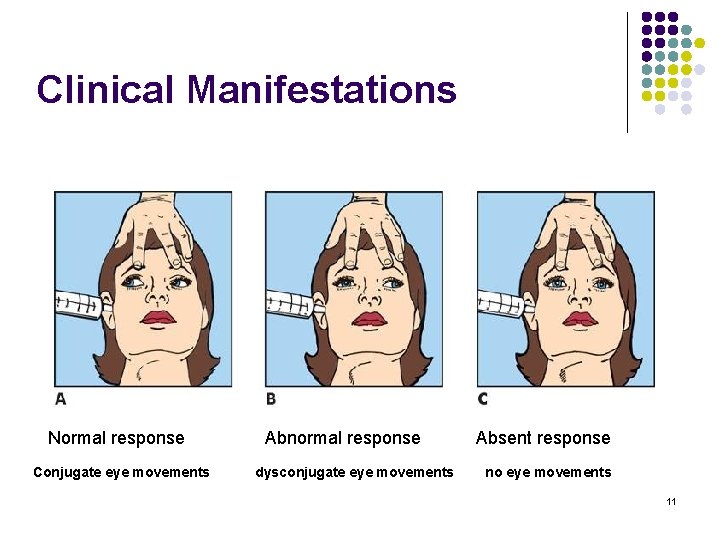
Clinical Manifestations Normal response Conjugate eye movements Abnormal response dysconjugate eye movements Absent response no eye movements 11
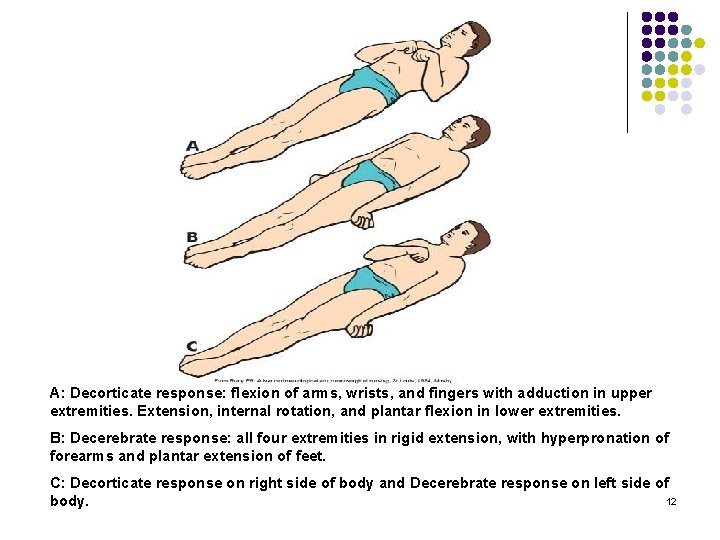
A: Decorticate response: flexion of arms, wrists, and fingers with adduction in upper extremities. Extension, internal rotation, and plantar flexion in lower extremities. B: Decerebrate response: all four extremities in rigid extension, with hyperpronation of forearms and plantar extension of feet. C: Decorticate response on right side of body and Decerebrate response on left side of 12 body.
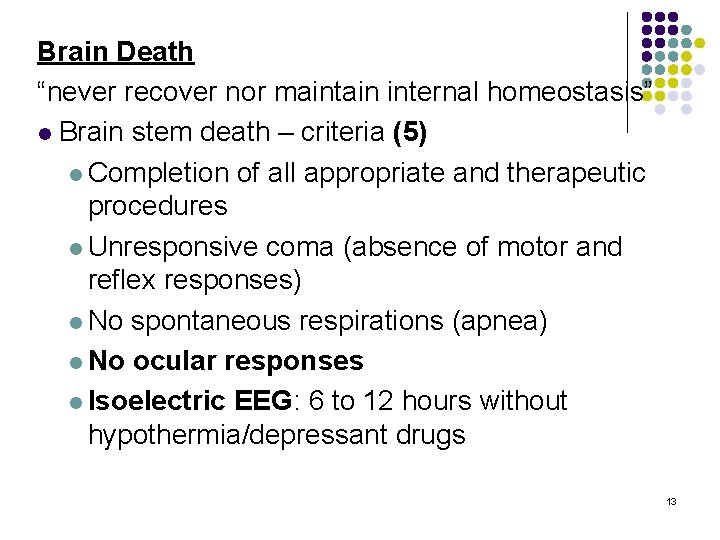
Brain Death “never recover nor maintain internal homeostasis” l Brain stem death – criteria (5) l Completion of all appropriate and therapeutic procedures l Unresponsive coma (absence of motor and reflex responses) l No spontaneous respirations (apnea) l No ocular responses l Isoelectric EEG: 6 to 12 hours without hypothermia/depressant drugs 13
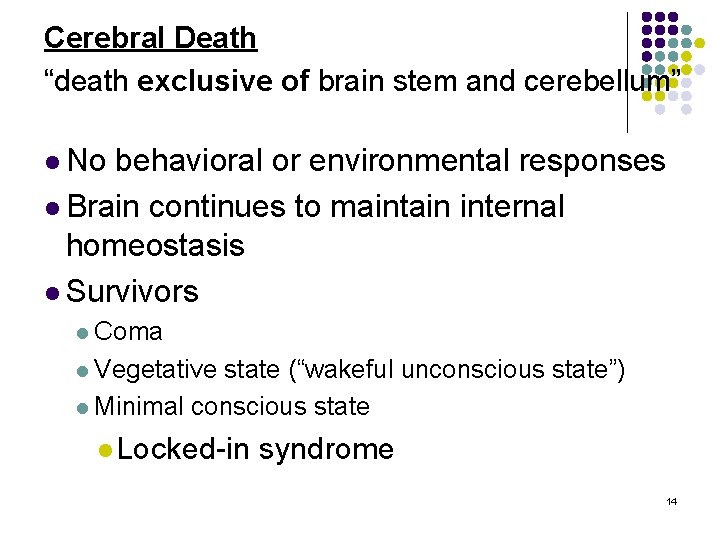
Cerebral Death “death exclusive of brain stem and cerebellum” l No behavioral or environmental responses l Brain continues to maintain internal homeostasis l Survivors l Coma l Vegetative state (“wakeful unconscious state”) l Minimal conscious state l Locked-in syndrome 14
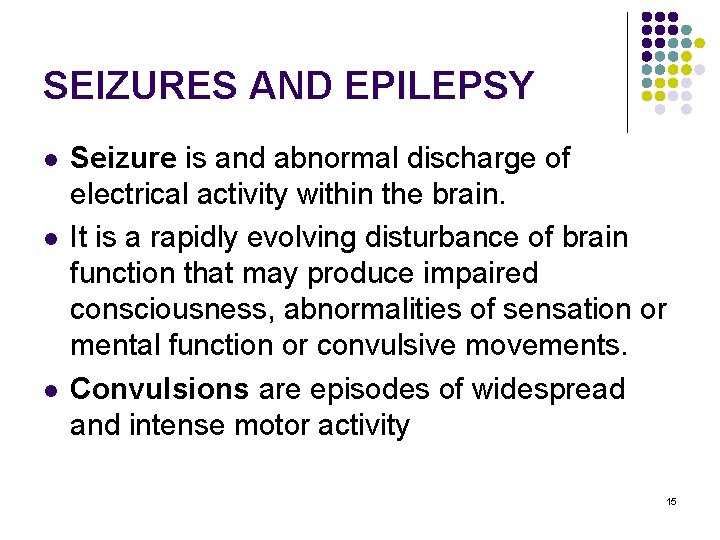
SEIZURES AND EPILEPSY l l l Seizure is and abnormal discharge of electrical activity within the brain. It is a rapidly evolving disturbance of brain function that may produce impaired consciousness, abnormalities of sensation or mental function or convulsive movements. Convulsions are episodes of widespread and intense motor activity 15
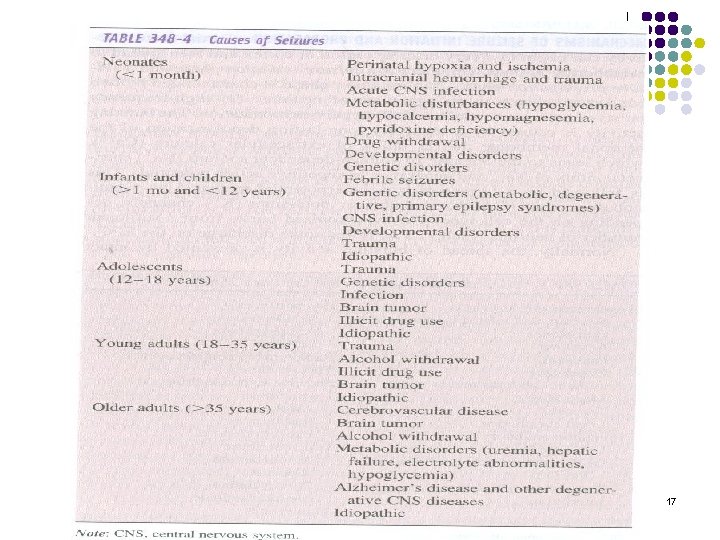
l l Epilepsy, a recurrent disorder of cerebral function marked by sudden, brief attacks of altered consciousness, motor activity or sensory phenomenon. Convulsive seizures are the most common form. Using the definition of epilepsy as two or more unprovoked seizures the incidence of epilepsy is 0. 3 to 0. 5 % in different populations throughout the world. Incidence increases with age, with 30% initially occurring before 4 years and 75 -80 % before 20 years. 16
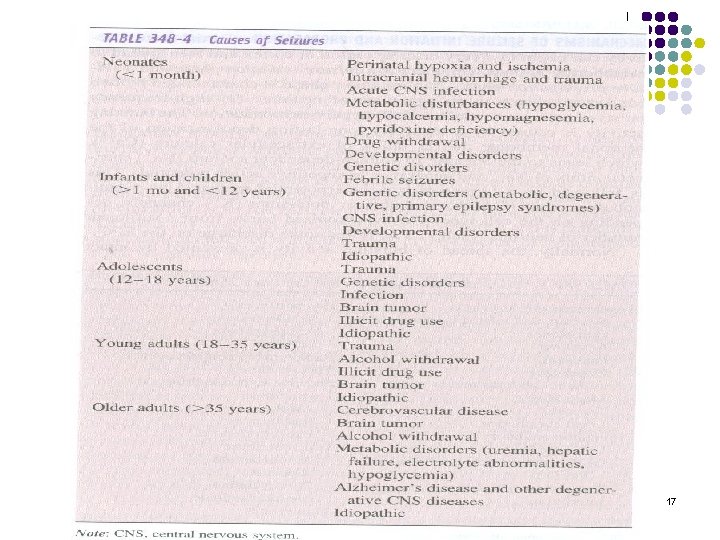
17
l l great majority of cases are idiopathic. Signs and symptoms vary: petit mal – almost imperceptible alterations in consciousness grand mal – generalized tonic-clonic seizures – dramatic loss of consciousness, falling, generalized tonic-clonic convulsions of all extremities, incontinence, and amnesia for the event. 18
Epileptogenic focus l l Group of brain neurons susceptible to activation. Plasma membranes may be more permeable to ion movement. Firing of these neurons may be greater in frequency and amplitude. Electrical activity can spread to other hemisphere and then to the spinal cord. 19
Eliciting stimuli: l l l Hypoglycemia Fatigue Emotional or physical stress Fever Hyperventilation Environmental stimuli 20
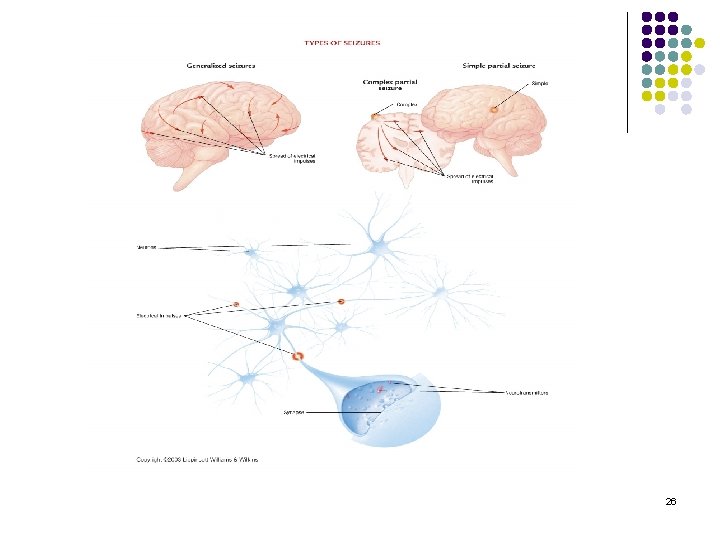
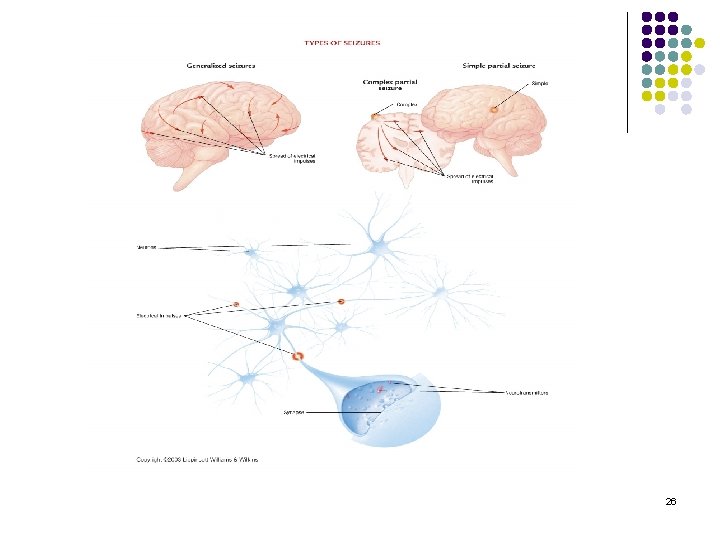
MECHANISM OF SEIZURE INITIATION AND PROPAGATION l l l Partial seizure activity can begin in avery discrete region of cortex and then spread to neighboring regions; i. e. There are two phases: 1 - the seizure initiation phase 2 - the seizure propagation phase. The seizure initiation phase is characterized by two concurrent events in an aggregate of neurons: 1 - high-frequency burst of action potentials, 2 - hypersynchronization. 21
l The bursting activity is caused by a relatively long-lasting depolarization of the neuronal membrane due to influx of extracellular calcium. l The influx of extracellular calcium leads to 1 - the opening of voltage-dependent sodium channels, 2 - influx of sodium, 3 - Generation of repetetive action potentials. l l This is followed by a hyperpolarizing afterpotential mediated by GABA receptors or potassium channels, depending on the cell type. 22
l l Repetitive discharges leads to the following: 1 - an increase in extracellular potassium which blunts hyperpolarization and depolarizes neighboring neurons, 2 - accumulation of calcium in presynaptic terminals, leading to enhanced neurotransmitter release, 3 - depolarization-induced activation of the Nmethyl-D-aspartate (NMDA) subtype of the excitatory aminoacid receptor, which causes calcium influx and neuronal activation. 23
l l The recruitment of a sufficient number of neurons leads to: a loss of the surrounding inhibition and propagation of seizure activity into contiguous areas via local cortical connections, and to more distant areas via long commissural pathways such as corpus callosum. 24
Seizures l Partial (focal/local) l. Simple, complex, secondary, generalized l Generalized (bilateral/symmetric) l Unclassified 25
26
CEREBROVASCULAR DISEASES l l Most frequent of all neurological problems Due to blood vessel pathology: l l Lesions on walls of vessels leading to brain Occlusions of vessel lumen by thrombus or embolus Vessel rupture Alterations of blood quality CV disease leads to two types of brain abnormalities : l l Ischemia (with or without infarct) Hemorrhage 27
Cerebrovascular Accident (Stroke) l Clinical expression of cerebrovascular disease: a sudden, nonconvulsive focal neurological deficit l Incidence: l third leading cause of death in U. S. – half a million people a year – one third will die from it Highest risk > 65 years of age But about 1/3 (28%) are < 65 years old Tends to run in families More often seen in females l l 28
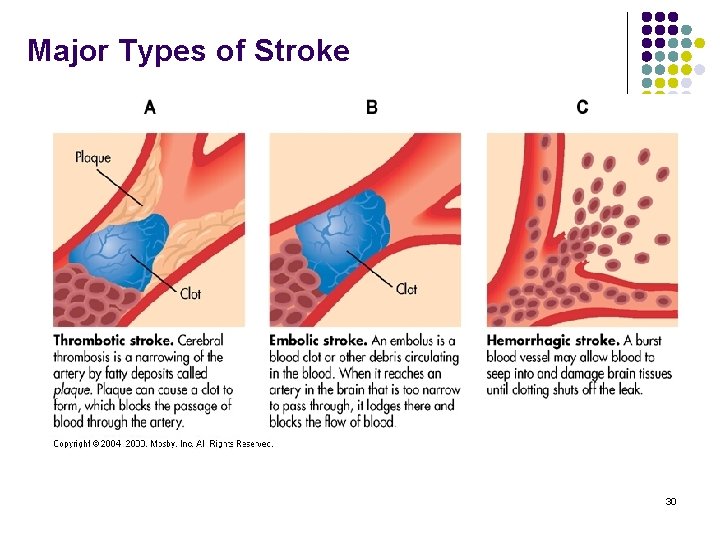
Stroke l Classification based on underlying pathophysiologic findings; l 1 - Oclussive stroke (Ischemia – thrombotic and embolic) 2 - Hemorrhagic stroke l l 29
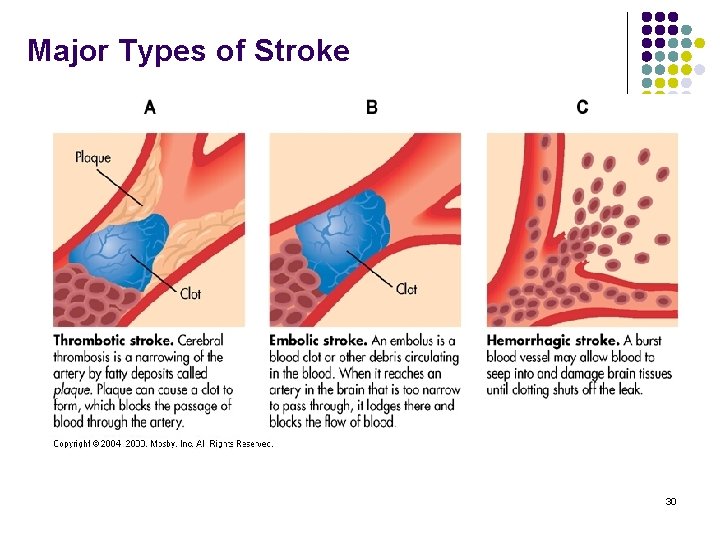
Major Types of Stroke 30
Risk Factors l l Arterial hypertension Heart disease l l l l Myocardial infarction or endocarditis Atrial fibrillation Elevated plasma cholesterol Diabetes mellitus Oral contraceptives Smoking Polycythemia and thrombocythemia 31
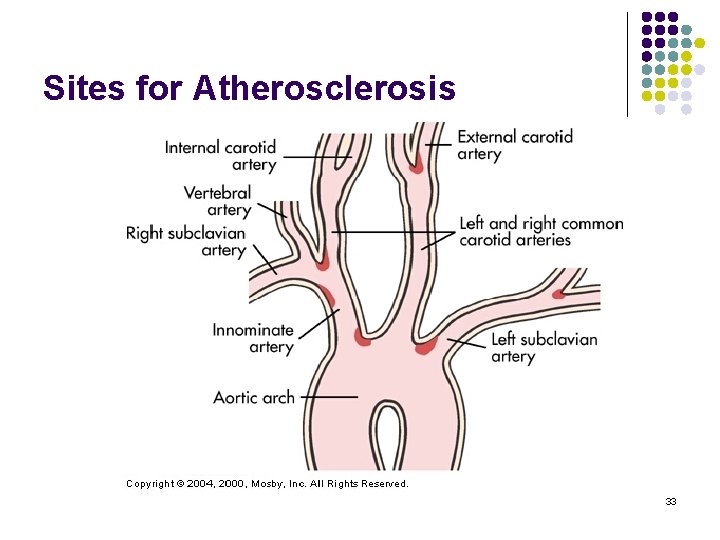
Occlusive strokes l l Occurs with blockage of blood vessel by a thrombus or embolus Atherosclerosis is a major cause of stroke l l Can lead to thrombus formation and contribute to emboli May be temporary or permanent Thrombotic stroke: 3 clinical types: l TIAs l Stroke-in-evolution l Completed stroke 32
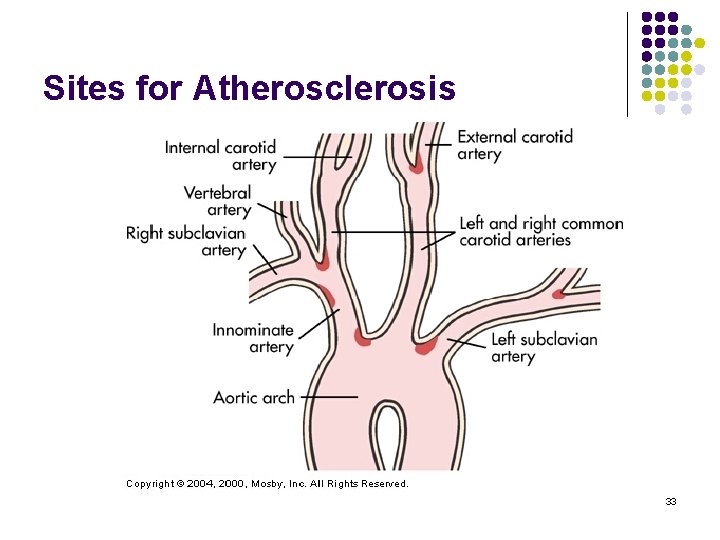
Sites for Atherosclerosis 33
Transient Ischemic Attacks l l l Last for only a few minutes, always less than 24 hours All neurological deficits resolve Symptom of developing thrombosis 34
Causes of TIA: l Thrombus formation l l l Atherosclerosis Arteritis Hypertension Vasospasm Other: l l l Hypotension Anemia Polycythemia 35
Symptoms depend on location l l Ophthalmic branch of internal carotid artery – amaurosis fugax – fleeting blindness Anterior or middle cerebral arteries – contralateral monoparesis, hemiparesis, localized, tingling numbness in one arm, loss of right or left visual field or aphasia 36
Stroke-in-evolution l l Can have abrupt onset, but develop in a stepby-step fashion over minutes to hours, occasionally, from days to weeks Characteristic of thrombotic stroke or slow hemorrhage 37

Thrombotic Stroke l l l Involves permanent damage to brain due to ischemia, hypoxia and necrosis of neurons Most common form of CVA Causes: l l l Atherosclerosis associated with hypertension Diabetes mellitus, and vascular disease Trauma 38
l l l May take years to develop, often asymptomatic until major narrowing of arterial lumen Anything that lowers systemic B. P. will exacerbate symptoms (60 % during sleep) Area affected depends on artery and presence of anastomoses Area affected initially is greater than damage due to edema Infarcted tissue undergoes liquifaction necrosis 39
Embolic stroke l l l l l Second most common CVA Fragments that break from a thrombus outside the brain, or occasionally air, fat, clumps of bacteria, or tumors Impact is the same for thrombotic stroke Rapid onset of symptoms Often have a second stroke Common causes: Atrial fibrillation Myocardial infarction Endocarditis Rheumatic heart disease and other defects 40
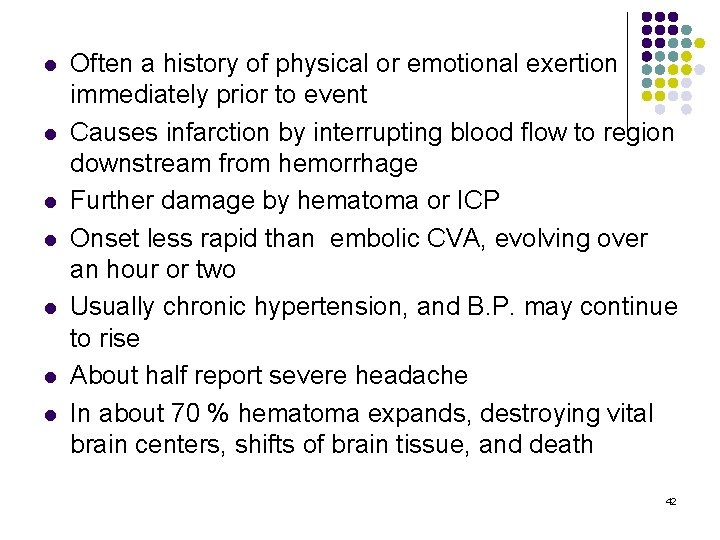
Hemorrhagic Stroke l Third most common, but most lethal Bleeding into cerebrum or subarachnoid space l Common causes: l Ruptured aneurysms Vascular malformations Hypertension Bleeding into tumors Bleeding disorders Head trauma l l l 41
l l l l Often a history of physical or emotional exertion immediately prior to event Causes infarction by interrupting blood flow to region downstream from hemorrhage Further damage by hematoma or ICP Onset less rapid than embolic CVA, evolving over an hour or two Usually chronic hypertension, and B. P. may continue to rise About half report severe headache In about 70 % hematoma expands, destroying vital brain centers, shifts of brain tissue, and death 42
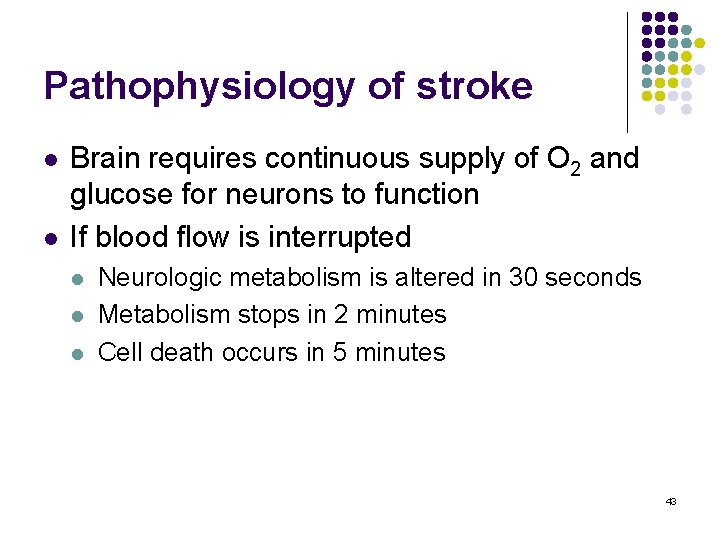
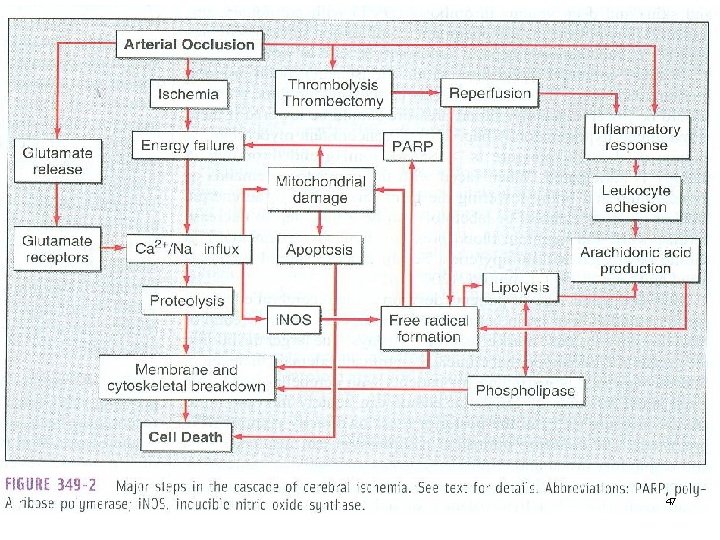
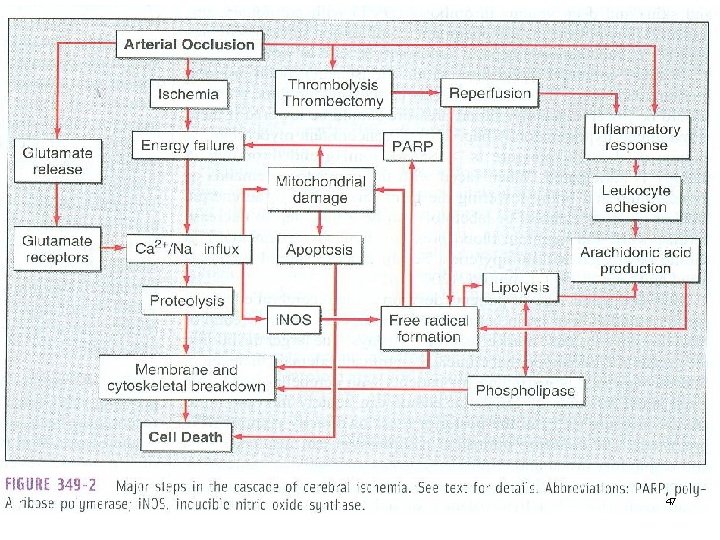
Pathophysiology of stroke l l Brain requires continuous supply of O 2 and glucose for neurons to function If blood flow is interrupted l l l Neurologic metabolism is altered in 30 seconds Metabolism stops in 2 minutes Cell death occurs in 5 minutes 43
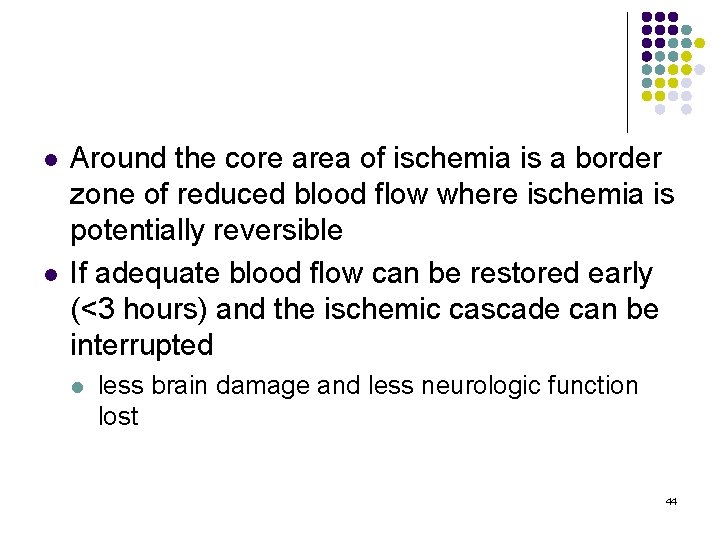
l l Around the core area of ischemia is a border zone of reduced blood flow where ischemia is potentially reversible If adequate blood flow can be restored early (<3 hours) and the ischemic cascade can be interrupted l less brain damage and less neurologic function lost 44
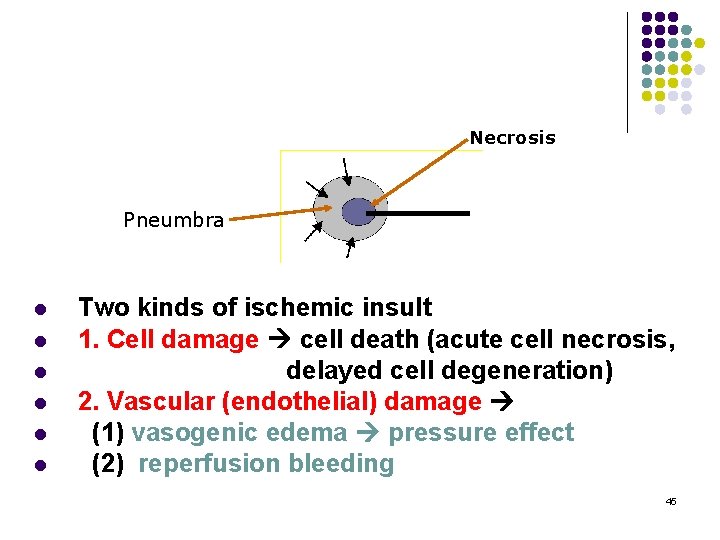
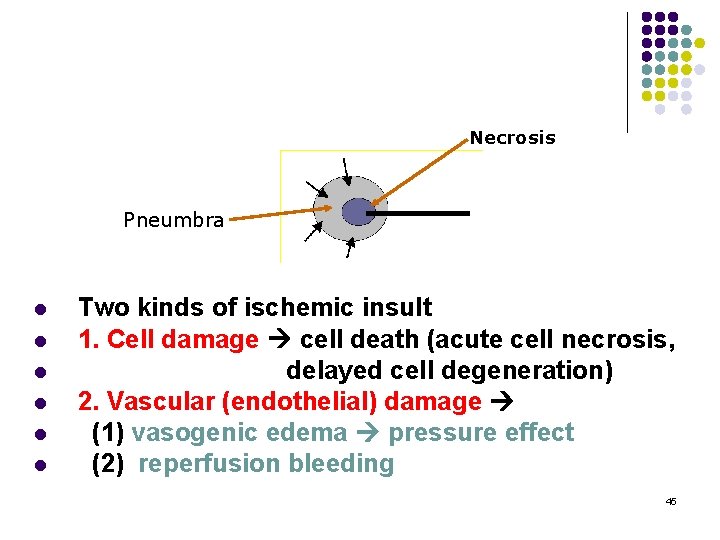
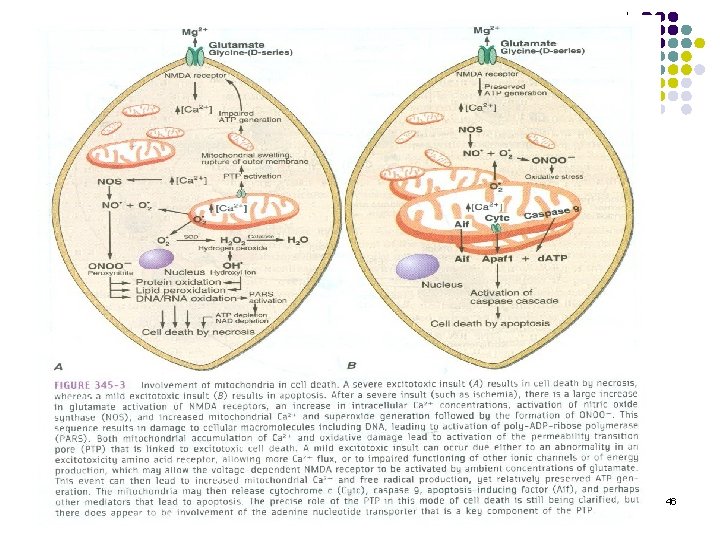
Necrosis Pneumbra l l l Two kinds of ischemic insult 1. Cell damage cell death (acute cell necrosis, delayed cell degeneration) 2. Vascular (endothelial) damage (1) vasogenic edema pressure effect (2) reperfusion bleeding 45
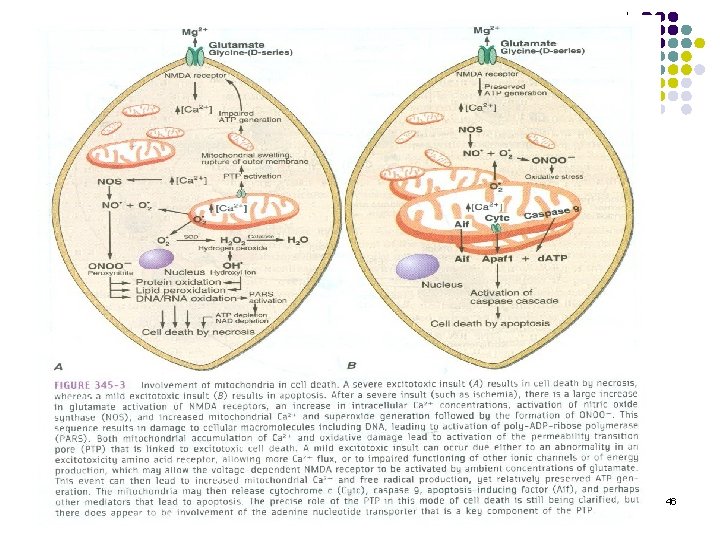
46
47
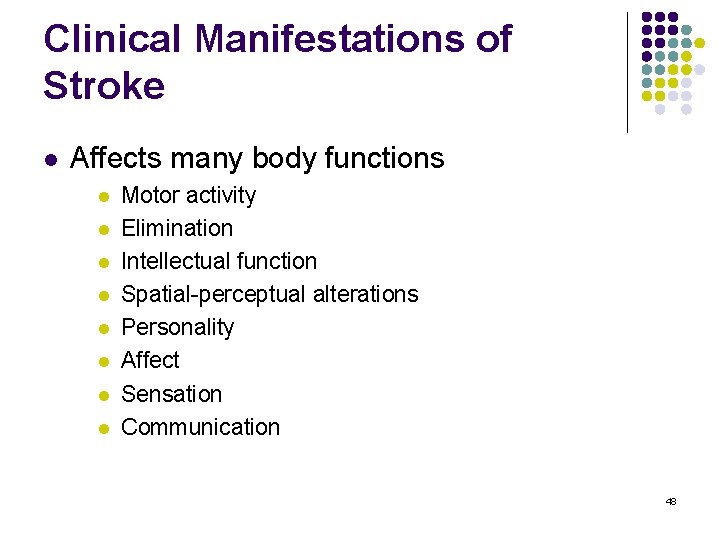
Clinical Manifestations of Stroke l Affects many body functions l l l l Motor activity Elimination Intellectual function Spatial-perceptual alterations Personality Affect Sensation Communication 48
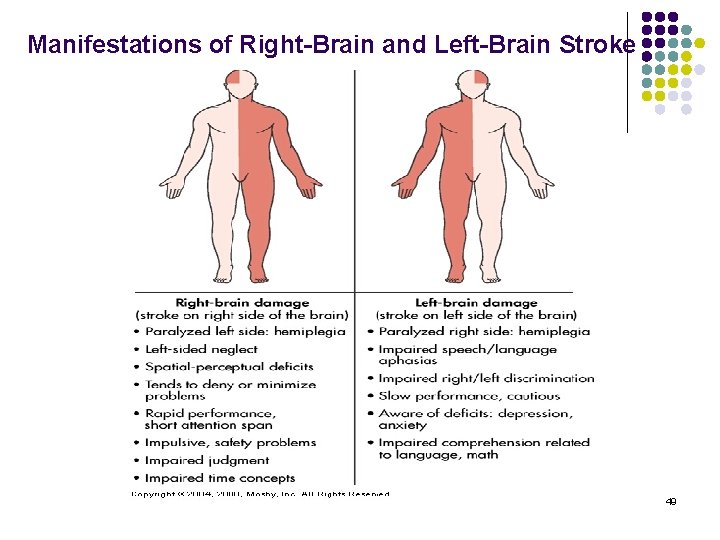
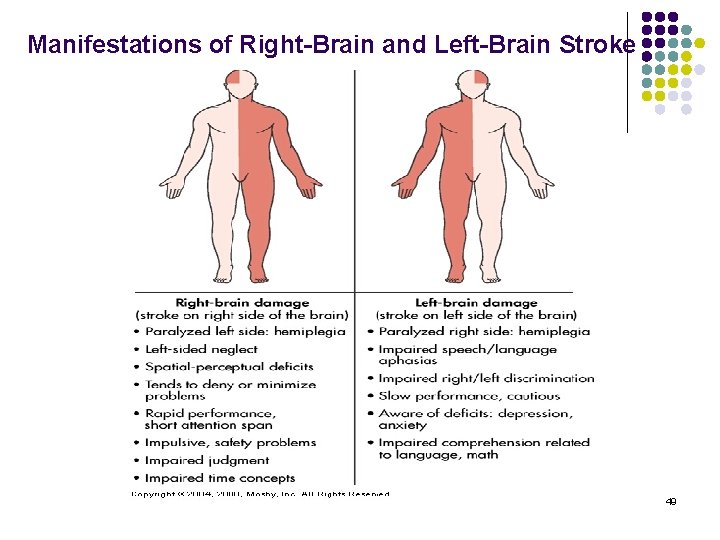
Manifestations of Right-Brain and Left-Brain Stroke 49
Neurodegenerative Disorders 50
Definition l l Neurodegenerative disease is a condition which affects brain function. Neurodegenerative diseases result from deterioration of neurons. They are divided into two groups: l conditions affecting memory and conditions related to dementia conditions causing problems with movements. l Examples: l l l l Alzheimer’s Parkinson’s Huntington’s Creutzfeldt-Jakob disease Multiple Sclerosis Amyotrophic Lateral Sclerosis (ALS or Lou Gehrig's Disease) 51
DEMENTIAS Learning = a change of behaviour based on previous experience, an entry to memory Memory = storage of information for further utilization 52
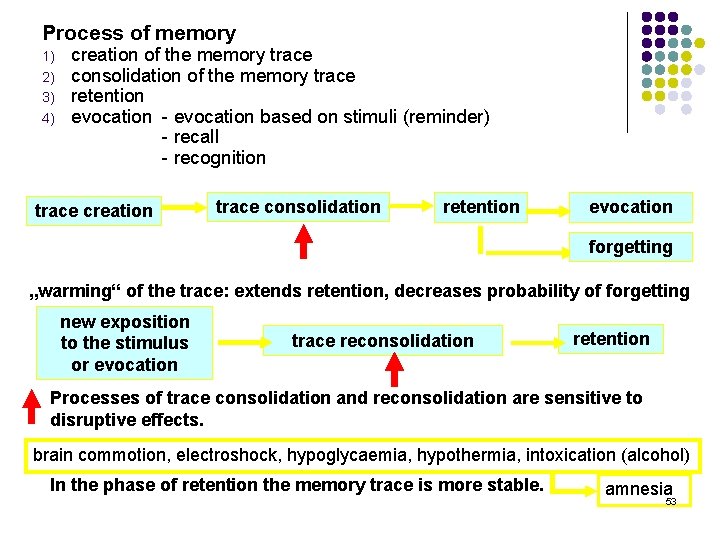
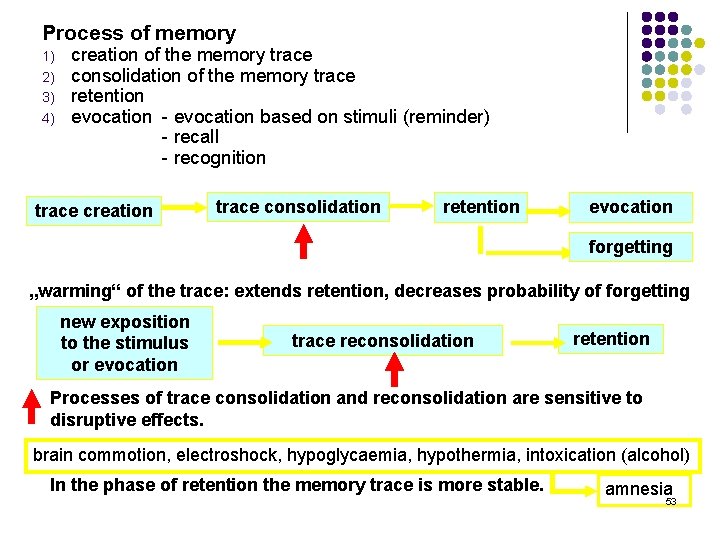
Process of memory 1) 2) 3) 4) creation of the memory trace consolidation of the memory trace retention evocation - evocation based on stimuli (reminder) - recall - recognition trace creation trace consolidation retention evocation forgetting „warming“ of the trace: extends retention, decreases probability of forgetting new exposition to the stimulus or evocation trace reconsolidation retention Processes of trace consolidation and reconsolidation are sensitive to disruptive effects. brain commotion, electroshock, hypoglycaemia, hypothermia, intoxication (alcohol) In the phase of retention the memory trace is more stable. amnesia 53
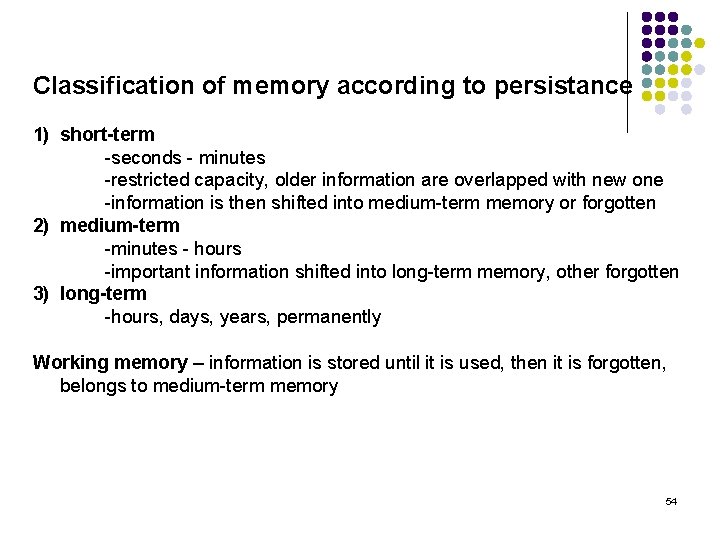
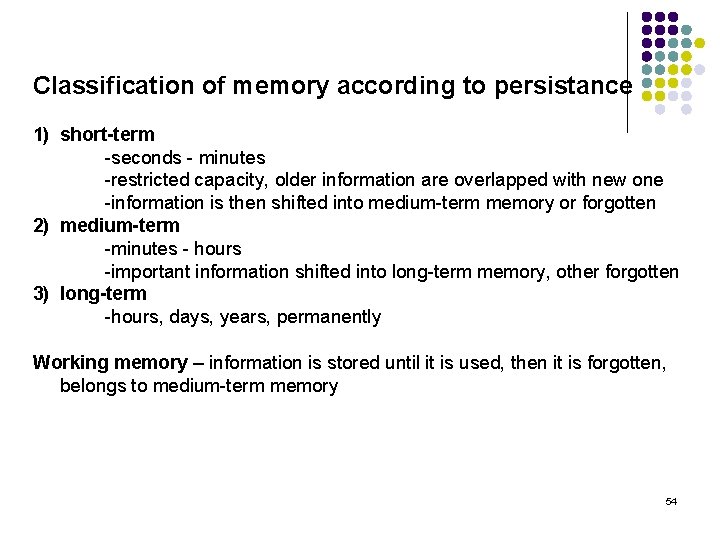
Classification of memory according to persistance 1) short-term -seconds - minutes -restricted capacity, older information are overlapped with new one -information is then shifted into medium-term memory or forgotten 2) medium-term -minutes - hours -important information shifted into long-term memory, other forgotten 3) long-term -hours, days, years, permanently Working memory – information is stored until it is used, then it is forgotten, belongs to medium-term memory 54
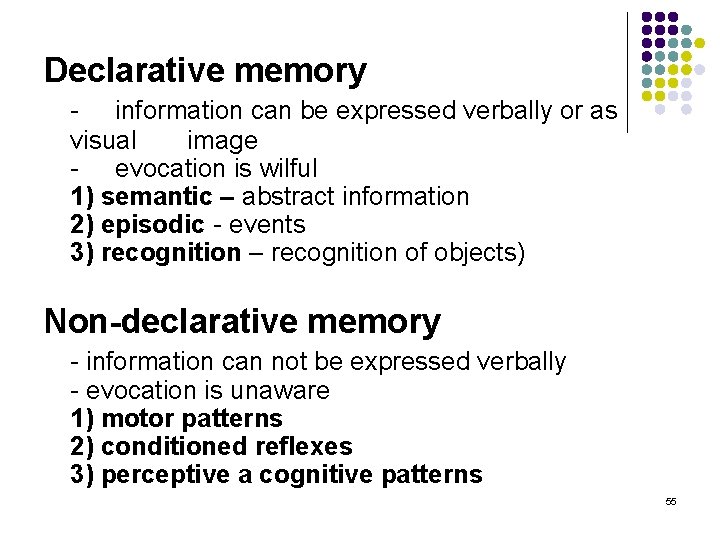
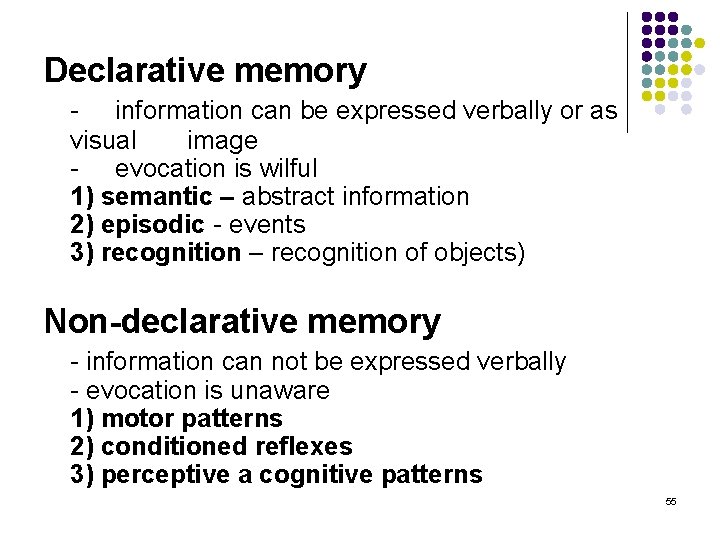
Declarative memory - information can be expressed verbally or as visual image - evocation is wilful 1) semantic – abstract information 2) episodic - events 3) recognition – recognition of objects) Non-declarative memory - information can not be expressed verbally - evocation is unaware 1) motor patterns 2) conditioned reflexes 3) perceptive a cognitive patterns 55
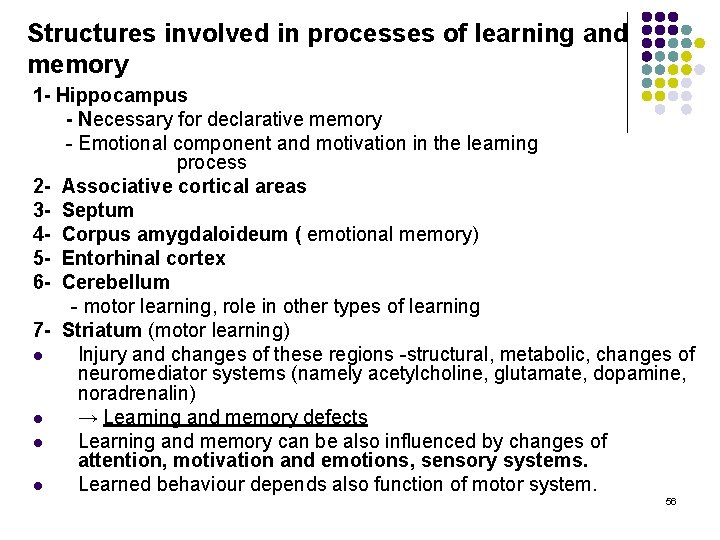
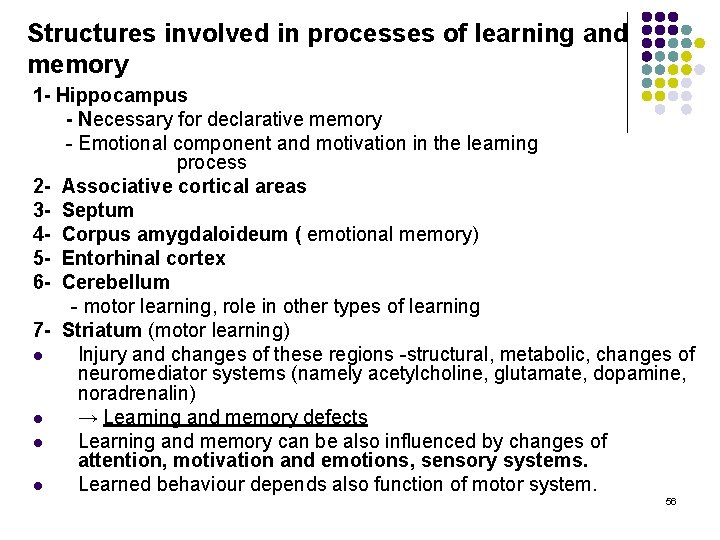
Structures involved in processes of learning and memory 1 - Hippocampus - Necessary for declarative memory - Emotional component and motivation in the learning process 2 - Associative cortical areas 3 - Septum 4 - Corpus amygdaloideum ( emotional memory) 5 - Entorhinal cortex 6 - Cerebellum - motor learning, role in other types of learning 7 - Striatum (motor learning) l Injury and changes of these regions -structural, metabolic, changes of neuromediator systems (namely acetylcholine, glutamate, dopamine, noradrenalin) l → Learning and memory defects l Learning and memory can be also influenced by changes of attention, motivation and emotions, sensory systems. l Learned behaviour depends also function of motor system. 56
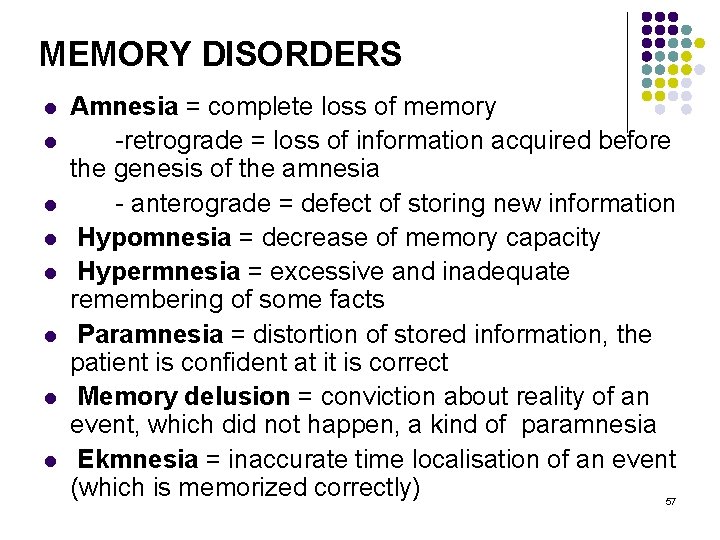
MEMORY DISORDERS l l l l Amnesia = complete loss of memory -retrograde = loss of information acquired before the genesis of the amnesia - anterograde = defect of storing new information Hypomnesia = decrease of memory capacity Hypermnesia = excessive and inadequate remembering of some facts Paramnesia = distortion of stored information, the patient is confident at it is correct Memory delusion = conviction about reality of an event, which did not happen, a kind of paramnesia Ekmnesia = inaccurate time localisation of an event (which is memorized correctly) 57
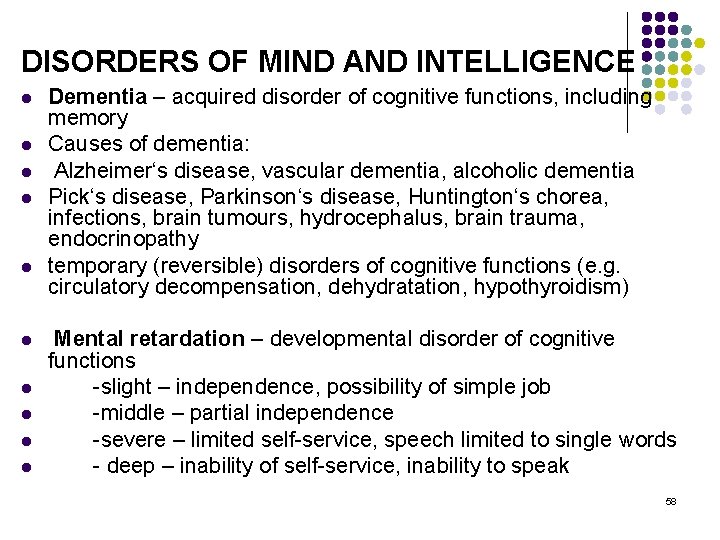
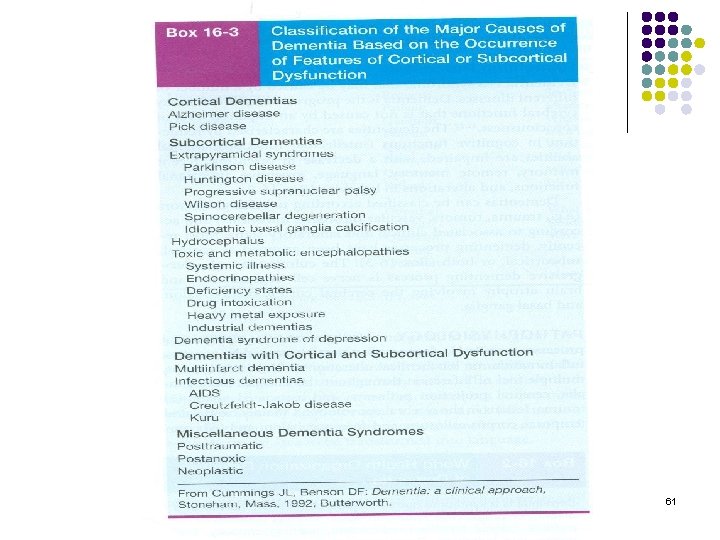
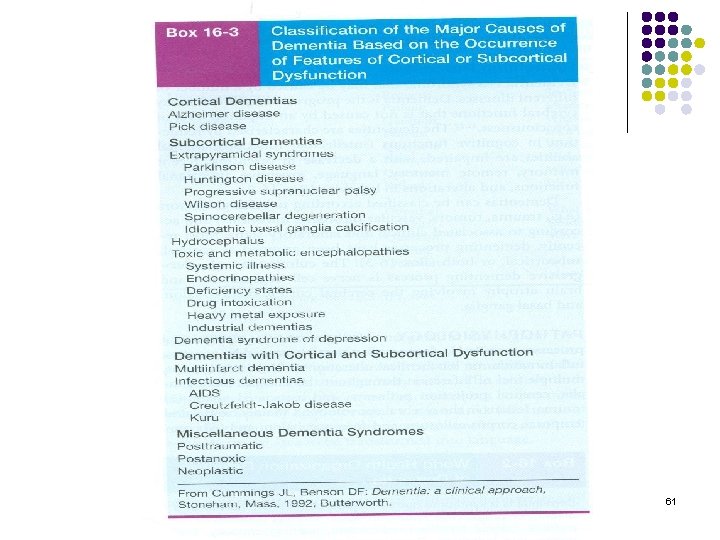
DISORDERS OF MIND AND INTELLIGENCE l l l l l Dementia – acquired disorder of cognitive functions, including memory Causes of dementia: Alzheimer‘s disease, vascular dementia, alcoholic dementia Pick‘s disease, Parkinson‘s disease, Huntington‘s chorea, infections, brain tumours, hydrocephalus, brain trauma, endocrinopathy temporary (reversible) disorders of cognitive functions (e. g. circulatory decompensation, dehydratation, hypothyroidism) Mental retardation – developmental disorder of cognitive functions -slight – independence, possibility of simple job -middle – partial independence -severe – limited self-service, speech limited to single words - deep – inability of self-service, inability to speak 58
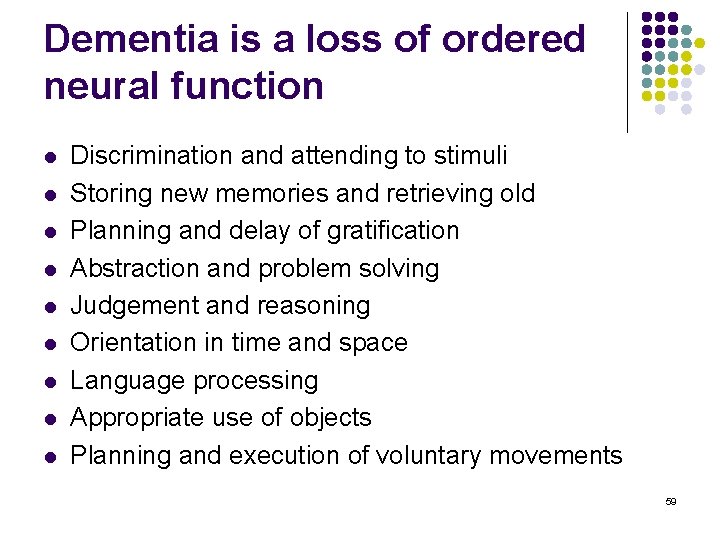
Dementia is a loss of ordered neural function l l l l l Discrimination and attending to stimuli Storing new memories and retrieving old Planning and delay of gratification Abstraction and problem solving Judgement and reasoning Orientation in time and space Language processing Appropriate use of objects Planning and execution of voluntary movements 59
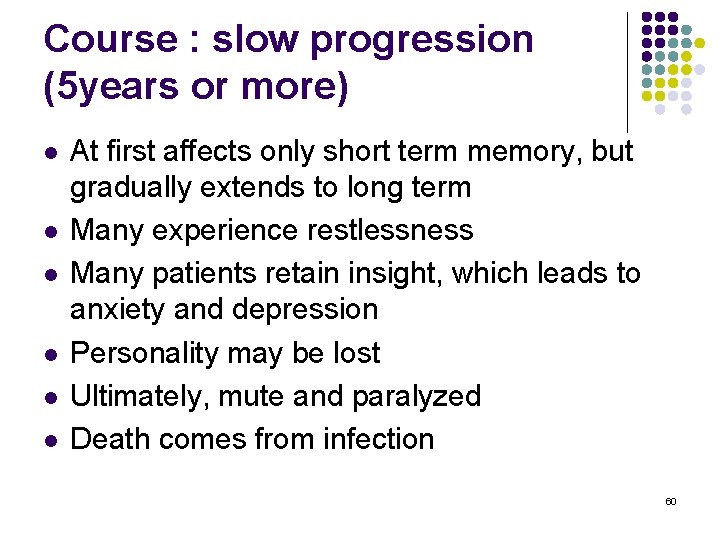
Course : slow progression (5 years or more) l l l At first affects only short term memory, but gradually extends to long term Many experience restlessness Many patients retain insight, which leads to anxiety and depression Personality may be lost Ultimately, mute and paralyzed Death comes from infection 60
61
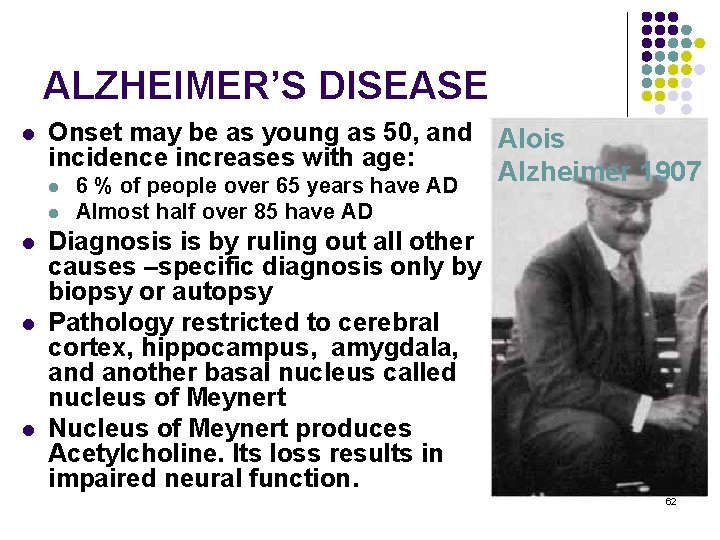
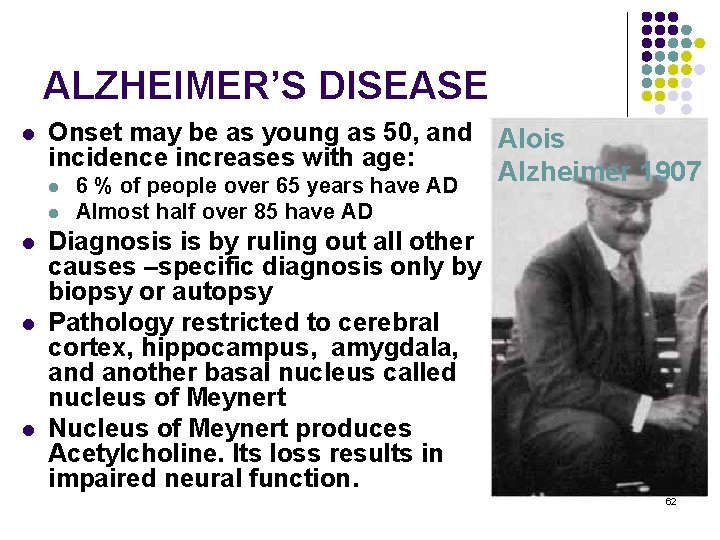
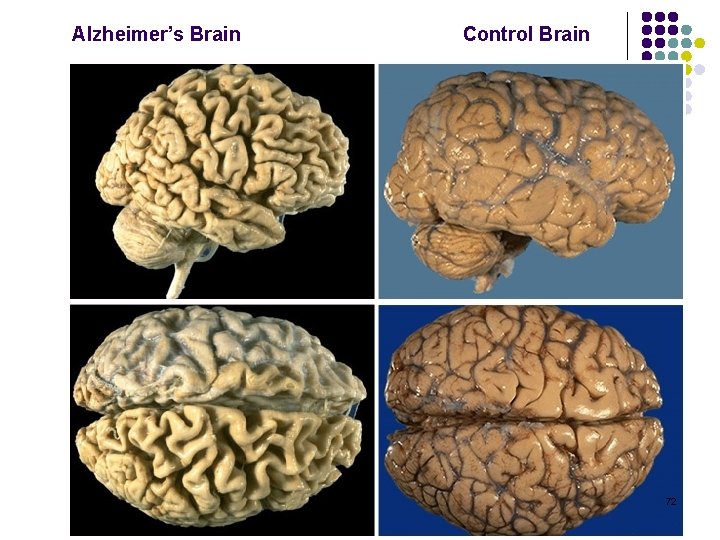
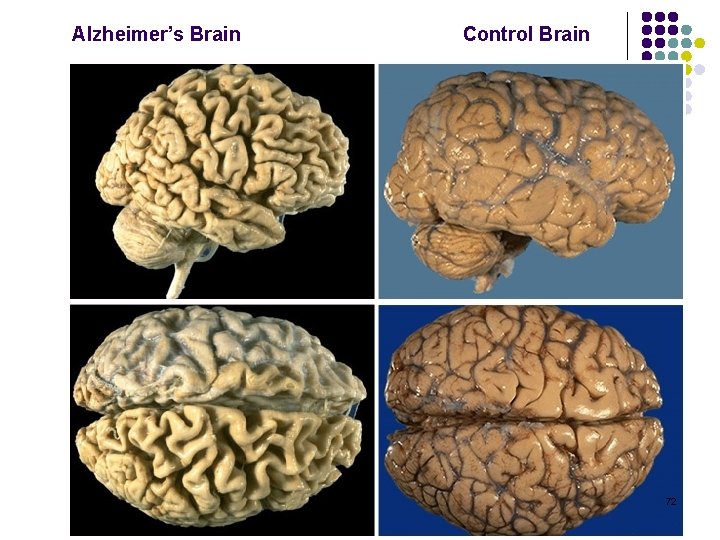
ALZHEIMER’S DISEASE l Onset may be as young as 50, and Alois incidence increases with age: l l l 6 % of people over 65 years have AD Almost half over 85 have AD Alzheimer 1907 Diagnosis is by ruling out all other causes –specific diagnosis only by biopsy or autopsy Pathology restricted to cerebral cortex, hippocampus, amygdala, and another basal nucleus called nucleus of Meynert Nucleus of Meynert produces Acetylcholine. Its loss results in impaired neural function. 62
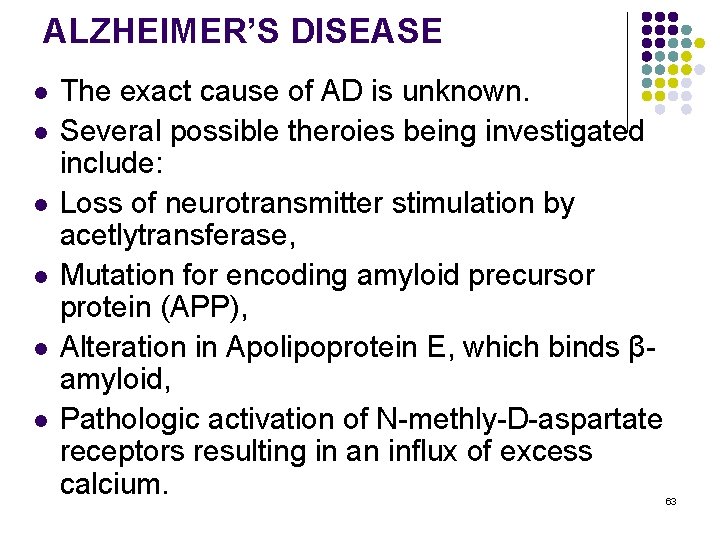
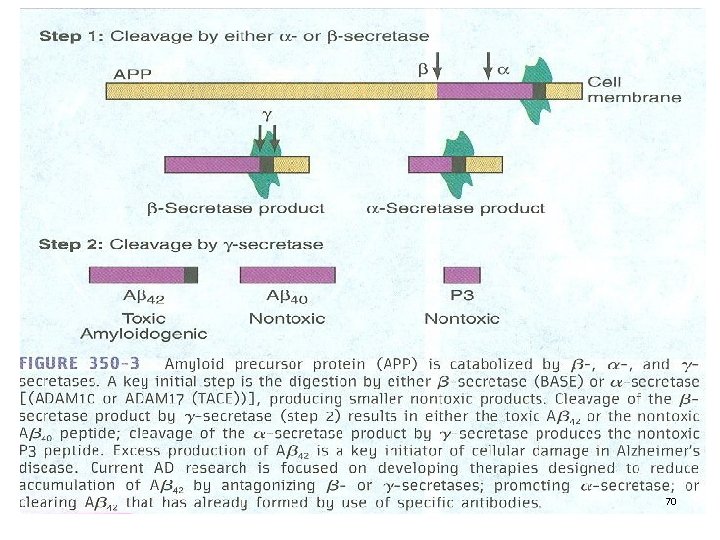
ALZHEIMER’S DISEASE l l l The exact cause of AD is unknown. Several possible theroies being investigated include: Loss of neurotransmitter stimulation by acetlytransferase, Mutation for encoding amyloid precursor protein (APP), Alteration in Apolipoprotein E, which binds βamyloid, Pathologic activation of N-methly-D-aspartate receptors resulting in an influx of excess calcium. 63
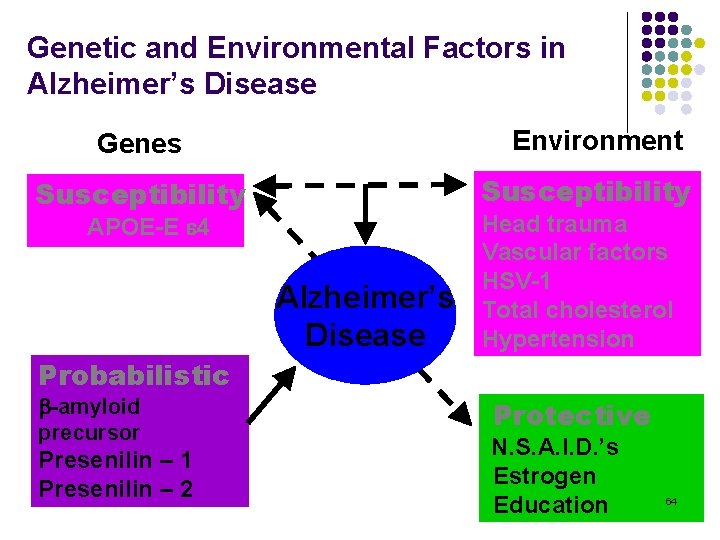
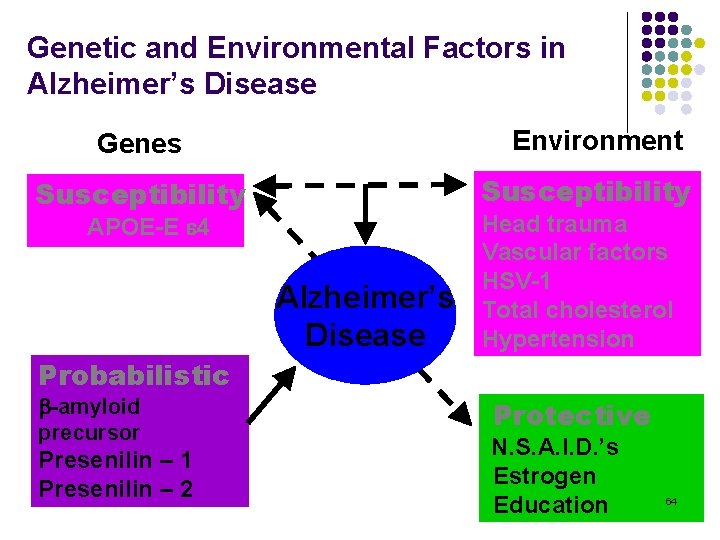
Genetic and Environmental Factors in Alzheimer’s Disease Environment Genes Susceptibility APOE-E 4 Alzheimer’s Disease Head trauma Vascular factors HSV-1 Total cholesterol Hypertension Probabilistic -amyloid precursor Presenilin – 1 Presenilin – 2 Protective N. S. A. I. D. ’s Estrogen Education 64
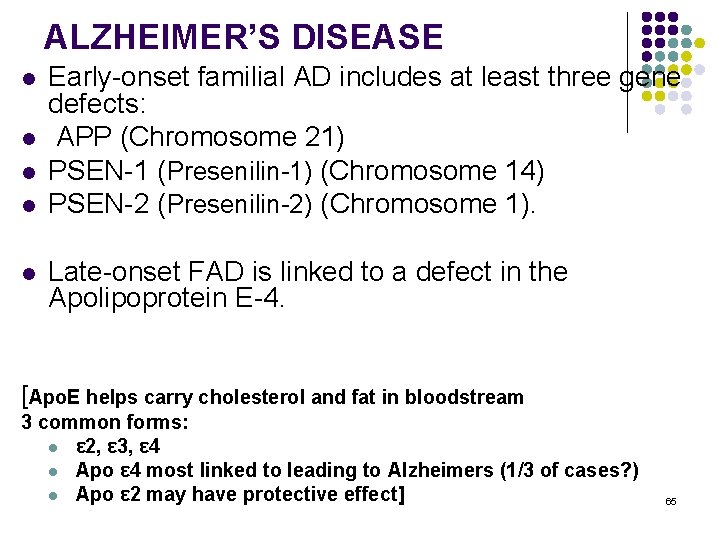
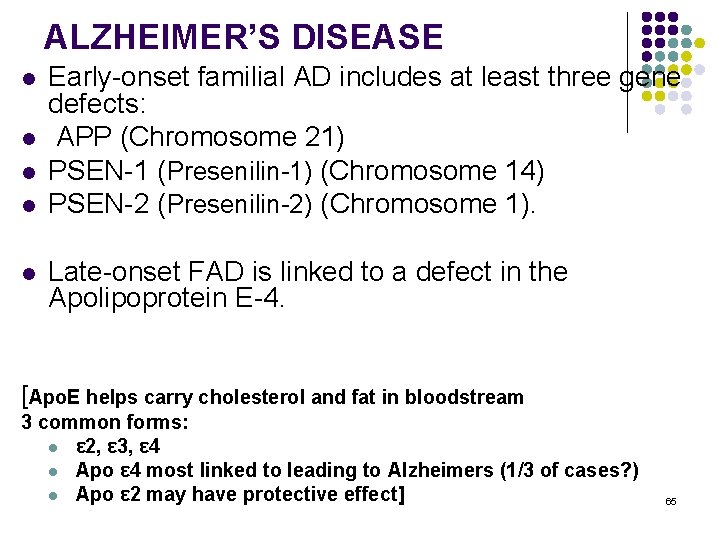
ALZHEIMER’S DISEASE l l l Early-onset familial AD includes at least three gene defects: APP (Chromosome 21) PSEN-1 (Presenilin-1) (Chromosome 14) PSEN-2 (Presenilin-2) (Chromosome 1). Late-onset FAD is linked to a defect in the Apolipoprotein E-4. [Apo. E helps carry cholesterol and fat in bloodstream 3 common forms: l ε 2, ε 3, ε 4 l Apo ε 4 most linked to leading to Alzheimers (1/3 of cases? ) l Apo ε 2 may have protective effect] 65
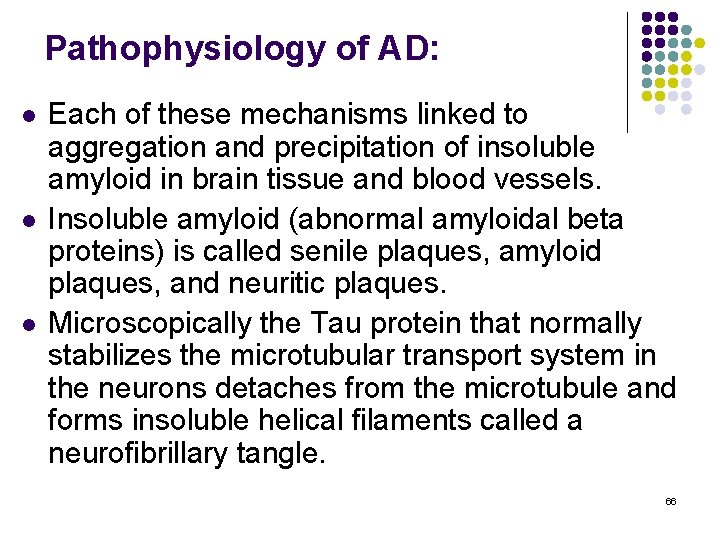
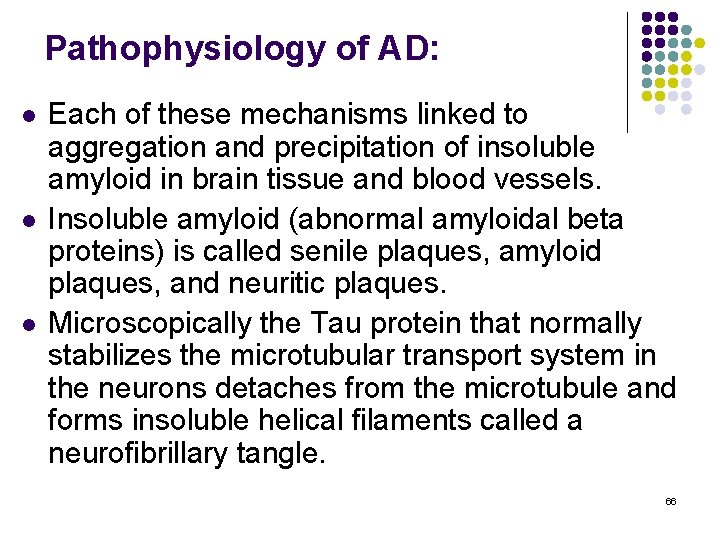
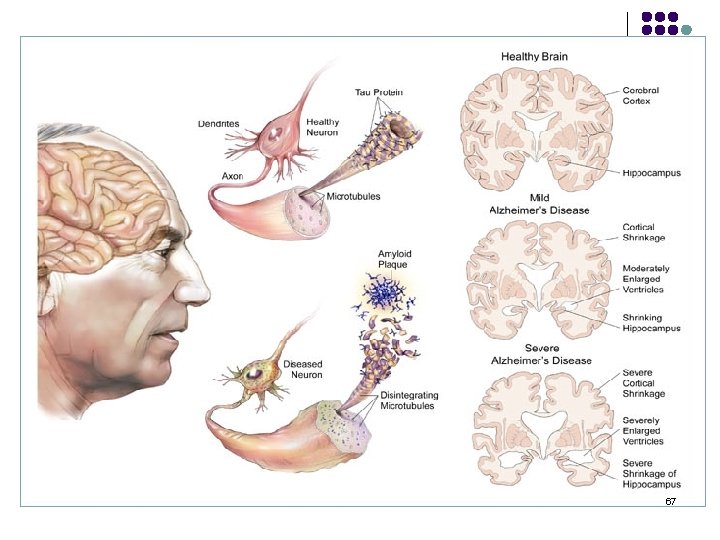
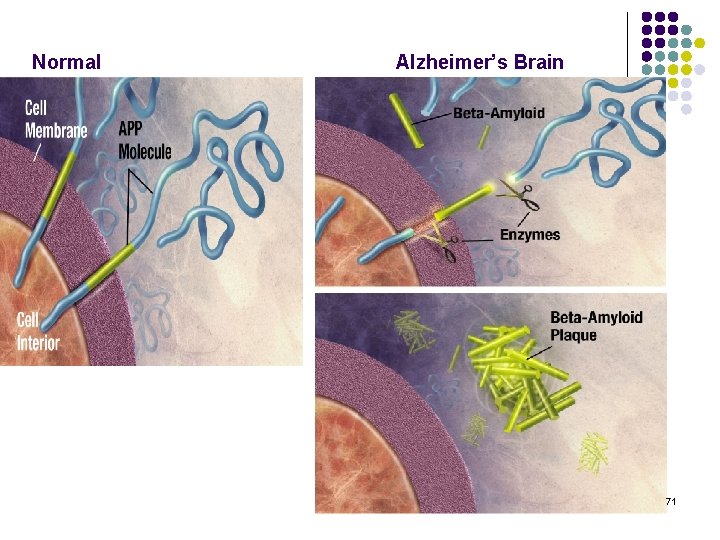
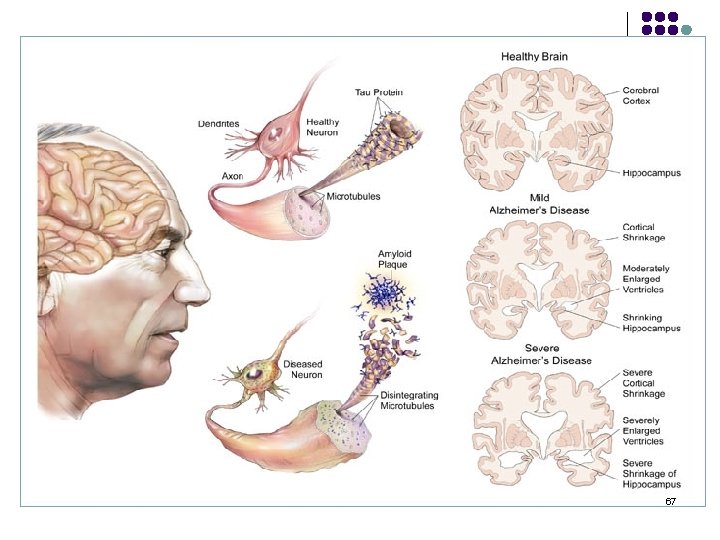
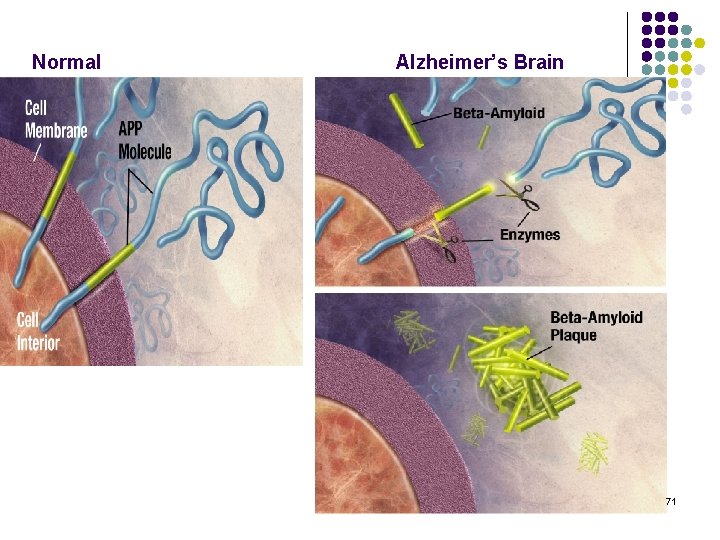
Pathophysiology of AD: l l l Each of these mechanisms linked to aggregation and precipitation of insoluble amyloid in brain tissue and blood vessels. Insoluble amyloid (abnormal amyloidal beta proteins) is called senile plaques, amyloid plaques, and neuritic plaques. Microscopically the Tau protein that normally stabilizes the microtubular transport system in the neurons detaches from the microtubule and forms insoluble helical filaments called a neurofibrillary tangle. 66
67
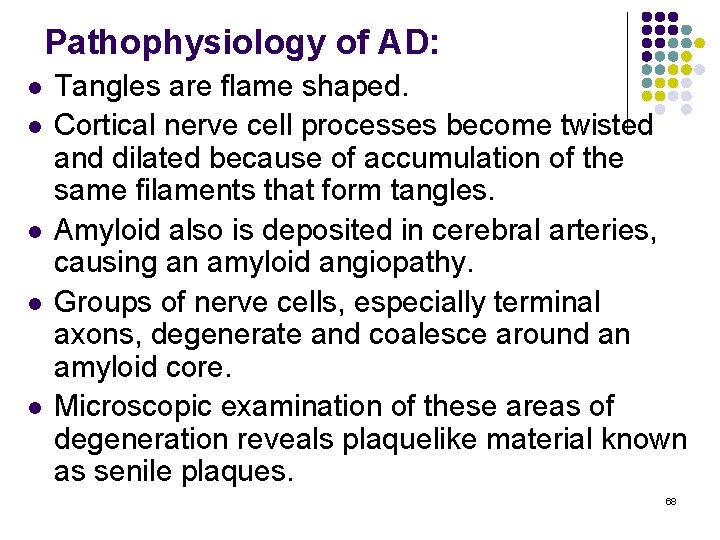
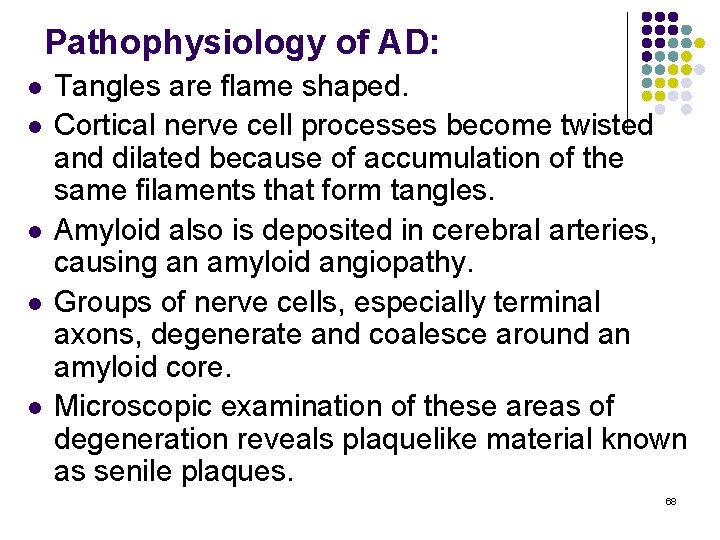
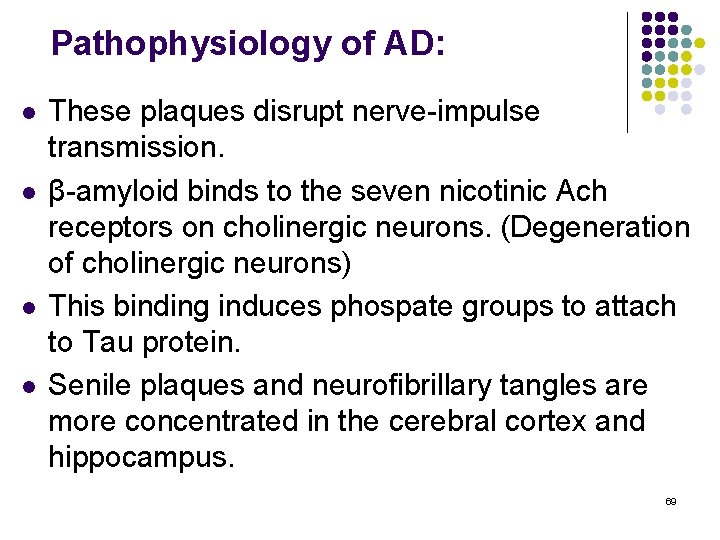
Pathophysiology of AD: l l l Tangles are flame shaped. Cortical nerve cell processes become twisted and dilated because of accumulation of the same filaments that form tangles. Amyloid also is deposited in cerebral arteries, causing an amyloid angiopathy. Groups of nerve cells, especially terminal axons, degenerate and coalesce around an amyloid core. Microscopic examination of these areas of degeneration reveals plaquelike material known as senile plaques. 68
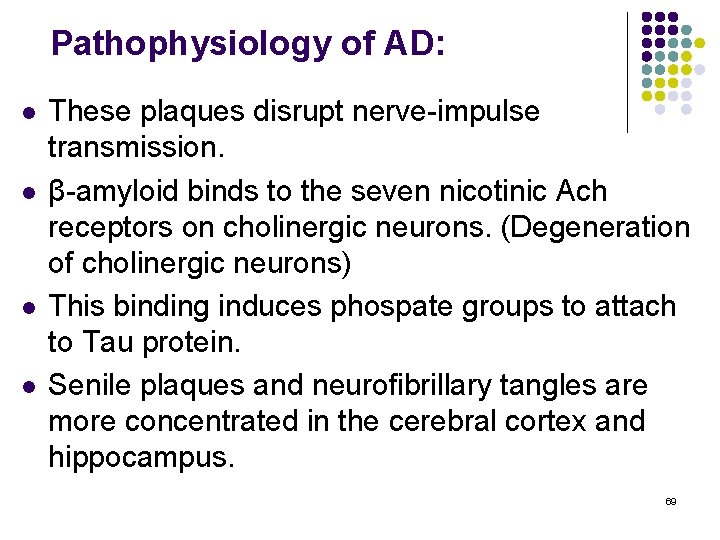
Pathophysiology of AD: l l These plaques disrupt nerve-impulse transmission. β-amyloid binds to the seven nicotinic Ach receptors on cholinergic neurons. (Degeneration of cholinergic neurons) This binding induces phospate groups to attach to Tau protein. Senile plaques and neurofibrillary tangles are more concentrated in the cerebral cortex and hippocampus. 69
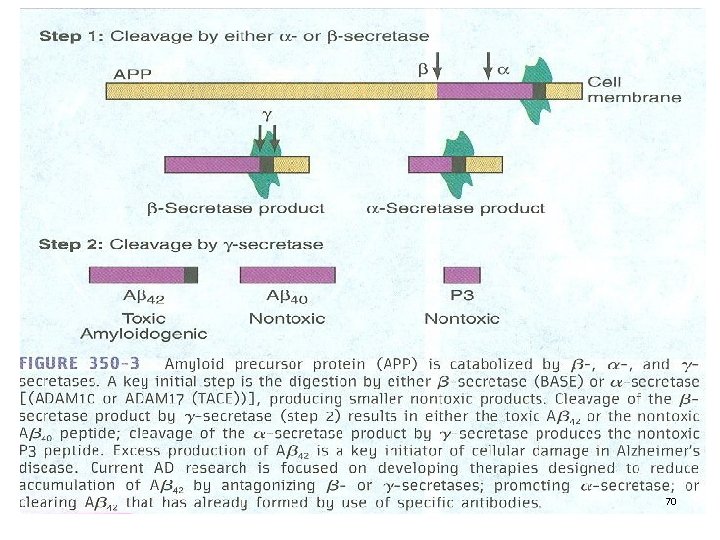
70
Normal Alzheimer’s Brain 71
Alzheimer’s Brain Control Brain 72
Alzheimer’s Disease l Clinical manifestations: l l l l Insidious onset Forgetfulness increasing over time Memory loss Deteriorating ability for problem solving Judgment deteriorates Behavioral changes Labile 73
PARKINSON’S DISEASE 1817 James Parkinson 74
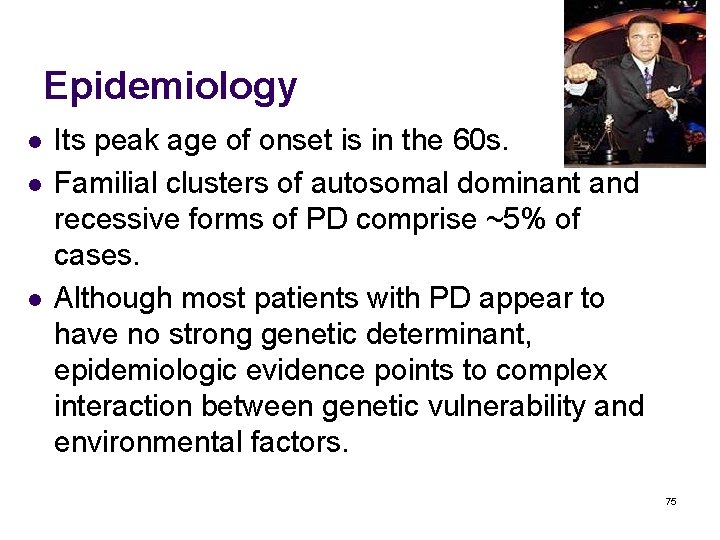
Epidemiology l l l Its peak age of onset is in the 60 s. Familial clusters of autosomal dominant and recessive forms of PD comprise ~5% of cases. Although most patients with PD appear to have no strong genetic determinant, epidemiologic evidence points to complex interaction between genetic vulnerability and environmental factors. 75
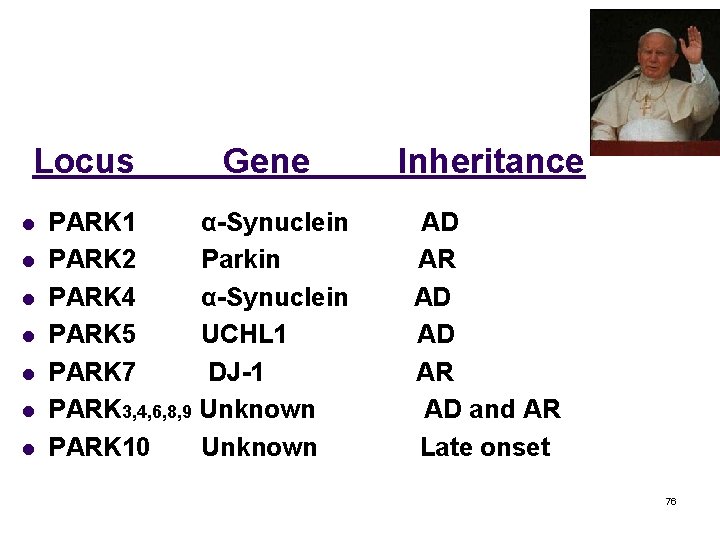
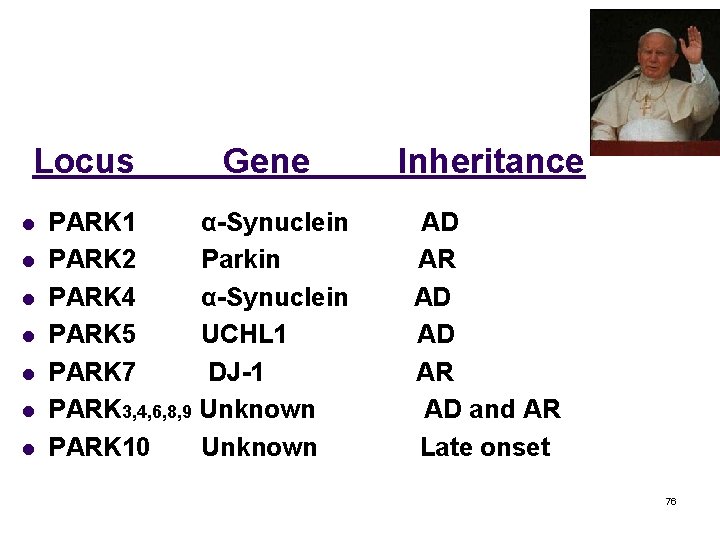
Locus l l l l Gene PARK 1 α-Synuclein PARK 2 Parkin PARK 4 α-Synuclein PARK 5 UCHL 1 PARK 7 DJ-1 PARK 3, 4, 6, 8, 9 Unknown PARK 10 Unknown Inheritance AD AR AD and AR Late onset 76
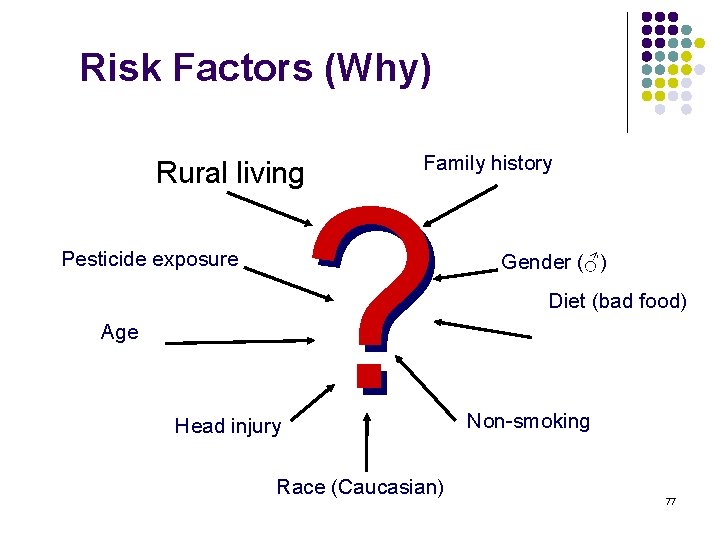
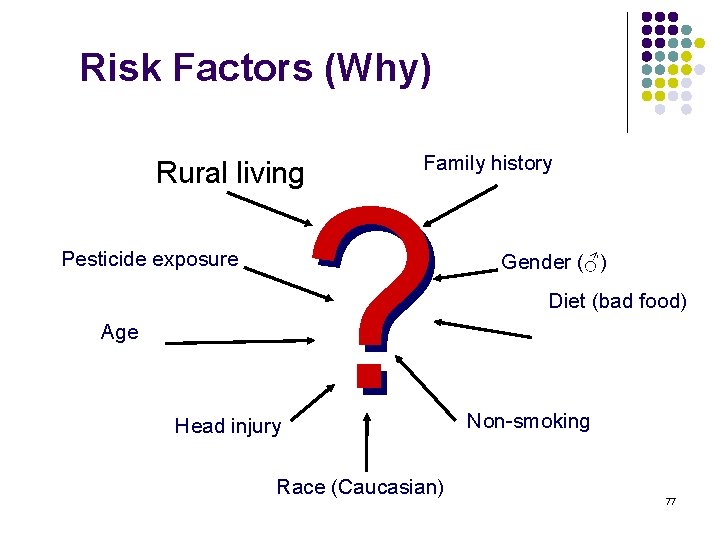
Risk Factors (Why) Rural living Pesticide exposure Age Head injury Family history ? Race (Caucasian) Gender (♂) Diet (bad food) Non-smoking 77
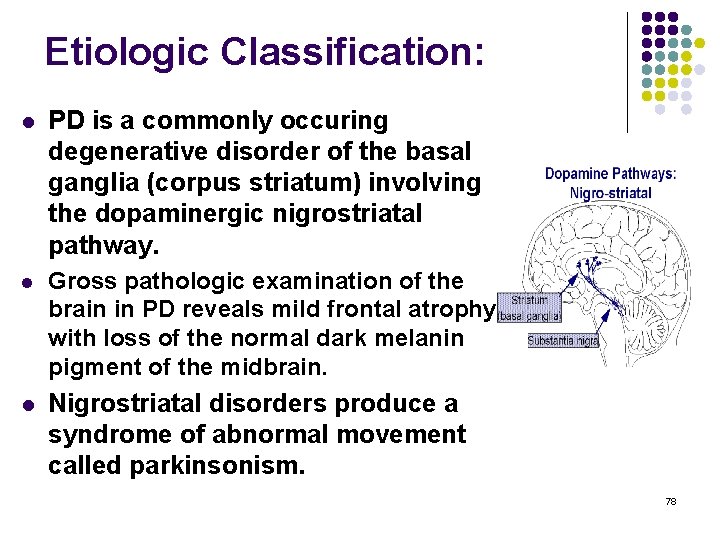
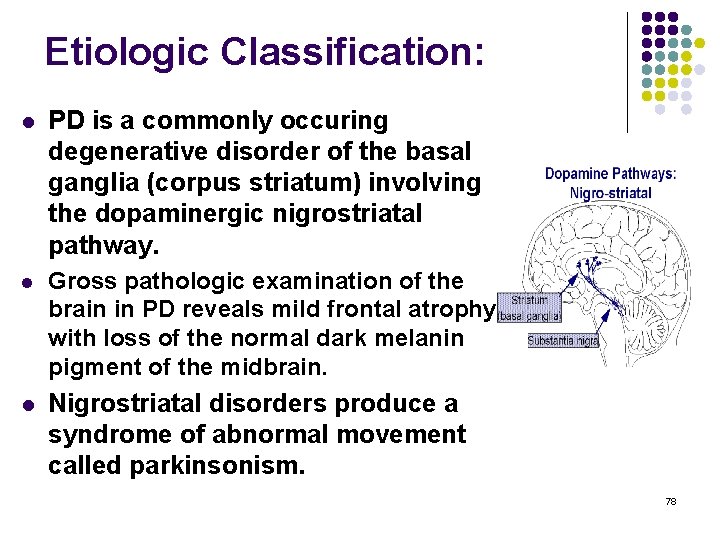
Etiologic Classification: l PD is a commonly occuring degenerative disorder of the basal ganglia (corpus striatum) involving the dopaminergic nigrostriatal pathway. l Gross pathologic examination of the brain in PD reveals mild frontal atrophy with loss of the normal dark melanin pigment of the midbrain. l Nigrostriatal disorders produce a syndrome of abnormal movement called parkinsonism. 78
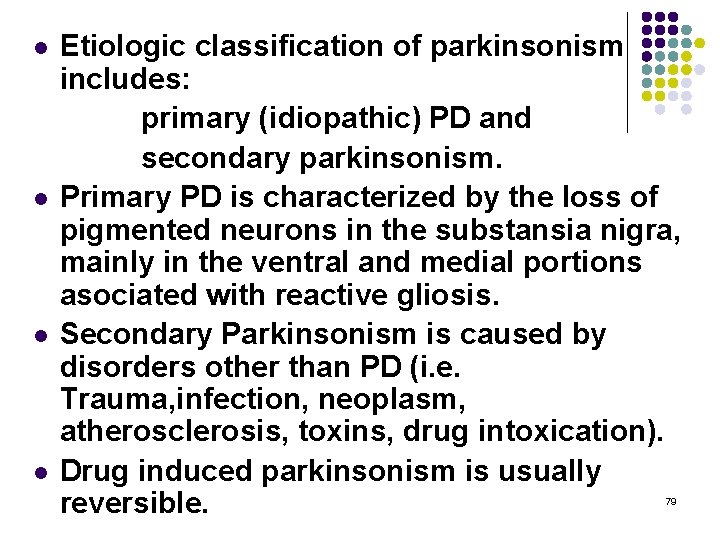
l l Etiologic classification of parkinsonism includes: primary (idiopathic) PD and secondary parkinsonism. Primary PD is characterized by the loss of pigmented neurons in the substansia nigra, mainly in the ventral and medial portions asociated with reactive gliosis. Secondary Parkinsonism is caused by disorders other than PD (i. e. Trauma, infection, neoplasm, atherosclerosis, toxins, drug intoxication). Drug induced parkinsonism is usually reversible. 79
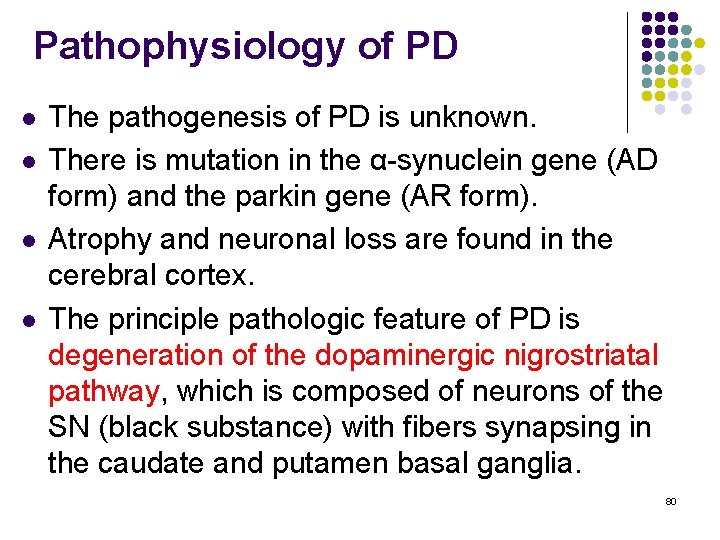
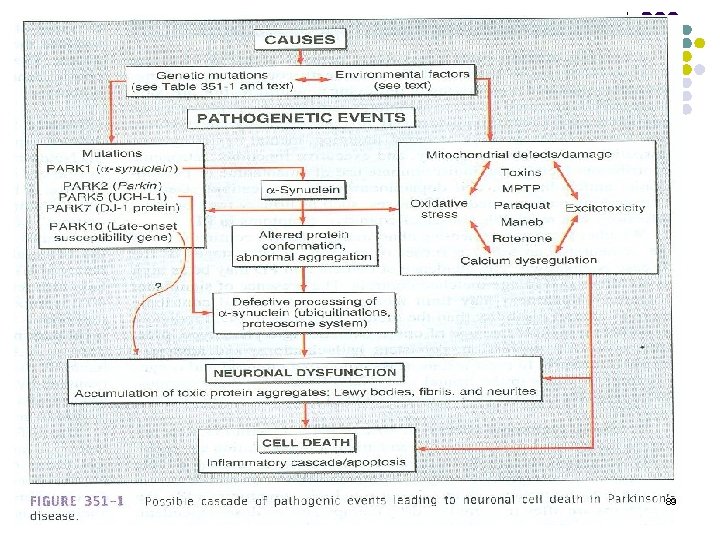
Pathophysiology of PD l l The pathogenesis of PD is unknown. There is mutation in the α-synuclein gene (AD form) and the parkin gene (AR form). Atrophy and neuronal loss are found in the cerebral cortex. The principle pathologic feature of PD is degeneration of the dopaminergic nigrostriatal pathway, which is composed of neurons of the SN (black substance) with fibers synapsing in the caudate and putamen basal ganglia. 80
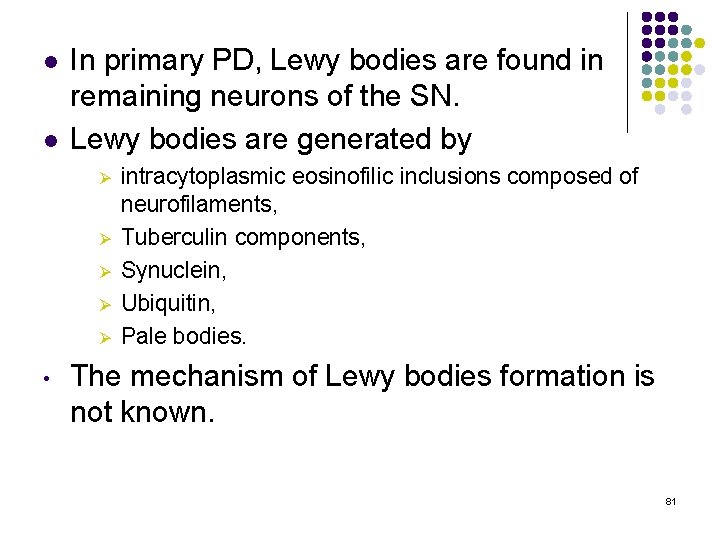
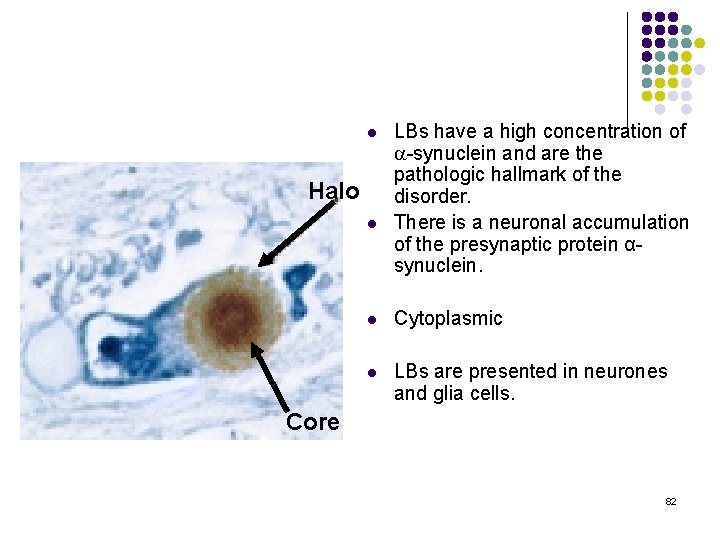
l l In primary PD, Lewy bodies are found in remaining neurons of the SN. Lewy bodies are generated by Ø Ø Ø • intracytoplasmic eosinofilic inclusions composed of neurofilaments, Tuberculin components, Synuclein, Ubiquitin, Pale bodies. The mechanism of Lewy bodies formation is not known. 81
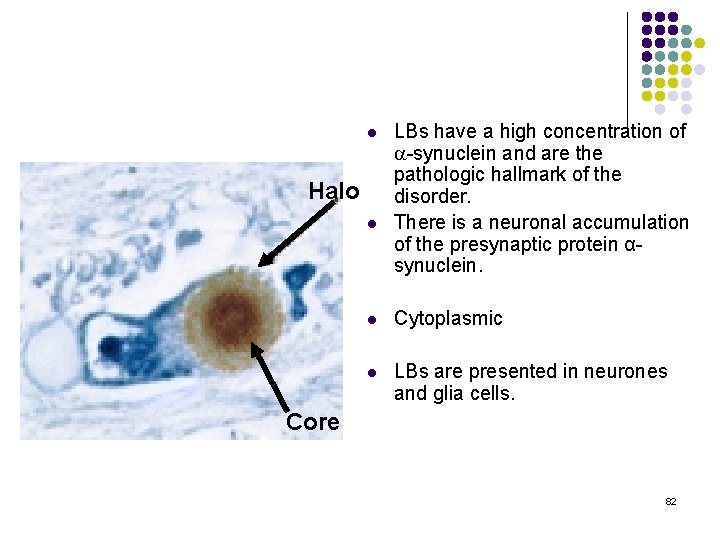
l Halo l LBs have a high concentration of a-synuclein and are the pathologic hallmark of the disorder. There is a neuronal accumulation of the presynaptic protein αsynuclein. l Cytoplasmic l LBs are presented in neurones and glia cells. Core 82
l l The another pathologic feature is significant reduction in certain dopamine receptors (D 1) in basal ganglia. Nigral and basal ganglial depletion of dopamine, an inhibitory neurotransmitter is the principal biochemical alteration in PD. There is a imbalance of dopaminergic (inhibitory) and cholinergic (excitatory) activity in the caudate nucleus and putamen of the basal ganglia in PD. Dopaminergic-cholinergic balance produces normal motor functions. 83
l l In PD, degeneration of the dopaminergic nigrostriatal pathway causes dopamine depletion, and a relative excess of cholinergic activity in the feedback circuit involving the cerebral cortex, basal ganglia, and thalamus. A relative excess of cholinergic activity in this circuit as in PD is manifested by hypertonia (tremor, rigidity) and akinesia. 84
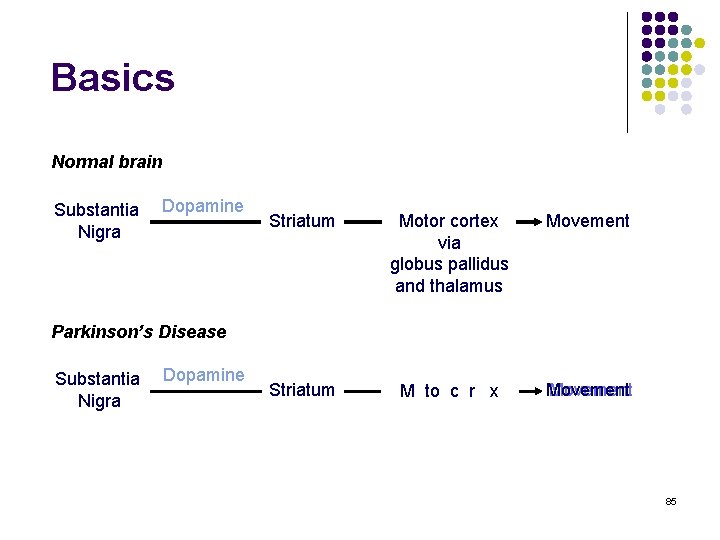
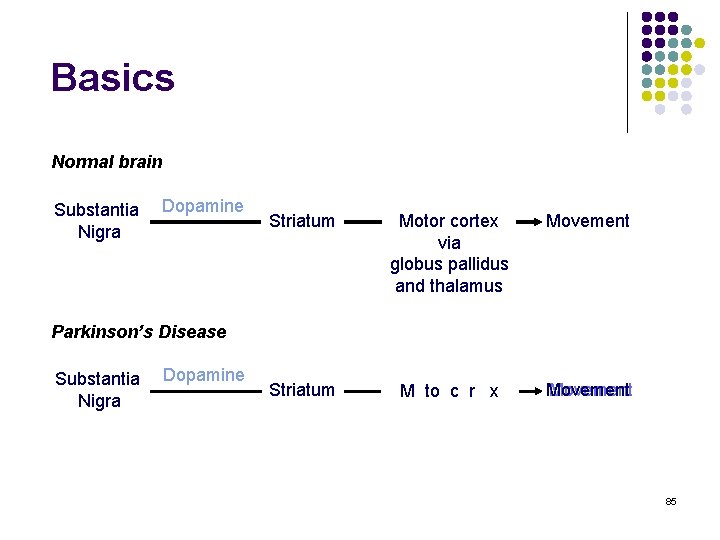
Basics Normal brain Substantia Nigra Dopamine Striatum Motor cortex via globus pallidus and thalamus Movement Striatum M Motor to ccortex r x Movement Parkinson’s Disease Substantia Nigra Dopamine 85
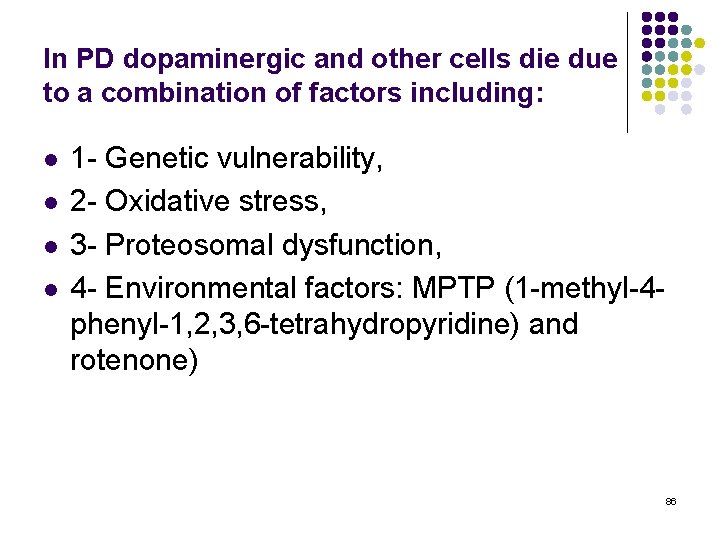
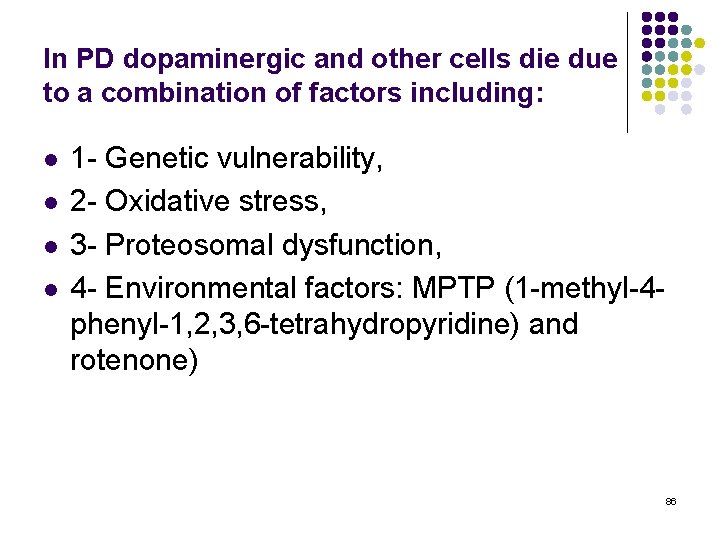
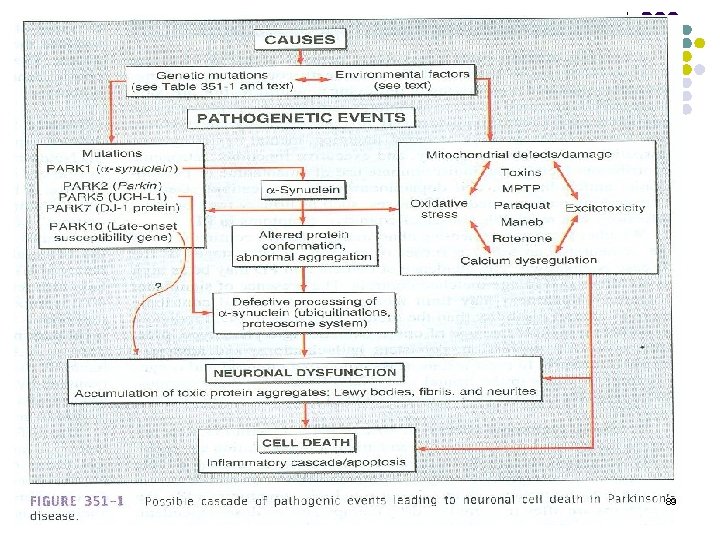
In PD dopaminergic and other cells die due to a combination of factors including: l l 1 - Genetic vulnerability, 2 - Oxidative stress, 3 - Proteosomal dysfunction, 4 - Environmental factors: MPTP (1 -methyl-4 phenyl-1, 2, 3, 6 -tetrahydropyridine) and rotenone) 86
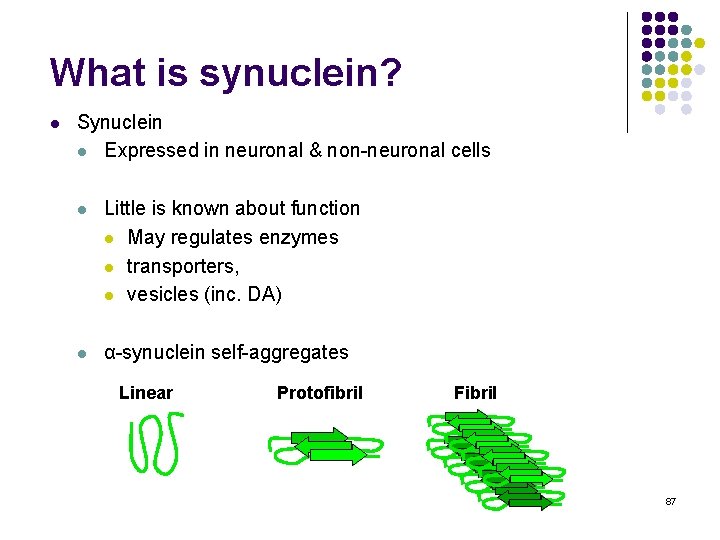
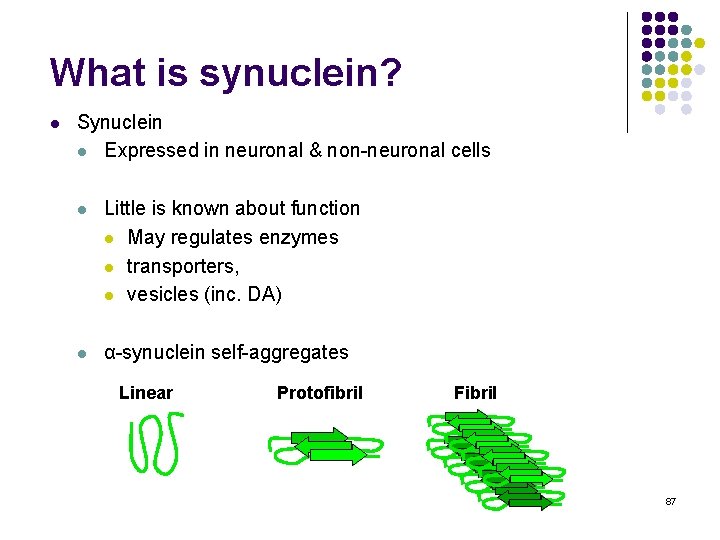
What is synuclein? l Synuclein l Expressed in neuronal & non-neuronal cells l Little is known about function l May regulates enzymes l transporters, l vesicles (inc. DA) l α-synuclein self-aggregates Linear Protofibril Fibril 87
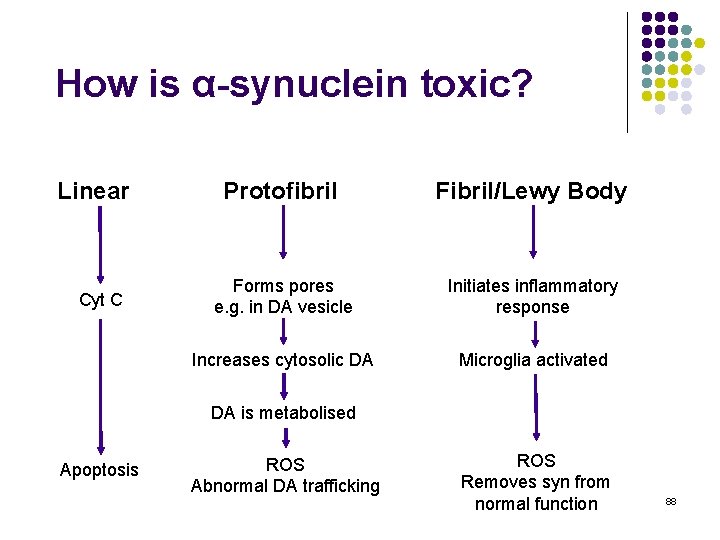
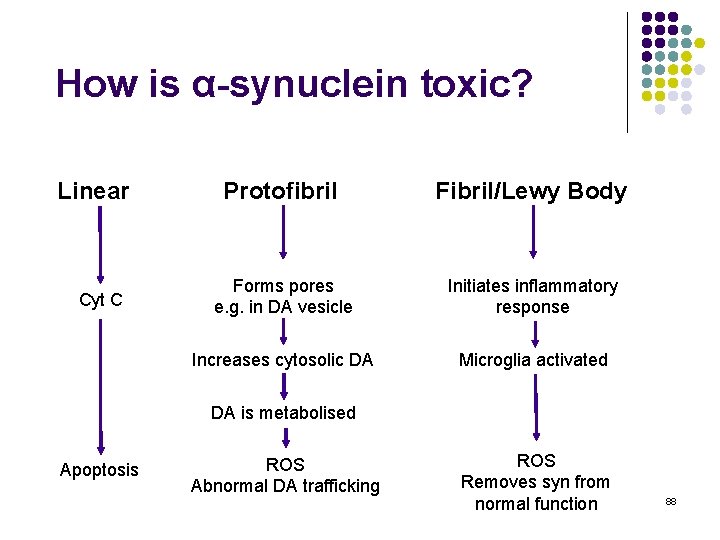
How is α-synuclein toxic? Linear Cyt C Protofibril Fibril/Lewy Body Forms pores e. g. in DA vesicle Initiates inflammatory response Increases cytosolic DA Microglia activated DA is metabolised Apoptosis ROS Abnormal DA trafficking ROS Removes syn from normal function 88
89
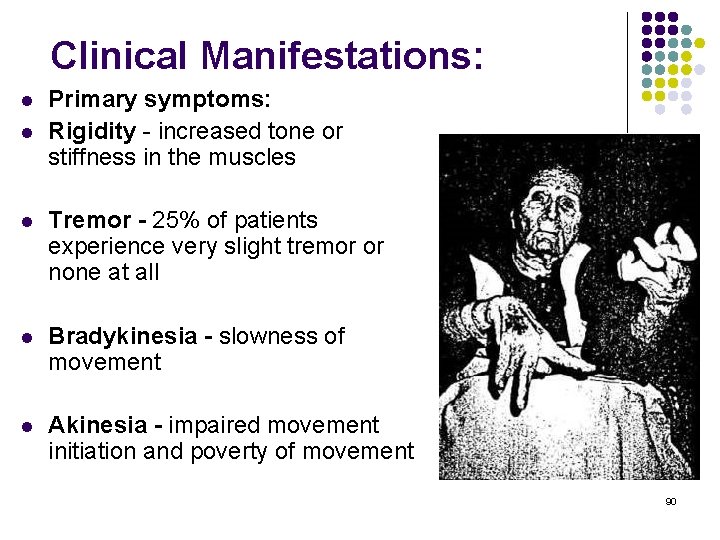
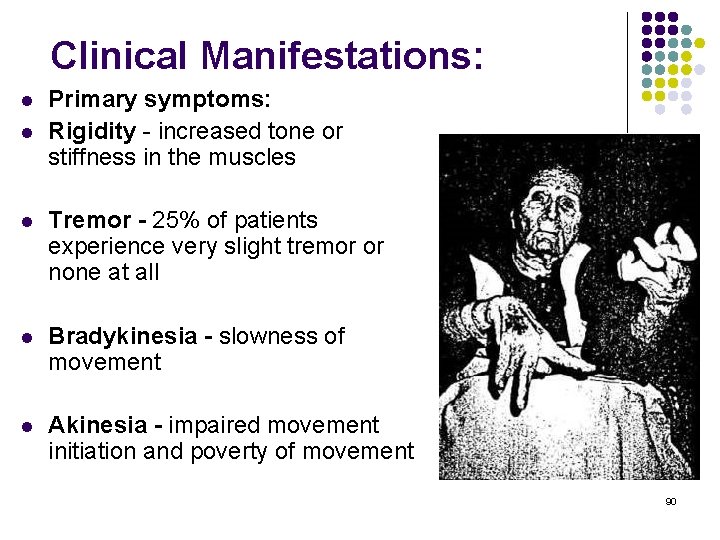
Clinical Manifestations: l l Primary symptoms: Rigidity - increased tone or stiffness in the muscles l Tremor - 25% of patients experience very slight tremor or none at all l Bradykinesia - slowness of movement l Akinesia - impaired movement initiation and poverty of movement 90
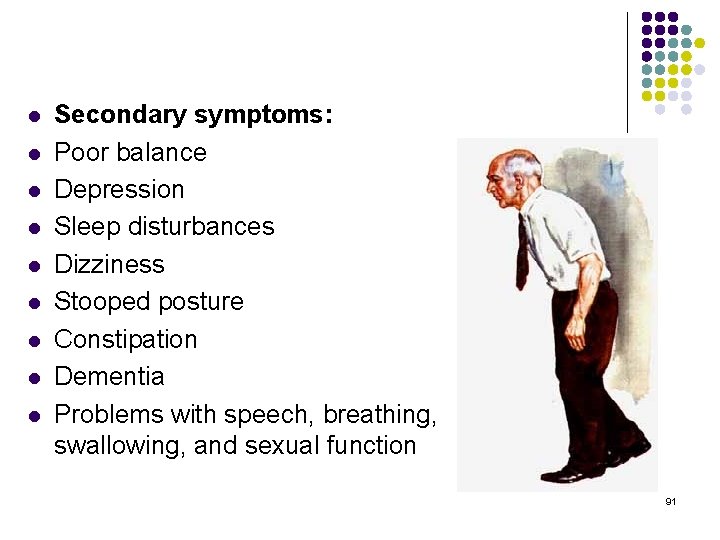
l l l l l Secondary symptoms: Poor balance Depression Sleep disturbances Dizziness Stooped posture Constipation Dementia Problems with speech, breathing, swallowing, and sexual function 91
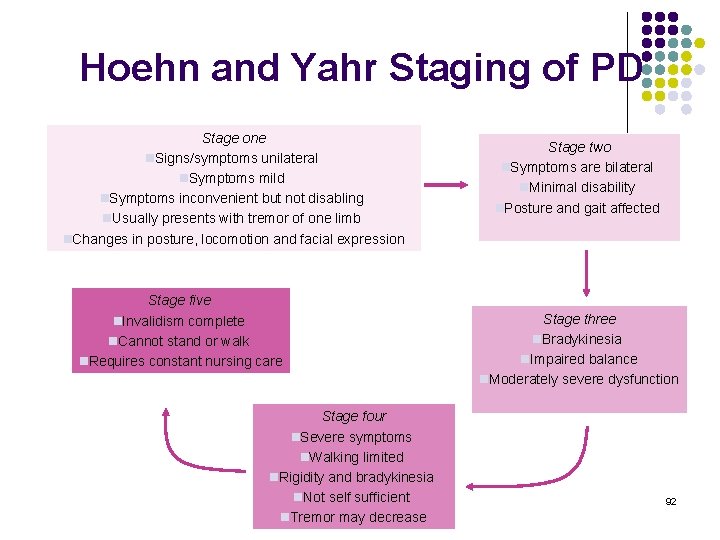
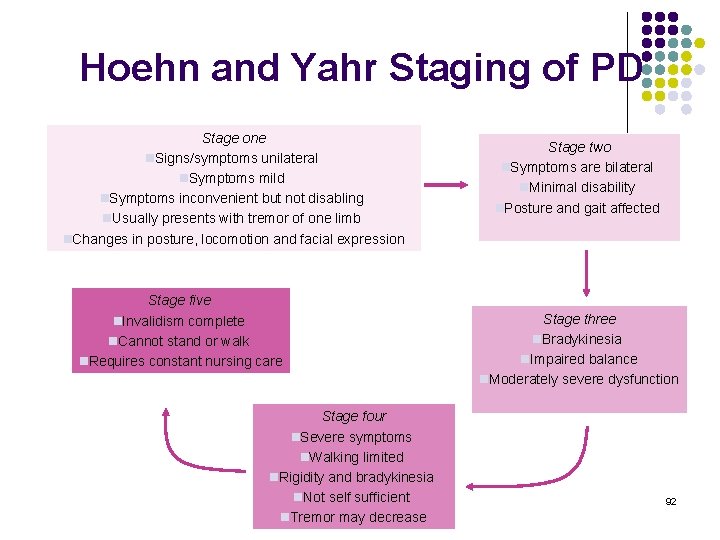
Hoehn and Yahr Staging of PD Stage one n. Signs/symptoms unilateral n. Symptoms mild n. Symptoms inconvenient but not disabling n. Usually presents with tremor of one limb n. Changes in posture, locomotion and facial expression Stage five n. Invalidism complete n. Cannot stand or walk n. Requires constant nursing care Stage four n. Severe symptoms n. Walking limited n. Rigidity and bradykinesia n. Not self sufficient n. Tremor may decrease Stage two n. Symptoms are bilateral n. Minimal disability n. Posture and gait affected Stage three n. Bradykinesia n. Impaired balance n. Moderately severe dysfunction 92
MOTOR NEURON DİSEASES (Amyotrophic Lateral Sclerosis) 93
Amyotrophic Lateral Sclerosis l Degenerative motor neuron disease that affects UMN & LMN lying within the brain, spinal cord and peripheral nerves l Lou Gehrig 94
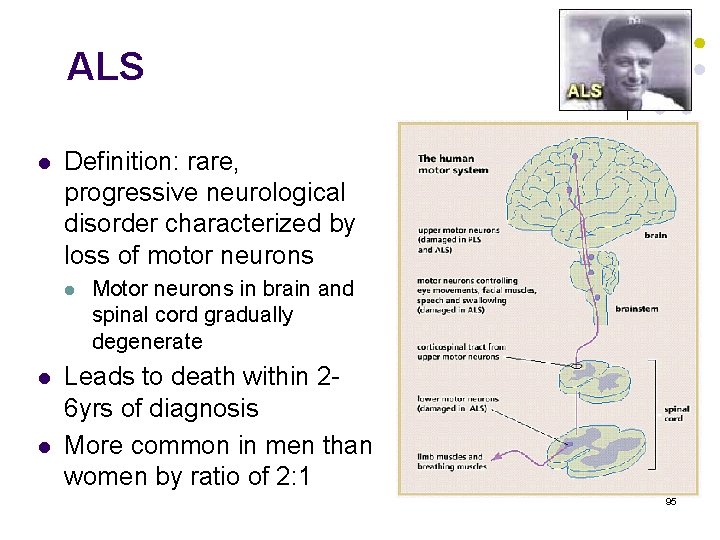
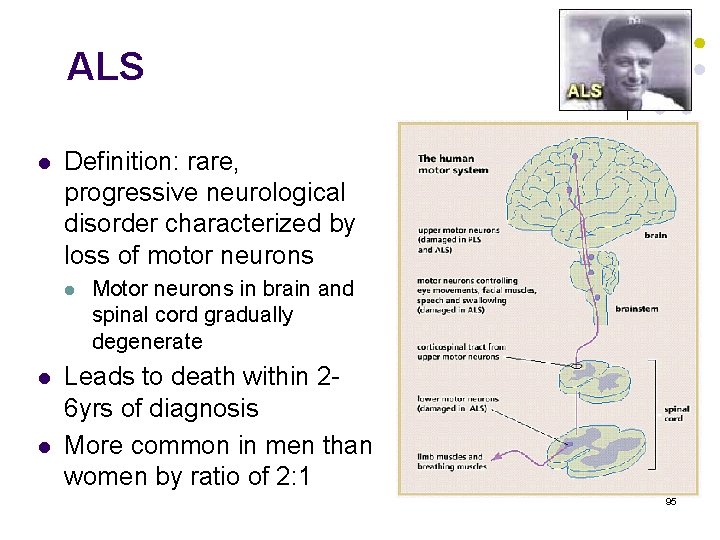
ALS l Definition: rare, progressive neurological disorder characterized by loss of motor neurons l l l Motor neurons in brain and spinal cord gradually degenerate Leads to death within 26 yrs of diagnosis More common in men than women by ratio of 2: 1 95
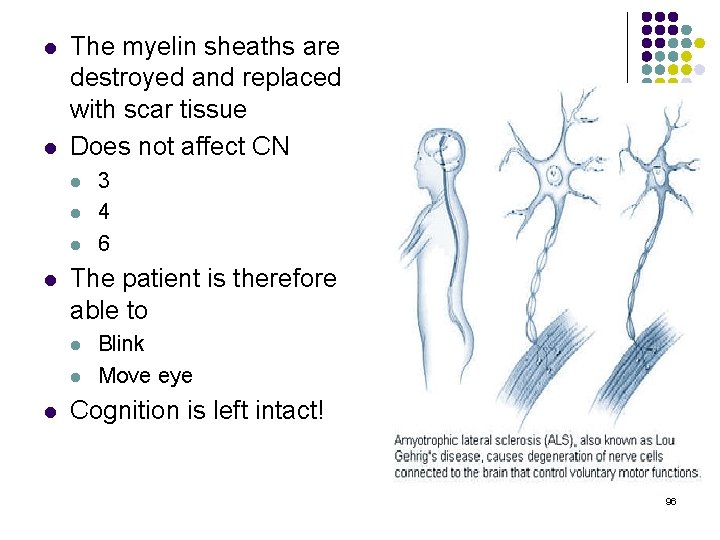
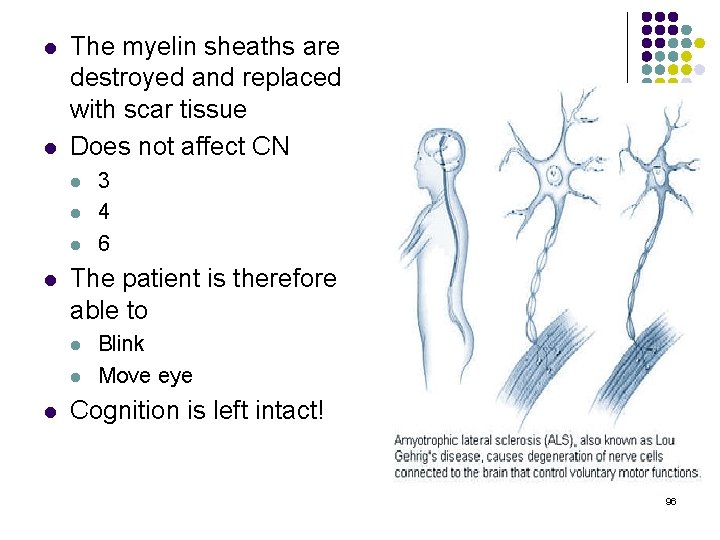
l l The myelin sheaths are destroyed and replaced with scar tissue Does not affect CN l l The patient is therefore able to l l l 3 4 6 Blink Move eye Cognition is left intact! 96
Etiology l Unknown l Men > Women Clinical manifestations l Progressive muscle weakness l Atrophy l Spasity l Dysphagia l Dysarthria l Jaw Clonus l Tongue fasciculation 97
Pathophysiology of ALS l l l Glutamate is the most abundant excitatory neurotransmitter in the CNS. Glutamate is removed from synapses by transport proteins on surrounding astrocytes and nerve terminals. In astrocytes, it is metabolized to glutamine. ALS associated with a loss of the astrocytic glutamate transporter protein excitatory amino acid transporter 2(EAAT 2) and Glu. R 2 receptor subunit. Thus, selective loss of glutamate transporter may cause excitotoxicity in ALS by increasing extracellular levels of glutamate. 98
Pathophysiology of ALS l ALS associated with mutant SOD 1 (cytosolic Cu -Zn SOD). l Thus, the levels of carbonyl proteins in the brain and the levels of free nitrotyrosine in the spinal cord elevate. ALS associated with neurofilament dysfunctions. (mutant heavy chain neurofilament subunit, increased peripherin expression) l 99
Demyelinating Diseases (Multiple Sclerosis) 100
Multiple Sclerosis l l l Focal, chronic, progressive, usually exacerbating and remitting demyelination of CNS tracts. Lesions can occur in a wide variety of locations and give rise to complex symptoms Areas of demyelination are called plaques, and can occur anywhere oligodendrocytes provide myelin sheath 101
Onset l Onset is between 20 and 40 years, rarely before 15 or after 50 l Females: Males 2: 1 102
ETIOLOGY l l Cause is still unknown Identified factors: l Autoimmune causes l l Human Leukocyte Antigens Viral causes l Roseola virus 103
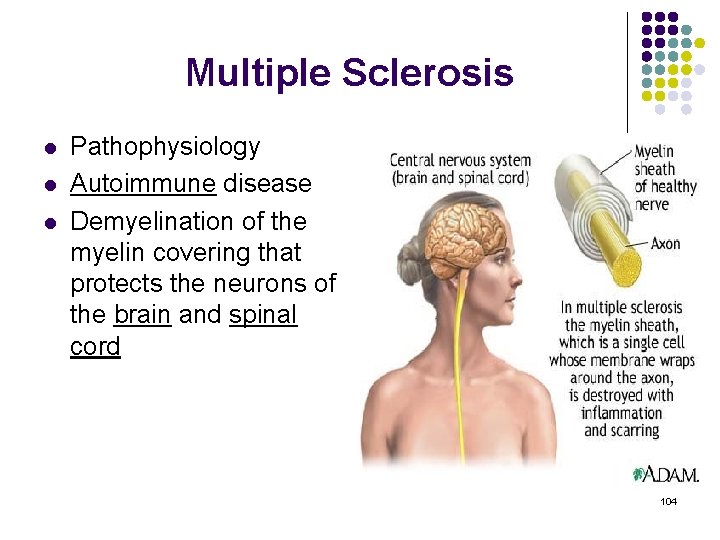
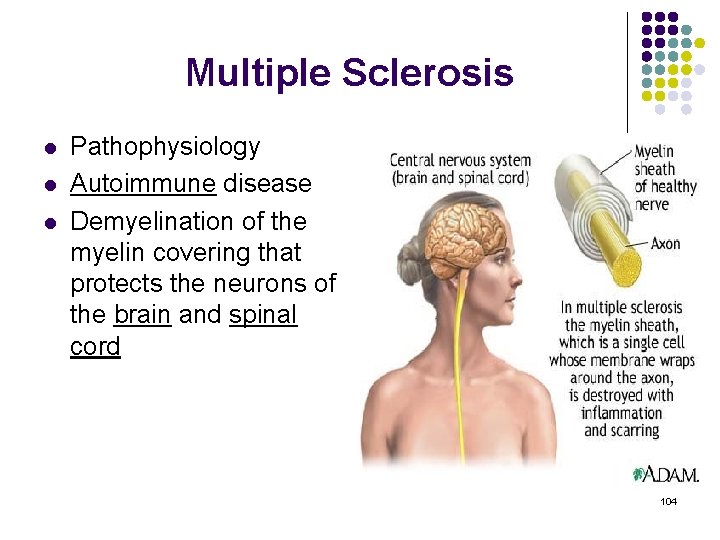
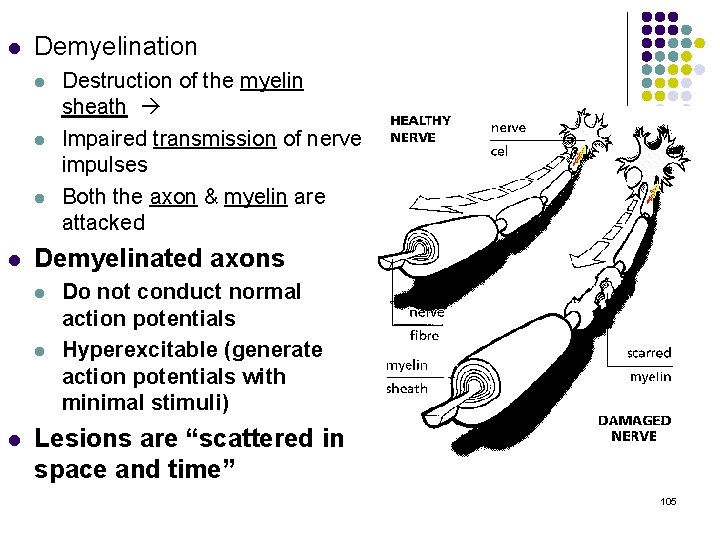
Multiple Sclerosis l l l Pathophysiology Autoimmune disease Demyelination of the myelin covering that protects the neurons of the brain and spinal cord 104
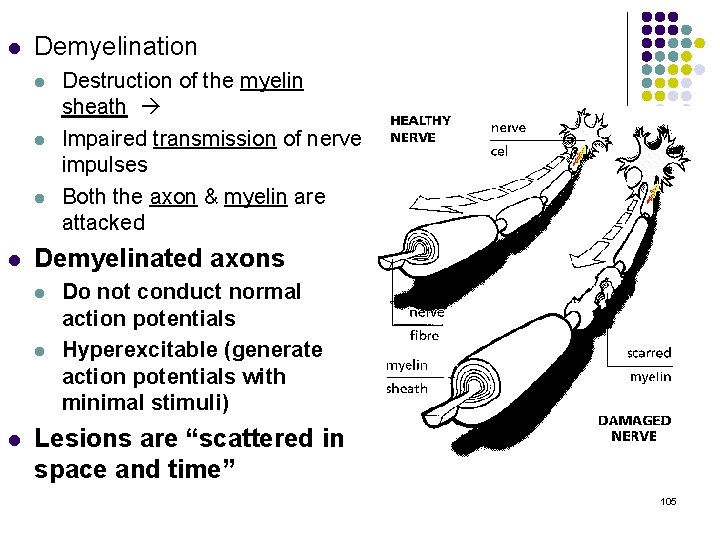
l Demyelination l l Demyelinated axons l l l Destruction of the myelin sheath Impaired transmission of nerve impulses Both the axon & myelin are attacked Do not conduct normal action potentials Hyperexcitable (generate action potentials with minimal stimuli) Lesions are “scattered in space and time” 105
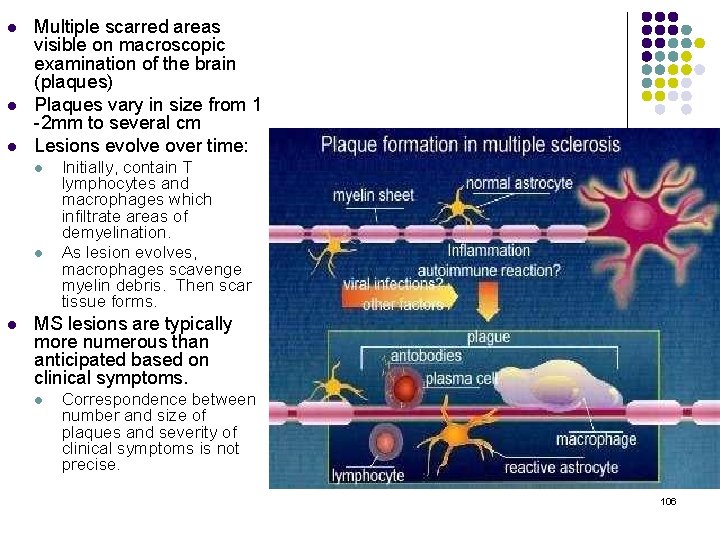
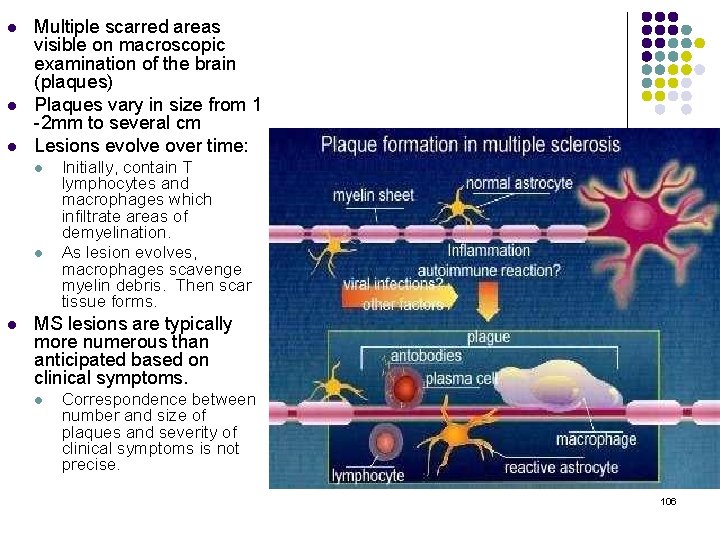
l l l Multiple scarred areas visible on macroscopic examination of the brain (plaques) Plaques vary in size from 1 -2 mm to several cm Lesions evolve over time: l l l Initially, contain T lymphocytes and macrophages which infiltrate areas of demyelination. As lesion evolves, macrophages scavenge myelin debris. Then scar tissue forms. MS lesions are typically more numerous than anticipated based on clinical symptoms. l Correspondence between number and size of plaques and severity of clinical symptoms is not precise. 106
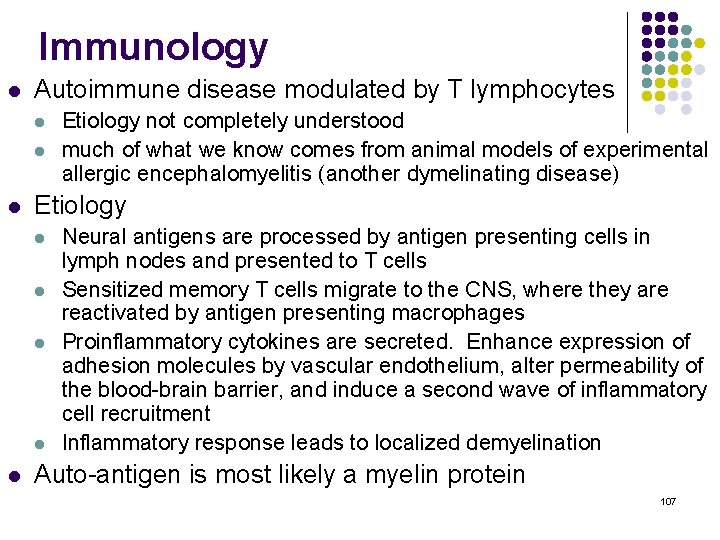
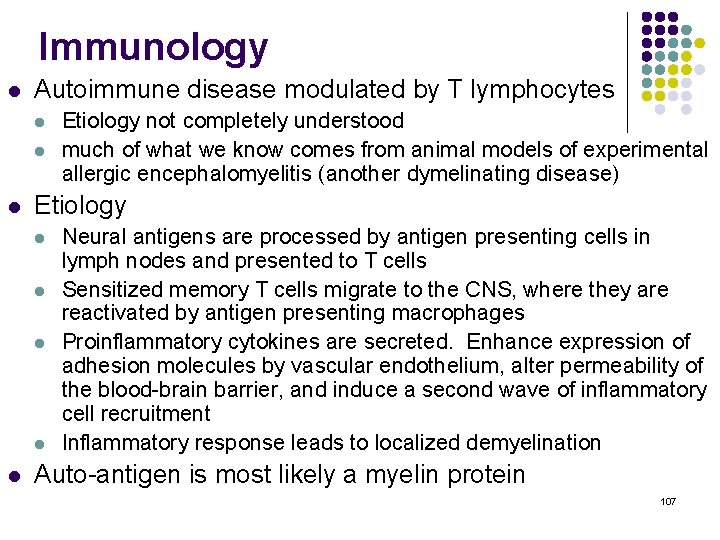
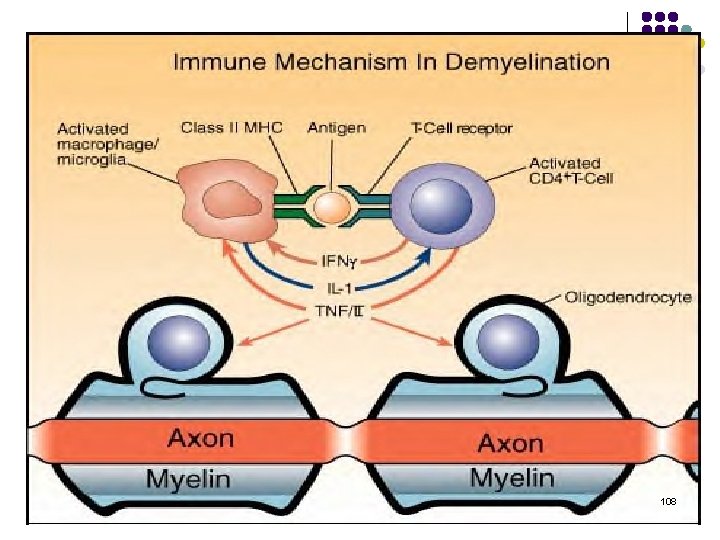
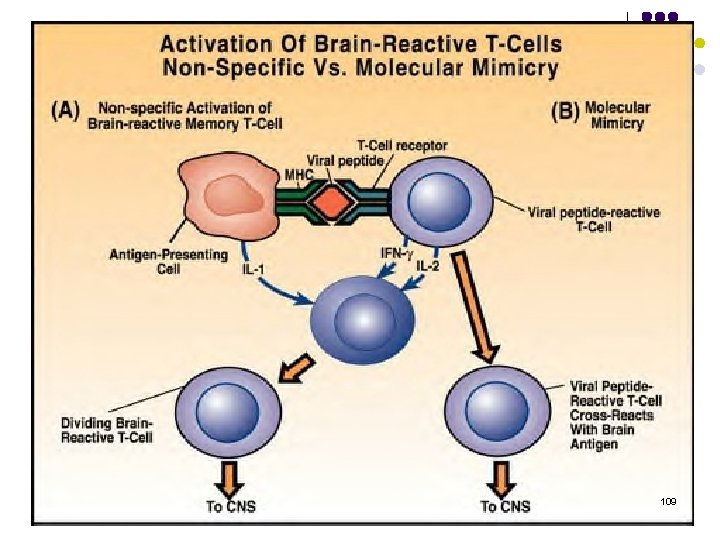
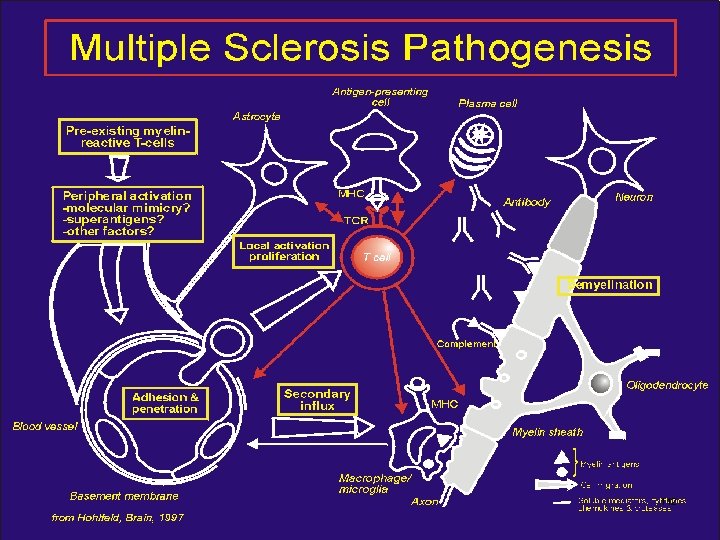
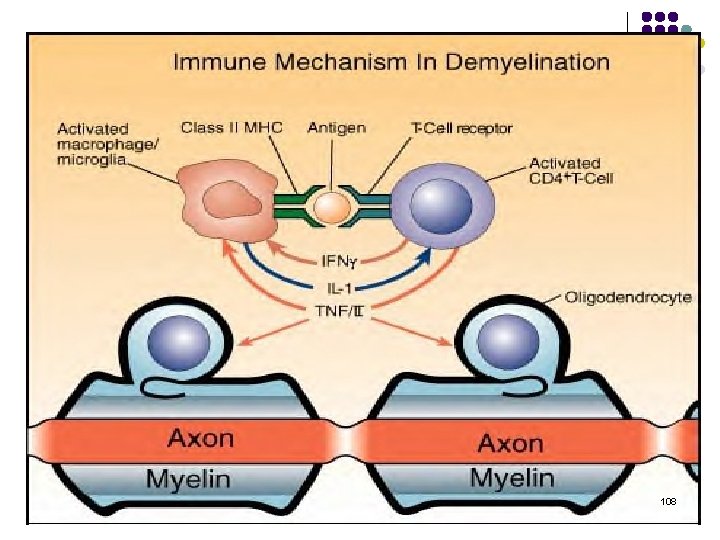
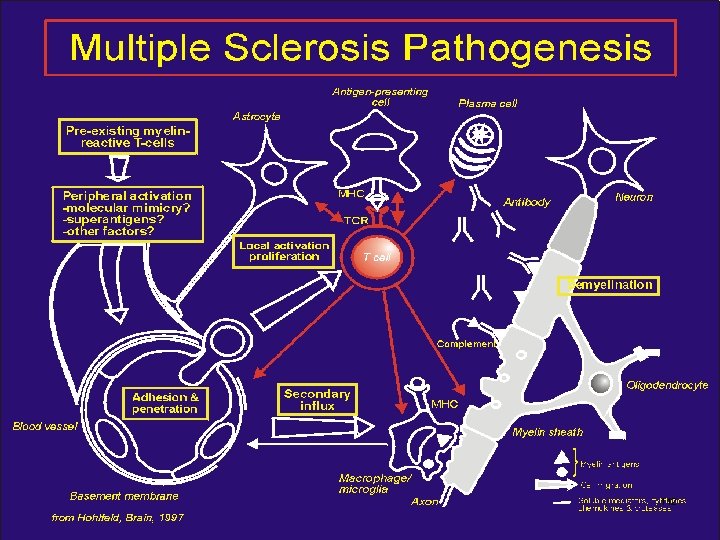
Immunology l Autoimmune disease modulated by T lymphocytes l l l Etiology not completely understood much of what we know comes from animal models of experimental allergic encephalomyelitis (another dymelinating disease) Neural antigens are processed by antigen presenting cells in lymph nodes and presented to T cells Sensitized memory T cells migrate to the CNS, where they are reactivated by antigen presenting macrophages Proinflammatory cytokines are secreted. Enhance expression of adhesion molecules by vascular endothelium, alter permeability of the blood-brain barrier, and induce a second wave of inflammatory cell recruitment Inflammatory response leads to localized demyelination Auto-antigen is most likely a myelin protein 107
108
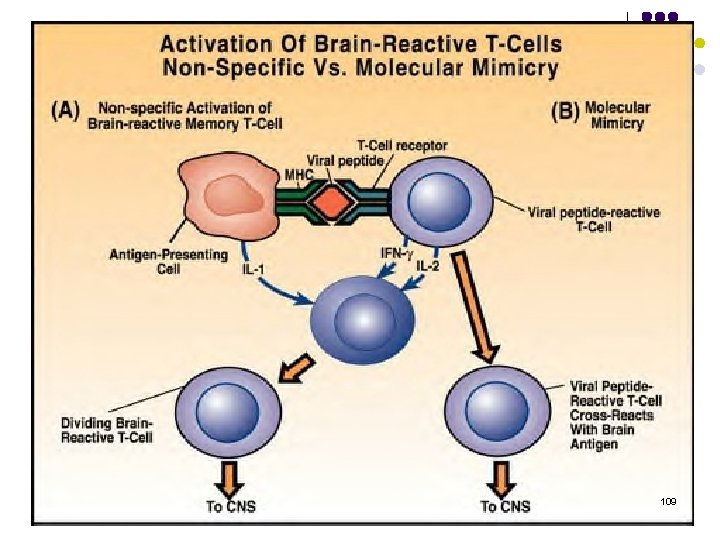
109
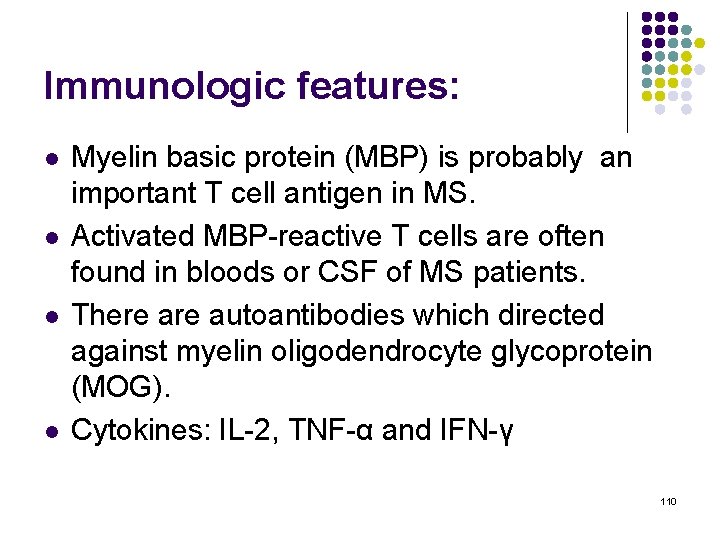
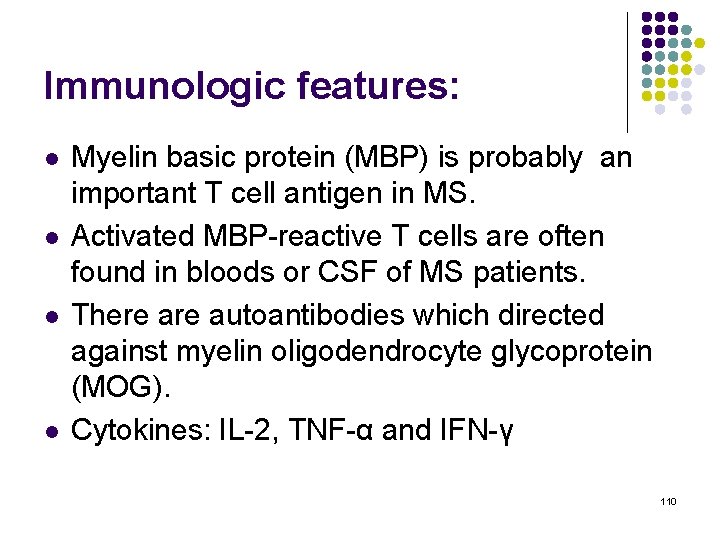
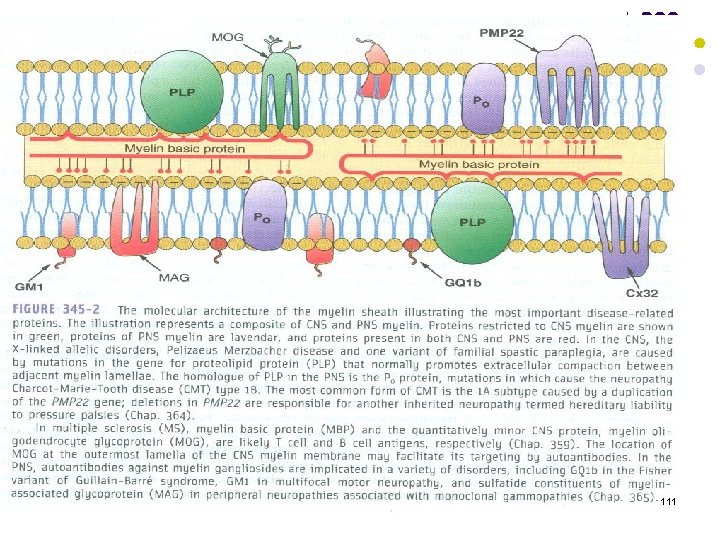
Immunologic features: l l Myelin basic protein (MBP) is probably an important T cell antigen in MS. Activated MBP-reactive T cells are often found in bloods or CSF of MS patients. There autoantibodies which directed against myelin oligodendrocyte glycoprotein (MOG). Cytokines: IL-2, TNF-α and IFN-γ 110
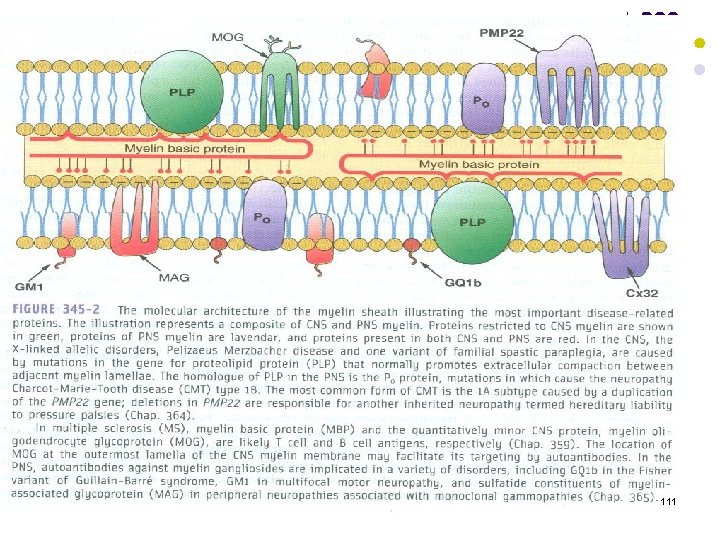
111
112
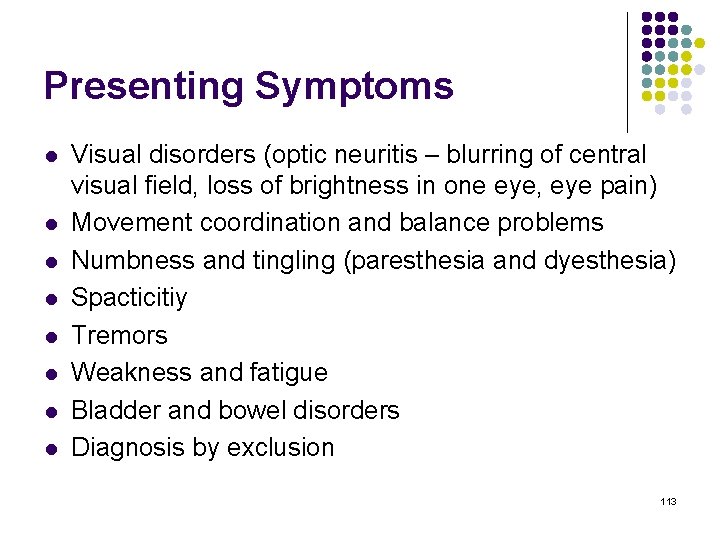
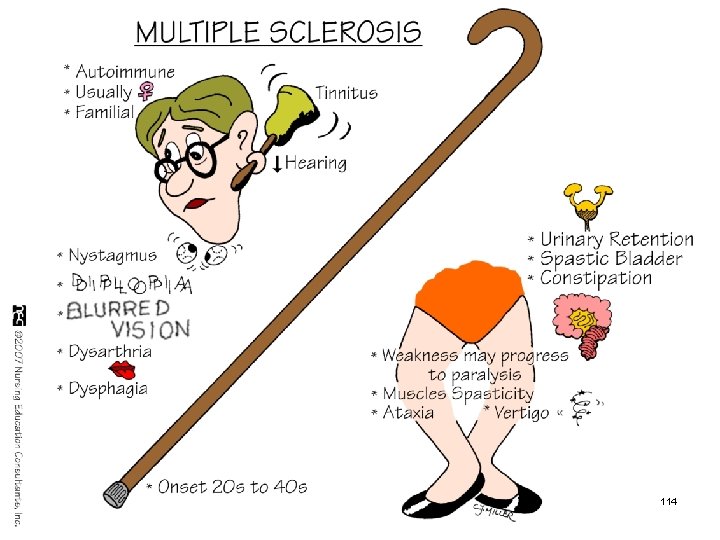
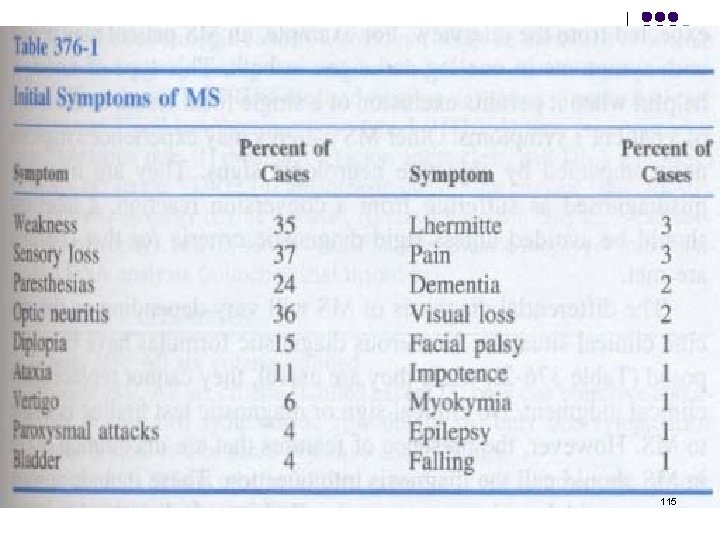
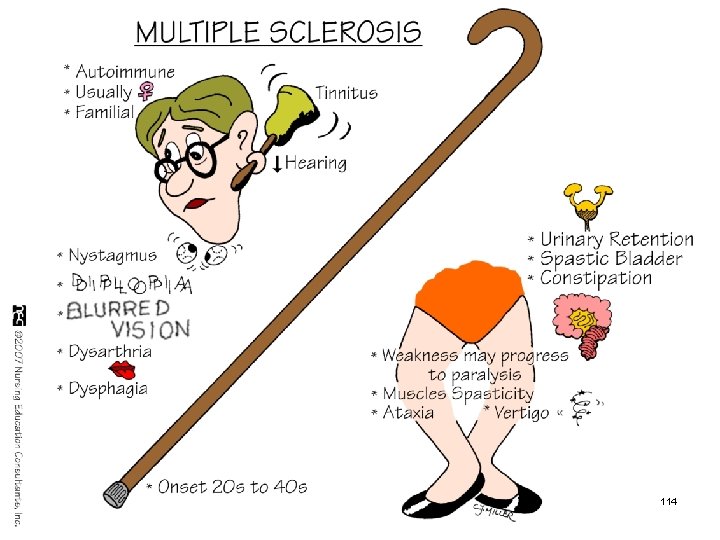
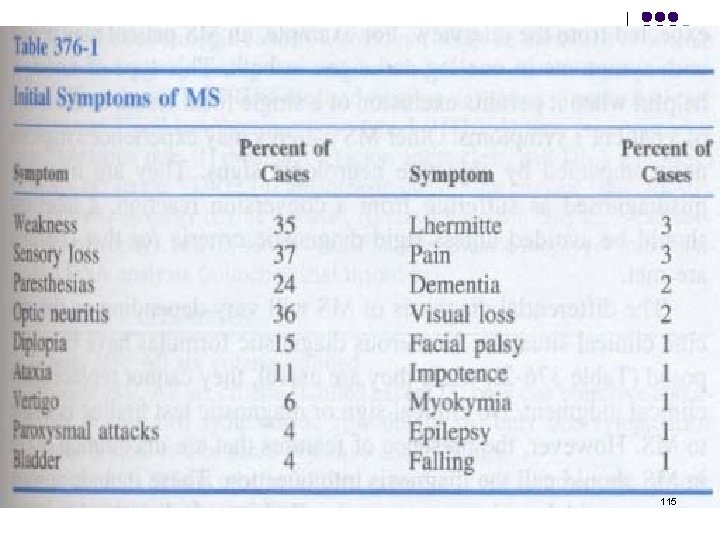
Presenting Symptoms l l l l Visual disorders (optic neuritis – blurring of central visual field, loss of brightness in one eye, eye pain) Movement coordination and balance problems Numbness and tingling (paresthesia and dyesthesia) Spacticitiy Tremors Weakness and fatigue Bladder and bowel disorders Diagnosis by exclusion 113
114
115
Neuromuscular Junction Diseases (Myasthenia Gravis) 116
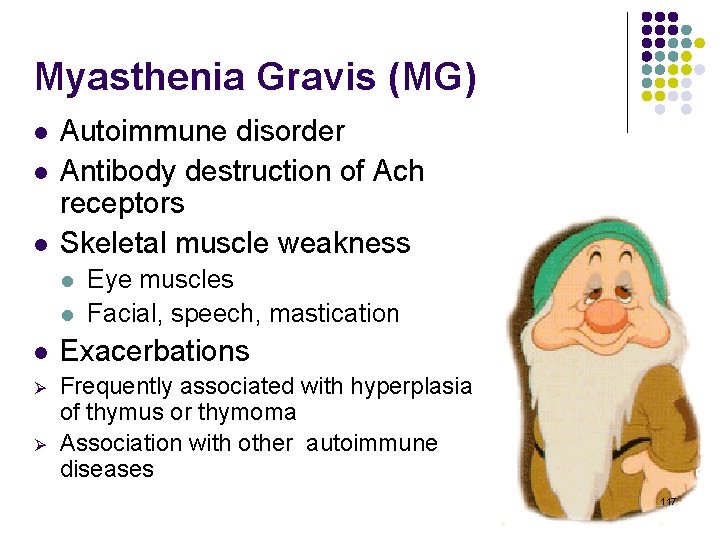
Myasthenia Gravis (MG) l l l Autoimmune disorder Antibody destruction of Ach receptors Skeletal muscle weakness l l Eye muscles Facial, speech, mastication l Exacerbations Ø Frequently associated with hyperplasia of thymus or thymoma Association with other autoimmune diseases Ø 117
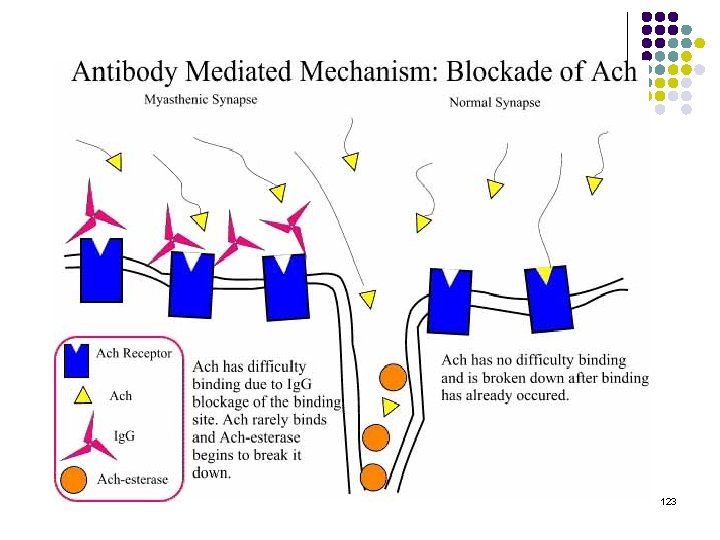
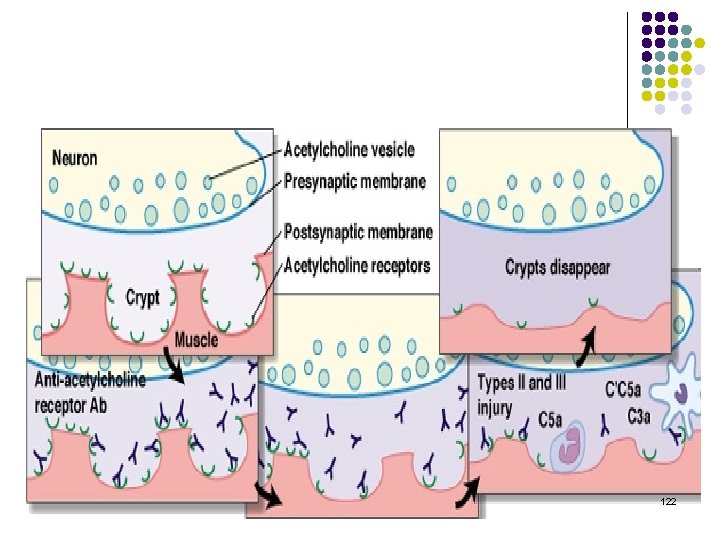
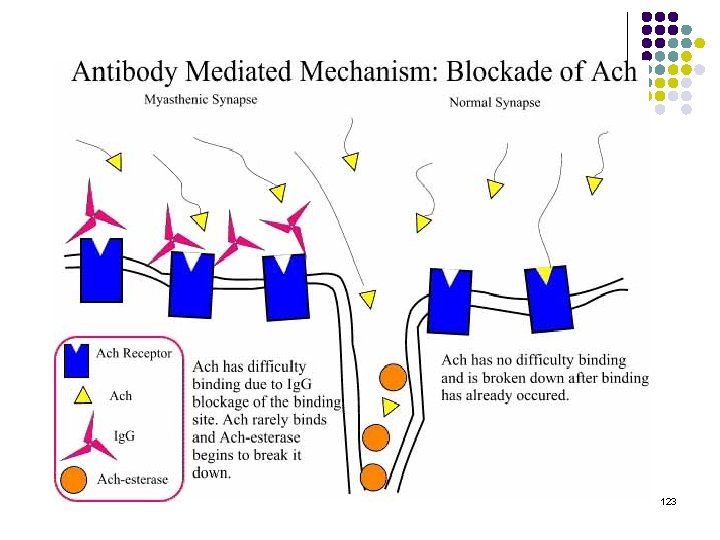
Neuromuscular Junction (NMJ) l Components: l l l Presynaptic membrane Postsynaptic membrane Synaptic cleft Presynaptic membrane contains vesicles with Acetylcholine (ACh) which are released into synaptic cleft in a calcium dependent manner ACh attaches to ACh receptors (ACh. R) on postsynaptic membrane 118
Neuromuscular Junction (NMJ) l The Acetylcholine receptor (ACh. R) is a sodium channel that opens when bound by ACh l l There is a partial depolarization of the postsynaptic membrane and this causes an excitatory postsynaptic potential (EPSP) If enough sodium channels open and a threshold potential is reached, a muscle action potential is generated in the postsynaptic membrane 119
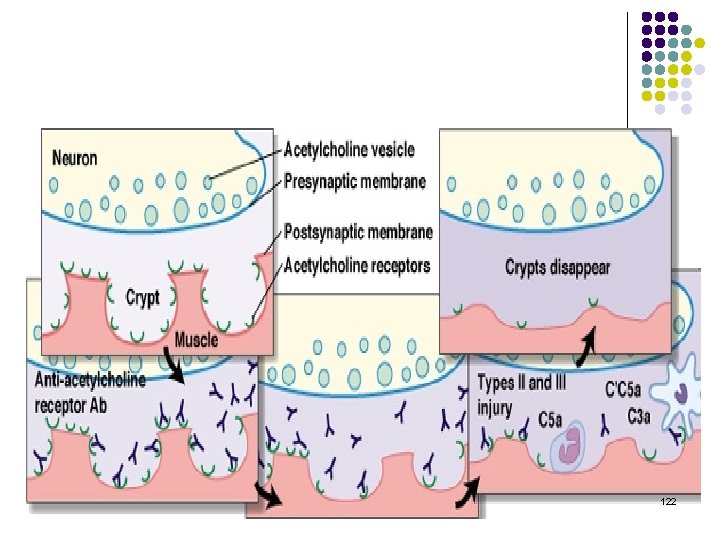
Pathophysiology l l In MG, antibodies are directed toward the acetylcholine receptor at the neuromuscular junction of skeletal muscles Results in: l l l Decreased number of nicotinic acetylcholine receptors at the motor end-plate Reduced postsynaptic membrane folds Widened synaptic cleft 120
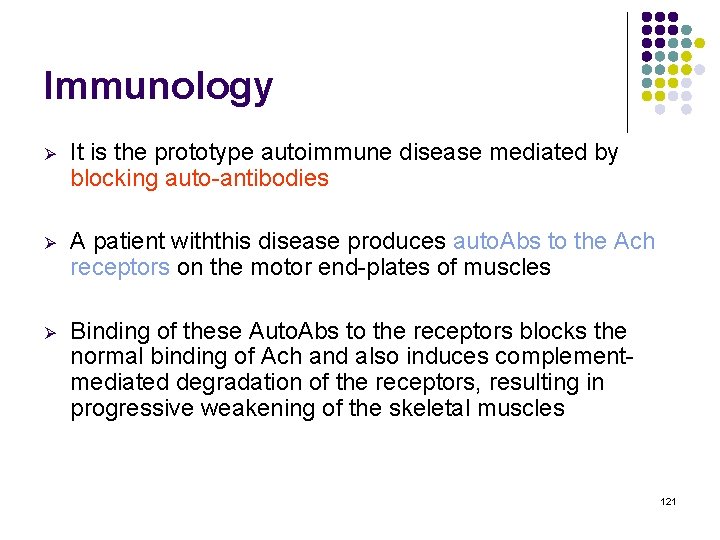
Immunology Ø It is the prototype autoimmune disease mediated by blocking auto-antibodies Ø A patient withthis disease produces auto. Abs to the Ach receptors on the motor end-plates of muscles Ø Binding of these Auto. Abs to the receptors blocks the normal binding of Ach and also induces complementmediated degradation of the receptors, resulting in progressive weakening of the skeletal muscles 121
122
123
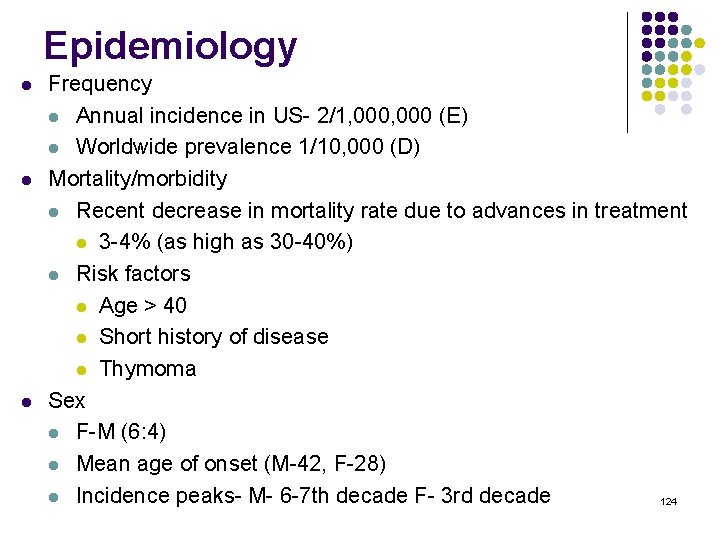
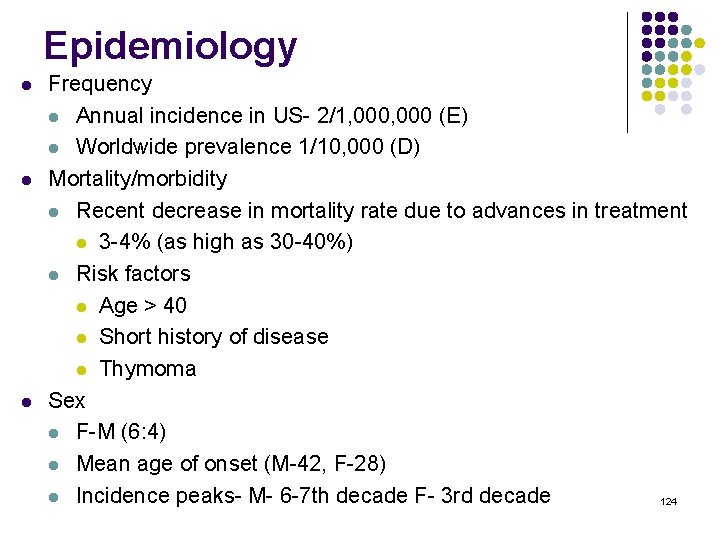
Epidemiology l l l Frequency l Annual incidence in US- 2/1, 000 (E) l Worldwide prevalence 1/10, 000 (D) Mortality/morbidity l Recent decrease in mortality rate due to advances in treatment l 3 -4% (as high as 30 -40%) l Risk factors l Age > 40 l Short history of disease l Thymoma Sex l F-M (6: 4) l Mean age of onset (M-42, F-28) l Incidence peaks- M- 6 -7 th decade F- 3 rd decade 124

Clinical presentation l Muscle strength l l l Facial muscle weakness Bulbar muscle weakness Limb muscle weakness Respiratory weakness Ocular muscle weakness 125

Clinical presentation l Facial muscle weakness is almost always present l l l Ptosis and bilateral facial muscle weakness Sclera below limbus may be exposed due to weak lower lids Occular muscle weakness l Asymmetric l l Usually affects more than one extraocular muscle and is not limited to muscles innervated by one cranial nerve Weakness of lateral and medial recti may produce a pseudointernuclear opthalmoplegia § l l Limited adduction of one eye with nystagmus of the abducting eye on attempted lateral gaze Ptosis caused by eyelid weakness Diplopia is very common 126
Meningitis (Acute Bacterial Meningitis) 127
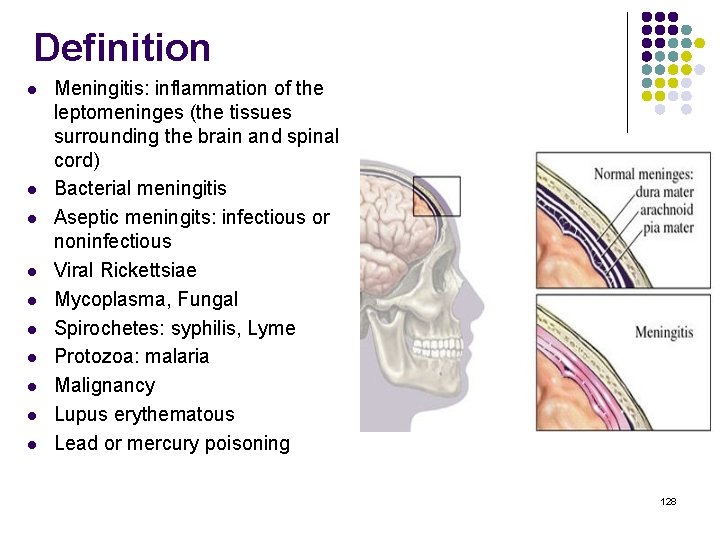
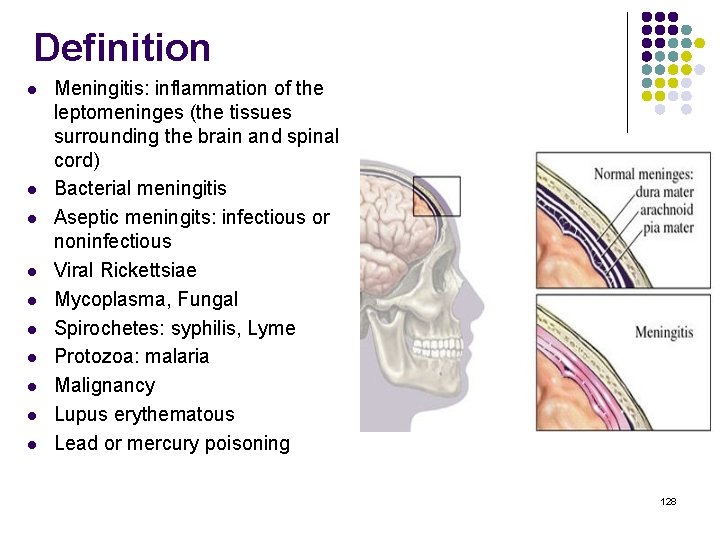
Definition l l l l l Meningitis: inflammation of the leptomeninges (the tissues surrounding the brain and spinal cord) Bacterial meningitis Aseptic meningits: infectious or noninfectious Viral Rickettsiae Mycoplasma, Fungal Spirochetes: syphilis, Lyme Protozoa: malaria Malignancy Lupus erythematous Lead or mercury poisoning 128
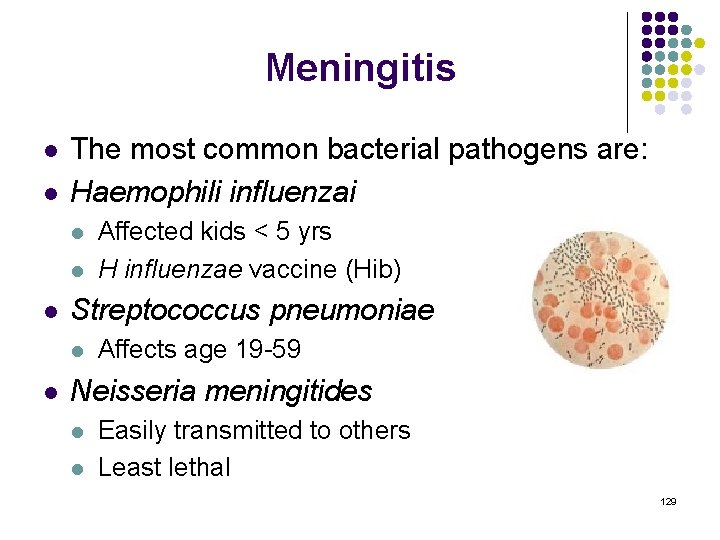
Meningitis l l The most common bacterial pathogens are: Haemophili influenzai l l l Streptococcus pneumoniae l l Affected kids < 5 yrs H influenzae vaccine (Hib) Affects age 19 -59 Neisseria meningitides l l Easily transmitted to others Least lethal 129
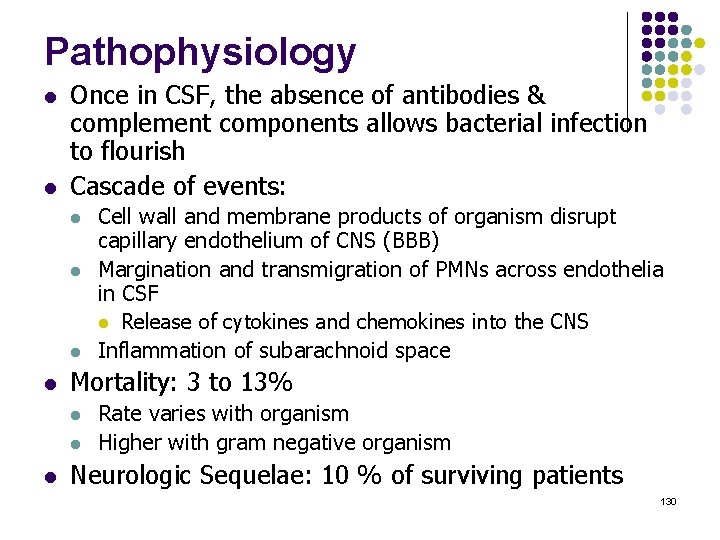
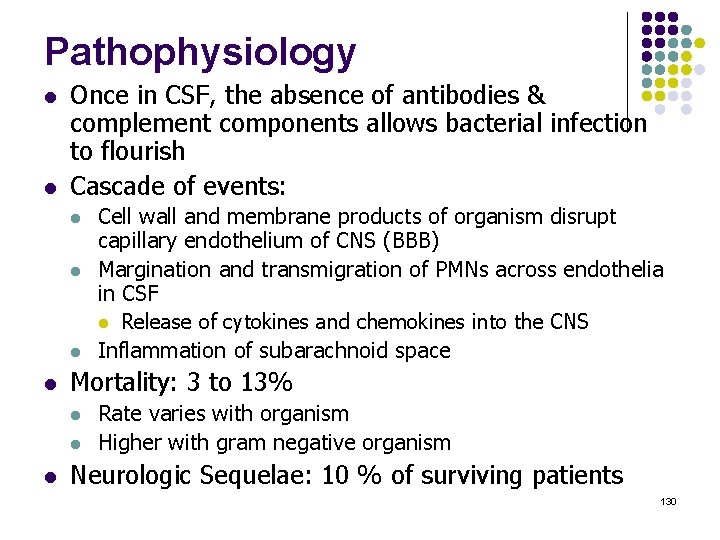
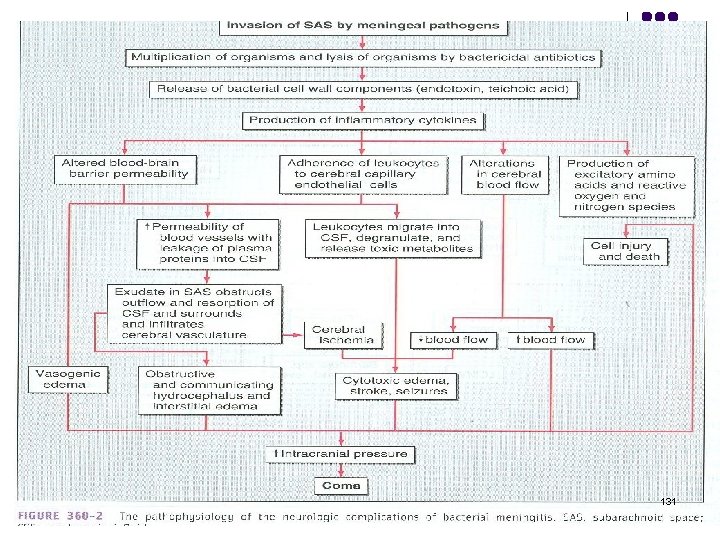
Pathophysiology l l Once in CSF, the absence of antibodies & complement components allows bacterial infection to flourish Cascade of events: l l Mortality: 3 to 13% l l l Cell wall and membrane products of organism disrupt capillary endothelium of CNS (BBB) Margination and transmigration of PMNs across endothelia in CSF l Release of cytokines and chemokines into the CNS Inflammation of subarachnoid space Rate varies with organism Higher with gram negative organism Neurologic Sequelae: 10 % of surviving patients 130
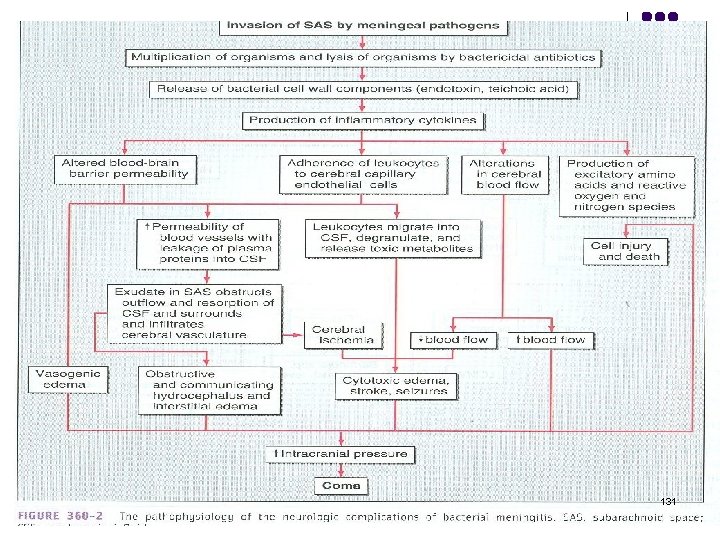
131
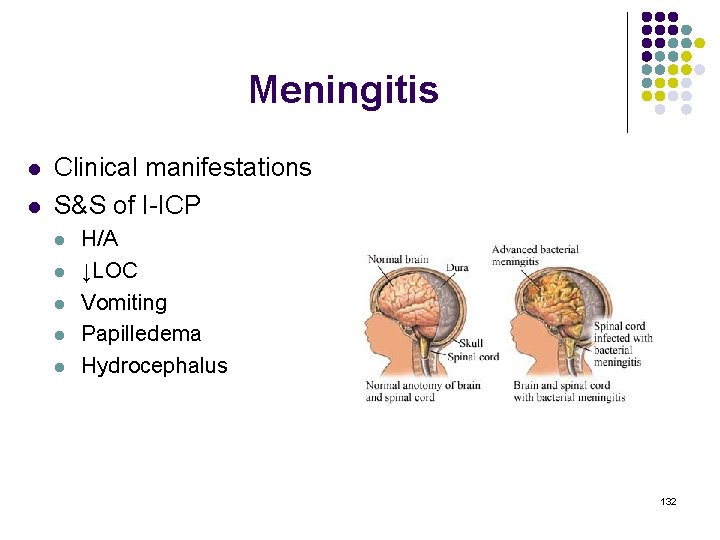
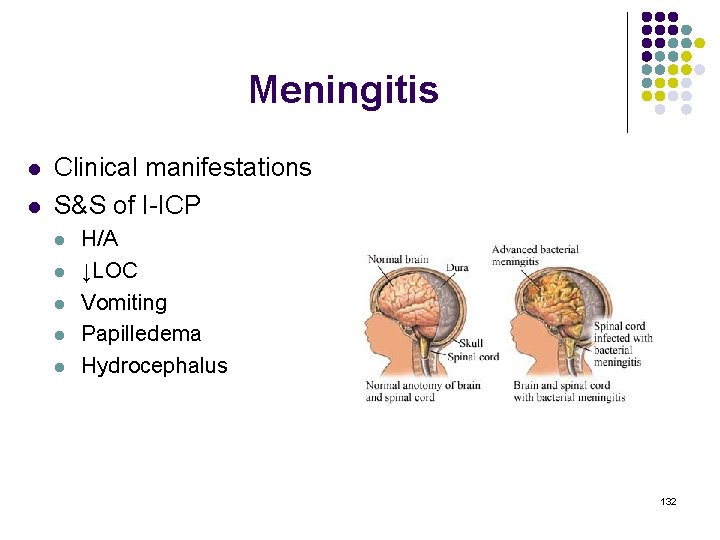
Meningitis l l Clinical manifestations S&S of I-ICP l l l H/A ↓LOC Vomiting Papilledema Hydrocephalus 132
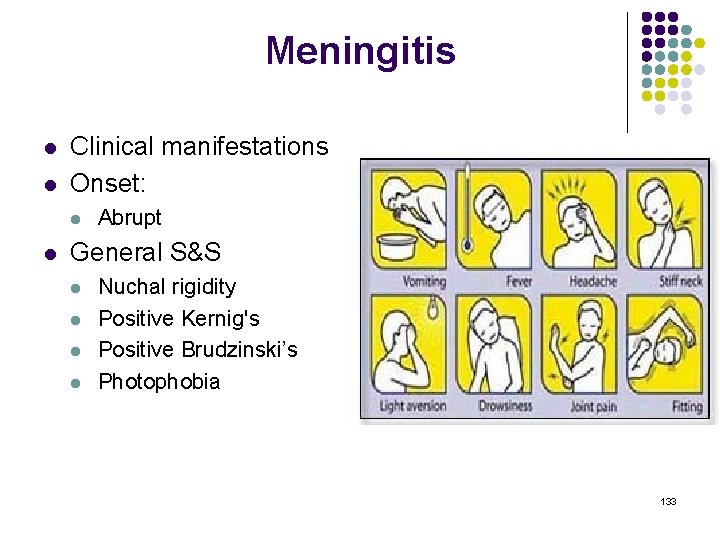
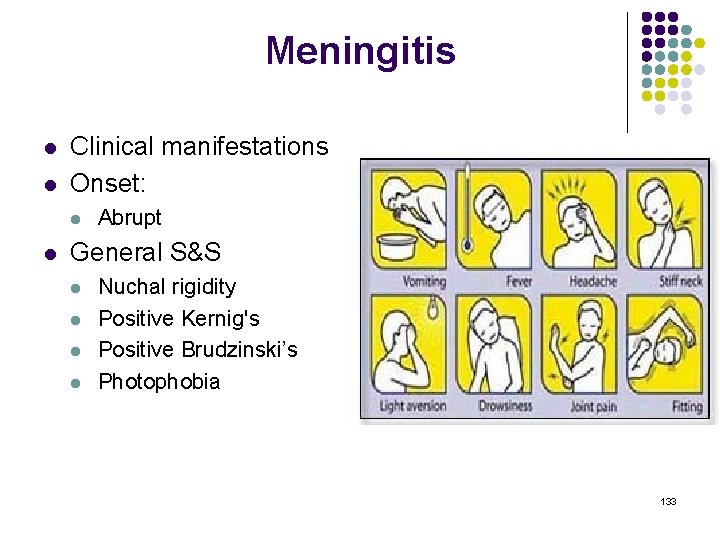
Meningitis l l Clinical manifestations Onset: l l Abrupt General S&S l l Nuchal rigidity Positive Kernig's Positive Brudzinski’s Photophobia 133
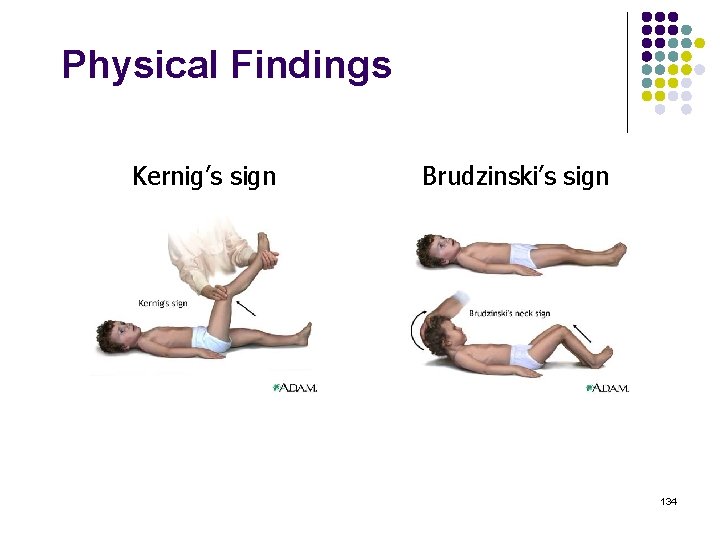
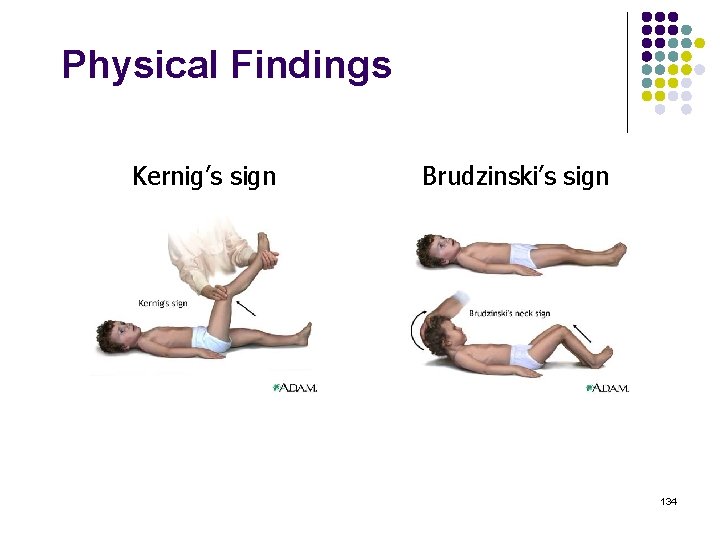
Physical Findings Kernig’s sign Brudzinski’s sign 134
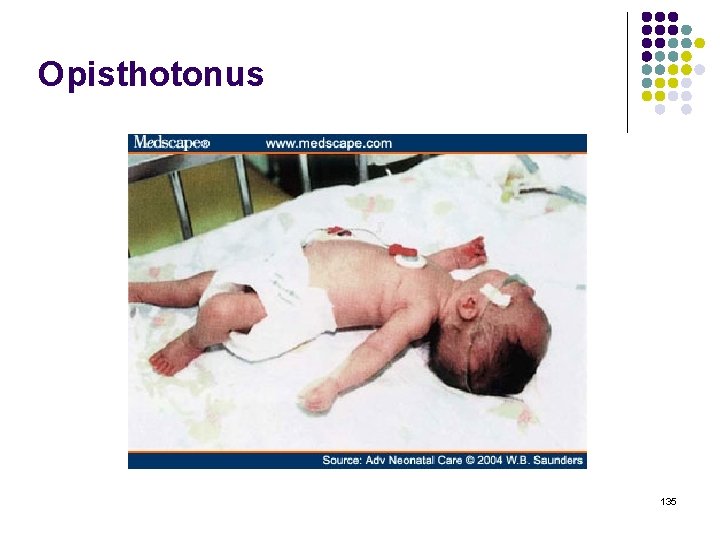
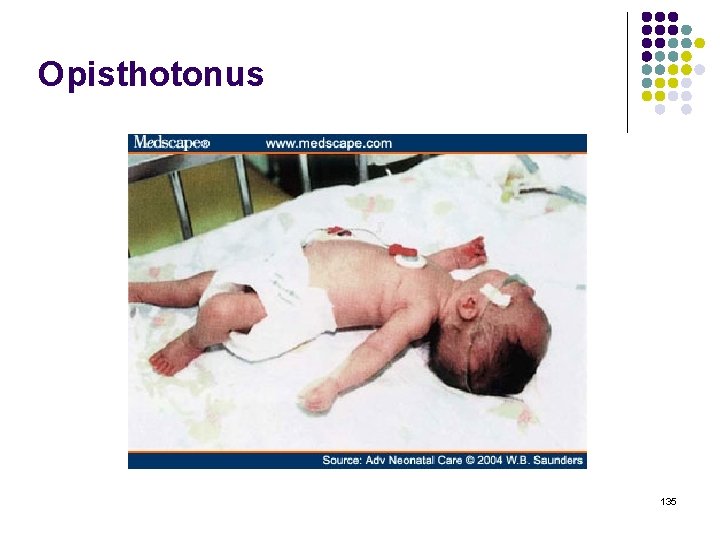
Opisthotonus 135
Stress and Disease 136
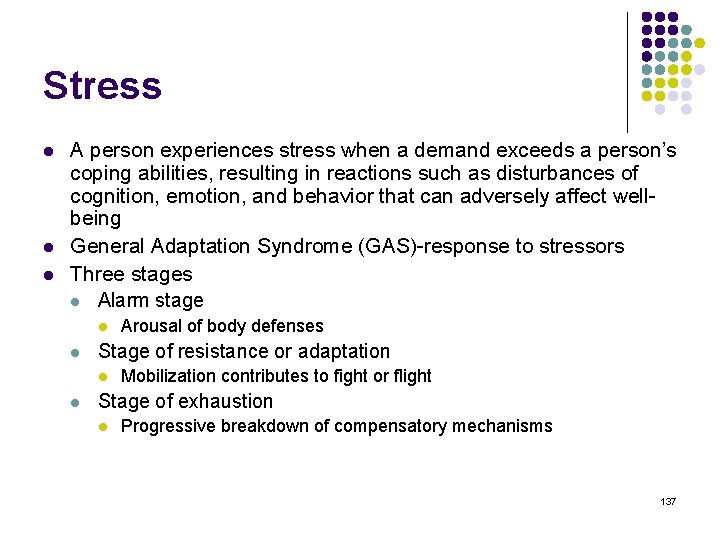
Stress l l l A person experiences stress when a demand exceeds a person’s coping abilities, resulting in reactions such as disturbances of cognition, emotion, and behavior that can adversely affect wellbeing General Adaptation Syndrome (GAS)-response to stressors Three stages l Alarm stage l l Stage of resistance or adaptation l l Arousal of body defenses Mobilization contributes to fight or flight Stage of exhaustion l Progressive breakdown of compensatory mechanisms 137
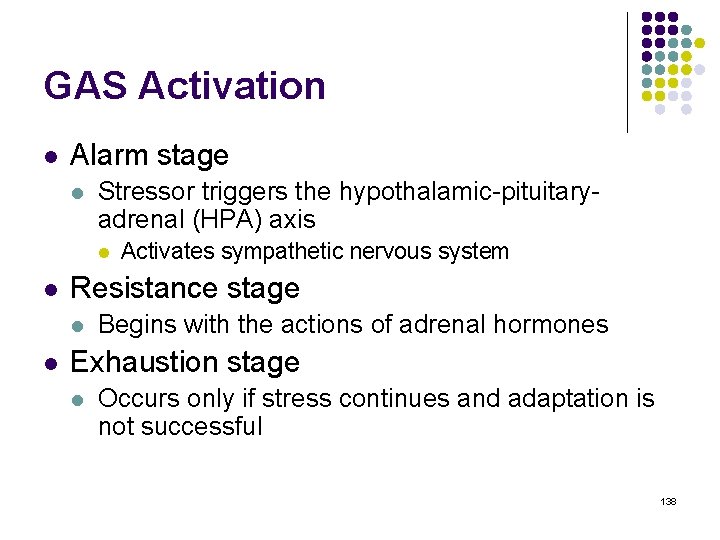
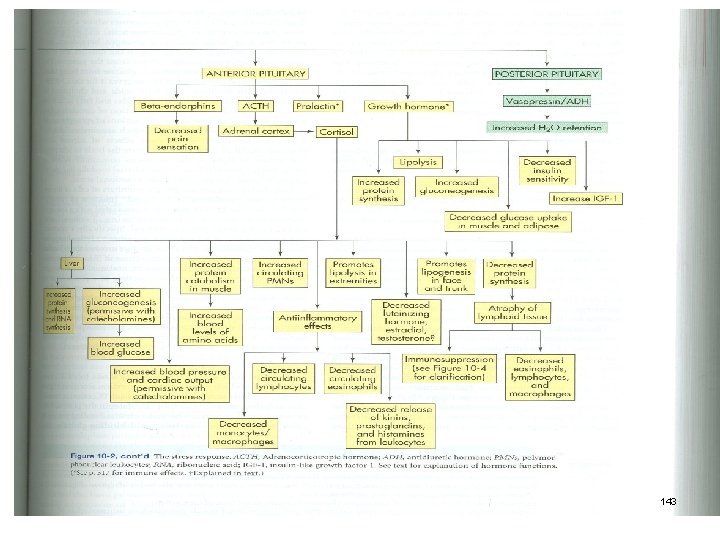
GAS Activation l Alarm stage l Stressor triggers the hypothalamic-pituitaryadrenal (HPA) axis l l Resistance stage l l Activates sympathetic nervous system Begins with the actions of adrenal hormones Exhaustion stage l Occurs only if stress continues and adaptation is not successful 138

Psychoneuroimmunologic Mediators l l Interactions of consciousness, the brain and spinal cord, and the body’s defense mechanisms Corticotropin-releasing hormone (CRH) is released from the hypothalamus CRH is also released peripherally at inflammatory sites Immune modulation by psychosocial stressors leads directly to health outcomes 139
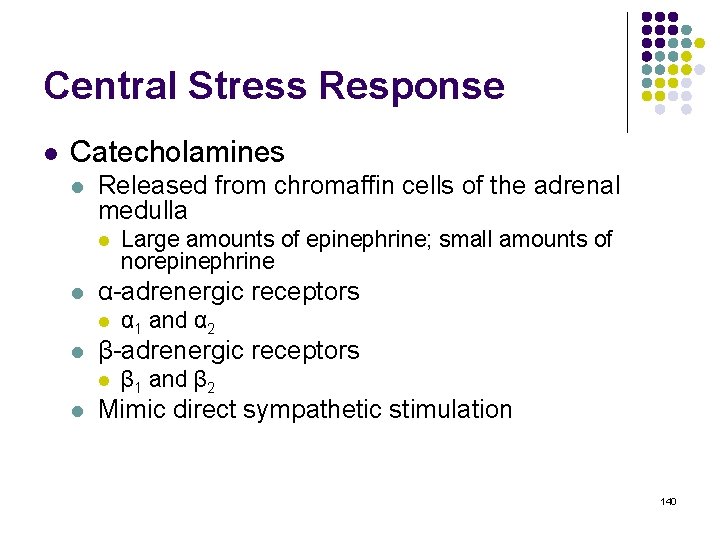
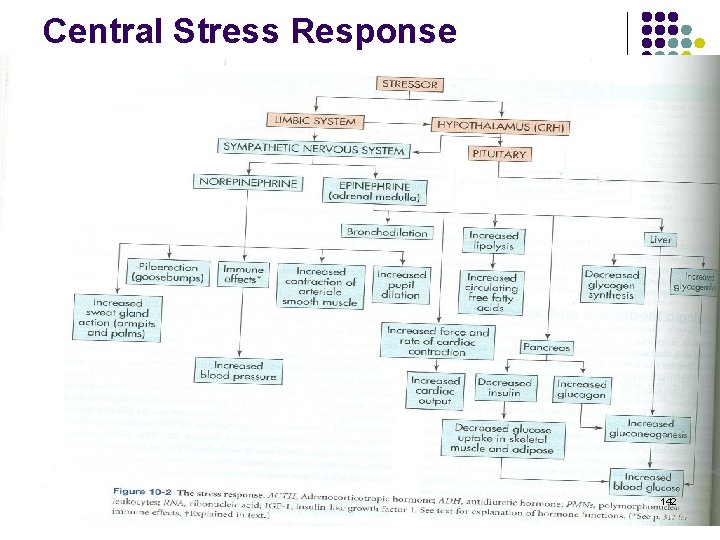
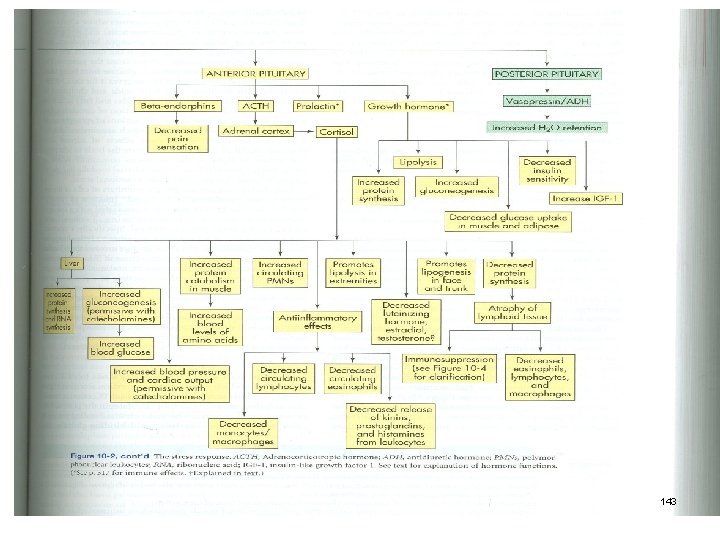
Central Stress Response l Catecholamines l Released from chromaffin cells of the adrenal medulla l l α-adrenergic receptors l l α 1 and α 2 β-adrenergic receptors l l Large amounts of epinephrine; small amounts of norepinephrine β 1 and β 2 Mimic direct sympathetic stimulation 140
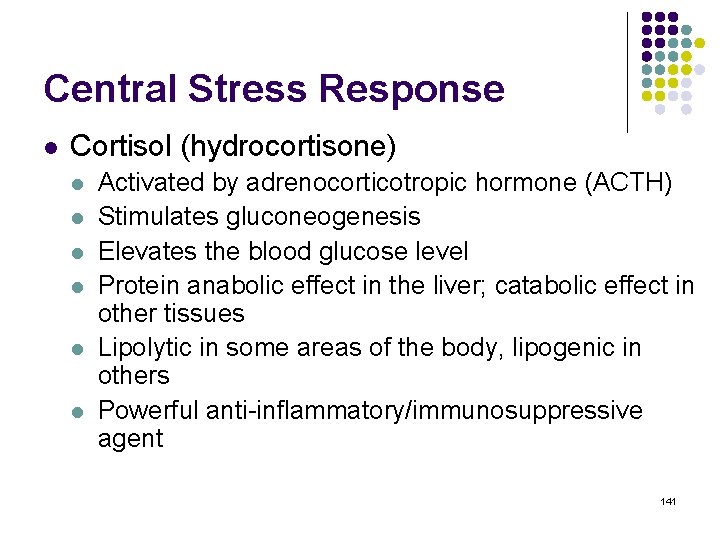
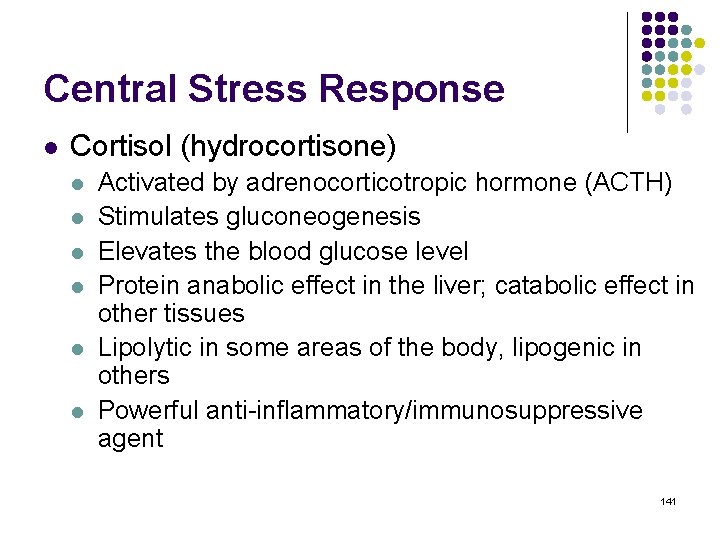
Central Stress Response l Cortisol (hydrocortisone) l l l Activated by adrenocorticotropic hormone (ACTH) Stimulates gluconeogenesis Elevates the blood glucose level Protein anabolic effect in the liver; catabolic effect in other tissues Lipolytic in some areas of the body, lipogenic in others Powerful anti-inflammatory/immunosuppressive agent 141
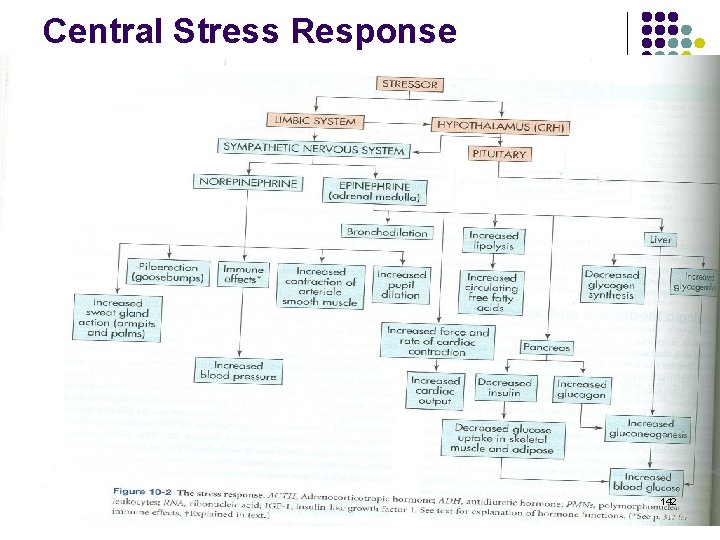
Central Stress Response 142
143

Central Stress Response 144
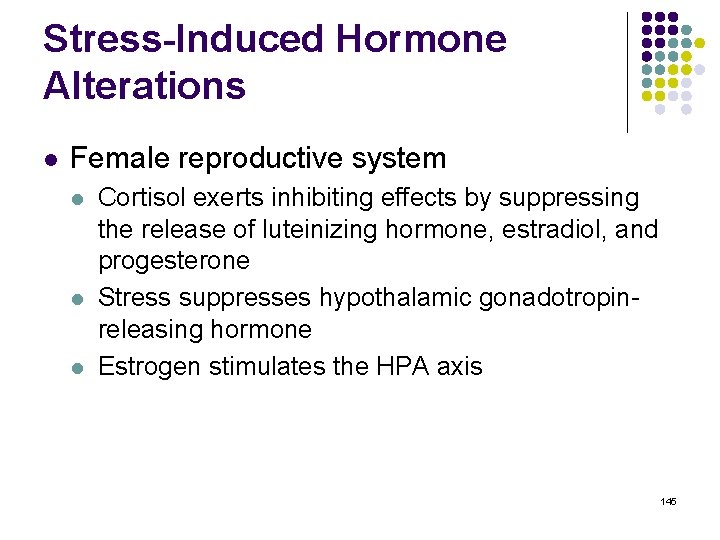
Stress-Induced Hormone Alterations l Female reproductive system l l l Cortisol exerts inhibiting effects by suppressing the release of luteinizing hormone, estradiol, and progesterone Stress suppresses hypothalamic gonadotropinreleasing hormone Estrogen stimulates the HPA axis 145
Stress-Induced Hormone Alterations l Endorphins and enkephalins l l Proteins found in the brain that have pain-relieving capabilities In a number of conditions, individuals not only experience insensitivity to pain but also increased feelings of excitement, positive well-being, and euphoria 146
Stress-Induced Hormone Alterations l Growth hormone (somatotropin) l l l Produced by the anterior pituitary and by lymphocytes and mononuclear phagocytic cells Affects protein, lipid, and carbohydrate metabolism and counters the effects of insulin Enhances immune function 147
Stress-Induced Hormone Alterations l Prolactin l l Released from the anterior pituitary Necessary for lactation and breast development Prolactin levels in the plasma increase as a result of stressful stimuli Oxytocin l l l Produced by the hypothalamus Produced during orgasm in both sexes May promote reduced anxiety 148
Stress-Induced Hormone Alterations l Testosterone l l l Secreted by Leydig cells Regulates male secondary sex characteristics and libido Testosterone levels decrease due to stressful stimuli 149
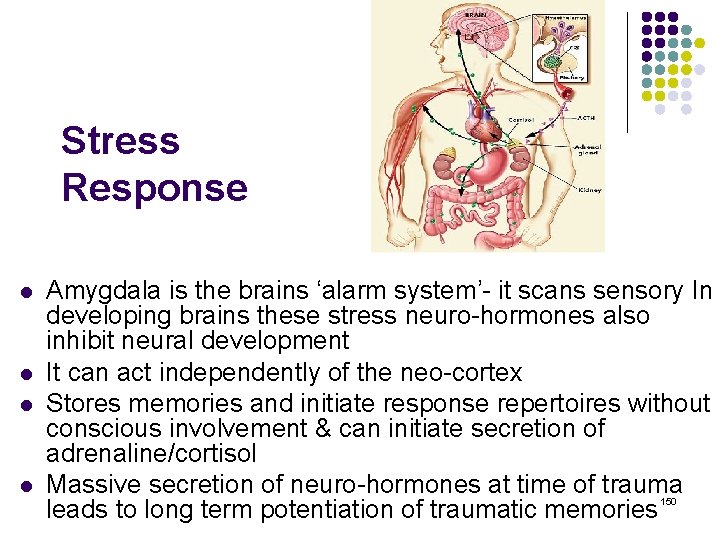
Stress Response l l Amygdala is the brains ‘alarm system’- it scans sensory In developing brains these stress neuro-hormones also inhibit neural development It can act independently of the neo-cortex Stores memories and initiate response repertoires without conscious involvement & can initiate secretion of adrenaline/cortisol Massive secretion of neuro-hormones at time of trauma leads to long term potentiation of traumatic memories 150
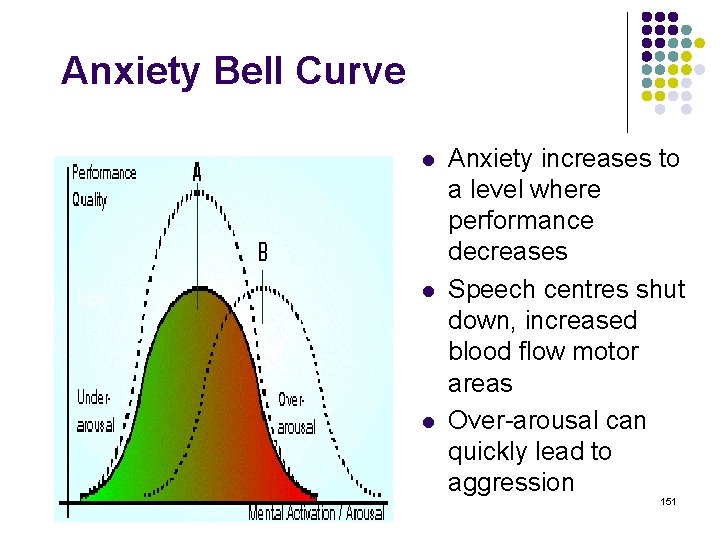
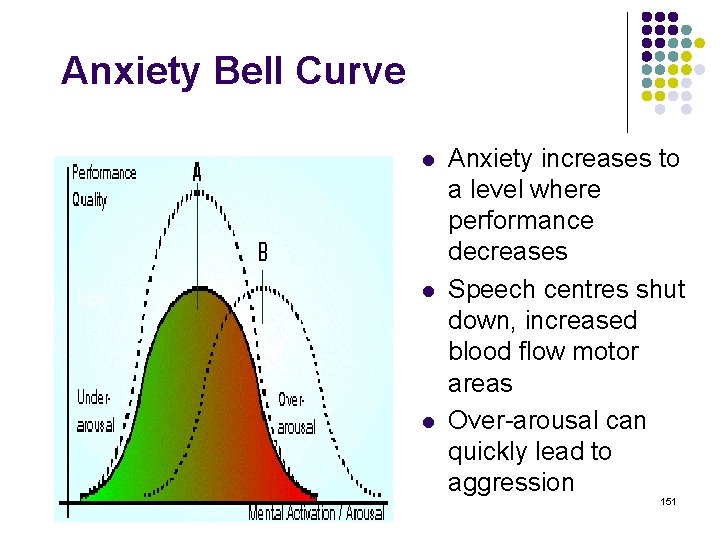
Anxiety Bell Curve l l l Anxiety increases to a level where performance decreases Speech centres shut down, increased blood flow motor areas Over-arousal can quickly lead to aggression 151
Stress, Personality, Coping, and Illness l l A stressor for one person may not be a stressor for another Psychologic distress l l General state of unpleasant arousal after life events that manifests as physiologic, emotional, cognitive, and behavior changes Coping l Managing stressful demands and challenges that are appraised as taxing or exceeding the resources of the person 152
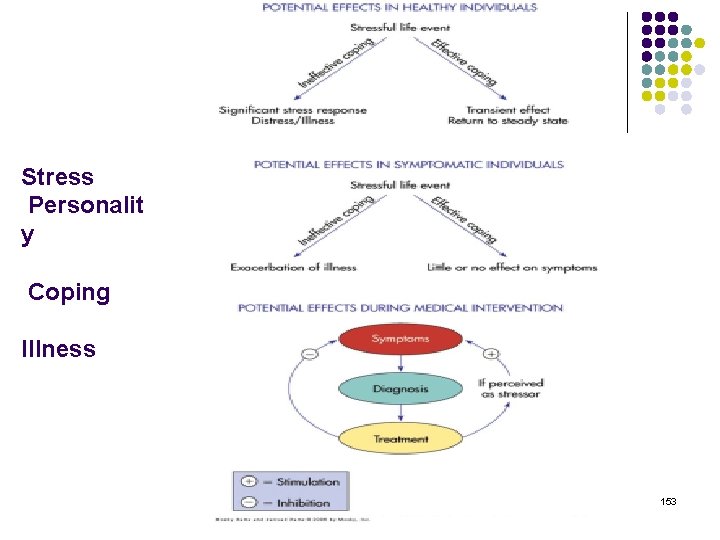
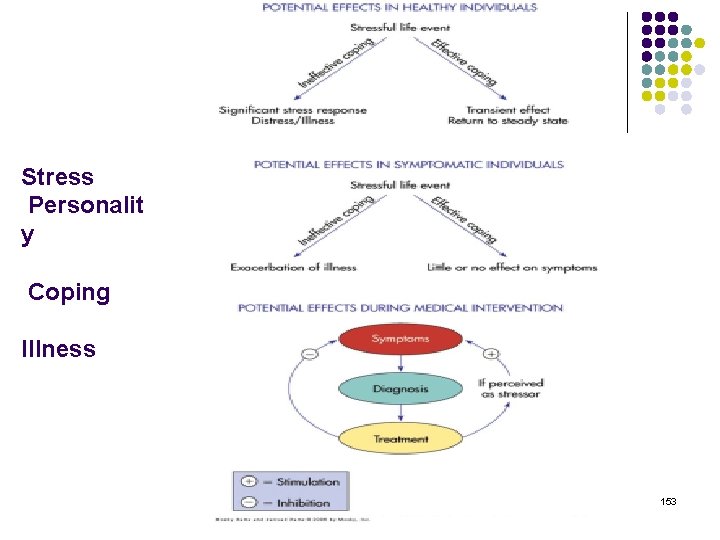
Stress Personalit y Coping Illness 153
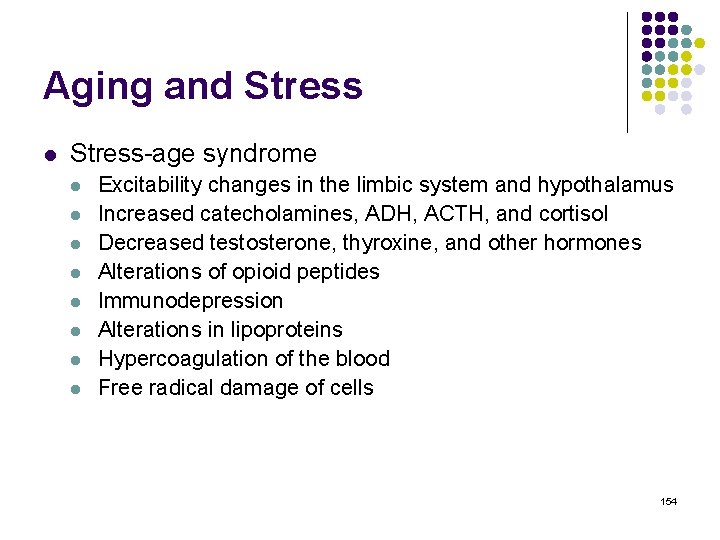
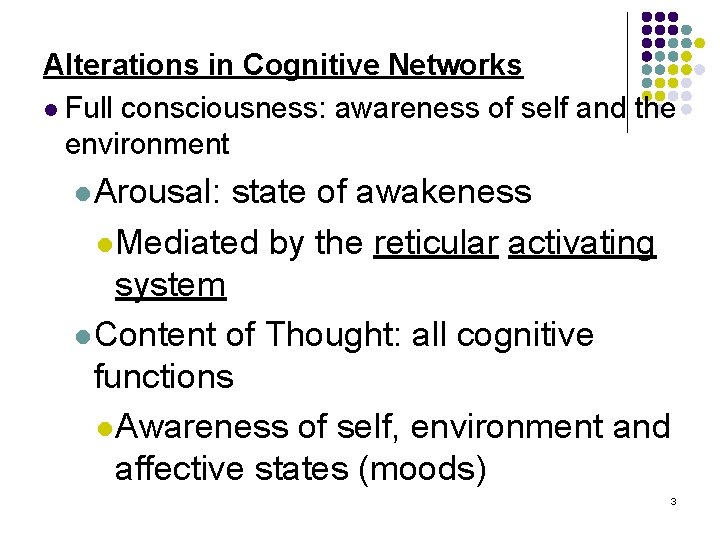
Aging and Stress l Stress-age syndrome l l l l Excitability changes in the limbic system and hypothalamus Increased catecholamines, ADH, ACTH, and cortisol Decreased testosterone, thyroxine, and other hormones Alterations of opioid peptides Immunodepression Alterations in lipoproteins Hypercoagulation of the blood Free radical damage of cells 154