Pathophysiology L 3 Bleeding Thrombosis Disorders Prof Fakhir
Patho-physiology L 3 Bleeding & Thrombosis Disorders Prof. Fakhir Al-Ani fakeralani 2000@yahoo. com
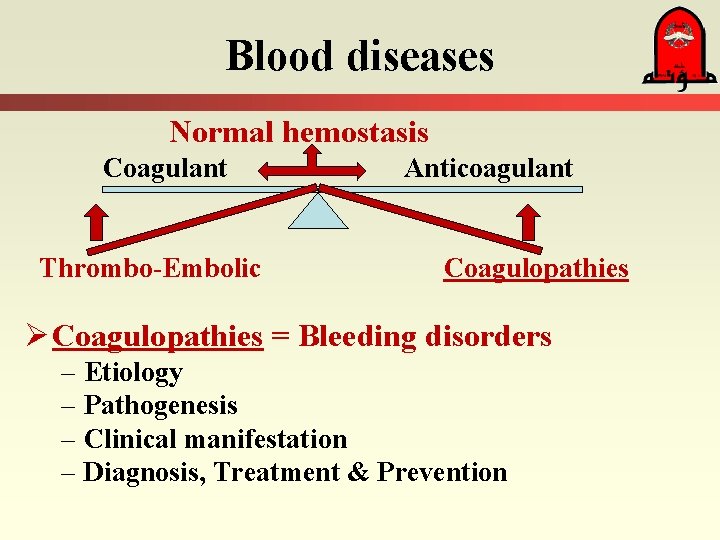
Blood diseases Normal hemostasis Coagulant Thrombo-Embolic Anticoagulant Coagulopathies Ø Coagulopathies = Bleeding disorders – Etiology – Pathogenesis – Clinical manifestation – Diagnosis, Treatment & Prevention
Normal haemostasis Major component of Hemostasis: - 1. Constriction of the B. V. 2. Aggregation of the Platelet. 3. Blood coagulation -Generation of thrombin from prothrombin. - Generation of Fibrin from fibrinogen. 4. Degradation of Fibrin & B. Vessel repair.
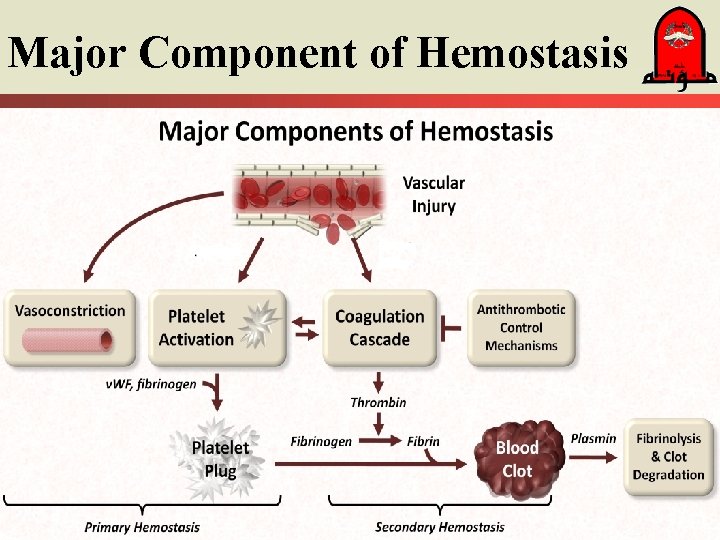
Major Component of Hemostasis
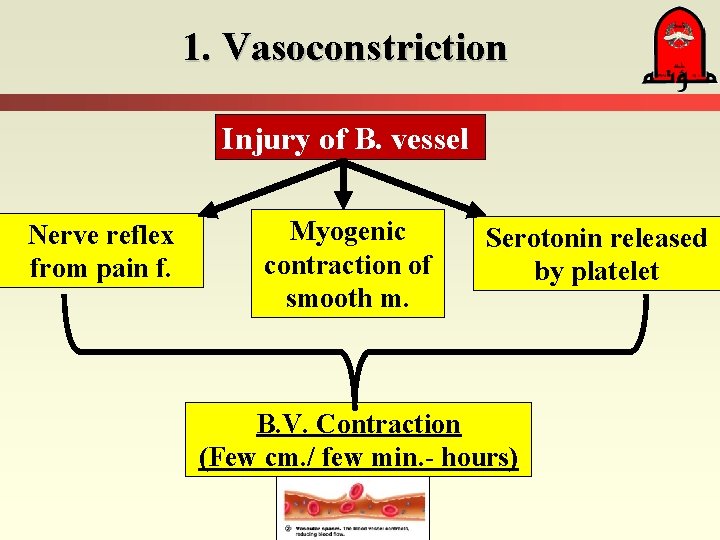
1. Vasoconstriction Injury of B. vessel Nerve reflex from pain f. Myogenic contraction of smooth m. Serotonin released by platelet B. V. Contraction (Few cm. / few min. - hours)
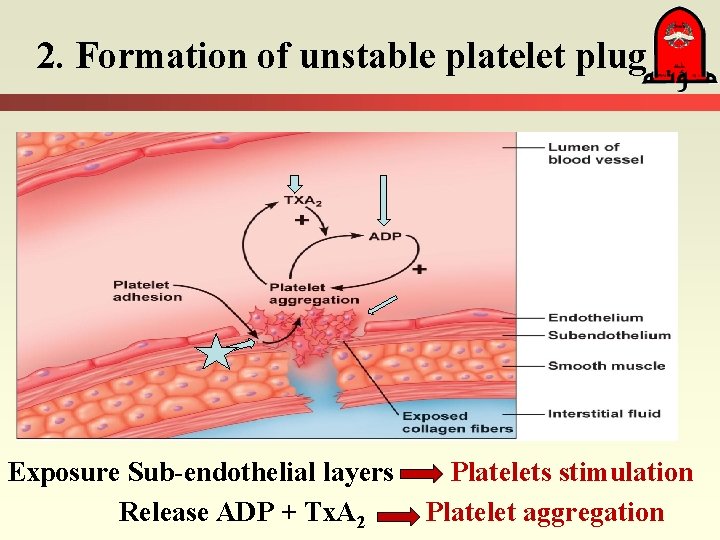
2. Formation of unstable platelet plug Exposure Sub-endothelial layers Release ADP + Tx. A 2 Platelets stimulation Platelet aggregation
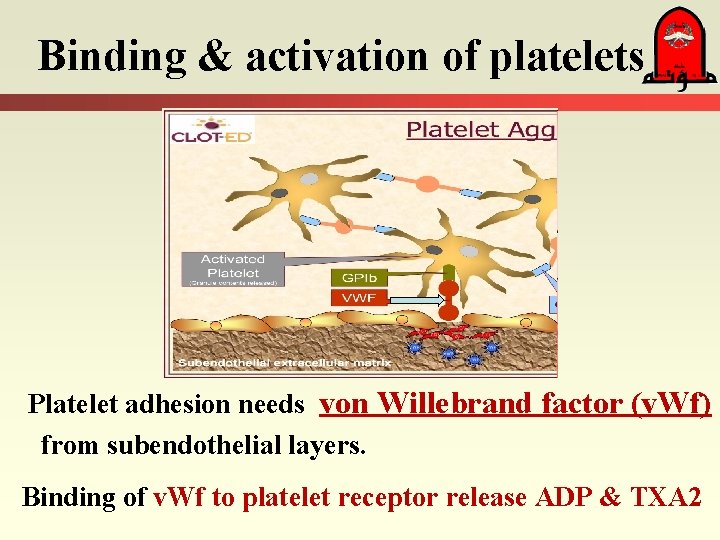
Binding & activation of platelets Platelet adhesion needs von Willebrand factor (v. Wf) from subendothelial layers. Binding of v. Wf to platelet receptor release ADP & TXA 2
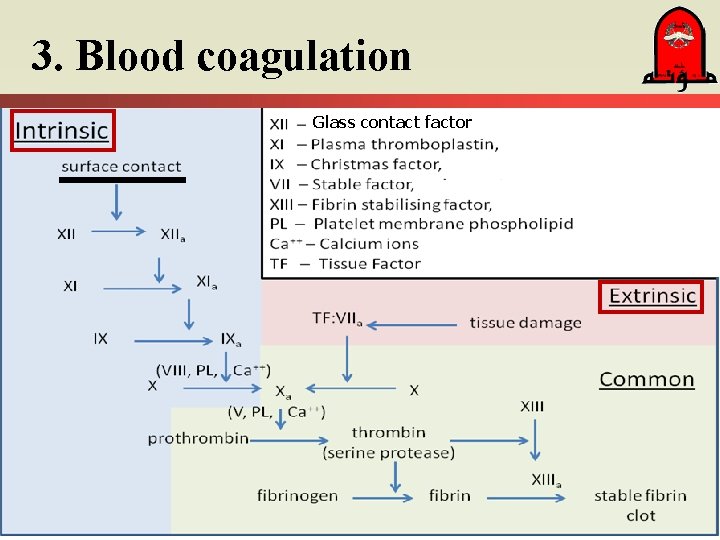
3. Blood coagulation Glass contact factor
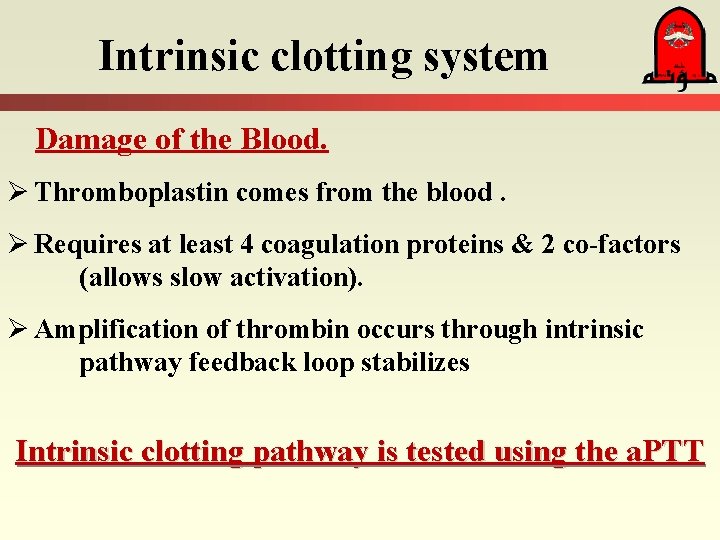
Intrinsic clotting system Damage of the Blood. Ø Thromboplastin comes from the blood. Ø Requires at least 4 coagulation proteins & 2 co-factors (allows slow activation). Ø Amplification of thrombin occurs through intrinsic pathway feedback loop stabilizes Intrinsic clotting pathway is tested using the a. PTT
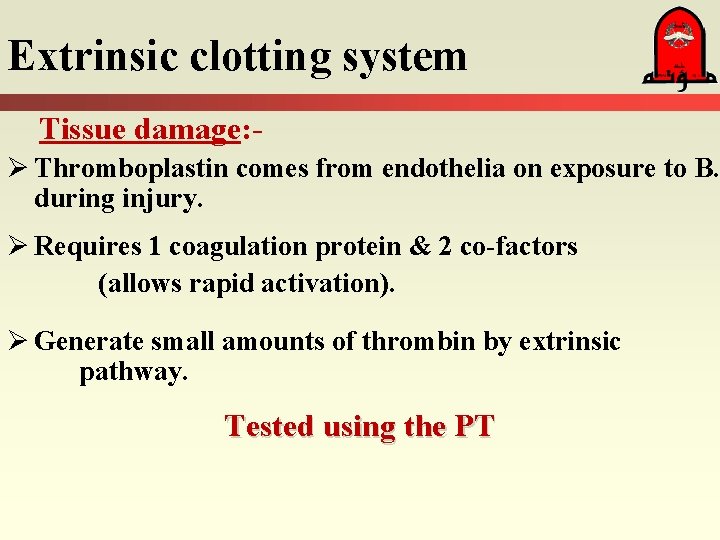
Extrinsic clotting system Tissue damage: Ø Thromboplastin comes from endothelia on exposure to B. during injury. Ø Requires 1 coagulation protein & 2 co-factors (allows rapid activation). Ø Generate small amounts of thrombin by extrinsic pathway. Tested using the PT
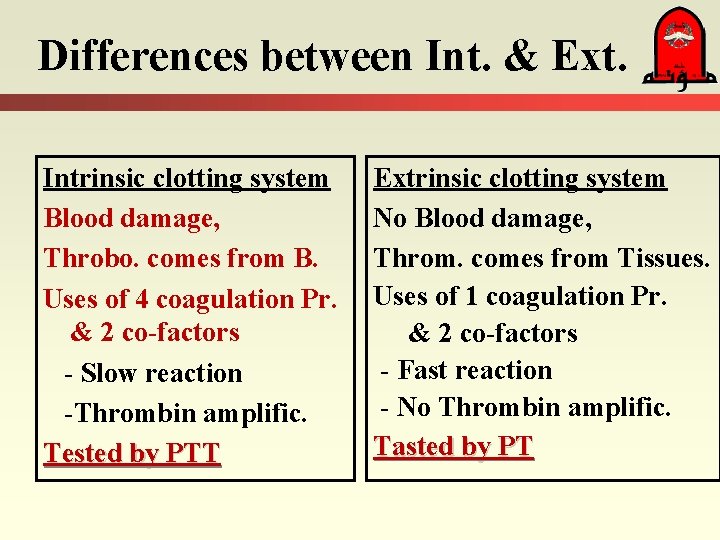
Differences between Int. & Ext. Intrinsic clotting system Blood damage, Throbo. comes from B. Uses of 4 coagulation Pr. & 2 co-factors - Slow reaction -Thrombin amplific. Tested by PTT Extrinsic clotting system No Blood damage, Throm. comes from Tissues. Uses of 1 coagulation Pr. & 2 co-factors - Fast reaction - No Thrombin amplific. Tasted by PT
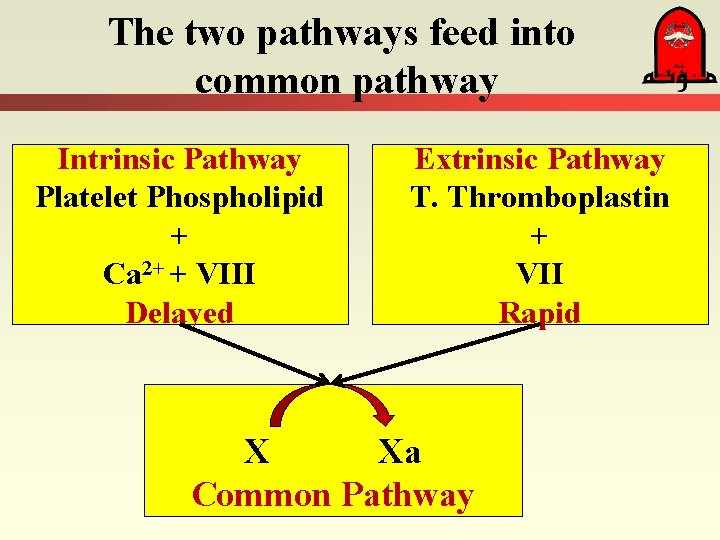
The two pathways feed into common pathway Intrinsic Pathway Platelet Phospholipid + Ca 2+ + VIII Delayed Extrinsic Pathway T. Thromboplastin + VII Rapid X Xa Common Pathway
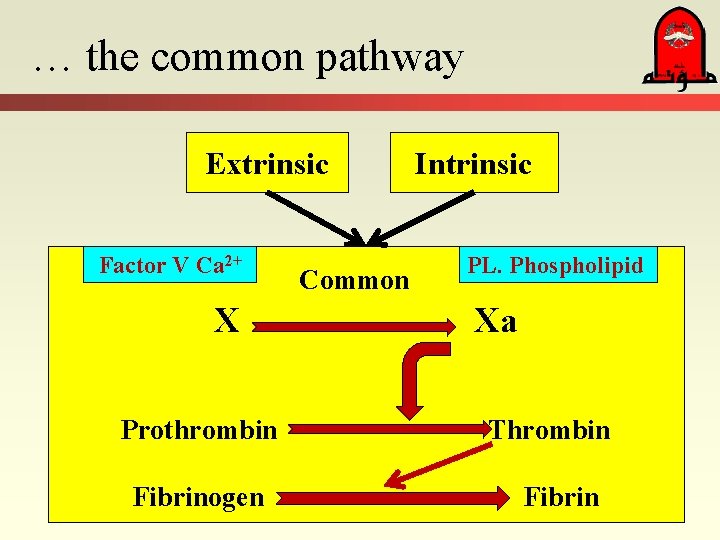
… the common pathway Extrinsic Factor V Ca 2+ X Prothrombin Fibrinogen Common Intrinsic PL. Phospholipid Xa Thrombin Fibrin
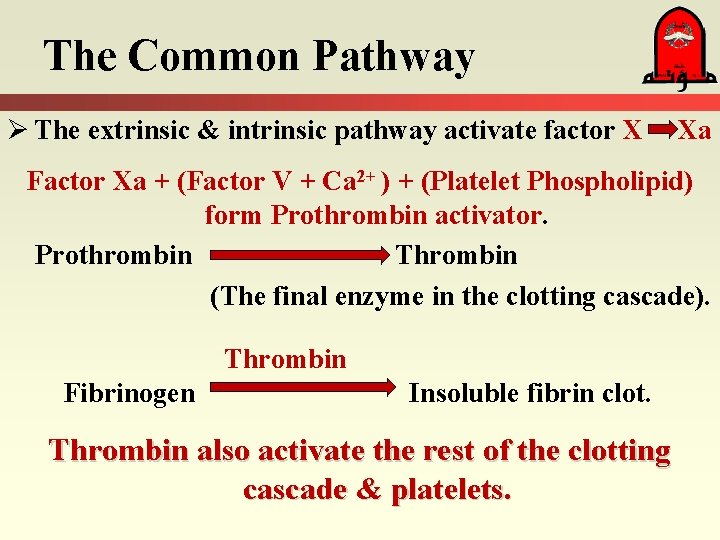
The Common Pathway Ø The extrinsic & intrinsic pathway activate factor X Xa Factor Xa + (Factor V + Ca 2+ ) + (Platelet Phospholipid) form Prothrombin activator. Prothrombin Thrombin (The final enzyme in the clotting cascade). Thrombin Fibrinogen Insoluble fibrin clot. Thrombin also activate the rest of the clotting cascade & platelets.
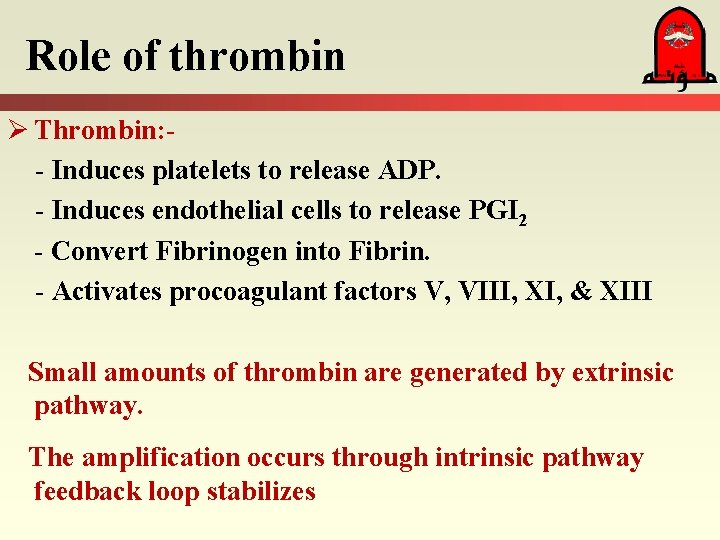
Role of thrombin Ø Thrombin: - Induces platelets to release ADP. - Induces endothelial cells to release PGI 2 - Convert Fibrinogen into Fibrin. - Activates procoagulant factors V, VIII, XI, & XIII Small amounts of thrombin are generated by extrinsic pathway. The amplification occurs through intrinsic pathway feedback loop stabilizes
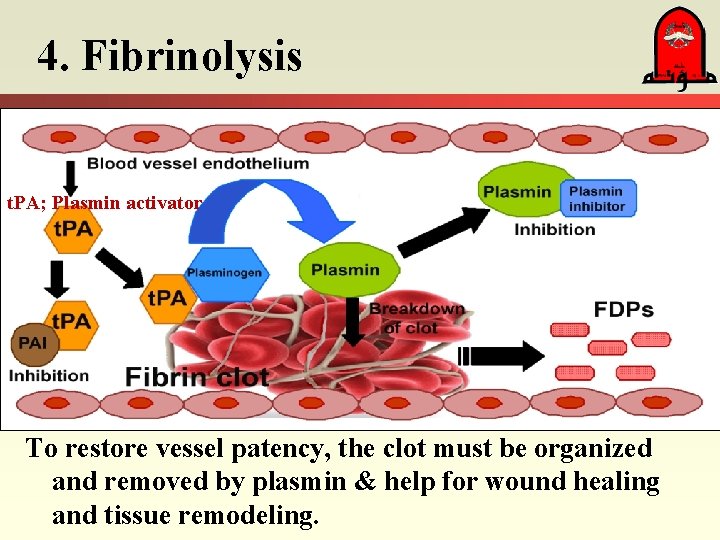
4. Fibrinolysis t. PA; Plasmin activator To restore vessel patency, the clot must be organized and removed by plasmin & help for wound healing and tissue remodeling.
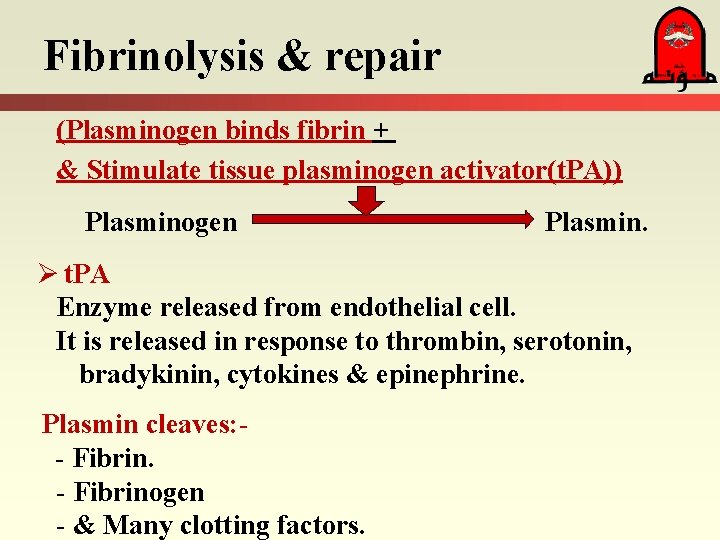
Fibrinolysis & repair (Plasminogen binds fibrin + & Stimulate tissue plasminogen activator(t. PA)) Plasminogen Plasmin. Ø t. PA Enzyme released from endothelial cell. It is released in response to thrombin, serotonin, bradykinin, cytokines & epinephrine. Plasmin cleaves: - Fibrinogen - & Many clotting factors.
Fibrin induces + ve feed back to increase plasmenogen activation Ø As plasmin degrade fibrin Ø Fibrin degrades activate more plasminogen (creating a +ve feedback loop).
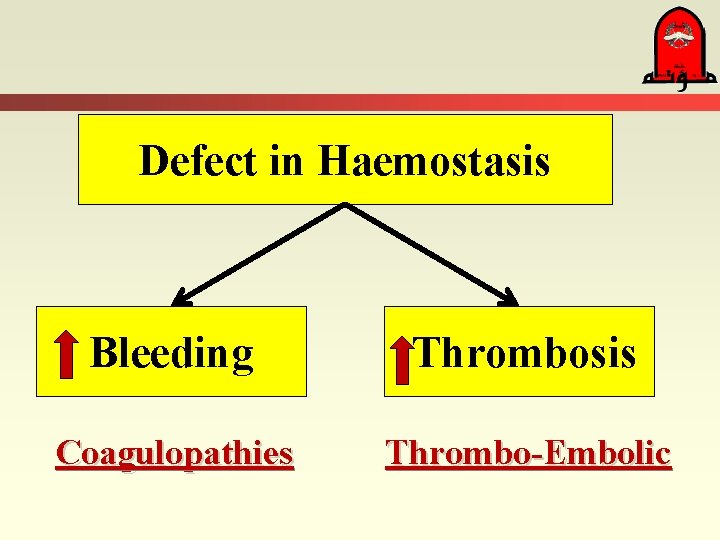
Defect in Haemostasis Bleeding Thrombosis Coagulopathies Thrombo-Embolic
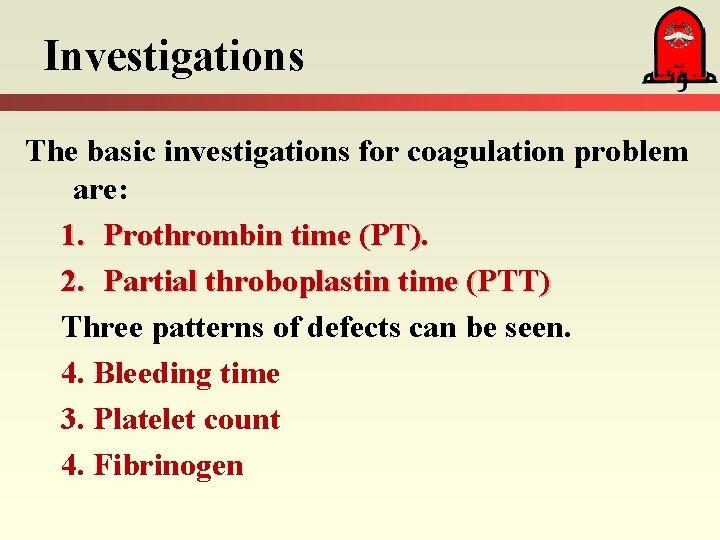
Investigations The basic investigations for coagulation problem are: 1. Prothrombin time (PT). 2. Partial throboplastin time (PTT) Three patterns of defects can be seen. 4. Bleeding time 3. Platelet count 4. Fibrinogen
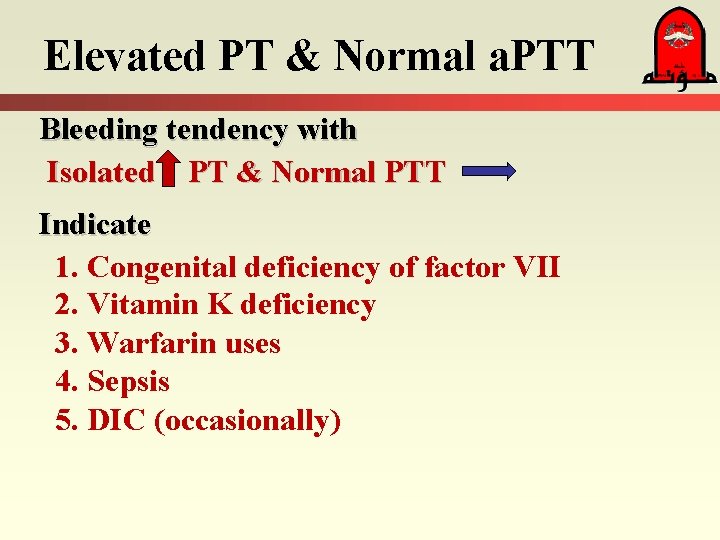
Elevated PT & Normal a. PTT Bleeding tendency with Isolated PT & Normal PTT Indicate 1. Congenital deficiency of factor VII 2. Vitamin K deficiency 3. Warfarin uses 4. Sepsis 5. DIC (occasionally)
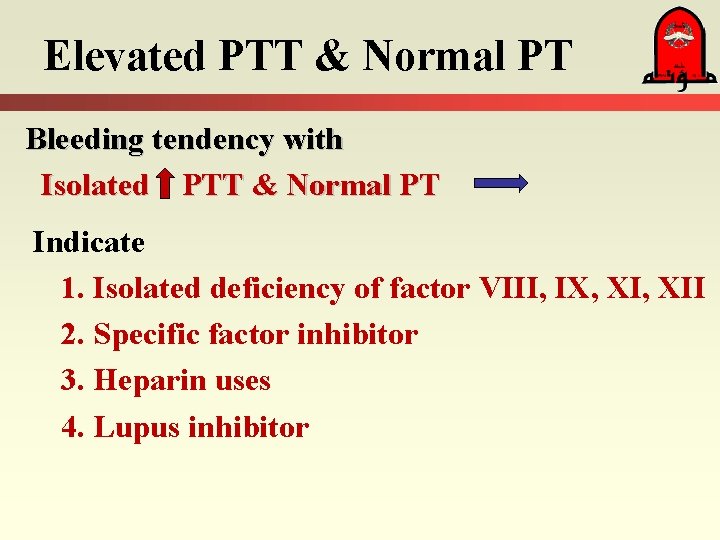
Elevated PTT & Normal PT Bleeding tendency with Isolated PTT & Normal PT Indicate 1. Isolated deficiency of factor VIII, IX, XII 2. Specific factor inhibitor 3. Heparin uses 4. Lupus inhibitor
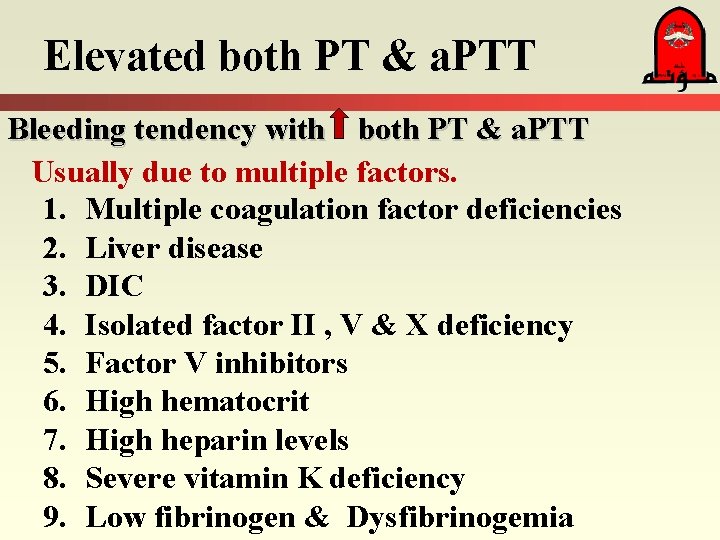
Elevated both PT & a. PTT Bleeding tendency with both PT & a. PTT Usually due to multiple factors. 1. Multiple coagulation factor deficiencies 2. Liver disease 3. DIC 4. Isolated factor II , V & X deficiency 5. Factor V inhibitors 6. High hematocrit 7. High heparin levels 8. Severe vitamin K deficiency 9. Low fibrinogen & Dysfibrinogemia
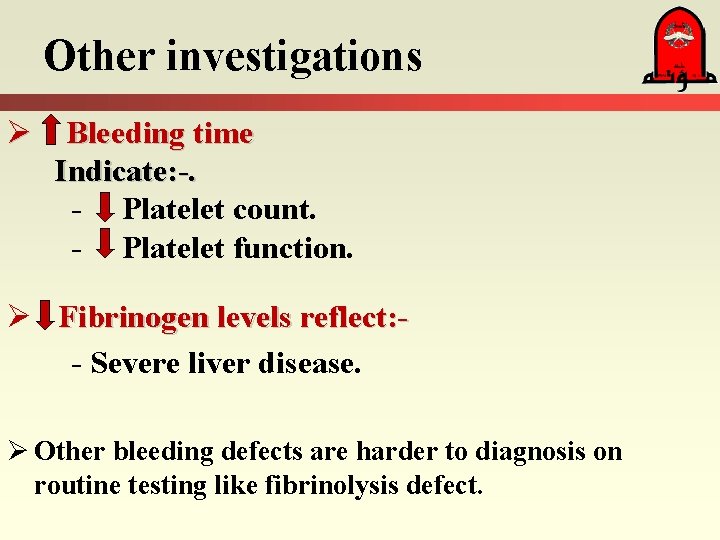
Other investigations Ø Bleeding time Indicate: -. - Platelet count. - Platelet function. Ø Fibrinogen levels reflect: - Severe liver disease. Ø Other bleeding defects are harder to diagnosis on routine testing like fibrinolysis defect.
Therapy Ø Replacement therapy should be based on: - Lab results. - Patient’s clinical situation. Ø The transfusion for platelets supplement: - Can be < 10, 000/u. L if the patient is not bleeding. - If the subject is: Not on platelet inhibitors. Preserved renal function. Does not have DIC. - More concentration is needed in the other conditions
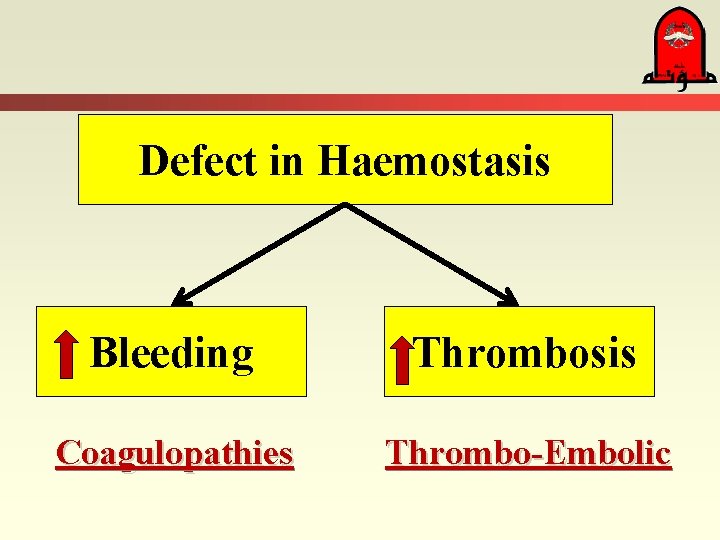
Defect in Haemostasis Bleeding Thrombosis Coagulopathies Thrombo-Embolic
Clinicaly Coagulopathies
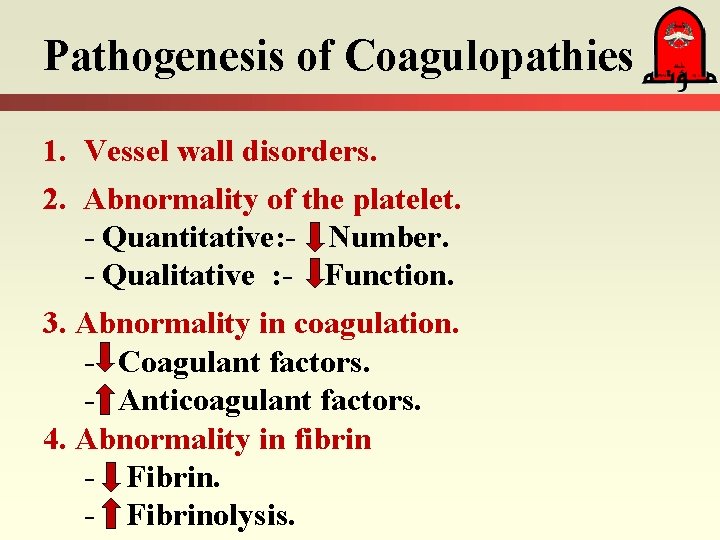
Pathogenesis of Coagulopathies 1. Vessel wall disorders. 2. Abnormality of the platelet. - Quantitative: - Number. - Qualitative : - Function. 3. Abnormality in coagulation. - Coagulant factors. - Anticoagulant factors. 4. Abnormality in fibrin - Fibrinolysis.
1. Vascular disorders Inherited - Structural. Acquired - Inflammation = Vasculitis. - Immune vessel damage = Autoimmune diseases
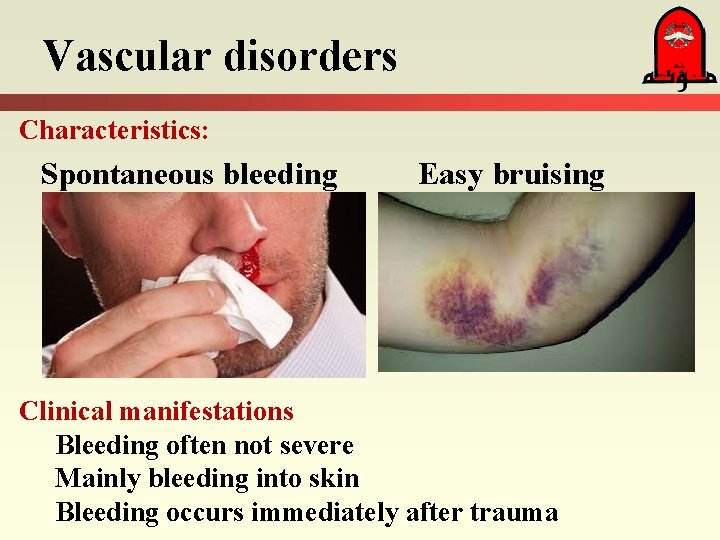
Vascular disorders Characteristics: Spontaneous bleeding Easy bruising Clinical manifestations Bleeding often not severe Mainly bleeding into skin Bleeding occurs immediately after trauma
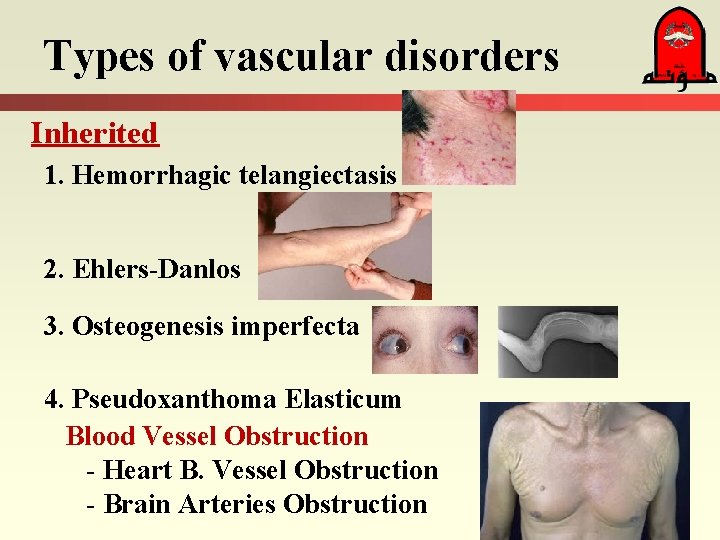
Types of vascular disorders Inherited 1. Hemorrhagic telangiectasis 2. Ehlers-Danlos 3. Osteogenesis imperfecta 4. Pseudoxanthoma Elasticum Blood Vessel Obstruction - Heart B. Vessel Obstruction - Brain Arteries Obstruction
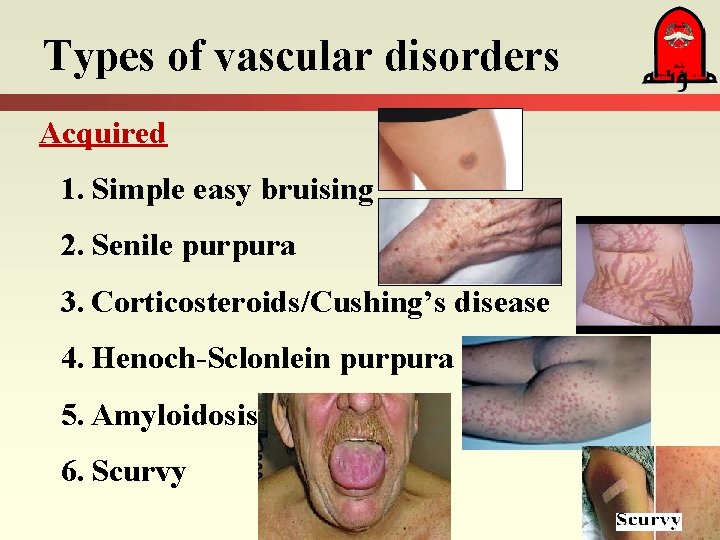
Types of vascular disorders Acquired 1. Simple easy bruising 2. Senile purpura 3. Corticosteroids/Cushing’s disease 4. Henoch-Sclonlein purpura 5. Amyloidosis 6. Scurvy
2. Abnormality of the platelet. Decreased number Thrombocytopenia = No. of Platelet Mechanism: - Production - thrombopoietin production in liver disease B. M. suppression by viral, drugs, toxins, nutrition Disorders of hematopoiesis (Congenital or acquired). Destruction - Immune or Non-immune processes. - Dilution & distribution - Massive transfusion & splenic sequestration.
Causes of Increased Platelet Destruction 1. 2. 3. 4. Idiopathic thrombocytopenia purpura (ITP). Auto-immune. Post-transfusion. Drug induced (especially heparin, cyclosporin, tacrolimus & ticlopidine) 5. Infection associated (Viral) 6. DIC 7. Physical destruction (by pass, hemangiomas
Thrombocytopenia Pre-eclampsia Presents as part of the spectrum of pre-eclampsia. Ø First sign is a fall in platelets, then abnormal liver function tests, & hemolysis. Ø Can progress to liver failure. Ø Hypertension. Ø May require steroids or plasma exchange if condition worsens. Ø Delivery usually resolves the condition.
Platelet Dysfunction ( Function) Uremia & Drugs Renal failure: Uremia can cause bleeding from platelet dysfunction. - As in aggressive dialysis to control the uremia. Treated by Desmopressin acetate (ADH 20 ug IV) for acute bleeding or pre-procedure. - Acetylsalicylic acid irreversibly inhibits platelet function & so platelets must be replaced if bleeding occurs. - Other drugs such as ketorolac & hydroxyethyl starch reversible inhibit & platelet function will recover as the drug clears.
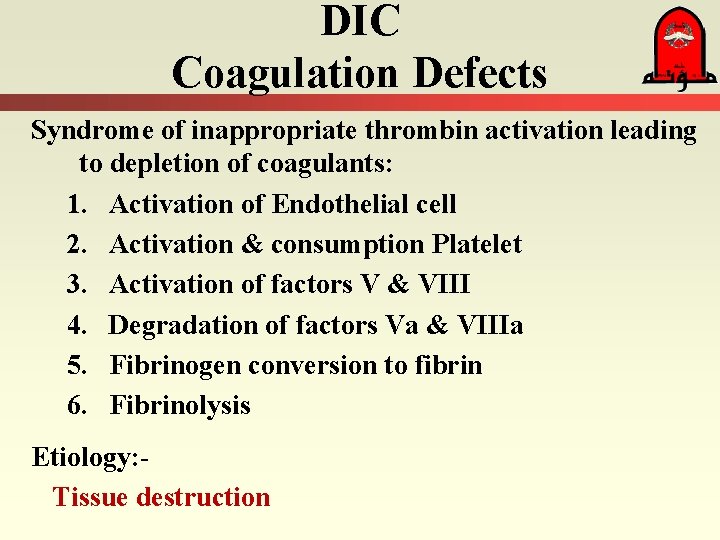
DIC Coagulation Defects Syndrome of inappropriate thrombin activation leading to depletion of coagulants: 1. Activation of Endothelial cell 2. Activation & consumption Platelet 3. Activation of factors V & VIII 4. Degradation of factors Va & VIIIa 5. Fibrinogen conversion to fibrin 6. Fibrinolysis Etiology: Tissue destruction
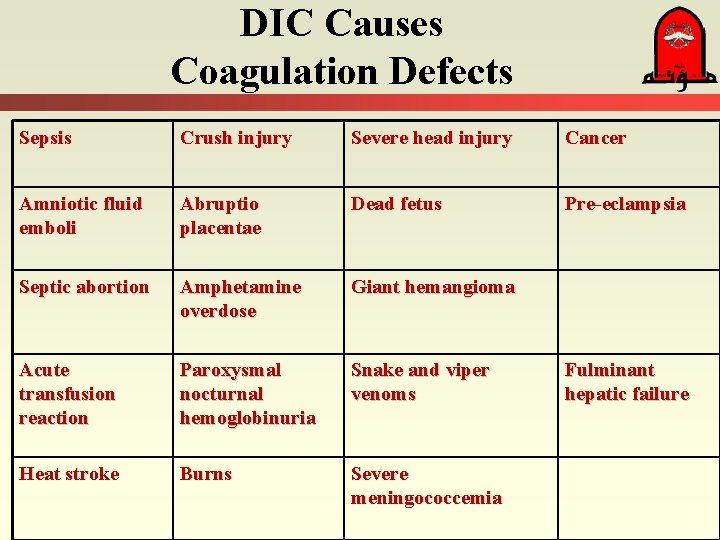
DIC Causes Coagulation Defects Sepsis Crush injury Severe head injury Cancer Amniotic fluid emboli Abruptio placentae Dead fetus Pre-eclampsia Septic abortion Amphetamine overdose Giant hemangioma Acute transfusion reaction Paroxysmal nocturnal hemoglobinuria Snake and viper venoms Heat stroke Burns Severe meningococcemia Fulminant hepatic failure
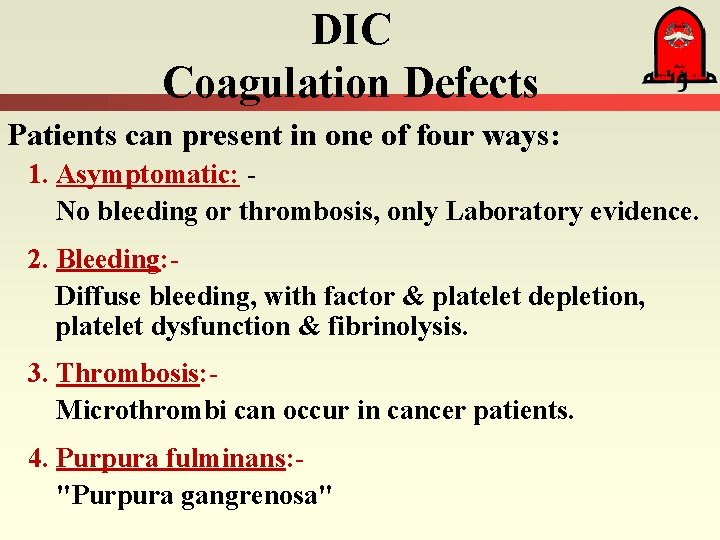
DIC Coagulation Defects Patients can present in one of four ways: 1. Asymptomatic: No bleeding or thrombosis, only Laboratory evidence. 2. Bleeding: Diffuse bleeding, with factor & platelet depletion, platelet dysfunction & fibrinolysis. 3. Thrombosis: Microthrombi can occur in cancer patients. 4. Purpura fulminans: "Purpura gangrenosa"
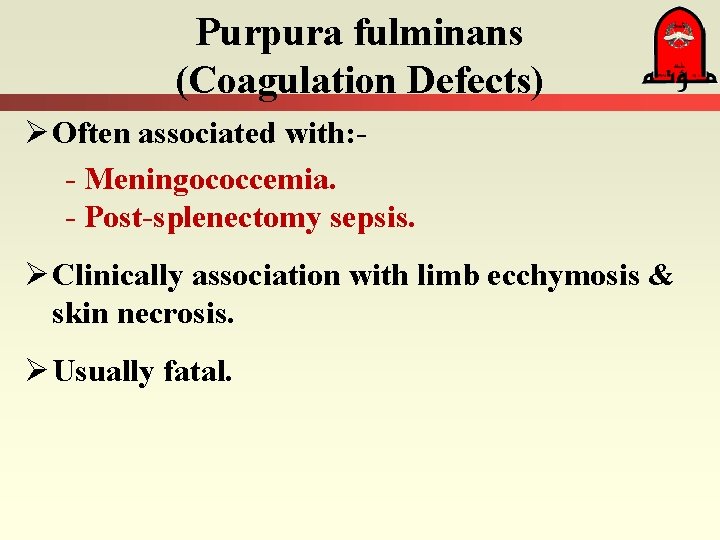
Purpura fulminans (Coagulation Defects) Ø Often associated with: - Meningococcemia. - Post-splenectomy sepsis. Ø Clinically association with limb ecchymosis & skin necrosis. Ø Usually fatal.
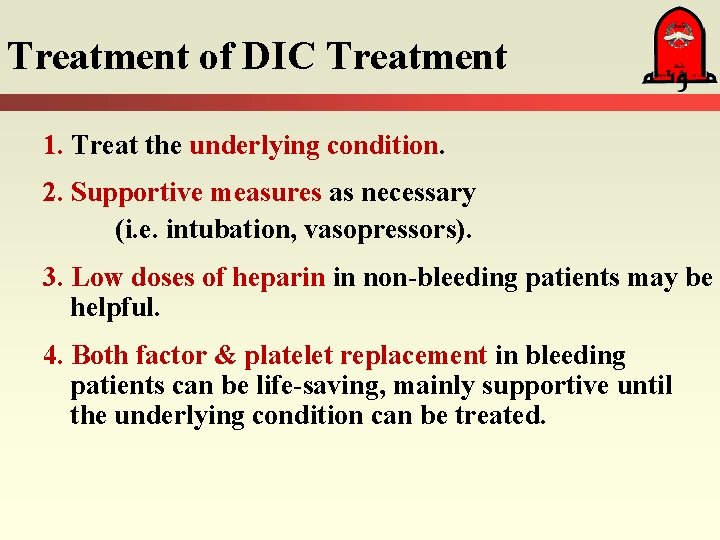
Treatment of DIC Treatment 1. Treat the underlying condition. 2. Supportive measures as necessary (i. e. intubation, vasopressors). 3. Low doses of heparin in non-bleeding patients may be helpful. 4. Both factor & platelet replacement in bleeding patients can be life-saving, mainly supportive until the underlying condition can be treated.
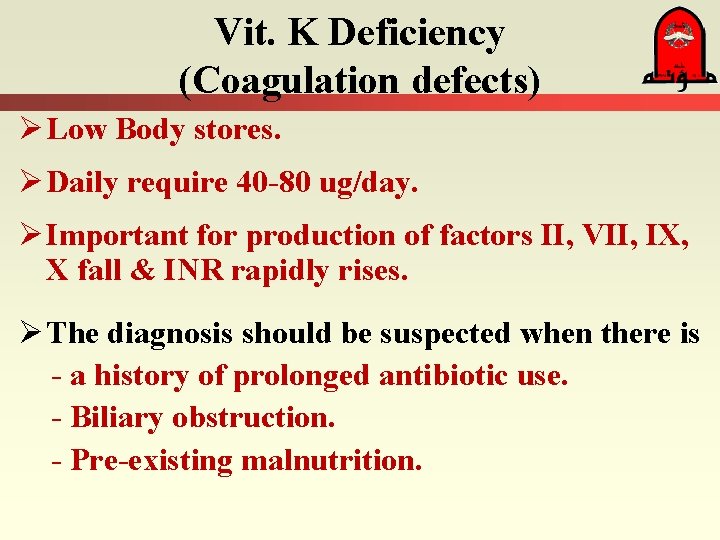
Vit. K Deficiency (Coagulation defects) Ø Low Body stores. Ø Daily require 40 -80 ug/day. Ø Important for production of factors II, VII, IX, X fall & INR rapidly rises. Ø The diagnosis should be suspected when there is - a history of prolonged antibiotic use. - Biliary obstruction. - Pre-existing malnutrition.
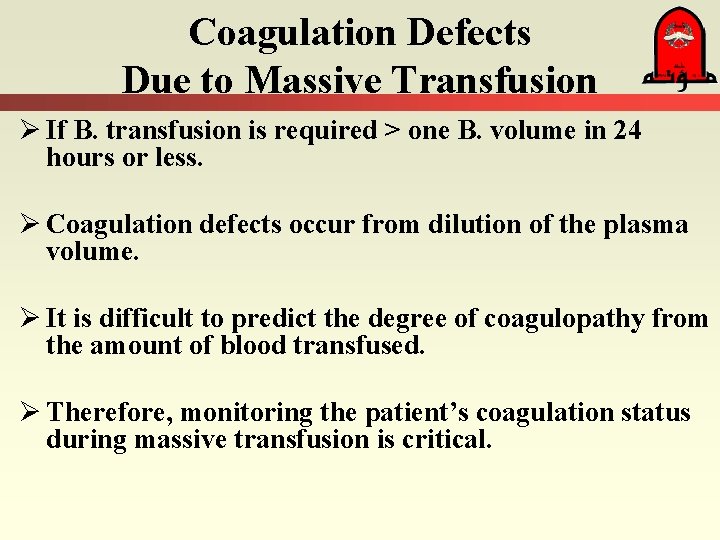
Coagulation Defects Due to Massive Transfusion Ø If B. transfusion is required > one B. volume in 24 hours or less. Ø Coagulation defects occur from dilution of the plasma volume. Ø It is difficult to predict the degree of coagulopathy from the amount of blood transfused. Ø Therefore, monitoring the patient’s coagulation status during massive transfusion is critical.
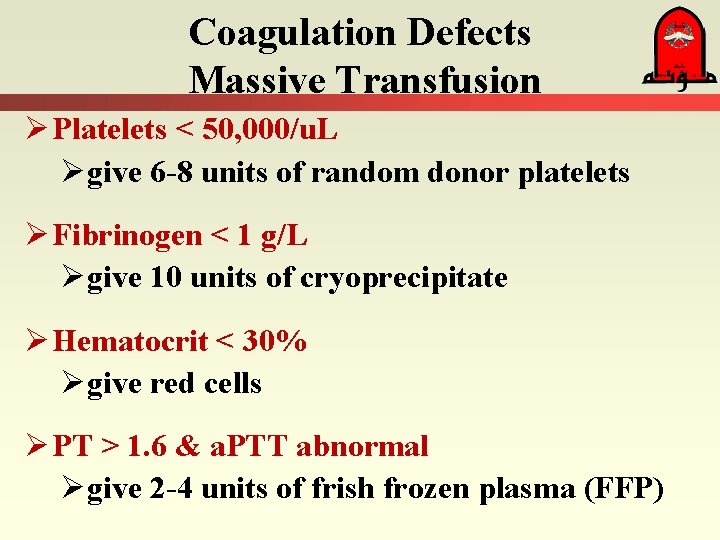
Coagulation Defects Massive Transfusion Ø Platelets < 50, 000/u. L Øgive 6 -8 units of random donor platelets Ø Fibrinogen < 1 g/L Øgive 10 units of cryoprecipitate Ø Hematocrit < 30% Øgive red cells Ø PT > 1. 6 & a. PTT abnormal Øgive 2 -4 units of frish frozen plasma (FFP)
Coagulation Defects Use of Factor VIIa : Ø Recently released. Ø Used for the treatment of: - Congenital FVII, XI, or V deficiency. - Liver failure coagulopathy. - Warfarin overdose. - Thrombocytopenia due to antiplatelet antibodies - Intracerebral hemorrhage. - Localizes to sites of endothelial injury.
Thrombosis
Thrombosis - Incidence Ø Most ICU patients have one or more risk factors for thrombosis. - The incidence is about 33%. - 15% of DVT are in the upper limbs.
Thrombosis - Pathophysiology Ø Virchow triad: – - Endothelial damage. - Abnormal blood flow. - Altered blood composition. Ø Trauma & surgical patients: - Causes inevidently endothelial damage. Ø Inflammation & stress causes thrombocytosis. Ø Hyperfibrinogenemia, altered coagulation factors. Ø Immobilization.
Thrombosis - Pathophysiology Other causes: Ø Inherited hypercoagable states: - These increase the relative risk by 10 X. on top of the acquired risks. Ø Previous episode of thrombosis. Ø Family history of DVT.
Thrombosis – PE Pathophysiology Ø Pulmonary artery obstruction: Pulmonary artery Pr. Rt Vent. failure Central venous Pr. C. O. RV O 2 demands In the presence of hypoxia, hypotension, & perfusion causing infarction. coronary Ø Infarction leads to worsening RV function & output perpetuating the vicious cycle. Ø Patients can also develop paradoxical embolism.
Thrombosis - Diagnosis 1. Clinical symptoms & signs: Poor sensitivity & specificity. ØAcute onset dyspnea ØPleuritic chest pain ØCough ØHemoptysis ØTachypnea ØSinus tachycardia ØSyncope Ø Pulmonary angiogram. Ø CT chest angiogram.
Thrombosis – DVT/PE Treatment Ø Once detected, both DVT require full anticoagulation with heparin. Ø Low mol. Weigt heparin is a therapeutic option but can be contraindication by it long half life & renal clearance. Ø Coumadin is best avoided in the critical care phase because of the number of interactions with other medications & difficult reversibility.
Thrombosis – DVT Prevention Preventative strategies fall into two groups: - Pharmacological. Heparin: Treatment & Prophylaxis: Reduces incidence by over 50%. - Mechanical. Stockings & compression devices.
- Slides: 53