Pathophysiology Glucose Homeostasis Diabetes Mellitus Glucose Homeostasis Insulin
Pathophysiology Glucose Homeostasis & Diabetes Mellitus
Glucose Homeostasis Insulin secretion u Counter-regulatory Hormones u
Insulin Secretion u Daily basilar level – 40 -50 U/day u Stimulated secretion – BS 80 -100 mg/dl – Secreted through glucose metabolism mediated depolarization – Membrane changes promote Ca influx and insulin secretion
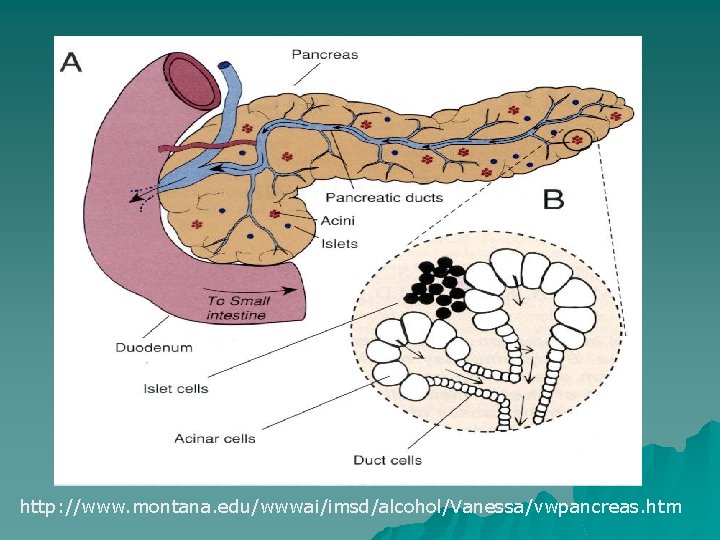
http: //www. montana. edu/wwwai/imsd/alcohol/Vanessa/vwpancreas. htm
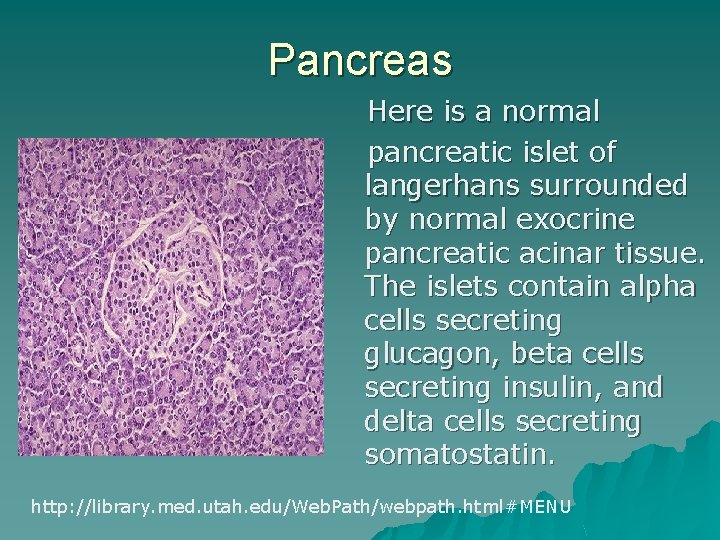
Pancreas Here is a normal pancreatic islet of langerhans surrounded by normal exocrine pancreatic acinar tissue. The islets contain alpha cells secreting glucagon, beta cells secreting insulin, and delta cells secreting somatostatin. http: //library. med. utah. edu/Web. Path/webpath. html#MENU
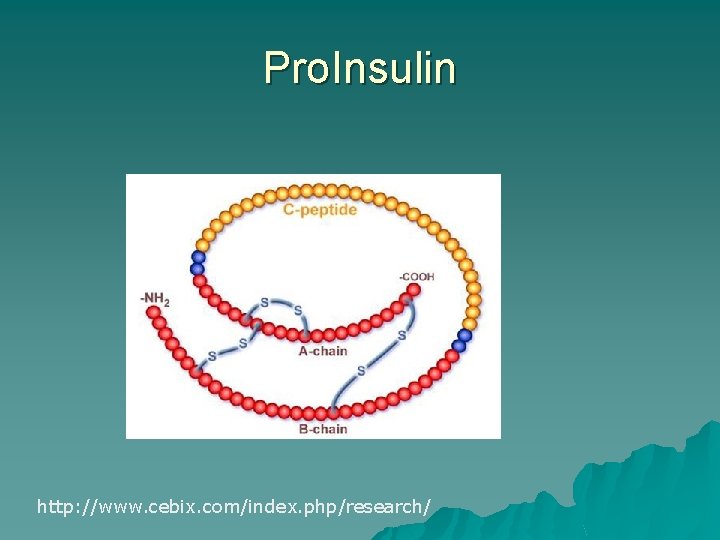
Pro. Insulin http: //www. cebix. com/index. php/research/

Insulin Action u Insulin dependent transporters u Storage of energy glucose substrates – fats – amino acids – glucose to glycogen u Enhancement of growth factor activity u Increase cellular uptake of K, Phosphorus, and Mg
Counter Regulatory Hormones u Glucagon – opposes insulin u Epinephrine – mobilization of glucose stores u Glucocorticoids – decreases peripheral utilization of glucose u Growth Hormone – decreases glucose uptake by tissues
Incretins u Incretins – group of gastrointestinal hormones released in response to eating – Includes glucagon like peptide (GLP – 1) which decreases need for glucagon secretion u Result is increased insulin levels and decreased glucagon levels u Decrease gastric emptying and slow the rate of absorption of nutrients.
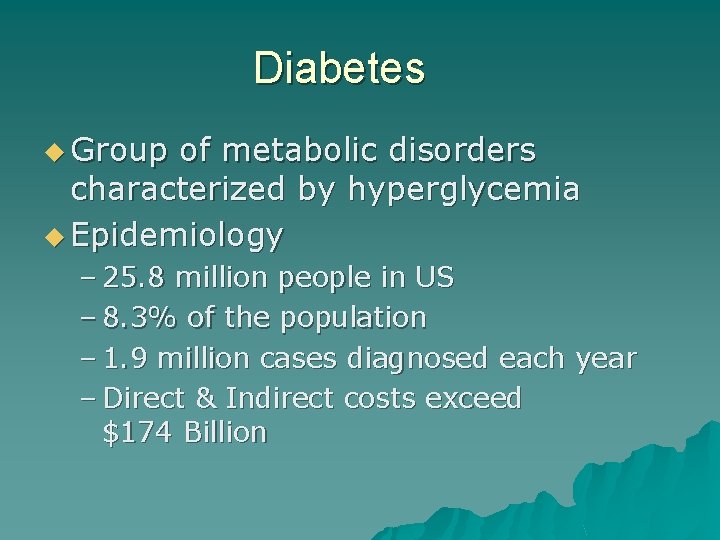
Diabetes u Group of metabolic disorders characterized by hyperglycemia u Epidemiology – 25. 8 million people in US – 8. 3% of the population – 1. 9 million cases diagnosed each year – Direct & Indirect costs exceed $174 Billion
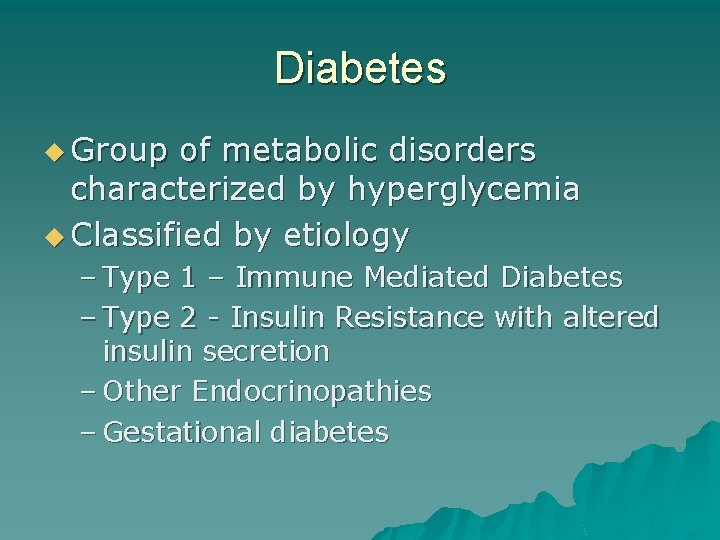
Diabetes u Group of metabolic disorders characterized by hyperglycemia u Classified by etiology – Type 1 – Immune Mediated Diabetes – Type 2 - Insulin Resistance with altered insulin secretion – Other Endocrinopathies – Gestational diabetes
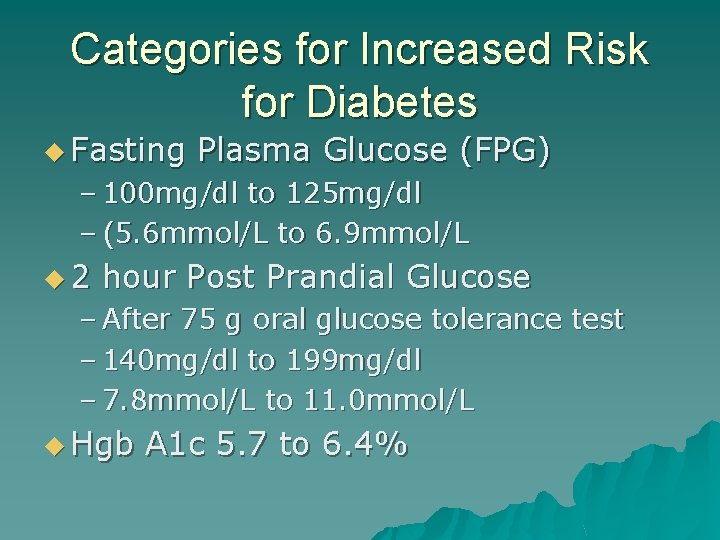
Categories for Increased Risk for Diabetes u Fasting Plasma Glucose (FPG) – 100 mg/dl to 125 mg/dl – (5. 6 mmol/L to 6. 9 mmol/L u 2 hour Post Prandial Glucose – After 75 g oral glucose tolerance test – 140 mg/dl to 199 mg/dl – 7. 8 mmol/L to 11. 0 mmol/L u Hgb A 1 c 5. 7 to 6. 4%
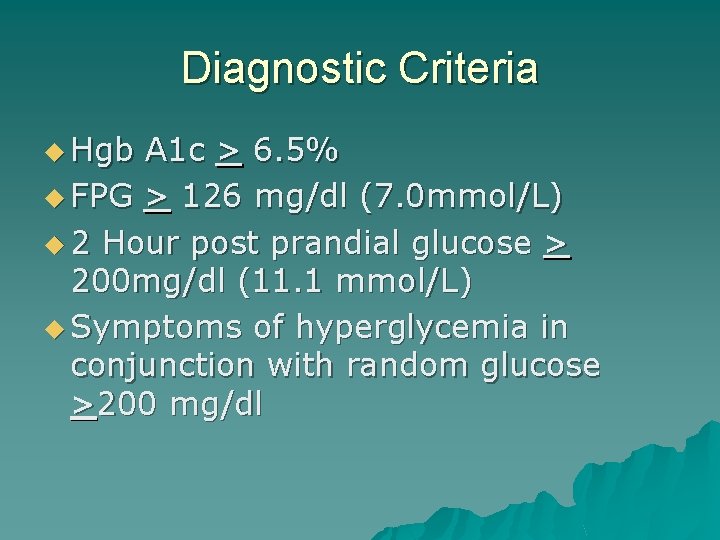
Diagnostic Criteria u Hgb A 1 c > 6. 5% u FPG > 126 mg/dl (7. 0 mmol/L) u 2 Hour post prandial glucose > 200 mg/dl (11. 1 mmol/L) u Symptoms of hyperglycemia in conjunction with random glucose >200 mg/dl

Diabetes u Insulin Secretion & Patterns of Administration – Link
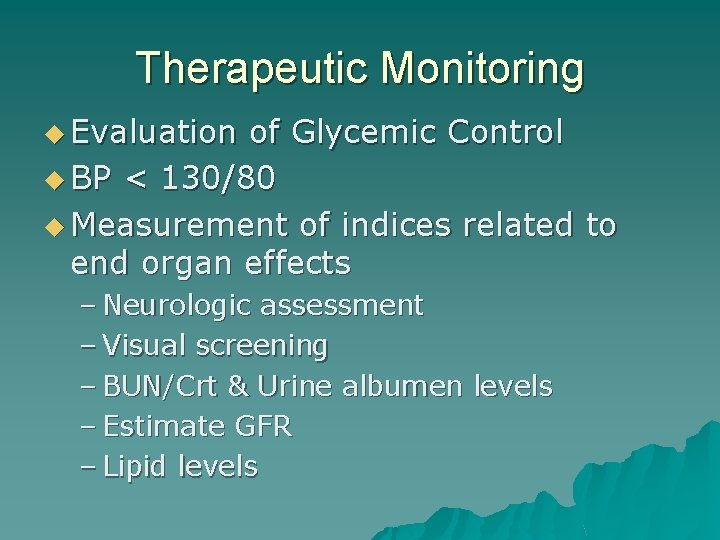
Therapeutic Monitoring u Evaluation of Glycemic Control u BP < 130/80 u Measurement of indices related to end organ effects – Neurologic assessment – Visual screening – BUN/Crt & Urine albumen levels – Estimate GFR – Lipid levels
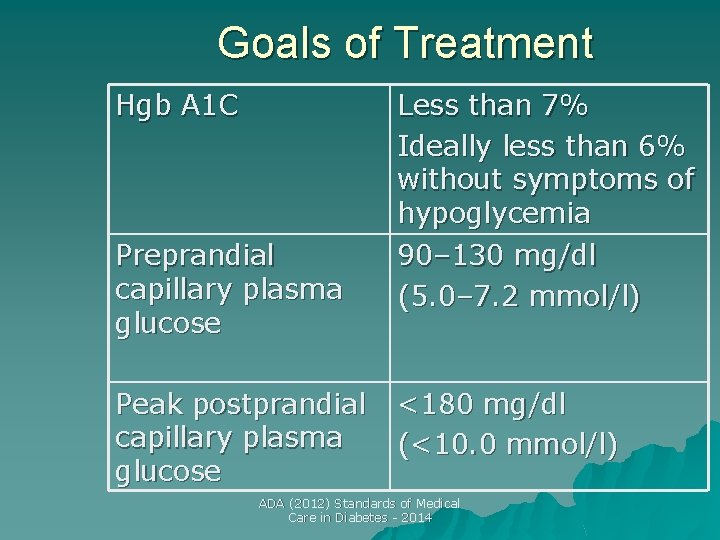
Goals of Treatment Hgb A 1 C Preprandial capillary plasma glucose Peak postprandial capillary plasma glucose Less than 7% Ideally less than 6% without symptoms of hypoglycemia 90– 130 mg/dl (5. 0– 7. 2 mmol/l) <180 mg/dl (<10. 0 mmol/l) ADA (2012) Standards of Medical Care in Diabetes - 2014
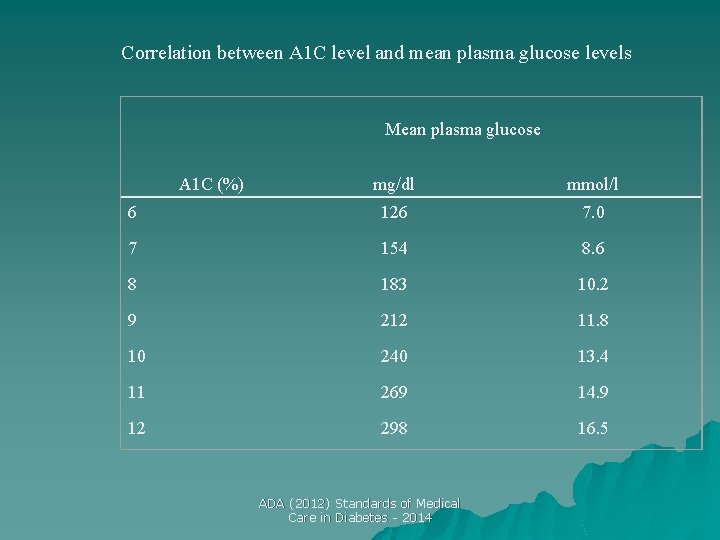
Correlation between A 1 C level and mean plasma glucose levels Mean plasma glucose mg/dl mmol/l 6 126 7. 0 7 154 8. 6 8 183 10. 2 9 212 11. 8 10 240 13. 4 11 269 14. 9 12 298 16. 5 A 1 C (%) ADA (2012) Standards of Medical Care in Diabetes - 2014
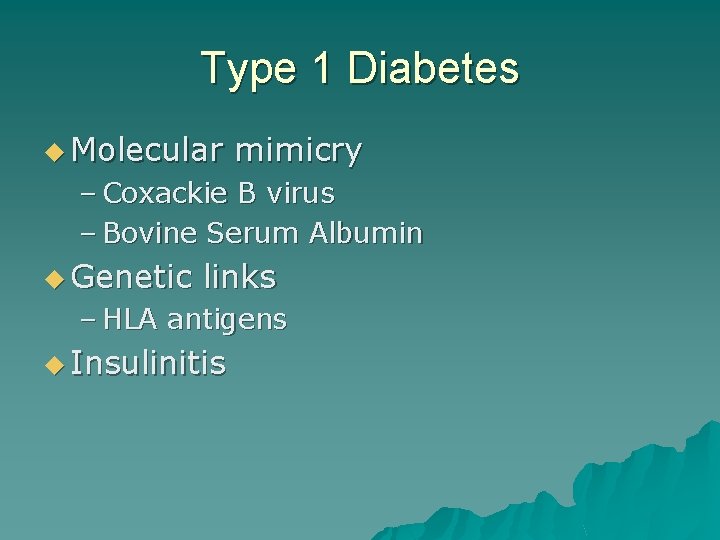
Type 1 Diabetes u Molecular mimicry – Coxackie B virus – Bovine Serum Albumin u Genetic links – HLA antigens u Insulinitis
Type 2 Diabetes u Insulin Resistance u Reduction in Insulin secretion u Genetic & Environmental factors
Type 2 Diabetes u Genetic & Environmental Issues u Pathophysiology – Abnormalities in adipoctes (accelerated lipolysis) – Neuroprotective mechanisms (excessive appetite) – Excessive hepatic glucose production triggered by insulin resistance, insulinopenia, and increased glucagon secretion.
Acute Complications u Hyperglycemia – osmotic diuresis u fluid & electrolytes – glucosuria u Candida – hyperphagia u DKA u HHNK
Hypoglycemia u Counter -regulatory hormone secretion u Enhanced Catecholamine secretion u Neuroglycopenia u Nocturnal Hypoglycemia
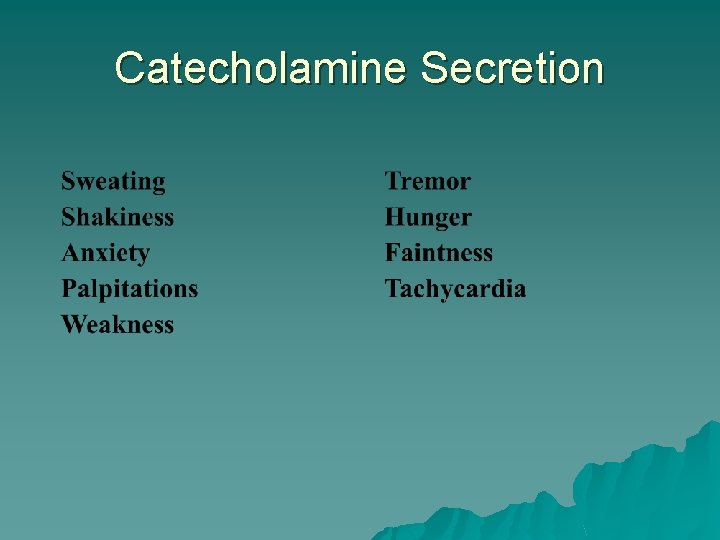
Catecholamine Secretion
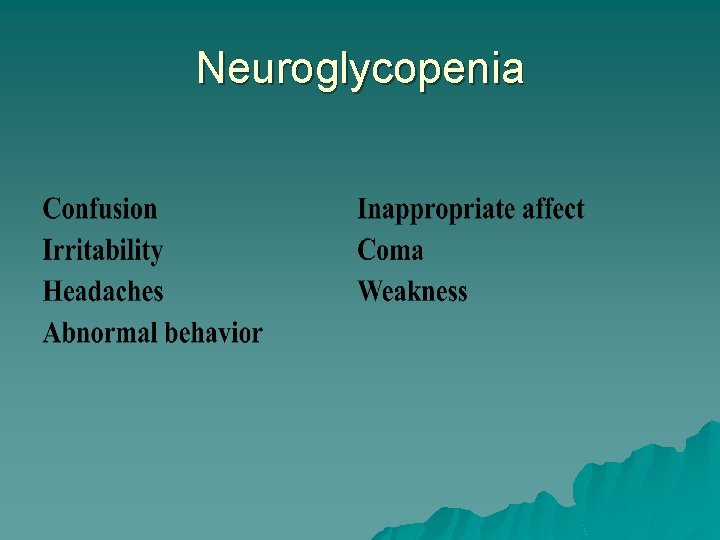
Neuroglycopenia
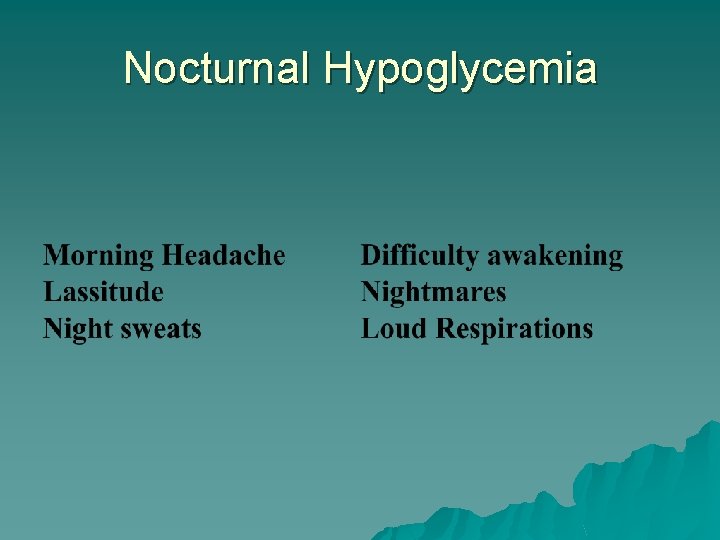
Nocturnal Hypoglycemia
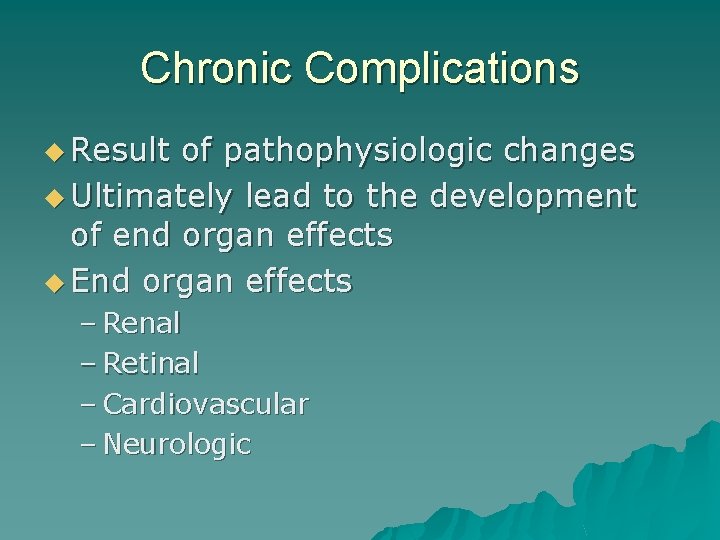
Chronic Complications u Result of pathophysiologic changes u Ultimately lead to the development of end organ effects u End organ effects – Renal – Retinal – Cardiovascular – Neurologic
Chronic Complications u Complications – Link u Microvascular disease u Macrovascular disease u Neuropathy
Microvascular Disease u Thickening of basement membranes u Advanced Glycosylated end products u End organ effects – Retinopathy – Nephropathy
Microvascular Disease u Retinopathy – Microaneurysms, exudates, edema – Neovascularization promotes retinal detachment u Nephropathy – Alteration in glomerular function – Proteinuria, hypertension, renal insufficiency – Glomerular sclersosi
Macrovascular Disease u Acceleration of atherosclerosis u Increased VLDL u Increased foam cell activity u Imbalance in thrombotic and fibrinolytic factors
Neuropathy u Vascular insufficiency - ischemia u Neuronal tissues -Altered metabolism – non insulin dependent glucose transporters u Fructose & Sorbitol – Sorbitol excess – altered cellular osmolality – increased free radical formation
Autonomic Neuropathy u Tachycardia u Orthostatic hypotension u Incontinence u Headaches
- Slides: 32