PATHOPHARMACOLOGY OF FLUID ELECTROLYTE IMBALANCES Wanda Lovitz APRN
PATHOPHARMACOLOGY OF FLUID & ELECTROLYTE IMBALANCES Wanda Lovitz, APRN
OBJECTIVES: FLUID AND ELECTROLYTES 1. Compare and contrast the different types of capillary and interstitial fluid exchange: 1. Capillary hydrostatic pressure (CHP) 2. Colloid osmotic pressure (COP) “oncotic” pressure 3. Interstitial fluid hydrostatic pressure (IFHP) 4. Interstitial fluid osmotic pressure (IFOP) 2. Discuss the key regulators in F&E balance: 1. Renin-angiotensin-aldosterone mechanism 2. Antidiuretic hormone (ADH) 3. Thirst mechanism* 3. Describe the physiologic mechanisms that contribute to edema. * 1. Explain the clinical manifestations of selected electrolyte imbalances on the patien 1. Sodium 2. Potassium 2. Discuss the treatment of electrolyte imbalances. (sodium & potassium)
DRUGS TO KNOW sodium polystyrene sulfonate (Kayexlate)
REVIEW OF BASIC CONCEPTS: SLIDES 4 -17 (FROM NURSING LECTURE) It is expected that you will study these slides before coming to class. This content will not be presented in lecture. However, you are responsible for the material on the slides and there may be 1 -3 exam items related to this content.
WHAT IS DIURESIS? Diuresis is increased production of urine by the kidneys Diuretic drugs promote “diuresis” is a natural diuretic Exercise may produce diuresis Increased thirst and drinking (po) normally produces diuresis Caffeine
F&E LECTURE: RANDOM FACTS THAT WILL COME IN HANDY Osmolality defined: solute concentration in the blood Osmosis → movement of water across a semipermeable membrane from an area of lower (solute) concentration to an area of higher (solute) concentration Sodium (Na+) → a solute; makes up 80% of serum osmolality Water follows salt or you can memorize the simple rule that…

SALT SUCKS…. WATER FOLLOWS SALT
F&E LECTURE: RANDOM FACTS THAT WILL COME IN HANDY COP = oncotic pressure: “colloidal osmotic pressure” is synonymous with “oncotic pressure” Albumin: is the primary colloid (plasma protein); nml serum albumin = (3. 5 – 5) low albumin will result in COP “Water follows PROTEIN”
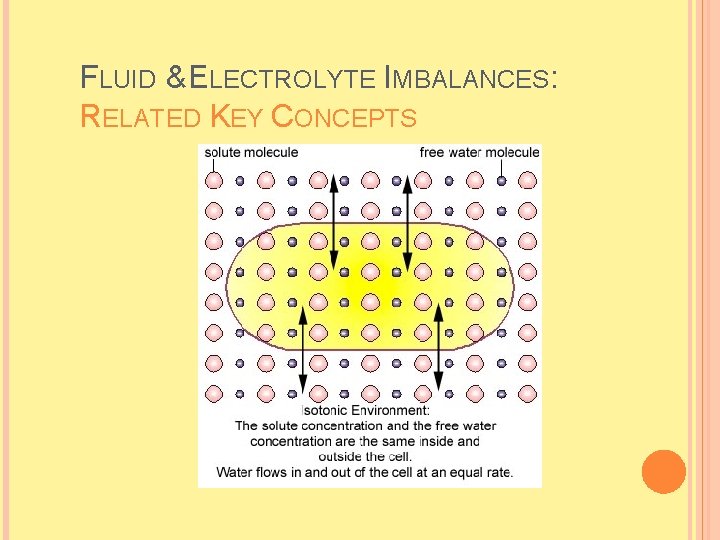
FLUID & ELECTROLYTE IMBALANCES: RELATED KEY CONCEPTS
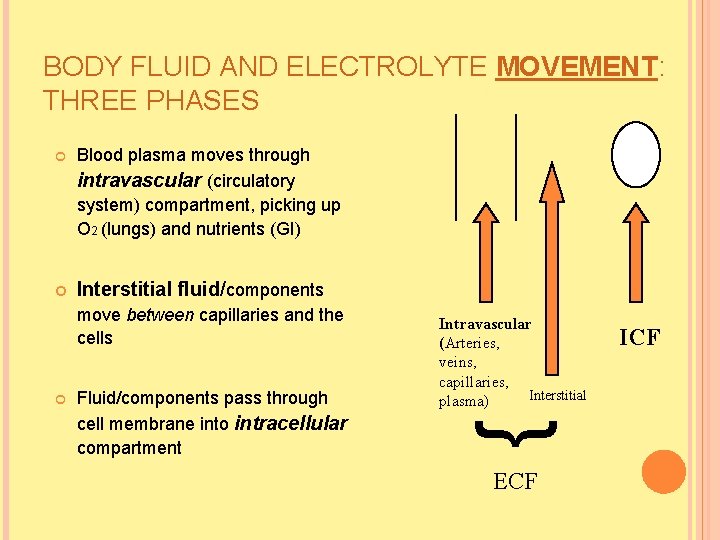
BODY FLUID AND ELECTROLYTE MOVEMENT: THREE PHASES Blood plasma moves through intravascular (circulatory system) compartment, picking up O 2 (lungs) and nutrients (GI) Interstitial fluid/components move between capillaries and the cells Fluid/components pass through cell membrane into intracellular compartment Intravascular (Arteries, veins, capillaries, Interstitial plasma) { ECF ICF
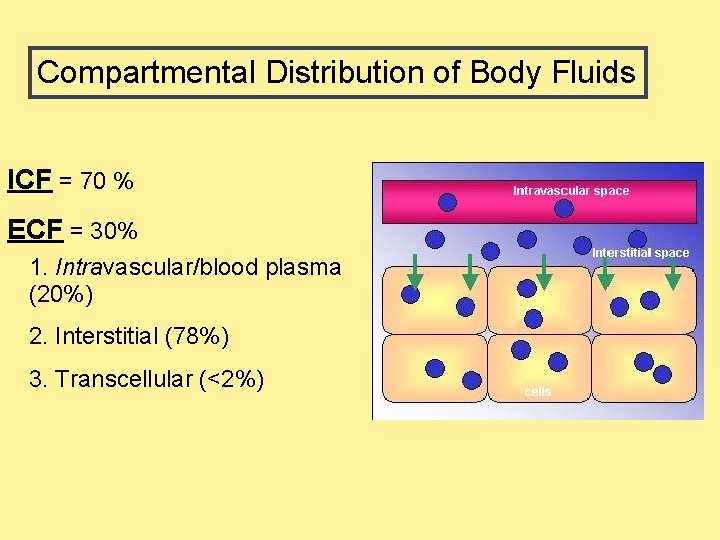
Compartmental Distribution of Body Fluids ICF = 70 % ECF = 30% 1. Intravascular/blood plasma (20%) 2. Interstitial (78%) 3. Transcellular (<2%)
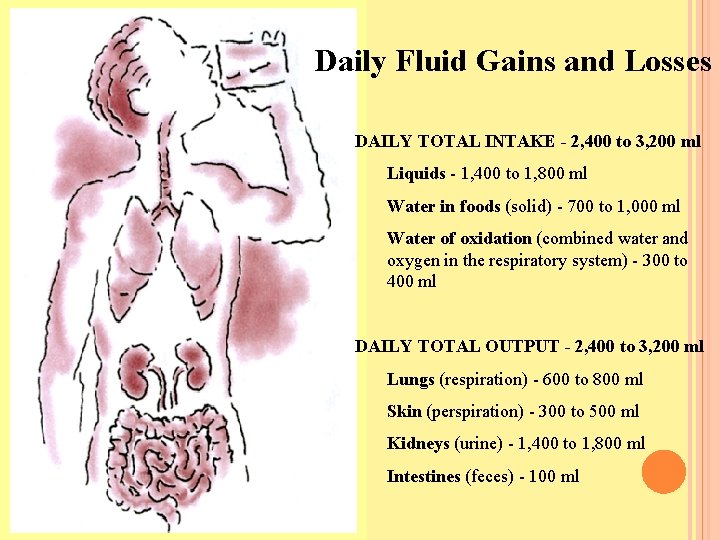
Daily Fluid Gains and Losses DAILY TOTAL INTAKE - 2, 400 to 3, 200 ml Liquids - 1, 400 to 1, 800 ml Water in foods (solid) - 700 to 1, 000 ml Water of oxidation (combined water and oxygen in the respiratory system) - 300 to 400 ml DAILY TOTAL OUTPUT - 2, 400 to 3, 200 ml Lungs (respiration) - 600 to 800 ml Skin (perspiration) - 300 to 500 ml Kidneys (urine) - 1, 400 to 1, 800 ml Intestines (feces) - 100 ml
FLUID VOLUME DEFICIT VS FLUID VOLUME EXCESS Happen to be NANDA diagnoses…
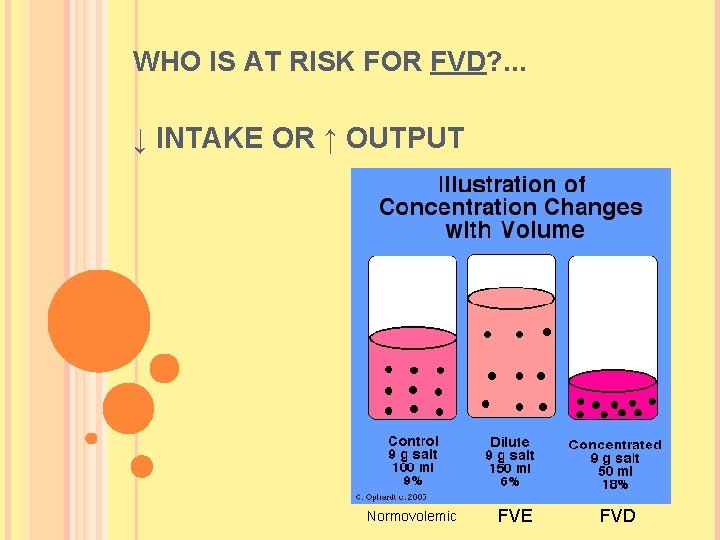
WHO IS AT RISK FOR FVD? . . . ↓ INTAKE OR ↑ OUTPUT Normovolemic FVE FVD
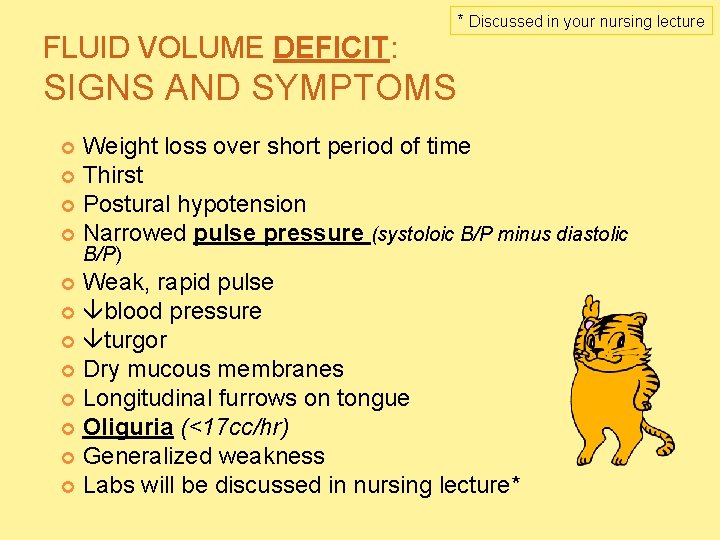
FLUID VOLUME DEFICIT: * Discussed in your nursing lecture SIGNS AND SYMPTOMS Weight loss over short period of time Thirst Postural hypotension Narrowed pulse pressure (systoloic B/P minus diastolic B/P) Weak, rapid pulse blood pressure turgor Dry mucous membranes Longitudinal furrows on tongue Oliguria (<17 cc/hr) Generalized weakness Labs will be discussed in nursing lecture*
WHO IS AT RISK FOR FVE? . . . ↑ INTAKE OR ↓ OUTPUT
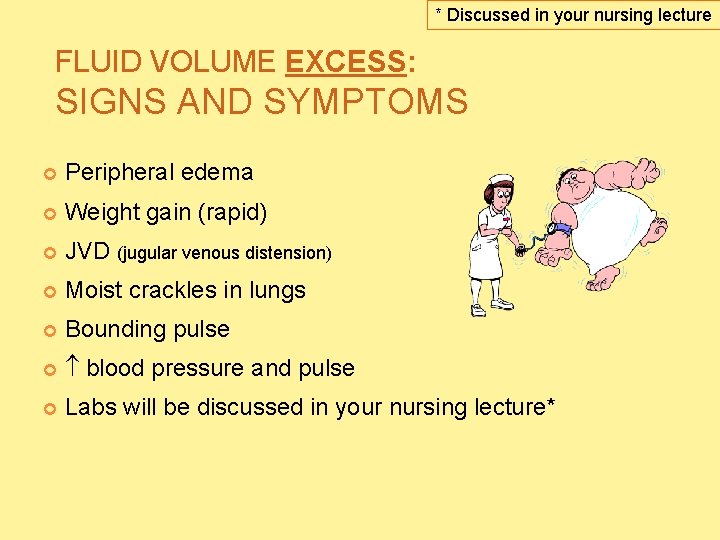
* Discussed in your nursing lecture FLUID VOLUME EXCESS: SIGNS AND SYMPTOMS Peripheral edema Weight gain (rapid) JVD (jugular venous distension) Moist crackles in lungs Bounding pulse blood pressure and pulse Labs will be discussed in your nursing lecture*
FLUID & ELECTROLYTES: PATHOPHARMACOLOGY

FLUID SHIFTS: HOW THEY HAPPEN…
PUSHING VS PULLING POWER Hydrostatic Pressure Osmotic Pressure has PUSHING POWER has PULLING POWER Capillary Interstital Interstitial Colloidal/oncotic
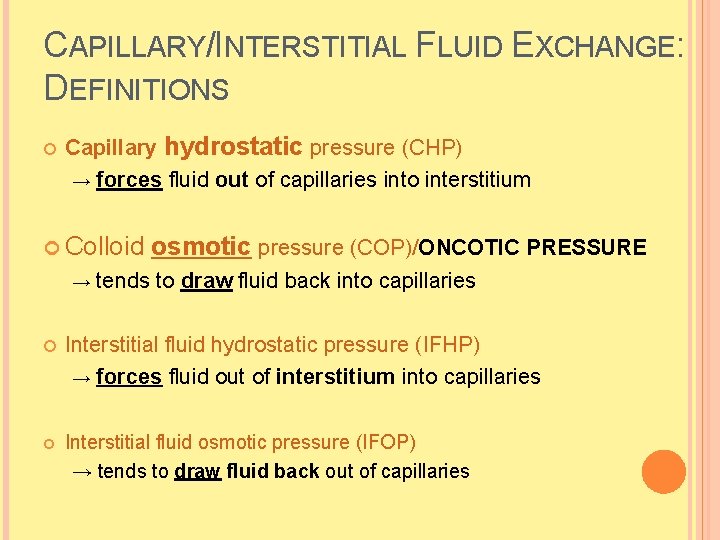
CAPILLARY/INTERSTITIAL FLUID EXCHANGE: DEFINITIONS Capillary hydrostatic pressure (CHP) → forces fluid out of capillaries into interstitium Colloid osmotic pressure (COP)/ONCOTIC PRESSURE → tends to draw fluid back into capillaries Interstitial fluid hydrostatic pressure (IFHP) → forces fluid out of interstitium into capillaries Interstitial fluid osmotic pressure (IFOP) → tends to draw fluid back out of capillaries
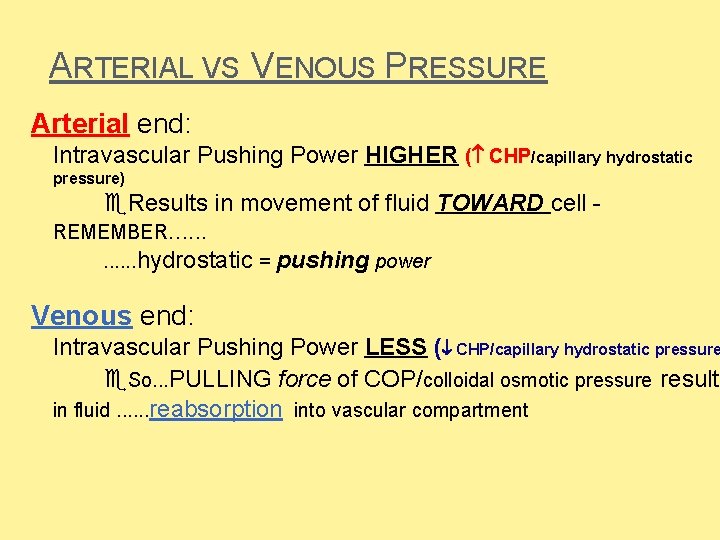
ARTERIAL VS VENOUS PRESSURE Arterial end: Intravascular Pushing Power HIGHER ( CHP/capillary hydrostatic pressure) Results in movement of fluid TOWARD cell REMEMBER. . . hydrostatic = pushing power Venous end: Intravascular Pushing Power LESS ( CHP/capillary hydrostatic pressure So. . . PULLING force of COP/colloidal osmotic pressure results in fluid. . . reabsorption into vascular compartment
KEY REGULATORS IN FLUID & ELECTROLYTE BALANCE Regulation of sodium balance Renin-angiotensin-aldosterone (RAA) mechanism Regulation of water balance Anti-Diuretic Hormone (ADH) Perception of thirst
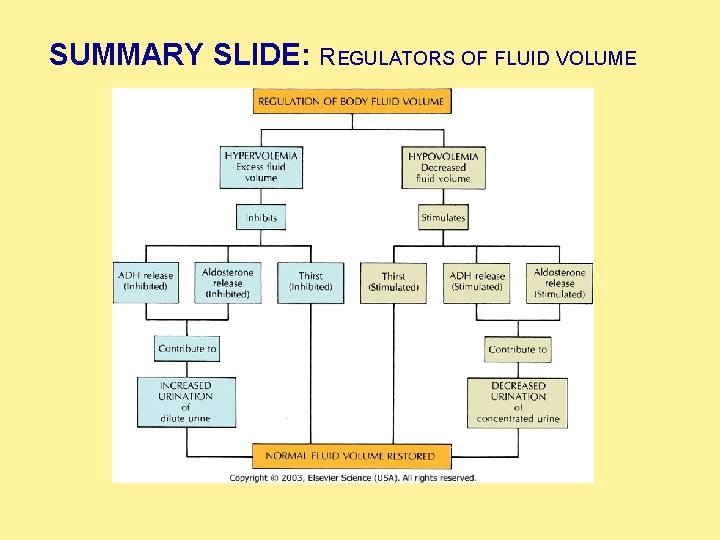
SUMMARY SLIDE: REGULATORS OF FLUID VOLUME
EDEMA
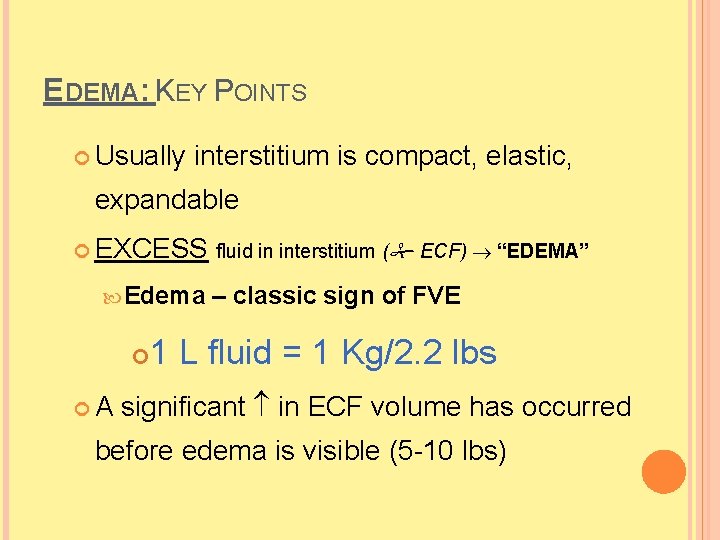
EDEMA: KEY POINTS Usually interstitium is compact, elastic, expandable EXCESS fluid in interstitium ( ECF) “EDEMA” Edema A – classic sign of FVE 1 L fluid = 1 Kg/2. 2 lbs significant in ECF volume has occurred before edema is visible (5 -10 lbs)
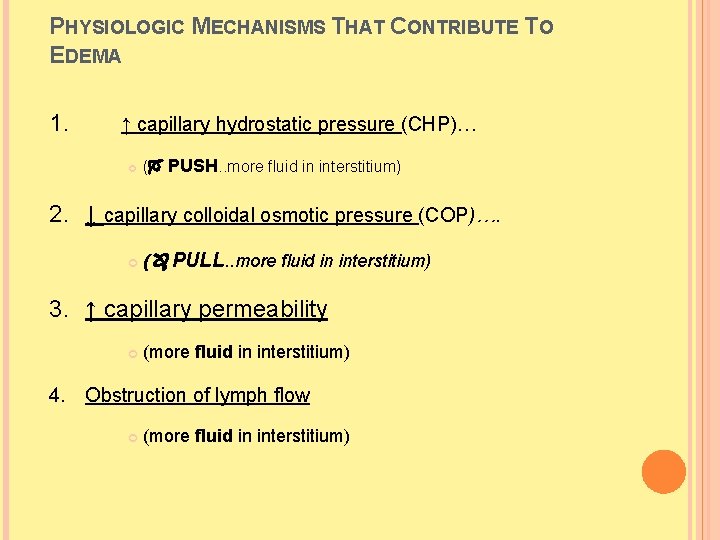
PHYSIOLOGIC MECHANISMS THAT CONTRIBUTE TO EDEMA 1. ↑ capillary hydrostatic pressure (CHP)… ( PUSH. . more fluid in interstitium) 2. ↓ capillary colloidal osmotic pressure (COP)…. ( PULL. . more fluid in interstitium) 3. ↑ capillary permeability (more fluid in interstitium) 4. Obstruction of lymph flow (more fluid in interstitium)
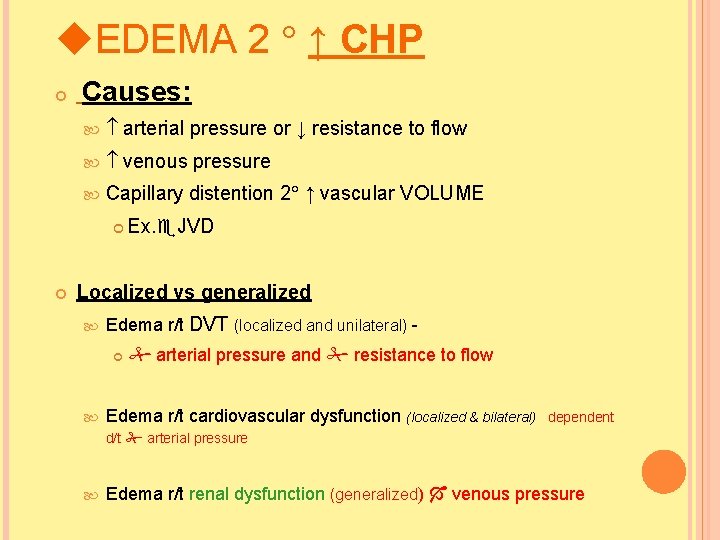
EDEMA 2 ↑ CHP Causes: arterial pressure or ↓ resistance to flow venous pressure Capillary distention 2 ↑ vascular VOLUME Ex. JVD Localized vs generalized Edema r/t DVT (localized and unilateral) arterial pressure and resistance to flow Edema r/t cardiovascular dysfunction (localized & bilateral) dependent d/t arterial pressure Edema r/t renal dysfunction (generalized) venous pressure
DVT: ANIMATION http: //www. nhlbi. nih. gov/healthtopics/dvt/
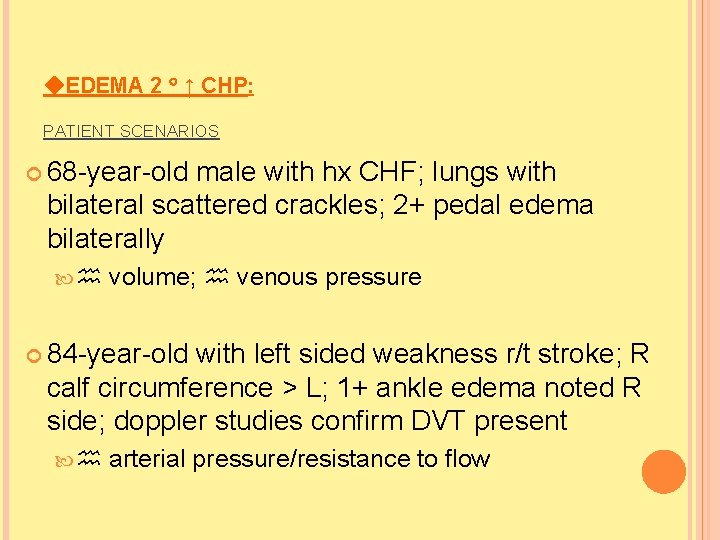
EDEMA 2 ↑ CHP: PATIENT SCENARIOS 68 -year-old male with hx CHF; lungs with bilateral scattered crackles; 2+ pedal edema bilaterally volume; venous pressure 84 -year-old with left sided weakness r/t stroke; R calf circumference > L; 1+ ankle edema noted R side; doppler studies confirm DVT present arterial pressure/resistance to flow
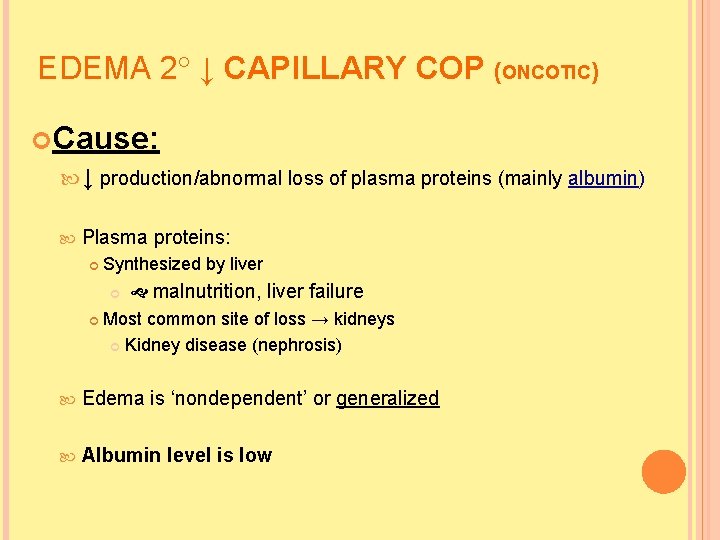
EDEMA 2 ↓ CAPILLARY COP (ONCOTIC) Cause: ↓ production/abnormal loss of plasma proteins (mainly albumin) Plasma proteins: Synthesized by liver malnutrition, liver failure Most common site of loss → kidneys Kidney disease (nephrosis) Edema is ‘nondependent’ or generalized Albumin level is low
VEDEMA 2º CAPILLARY COP: (LOW ALBUMIN PRESENT) PATIENT SCENARIOS 52 -year-old male with hx ETOH abuse, liver failure and cirrhosis, ascites and generalized swelling 42 -year-old female with severe chronic malnutrition; serum albumin = 1. 6 g/dl; 1+ non-pitting edema in hands/feet bilaterally
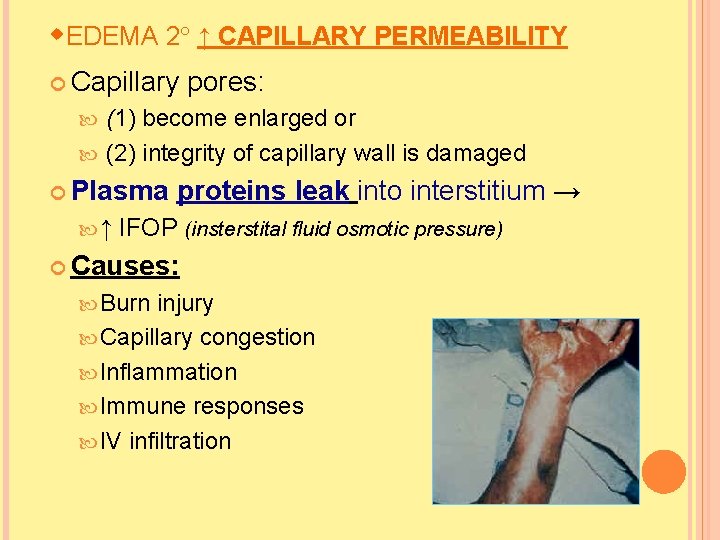
EDEMA 2 ↑ CAPILLARY PERMEABILITY Capillary pores: (1) become enlarged or (2) integrity of capillary wall is damaged Plasma ↑ proteins leak into interstitium → IFOP (insterstital fluid osmotic pressure) Causes: Burn injury Capillary congestion Inflammation Immune responses IV infiltration
EDEMA 2 ↑ CAPILLARY PERMEABILITY: PATIENT SCENARIO 6 -year-old male received partial and fullthickness burns on 25% of body; generalized edema/oozing from tissues noted Damaged capillary wall
EDEMA 2 OBSTRUCTION OF LYMPH FLOW “Lymphedema” Edema due to impaired lymph flow Lymph system normally allows for movement of plasma proteins that cannot be reabsorbed via pores in capillary membrane back into circulatory system Causes of obstruction: Malignant involvement of lymph structures Removal of lymph nodes r/t cancer Infection involving lymph nodes (lymphangitis)
EDEMA 2 OBSTRUCTION OF LYMPH FLOW: PATIENT SCENARIO 57 -year-old female diagnosed with breast cancer undergoes right-sided radical mastectomy; no B/P’s/IV’s in R arm; R arm 1+ nonpitting edema noted
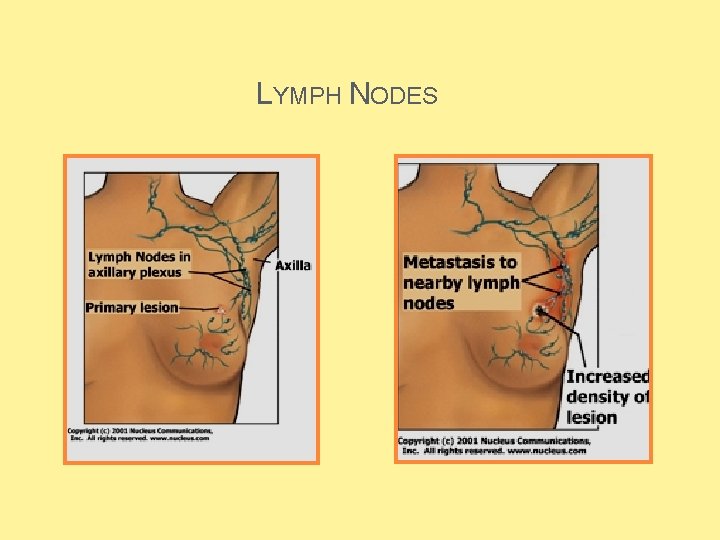
LYMPH NODES
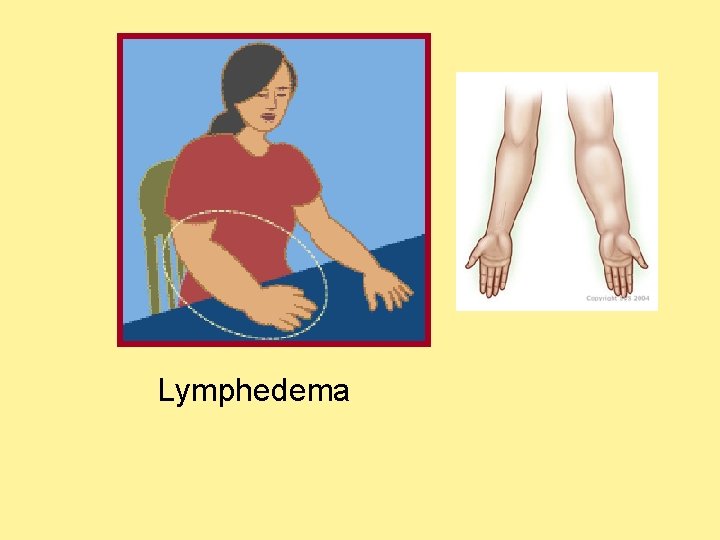
Lymphedema
EDEMA: ASSESSMENT Assessment Location Localized Limited to site of trauma Sprained ankle, DVT Generalized 1. Dependent Ex. , cardiovascular and renal dysfunction 2. Nondependent (generalized) Ex. , Burns, malnutrition
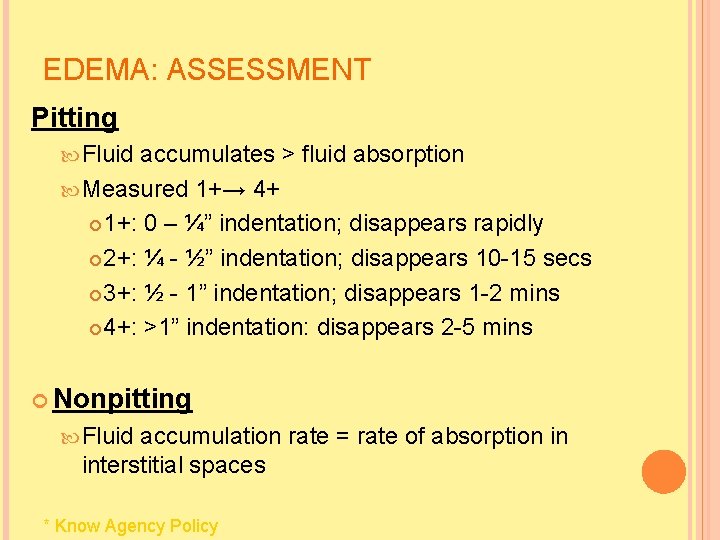
EDEMA: ASSESSMENT Pitting Fluid accumulates > fluid absorption Measured 1+→ 4+ 1+: 0 – ¼” indentation; disappears rapidly 2+: ¼ - ½” indentation; disappears 10 -15 secs 3+: ½ - 1” indentation; disappears 1 -2 mins 4+: >1” indentation: disappears 2 -5 mins Nonpitting Fluid accumulation rate = rate of absorption in interstitial spaces * Know Agency Policy
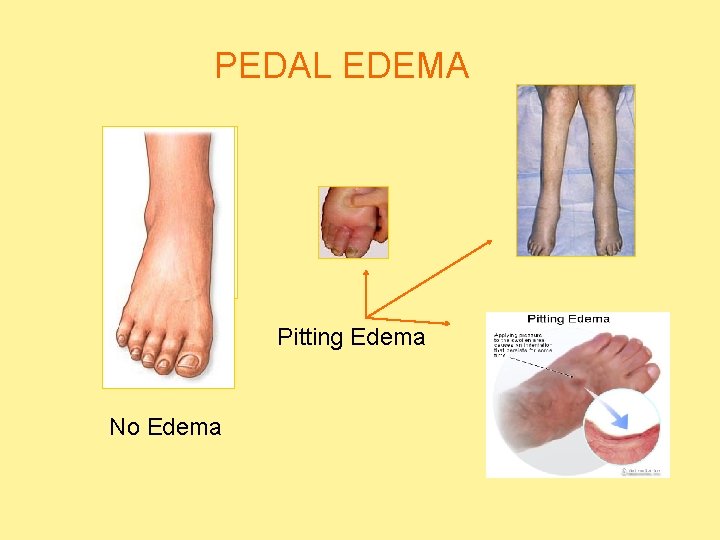
PEDAL EDEMA Pitting Edema No Edema
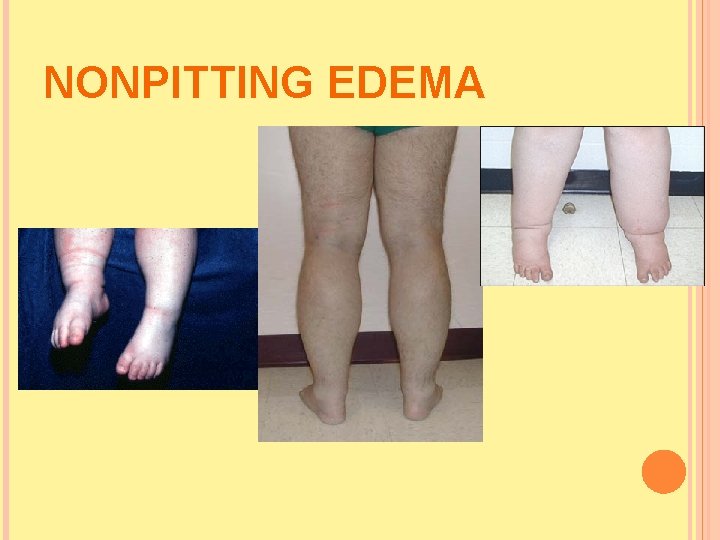
NONPITTING EDEMA
THIRD - SPACING A shift of fluid from intravascular space to a portion of body in which the fluid is not easily exchanged with rest of ECF (unavailable for functional use) <Fluid shifts to the ‘transcellular compartment’>
THIRD SPACING Shift of fluid from intravascular compartment into that “third” space Usually a serous cavity (“transcellular”) Joints, cererospinal, peritoneum, pleura Problem: Fluids in the 3 rd space tend to accumulate rather than reabsorb Exudative fluids (from inflammatory conditions) usually protein/albumin rich Protein rich attract even more fluid into space Transudative fluids (from liver failure) low in protein/albumin…so can’t hold fluid in the intravascular space Ascites develops d/t decreased capillary pressure allowing fluid to leak out of intravascular space into the peritoneum
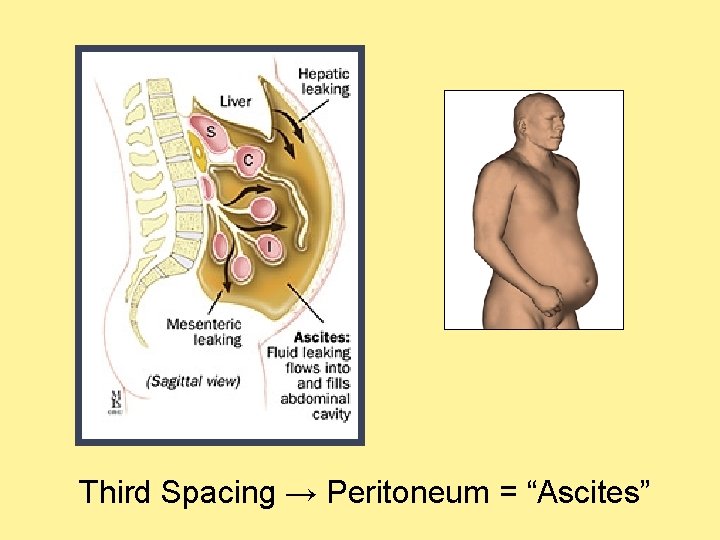
Third Spacing → Peritoneum = “Ascites”
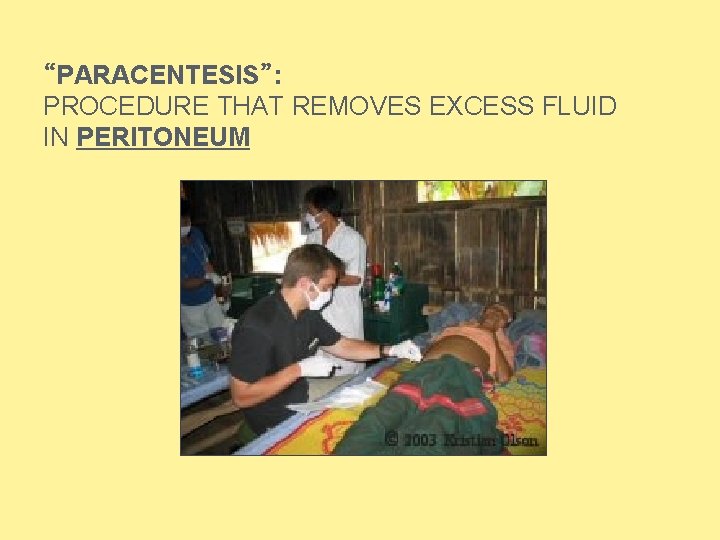
“PARACENTESIS”: PROCEDURE THAT REMOVES EXCESS FLUID IN PERITONEUM
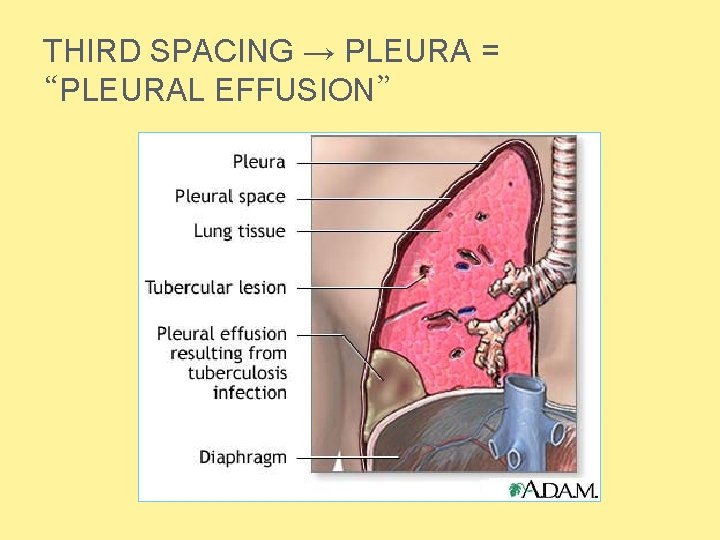
THIRD SPACING → PLEURA = “PLEURAL EFFUSION”
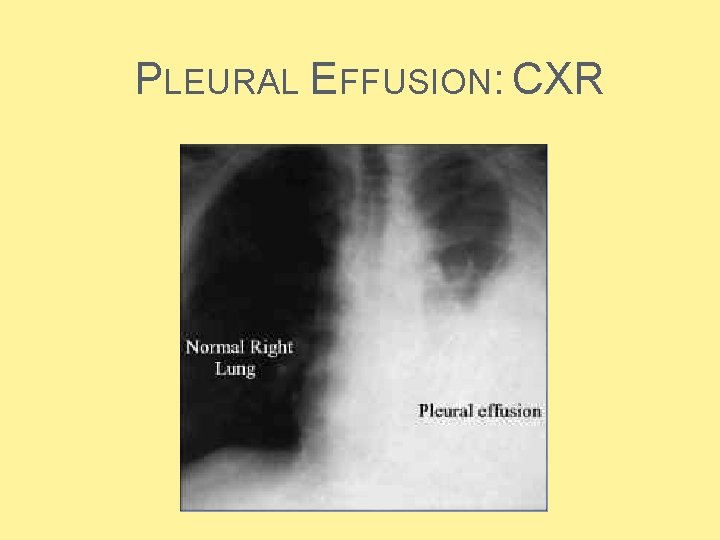
PLEURAL EFFUSION: CXR
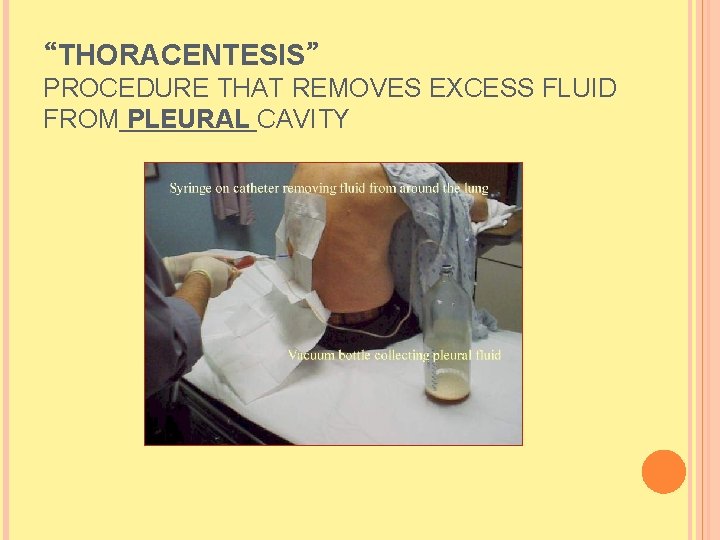
“THORACENTESIS” PROCEDURE THAT REMOVES EXCESS FLUID FROM PLEURAL CAVITY
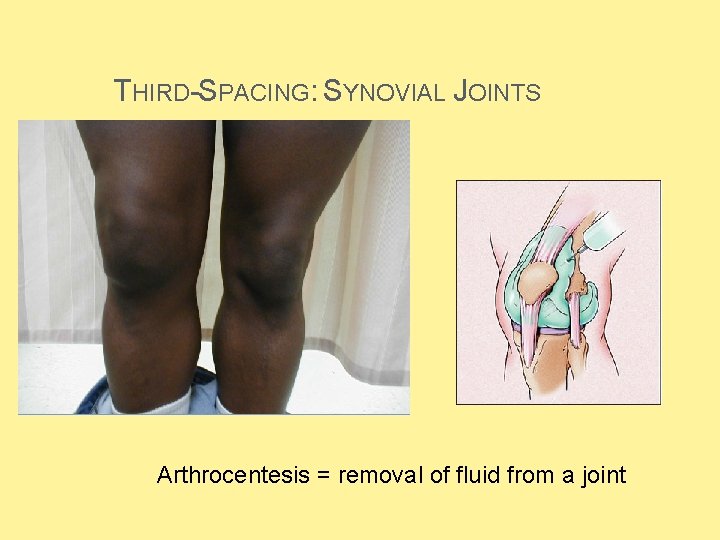
THIRD-SPACING: SYNOVIAL JOINTS Arthrocentesis = removal of fluid from a joint
ELECTROLYTE IMBALANCES: KEY CONCEPTS
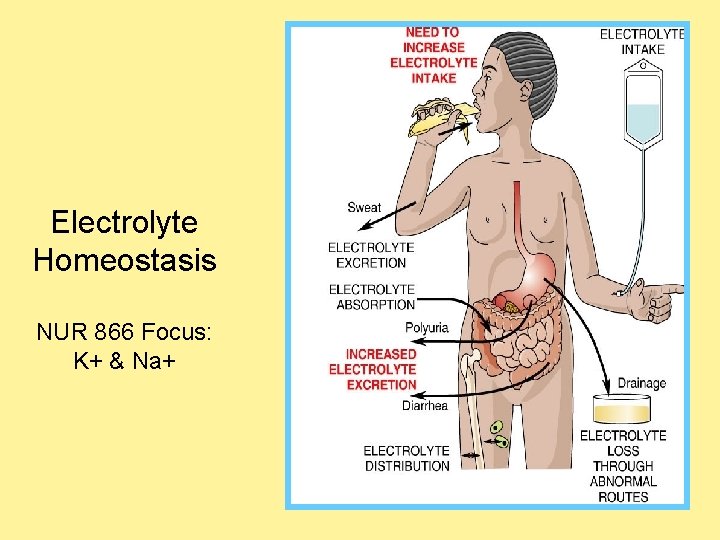
Electrolyte Homeostasis NUR 866 Focus: K+ & Na+
SODIUM “NA+” Needed for: Maintaining water balance (osmolality) “Salt Sucks” water follows salt Transmitting Contracting Normal nerve impulses muscles serum levels = 135 – 145 m. Eq/L
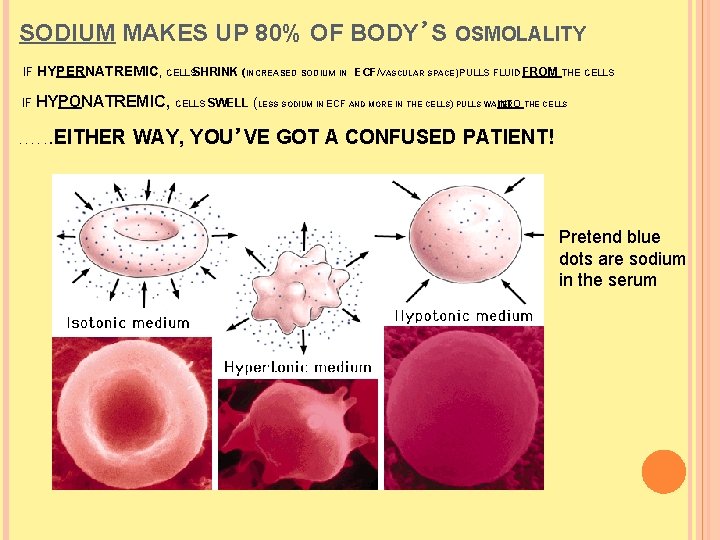
SODIUM MAKES UP 80% OF BODY’S OSMOLALITY IF HYPERNATREMIC, CELLSSHRINK (INCREASED SODIUM IN ECF/VASCULAR SPACE) PULLS FLUID FROM THE CELLS IF HYPONATREMIC, . . . CELLS SWELL (LESS SODIUM IN ECF AND MORE IN THE CELLS) PULLS WATER INTO THE CELLS EITHER WAY, YOU’VE GOT A CONFUSED PATIENT! Pretend blue dots are sodium in the serum
HYPONATREMIA (MOST FREQUENT ELECTROLYTE DISORDER IN CLINICAL PRACTICE!!)
HYPONATREMIA Low < serum sodium 135 m. Eq/L Associated with hypo-osmolality Causes: Excess Na+ loss Renal (Diuretics) GI (N/V/D, NG suction) Skin (Burns, wound drainage) Excess H²O gain Excessive hypotonic IVF’s or IVF without sodium DILUTIONAL HYPONATREMIA Polydipsia Diseases (SIADH <Syndrome of Inappropriate ADH>)
HYPONATREMIA Signs & Symptoms Anorexia Confusion, personality change * (ICF swells) Muscle weakness (need NA to conduct nerve impulses) SEIZURES Hypotension
HYPONATREMIA Treatment: Sodium replacement PO or IV IV – NS 0. 9% 3 -5% Fluid “to Very restriction reconstitute the serum” important to“GRADUALLY” treat the cause of the problem; give cells time to adapt to fluid shifts
HYPERNATREMIA -- VIRTUALLY NEVER SEEN IN AN ALERT PERSON WITH NORMAL THIRST MECHANISM WHO HAS ACCESS TO WATER
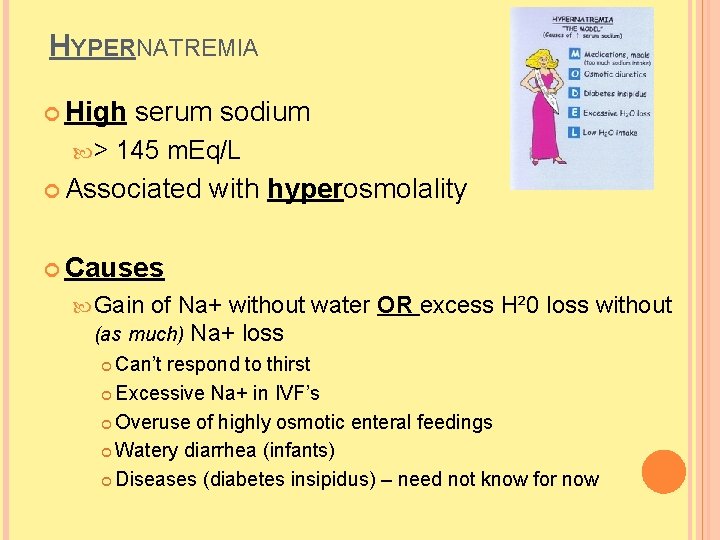
HYPERNATREMIA High > serum sodium 145 m. Eq/L Associated with hyperosmolality Causes Gain of Na+ without (as much) Na+ loss water OR excess H² 0 loss without Can’t respond to thirst Excessive Na+ in IVF’s Overuse of highly osmotic enteral feedings Watery diarrhea (infants) Diseases (diabetes insipidus) – need not know for now
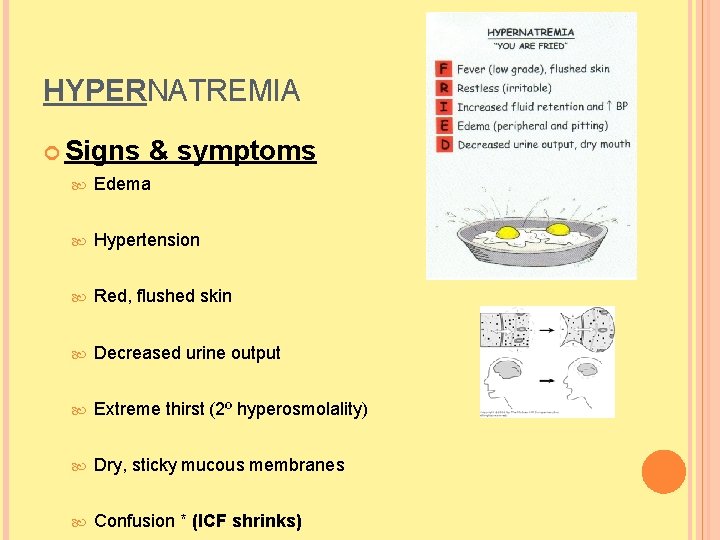
HYPERNATREMIA Signs & symptoms Edema Hypertension Red, flushed skin Decreased urine output Extreme thirst (2º hyperosmolality) Dry, sticky mucous membranes Confusion * (ICF shrinks)
HYPERNATREMIA Treatment: If water loss is cause, water needs to be added If sodium excess is cause, sodium needs to be removed Gradually treat the cause of the problem; give cells time to adapt to fluid shifts
REMEMBER THE RULES ABOUT FLUID SHIFTS & SODIUM/PROTEIN! Water follows sodium salt sucks …. and Water follows protein …. also Water follows glucose
POTASSIUM “K+” Needed for: Cardiac function Neural function Muscle function Normal serum levels = 3. 5 – 5. 0 m. Eq/L
POTASSIUM PROBLEMS: HYPOKALEMIA Low < serum potassium 3. 5 m. Eq/L Causes: ↑ K+ loss Via kidneys - diuretics Via GI tract – vomiting K+ intake (need 10 -30 m. Eq/day) Shift of K+ from ECF to ICF (K goes into the cells, serum level decreases)
HYPOKALEMIA: S&S Signs & Symptoms Cardiac Muscle Leg disturbances weakness cramps bowel sounds/decreased motility
HYPOKALEMIA: PHARMACOLOGIC TREATMENT Potassium chloride (KCl) Indications Treat/prevent K+ depletions when dietary measures prove inadequate Nursing for use: Implications: Oral liquids: dilute with water/juice to ↓ GI distress; taste awful!; powders, tablets; may cause GI ulcers/bleeding; assess for N/V, GI pain/bleeding
HYPOKALEMIA: PHARMACOLOGIC TREATMENT Potassium Nursing chloride Implications (cont): IV: MUST BE DILUTED!!! and ADMINISTERED SLOWLY give only to clients with documented urine output; may cause phlebitis/pain; IV solutions should not contain more than 40 m. Eq/L of K+; rate should not exceed 10 -20 m. Eq/hr Contraindicated: Renal failure (K levels already high, kidneys can’t excrete) Nurse should akways question an order to give KCL to a patient on dialysis Those receiving potassium-sparing diuretics
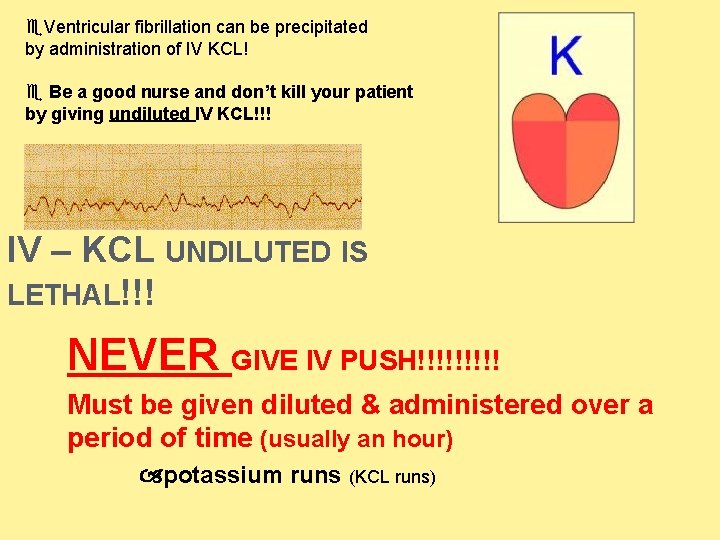
Ventricular fibrillation can be precipitated by administration of IV KCL! Be a good nurse and don’t kill your patient by giving undiluted IV KCL!!! IV – KCL UNDILUTED IS LETHAL!!! NEVER GIVE IV PUSH!!!!! Must be given diluted & administered over a period of time (usually an hour) potassium runs (KCL runs)
POTASSIUM PROBLEMS: HYPERKALEMIA High > serum potassium 5. 0 m. Eq/L Causes: ↑ K+ intake (po or IV) ↓ K+ excretion – most common cause (renal) Shift of K+ from ICF to ECF Acid-base problem Acidosis – excess H+ shifts into cells & shifts K+ out Massive cell injury K+ escapes into serum (burns)
HYPERKALEMIA TREATMENT Emergency vs. Subacute…
HYPERKALEMIA: TREATMENT EMERGENCY A number of IV meds… Na. HCO 3 (sodium bicarbonate) Calcium gluconate Glucose/insulin Dialysis
Hemodialysis
HYPERKALEMIA: TREATMENT SUBACUTE Treat cause of problem Discontinue Cation exchange resins (i. e. , Kayexalate)~q 6 hrs K+ supplements; limit K+-rich foods Exhanges sodium ions for potassium ions in the intestine Administered enterally via feeding tube or retention enema Effect not seen for several hours to 1 day after administration
THE END
- Slides: 75