Pathology Phase 2 a Recap Olivia Stevens and

- Slides: 48
Pathology Phase 2 a Recap Olivia Stevens and Judith Scott
What we’ll cover: • Inflammation • Thrombosis and emboli • Infarction • Cell growth and death • Classification of tumours • Mechanisms of carcinogenesis • Main tumour types
Inflammation 2 types Acute and Chronic Acute • • Initial response of tissue to injury Early onset (seconds to minutes) Short duration (hours to days) Cells involved = neutrophils and monocytes • Acute Inflammation Steps: • Vascular component: dilation of vessels • Exudative component: vascular leakage of protein-rich fluid • Neutrophil polymorph: cells type recruited to tissue
Acute Inflammation Causes • Microbial infections – bacteria, viruses • Hypersensitivity reactions – parasites • Physical agents – trauma, heat, cold • Chemicals – corrosives, acids • Bacterial toxins • Tissue necrosis – ischemic infarction Appearance: • • • Rubor – redness; due to dilation of small vessels) Calor – heat; only seen peripherally Tumor – swelling; results from oedema or a physical mass Dolor - pain Loss of function
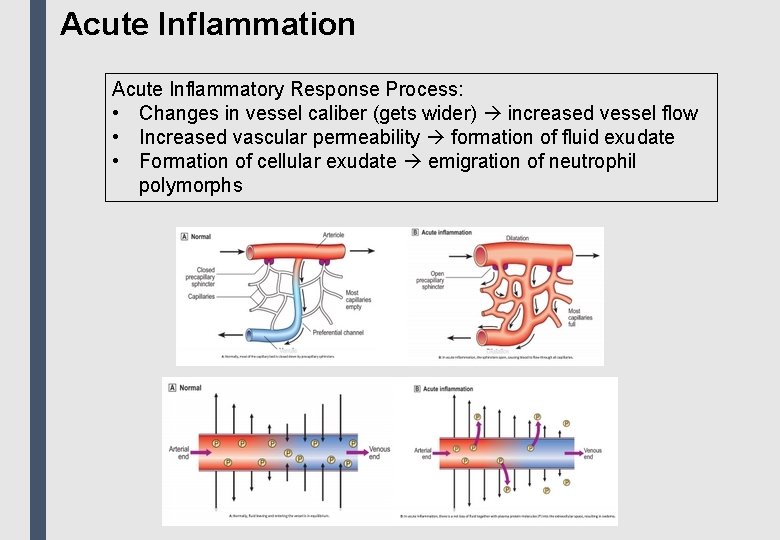
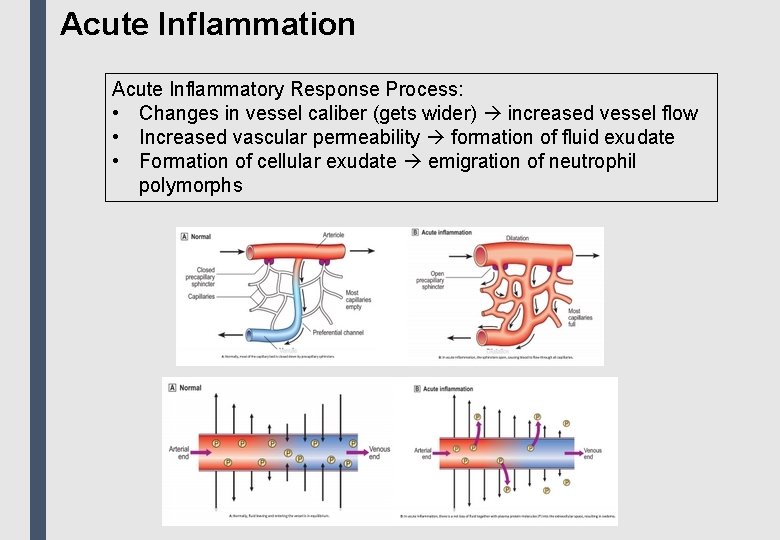
Acute Inflammation Acute Inflammatory Response Process: • Changes in vessel caliber (gets wider) increased vessel flow • Increased vascular permeability formation of fluid exudate • Formation of cellular exudate emigration of neutrophil polymorphs
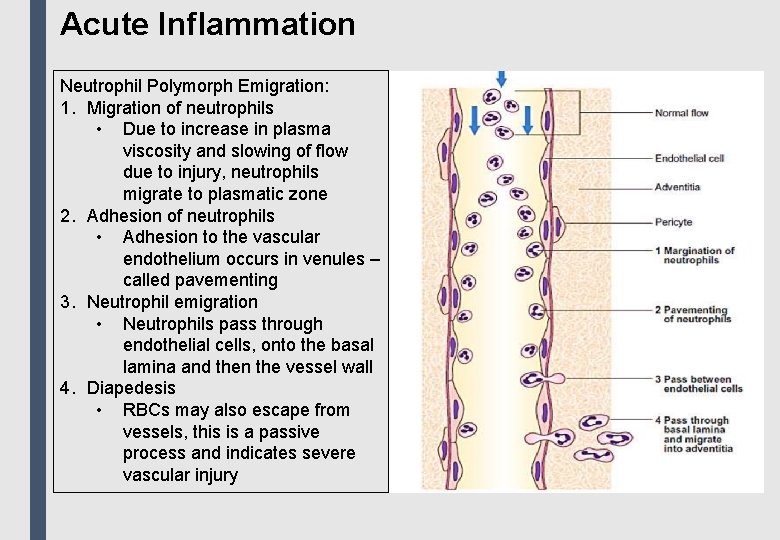
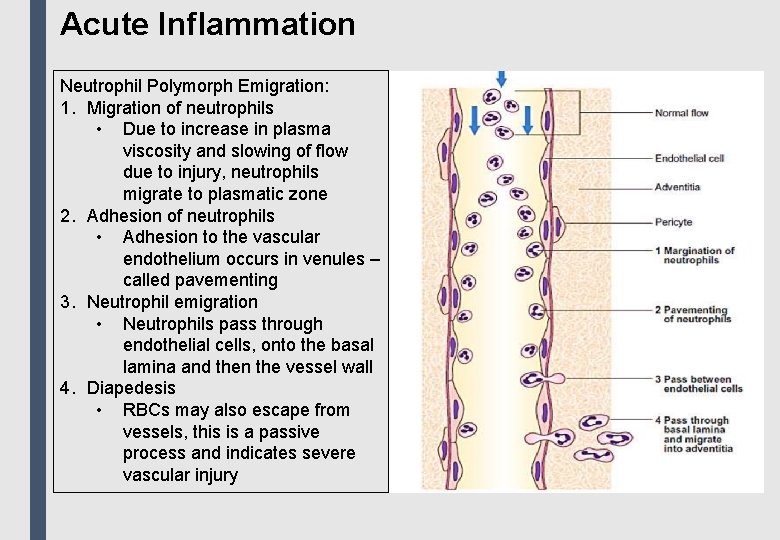
Acute Inflammation Neutrophil Polymorph Emigration: 1. Migration of neutrophils • Due to increase in plasma viscosity and slowing of flow due to injury, neutrophils migrate to plasmatic zone 2. Adhesion of neutrophils • Adhesion to the vascular endothelium occurs in venules – called pavementing 3. Neutrophil emigration • Neutrophils pass through endothelial cells, onto the basal lamina and then the vessel wall 4. Diapedesis • RBCs may also escape from vessels, this is a passive process and indicates severe vascular injury
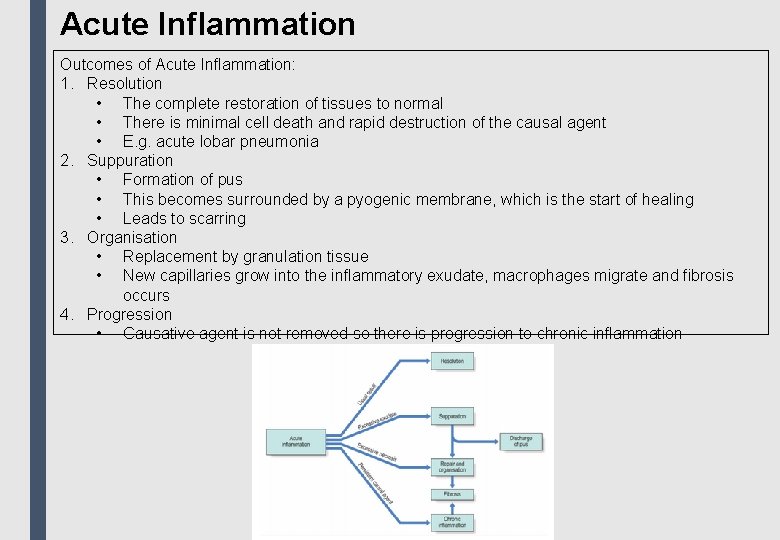
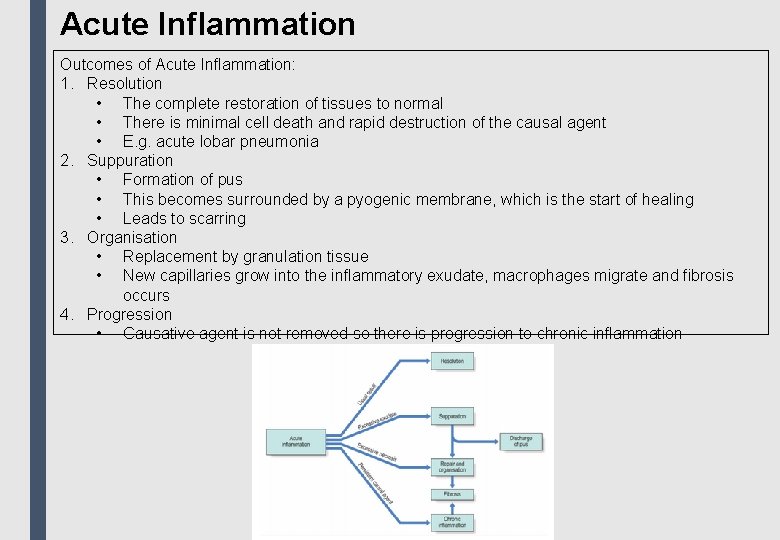
Acute Inflammation Outcomes of Acute Inflammation: 1. Resolution • The complete restoration of tissues to normal • There is minimal cell death and rapid destruction of the causal agent • E. g. acute lobar pneumonia 2. Suppuration • Formation of pus • This becomes surrounded by a pyogenic membrane, which is the start of healing • Leads to scarring 3. Organisation • Replacement by granulation tissue • New capillaries grow into the inflammatory exudate, macrophages migrate and fibrosis occurs 4. Progression • Causative agent is not removed so there is progression to chronic inflammation
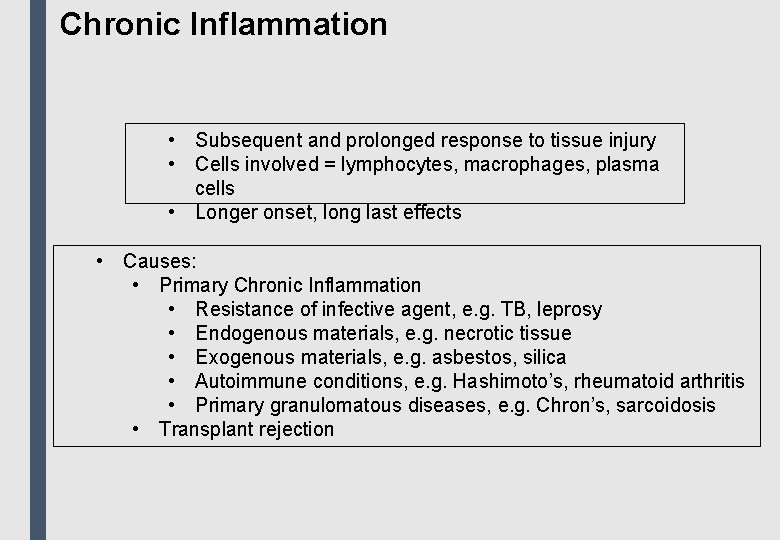
Chronic Inflammation • Subsequent and prolonged response to tissue injury • Cells involved = lymphocytes, macrophages, plasma cells • Longer onset, long last effects • Causes: • Primary Chronic Inflammation • Resistance of infective agent, e. g. TB, leprosy • Endogenous materials, e. g. necrotic tissue • Exogenous materials, e. g. asbestos, silica • Autoimmune conditions, e. g. Hashimoto’s, rheumatoid arthritis • Primary granulomatous diseases, e. g. Chron’s, sarcoidosis • Transplant rejection
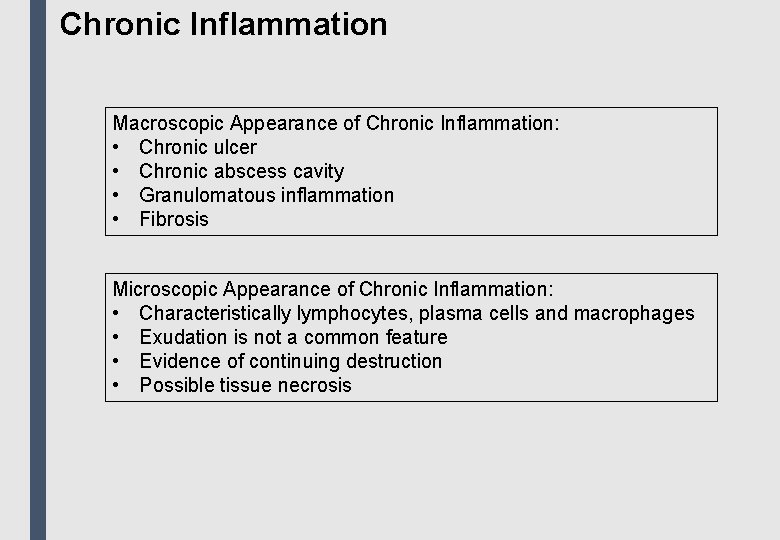
Chronic Inflammation Macroscopic Appearance of Chronic Inflammation: • Chronic ulcer • Chronic abscess cavity • Granulomatous inflammation • Fibrosis Microscopic Appearance of Chronic Inflammation: • Characteristically lymphocytes, plasma cells and macrophages • Exudation is not a common feature • Evidence of continuing destruction • Possible tissue necrosis
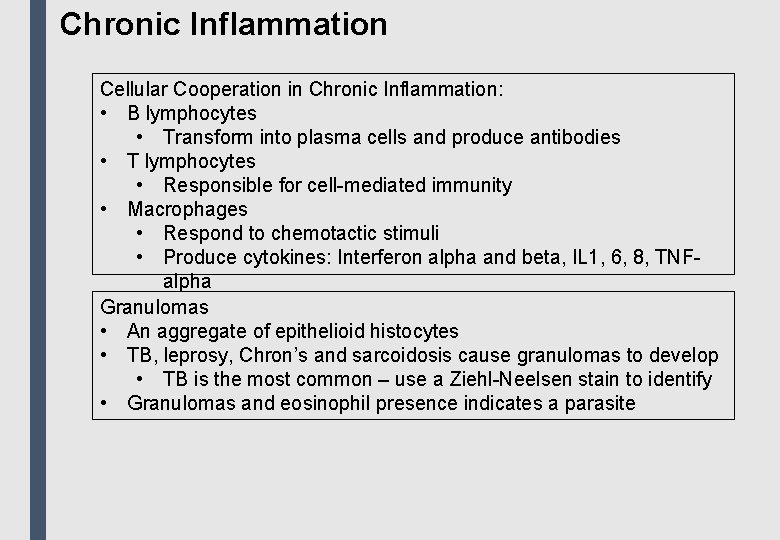
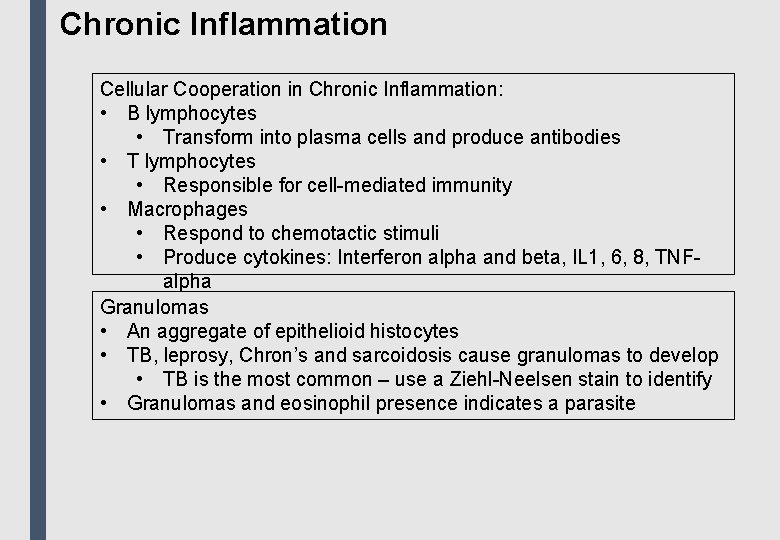
Chronic Inflammation Cellular Cooperation in Chronic Inflammation: • B lymphocytes • Transform into plasma cells and produce antibodies • T lymphocytes • Responsible for cell-mediated immunity • Macrophages • Respond to chemotactic stimuli • Produce cytokines: Interferon alpha and beta, IL 1, 6, 8, TNFalpha Granulomas • An aggregate of epithelioid histocytes • TB, leprosy, Chron’s and sarcoidosis cause granulomas to develop • TB is the most common – use a Ziehl-Neelsen stain to identify • Granulomas and eosinophil presence indicates a parasite
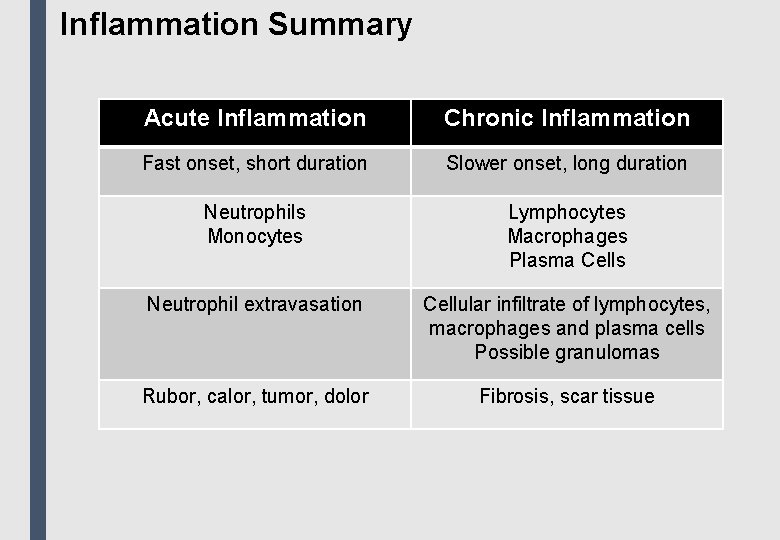
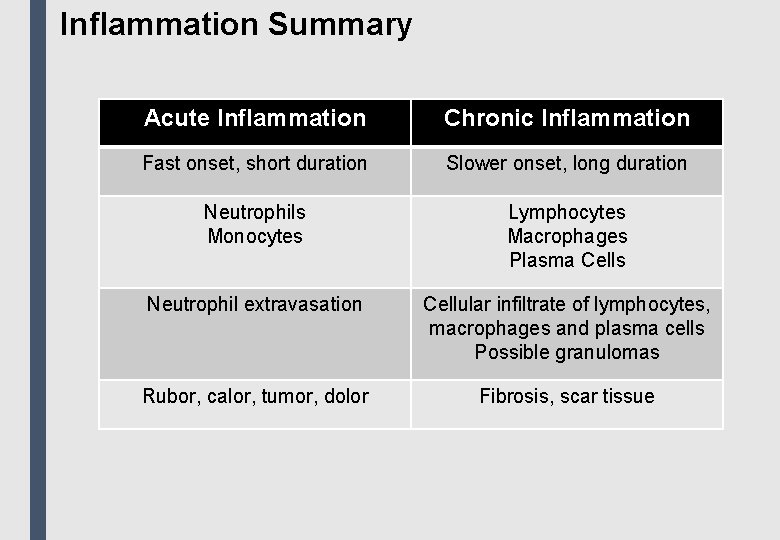
Inflammation Summary Acute Inflammation Chronic Inflammation Fast onset, short duration Slower onset, long duration Neutrophils Monocytes Lymphocytes Macrophages Plasma Cells Neutrophil extravasation Cellular infiltrate of lymphocytes, macrophages and plasma cells Possible granulomas Rubor, calor, tumor, dolor Fibrosis, scar tissue
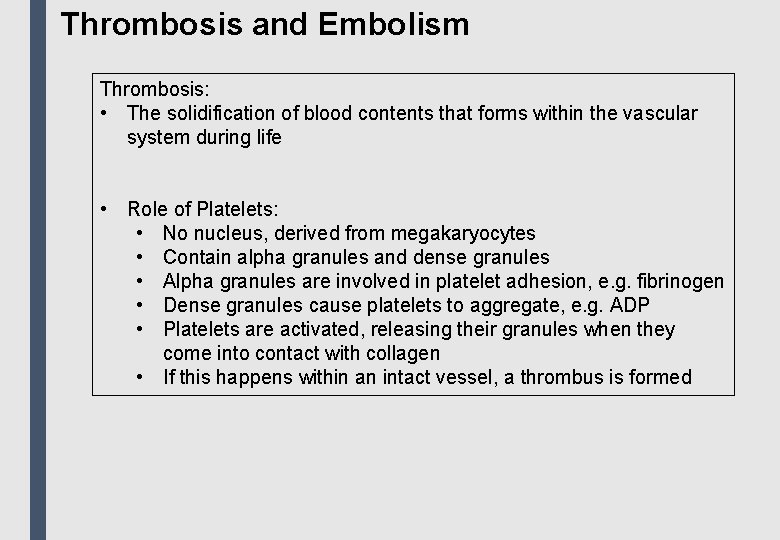
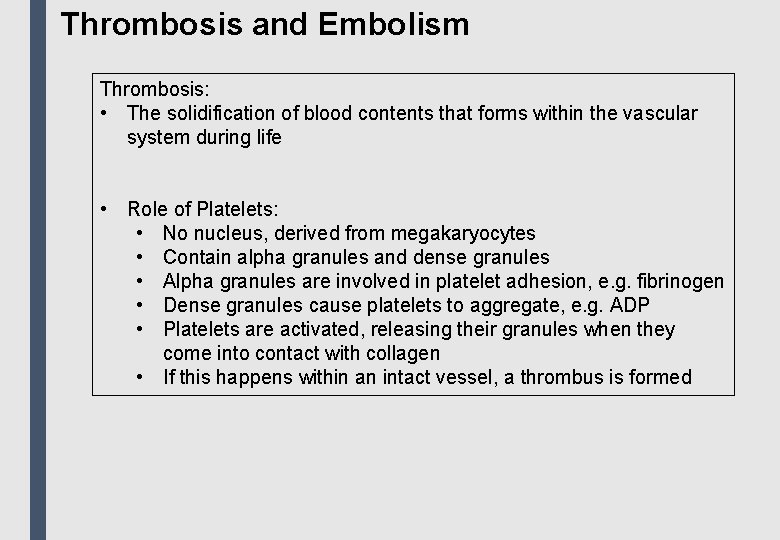
Thrombosis and Embolism Thrombosis: • The solidification of blood contents that forms within the vascular system during life • Role of Platelets: • No nucleus, derived from megakaryocytes • Contain alpha granules and dense granules • Alpha granules are involved in platelet adhesion, e. g. fibrinogen • Dense granules cause platelets to aggregate, e. g. ADP • Platelets are activated, releasing their granules when they come into contact with collagen • If this happens within an intact vessel, a thrombus is formed
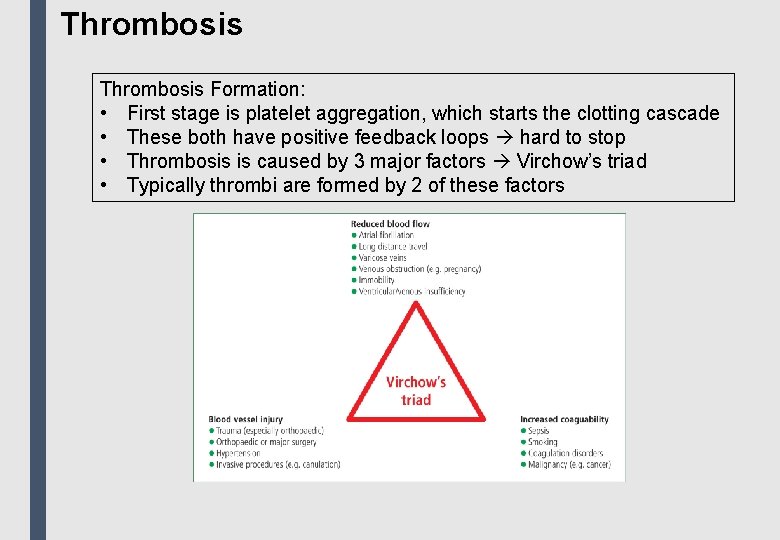
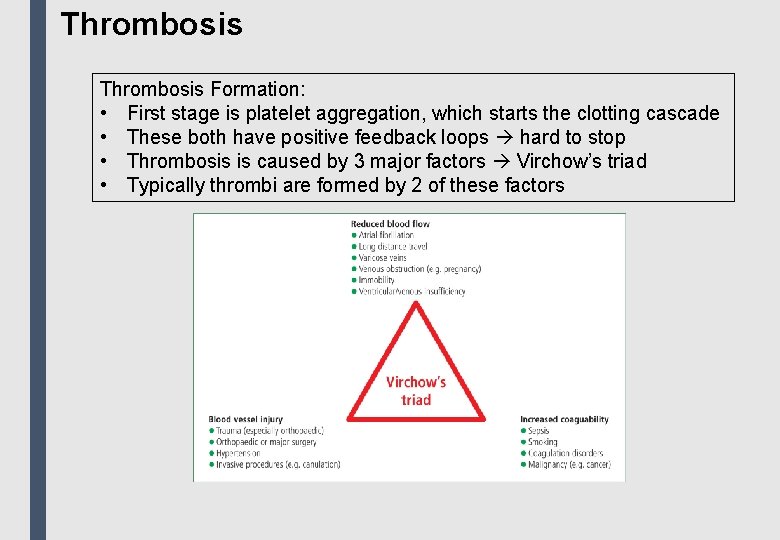
Thrombosis Formation: • First stage is platelet aggregation, which starts the clotting cascade • These both have positive feedback loops hard to stop • Thrombosis is caused by 3 major factors Virchow’s triad • Typically thrombi are formed by 2 of these factors
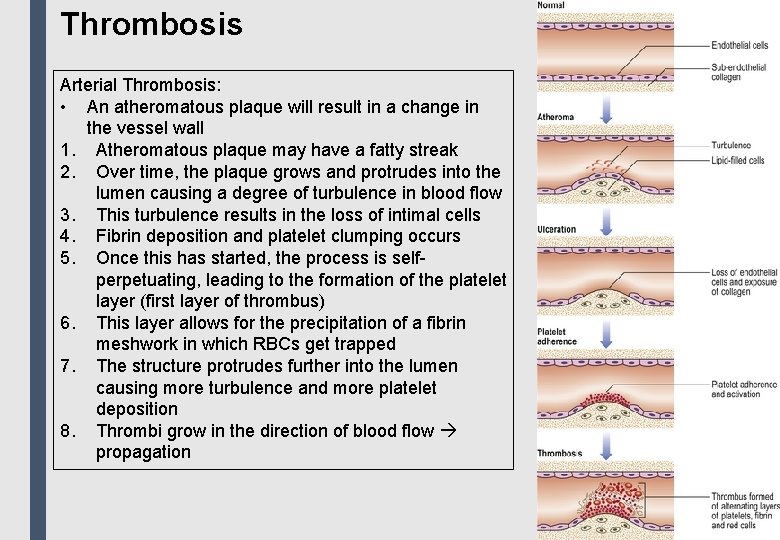
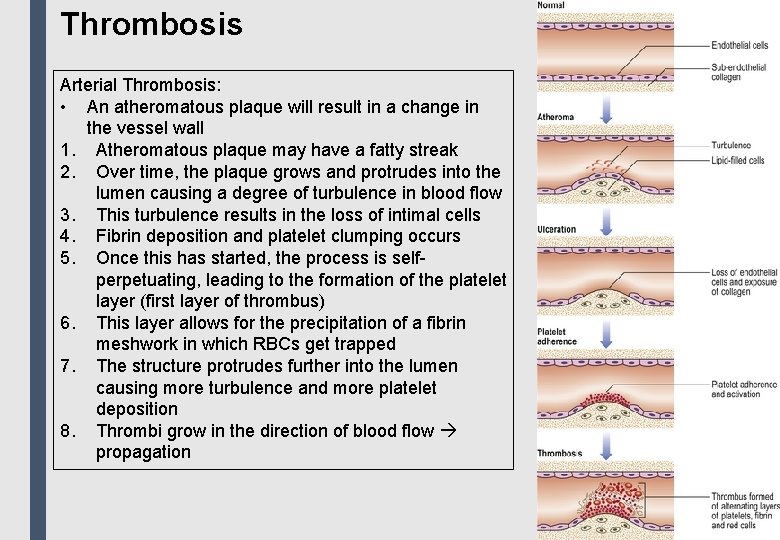
Thrombosis Arterial Thrombosis: • An atheromatous plaque will result in a change in the vessel wall 1. Atheromatous plaque may have a fatty streak 2. Over time, the plaque grows and protrudes into the lumen causing a degree of turbulence in blood flow 3. This turbulence results in the loss of intimal cells 4. Fibrin deposition and platelet clumping occurs 5. Once this has started, the process is selfperpetuating, leading to the formation of the platelet layer (first layer of thrombus) 6. This layer allows for the precipitation of a fibrin meshwork in which RBCs get trapped 7. The structure protrudes further into the lumen causing more turbulence and more platelet deposition 8. Thrombi grow in the direction of blood flow propagation
Thrombosis Venous Thrombosis: • There is lower blood pressure in veins and atheroma do not occur • Thrombi begin at valves • Valves produce a degree of turbulence, and can be damaged, e. g. trauma, stasis • When blood pressure falls, flow through the veins slows, allowing for a thrombus to form Clinical Features: • Arterial thrombi • Loss of pulse distal to thrombus • Area becomes cold, pale and painful • Possible gangrene • Venous thrombi • Tender • Area becomes reddened and swollen
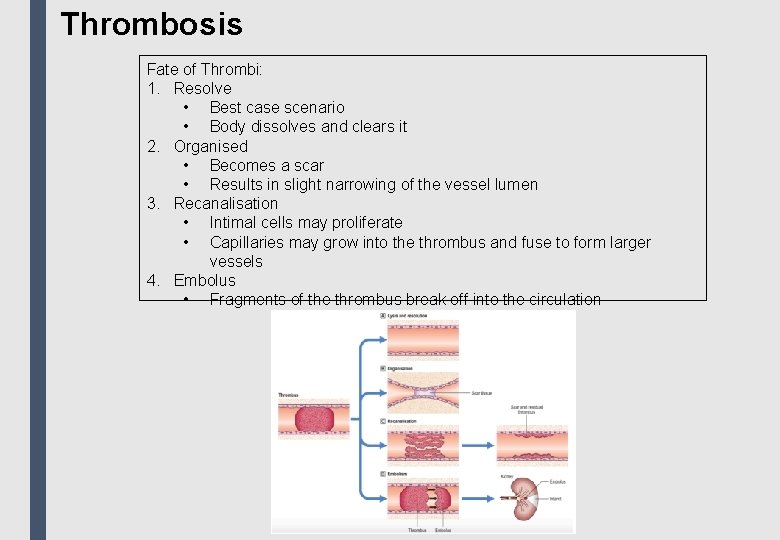
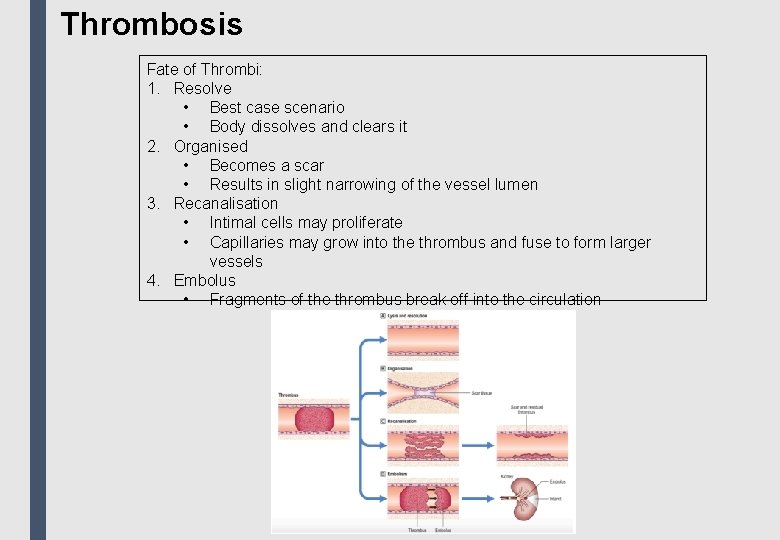
Thrombosis Fate of Thrombi: 1. Resolve • Best case scenario • Body dissolves and clears it 2. Organised • Becomes a scar • Results in slight narrowing of the vessel lumen 3. Recanalisation • Intimal cells may proliferate • Capillaries may grow into the thrombus and fuse to form larger vessels 4. Embolus • Fragments of the thrombus break off into the circulation
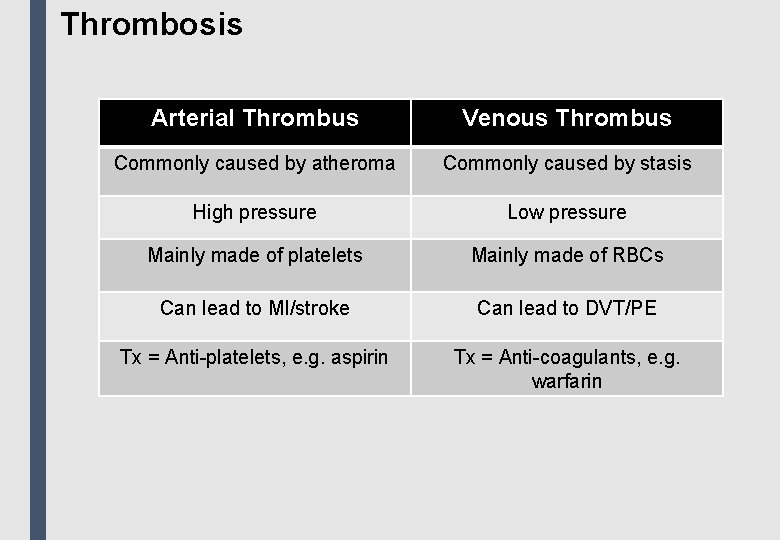
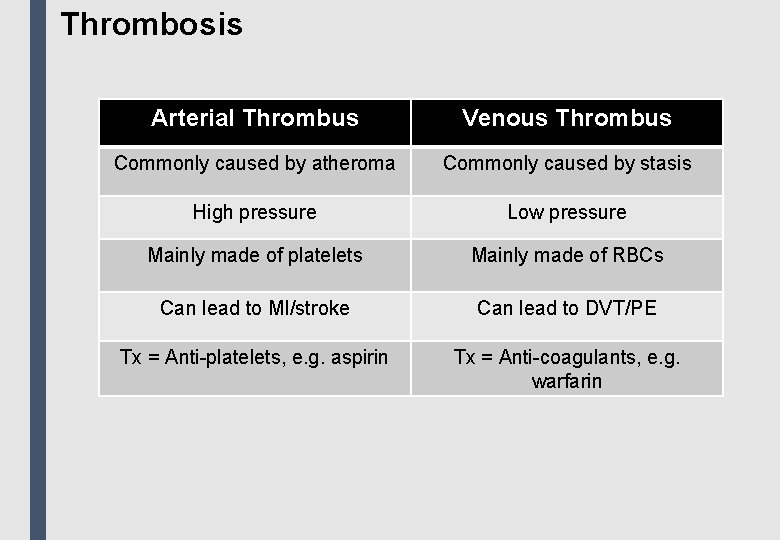
Thrombosis Arterial Thrombus Venous Thrombus Commonly caused by atheroma Commonly caused by stasis High pressure Low pressure Mainly made of platelets Mainly made of RBCs Can lead to MI/stroke Can lead to DVT/PE Tx = Anti-platelets, e. g. aspirin Tx = Anti-coagulants, e. g. warfarin
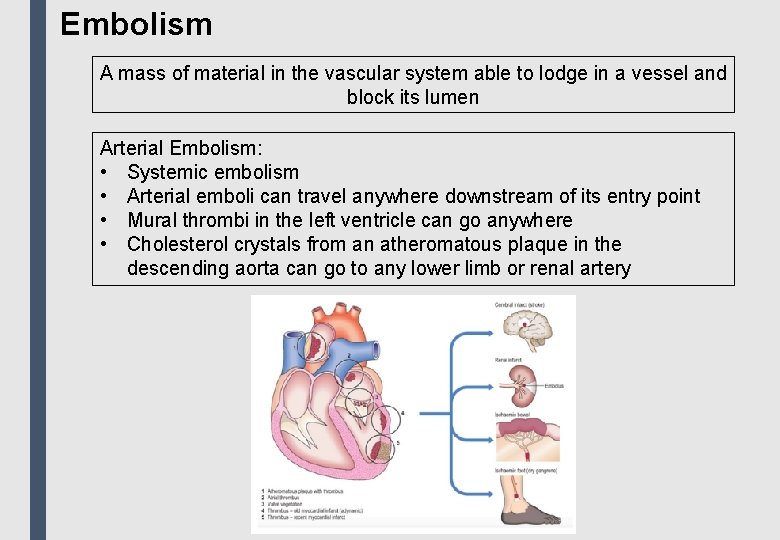
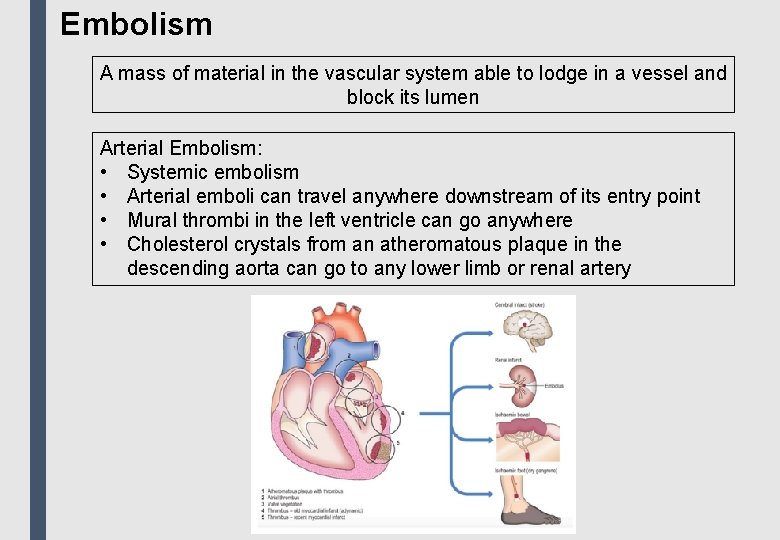
Embolism A mass of material in the vascular system able to lodge in a vessel and block its lumen Arterial Embolism: • Systemic embolism • Arterial emboli can travel anywhere downstream of its entry point • Mural thrombi in the left ventricle can go anywhere • Cholesterol crystals from an atheromatous plaque in the descending aorta can go to any lower limb or renal artery
Embolism Venous Embolism: • Pulmonary embolism • In the venous system, emboli travel to the vena cava and lodge in the pulmonary arteries • This results in a PE • Small emboli • May occur unnoticed • Can cause idiopathic pulmonary hypertension • Large emboli • Can result in acute respiratory or cardiac problems • Resolve slowly • Result in chest pain and shortness of breath • Massive emboli • Result in sudden death • Long thrombi derived from the leg veins • Often impacted across the bifurcation of one of the pulmonary arteries
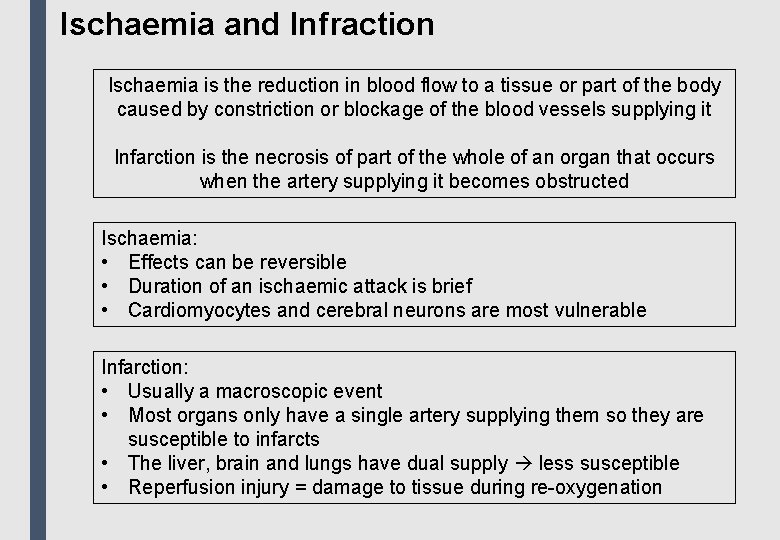
Ischaemia and Infraction Ischaemia is the reduction in blood flow to a tissue or part of the body caused by constriction or blockage of the blood vessels supplying it Infarction is the necrosis of part of the whole of an organ that occurs when the artery supplying it becomes obstructed Ischaemia: • Effects can be reversible • Duration of an ischaemic attack is brief • Cardiomyocytes and cerebral neurons are most vulnerable Infarction: • Usually a macroscopic event • Most organs only have a single artery supplying them so they are susceptible to infarcts • The liver, brain and lungs have dual supply less susceptible • Reperfusion injury = damage to tissue during re-oxygenation
Atherosclerosis Disease characterized by the formation of atherosclerotic plaques in the intima of large and medium-sized arteries, e. g. coronary arteries • Often asymptomatic • The accumulation of lipid, macrophages and smooth muscle cells in intimal plaques • Can cause life-threatening damage if a thrombus forms on a disrupted plaque • Cerebral infraction • Carotid atheroma, leading to TIAs • MI • Aortic aneurysm (can cause sudden death) • Peripheral vascular disease • Gangrene
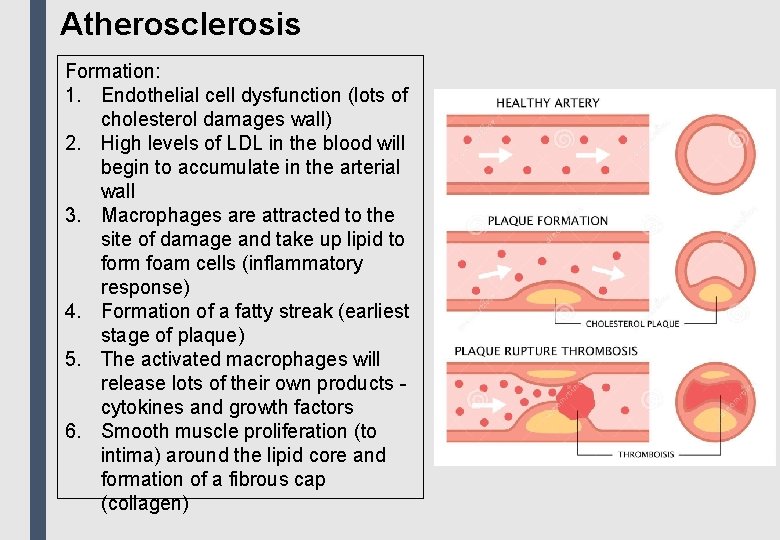
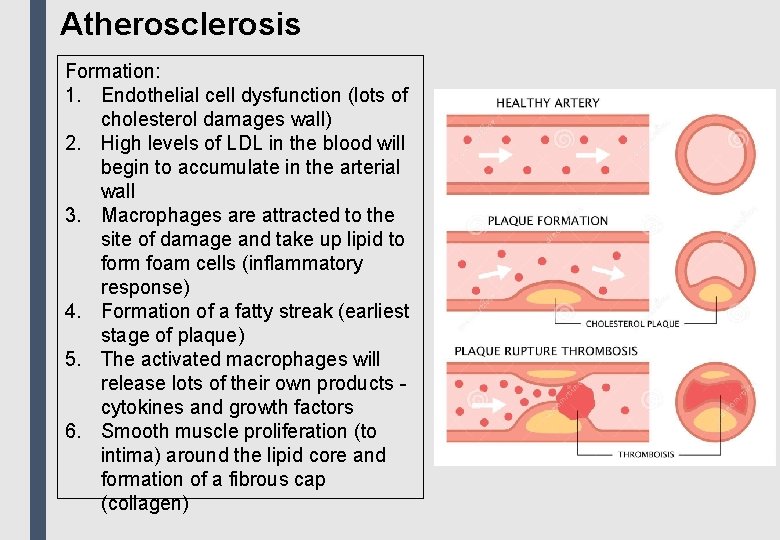
Atherosclerosis Formation: 1. Endothelial cell dysfunction (lots of cholesterol damages wall) 2. High levels of LDL in the blood will begin to accumulate in the arterial wall 3. Macrophages are attracted to the site of damage and take up lipid to form foam cells (inflammatory response) 4. Formation of a fatty streak (earliest stage of plaque) 5. The activated macrophages will release lots of their own products cytokines and growth factors 6. Smooth muscle proliferation (to intima) around the lipid core and formation of a fibrous cap (collagen)
Atherosclerosis Risk Factors: • Hypercholesterolaemia most important risk factor • Smoking • Hypertension • Diabetes • Male sex • Increasing age Preventative Measures: • Smoking cessation • Blood pressure control • Weight reduction • Low dose aspirin inhibits aggregation of platelets • Statins cholesterol reducing drug
Apoptosis and Necrosis Apoptosis is a cellular process in which a defined and programmed sequence of intracellular events leads to the removal of a cell without the release of products harmful to surrounding cells Regulation of Apoptosis: • Inhibitors • Growth factors • Extracellular cell matrix • Sex steroids • Inducers • Glucocorticoids • Free radicals • Ionising radiation • DNA damage
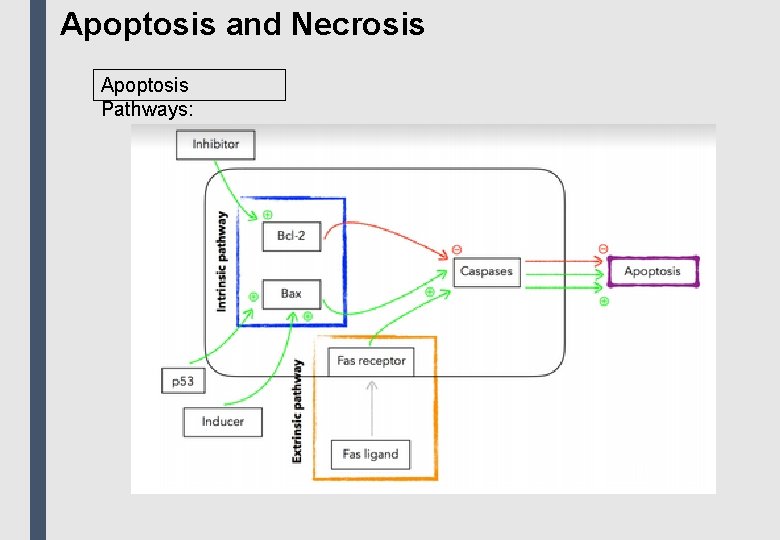
Apoptosis and Necrosis Apoptosis Pathways: Intrinsic: • Uses pro- and anti-apoptotic members of the Blc-2 family • Bax forms Bax-Bax dimers which enhance apoptotic stimuli • The Bcl-2: Bax ratio determines the cell’s susceptibility to apoptotic stimuli • Responds to growth factors and biochemical stress • p 53 gene induces cell cycle arrest and initiates DNA damage repair • If damage is difficult to repair, p 53 can induce apoptosis Extrinsic: • Ligand-binding at death receptors on the cell surface • Receptors include TNFR 1 and CD 95 • Ligand-binding results in the clustering or receptor molecules on the cell surface and the initiation of signal transduction cascade • Caspases are activated, triggering apoptosis • This pathway is used by the immune system to eliminate lymphocytes
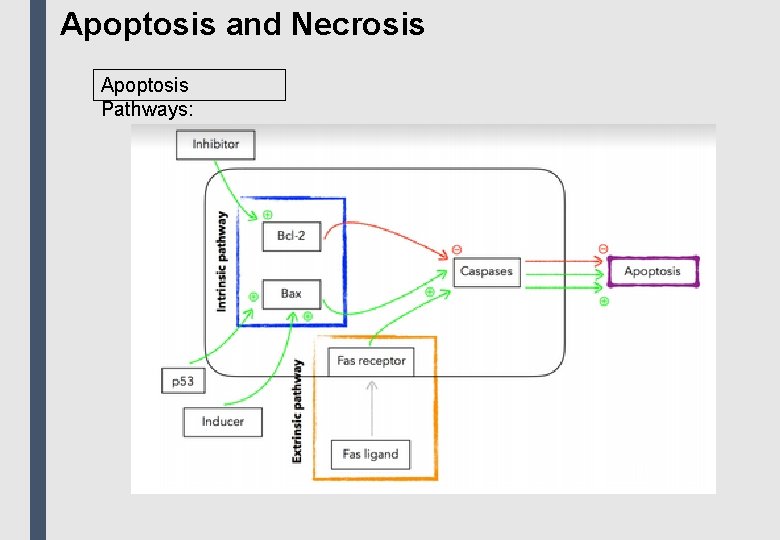
Apoptosis and Necrosis Apoptosis Pathways:
Apoptosis and Necrosis is traumatic cell death which indices inflammation and repair • Characterised by bioenergetic failure and loss of plasma membrane integrity • Coagulative necrosis • Most common type • Can occur in most organs • Cause by ischaemia • Liquefactive necrosis • Occurs in the brain due to its lack of substantial supporting stroma • Caseous necrosis • Causes a ‘cheese’ pattern • TB is characterized by this form of necrosis • Gangrene • Necrosis with rotting of the tissue • Affected tissue appears black due to deposition of iron sulphide (from degraded haemoglobin)
Cell Growth and Other Tissue Changes Hypertrophy: • Increase in cell size without cell division • Muscle hypertrophy can be seen in athletes due to increased muscle activity • Uterine hypertrophy is seen in pregnancy Hyperplasia: • Increase in cell number by mitosis • This can only happen in cells that divide cannot happen in myocardial cells or nerve cells • Hyperplasia of bone marrow cells can be seen in those living at high altitudes Atrophy: • The decrease in the size of an organ or cell be reduction in cell size and/or number • Occurs naturally during the development of the GU tract • Occurs in disease, e. g. muscle atrophy in ALS
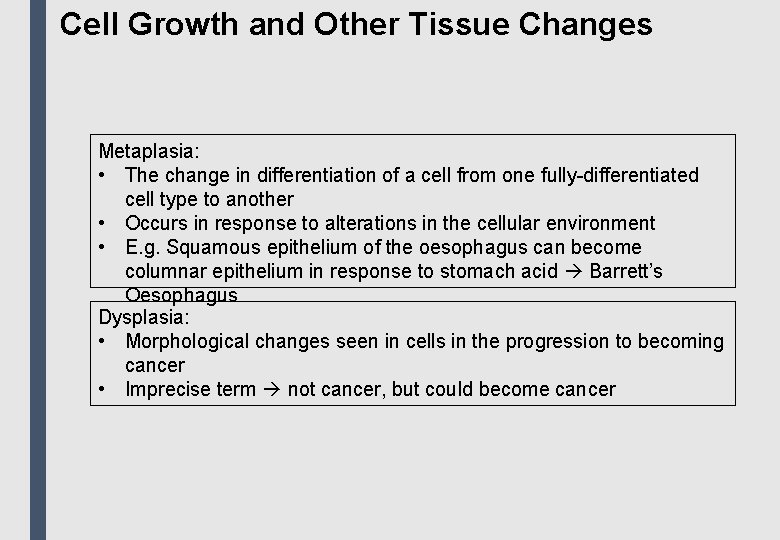
Cell Growth and Other Tissue Changes Metaplasia: • The change in differentiation of a cell from one fully-differentiated cell type to another • Occurs in response to alterations in the cellular environment • E. g. Squamous epithelium of the oesophagus can become columnar epithelium in response to stomach acid Barrett’s Oesophagus Dysplasia: • Morphological changes seen in cells in the progression to becoming cancer • Imprecise term not cancer, but could become cancer
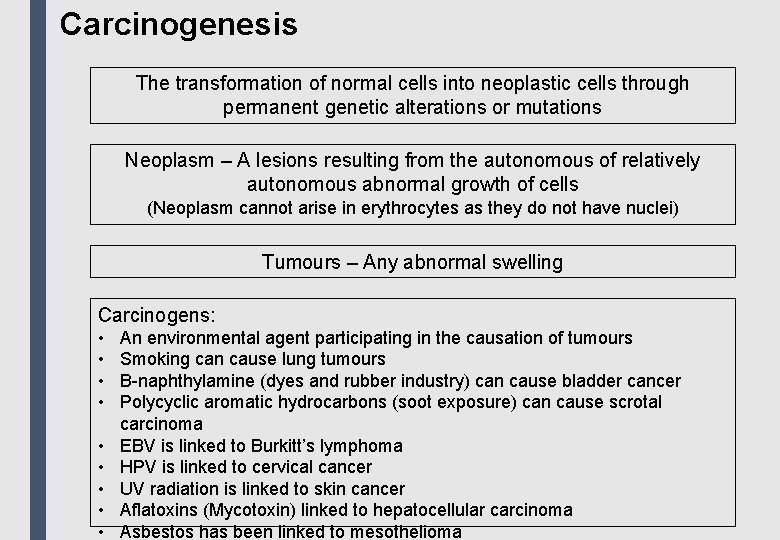
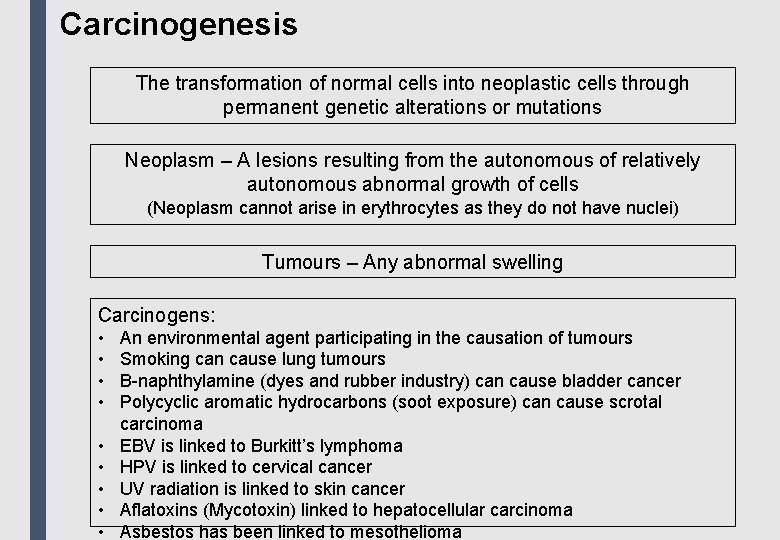
Carcinogenesis The transformation of normal cells into neoplastic cells through permanent genetic alterations or mutations Neoplasm – A lesions resulting from the autonomous of relatively autonomous abnormal growth of cells (Neoplasm cannot arise in erythrocytes as they do not have nuclei) Tumours – Any abnormal swelling Carcinogens: • • • An environmental agent participating in the causation of tumours Smoking can cause lung tumours B-naphthylamine (dyes and rubber industry) can cause bladder cancer Polycyclic aromatic hydrocarbons (soot exposure) can cause scrotal carcinoma EBV is linked to Burkitt’s lymphoma HPV is linked to cervical cancer UV radiation is linked to skin cancer Aflatoxins (Mycotoxin) linked to hepatocellular carcinoma Asbestos has been linked to mesothelioma
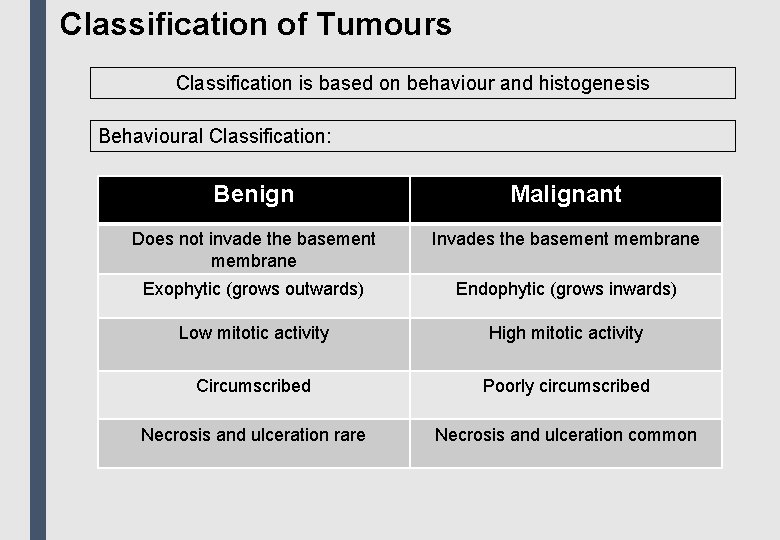
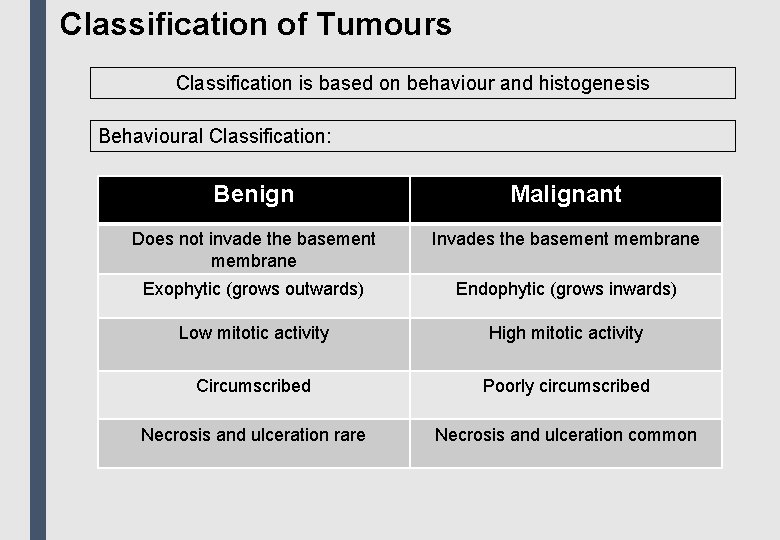
Classification of Tumours Classification is based on behaviour and histogenesis Behavioural Classification: Benign Malignant Does not invade the basement membrane Invades the basement membrane Exophytic (grows outwards) Endophytic (grows inwards) Low mitotic activity High mitotic activity Circumscribed Poorly circumscribed Necrosis and ulceration rare Necrosis and ulceration common
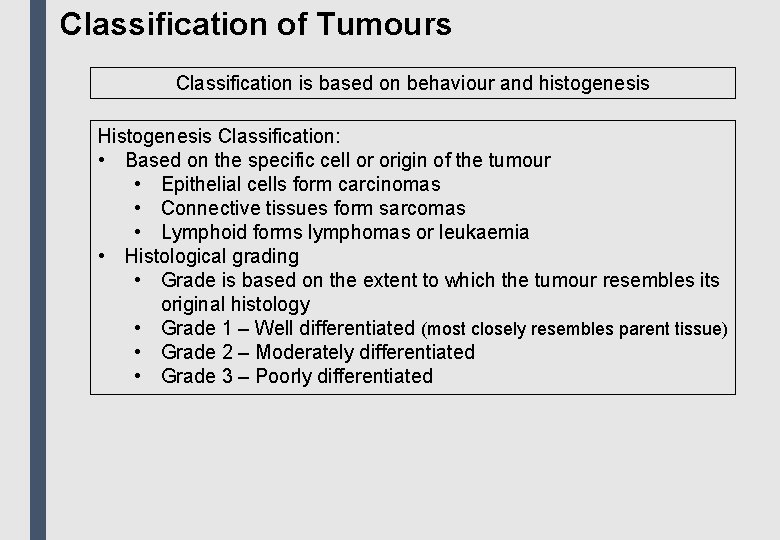
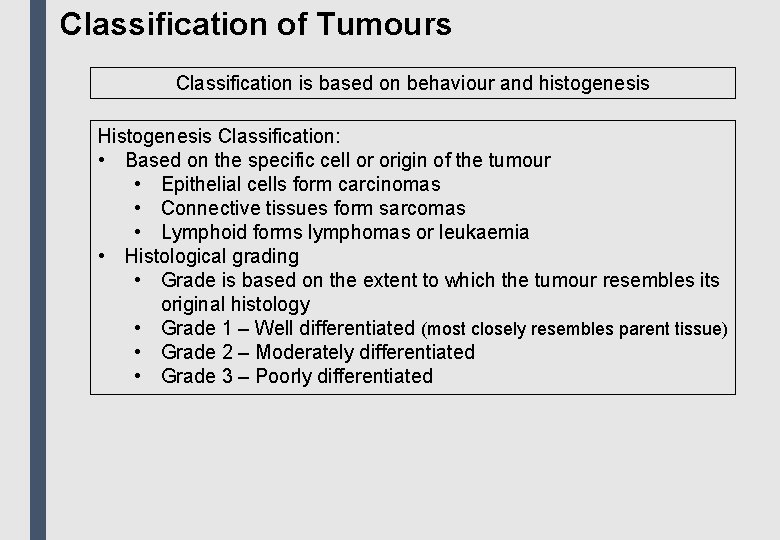
Classification of Tumours Classification is based on behaviour and histogenesis Histogenesis Classification: • Based on the specific cell or origin of the tumour • Epithelial cells form carcinomas • Connective tissues form sarcomas • Lymphoid forms lymphomas or leukaemia • Histological grading • Grade is based on the extent to which the tumour resembles its original histology • Grade 1 – Well differentiated (most closely resembles parent tissue) • Grade 2 – Moderately differentiated • Grade 3 – Poorly differentiated
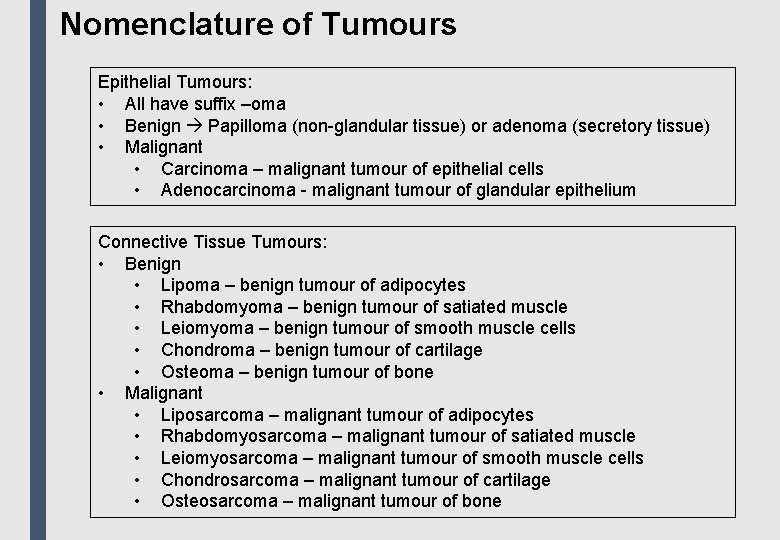
Nomenclature of Tumours Epithelial Tumours: • All have suffix –oma • Benign Papilloma (non-glandular tissue) or adenoma (secretory tissue) • Malignant • Carcinoma – malignant tumour of epithelial cells • Adenocarcinoma - malignant tumour of glandular epithelium Connective Tissue Tumours: • Benign • Lipoma – benign tumour of adipocytes • Rhabdomyoma – benign tumour of satiated muscle • Leiomyoma – benign tumour of smooth muscle cells • Chondroma – benign tumour of cartilage • Osteoma – benign tumour of bone • Malignant • Liposarcoma – malignant tumour of adipocytes • Rhabdomyosarcoma – malignant tumour of satiated muscle • Leiomyosarcoma – malignant tumour of smooth muscle cells • Chondrosarcoma – malignant tumour of cartilage • Osteosarcoma – malignant tumour of bone
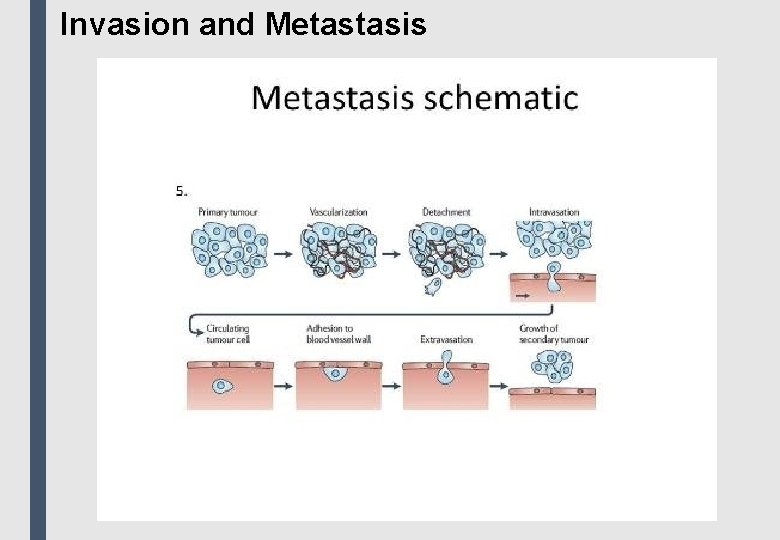
Invasion and Metastasis: • The process whereby malignant tumours spread from their site of origin to form other tumours at distant sites • Exception: Basal cell carcinoma never metastasises Process: 1. Detachment of tumour cells from their neighbours 2. Invasion of the surrounding connective tissue to reach conduits of metastasis 3. Intravasation into the lumen of vessels 4. Evasion of host defence mechanisms, such as NK cells 5. Adherence to endothelium at a remote location 6. Extravasation of the cells from the vessel lumen into the surrounding tissue 7. Tumour cells proliferate in the new environment Routes of Metastasis: • Bone metastasises from lung, breast, kidney, thyroid, prostate • Lymphatic metastasis is common (secondary tumours in lymph nodes) • Carcinomas prefer lymphatic spread • Sarcomas prefer haematogenous spread
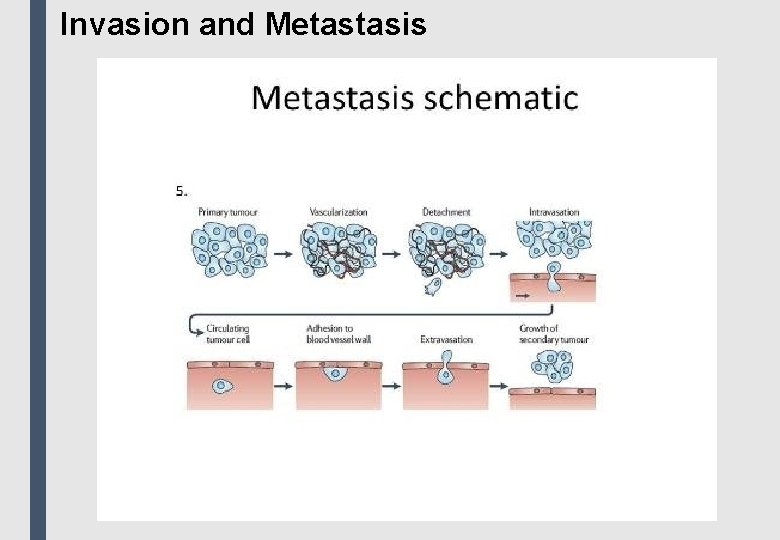
Invasion and Metastasis
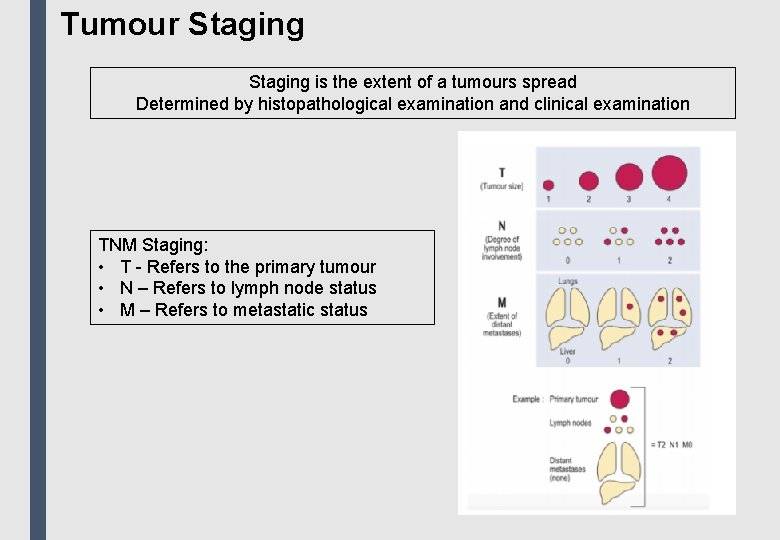
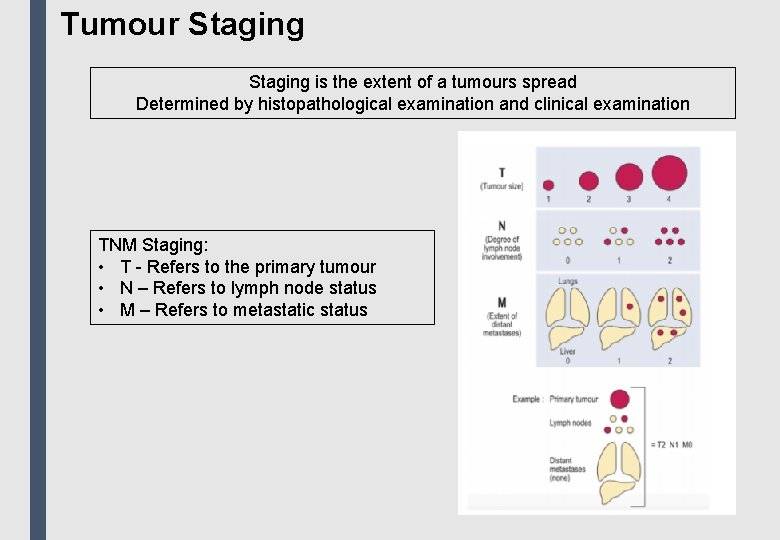
Tumour Staging is the extent of a tumours spread Determined by histopathological examination and clinical examination TNM Staging: • T - Refers to the primary tumour • N – Refers to lymph node status • M – Refers to metastatic status
Formative Questions
Question 1 Which 2 cell types are involved in the response to acute inflammation? a) Neutrophils and basophils b) Eosinophils and basophils c) Neutrophils and monocytes d) Neutrophils and lymphocytes e) Lymphocytes and monocytes
Question 1 Answer = C • Neutrophils (6 -24 hrs) and monocytes (24 -48 hrs) are the cells involved in acute inflammation • Neutrophils phagocytose pathogens while monocytes migrate to tissue and become macrophages which secrete chemical mediators for chemotaxis
Question 2 Which of these is NOT an outcome of acute inflammation? a) Pus formation b) Destruction c) Organisation d) Resolution e) Progression to chronic inflammation
Question 2 Answer = B Pus formation (also known as suppuration) occurs when there is excessive exudate production during acute inflammation, organisation occurs when a tissue is replaced with granulation tissue as part of the healing process, resolution is complete restoration of tissues to normal and progression to chronic inflammation.
Question 3 Hypertrophy is best described as: a) Increased size of organ/tissue due to increased number of cells b) Increased size of organ/tissue due to decreased number of cells c) Increased cell growth and decreased differentiation d) Increased size of organ/tissue due to increased size of cells e) Replacement of one differentiated tissue by another
Question 3 Answer = D Hypertrophy is an increase in size of organ/tissue due to an increase in the size of cells (this is due to an increase in protein synthesis and an increase in the size of intracellular organelles). Option a = hyperplasia e. g. uterine enlargement, option b = doesn’t make sense, option c = dysplasia e. g. pre-cancer state, option e = metaplasia e. g. Barrett’s oesophagus
Question 4 In which pathological process would you expect: - Organelles to be damaged - Cell lysis - Inflammation - Altered chromatin a) Metaplasia b) Apoptosis c) Dysplasia d) Hypertrophy e) Necrosis
Question 4 Answer = E This is a description of cell death therefore the only answers can be B or E – apoptosis, however, is programmed cell death
Question 5 What is a malignant neoplasm of smooth muscle called? a) Adenocarcinoma b) Leiomyoma c) Rhabdomyoma d) Leiomyosarcoma e) Adenoma
Question 5 Answer = D An adenocarcinoma is a malignant neoplasm of glandular origin, a leiomyoma is a benign neoplasm of smooth muscle, a rhabdomyoma is a benign neoplasm of striated muscle and an adenoma is a benign neoplasm of glandular origin.

Thank you for coming! ostevens 2@sheffield. ac. uk jlscott 2@sheffield. ac. uk