Pathology of the Respiratory System Dr Bushra AlTarawneh
Pathology of the Respiratory System Dr. Bushra Al-Tarawneh, MD Consultant Pathologist
Normal structure. There are multiple primary lung diseases that can broadly be divided into those primarily affecting: (1) the airways. 2) the interstitium. (3) the pulmonary vascular system.
ATELECTASIS
Atelectasis (collapse): is loss of lung volume caused by inadequate expansion of air spaces. May involve : 1 - Segment 2 - Lobe 3 - Lung Maybe reversible if cause is removed

Types of Atelectasis : 1 -Resorption atelectasis ( obstructive ) : - Foreign body - Mucus plug in asthma chronic bronchitis - Post surgery - Tumor. & Mediastinal Shift to Same Side

2 - Compression atelectasis causes include: -Air, fluid, tumor in pleural cavity. - Elevated diaphragm Mediastinal Shift to Opposite Side

3 - Contraction atelectasis : - Localized or generalized - Post inflammatory scarring - Fibrotic changes Note : No mediastinal shift
Morphology of Atelectasis : Gross : - Shrunken, purple & subcrepitant lung Microscopic : - Slit like alveoli, congested septae , fluid in spaces
Significant atelectasis reduces oxygenation and predisposes to infection. Because the collapsed lung parenchyma can be re-expanded, Atelectasis is a reversible disorder (except that caused by contraction). Outcome of atelectasis depends on the cause.
DISTURBANCES OF PULMONARY CIRCULATION
1 - Pulmonary edema :
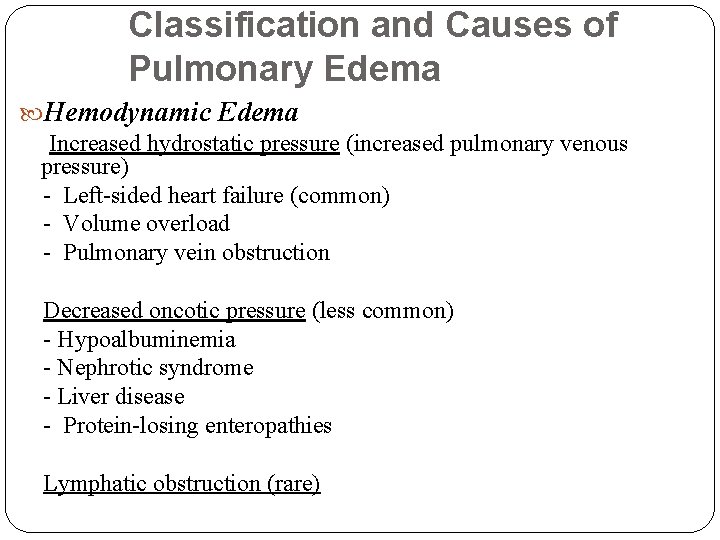
Classification and Causes of Pulmonary Edema Hemodynamic Edema Increased hydrostatic pressure (increased pulmonary venous pressure) - Left-sided heart failure (common) - Volume overload - Pulmonary vein obstruction Decreased oncotic pressure (less common) - Hypoalbuminemia - Nephrotic syndrome - Liver disease - Protein-losing enteropathies Lymphatic obstruction (rare)
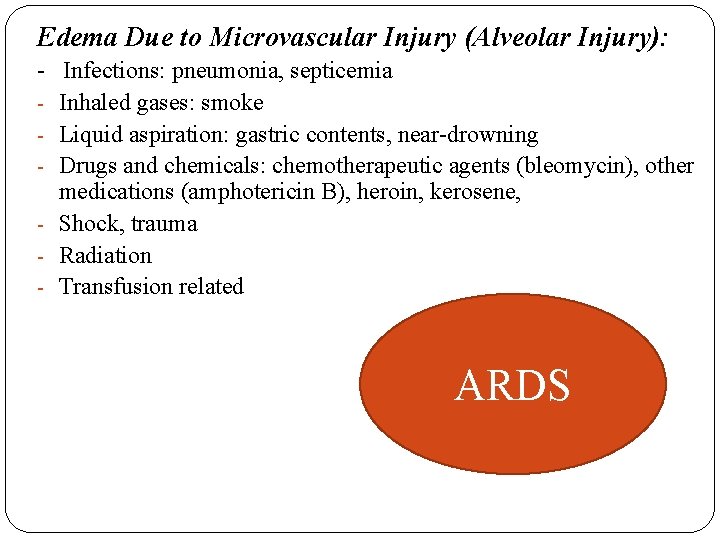
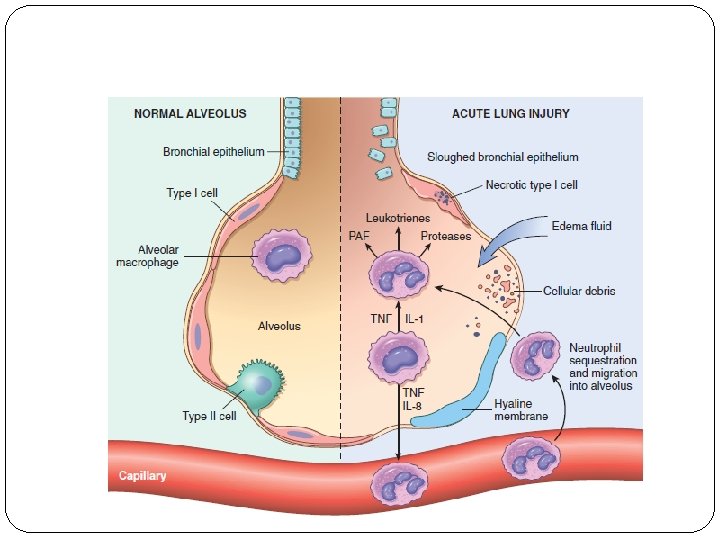
Edema Due to Microvascular Injury (Alveolar Injury): - Infections: pneumonia, septicemia - Inhaled gases: smoke - Liquid aspiration: gastric contents, near-drowning - Drugs and chemicals: chemotherapeutic agents (bleomycin), other medications (amphotericin B), heroin, kerosene, - Shock, trauma - Radiation - Transfusion related ARDS
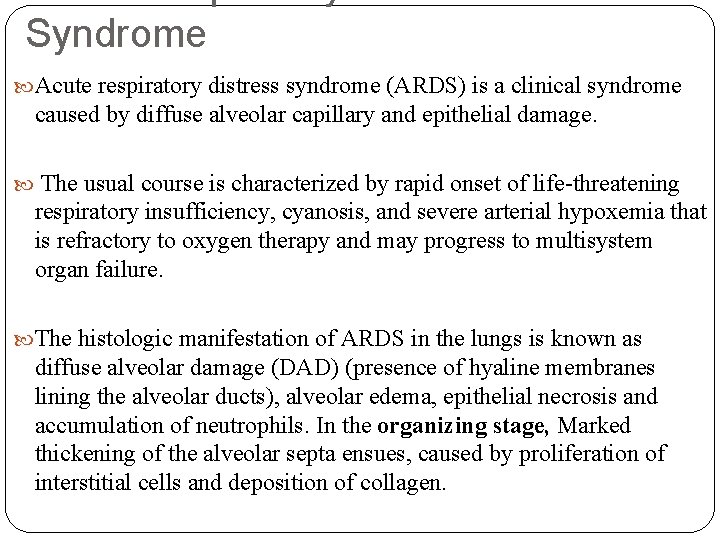
Syndrome Acute respiratory distress syndrome (ARDS) is a clinical syndrome caused by diffuse alveolar capillary and epithelial damage. The usual course is characterized by rapid onset of life-threatening respiratory insufficiency, cyanosis, and severe arterial hypoxemia that is refractory to oxygen therapy and may progress to multisystem organ failure. The histologic manifestation of ARDS in the lungs is known as diffuse alveolar damage (DAD) (presence of hyaline membranes lining the alveolar ducts), alveolar edema, epithelial necrosis and accumulation of neutrophils. In the organizing stage, Marked thickening of the alveolar septa ensues, caused by proliferation of interstitial cells and deposition of collagen.
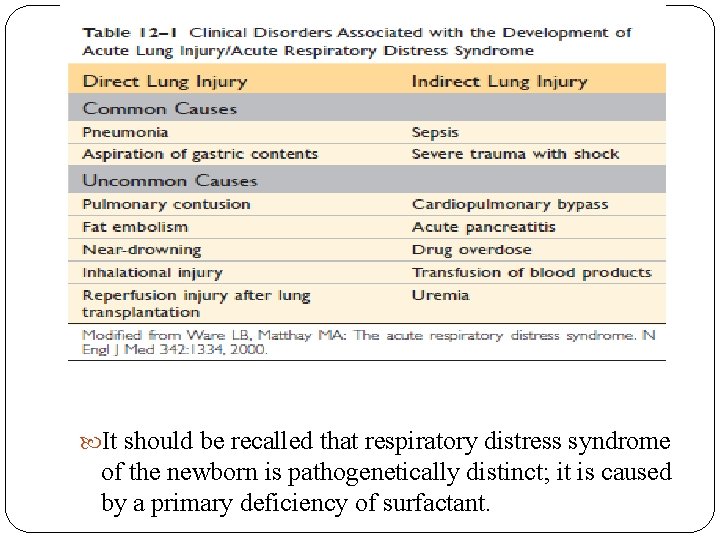
It should be recalled that respiratory distress syndrome of the newborn is pathogenetically distinct; it is caused by a primary deficiency of surfactant.
Edema of Undetermined Origin - High altitude - Neurogenic (central nervous system trauma)
Morphology : - Acute Wet lung due to frothy fluid in alveoli - Chronic Failure - Severe congestion in alveolar septae , microhemorrhages macrophages & fibrosis.
2 - Pulmonary thromboembolism - Commonest cause of preventable death in hospital - 95% originate from deep veins in legs - Predisposing causes : Surgery Pregnancy High estrogen pills Cancer
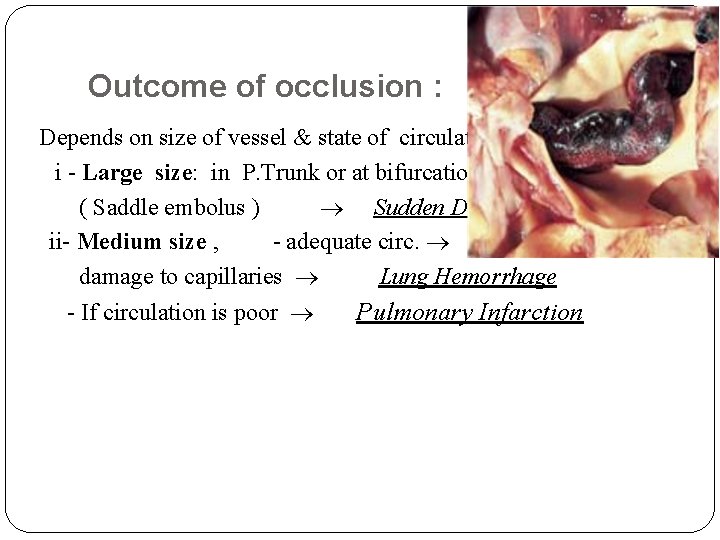
Outcome of occlusion : Depends on size of vessel & state of circulation i - Large size: in P. Trunk or at bifurcation ( Saddle embolus ) Sudden Death ii- Medium size , - adequate circ. damage to capillaries Lung Hemorrhage - If circulation is poor Pulmonary Infarction
Morphology : 1. Negative if sudden death. 2. Pulmonary infarct is classically hemorrhagic. - pleural surface is covered by a fibrinous exudate. - The red cells begin to lyse within 48 hours, and the infarct becomes paler and eventually red-brown as hemosiderin is produced. - With the passage of time, fibrous replacement begins at the margins and eventually converts the infarct into a contracted scar. 3 - Nonthrombotic forms of pulmonary embolism include several uncommon but potentially lethal forms, such as air, fat, and amniotic fluid embolism. Additionallly, Bone marrow embolism (presence of hematopoietic and fat elements within pulmonary circulation) can occur after massive trauma and in
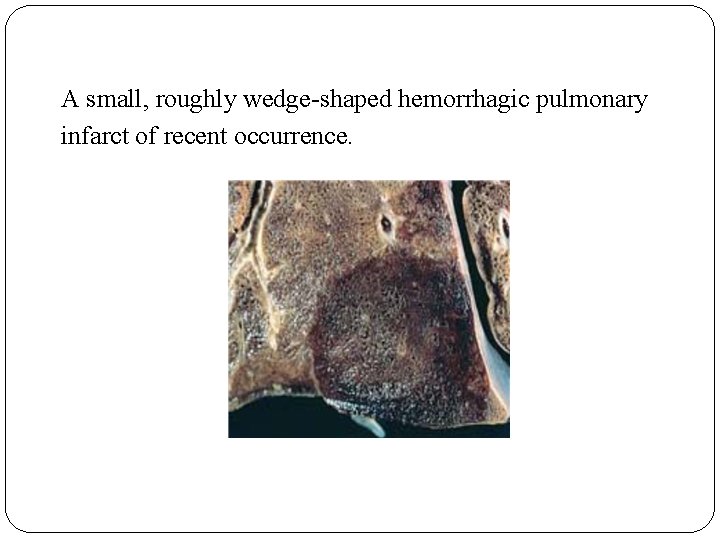
A small, roughly wedge-shaped hemorrhagic pulmonary infarct of recent occurrence.
Clinical Presentation : - Asymptomatic (60 -80%) - If more than 60% reduction in blood flow Acute cor pulmonale &sudden death (5%) - Sudden dyspnea, chest pain due to infarction - Recurrent multiple emboli & infarcts leading to chronic pulmonary hypertension (3%)
3 - Pulmonary Hypertension : The pulmonary circulation is normally one of low resistance, and pulmonary blood pressure is only about one eighth of systemic blood pressure. Pulmonary hypertension occurs when mean pulmonary pressure reaches one fourth of systemic levels.
- Arises in one of two ways : i- Decrease in the cross sectional area of pulmonary vascular bed ii-Increase in pulmonary vascular flow - Primary OR Secondary
Causes of secondary hypertension : i - Cardiac disease ii - Chronic lung disease iii- Inflammatory vascular disease iv- Recurrent thromboembolism v-Congenital left-to-right shunts
Primary Pulmonary Hypertension : Pulmonary hypertension is encountered in patients in whom all known causes of increased pulmonary pressure are excluded This is referred to as primary, or idiopathic, pulmonary hypertension. - most commonly sporadic; -only 6% of patients have the familial form with autosomaldominant mode of inheritance.
Primary Pulmonary Hypertension : - More common in young females , 10% Raynaud’s disease - Causes : ? Autoimmune disease ? Hypersensitivity of endothelium dysfunction, No relaxation Vasoconstriction - Poor prognosis - Treatment is lung transplant
Pathology of pulmonary hypertension : 1 - Main arteries Atheromatous plaques 2 - Medium sized muscular arteries myointimal & smooth muscle proliferation 3 - Small arteries & arterioles medial hypertrophy, duplication elastic lamina 4 - Persons with idiopathic pulmonary arterial hypertension or advanced pulmonary hypertension have characteristic plexiform lesions, in which endothelial proliferation forms multiple lumina within small arteries where they branch from a medium-sized artery. Complicated Plexiform Lesions ( plexogenic pulmonary arteriopathy)
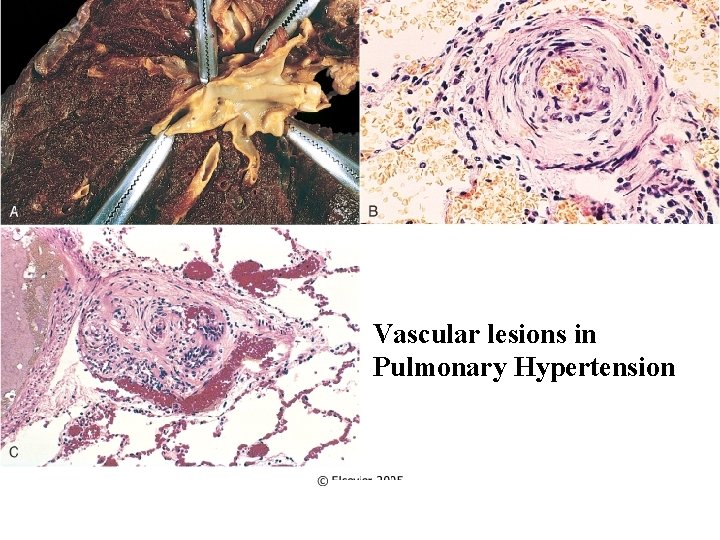
Vascular lesions in Pulmonary Hypertension
Diffuse Alveolar Hemorrhage Syndromes a group of “primary” immune-mediated diseases that manifest as the triad of hemoptysis, anemia, and diffuse pulmonary infiltrates. 1 - Goodpasture Syndrome: proliferative, usually rapidly progressive, glomerulonephritis and hemorrhagic interstitial pneumonitis. These antibodies (antibodies targeted against the noncollagenous domain of the α 3 chain of collagen IV) can be detected in the serum of more than 90% of persons with Goodpasture syndrome. Treatred by Plasmapheresis and immunosuppressive therapy.
2 - Idiopathic Pulmonary Hemosiderosis: a rare disease of uncertain etiology that has pulmonary manifestations and histologic features similar to those of Goodpasture syndrome, but there is no associated renal disease or circulating antibasement membrane antibody. Treated with steroid and immunosuppressive therapy. 3 - Pulmonary Angiitis and Granulomatosis (Wegener Granulomatosis): The lung lesions are characterized by a combination of necrotizing vasculitis (“angiitis”) and parenchymal necrotizing granulomatous inflammation. The manifestations of WG can include both upper respiratory symptoms (chronic sinusitis, epistaxis, nasal perforation) and pulmonary signs and symptoms
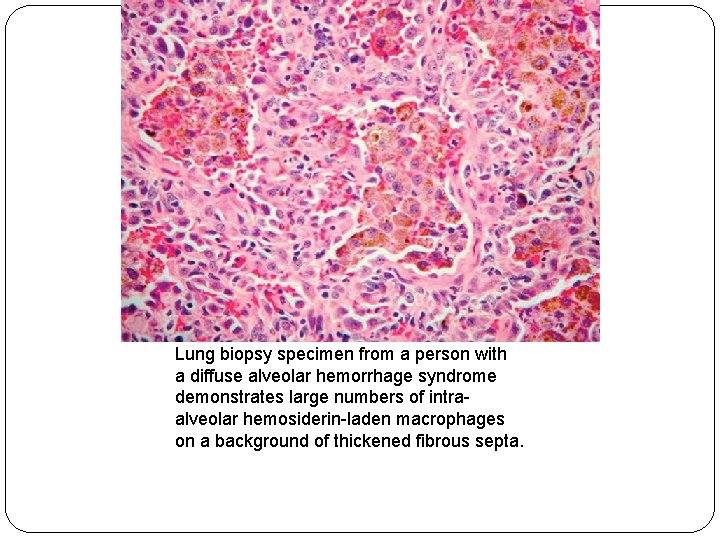
Lung biopsy specimen from a person with a diffuse alveolar hemorrhage syndrome demonstrates large numbers of intraalveolar hemosiderin-laden macrophages on a background of thickened fibrous septa.
THANK YOU
- Slides: 34