Pathology of the immune system Diseases of the


- Slides: 21
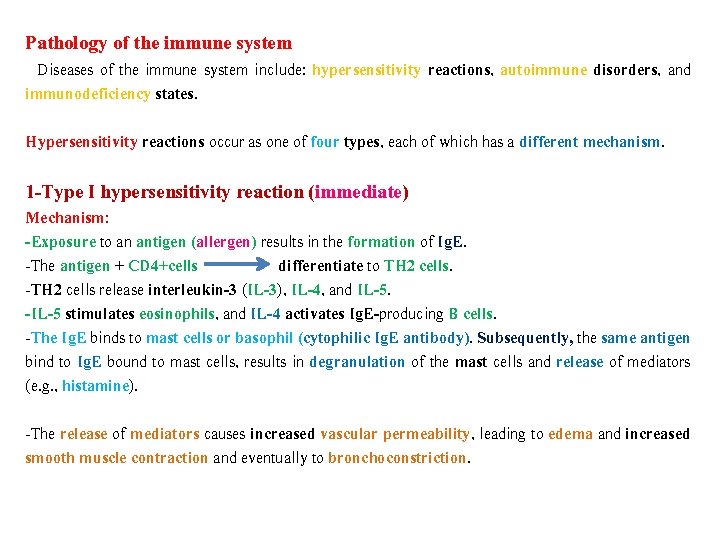
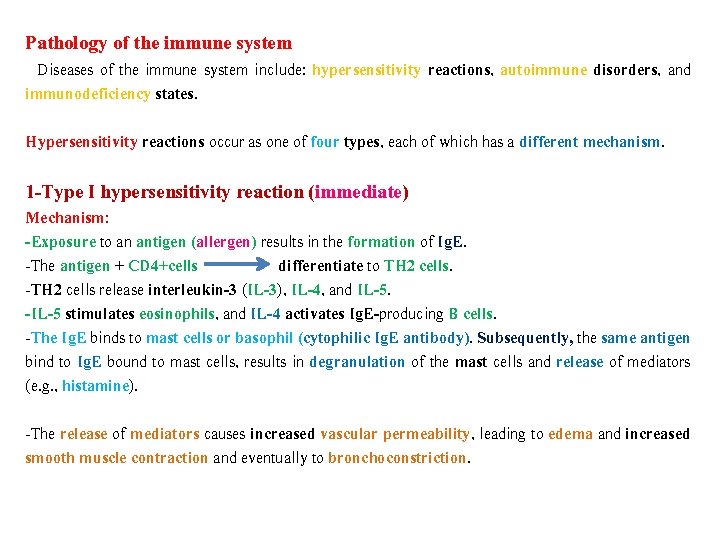
Pathology of the immune system Diseases of the immune system include: hypersensitivity reactions, autoimmune disorders, and immunodeficiency states. Hypersensitivity reactions occur as one of four types, each of which has a different mechanism. 1 -Type I hypersensitivity reaction (immediate) Mechanism: -Exposure to an antigen (allergen) results in the formation of Ig. E. -The antigen + CD 4+cells differentiate to TH 2 cells. -TH 2 cells release interleukin-3 (IL-3), IL-4, and IL-5. -IL-5 stimulates eosinophils, and IL-4 activates Ig. E-producing B cells. -The Ig. E binds to mast cells or basophil (cytophilic Ig. E antibody). Subsequently, the same antigen bind to Ig. E bound to mast cells, results in degranulation of the mast cells and release of mediators (e. g. , histamine). -The release of mediators causes increased vascular permeability, leading to edema and increased smooth muscle contraction and eventually to bronchoconstriction.
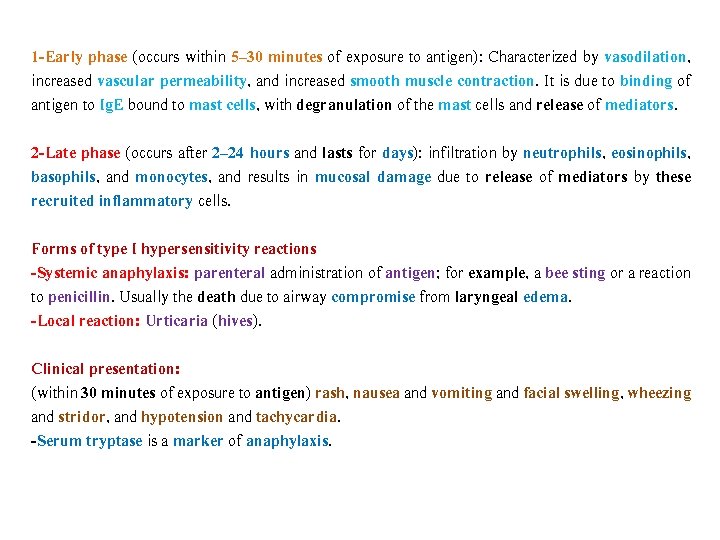
1 -Early phase (occurs within 5– 30 minutes of exposure to antigen): Characterized by vasodilation, increased vascular permeability, and increased smooth muscle contraction. It is due to binding of antigen to Ig. E bound to mast cells, with degranulation of the mast cells and release of mediators. 2 -Late phase (occurs after 2– 24 hours and lasts for days): infiltration by neutrophils, eosinophils, basophils, and monocytes, and results in mucosal damage due to release of mediators by these recruited inflammatory cells. Forms of type I hypersensitivity reactions -Systemic anaphylaxis: parenteral administration of antigen; for example, a bee sting or a reaction to penicillin. Usually the death due to airway compromise from laryngeal edema. -Local reaction: Urticaria (hives). Clinical presentation: (within 30 minutes of exposure to antigen) rash, nausea and vomiting and facial swelling, wheezing and stridor, and hypotension and tachycardia. -Serum tryptase is a marker of anaphylaxis.
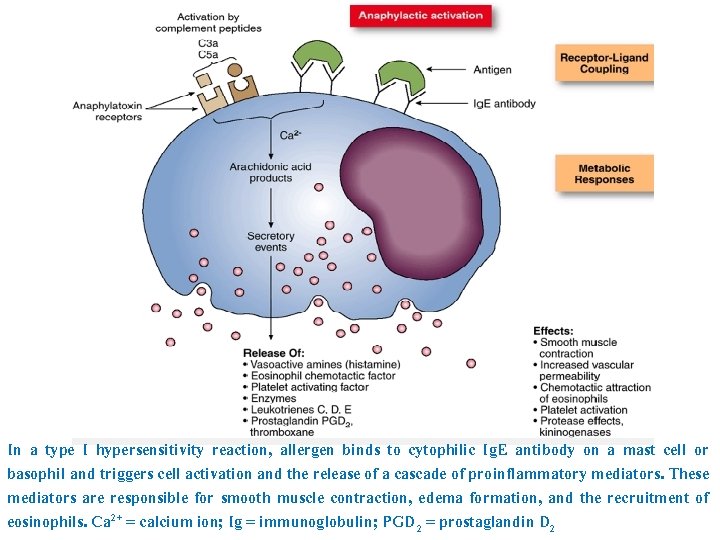
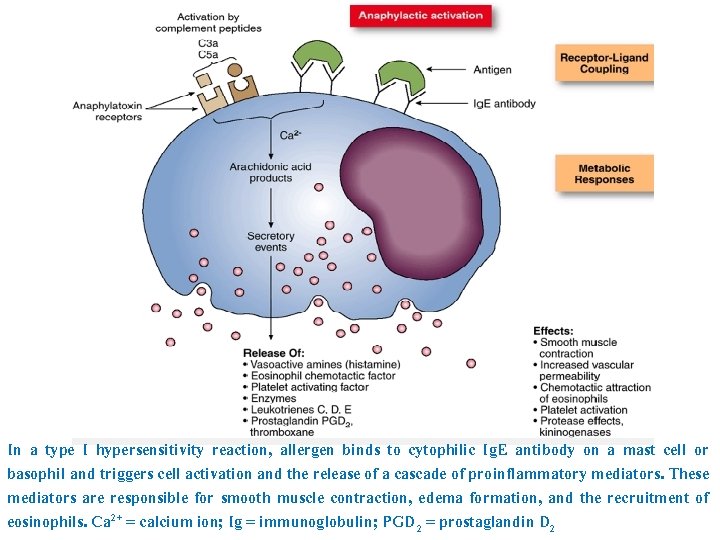
In a type I hypersensitivity reaction, allergen binds to cytophilic Ig. E antibody on a mast cell or basophil and triggers cell activation and the release of a cascade of proinflammatory mediators. These mediators are responsible for smooth muscle contraction, edema formation, and the recruitment of eosinophils. Ca 2+ = calcium ion; Ig = immunoglobulin; PGD 2 = prostaglandin D 2

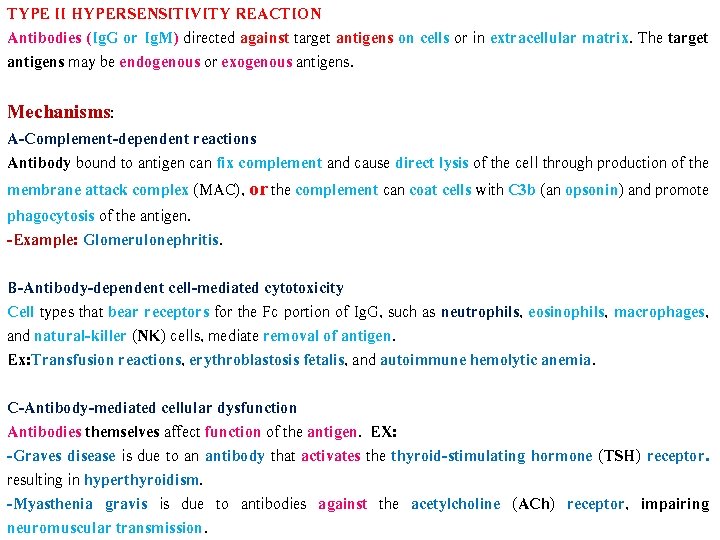
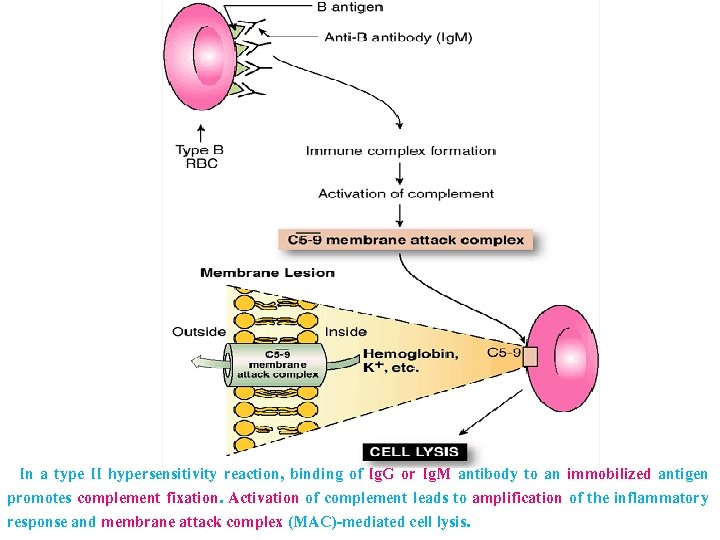
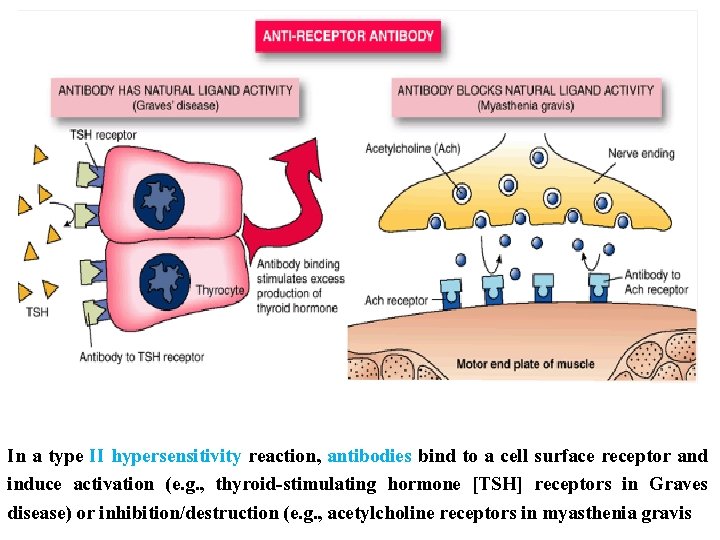
TYPE II HYPERSENSITIVITY REACTION Antibodies (Ig. G or Ig. M) directed against target antigens on cells or in extracellular matrix. The target antigens may be endogenous or exogenous antigens. Mechanisms: A-Complement-dependent reactions Antibody bound to antigen can fix complement and cause direct lysis of the cell through production of the membrane attack complex (MAC), or the complement can coat cells with C 3 b (an opsonin) and promote phagocytosis of the antigen. -Example: Glomerulonephritis. B-Antibody-dependent cell-mediated cytotoxicity Cell types that bear receptors for the Fc portion of Ig. G, such as neutrophils, eosinophils, macrophages, and natural-killer (NK) cells, mediate removal of antigen. Ex: Transfusion reactions, erythroblastosis fetalis, and autoimmune hemolytic anemia. C-Antibody-mediated cellular dysfunction Antibodies themselves affect function of the antigen. EX: -Graves disease is due to an antibody that activates the thyroid-stimulating hormone (TSH) receptor. resulting in hyperthyroidism. -Myasthenia gravis is due to antibodies against the acetylcholine (ACh) receptor, impairing neuromuscular transmission.
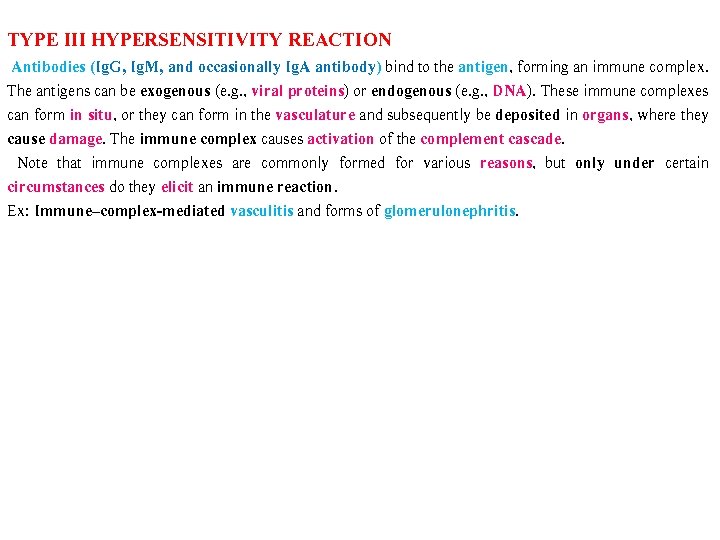
TYPE III HYPERSENSITIVITY REACTION Antibodies (Ig. G, Ig. M, and occasionally Ig. A antibody) bind to the antigen, forming an immune complex. The antigens can be exogenous (e. g. , viral proteins) or endogenous (e. g. , DNA). These immune complexes can form in situ, or they can form in the vasculature and subsequently be deposited in organs, where they cause damage. The immune complex causes activation of the complement cascade. Note that immune complexes are commonly formed for various reasons, but only under certain circumstances do they elicit an immune reaction. Ex: Immune–complex-mediated vasculitis and forms of glomerulonephritis.
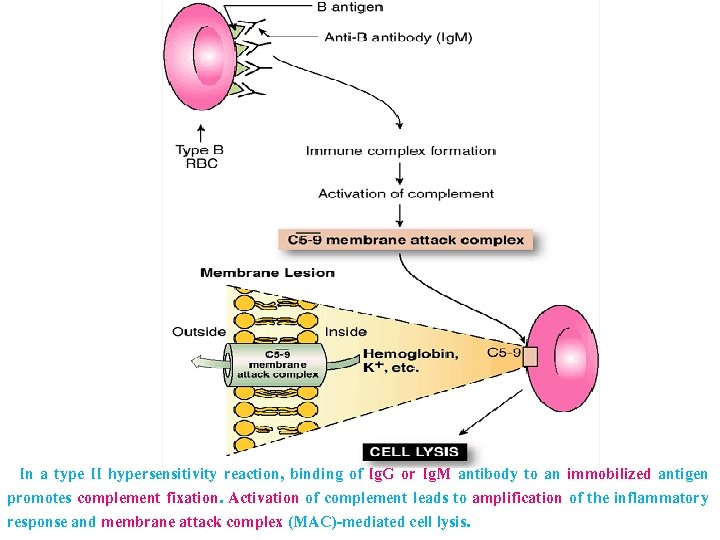
In a type II hypersensitivity reaction, binding of Ig. G or Ig. M antibody to an immobilized antigen promotes complement fixation. Activation of complement leads to amplification of the inflammatory response and membrane attack complex (MAC)-mediated cell lysis.
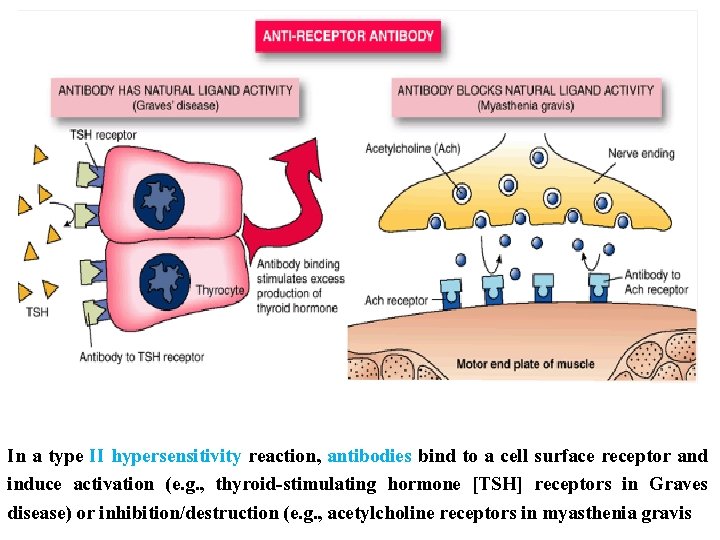
In a type II hypersensitivity reaction, antibodies bind to a cell surface receptor and induce activation (e. g. , thyroid-stimulating hormone [TSH] receptors in Graves disease) or inhibition/destruction (e. g. , acetylcholine receptors in myasthenia gravis

Systemic lupus erthematosus (Malar rash): This is a "butterfly-shaped" red rash over the mala eminence and cheeks below the eyes and across the bridge of the nose.
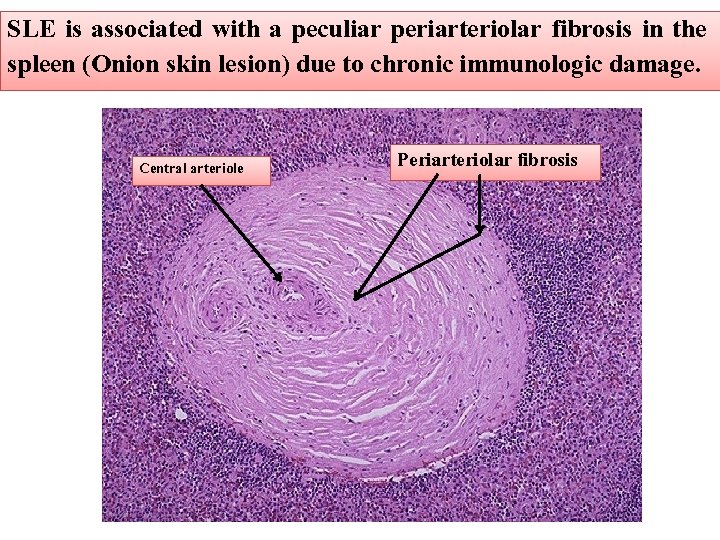
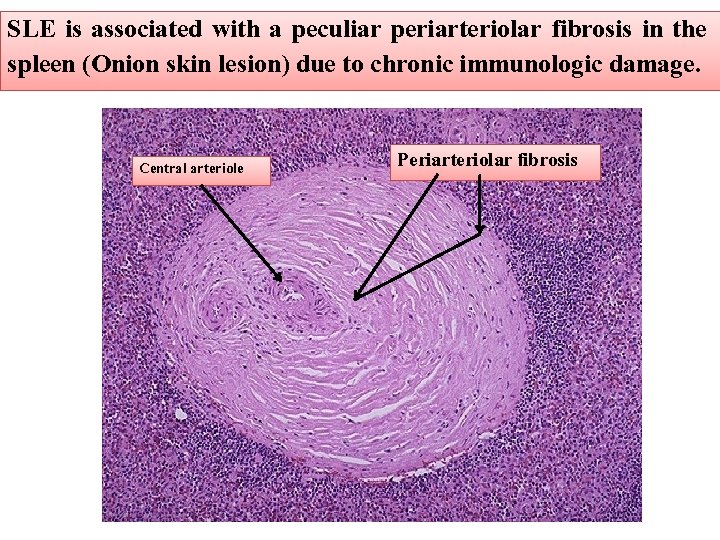
SLE is associated with a peculiar periarteriolar fibrosis in the spleen (Onion skin lesion) due to chronic immunologic damage. Central arteriole Periarteriolar fibrosis
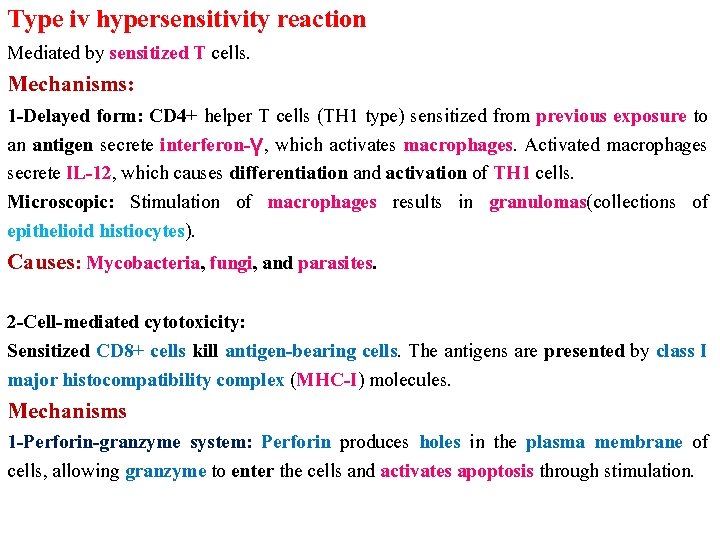
Type iv hypersensitivity reaction Mediated by sensitized T cells. Mechanisms: 1 -Delayed form: CD 4+ helper T cells (TH 1 type) sensitized from previous exposure to an antigen secrete interferon-γ, which activates macrophages. Activated macrophages secrete IL-12, which causes differentiation and activation of TH 1 cells. Microscopic: Stimulation of macrophages results in granulomas(collections of epithelioid histiocytes). Causes: Mycobacteria, fungi, and parasites. 2 -Cell-mediated cytotoxicity: Sensitized CD 8+ cells kill antigen-bearing cells. The antigens are presented by class I major histocompatibility complex (MHC-I) molecules. Mechanisms 1 -Perforin-granzyme system: Perforin produces holes in the plasma membrane of cells, allowing granzyme to enter the cells and activates apoptosis through stimulation.
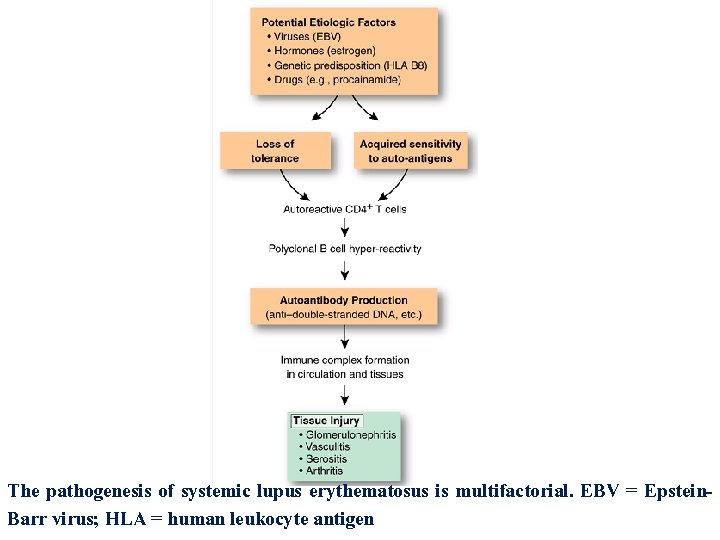
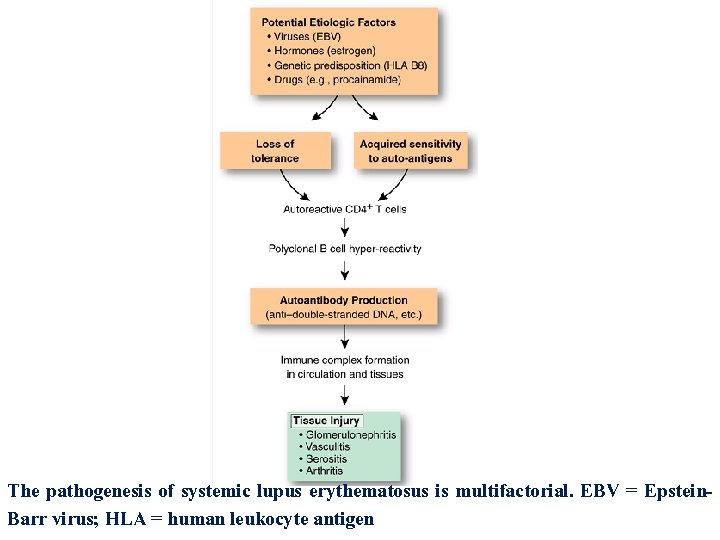
The pathogenesis of systemic lupus erythematosus is multifactorial. EBV = Epstein. Barr virus; HLA = human leukocyte antigen
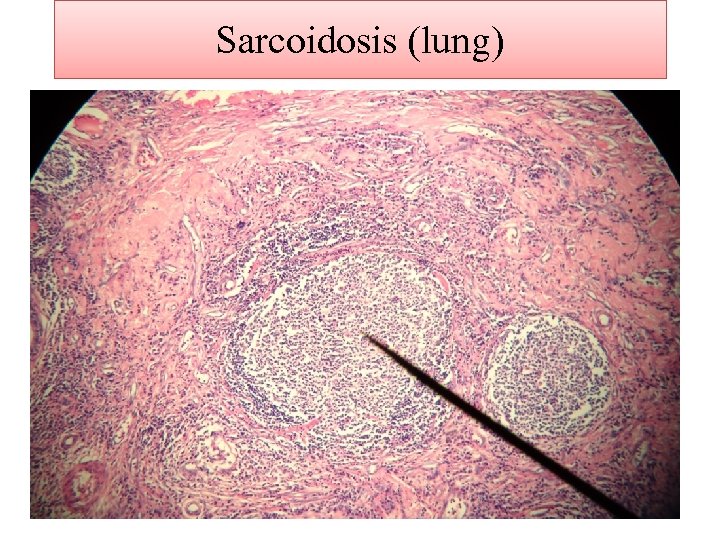
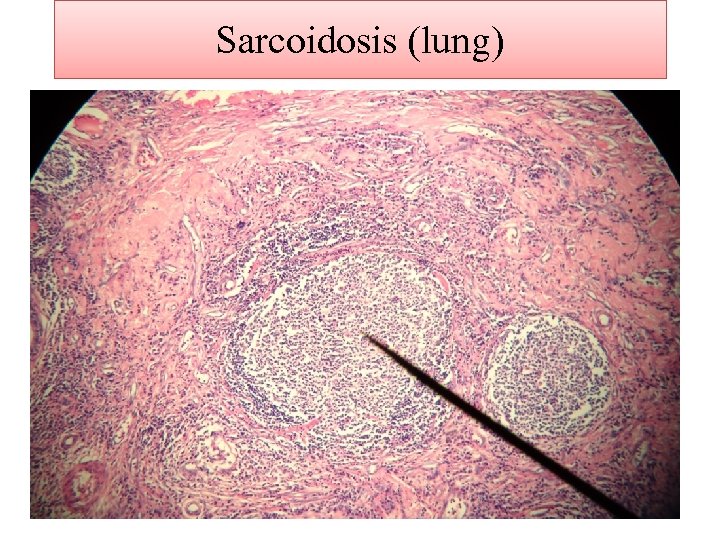
Sarcoidosis (lung)
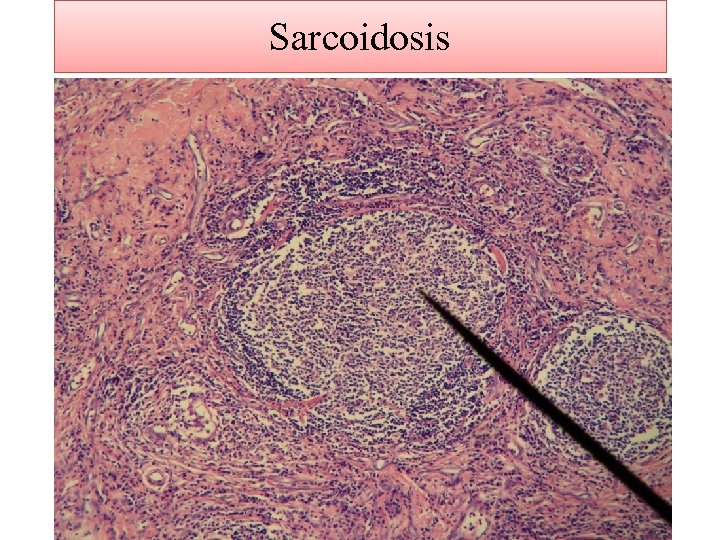
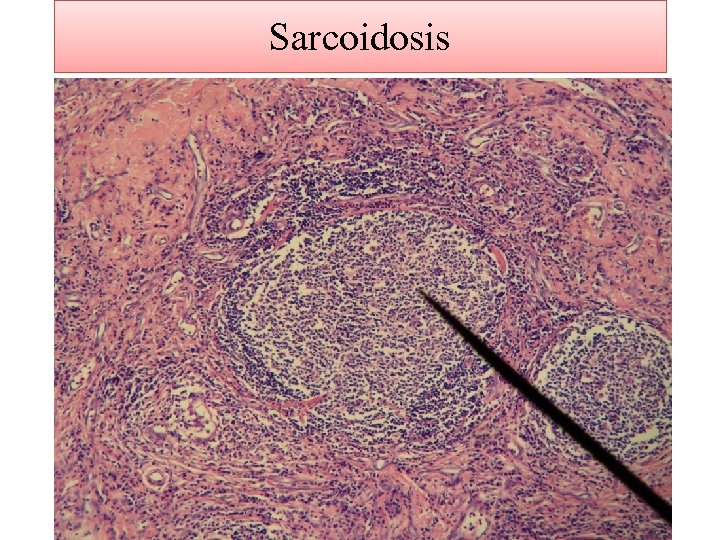
Sarcoidosis
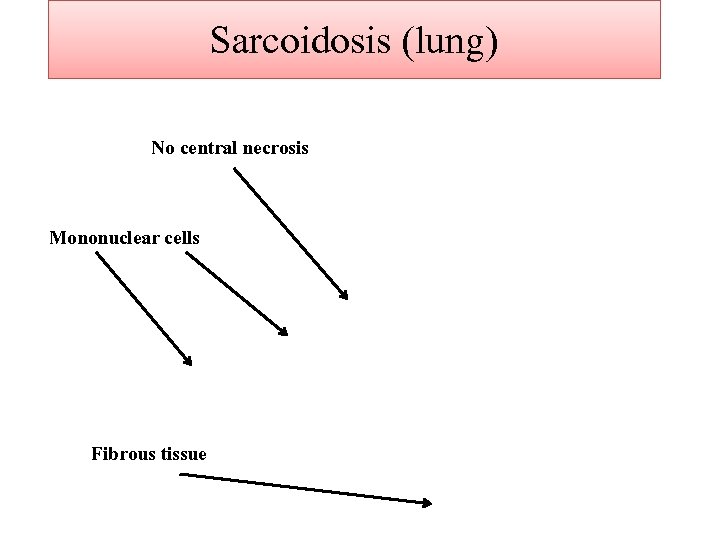
Sarcoidosis (lung) No central necrosis Mononuclear cells Fibrous tissue
Sarcoidosis (lung)
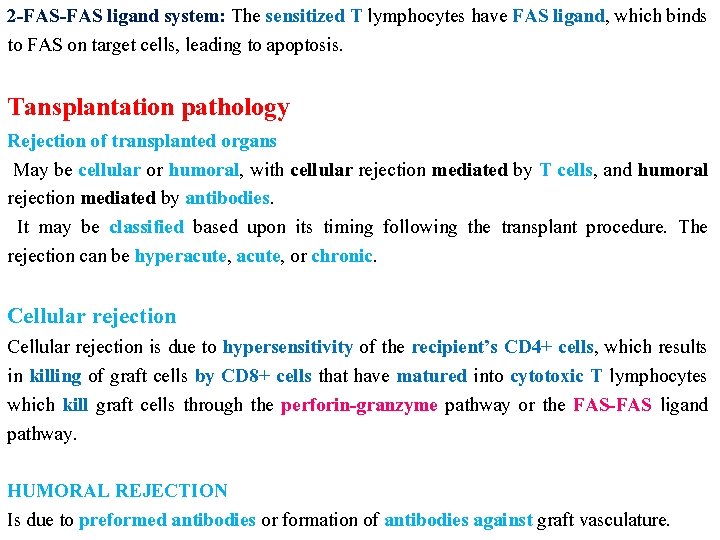
2 -FAS ligand system: The sensitized T lymphocytes have FAS ligand, which binds to FAS on target cells, leading to apoptosis. Tansplantation pathology Rejection of transplanted organs May be cellular or humoral, with cellular rejection mediated by T cells, and humoral rejection mediated by antibodies. It may be classified based upon its timing following the transplant procedure. The rejection can be hyperacute, or chronic. Cellular rejection is due to hypersensitivity of the recipient’s CD 4+ cells, which results in killing of graft cells by CD 8+ cells that have matured into cytotoxic T lymphocytes which kill graft cells through the perforin-granzyme pathway or the FAS-FAS ligand pathway. HUMORAL REJECTION Is due to preformed antibodies or formation of antibodies against graft vasculature.
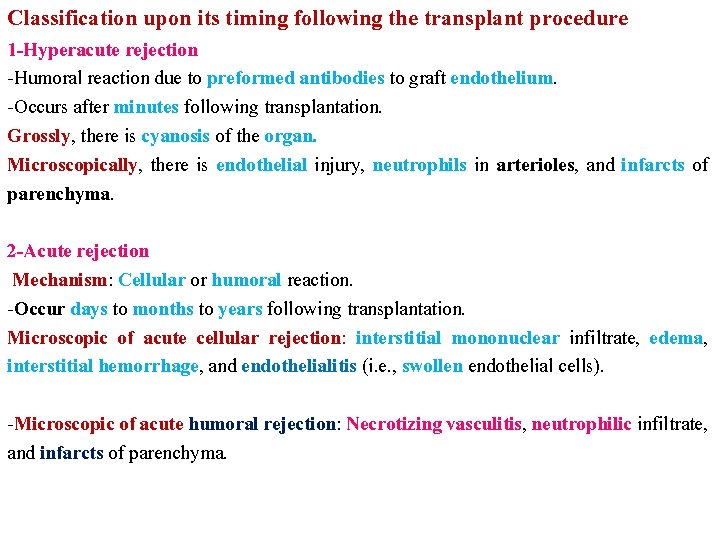
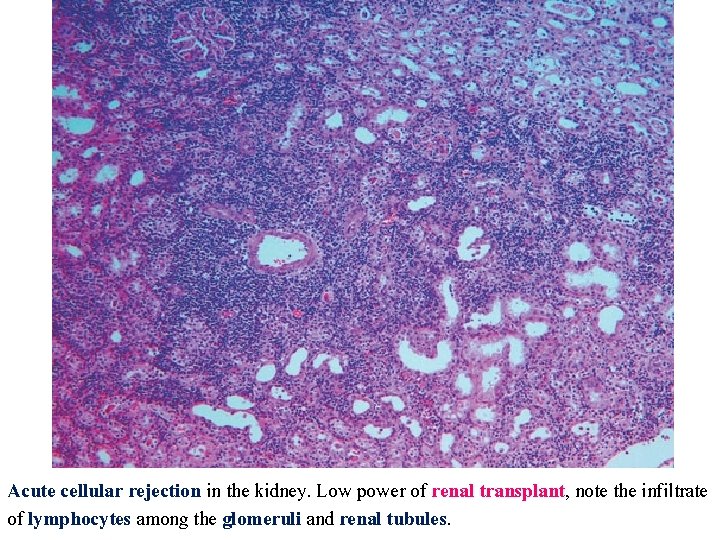
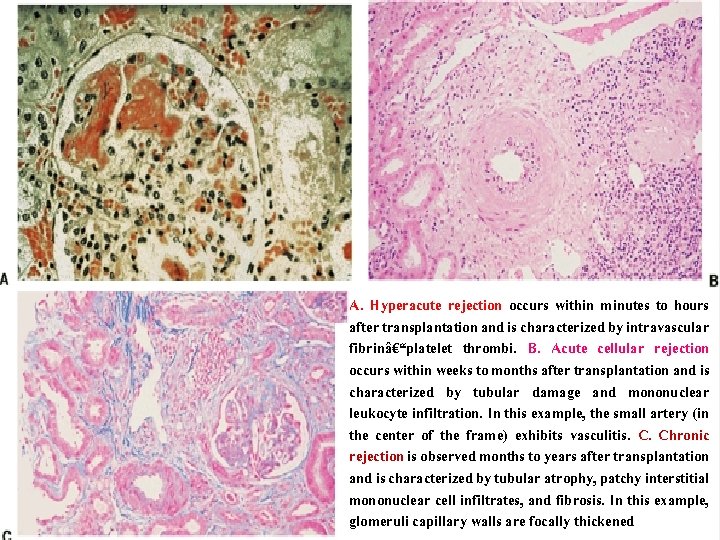
Classification upon its timing following the transplant procedure 1 -Hyperacute rejection -Humoral reaction due to preformed antibodies to graft endothelium. -Occurs after minutes following transplantation. Grossly, there is cyanosis of the organ. Microscopically, there is endothelial injury, neutrophils in arterioles, and infarcts of parenchyma. 2 -Acute rejection Mechanism: Cellular or humoral reaction. -Occur days to months to years following transplantation. Microscopic of acute cellular rejection: interstitial mononuclear infiltrate, edema, interstitial hemorrhage, and endothelialitis (i. e. , swollen endothelial cells). -Microscopic of acute humoral rejection: Necrotizing vasculitis, neutrophilic infiltrate, and infarcts of parenchyma.
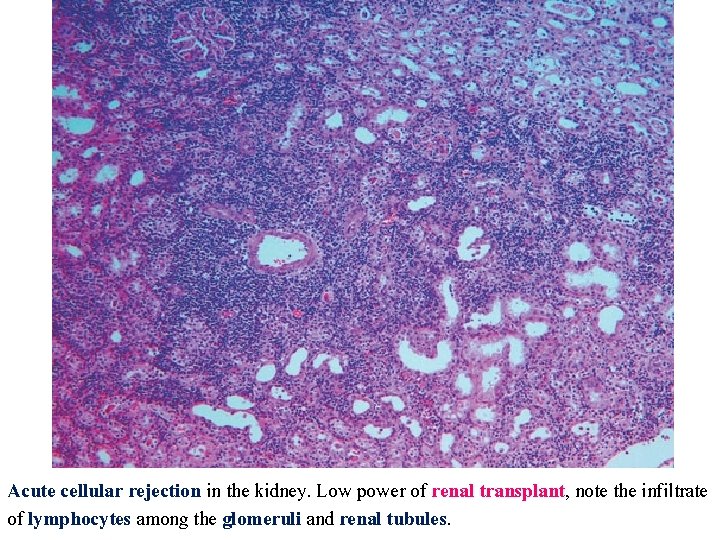
Acute cellular rejection in the kidney. Low power of renal transplant, note the infiltrate of lymphocytes among the glomeruli and renal tubules.
Chronic rejection -Mechanism: Cellular rejection plays an important role. -(4– 6 )months to years following the graft. -Microscopic: Vascular changes, interstitial fibrosis, interstitial mononuclear infiltrate, and ischemia with subsequent tissue loss.
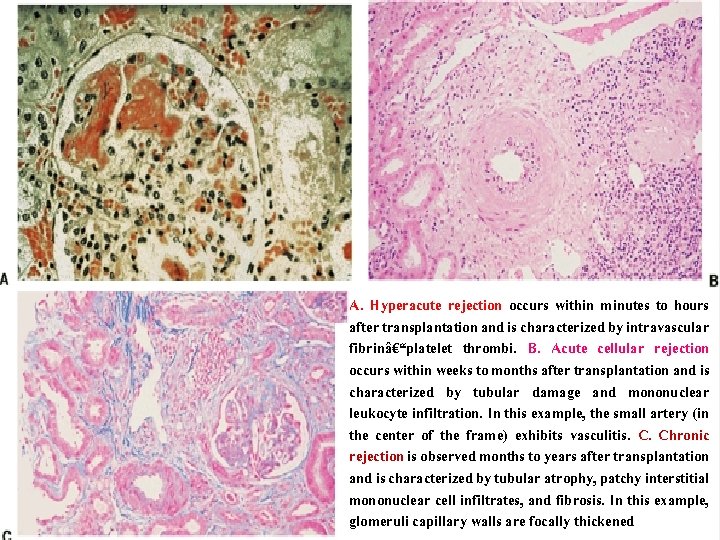
A. Hyperacute rejection occurs within minutes to hours after transplantation and is characterized by intravascular fibrin–platelet thrombi. B. Acute cellular rejection occurs within weeks to months after transplantation and is characterized by tubular damage and mononuclear leukocyte infiltration. In this example, the small artery (in the center of the frame) exhibits vasculitis. C. Chronic rejection is observed months to years after transplantation and is characterized by tubular atrophy, patchy interstitial mononuclear cell infiltrates, and fibrosis. In this example, glomeruli capillary walls are focally thickened