Pathology of lung pleura and upper airways Assoc


- Slides: 59
Pathology of lung, pleura and upper airways Assoc. Professor Jan Laco, MD, Ph. D
Summary l l l l 1. Atelectasis 2. Obstructive lung diseases 3. Restrictive lung diseases 4. Vascular lung diseases 5. Pulmonary infections 6. Lung tumors 7. Pleural lesions 8. Lesions of upper RT
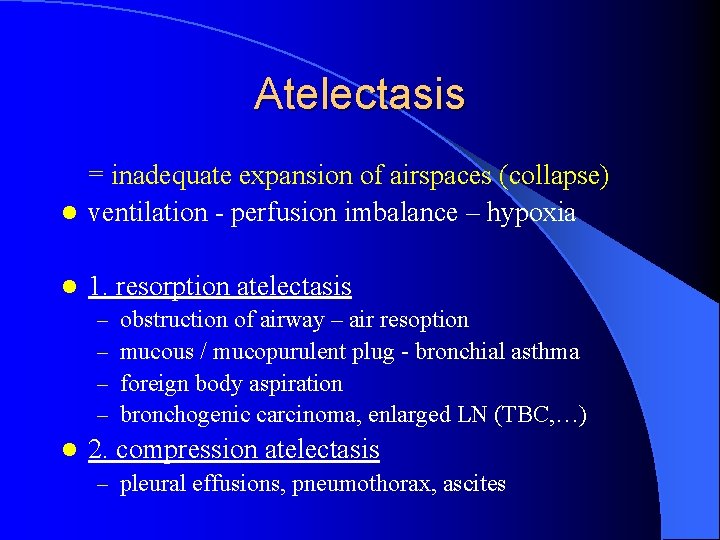
Atelectasis = inadequate expansion of airspaces (collapse) l ventilation - perfusion imbalance – hypoxia l 1. resorption atelectasis – – l obstruction of airway – air resoption mucous / mucopurulent plug - bronchial asthma foreign body aspiration bronchogenic carcinoma, enlarged LN (TBC, …) 2. compression atelectasis – pleural effusions, pneumothorax, ascites
Summary l l l l 1. Atelectasis 2. Obstructive lung diseases 3. Restrictive lung diseases 4. Vascular lung diseases 5. Pulmonary infections 6. Lung tumors 7. Pleural lesions 8. Lesions of upper RT
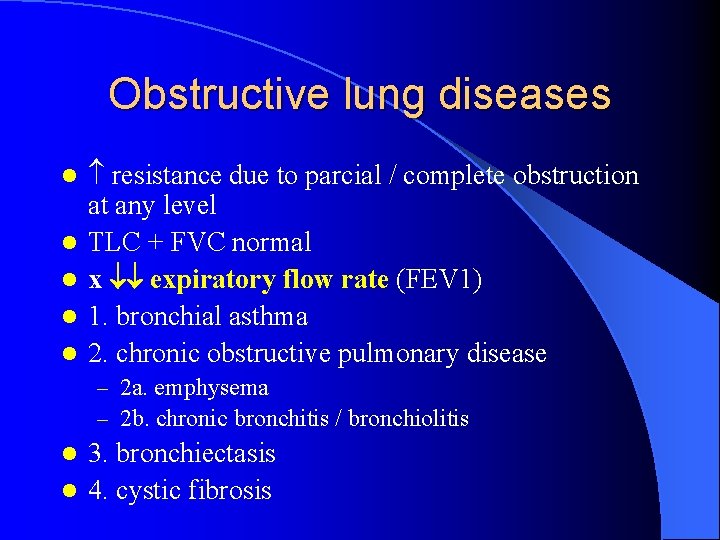
Obstructive lung diseases l l l resistance due to parcial / complete obstruction at any level TLC + FVC normal x expiratory flow rate (FEV 1) 1. bronchial asthma 2. chronic obstructive pulmonary disease – 2 a. emphysema – 2 b. chronic bronchitis / bronchiolitis 3. bronchiectasis l 4. cystic fibrosis l
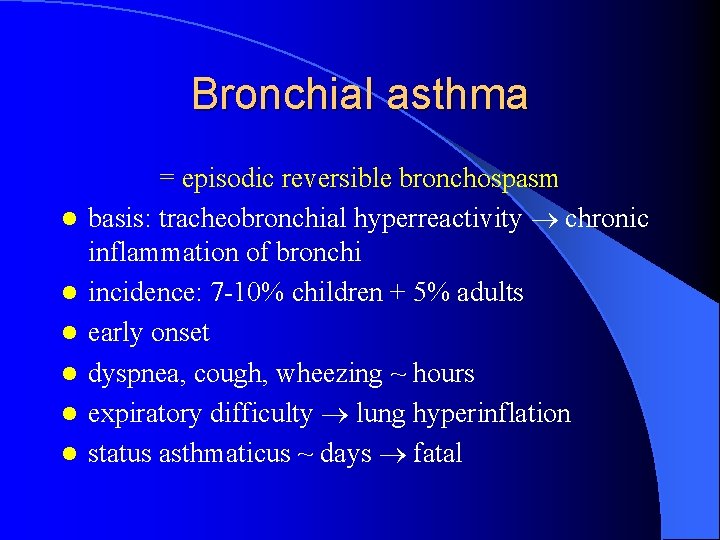
Bronchial asthma l l l = episodic reversible bronchospasm basis: tracheobronchial hyperreactivity chronic inflammation of bronchi incidence: 7 -10% children + 5% adults early onset dyspnea, cough, wheezing ~ hours expiratory difficulty lung hyperinflation status asthmaticus ~ days fatal
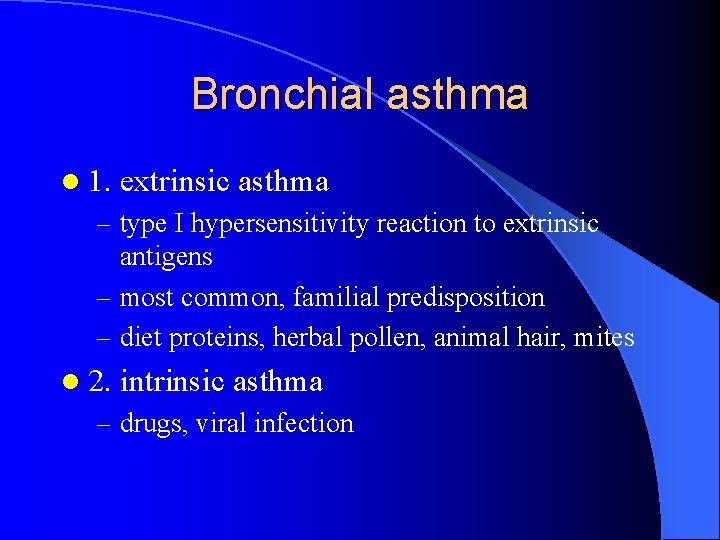
Bronchial asthma l 1. extrinsic asthma – type I hypersensitivity reaction to extrinsic antigens – most common, familial predisposition – diet proteins, herbal pollen, animal hair, mites l 2. intrinsic asthma – drugs, viral infection
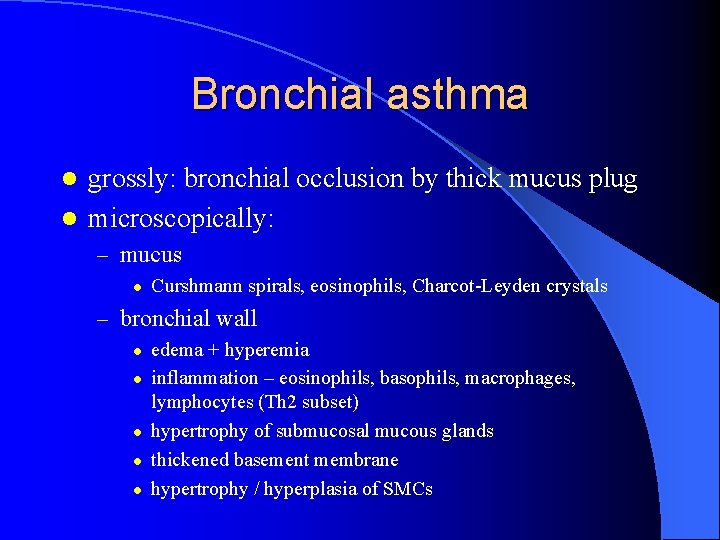
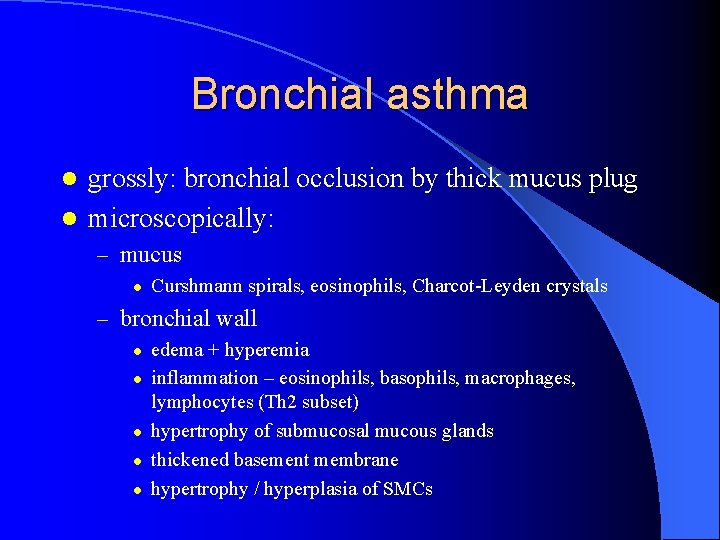
Bronchial asthma grossly: bronchial occlusion by thick mucus plug l microscopically: l – mucus l Curshmann spirals, eosinophils, Charcot-Leyden crystals – bronchial wall l l edema + hyperemia inflammation – eosinophils, basophils, macrophages, lymphocytes (Th 2 subset) hypertrophy of submucosal mucous glands thickened basement membrane hypertrophy / hyperplasia of SMCs
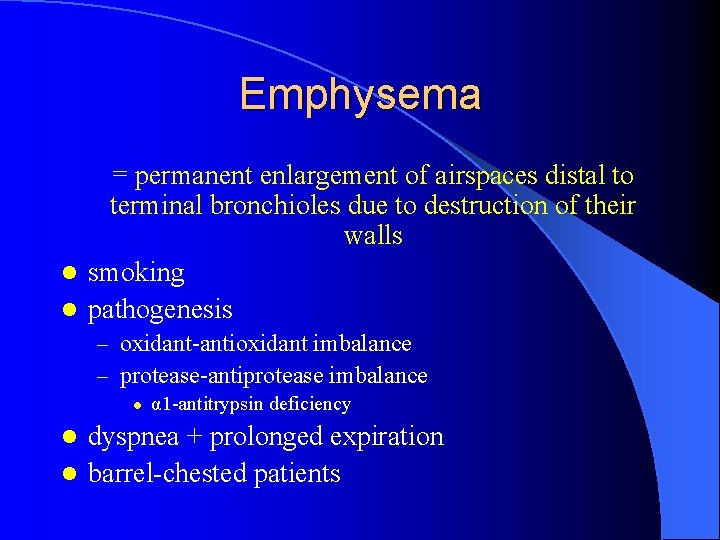
Emphysema = permanent enlargement of airspaces distal to terminal bronchioles due to destruction of their walls l smoking l pathogenesis – oxidant-antioxidant imbalance – protease-antiprotease imbalance l α 1 -antitrypsin deficiency dyspnea + prolonged expiration l barrel-chested patients l
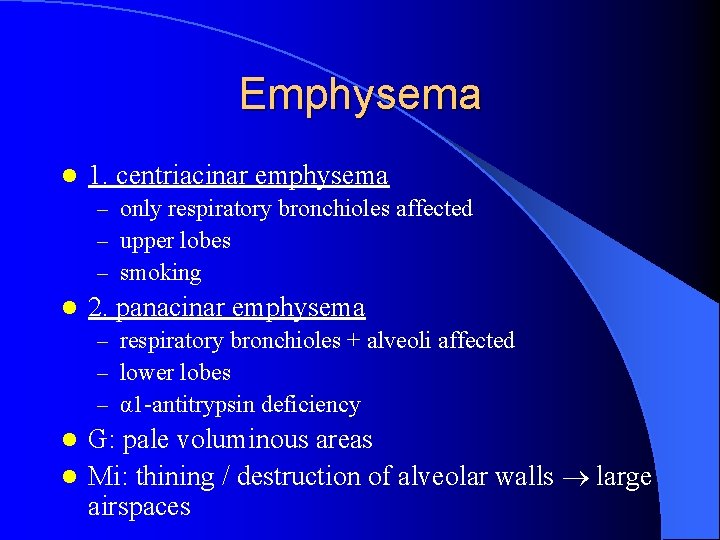
Emphysema l 1. centriacinar emphysema – only respiratory bronchioles affected – upper lobes – smoking l 2. panacinar emphysema – respiratory bronchioles + alveoli affected – lower lobes – α 1 -antitrypsin deficiency G: pale voluminous areas l Mi: thining / destruction of alveolar walls large airspaces l
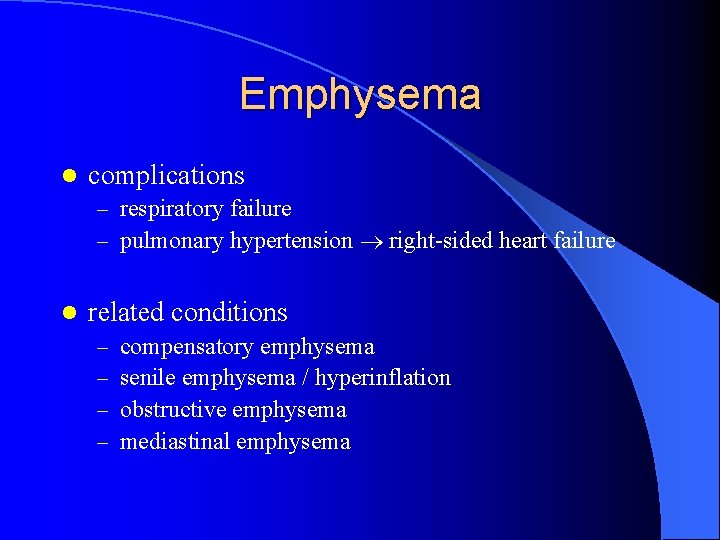
Emphysema l complications – respiratory failure – pulmonary hypertension right-sided heart failure l related conditions – – compensatory emphysema senile emphysema / hyperinflation obstructive emphysema mediastinal emphysema
Chronic bronchitis = persistent productive cough for 3 consecutive months in 2 consecutive years l smoking, air pollutants l several forms: – – simple CB mucopurulent CB asthmatic CB obstructive CB
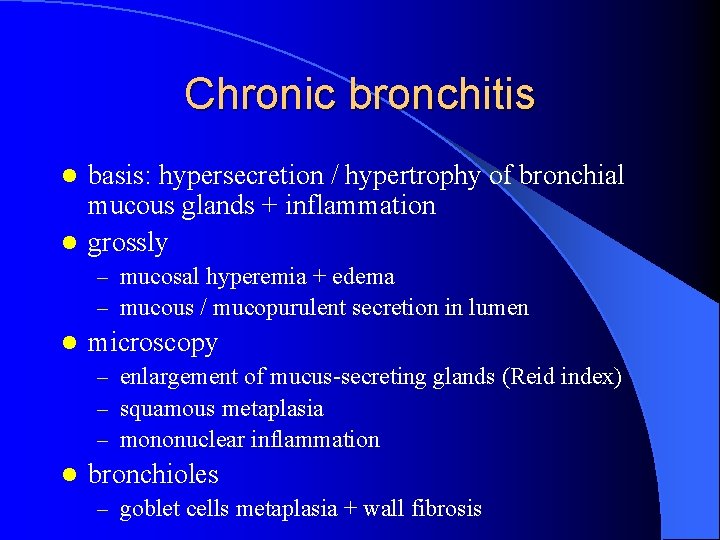
Chronic bronchitis basis: hypersecretion / hypertrophy of bronchial mucous glands + inflammation l grossly l – mucosal hyperemia + edema – mucous / mucopurulent secretion in lumen l microscopy – enlargement of mucus-secreting glands (Reid index) – squamous metaplasia – mononuclear inflammation l bronchioles – goblet cells metaplasia + wall fibrosis
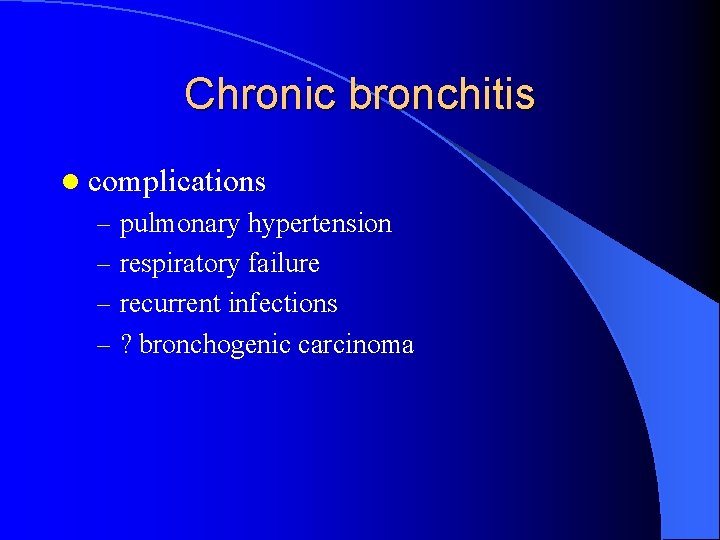
Chronic bronchitis l complications – pulmonary hypertension – respiratory failure – recurrent infections – ? bronchogenic carcinoma
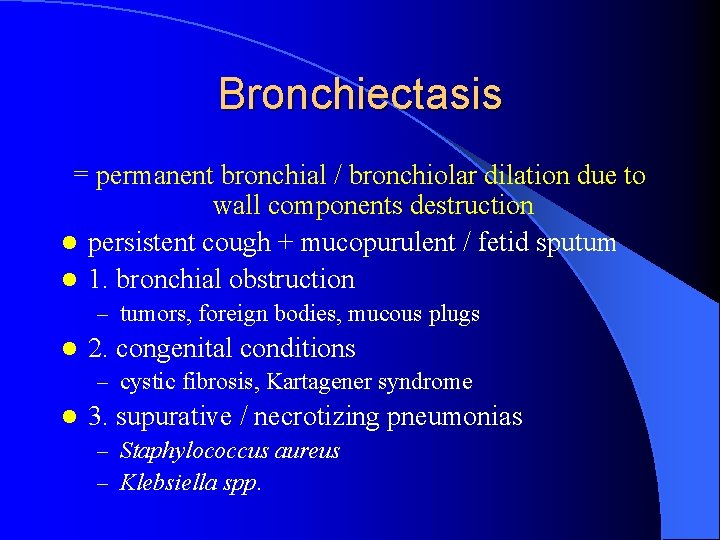
Bronchiectasis = permanent bronchial / bronchiolar dilation due to wall components destruction l persistent cough + mucopurulent / fetid sputum l 1. bronchial obstruction – tumors, foreign bodies, mucous plugs l 2. congenital conditions – cystic fibrosis, Kartagener syndrome l 3. supurative / necrotizing pneumonias – Staphylococcus aureus – Klebsiella spp.
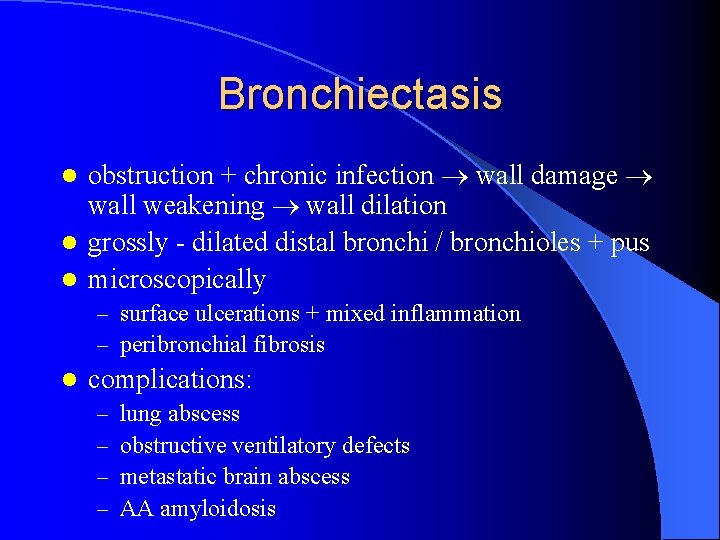
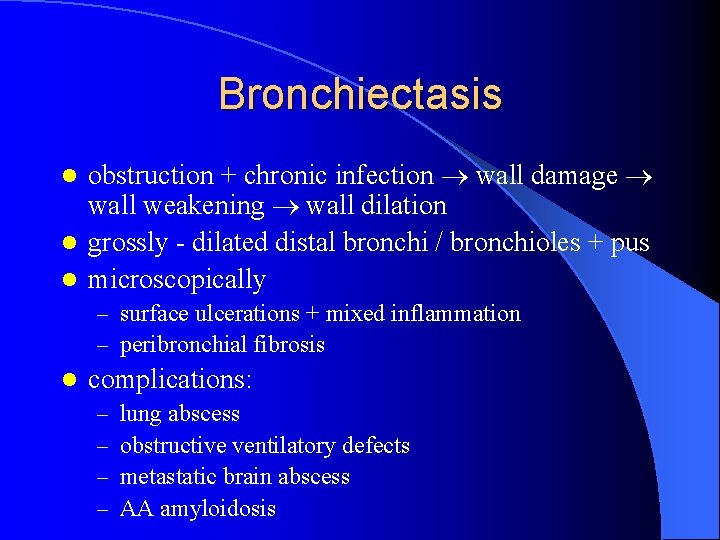
Bronchiectasis obstruction + chronic infection wall damage wall weakening wall dilation l grossly - dilated distal bronchi / bronchioles + pus l microscopically l – surface ulcerations + mixed inflammation – peribronchial fibrosis l complications: – – lung abscess obstructive ventilatory defects metastatic brain abscess AA amyloidosis
Summary l l l l 1. Atelectasis 2. Obstructive lung diseases 3. Restrictive lung diseases 4. Vascular lung diseases 5. Pulmonary infections 6. Lung tumors 7. Pleural lesions 8. Lesions of upper RT
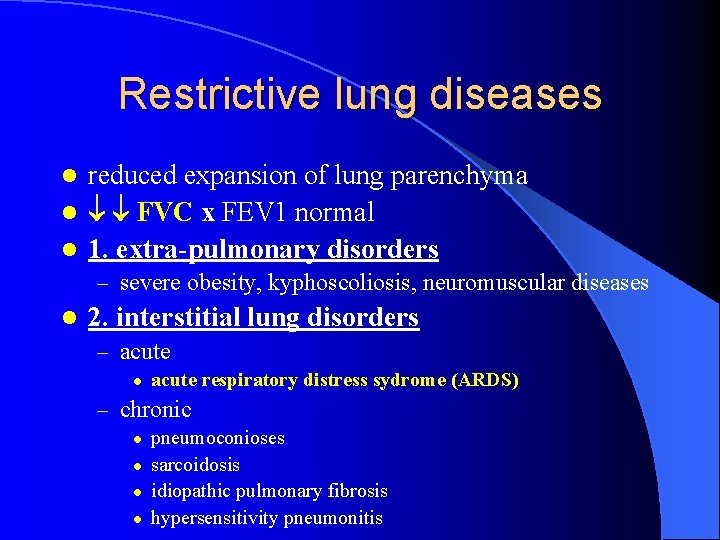
Restrictive lung diseases reduced expansion of lung parenchyma l FVC x FEV 1 normal l 1. extra-pulmonary disorders l – severe obesity, kyphoscoliosis, neuromuscular diseases l 2. interstitial lung disorders – acute l acute respiratory distress sydrome (ARDS) – chronic l l pneumoconioses sarcoidosis idiopathic pulmonary fibrosis hypersensitivity pneumonitis
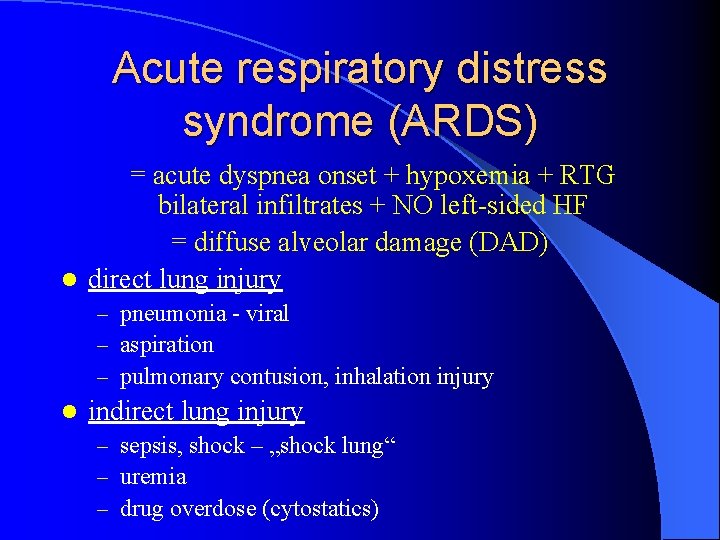
Acute respiratory distress syndrome (ARDS) = acute dyspnea onset + hypoxemia + RTG bilateral infiltrates + NO left-sided HF = diffuse alveolar damage (DAD) l direct lung injury – pneumonia - viral – aspiration – pulmonary contusion, inhalation injury l indirect lung injury – sepsis, shock – „shock lung“ – uremia – drug overdose (cytostatics)
Acute respiratory distress syndrome (ARDS) epithelium + endothelium injury alveolar capillary membrane damage vascular permeability alveolar flooding + surfactant abnormalities l grossly l – dark red + firm + airless + heavy lung ~ liver l microscopically - acute phase – capillary congestion + alveolar cells necrosis – interstitial + alveolar edema + hemorrhage – hyaline membranes (edema fluid + cell debries)
Acute respiratory distress syndrome (ARDS) l microscopically - proliferative phase – pneumocytes II proliferation + hyaline membranes phagocytosis (macrophages) – P II differentiate into pneumocytes I – interstitial fibroblasts proliferation interstitial fibrosis = honeycomb lung
Acute respiratory distress syndrome (ARDS) l clinical course – !!! mortality 30 -40% !!! – normal respiratory function within 6 -12 months – diffuse interstitial fibrosis
Sudden Infant Death Syndrome l l l „sudden death of infant < 1 year + complete autopsy does not reveal other cause of death“ 1 to 700 -1, 000 liveborn age: 2 - 4 months, boys (2 : 1) crib death x night ~ day winter (infection – trigger ? ? ? ) mother´s smoking autopsy: big thymus + serosal petechiae ? ? ? brain stem ganglia abnomalities ? ? ? heart conductive system abnormalities
Sarcoidosis l l l = multisystemic disease with noncaseating granulomas in many tissues and organs etiology – unknown (? ? ? Th lymphocytes) younger adults, non-smokers familial clustering, Scandinavia hypercalcemia + hypercalciuria microscopy (dg. of exclusion) – noncaseating granulomas + specific granulation tissue – epithelioid + multinucleated cells – Schaumann bodies + asteroid bodies
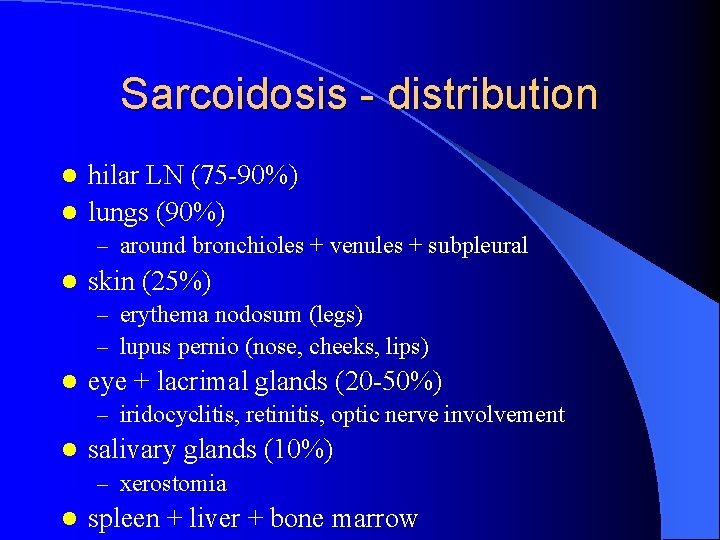
Sarcoidosis - distribution hilar LN (75 -90%) l lungs (90%) l – around bronchioles + venules + subpleural l skin (25%) – erythema nodosum (legs) – lupus pernio (nose, cheeks, lips) l eye + lacrimal glands (20 -50%) – iridocyclitis, retinitis, optic nerve involvement l salivary glands (10%) – xerostomia l spleen + liver + bone marrow
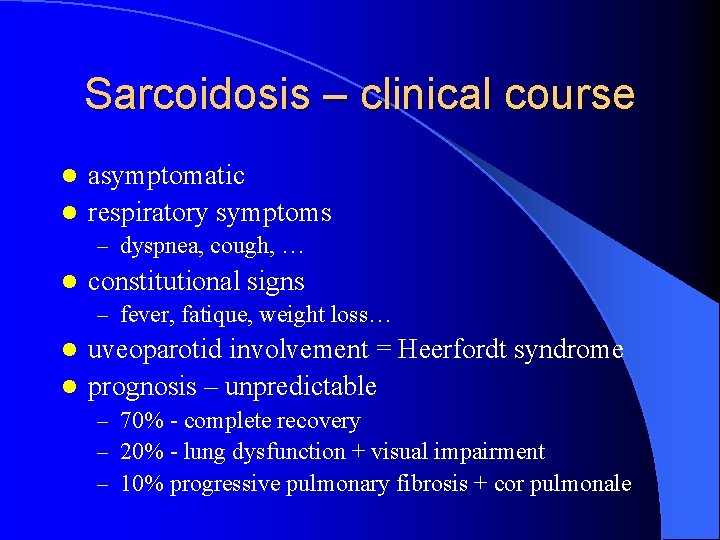
Sarcoidosis – clinical course asymptomatic l respiratory symptoms l – dyspnea, cough, … l constitutional signs – fever, fatique, weight loss… uveoparotid involvement = Heerfordt syndrome l prognosis – unpredictable l – 70% - complete recovery – 20% - lung dysfunction + visual impairment – 10% progressive pulmonary fibrosis + cor pulmonale
Summary l l l l 1. Atelectasis 2. Obstructive lung diseases 3. Restrictive lung diseases 4. Vascular lung diseases 5. Pulmonary infections 6. Lung tumors 7. Pleural lesions 8. Lesions of upper RT
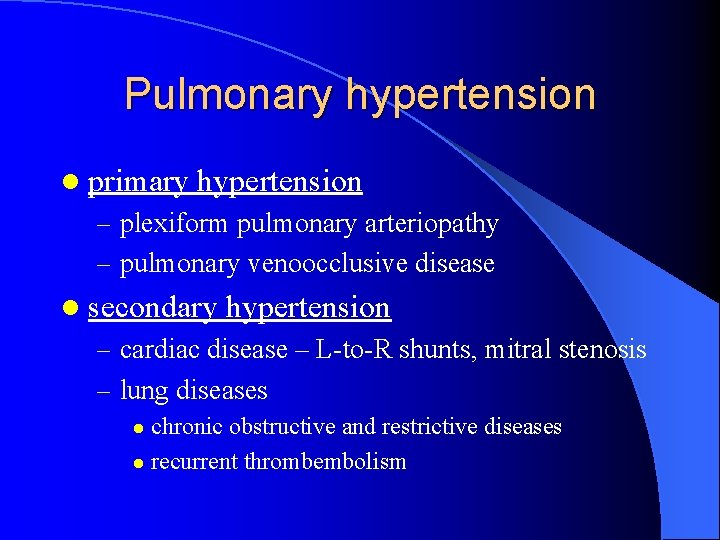
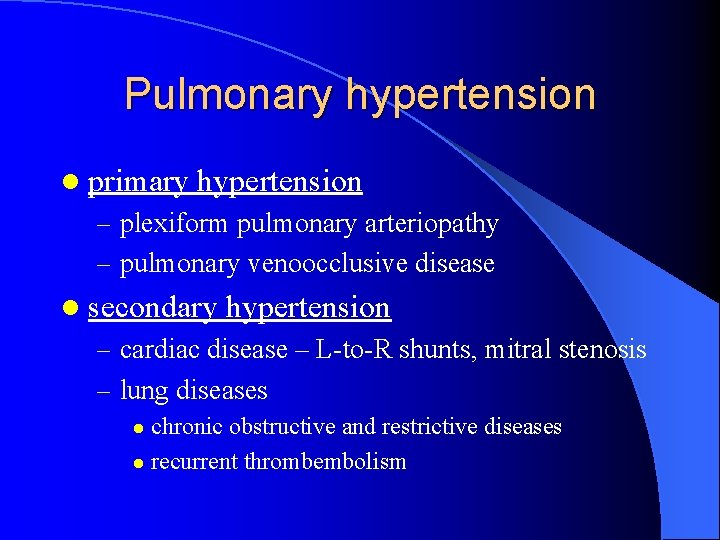
Pulmonary hypertension l primary hypertension – plexiform pulmonary arteriopathy – pulmonary venoocclusive disease l secondary hypertension – cardiac disease – L-to-R shunts, mitral stenosis – lung diseases chronic obstructive and restrictive diseases l recurrent thrombembolism l
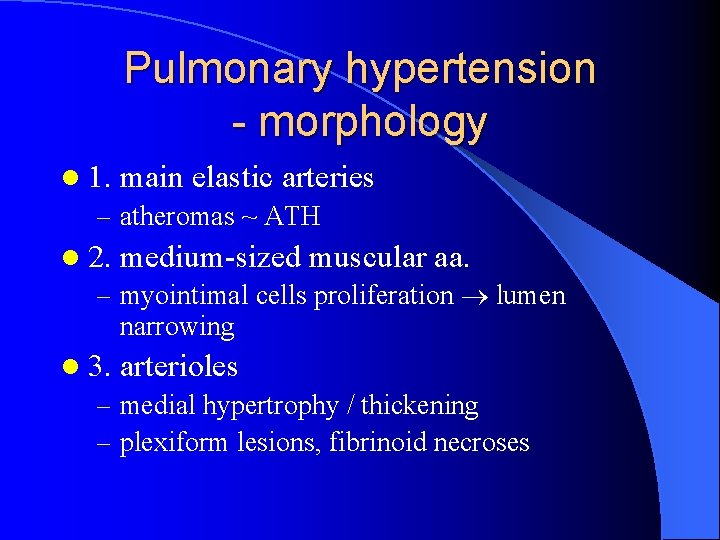
Pulmonary hypertension - morphology l 1. main elastic arteries – atheromas ~ ATH l 2. medium-sized muscular aa. – myointimal cells proliferation lumen narrowing l 3. arterioles – medial hypertrophy / thickening – plexiform lesions, fibrinoid necroses
Summary l l l l 1. Atelectasis 2. Obstructive lung diseases 3. Restrictive lung diseases 4. Vascular lung diseases 5. Pulmonary infections 6. Lung tumors 7. Pleural lesions 8. Lesions of upper RT
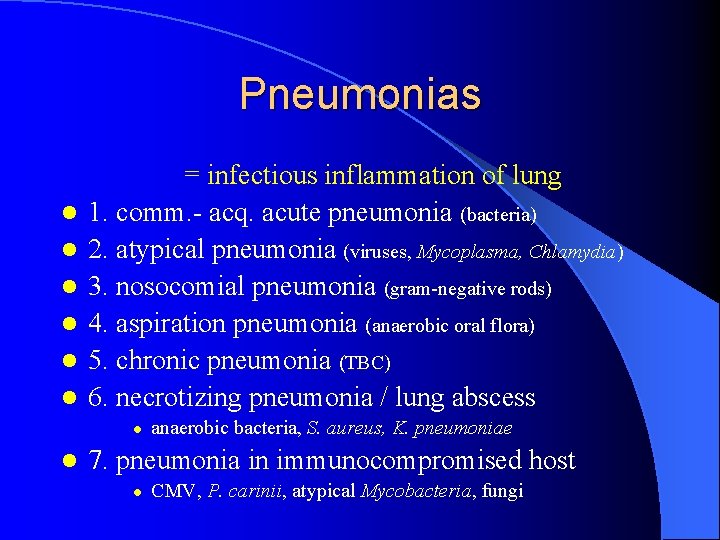
Pneumonias l l l = infectious inflammation of lung 1. comm. - acq. acute pneumonia (bacteria) 2. atypical pneumonia (viruses, Mycoplasma, Chlamydia) 3. nosocomial pneumonia (gram-negative rods) 4. aspiration pneumonia (anaerobic oral flora) 5. chronic pneumonia (TBC) 6. necrotizing pneumonia / lung abscess l l anaerobic bacteria, S. aureus, K. pneumoniae 7. pneumonia in immunocompromised host l CMV, P. carinii, atypical Mycobacteria, fungi
Bronchopneumonia Streptococci, Staphylococci, H. influenzae l from lower airways alveoli l grossly l – patchy inflammatory consolidation – bilateral basal localization – 3 -4 cm, red to yellow patches l microscopically – suppurative inflammation in bronchi + bronchioles + alveoli
Lobar pneumonia Streptococcus pneumoniae 1, 2, 3 l rapid spread within alveoli l 1. congestion - heavy, red, boggy l – alveolar edema + neutrophils l 2. red hepatization - liver-like consistency – alveoli fulfilled by neutrophils, RBCs, fibrin – fibrinous / fibrinopurulent pleuritis l 3. gray hepatization - dry, firm – RBCs lysis + fibrin persistance l 4. resolution
Pneumonia - complications l 1. lung abscess – – – acute x chronic bronchogenic – S. aureus, K. pneumoniae x hematogenic (peripheral pyemia) bronchopleural fistulas – pneumothorax + empyema brain abscess + AA amyloidosis 2. empyema l 3. lung fibrosis + pleural adhesions l 4. bacteremia l – meningitis, arthritis, infective endocarditis
Atypical pneumonia viruses (influenza, adenovirus, RSV, CMV) l Chlamydiae, Rickettsiae l grossly l – patchy x segmental x lobular, red-blue, congested areas l microscopically – alveolar septa – edema + mononuclear infiltrate l prognosis – complete recovery – bacterial superinfection – ARDS
Tuberculosis Mycobacterium tuberculosis l Ziehl-Neelsen – acid-fast red rod l inhalation lungs l T cells mediated immunity l – organism resistance – tissue hypersensitivity – caseous necrosis l caseating granulomas – central caseous necrosis – epithelioid cells + multinucleated giant cells (Langhans) – T-lymphocytic rim
Primary TBC l previously unexposed (unsensitized) person l Ghon focus – lung middle line + subpleural location – 1 -1. 5 cm, gray-white lesion l Ghon complex: + TBC hilar LNitis l + lympho / hematogenous dissemination – under immune control
Primary TBC - further course 1. healed lesions – fibrocalcific scar l 2. latent lesions (dormant TBC organisms) l 3. cervical LNitis („scrophula“) l 3. progressive primary TBC l – miliary („millet“) TBC - 2 mm, yellow-white – pulmonary l l lymphatics – thoracic duct – venous circulation – right heart – pulmonary a. – lungs pleural effusion, TBC empyema – systemic l l pulmonary veins – left heart – systemic circulation liver, BM, spleen, adrenals, menings, kidneys, fall. t. , epid.
Secondary TBC in previously sensitized person l 1. exogenous reinfection l 2. reactivation l – pulmonary TBC (from adenobronchial fistula) l l l upper lobes apex cavitation – airways dissemination – progressive pulmonary TBC bronchus erosion - endo-bronchial, -tracheal, laryngeal TBC blood vessel erosion – hemoptysis pulmonary + systemic miliary TBC – isolated-organ metastasis (from primary TBC metast. ) l TBC meningitis, epinephritis, osteomyelitis, salpingitis
Summary l l l l 1. Atelectasis 2. Obstructive lung diseases 3. Restrictive lung diseases 4. Vascular lung diseases 5. Pulmonary infections 6. Lung tumors 7. Pleural lesions 8. Lesions of upper RT
Lung carcinoma l primary x secondary (metastases) l 95 % bronchogenic carcinoma – bronchial epithelium l 5% miscellaneous – carcinoid, bronchial glands, mesenchyma l benign - hamartomas
Bronchogenic carcinoma very common, !!! smoking !!! l peak incidence 55 – 65 years l M: F… 2: 1 l 1. non-small cell lung carcinoma (70 -75%) l l surgery – squamous cell carcinoma (25 -30%) – adenocarcinoma (30 -35%) – large cell carcinoma (10 -15%) l 2. small cell lung carcinoma (20 -25%) l l chemotherapy +/- actinotherapy 3. combined carcinoma (5 -10%)
Bronchogenic carcinoma advanced stage + metastases – symptoms l chronic cough, hoarseness, chest pain l Pancoast tumors – upper lobe apex l – branchial plexus invasion – sympathetic plexus invasion – Horner syndrome l paraneoplastic syndromes – – – hypercalcemia – PTH-related peptide Cushing syndrome - ACTH SIADH - ADH neuromuscular syndromes – myasthenic syndrome hematologic – NBTE, DIC
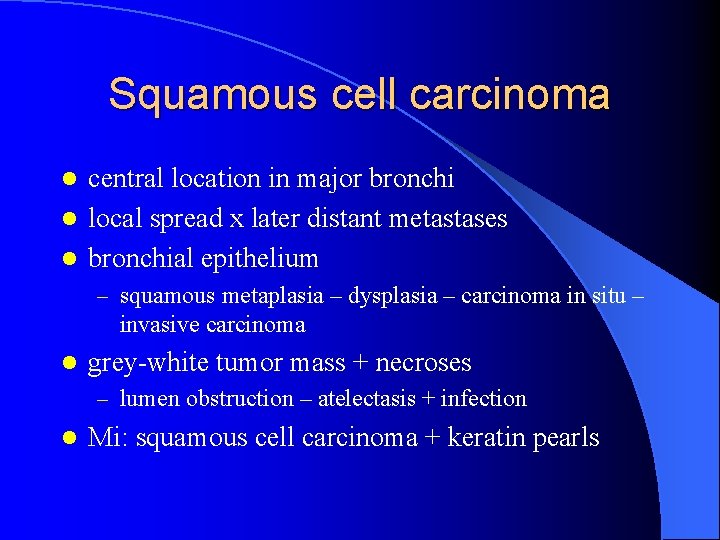
Squamous cell carcinoma central location in major bronchi l local spread x later distant metastases l bronchial epithelium l – squamous metaplasia – dysplasia – carcinoma in situ – invasive carcinoma l grey-white tumor mass + necroses – lumen obstruction – atelectasis + infection l Mi: squamous cell carcinoma + keratin pearls
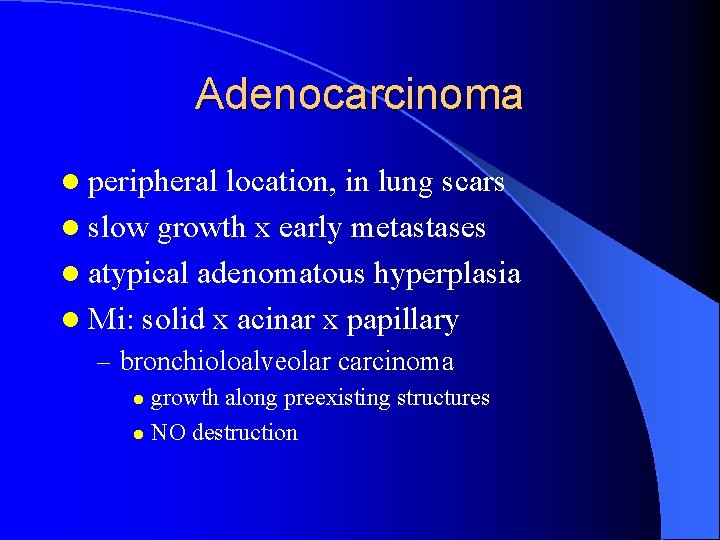
Adenocarcinoma l peripheral location, in lung scars l slow growth x early metastases l atypical adenomatous hyperplasia l Mi: solid x acinar x papillary – bronchioloalveolar carcinoma growth along preexisting structures l NO destruction l
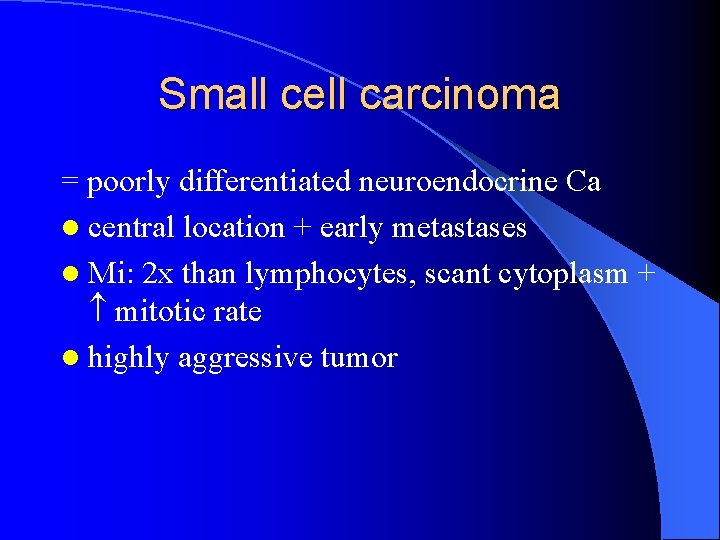
Small cell carcinoma = poorly differentiated neuroendocrine Ca l central location + early metastases l Mi: 2 x than lymphocytes, scant cytoplasm + mitotic rate l highly aggressive tumor
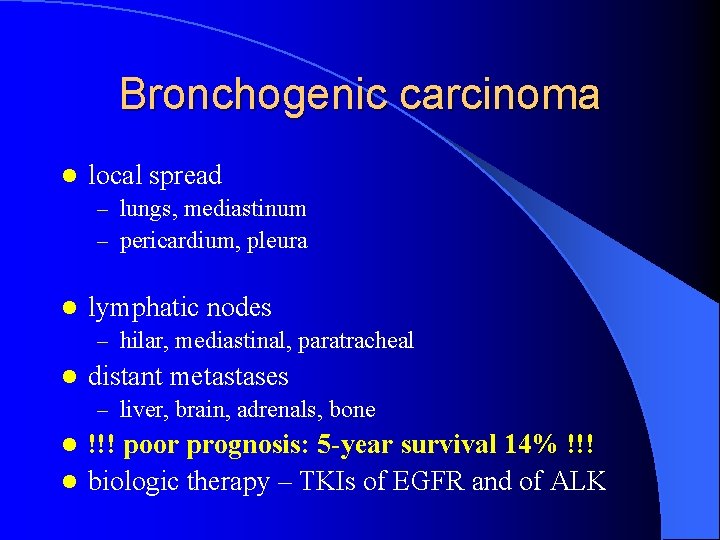
Bronchogenic carcinoma l local spread – lungs, mediastinum – pericardium, pleura l lymphatic nodes – hilar, mediastinal, paratracheal l distant metastases – liver, brain, adrenals, bone !!! poor prognosis: 5 -year survival 14% !!! l biologic therapy – TKIs of EGFR and of ALK l
Summary l l l l 1. Atelectasis 2. Obstructive lung diseases 3. Restrictive lung diseases 4. Vascular lung diseases 5. Pulmonary infections 6. Lung tumors 7. Pleural lesions 8. Lesions of upper RT
Pleural effusion l 1. hydrothorax – transudate – congestive heart failure l 2. pleuritis + exudate – – l pulmonary infections + TBC neoplasms (lung, mesothelioma) pulmonary infarction viral pleuritis complications – suppurative, fibrinous pleuritis organization adhesions + calcification
Other pleural conditions l 3. pneumothorax – air in pleural sac – lung disease (emphysema, abscess, carcinoma) – thoracic wall injury (rib fracture) – complications l l mediastinum shift + lung compression 4. hemothorax – blood in pleural sac – thoracic aorta aneurysm rupture l 5. chylothorax – lymph in pleural sac – obstruction of lymphatic ducts (mediastinal neoplasms)
Mesothelioma rare malignant tumor of mesothelial cells l asbestos exposure + long latent period l grossly l – lung ensheathed by yellow-white firm / gelatinous mass + pleural obliteration – invasion into lung + thoracic wall l microscopically – epithelial + sarcomatoid + biphasic l poor prognosis
Summary l l l l 1. Atelectasis 2. Obstructive lung diseases 3. Restrictive lung diseases 4. Vascular lung diseases 5. Pulmonary infections 6. Lung tumors 7. Pleural lesions 8. Lesions of upper RT
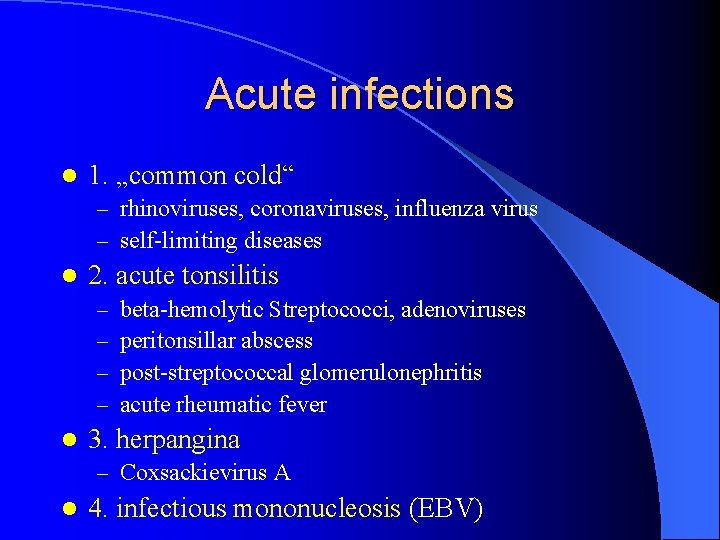
Acute infections l 1. „common cold“ – rhinoviruses, coronaviruses, influenza virus – self-limiting diseases l 2. acute tonsilitis – – l beta-hemolytic Streptococci, adenoviruses peritonsillar abscess post-streptococcal glomerulonephritis acute rheumatic fever 3. herpangina – Coxsackievirus A l 4. infectious mononucleosis (EBV)
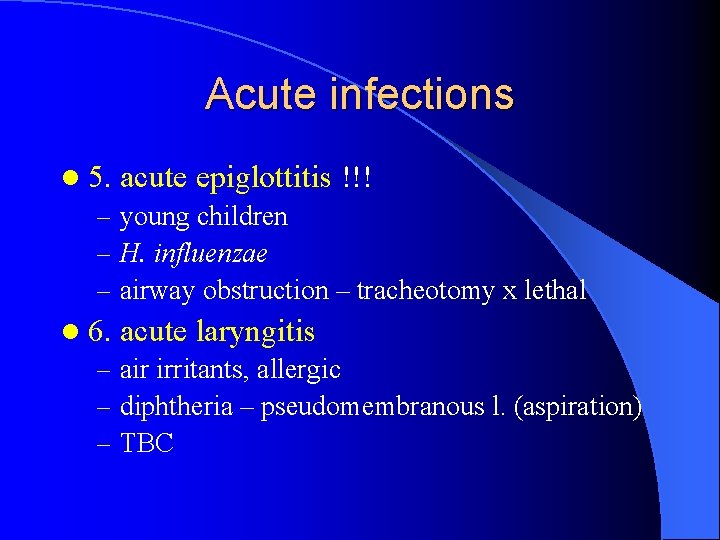
Acute infections l 5. acute epiglottitis !!! – young children – H. influenzae – airway obstruction – tracheotomy x lethal l 6. acute laryngitis – air irritants, allergic – diphtheria – pseudomembranous l. (aspiration) – TBC
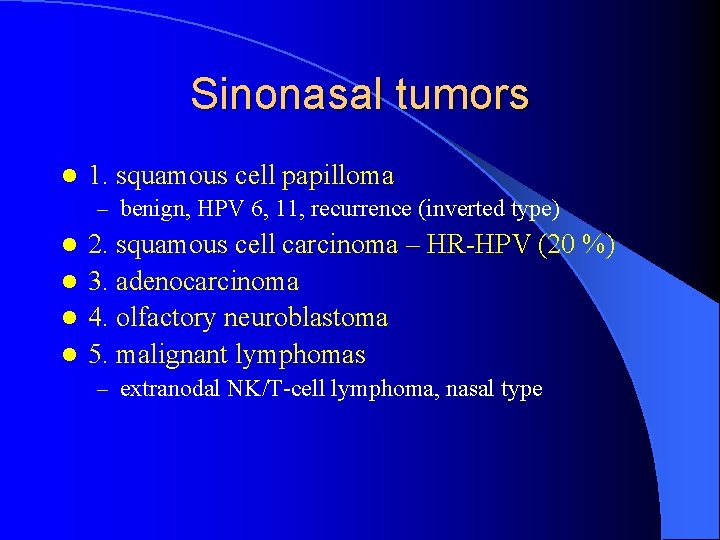
Sinonasal tumors l 1. squamous cell papilloma – benign, HPV 6, 11, recurrence (inverted type) 2. squamous cell carcinoma – HR-HPV (20 %) l 3. adenocarcinoma l 4. olfactory neuroblastoma l 5. malignant lymphomas l – extranodal NK/T-cell lymphoma, nasal type

Nasopharyngeal tumors l 1. angiofibroma – young boys – benign x locally destructive + bleeding l 2. keratinizing squamous cell carcinoma l 3. nonkeratinizing carcinoma (lymphoepithelial carcinoma) – EBV, China l 4. malignant lymphomas
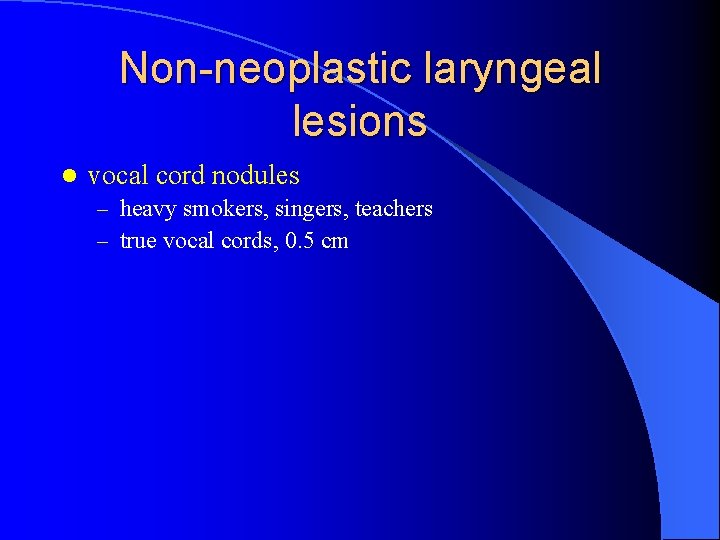
Non-neoplastic laryngeal lesions l vocal cord nodules – heavy smokers, singers, teachers – true vocal cords, 0. 5 cm

Benign laryngeal tumors l squamous papilloma – – benign true vocal cords soft excrescence, 1 cm children – multiple l l l juvenile laryngeal papillomatosis HPV 6, 11 spontaneous regress
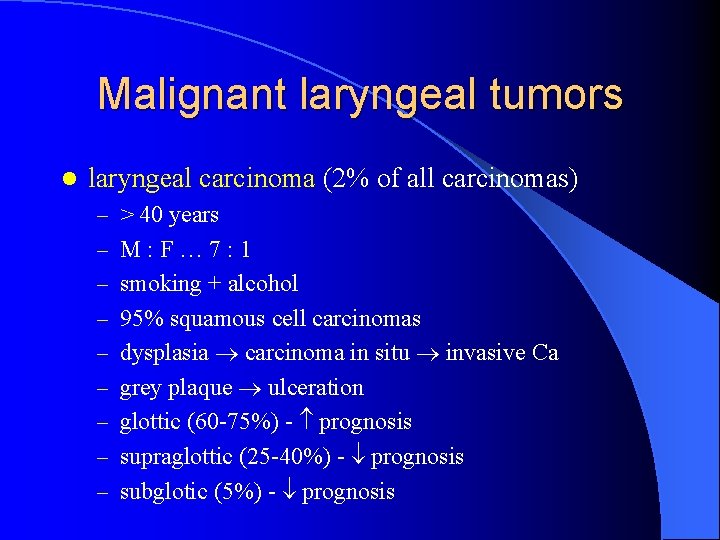
Malignant laryngeal tumors l laryngeal carcinoma (2% of all carcinomas) – > 40 years – M: F… 7: 1 – smoking + alcohol – 95% squamous cell carcinomas – dysplasia carcinoma in situ invasive Ca – grey plaque ulceration – glottic (60 -75%) - prognosis – supraglottic (25 -40%) - prognosis – subglotic (5%) - prognosis