PATHOLOGY OF CERVIX Cervix Anatomy n n n



- Slides: 111
PATHOLOGY OF CERVIX
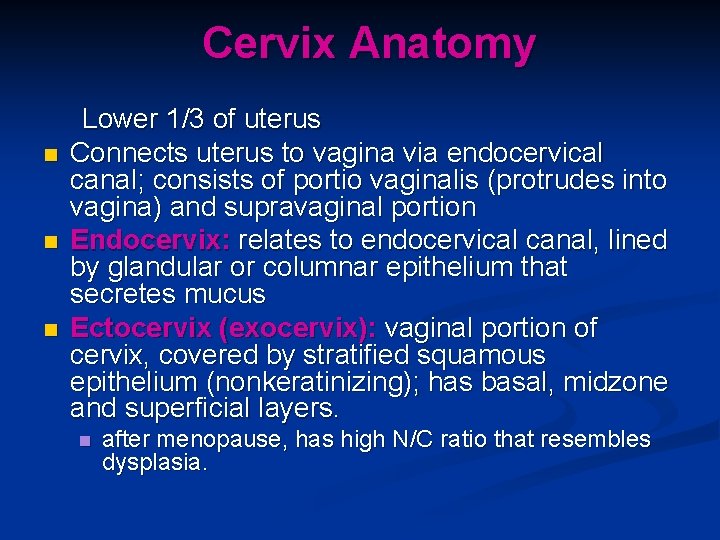
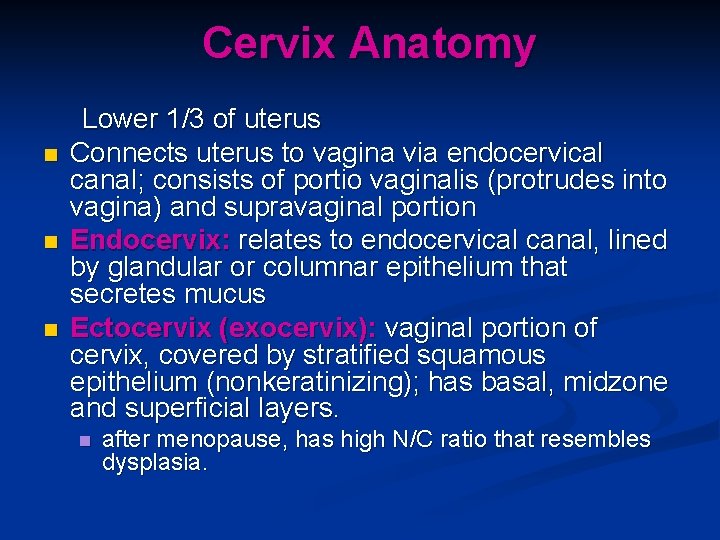
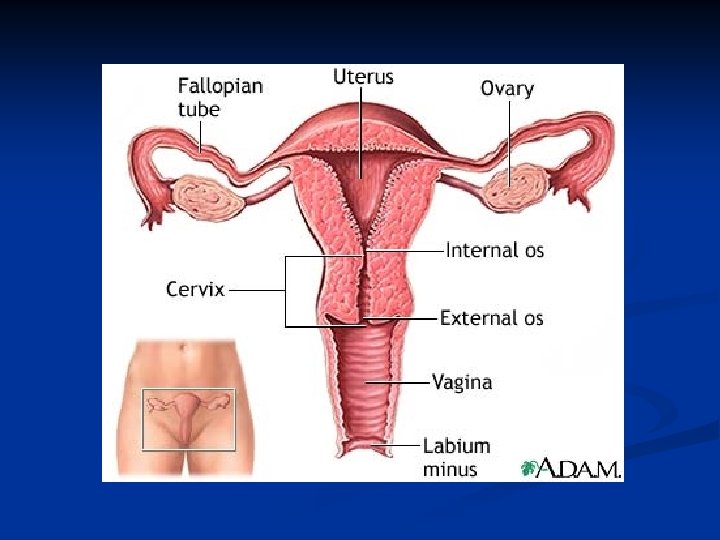
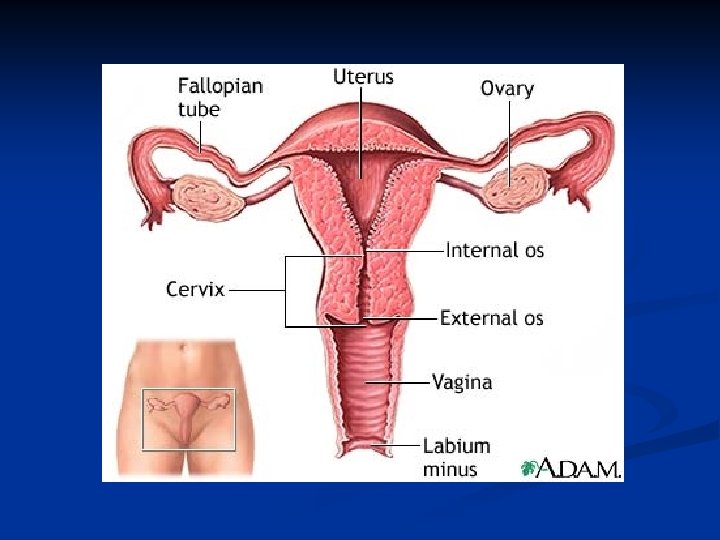
Cervix Anatomy n n n Lower 1/3 of uterus Connects uterus to vagina via endocervical canal; consists of portio vaginalis (protrudes into vagina) and supravaginal portion Endocervix: relates to endocervical canal, lined by glandular or columnar epithelium that secretes mucus Ectocervix (exocervix): vaginal portion of cervix, covered by stratified squamous epithelium (nonkeratinizing); has basal, midzone and superficial layers. n after menopause, has high N/C ratio that resembles dysplasia.
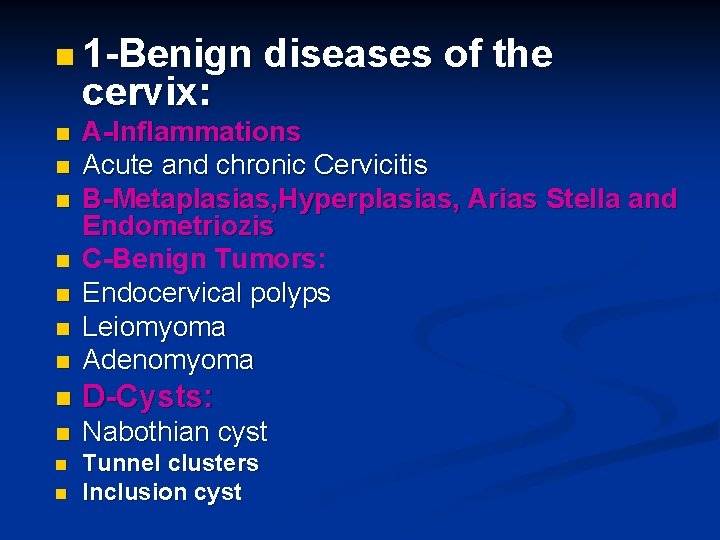
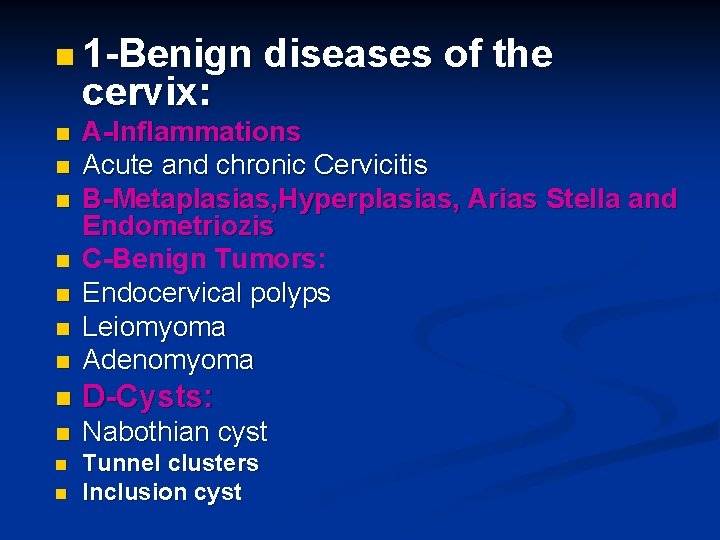
n 1 -Benign cervix: diseases of the n A-Inflammations Acute and chronic Cervicitis B-Metaplasias, Hyperplasias, Arias Stella and Endometriozis C-Benign Tumors: Endocervical polyps Leiomyoma Adenomyoma n D-Cysts: n Nabothian cyst n Tunnel clusters Inclusion cyst n n n n
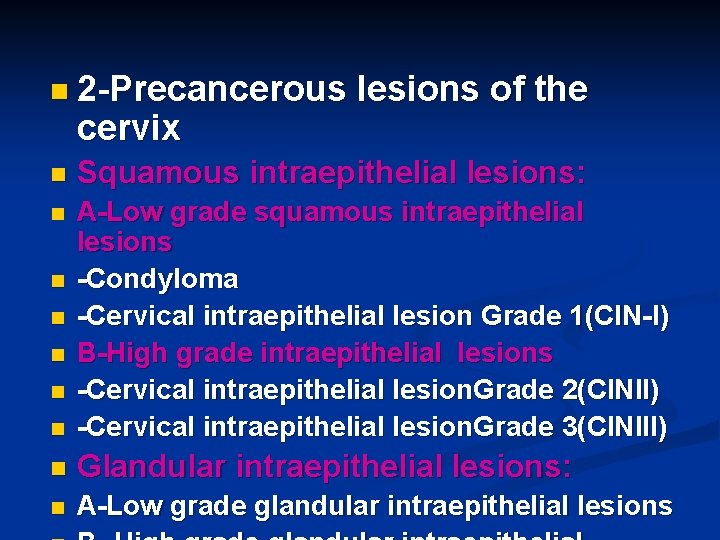
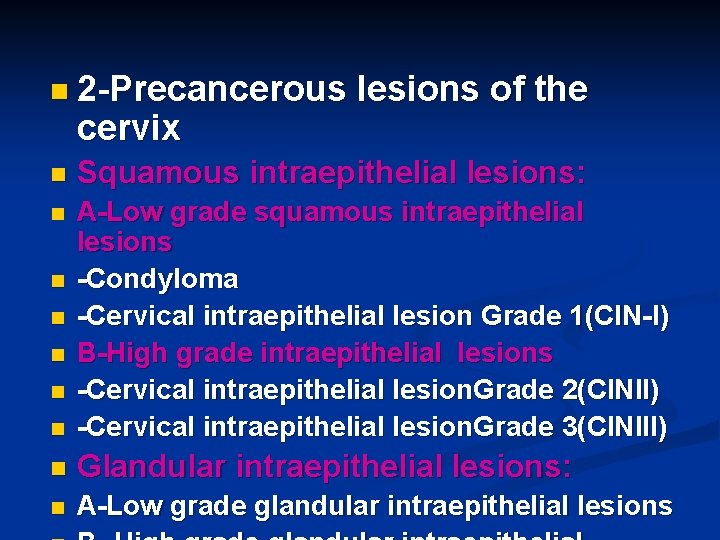
n 2 -Precancerous cervix lesions of the n Squamous intraepithelial lesions: n n A-Low grade squamous intraepithelial lesions -Condyloma -Cervical intraepithelial lesion Grade 1(CIN-I) B-High grade intraepithelial lesions -Cervical intraepithelial lesion. Grade 2(CINII) -Cervical intraepithelial lesion. Grade 3(CINIII) n Glandular intraepithelial lesions: n A-Low grade glandular intraepithelial lesions n n
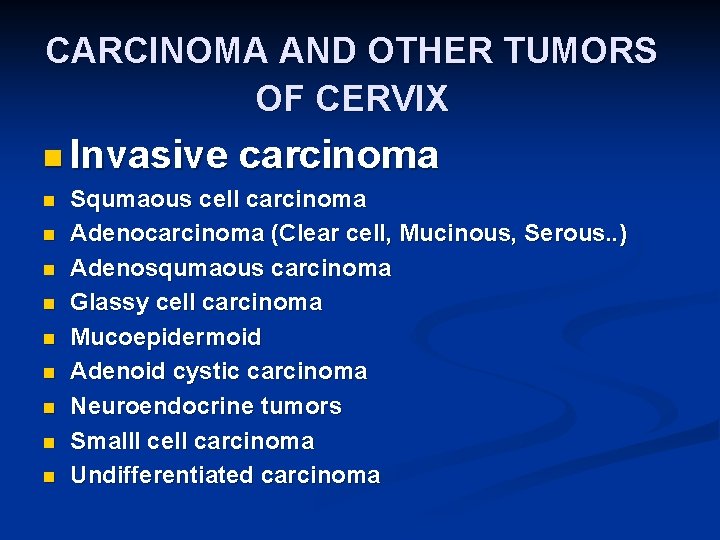
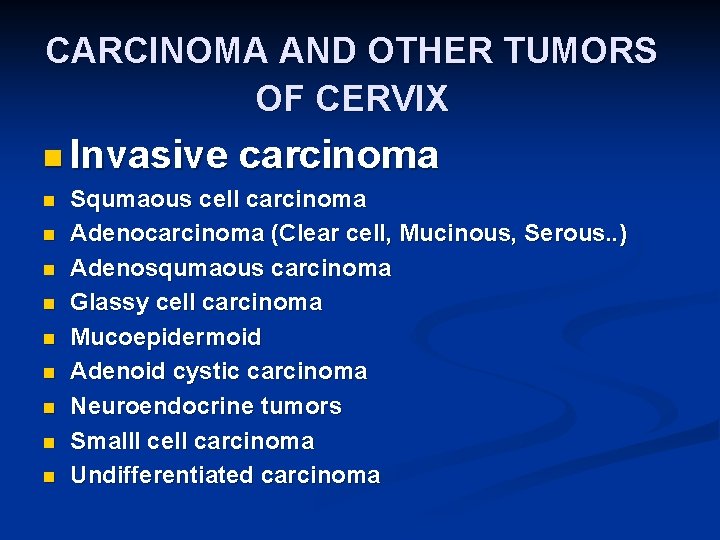
CARCINOMA AND OTHER TUMORS OF CERVIX n Invasive n n n n n carcinoma Squmaous cell carcinoma Adenocarcinoma (Clear cell, Mucinous, Serous. . ) Adenosqumaous carcinoma Glassy cell carcinoma Mucoepidermoid Adenoid cystic carcinoma Neuroendocrine tumors Smalll cell carcinoma Undifferentiated carcinoma
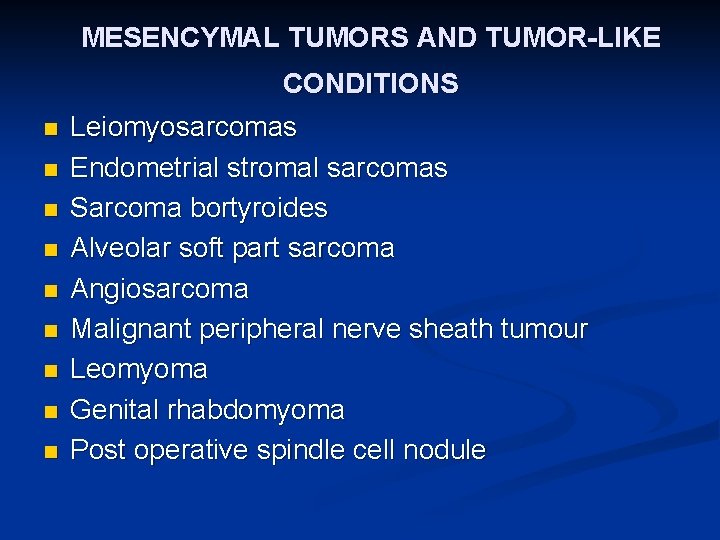
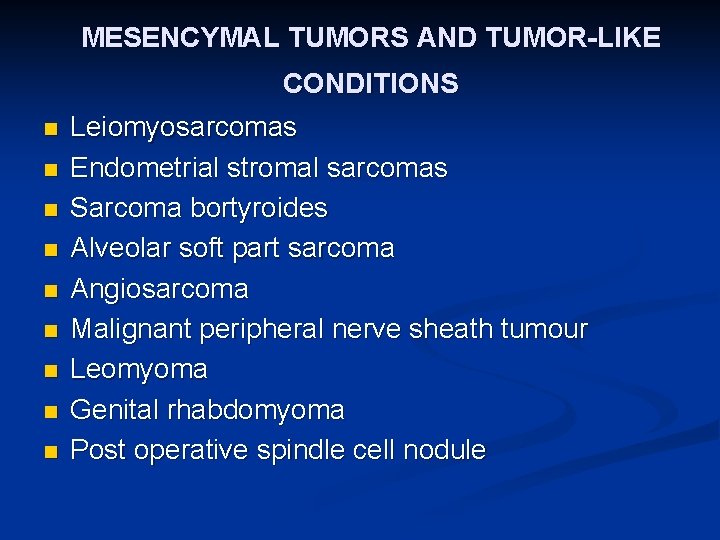
MESENCYMAL TUMORS AND TUMOR-LIKE CONDITIONS n n n n n Leiomyosarcomas Endometrial stromal sarcomas Sarcoma bortyroides Alveolar soft part sarcoma Angiosarcoma Malignant peripheral nerve sheath tumour Leomyoma Genital rhabdomyoma Post operative spindle cell nodule
MIXED EPITHELIAL MESENCYMAL TUMOURS Carcinosarcoma n Adenosarcoma n Wilms tumour n Adenofibroma n Adenomyoma n
Melanocytic tumors n Lymphoid and haematopoetic tumours n Metastatic tumors n Other tumors: Yolk sac tumour Dermoid cyst Mature cystic teratoma n
ACUTE AND CHRONIC CERVICITIS n n n Menarche- the production of estrogens by the ovary stimulates maturation (glycogen uptake) of cervical and vaginal squamous mucosa. These cells are shed, the glycogen provides a substrate for endogenous vaginal aerobes and anaerobes, streptococci, enterococci, Escherichia coli, and staphylococci. The bacterial growth produces a drop in vaginal p. H.
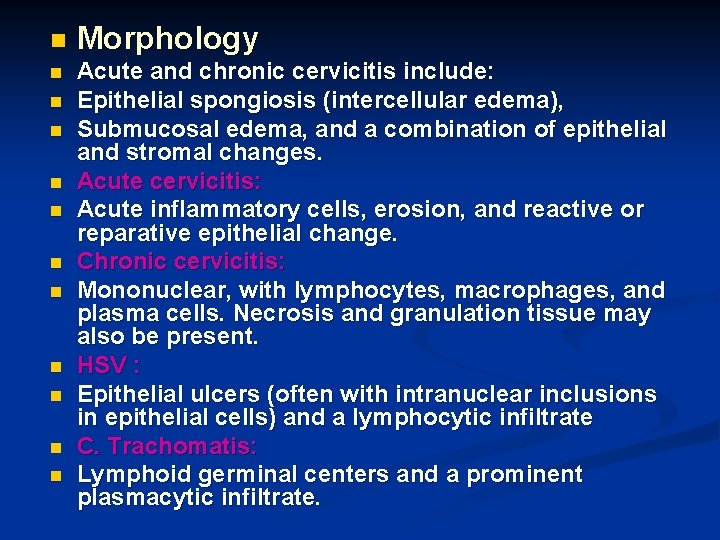
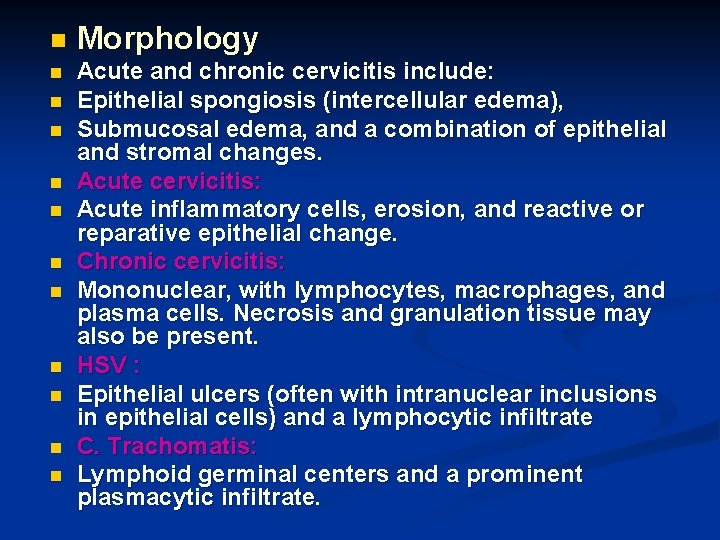
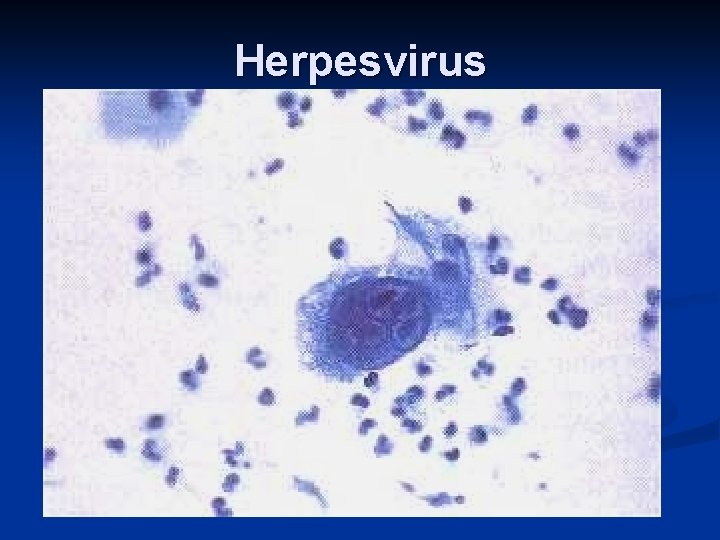
n Morphology n Acute and chronic cervicitis include: Epithelial spongiosis (intercellular edema), Submucosal edema, and a combination of epithelial and stromal changes. Acute cervicitis: Acute inflammatory cells, erosion, and reactive or reparative epithelial change. Chronic cervicitis: Mononuclear, with lymphocytes, macrophages, and plasma cells. Necrosis and granulation tissue may also be present. HSV : Epithelial ulcers (often with intranuclear inclusions in epithelial cells) and a lymphocytic infiltrate C. Trachomatis: Lymphoid germinal centers and a prominent plasmacytic infiltrate. n n n n n
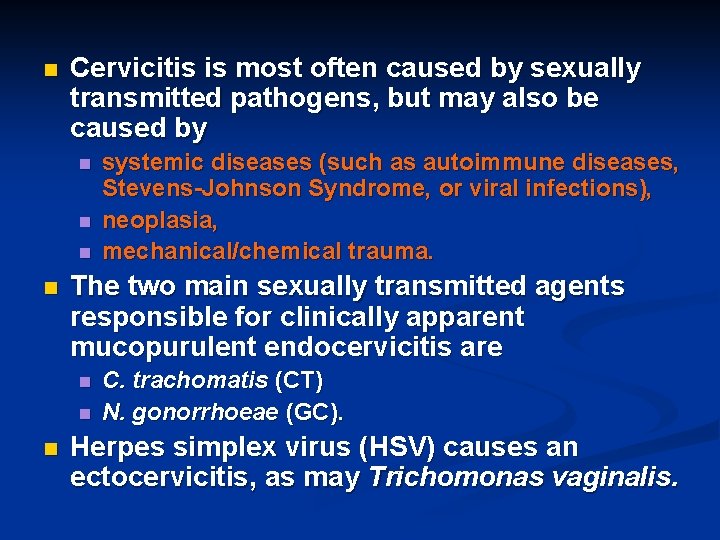
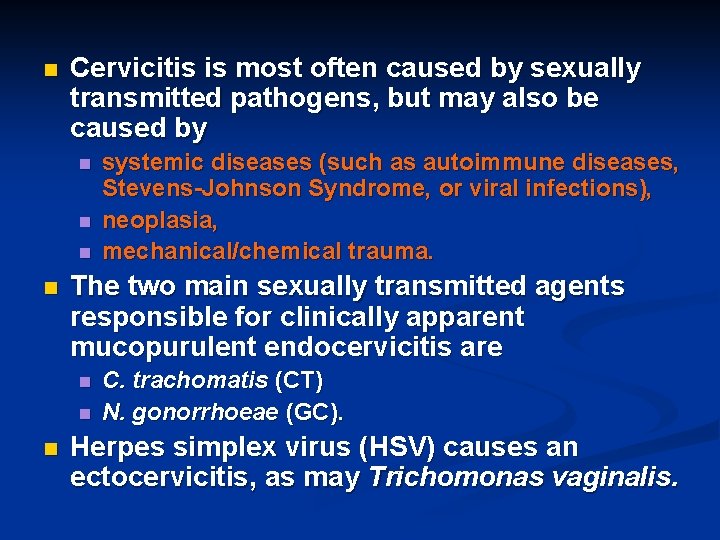
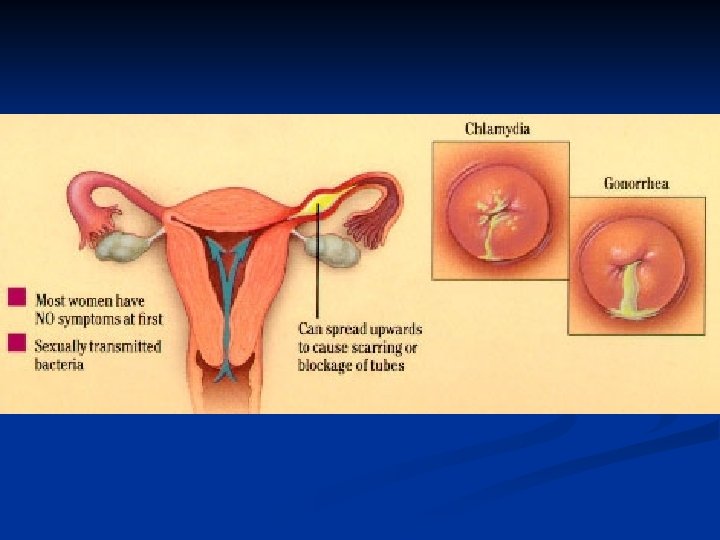
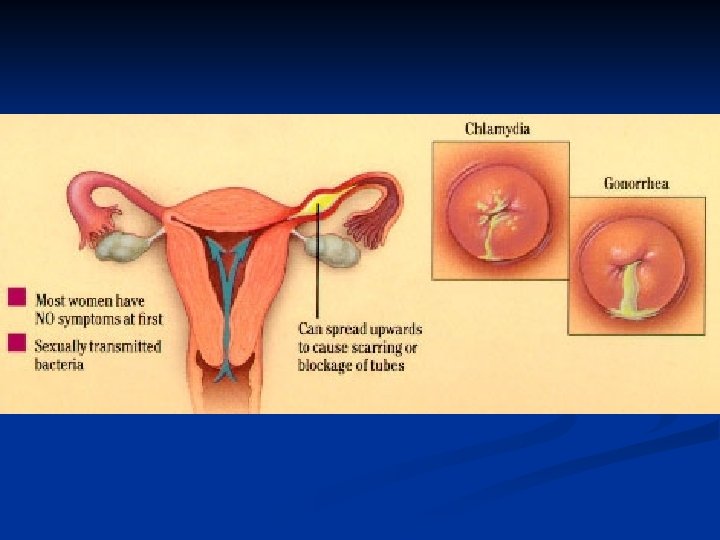
n Cervicitis is most often caused by sexually transmitted pathogens, but may also be caused by n n The two main sexually transmitted agents responsible for clinically apparent mucopurulent endocervicitis are n n n systemic diseases (such as autoimmune diseases, Stevens-Johnson Syndrome, or viral infections), neoplasia, mechanical/chemical trauma. C. trachomatis (CT) N. gonorrhoeae (GC). Herpes simplex virus (HSV) causes an ectocervicitis, as may Trichomonas vaginalis.
n n n The exposed endocervix is sensitive to these changes in chemical environment and bacterial flora and responds by undergoing a variety of changes including proliferation of reserve cells leading to squamous metaplasia (in the reproductive years) This process is invariably associated with an inflammatory infiltrate composed of a mixture of polymorphonuclear leukocytes and mononuclear cells, and if the inflammation is severe, it may be associated with loss of the epithelial lining (erosion or ulceration) and epithelial repair (reparative atypia ). All of these components characterize what is known as chronic cervicitis
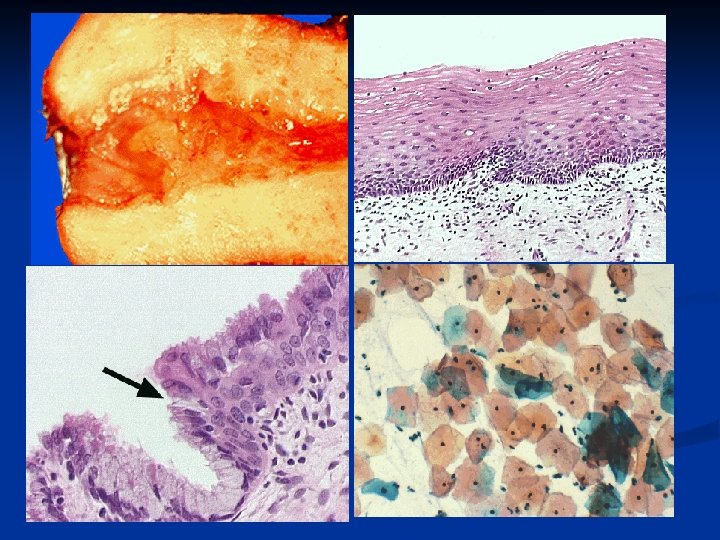
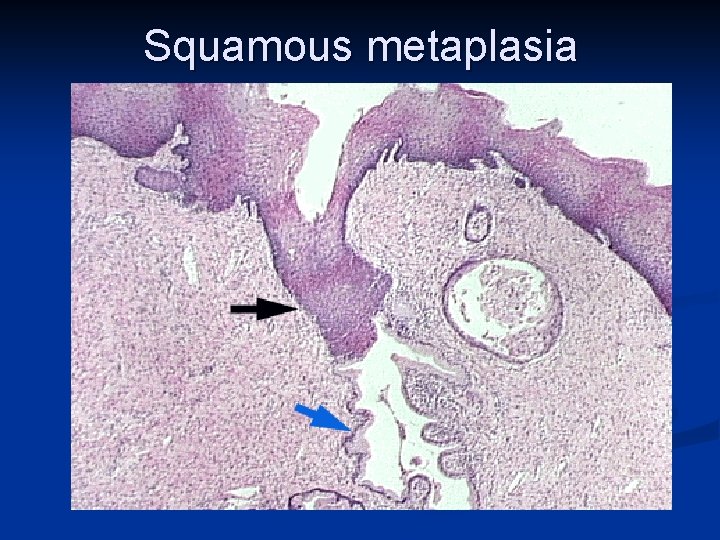
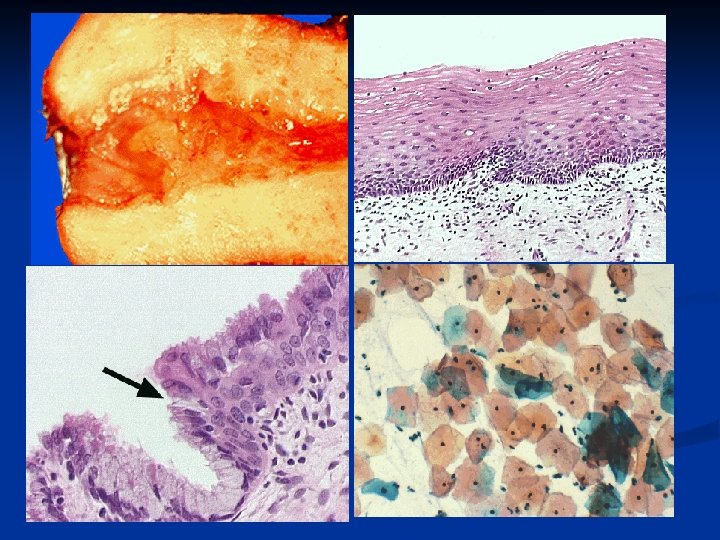
Squamous Metaplasia of Cervix Etiology: Associated with irritation, inflammation, low vaginal p. H n Pathogenesis: Appropriate stimulus triggers squamous rather than glandular differentation from the basal cells. n Epidemiology: Normal finding in the reproductive age woman n General Gross Description: Tan gray surface similar to mature squamous epithelium n
General Microscopic Description n Seen in the transformation zone bound by a proximal margin of current squamocolumnar junction and distal margin of the original squamocolumnar junction n Epithelium in between derived from squamous metaplasia. n Mature metaplastic epithelium is indistinguishable from non-metaplastic stratified squamous epithelium, a look at the submucosa will show underlying endocervical clefts. n Begins as a proliferation of the subcolumnar reserve cells. The nuclei are large with prominent nucleoli and basal mitoses. Initially little maturation of the squamous epithelium is seen but this changes over
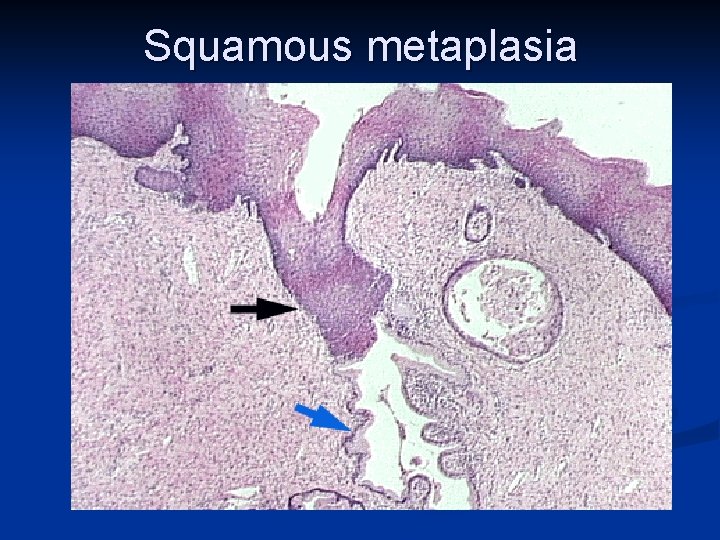
Squamous metaplasia
Microglandular hyperplasia n Results from progesterone stimulation of the endocervix n pregnancy, n old-fashioned n contraceptive pills. The glands are abundant and have only a lacy stroma between them, along with many neutrophils.
Arias-Stella reaction in endocx n Nuclear changes similar to that in endometrium, commonly seen during pregnancy or post-partum. n Microscopy: enlarged, dilated glands n lined by polyhedral cells with abundant eosinophilic cytoplasm with large clear vacuoles n hyperchromatic, and enlarged nuclei. n
Nabothian cysts As the squamous epithelium overgrows and obliterates the surface columnar papillae, it covers and obstructs crypt openings, with the accumulation of mucus in deeper crypts (glands) to form mucous (nabothian) cysts.
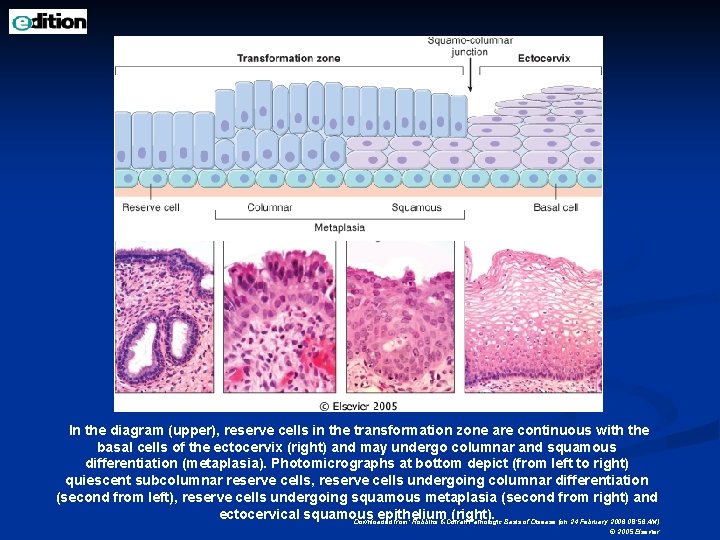
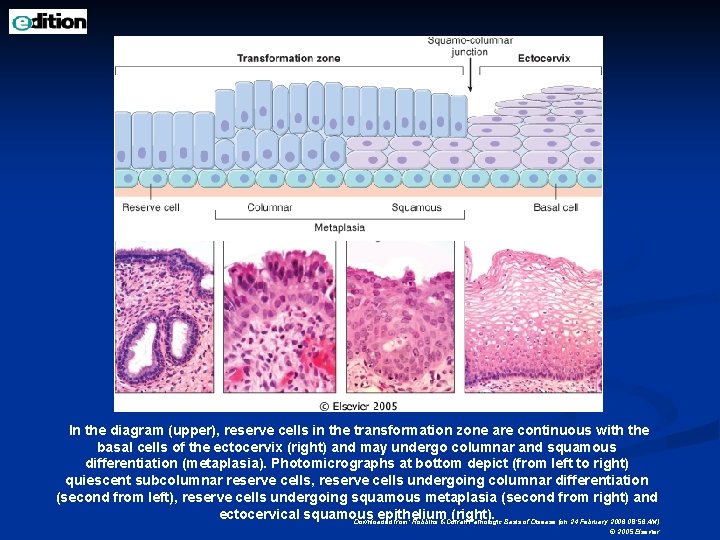
In the diagram (upper), reserve cells in the transformation zone are continuous with the basal cells of the ectocervix (right) and may undergo columnar and squamous differentiation (metaplasia). Photomicrographs at bottom depict (from left to right) quiescent subcolumnar reserve cells, reserve cells undergoing columnar differentiation (second from left), reserve cells undergoing squamous metaplasia (second from right) and ectocervical squamous epithelium (right). Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
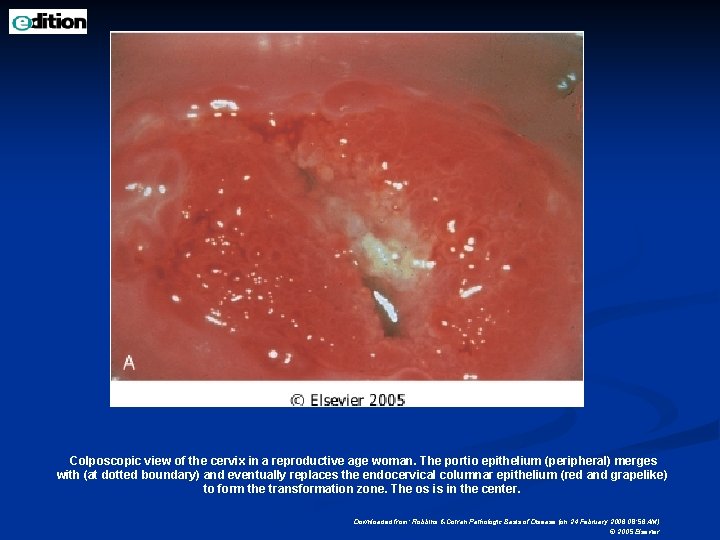
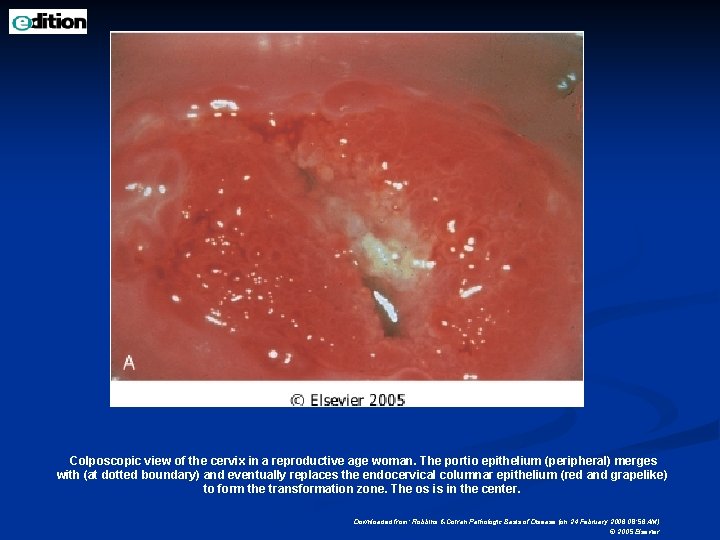
Colposcopic view of the cervix in a reproductive age woman. The portio epithelium (peripheral) merges with (at dotted boundary) and eventually replaces the endocervical columnar epithelium (red and grapelike) to form the transformation zone. The os is in the center. Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
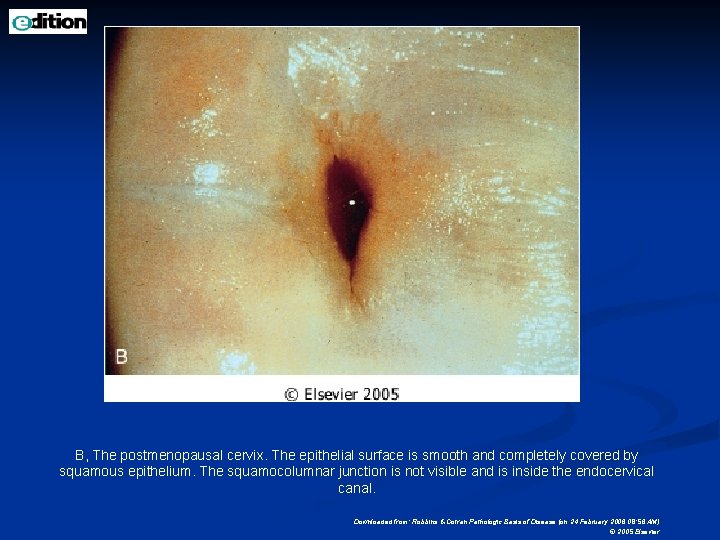
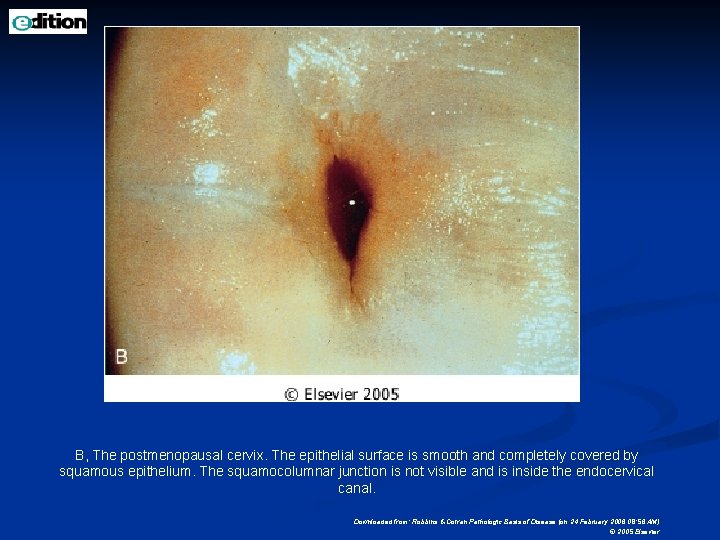
B, The postmenopausal cervix. The epithelial surface is smooth and completely covered by squamous epithelium. The squamocolumnar junction is not visible and is inside the endocervical canal. Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
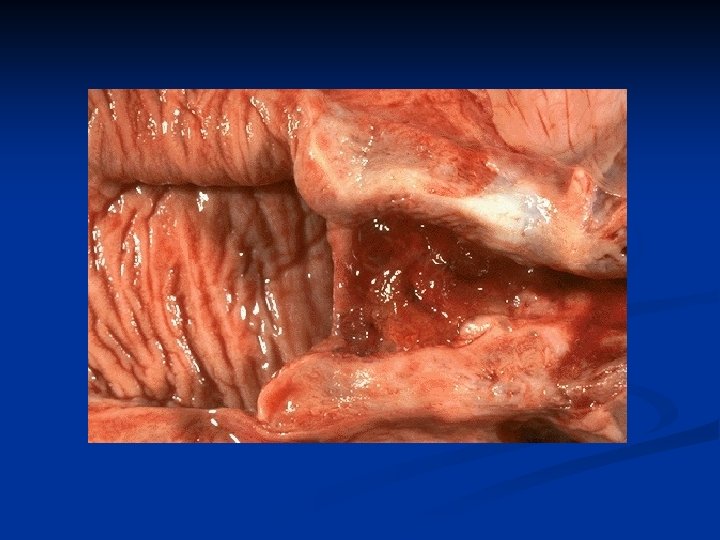
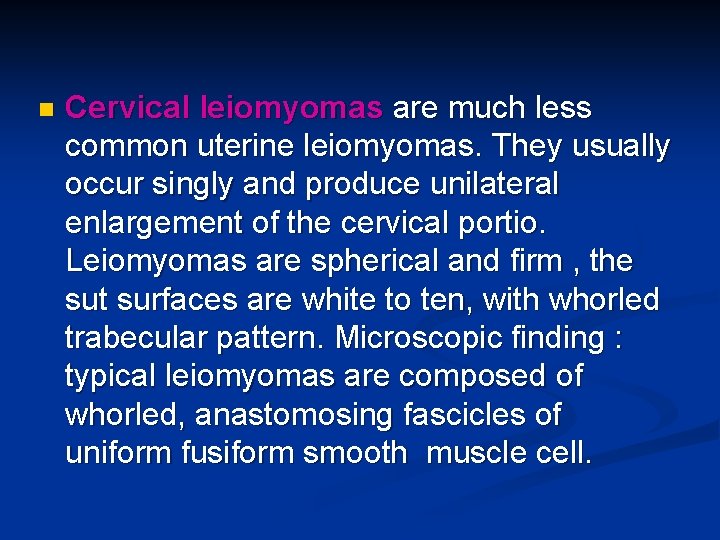
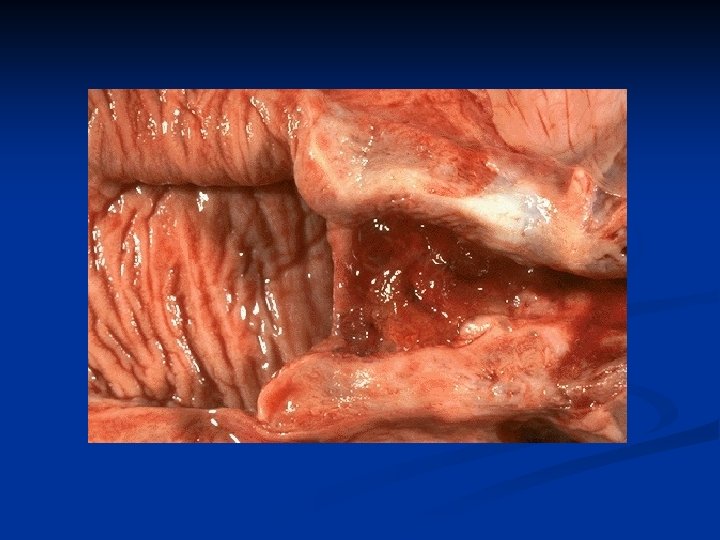
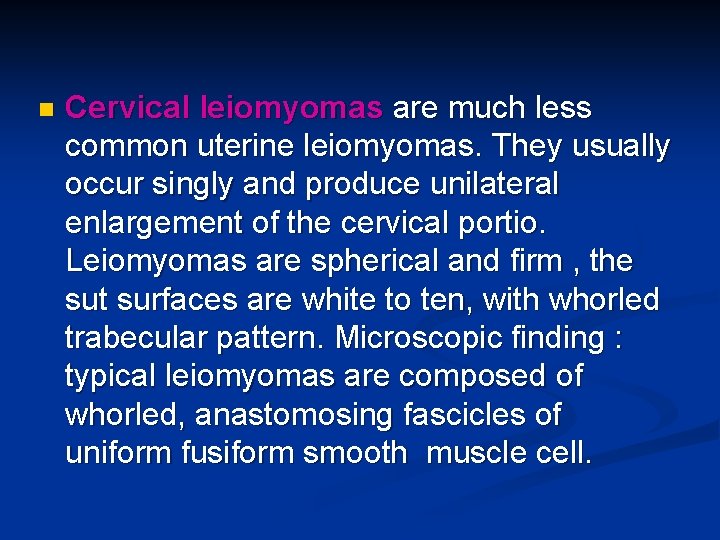
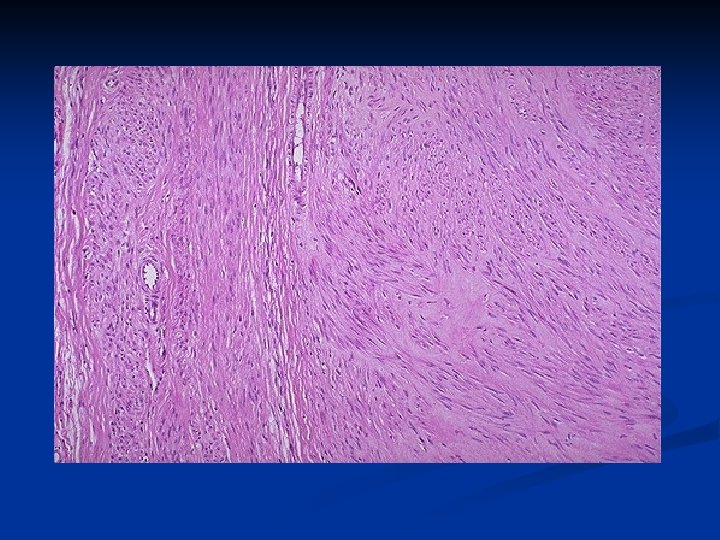
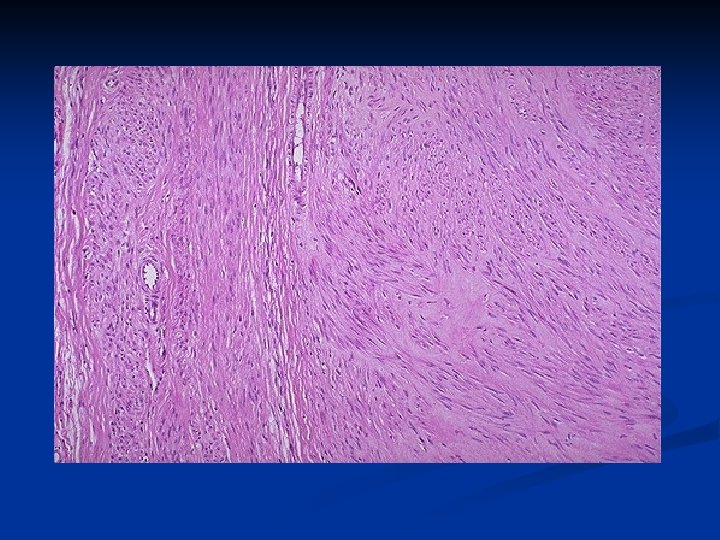
n Cervical leiomyomas are much less common uterine leiomyomas. They usually occur singly and produce unilateral enlargement of the cervical portio. Leiomyomas are spherical and firm , the sut surfaces are white to ten, with whorled trabecular pattern. Microscopic finding : typical leiomyomas are composed of whorled, anastomosing fascicles of uniform fusiform smooth muscle cell.
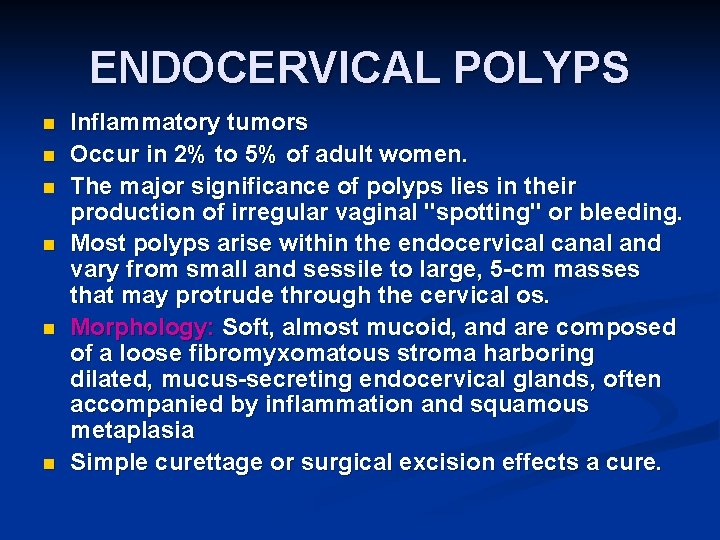
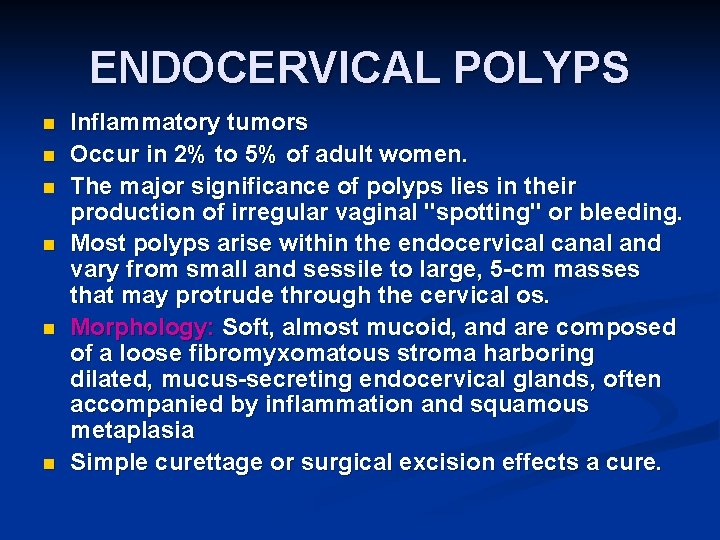
ENDOCERVICAL POLYPS n n n Inflammatory tumors Occur in 2% to 5% of adult women. The major significance of polyps lies in their production of irregular vaginal "spotting" or bleeding. Most polyps arise within the endocervical canal and vary from small and sessile to large, 5 -cm masses that may protrude through the cervical os. Morphology: Soft, almost mucoid, and are composed of a loose fibromyxomatous stroma harboring dilated, mucus-secreting endocervical glands, often accompanied by inflammation and squamous metaplasia Simple curettage or surgical excision effects a cure.
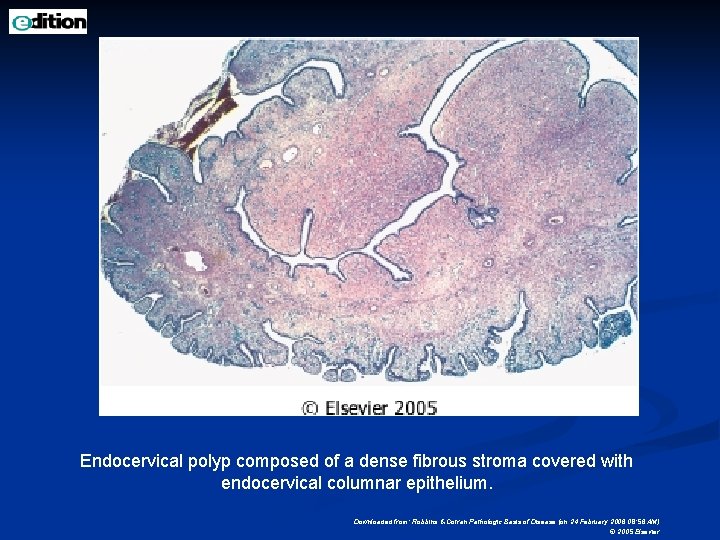
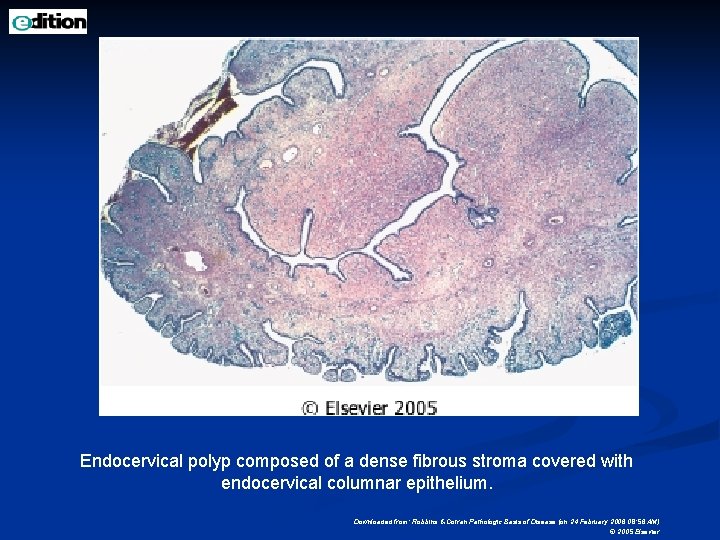
Endocervical polyp composed of a dense fibrous stroma covered with endocervical columnar epithelium. Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
Intraepithelial and Invasive Squamous Neoplasia
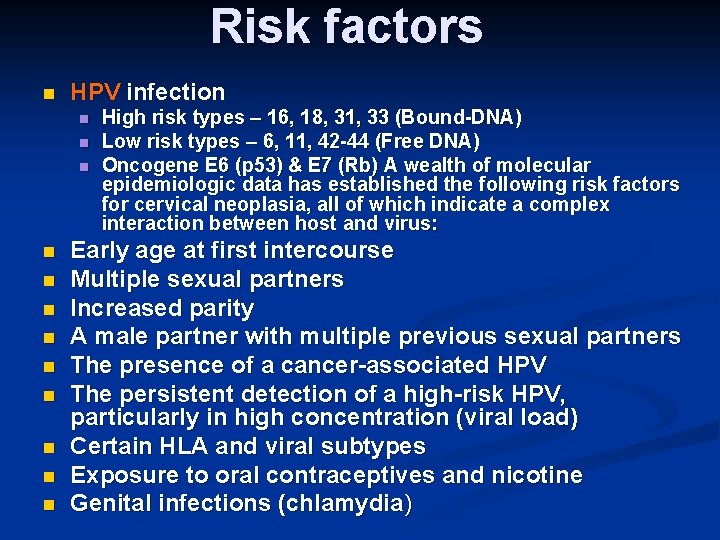
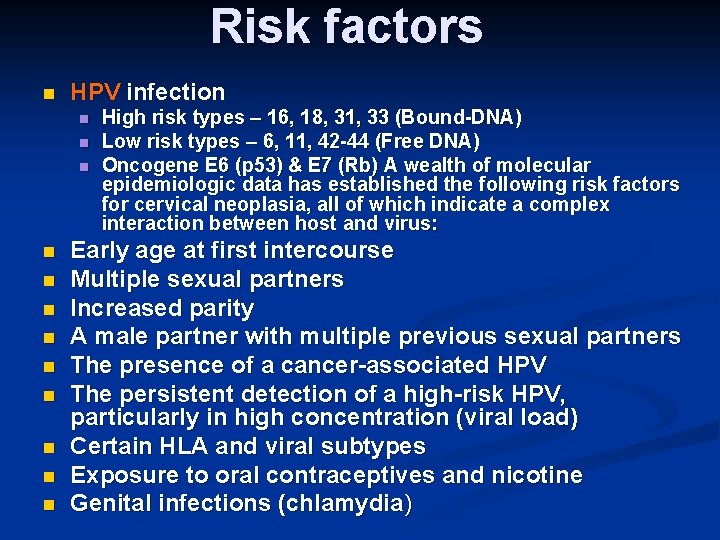
Risk factors n HPV infection n n n High risk types – 16, 18, 31, 33 (Bound-DNA) Low risk types – 6, 11, 42 -44 (Free DNA) Oncogene E 6 (p 53) & E 7 (Rb) A wealth of molecular epidemiologic data has established the following risk factors for cervical neoplasia, all of which indicate a complex interaction between host and virus: Early age at first intercourse Multiple sexual partners Increased parity A male partner with multiple previous sexual partners The presence of a cancer-associated HPV The persistent detection of a high-risk HPV, particularly in high concentration (viral load) Certain HLA and viral subtypes Exposure to oral contraceptives and nicotine Genital infections (chlamydia)
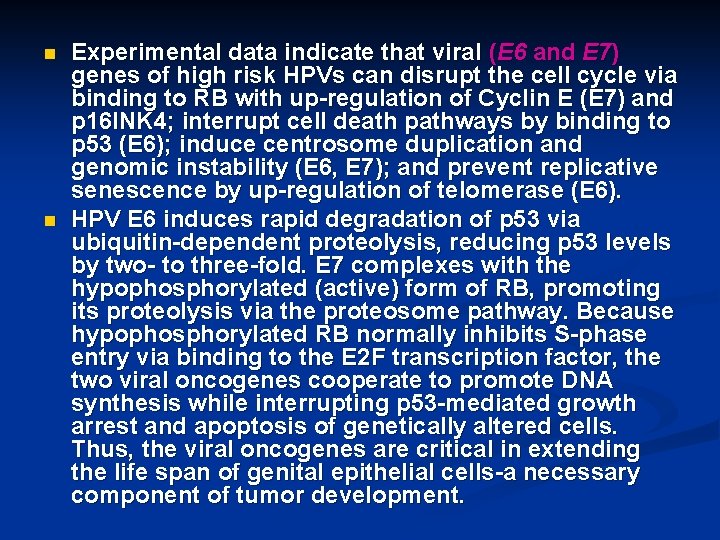
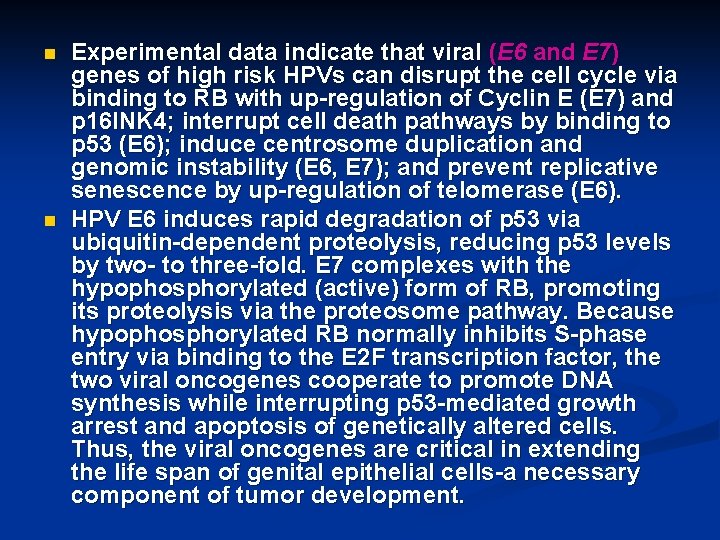
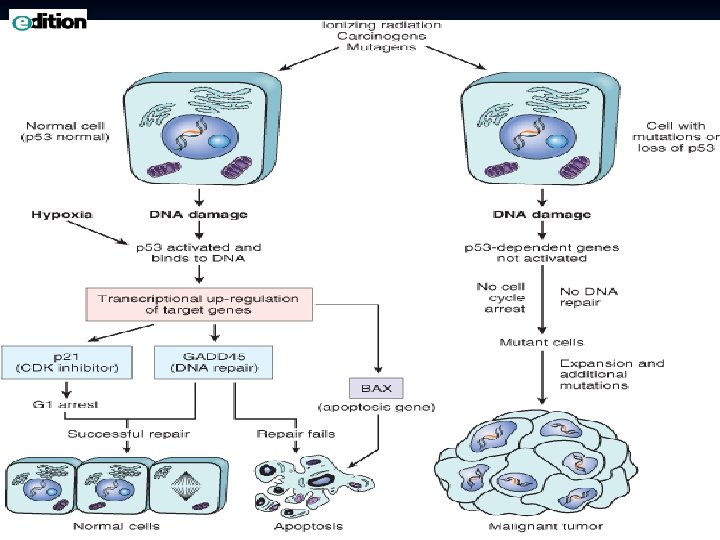
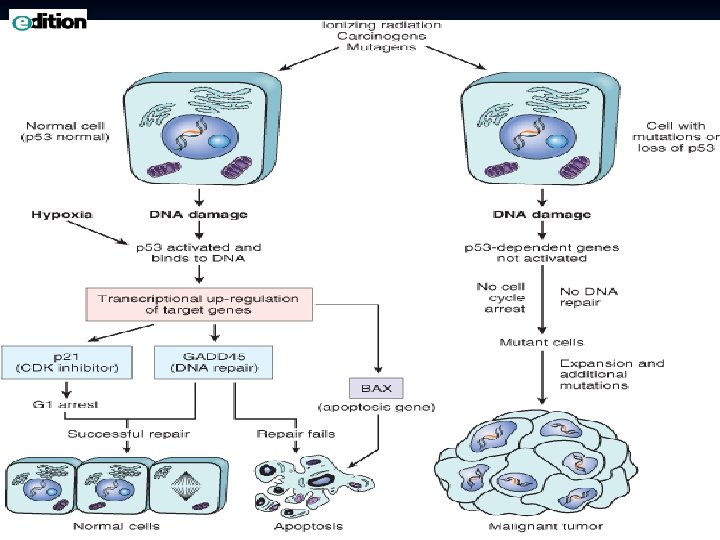
n n Experimental data indicate that viral (E 6 and E 7) genes of high risk HPVs can disrupt the cell cycle via binding to RB with up-regulation of Cyclin E (E 7) and p 16 INK 4; interrupt cell death pathways by binding to p 53 (E 6); induce centrosome duplication and genomic instability (E 6, E 7); and prevent replicative senescence by up-regulation of telomerase (E 6). HPV E 6 induces rapid degradation of p 53 via ubiquitin-dependent proteolysis, reducing p 53 levels by two- to three-fold. E 7 complexes with the hypophosphorylated (active) form of RB, promoting its proteolysis via the proteosome pathway. Because hypophosphorylated RB normally inhibits S-phase entry via binding to the E 2 F transcription factor, the two viral oncogenes cooperate to promote DNA synthesis while interrupting p 53 -mediated growth arrest and apoptosis of genetically altered cells. Thus, the viral oncogenes are critical in extending the life span of genital epithelial cells-a necessary component of tumor development.
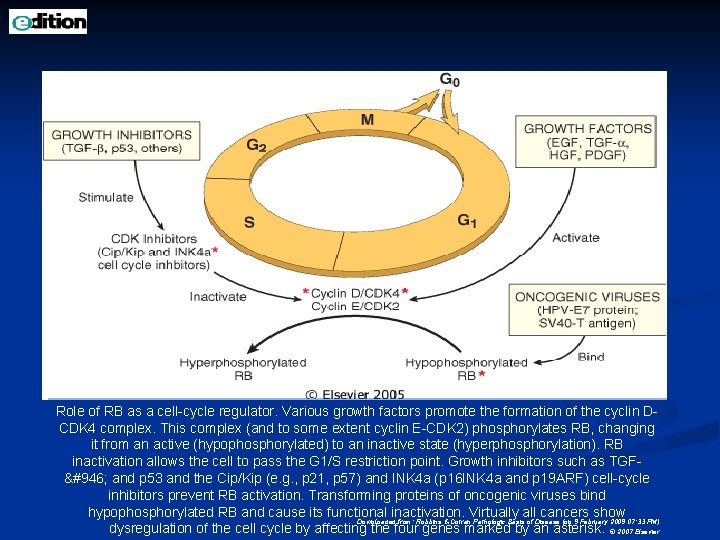
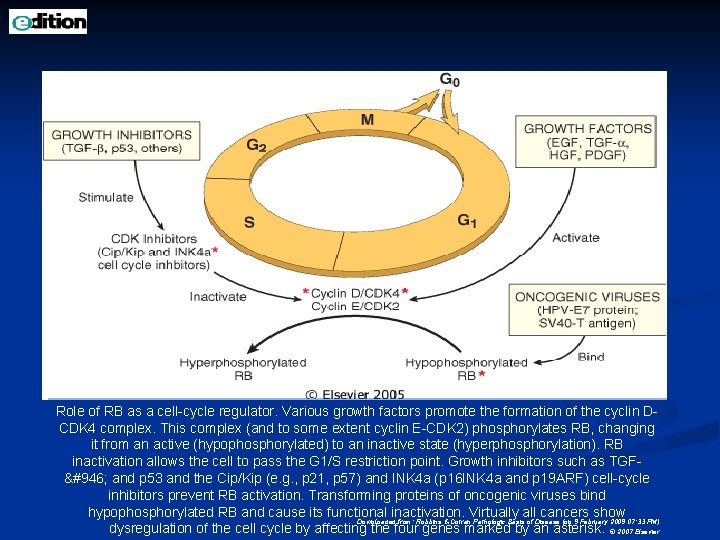
Role of RB as a cell-cycle regulator. Various growth factors promote the formation of the cyclin DCDK 4 complex. This complex (and to some extent cyclin E-CDK 2) phosphorylates RB, changing it from an active (hypophosphorylated) to an inactive state (hyperphosphorylation). RB inactivation allows the cell to pass the G 1/S restriction point. Growth inhibitors such as TGFβ and p 53 and the Cip/Kip (e. g. , p 21, p 57) and INK 4 a (p 16 INK 4 a and p 19 ARF) cell-cycle inhibitors prevent RB activation. Transforming proteins of oncogenic viruses bind hypophosphorylated RB and cause its functional inactivation. Virtually all cancers show Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 9 February 2009 07: 33 PM) dysregulation of the cell cycle by affecting the four genes marked by an asterisk. © 2007 Elsevier
Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 9 February 2009 07: 33 PM) © 2007 Elsevier
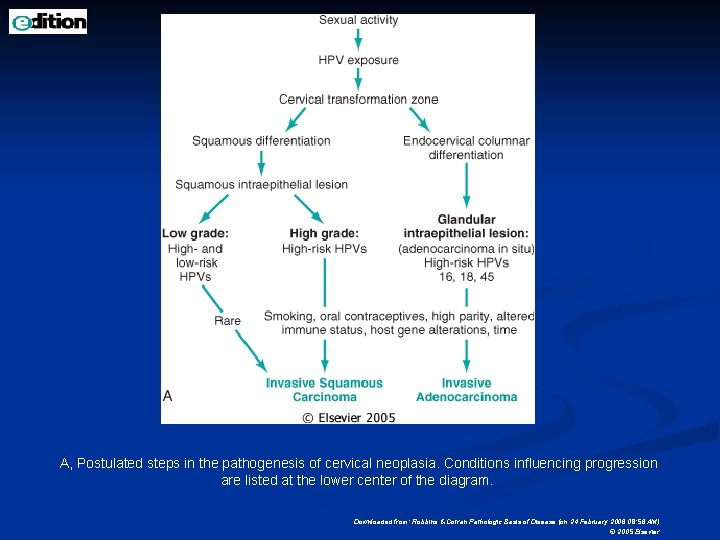
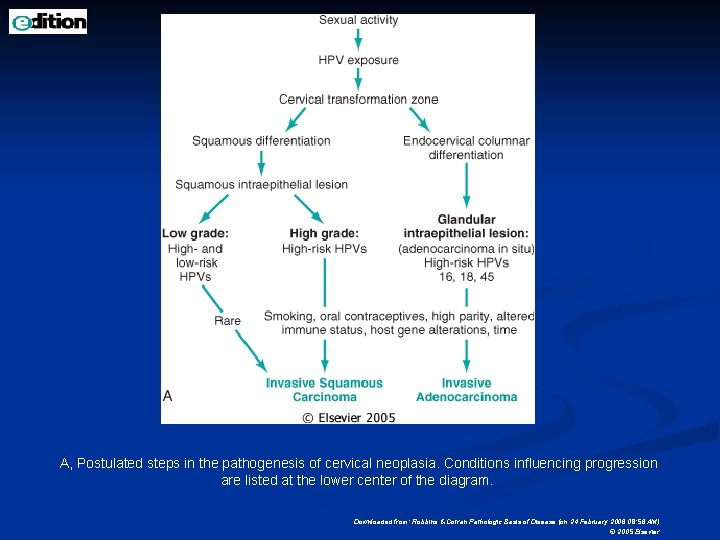
A, Postulated steps in the pathogenesis of cervical neoplasia. Conditions influencing progression are listed at the lower center of the diagram. Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
n n The physical state of the virus differs in different lesions, being integrated into the host DNA in cancers, and present as free (episomal) viral DNA in condylomata and most precancerous lesions. Certain chromosome abnormalities, including deletions at 3 p and amplifications of 3 q, have been associated with cancers containing specific (HPV-16) papillomaviruses Most compelling, recent data indicate that vaccines directed against papillomaviruses can prevent infection and the development of precancerous disorders However, the evidence does not implicate HPV as the only factor.
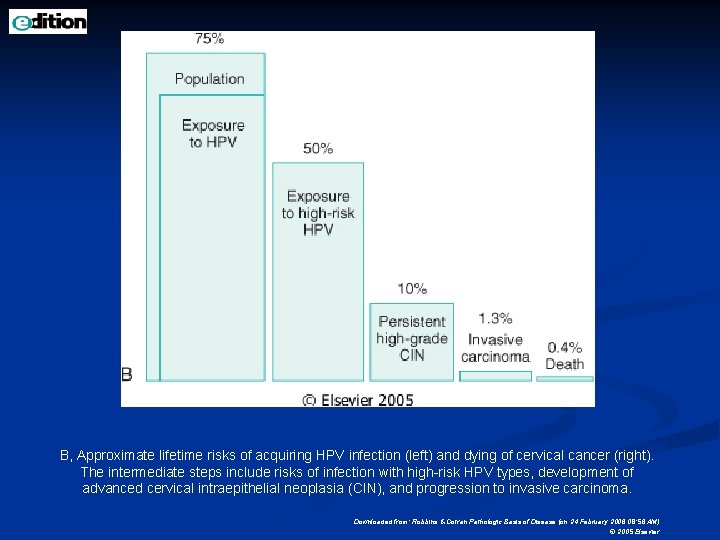
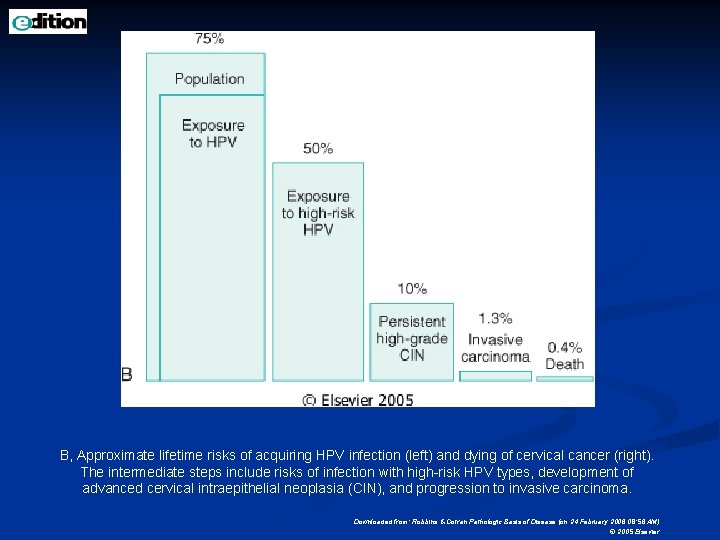
B, Approximate lifetime risks of acquiring HPV infection (left) and dying of cervical cancer (right). The intermediate steps include risks of infection with high-risk HPV types, development of advanced cervical intraepithelial neoplasia (CIN), and progression to invasive carcinoma. Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
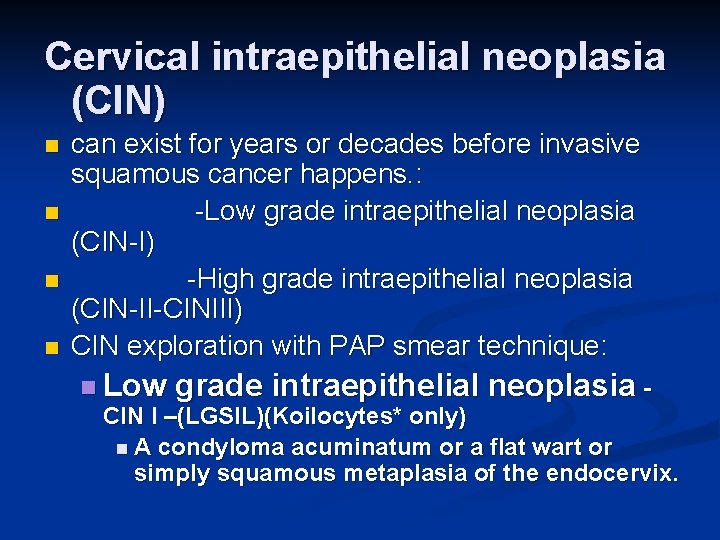
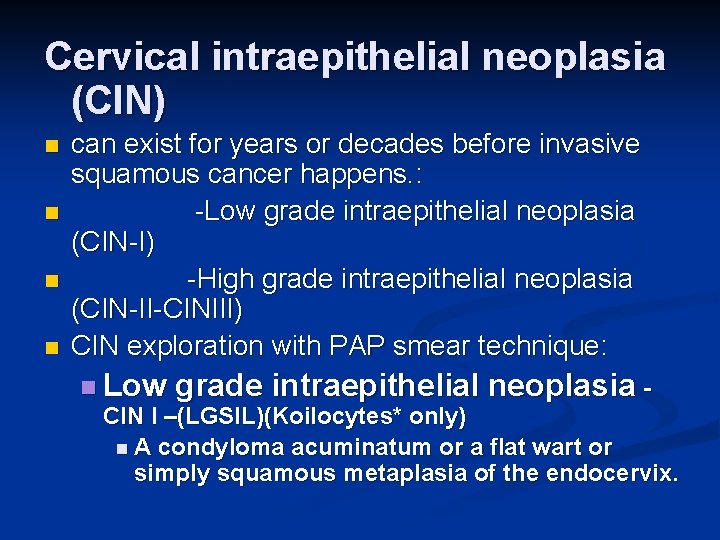
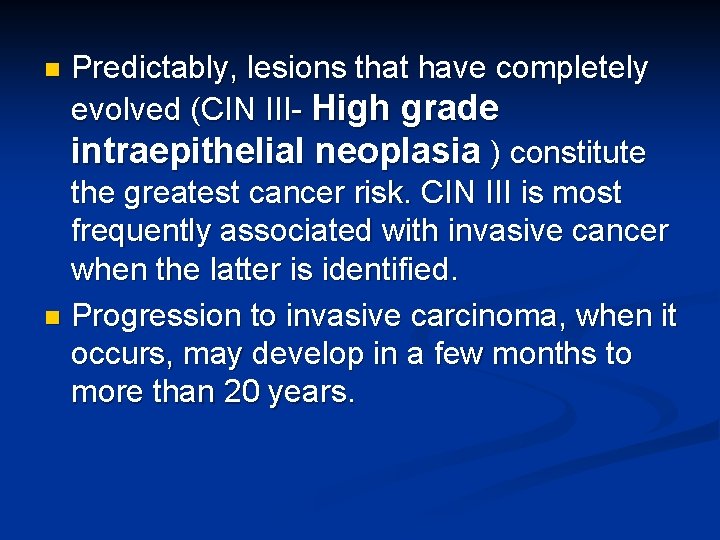
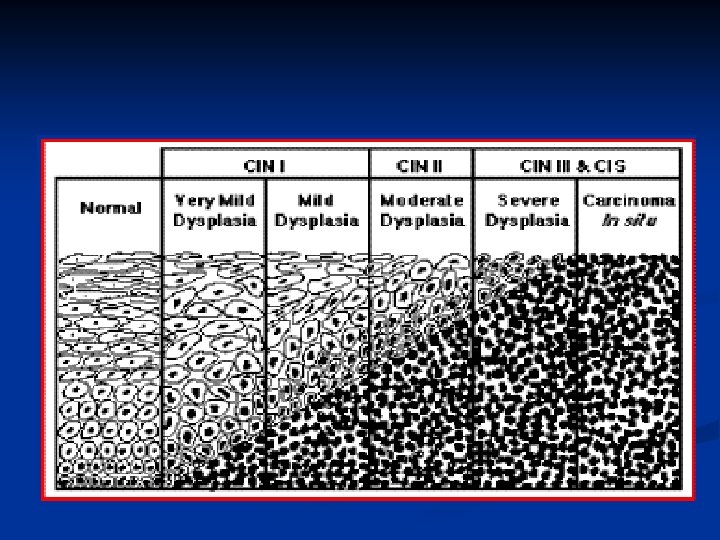
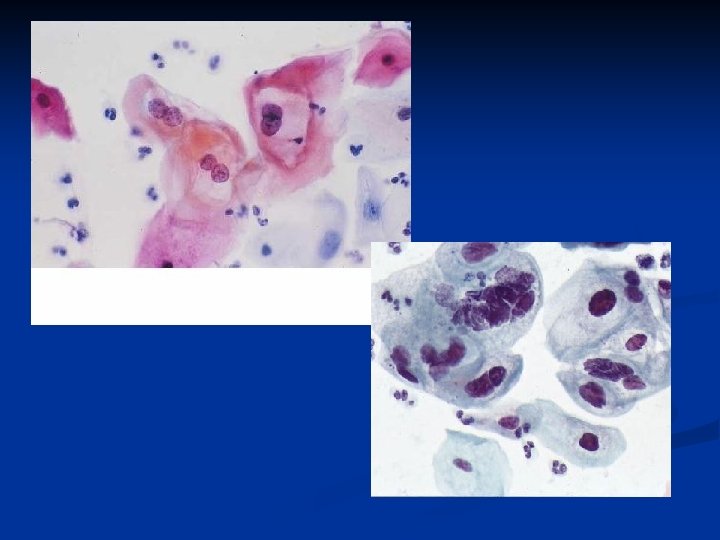
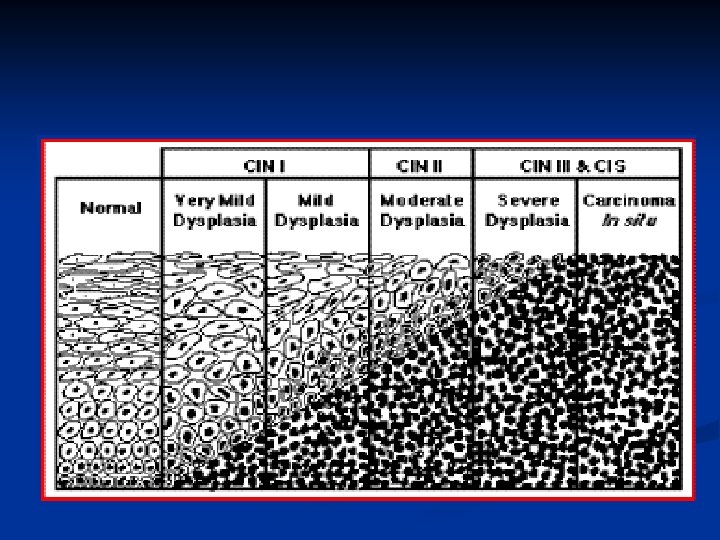
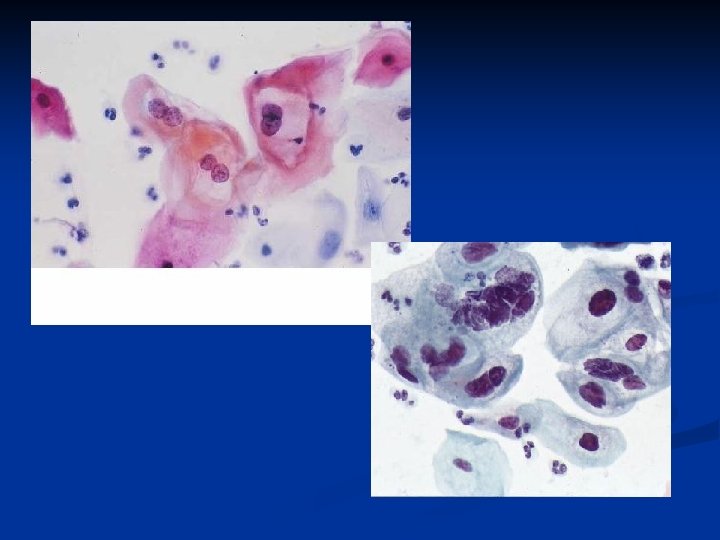
Cervical intraepithelial neoplasia (CIN) n n can exist for years or decades before invasive squamous cancer happens. : -Low grade intraepithelial neoplasia (CIN-I) -High grade intraepithelial neoplasia (CIN-II-CINIII) CIN exploration with PAP smear technique: n Low grade intraepithelial neoplasia CIN I –(LGSIL)(Koilocytes* only) n A condyloma acuminatum or a flat wart or simply squamous metaplasia of the endocervix.
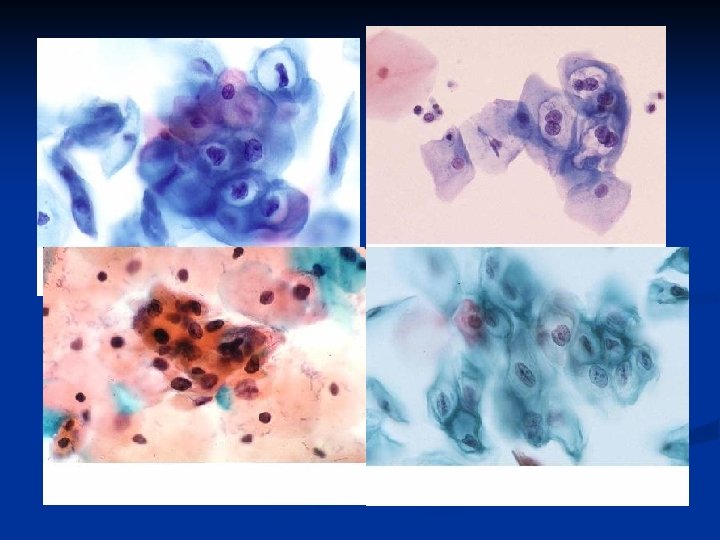
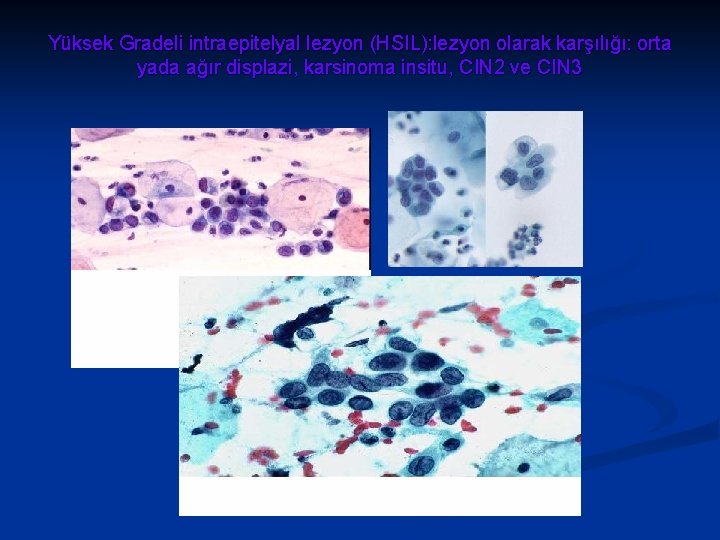
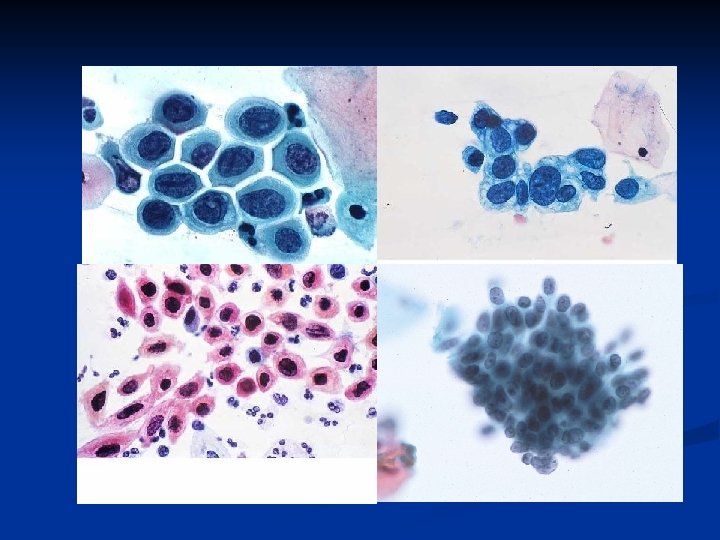
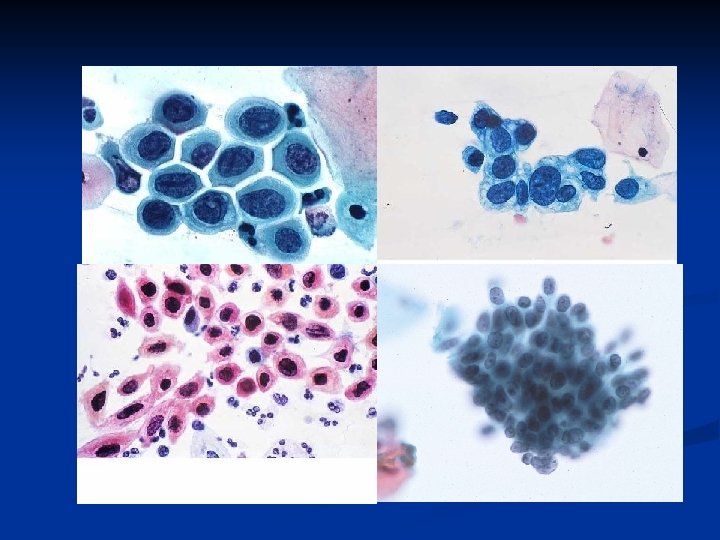
n -High grade intraepithelial neoplasia- (HGSIL) n CIN II: n Plenty of atypical cells in the lower portions, normal maturation toward the surface (The old "moderate dysplasia" and "severe dysplasia"). n CIN III: n The cells no longer mature as they reach the surface (The old "carcinoma in situ"). Koilocyte: A squamous cell, often binucleated, showing a perinuclear halo; characteristic of condyloma acuminatum.
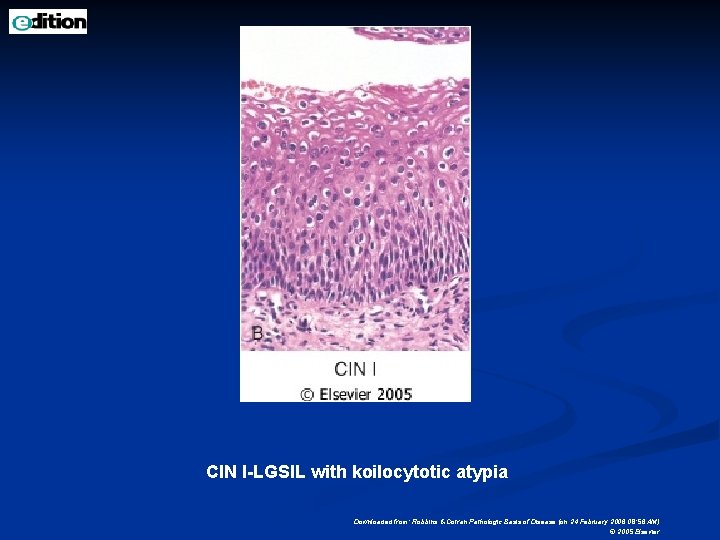
Morphology n n On the extreme low end of the spectrum are lesions that are often indistinguishable histologically from condylomata acuminata and may be either raised (acuminatum) or macular (flat condyloma) in appearance Such changes fall within the range of CIN I- Low grade intraepithelial neoplasia -. CIN I often contains abundant papillomavirus nucleic acids. Raised lesions (acuminatum) often contain low-risk HPVs. Flat CIN usually contain high-risk HPVs.
These lesions typically exhibit nuclear enlargement and hyperchromasia in the superficial epithelial cells, signifying the effects of active viral replication in the maturing cells (viral cytopathic effect). n The nuclear changes may be accompanied by cytoplasmic halos (koilocytotic atypia) with few alterations in the lower epithelial cells. n
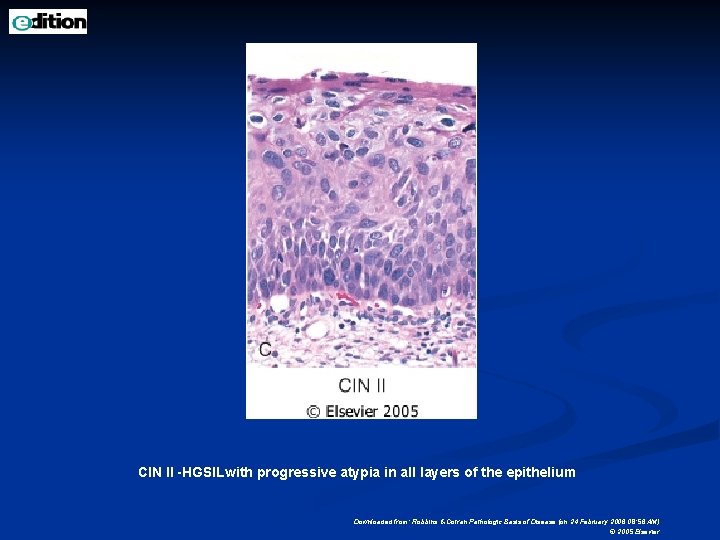
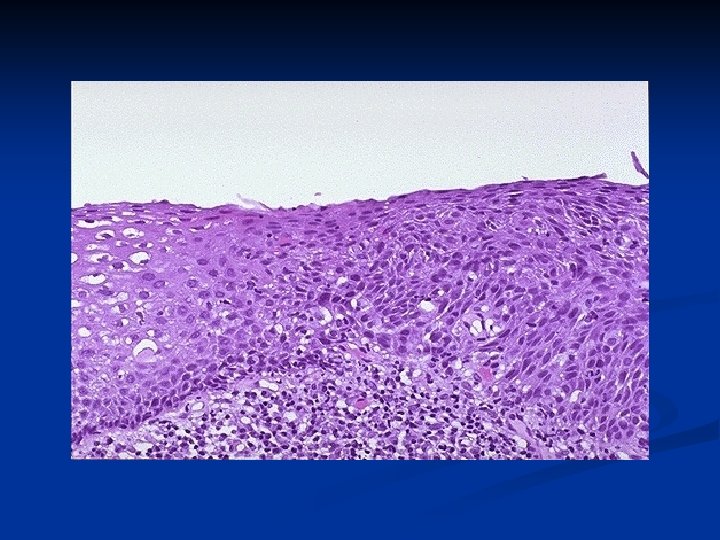
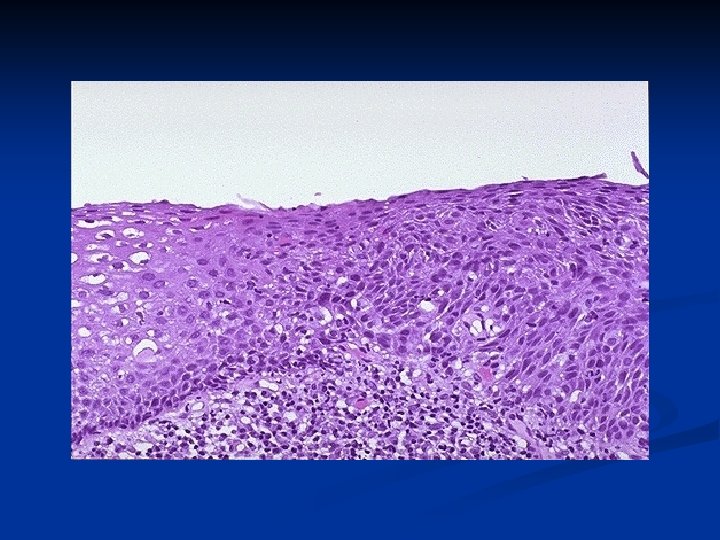
n n The next change in the spectrum consists of the appearance of atypical cells in the lower layers of the squamous epithelium but nonetheless with persistent (but abnormal) differentiation toward the prickle and keratinizing cell layers. The atypical cells show changes in nucleocytoplasmic ratio; variation in nuclear size; loss of polarity; increased mitotic figures, including abnormal mitoses; and hyperchromasia-in other words, they take on some of the characteristics of malignant cells. These lesions fall within the range of CIN II- High grade intraepithelial neoplasia n These features have been associated with aneuploid cell populations and correlate strongly with high-risk HPV types.
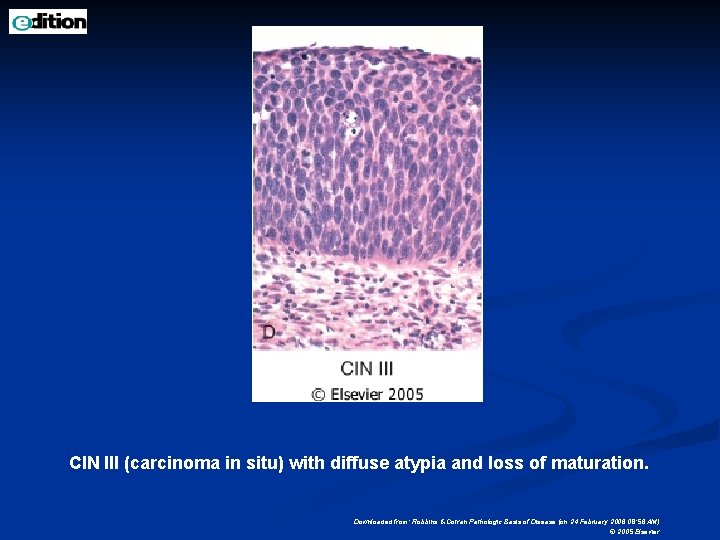
n n Presumably they reflect early changes in the replicating (basal/parabasal) cell population associated with the effects of the E 6/E 7 oncogenes on cell cycle and genomic stability. These include cell cycle disregulation and upregulation of p 16 INK 4 Increased expression of p 16, a cyclin-dependent kinase inhibitor, is possibly a compensatory response to cell disturbances brought on by the viral oncogenes. As the lesion evolves, there is progressive loss of differentiation accompanied by greater atypia in more layers of the epithelium, until it is totally replaced by immature atypical cells, exhibiting no surface differentiation (CIN III)- High grade intraepithelial
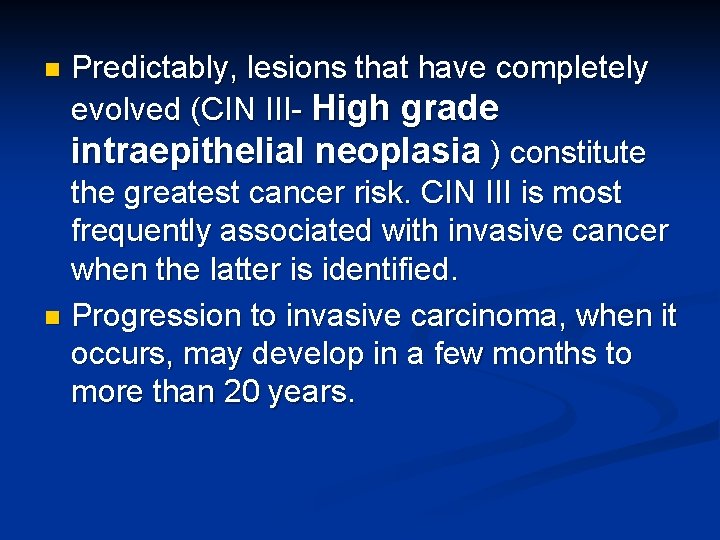
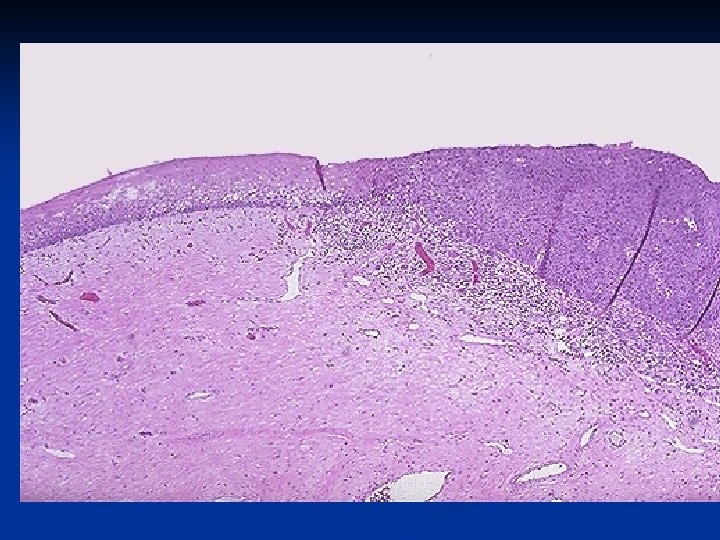
Predictably, lesions that have completely evolved (CIN III- High grade intraepithelial neoplasia ) constitute the greatest cancer risk. CIN III is most frequently associated with invasive cancer when the latter is identified. n Progression to invasive carcinoma, when it occurs, may develop in a few months to more than 20 years. n
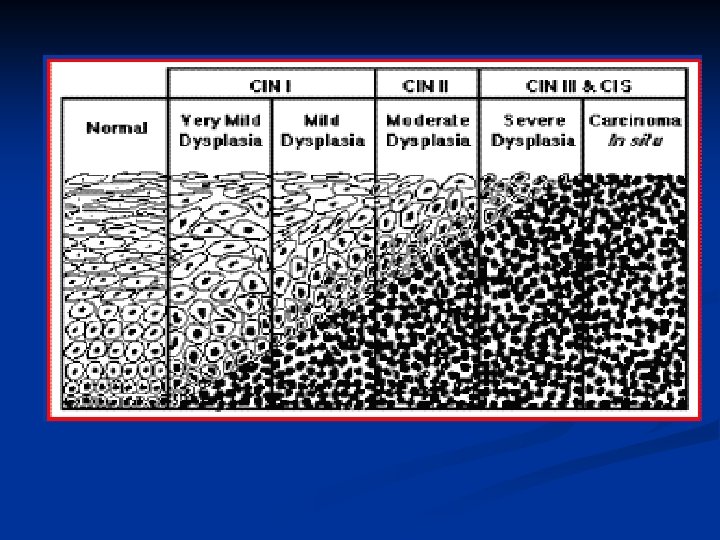
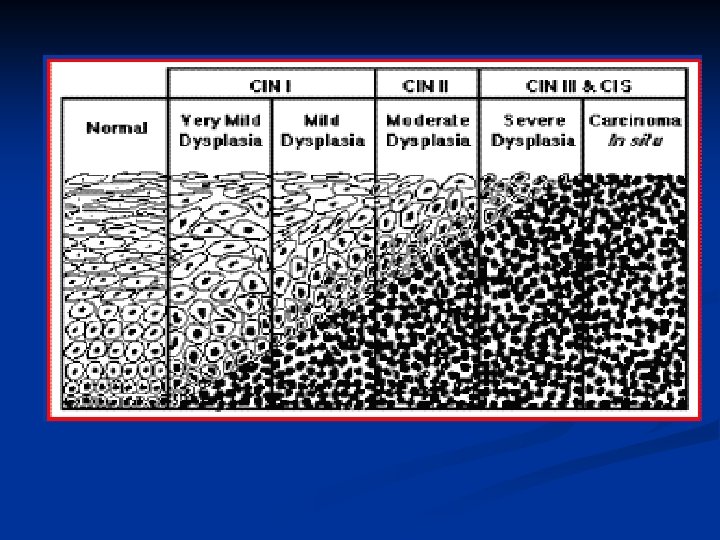
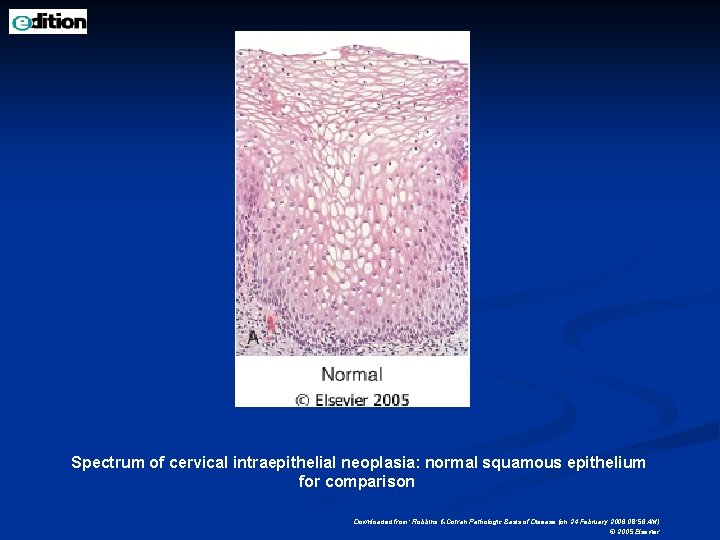
Spectrum of cervical intraepithelial neoplasia: normal squamous epithelium for comparison Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
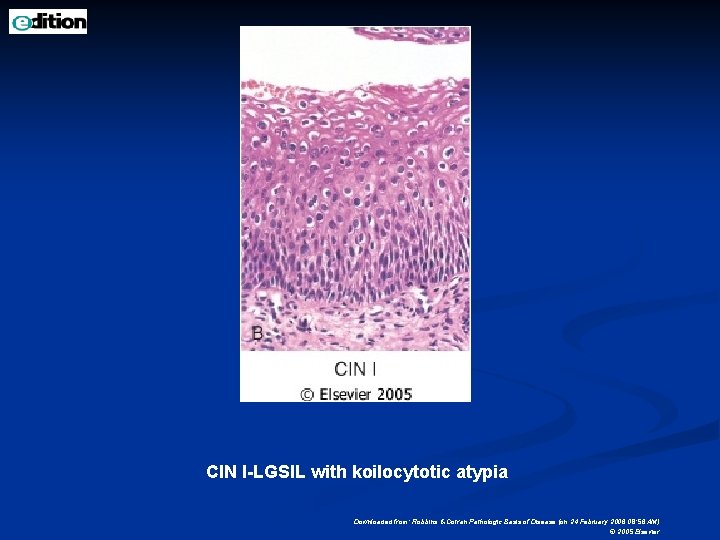
CIN I-LGSIL with koilocytotic atypia Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
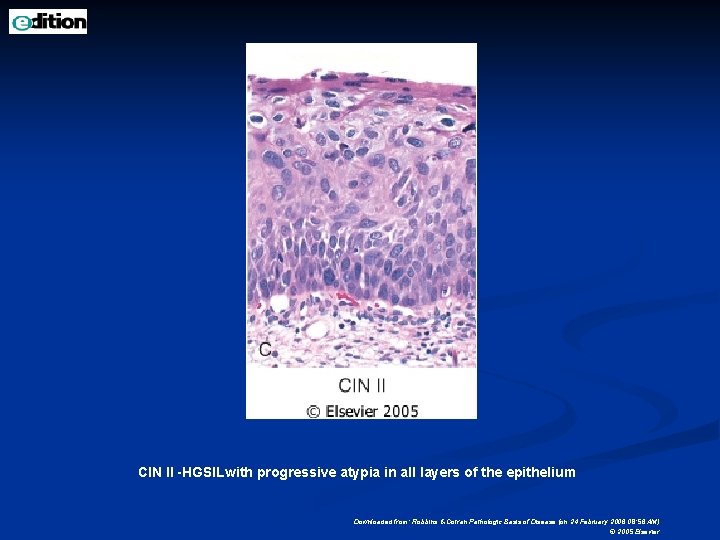
CIN II -HGSILwith progressive atypia in all layers of the epithelium Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
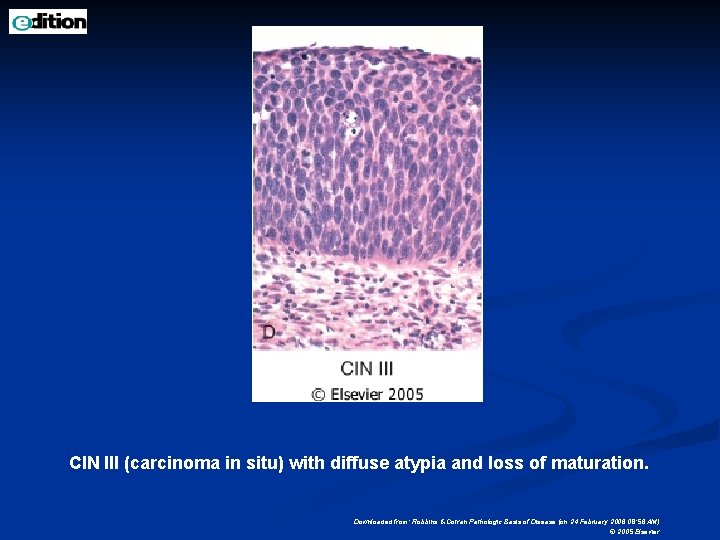
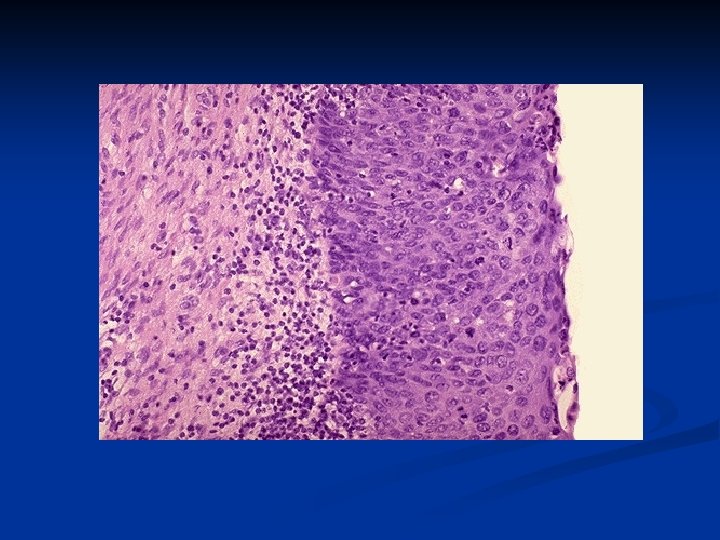
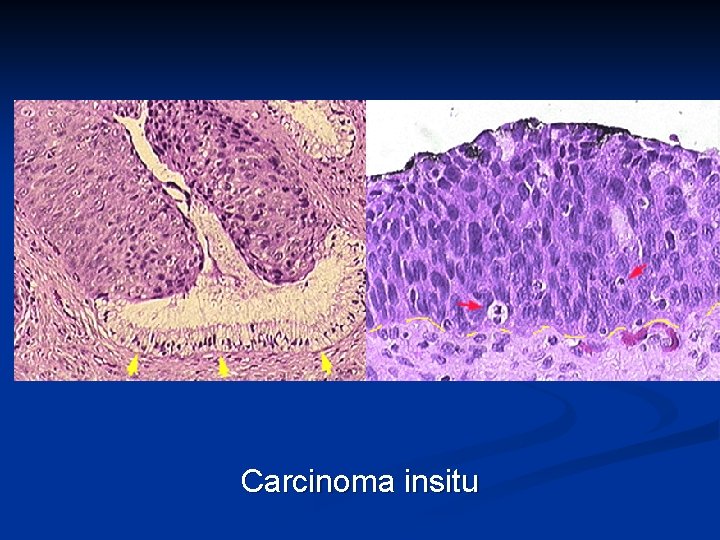
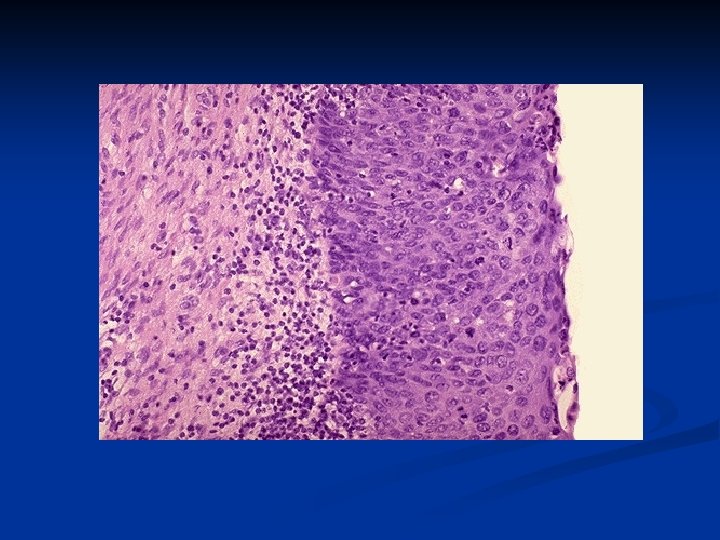
CIN III (carcinoma in situ) with diffuse atypia and loss of maturation. Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
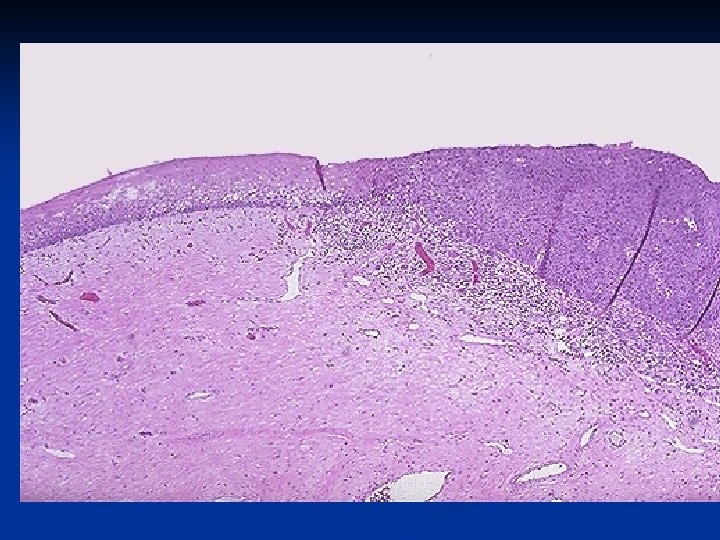
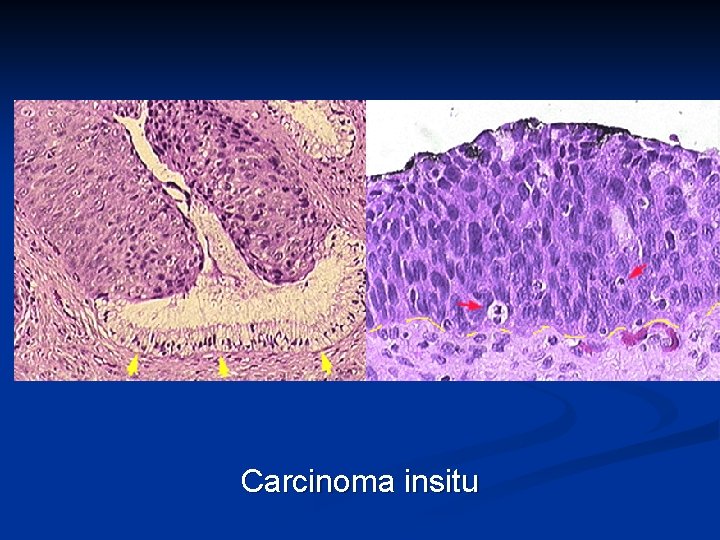
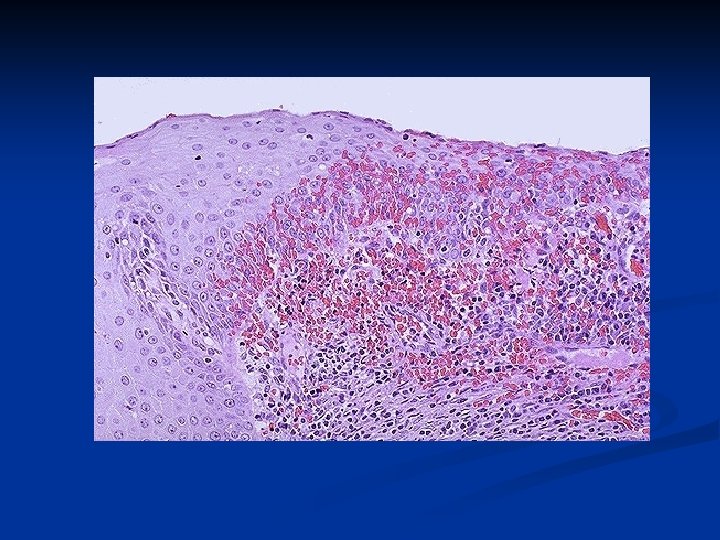
Carcinoma insitu
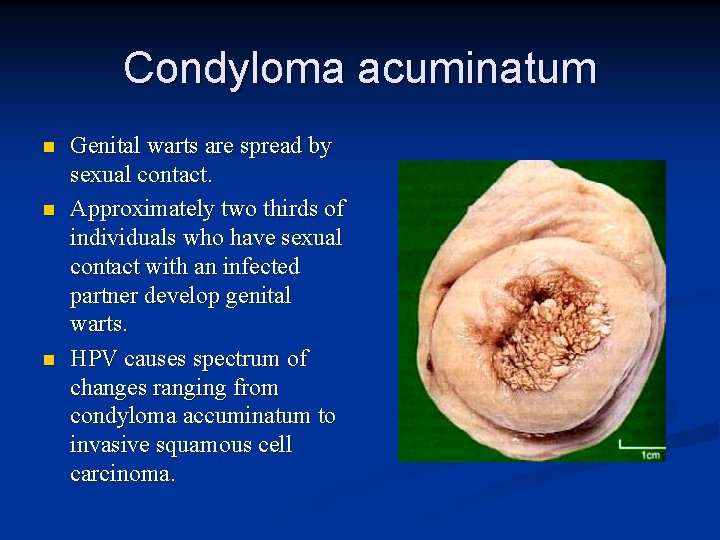
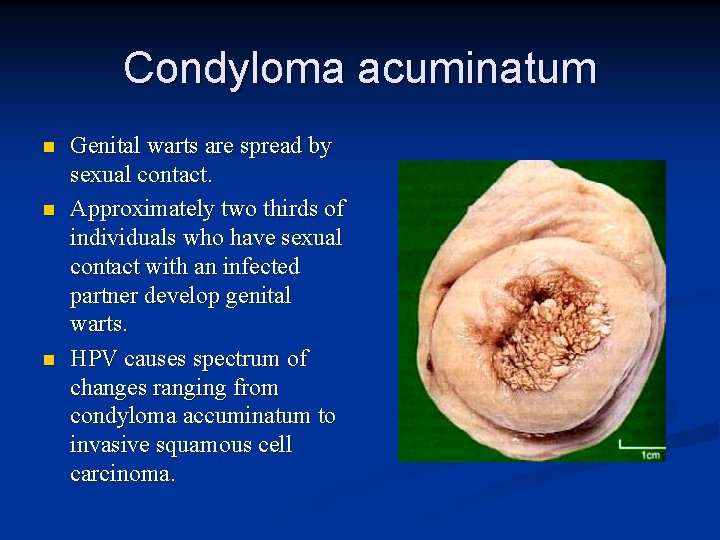
Condyloma acuminatum n n n Genital warts are spread by sexual contact. Approximately two thirds of individuals who have sexual contact with an infected partner develop genital warts. HPV causes spectrum of changes ranging from condyloma accuminatum to invasive squamous cell carcinoma.
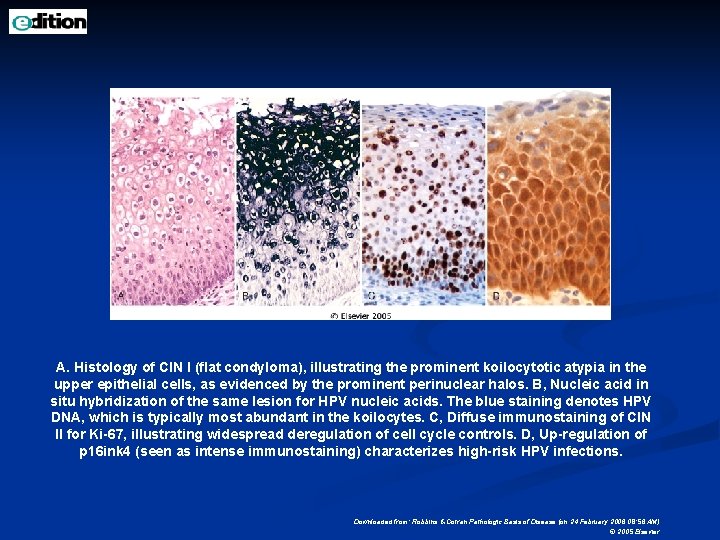
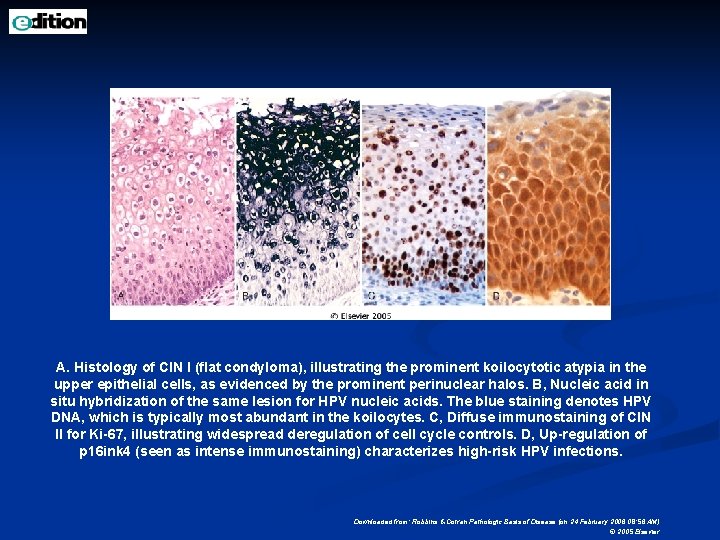
A. Histology of CIN I (flat condyloma), illustrating the prominent koilocytotic atypia in the upper epithelial cells, as evidenced by the prominent perinuclear halos. B, Nucleic acid in situ hybridization of the same lesion for HPV nucleic acids. The blue staining denotes HPV DNA, which is typically most abundant in the koilocytes. C, Diffuse immunostaining of CIN II for Ki-67, illustrating widespread deregulation of cell cycle controls. D, Up-regulation of p 16 ink 4 (seen as intense immunostaining) characterizes high-risk HPV infections. Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
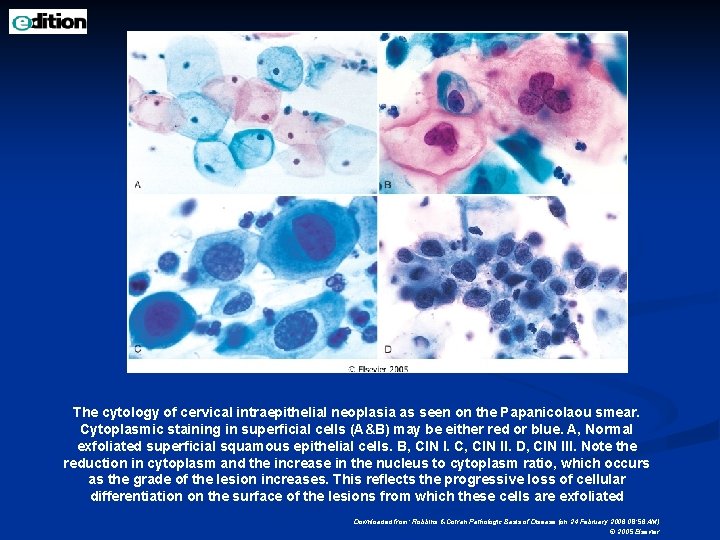
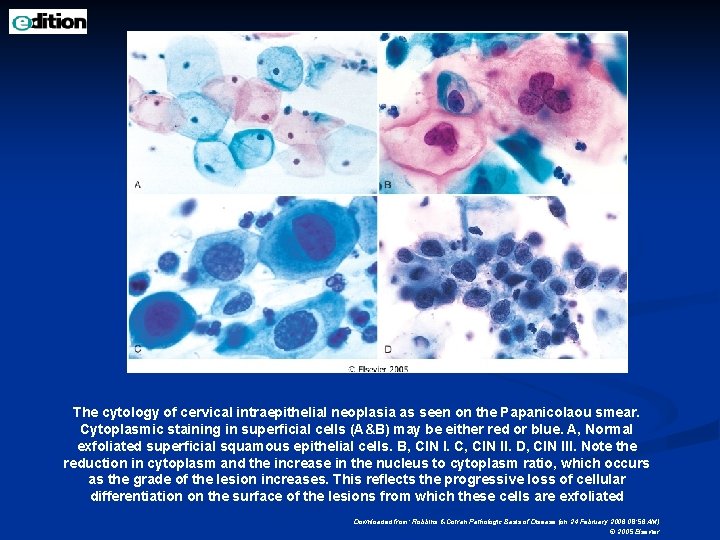
The cytology of cervical intraepithelial neoplasia as seen on the Papanicolaou smear. Cytoplasmic staining in superficial cells (A&B) may be either red or blue. A, Normal exfoliated superficial squamous epithelial cells. B, CIN I. C, CIN II. D, CIN III. Note the reduction in cytoplasm and the increase in the nucleus to cytoplasm ratio, which occurs as the grade of the lesion increases. This reflects the progressive loss of cellular differentiation on the surface of the lesions from which these cells are exfoliated Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
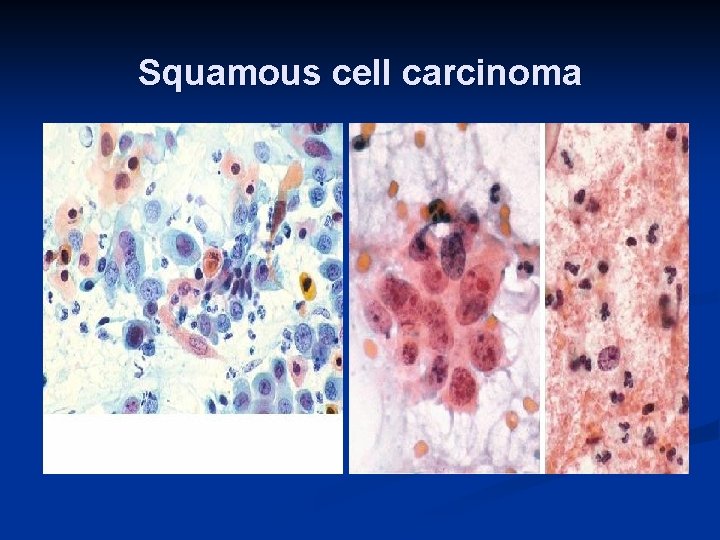
SQUAMOUS CELL CARCINOMA n n n Squamous cell carcinoma may occur at any age from the second decade of life to senility. The peak incidence is occurring at an increasingly younger age: 40 to 45 years for invasive cancer and about 30 years for highgrade precancers. This represents the combination of earlier onset of sexual activity (i. e. , earlier acquisition of HPV infection) and active Papanicolaou smear screening programs in the United States, which detect either cancers or precancerous lesions at an earlier point in life.
Clinical features n n n n Asymptomatic – Abnormal cells in smears Vaginal Bleeding 80% Squamous Ca, 20% other. Early diagnosis by cytological PAP test. Adenocarcinoma, Adenosquamous, Clearcell carcinoma etc. 40 -50 peak age. Treatments – Cone biopsy, hysterectomy 5 year survival n Stage 1 ->80%, Stage 2– 75%, Stage 3 -35% & 10 -15% with Stage 4 disease.
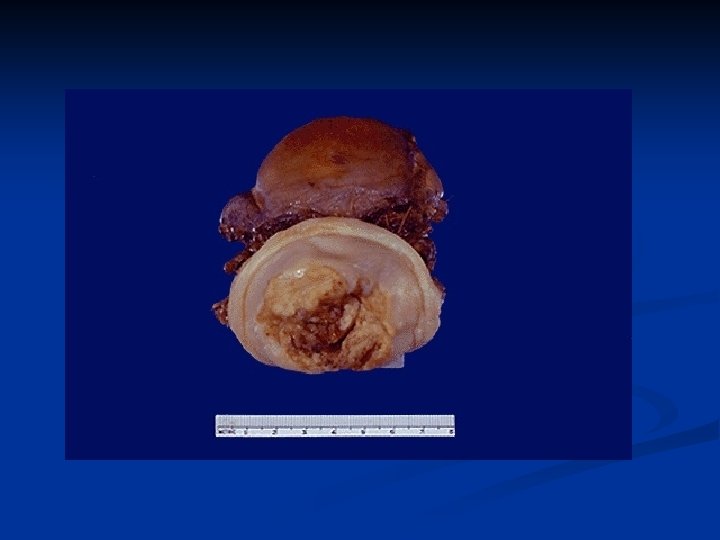
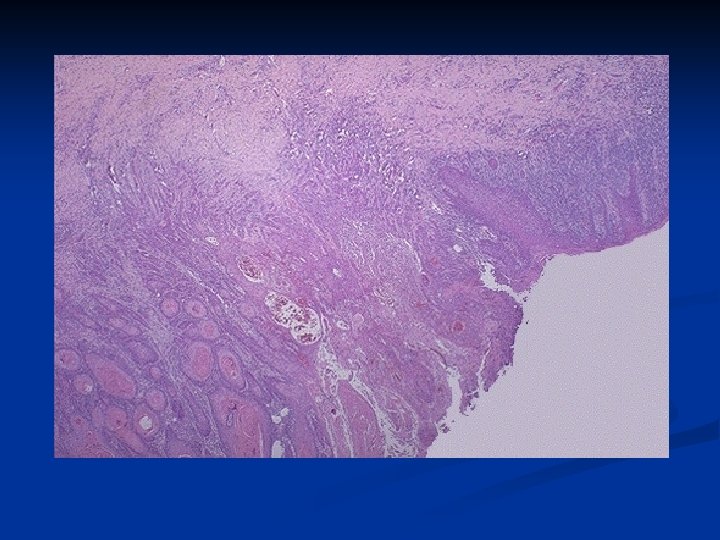
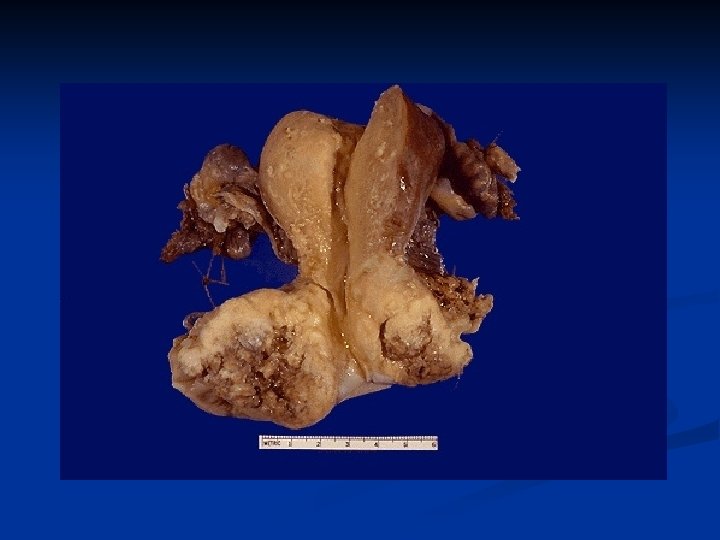
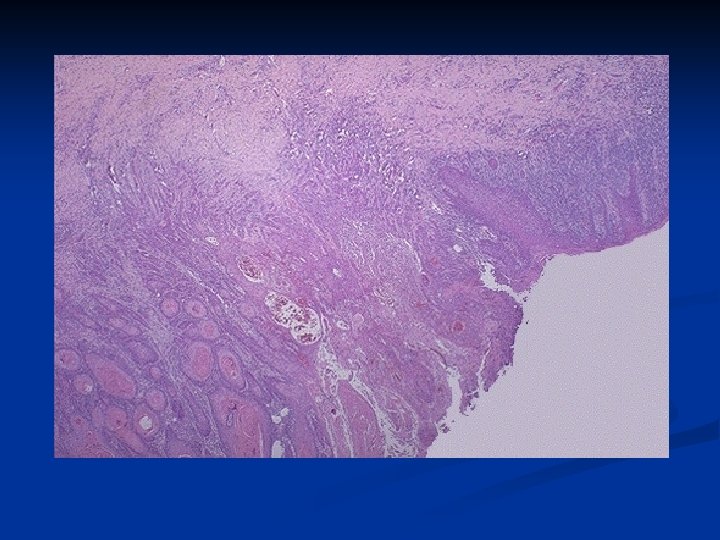
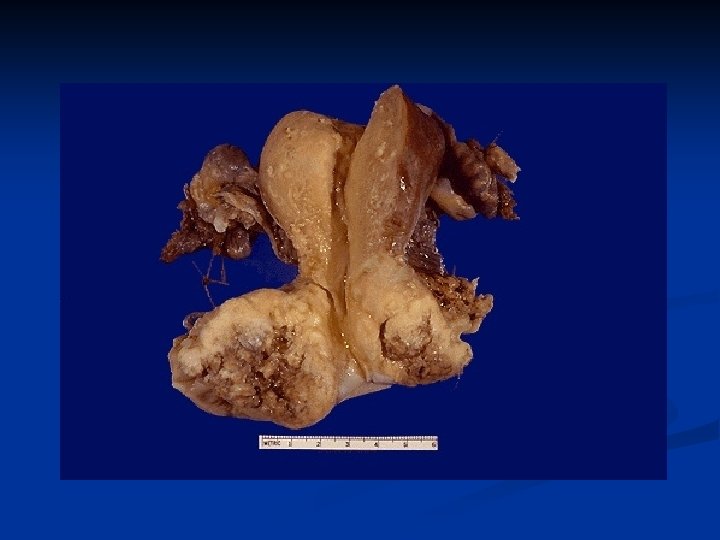
n Morphology n Invasive cervical carcinoma manifests in three somewhat distinctive patterns: n 1 -Fungating (or exophytic), n 2 -Ulcerating n 3 -Infiltrative cancers. n When obvious to the naked eye, the most common variant is the fungating tumor, which produces an obviously neoplastic
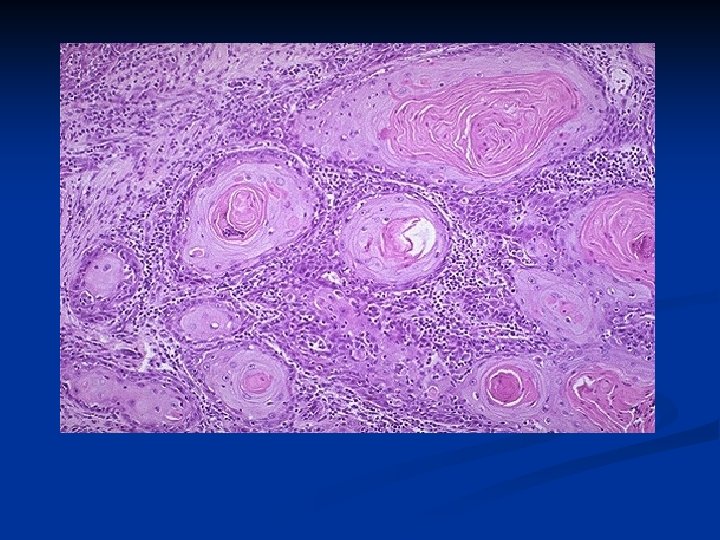
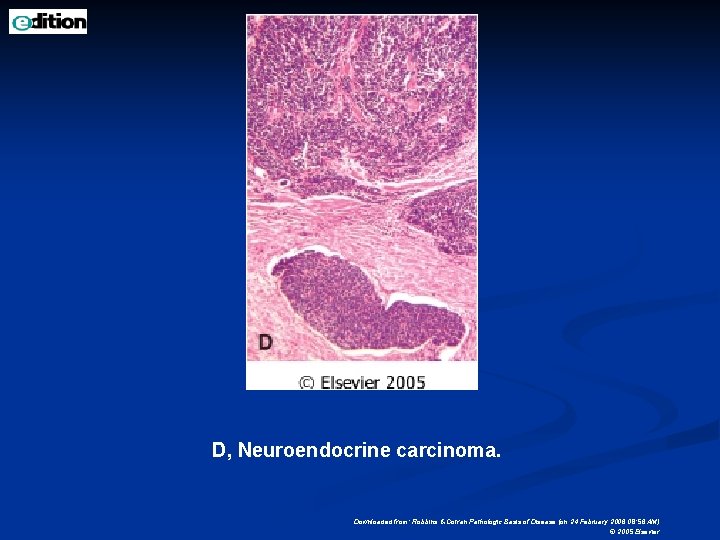
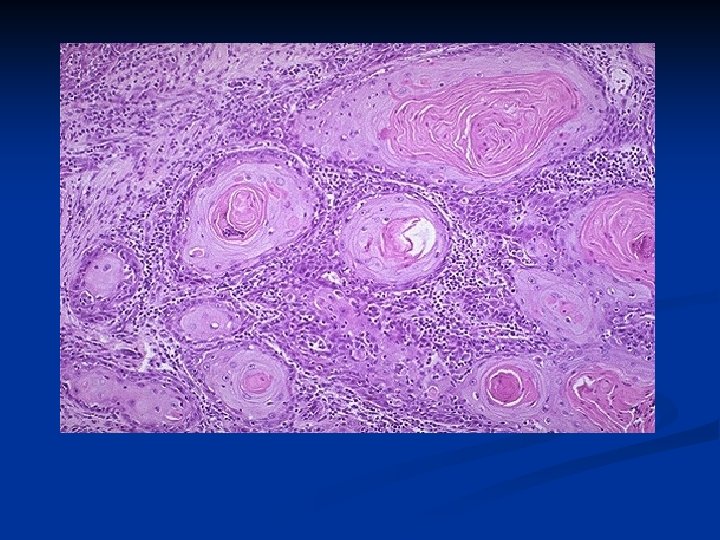
n n n On histologic examination: about 95% of squamous carcinomas are composed of relatively large cells, either keratinizing (welldifferentiated) or nonkeratinizing (moderately differentiated) patterns. A small subset of tumors (less than 5%) are poorly differentiated small cell squamous or, more rarely, small cell undifferentiated carcinomas (neuroendocrine or oat cell carcinomas). The latter closely resemble oat cell carcinomas of the lung and have an unusually poor prognosis owing to early spread by lymphatics and systemic spread. These tumors are also frequently associated with a specific high-risk HPV, type 18.
Spreading n Direct: Down – Vagina, Labia n Lateral – adnexa, ureter, ovary, Pelvic wall n Anterior – bladder n Posterior – Rectum n n Lymphatic: n n Paracervical, Obturator, Int & Ext iliac, Sacral, Common iliac, Aortic. Blood: Liver, lungs etc.
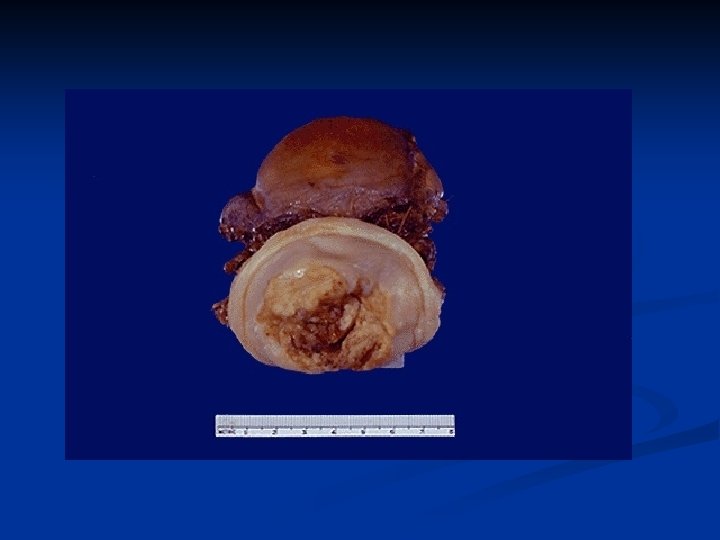

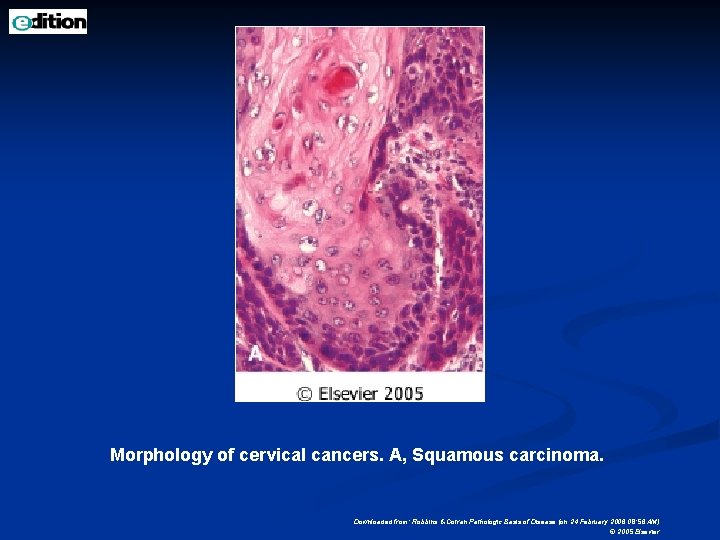
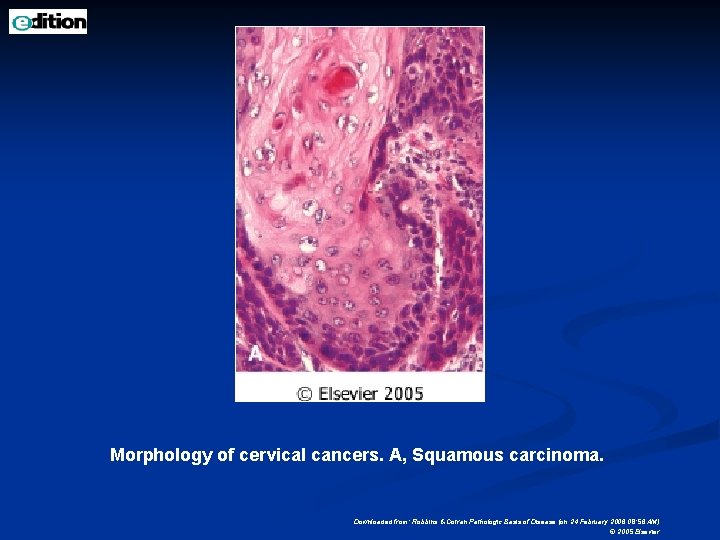
Morphology of cervical cancers. A, Squamous carcinoma. Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
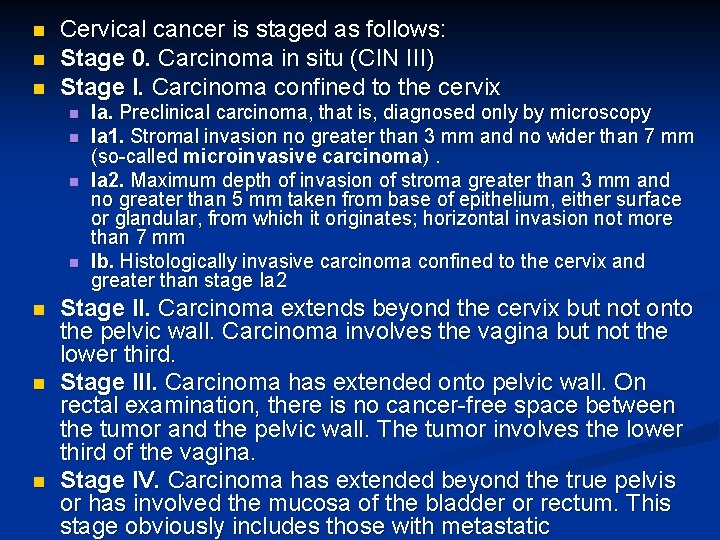
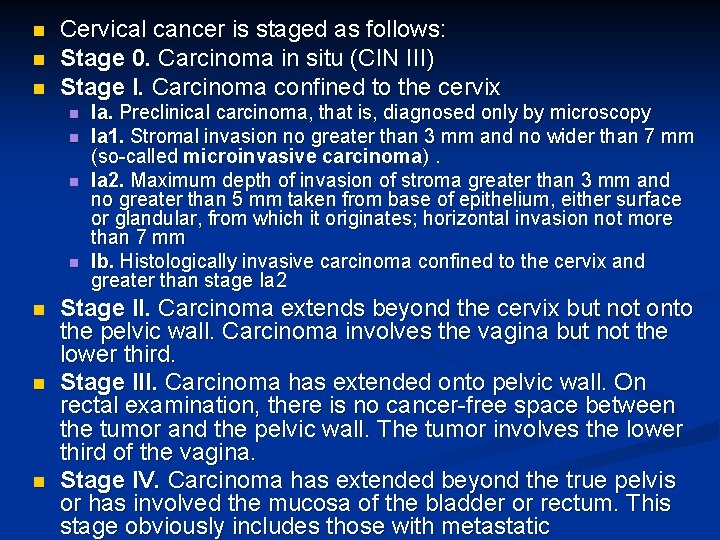
n n n Cervical cancer is staged as follows: Stage 0. Carcinoma in situ (CIN III) Stage I. Carcinoma confined to the cervix n n n n Ia. Preclinical carcinoma, that is, diagnosed only by microscopy Ia 1. Stromal invasion no greater than 3 mm and no wider than 7 mm (so-called microinvasive carcinoma). Ia 2. Maximum depth of invasion of stroma greater than 3 mm and no greater than 5 mm taken from base of epithelium, either surface or glandular, from which it originates; horizontal invasion not more than 7 mm Ib. Histologically invasive carcinoma confined to the cervix and greater than stage Ia 2 Stage II. Carcinoma extends beyond the cervix but not onto the pelvic wall. Carcinoma involves the vagina but not the lower third. Stage III. Carcinoma has extended onto pelvic wall. On rectal examination, there is no cancer-free space between the tumor and the pelvic wall. The tumor involves the lower third of the vagina. Stage IV. Carcinoma has extended beyond the true pelvis or has involved the mucosa of the bladder or rectum. This stage obviously includes those with metastatic


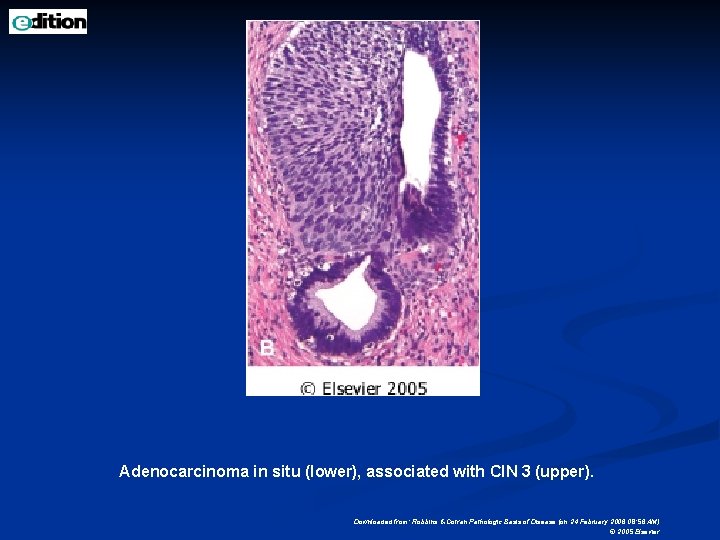
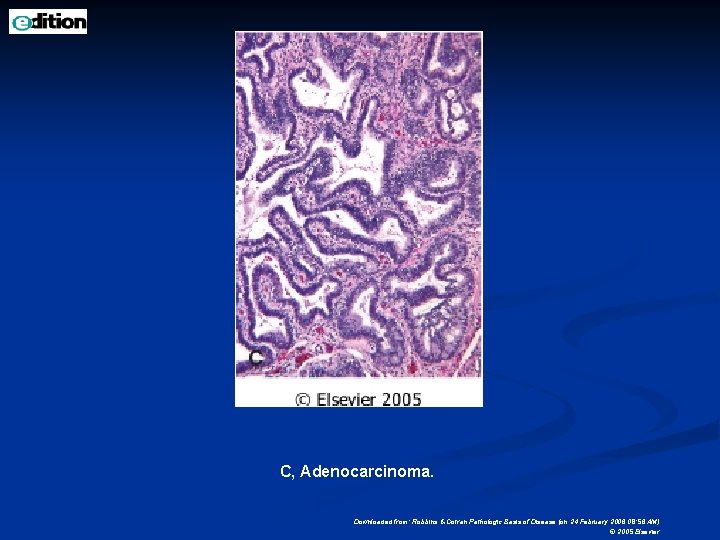
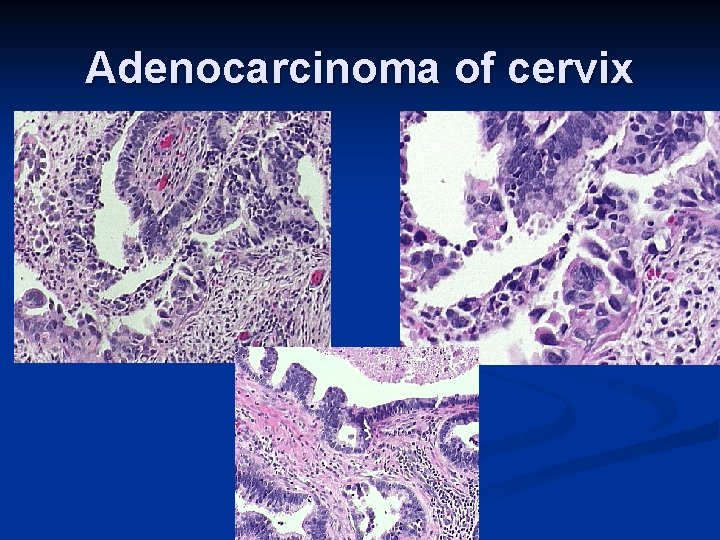
n n n n Ten per cent to 25% of cervical carcinomas are adenocarcinomas, adenosquamous carcinomas, undifferentiated carcinomas, or other rare histologic types. The adenocarcinomas : Arise in the endocervical glands and are often preceded by an intraepithelial glandular neoplasm (precancer) termed adenocarcinoma in situ that is approximately one fifth as common as its squamous counterpart. Once invasion develops, adenocarcinomas appear grossly and behave like the squamous cell lesions, with the exception of association with HPV type 18. The adenosquamous carcinomas : Mixed glandular and squamous patterns and are thought to arise from the multipotent reserve cells in the basal layers of the endocervical epithelium. They tend to have a less favorable prognosis than does squamous cell carcinoma of similar stage. Clear cell adenocarcinomas of the cervix in DESexposed women are similar to those occurring in the vagina, described earlier. Their relationship to
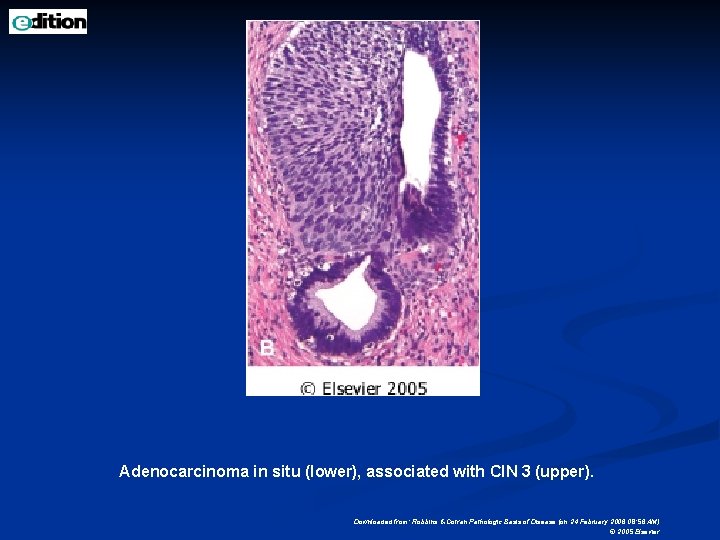
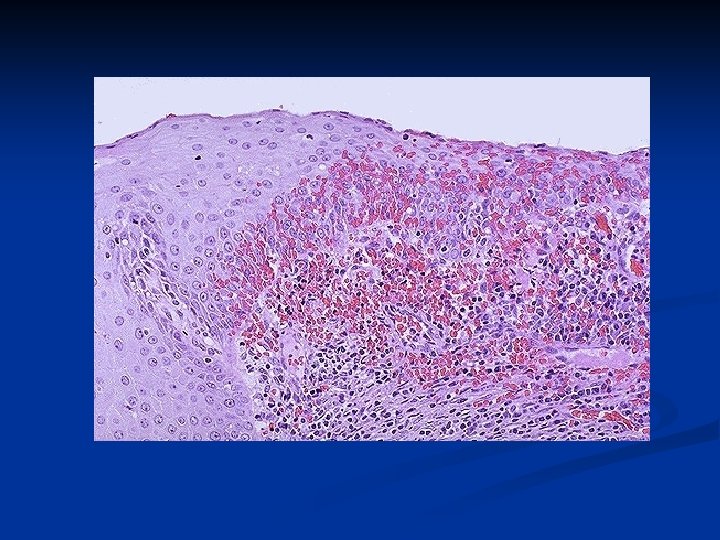
Adenocarcinoma in situ (lower), associated with CIN 3 (upper). Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
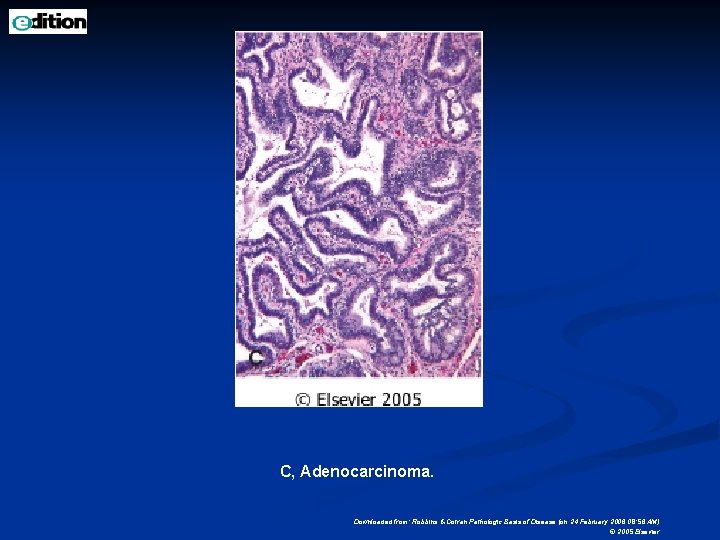
C, Adenocarcinoma. Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
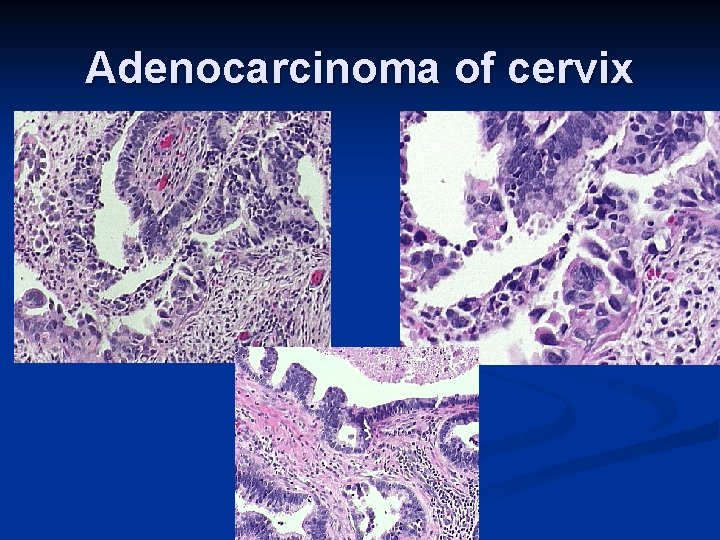
Adenocarcinoma of cervix
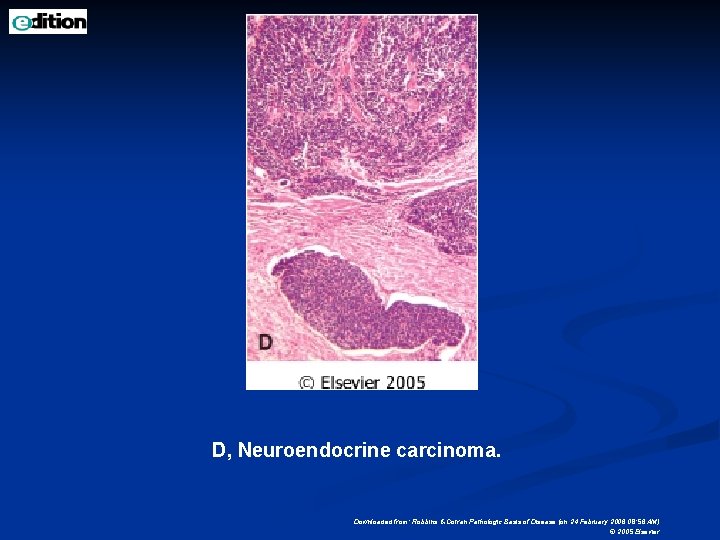
D, Neuroendocrine carcinoma. Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
n n n Clinical Course and Management Cervical cancer prevention and control can be divided into several components: One includes cytologic screening and management of Papanicolaou smear abnormalities, both of which may entail the use of HPV testing. Another is the histologic diagnosis and removal of precancers. Still another component is surgical removal of invasive cancers, with adjunctive radiation and chemotherapy. A final aspect that is currently under investigation is the use of vaccines, either for preventing HPV infection or treating existing disease.
n n n CIN lesions are characterized on colposcopic exam by white patches on the cervix after the application of acetic acid. In addition, distinct vascular mosaic or punctuation patterns can be observed. Highly abnormal vascular patterns regularly accompany invasive cervical cancer. If abnormalities are visualized, they must be confirmed by histologic examination of a punch biopsy. This is facilitated by both the application of morphologic criteria and also, recently, the immunohistochemical identification of increased expression of host cell biomarkers (such as p 16 INK 4, cyclin E, and Ki-67). These markers are expressed in a greater proportion of cells in precancerous lesions (due to cell cycle disturbances) and will frequently distinguish these from non-neoplastic epithelial changes.
n n Treatment of precursor lesions includes Papanicolaou smear follow-up for Low grade intraepithelial neoplasia-(CIN I), and cryotherapy, laser, loop electrical excision procedures (LEEP), and cone biopsy for High grade intraepithelial neoplasia (CIN II or CIN III). Rarely (approximately 1 in 500) a patient with a treated CIN III eventually develops an invasive cancer. The risk is minimized by follow-up pap smears. Although very early invasive cancers (microinvasive carcinomas) may be treated by cone biopsy alone, most invasive cancers are managed by hysterectomy with lymph node dissection and, for advanced lesions, radiation. The prognosis and survival for invasive carcinomas depend largely on the stage at which cancer is first discovered and to some degree on the cell type, with small cell neuroendocrine tumors having a poor prognosis.
n n n There is a 5 -year survival rate of at least 95% for stage IA (including microinvasive) carcinomas, About 80% to 90% with stage IB, 75% with stage II, Less than 50% for stage III and higher. Most patients with stage IV cancer die as a consequence of local extension of the tumor (e. g. , into and about the urinary bladder and ureters, leading to ureteral obstruction, pyelonephritis, and uremia) rather than distant metastases. Early detection has reduced the number of patients with stage IV cancer by over two-thirds in the past 50 years.
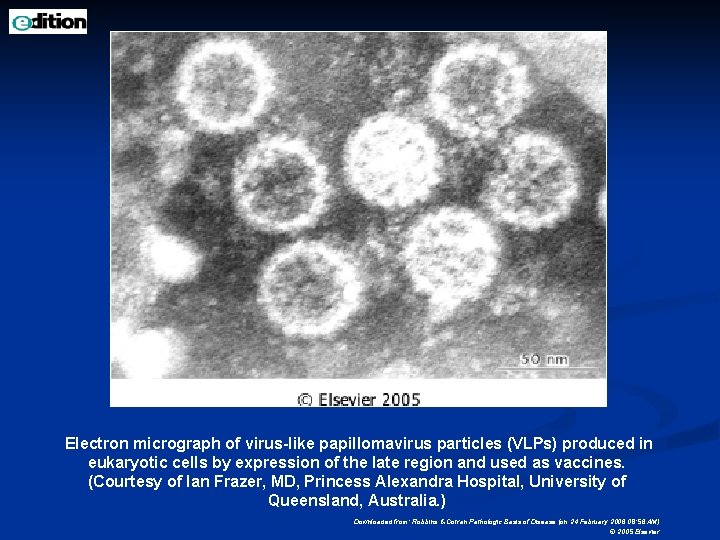
Recent publications have shown that HPV vaccines may prevent cervical HPV infection and, by inference, cervical cancer. n Assuming vaccination trials against cervical papillomaviruses bear fruit, it is conceivable that the next 20 years will witness the beginning of a significant and sustained reduction in not only cervical cancer incidence but also of other papillomavirusrelated diseases in both men and women. n
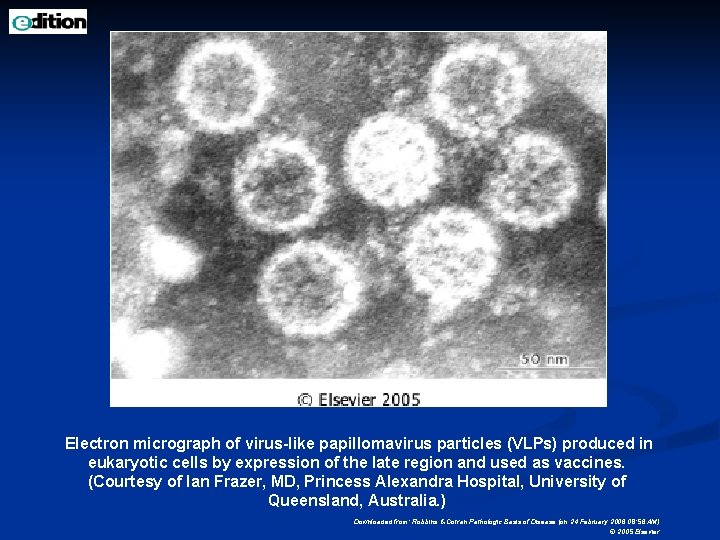
Electron micrograph of virus-like papillomavirus particles (VLPs) produced in eukaryotic cells by expression of the late region and used as vaccines. (Courtesy of Ian Frazer, MD, Princess Alexandra Hospital, University of Queensland, Australia. ) Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 24 February 2006 08: 56 AM) © 2005 Elsevier
Cervical carcinoma screening: PAP Smear "Where there is love of medicine, there is love of humankind" Hippocrates
Since the Pap examination was introduced after World War II, death rates from uterine cervical cancer have decreased by 70% in the US. “PAP smear is the most effective cancer screening test so far”
14, 000 women still die from cervical cancer every year, n related primarily to the fact that 80% of these women have never had a PAP smear or are tested only infrequently. n
Cytopathology is diagnosis of disease in cells. n Exfoliative & Non-Exfoliative - cytology. n Exfoliative: Cell samples are collected from normally shedding tissues like epithelium: use spatula or brush to enhances collection. n Non-Exfoliative: Cells samples collected by needles with suction pressure. n n Cytology specimen is fixed, stained and studied under microscope.
Screening test for cervical cancer. n It is a type of exfoliative cytology test. n Simple, safe, non-invasive method. n Developed by “George Papanicolaou” n Exfoliated cells from cervix are collected usually enhanced by using a variety of spatulas or brushes. n The specimen is processed and studied for morphology. n
Every woman should have an annual PAP examination when she becomes sexually active or turns 18 years old. n Regular PAP examinations (yearly) should continue even after menopause and after a hysterectomy. n
The best time for a PAP examination is during the two weeks following the end of menstrual flow (Proliferative phase). n If menopause, PAP examination can be scheduled anytime. n
Risk of Cervix Carcinoma · · · Any woman can develop Cervix carcinoma Multiple sex partners or a partner who has had multiple female partners Have had genital warts (HPV) Sexual relations before the age of 18 Previous abnormal PAP examination
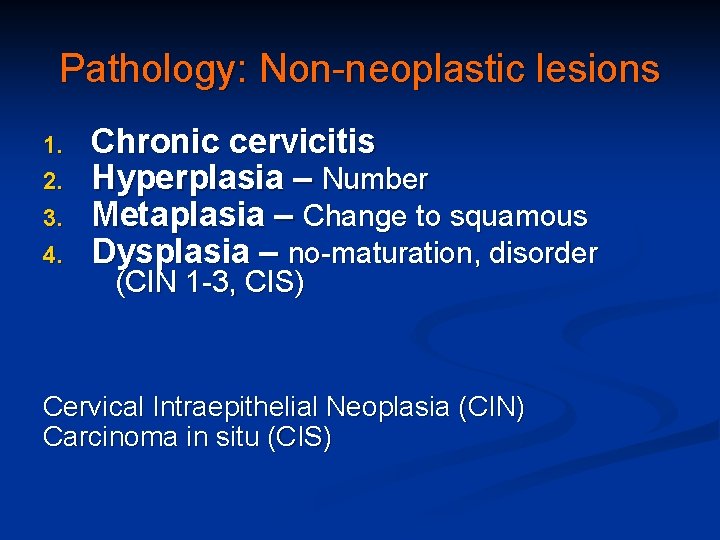
Pathology of Cervix The uterine cervix is continually being bombarded by a variety of stress including mechanical, microbiologic, chemical, and hormonal insults. n The cervix responds by n Acute or chronic inflammatory reactions n Adaptive proliferative responses like Hyperplasia, Metaplasia & Dysplasia. n Anaplasia - Benign & Malignant tumors. n
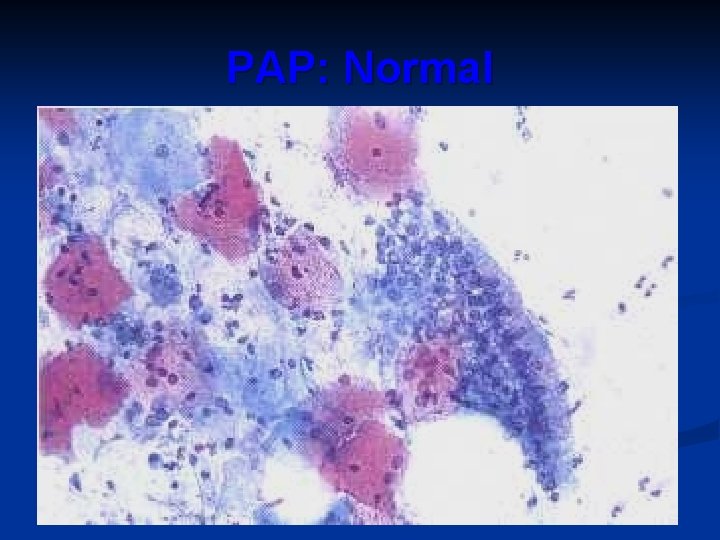
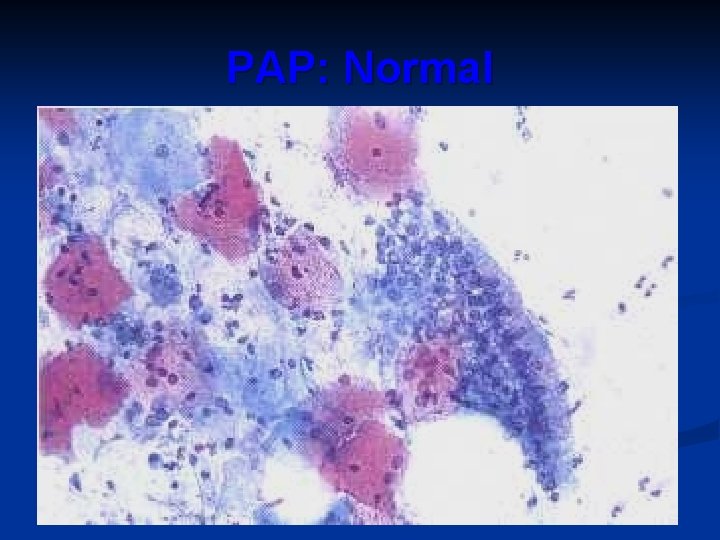
PAP: Normal
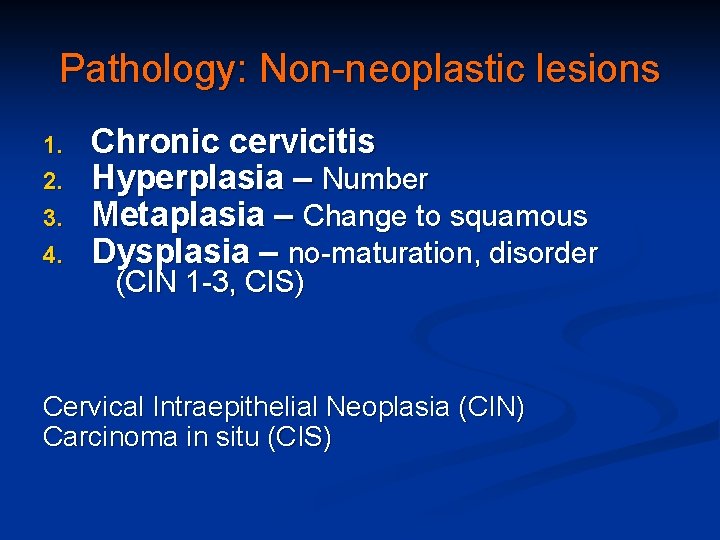
Pathology: Non-neoplastic lesions 1. 2. 3. 4. Chronic cervicitis Hyperplasia – Number Metaplasia – Change to squamous Dysplasia – no-maturation, disorder (CIN 1 -3, CIS) Cervical Intraepithelial Neoplasia (CIN) Carcinoma in situ (CIS)
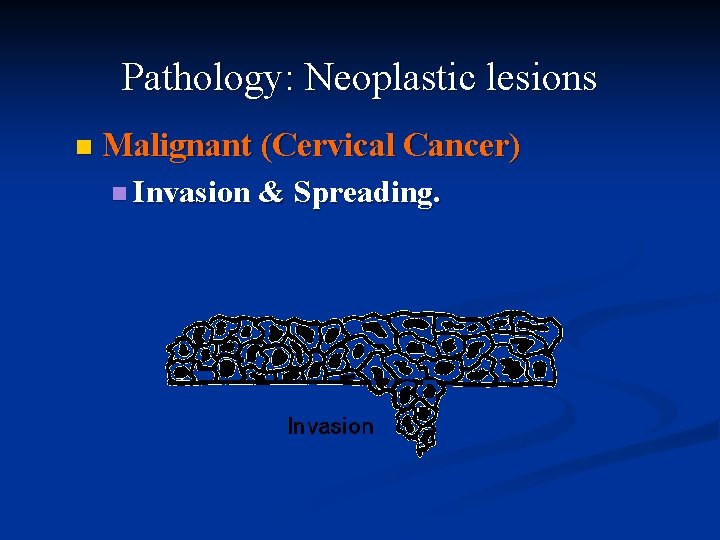
Pathology: Neoplastic lesions n Malignant (Cervical Cancer) n Invasion & Spreading.
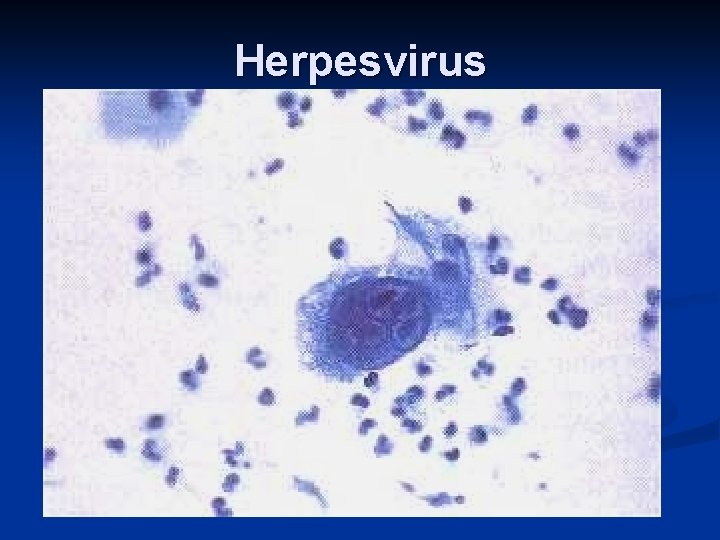
Herpesvirus
LSIL(Low grade intraepithelial lesion)
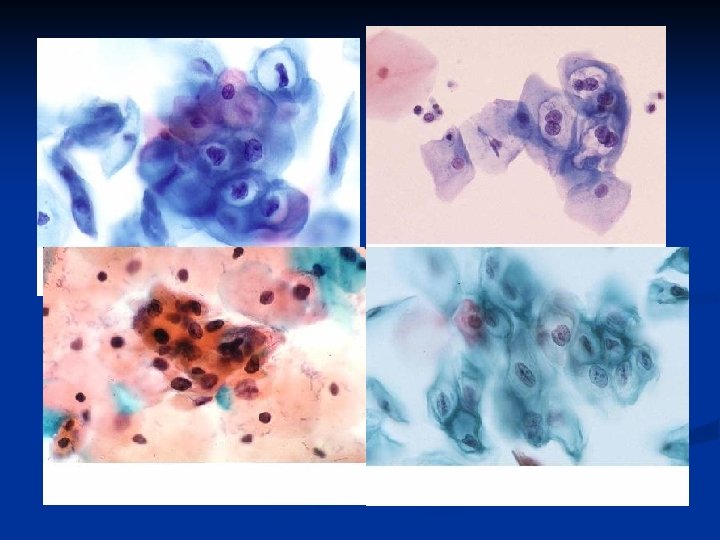
HSIL(High grade Intraepithelial Lesion)
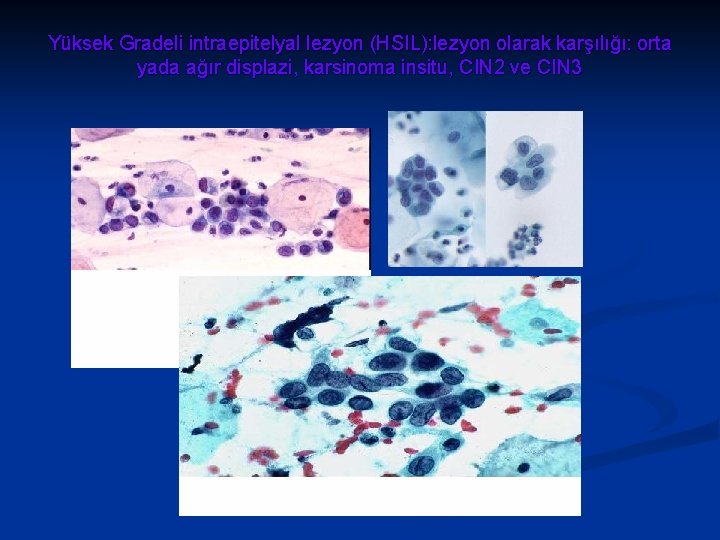
Yüksek Gradeli intraepitelyal lezyon (HSIL): lezyon olarak karşılığı: orta yada ağır displazi, karsinoma insitu, CIN 2 ve CIN 3
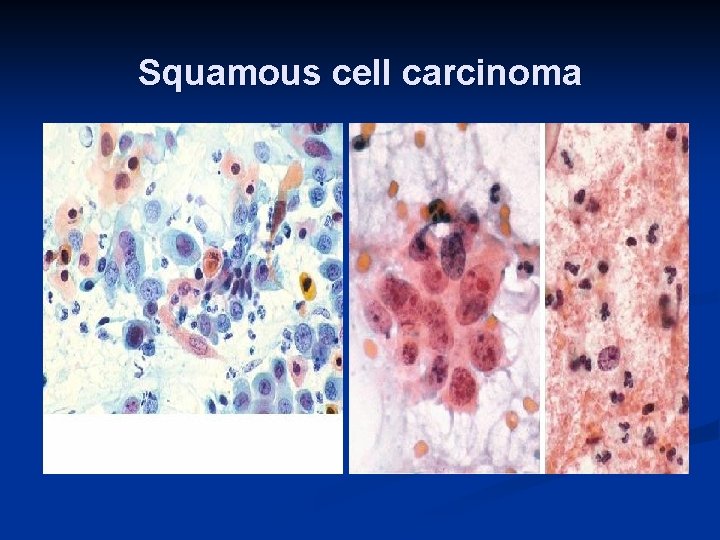
Squamous cell carcinoma
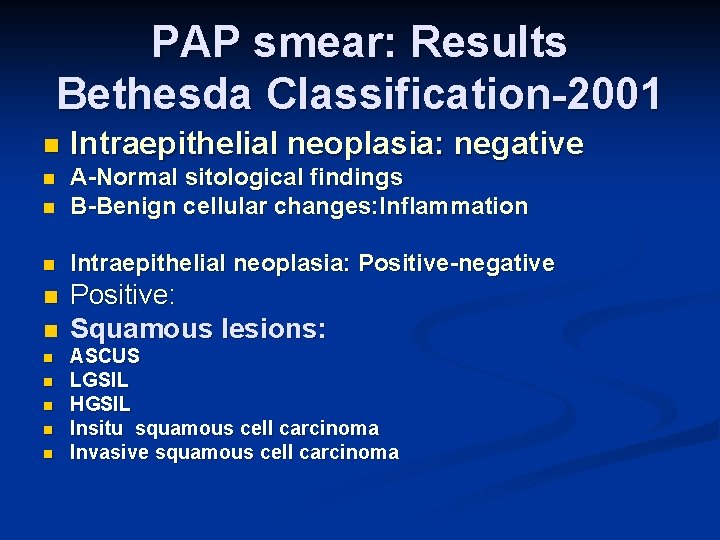
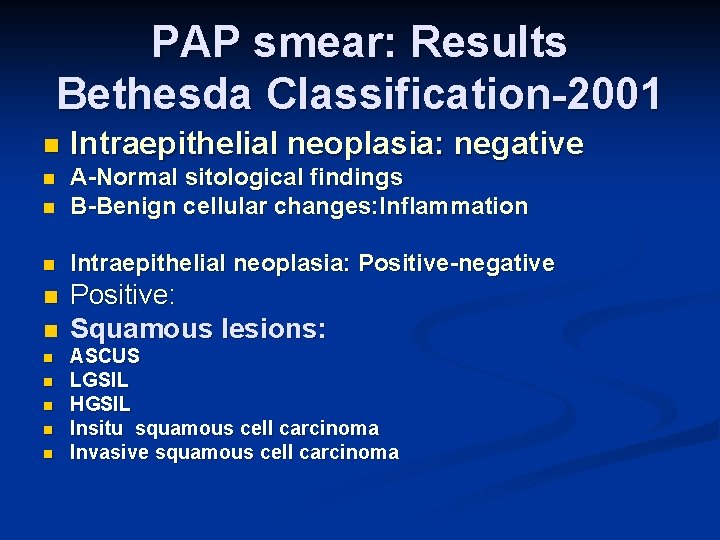
PAP smear: Results Bethesda Classification-2001 n Intraepithelial neoplasia: negative n n A-Normal sitological findings B-Benign cellular changes: Inflammation n Intraepithelial neoplasia: Positive-negative n Positive: Squamous lesions: n n n ASCUS LGSIL HGSIL Insitu squamous cell carcinoma Invasive squamous cell carcinoma
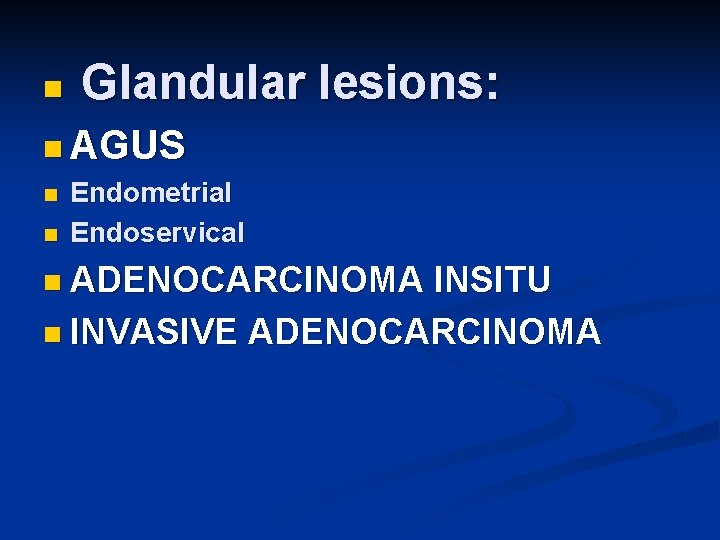
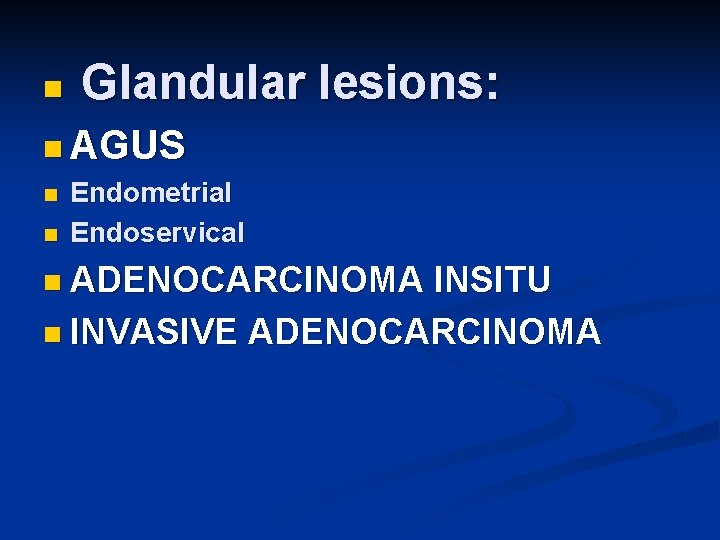
n Glandular lesions: n AGUS n Endometrial n Endoservical n ADENOCARCINOMA INSITU n INVASIVE ADENOCARCINOMA
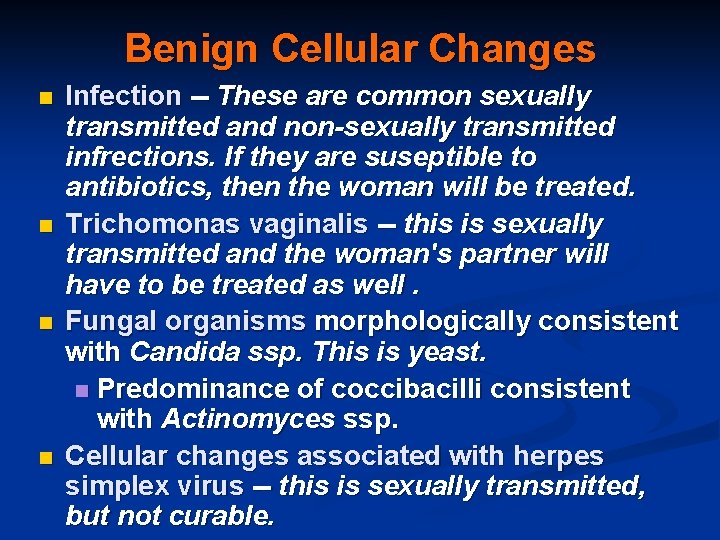
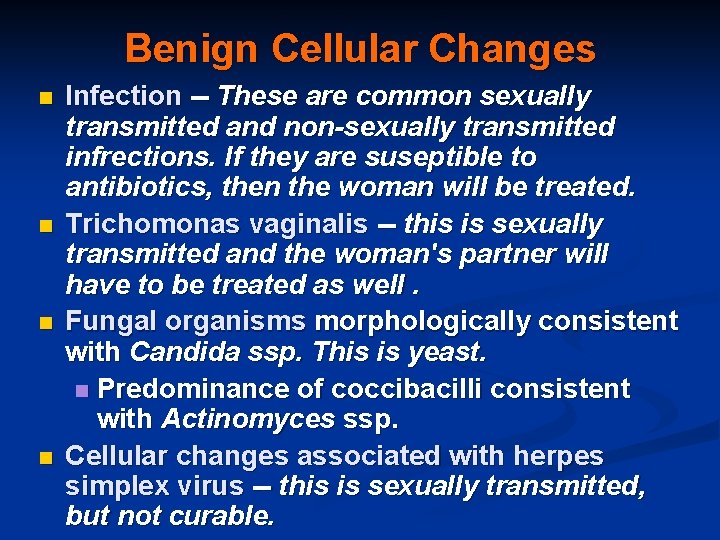
Benign Cellular Changes n n Infection -- These are common sexually transmitted and non-sexually transmitted infrections. If they are suseptible to antibiotics, then the woman will be treated. Trichomonas vaginalis -- this is sexually transmitted and the woman's partner will have to be treated as well. Fungal organisms morphologically consistent with Candida ssp. This is yeast. n Predominance of coccibacilli consistent with Actinomyces ssp. Cellular changes associated with herpes simplex virus -- this is sexually transmitted, but not curable.
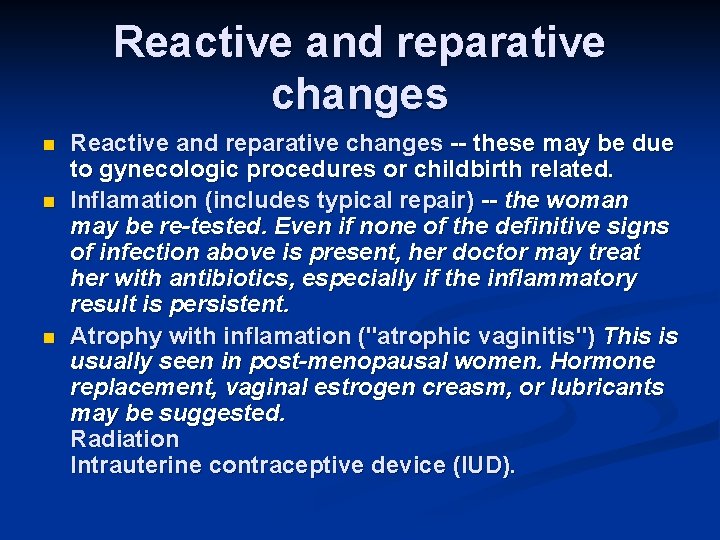
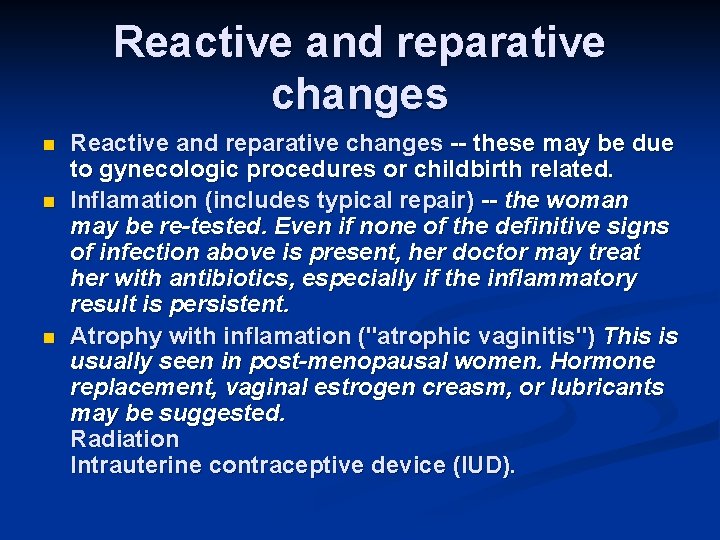
Reactive and reparative changes n n n Reactive and reparative changes -- these may be due to gynecologic procedures or childbirth related. Inflamation (includes typical repair) -- the woman may be re-tested. Even if none of the definitive signs of infection above is present, her doctor may treat her with antibiotics, especially if the inflammatory result is persistent. Atrophy with inflamation ("atrophic vaginitis") This is usually seen in post-menopausal women. Hormone replacement, vaginal estrogen creasm, or lubricants may be suggested. Radiation Intrauterine contraceptive device (IUD).
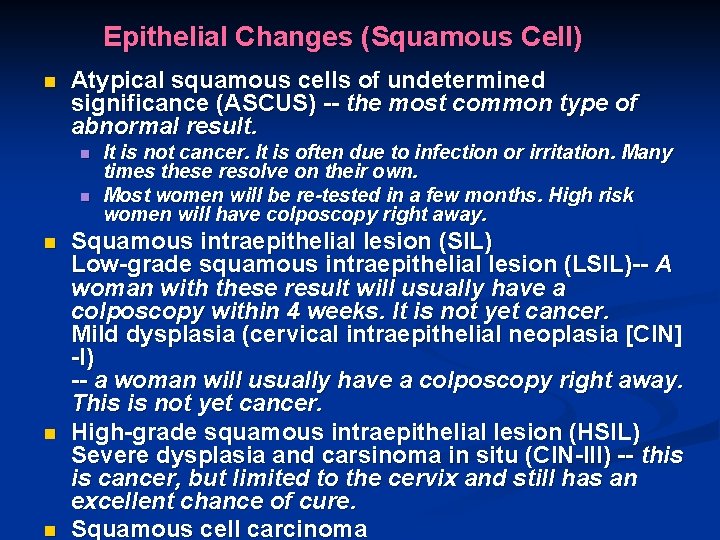
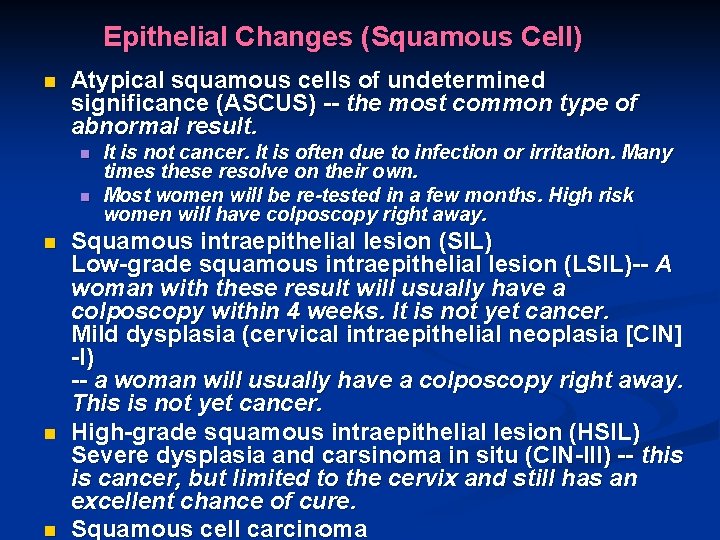
Epithelial Changes (Squamous Cell) n Atypical squamous cells of undetermined significance (ASCUS) -- the most common type of abnormal result. n n n It is not cancer. It is often due to infection or irritation. Many times these resolve on their own. Most women will be re-tested in a few months. High risk women will have colposcopy right away. Squamous intraepithelial lesion (SIL) Low-grade squamous intraepithelial lesion (LSIL)-- A woman with these result will usually have a colposcopy within 4 weeks. It is not yet cancer. Mild dysplasia (cervical intraepithelial neoplasia [CIN] -I) -- a woman will usually have a colposcopy right away. This is not yet cancer. High-grade squamous intraepithelial lesion (HSIL) Severe dysplasia and carsinoma in situ (CIN-III) -- this is cancer, but limited to the cervix and still has an excellent chance of cure. Squamous cell carcinoma
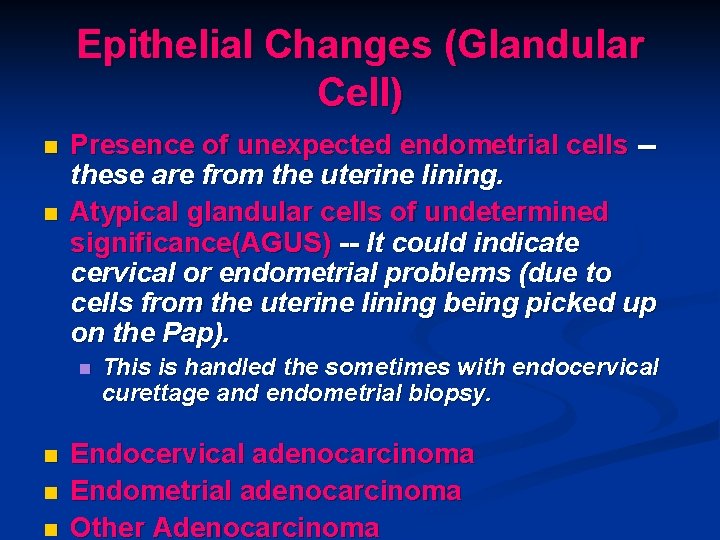
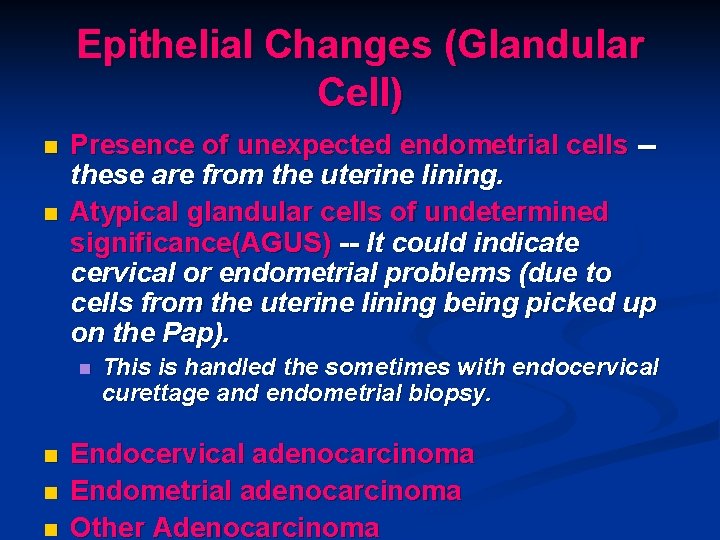
Epithelial Changes (Glandular Cell) n n Presence of unexpected endometrial cells -these are from the uterine lining. Atypical glandular cells of undetermined significance(AGUS) -- It could indicate cervical or endometrial problems (due to cells from the uterine lining being picked up on the Pap). n n This is handled the sometimes with endocervical curettage and endometrial biopsy. Endocervical adenocarcinoma Endometrial adenocarcinoma Other Adenocarcinoma
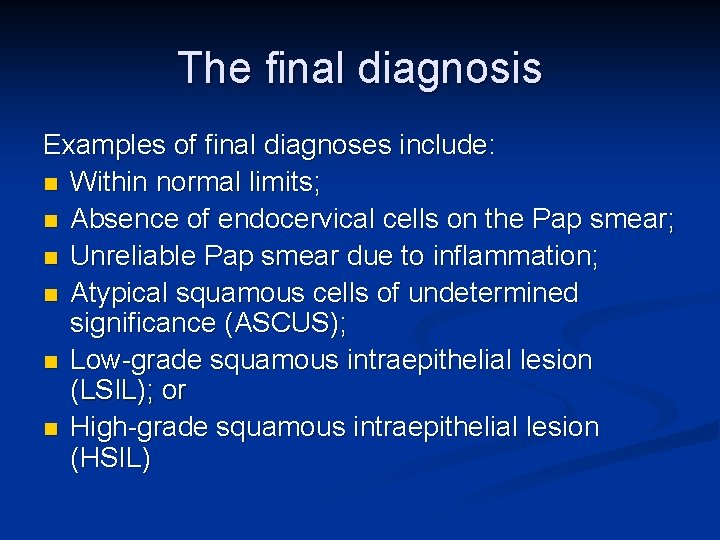
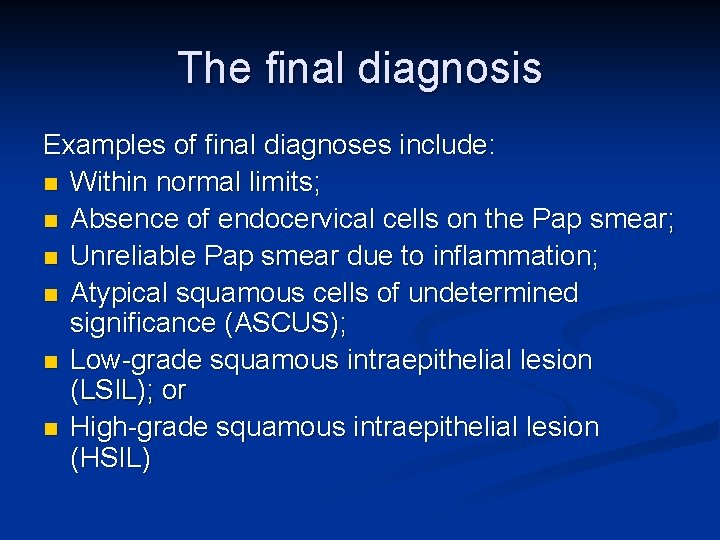
The final diagnosis Examples of final diagnoses include: n Within normal limits; n Absence of endocervical cells on the Pap smear; n Unreliable Pap smear due to inflammation; n Atypical squamous cells of undetermined significance (ASCUS); n Low-grade squamous intraepithelial lesion (LSIL); or n High-grade squamous intraepithelial lesion (HSIL)
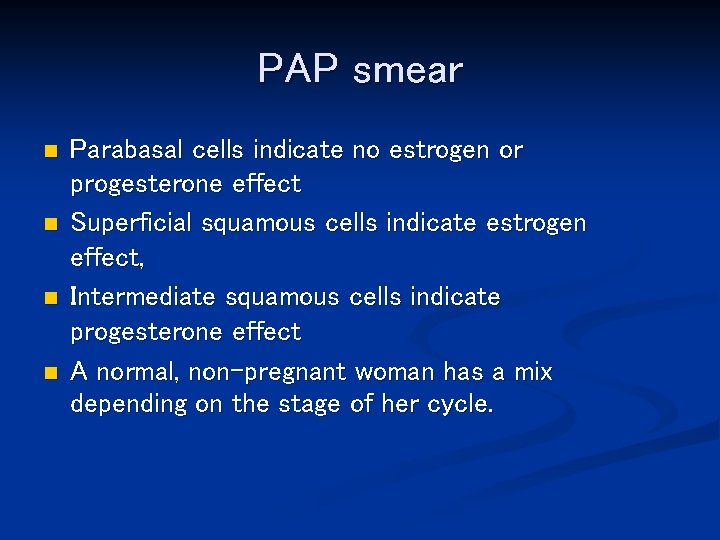
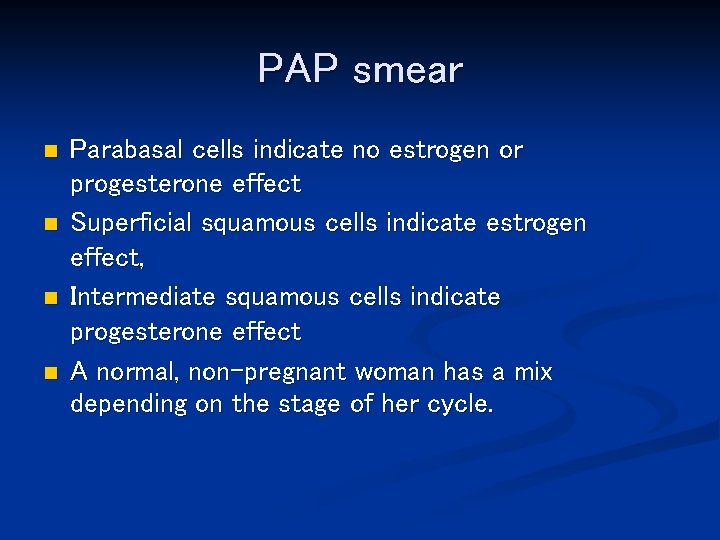
PAP smear n n Parabasal cells indicate no estrogen or progesterone effect Superficial squamous cells indicate estrogen effect, Intermediate squamous cells indicate progesterone effect A normal, non-pregnant woman has a mix depending on the stage of her cycle.