Pathology lec 2 Adaptation Cell injury Homeostasis Normal
- Slides: 51
Pathology lec 2 Adaptation & Cell injury
Homeostasis �Normal cell is in a state of functional and structural balance with neighboring cells. With a narrow range to handle its physiologic demand maintaining a steady state.
Adaptation � Adaptations are reversible functional and structural responses to more severe physiologic stresses and some pathologic stimuli, during which new but altered steady states are achieved, allowing the cell to survive and continue to function. �When the stress is eliminated the cell can recover to its original state without any harmful consequences
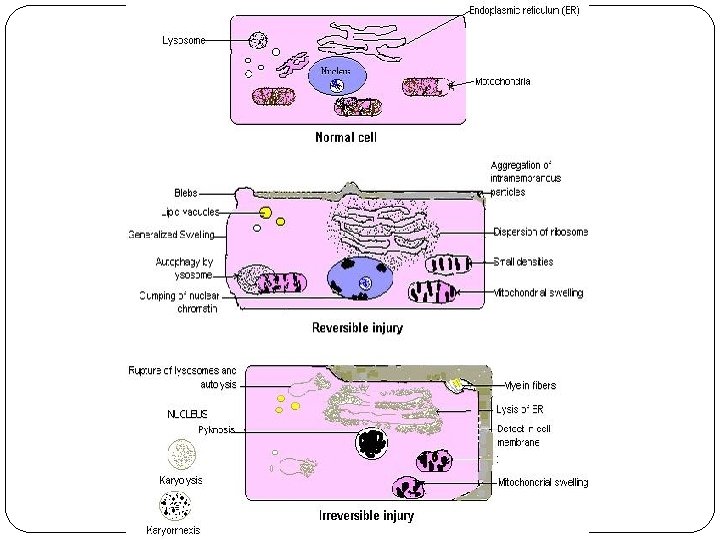
Cell injury �Normal cells are in a state of homeostasis ( equilibrium with their environment). �Injury is a set of biochemical and/or morphological changes that occur when the state of homeostasis is disturbed. �Cell injury is either reversible or irreversible. �Acute reversible injury include Cellular swelling and fatty change
Ø Intracellular accumulations Ø Pathologic calcification Ø Cell aging.
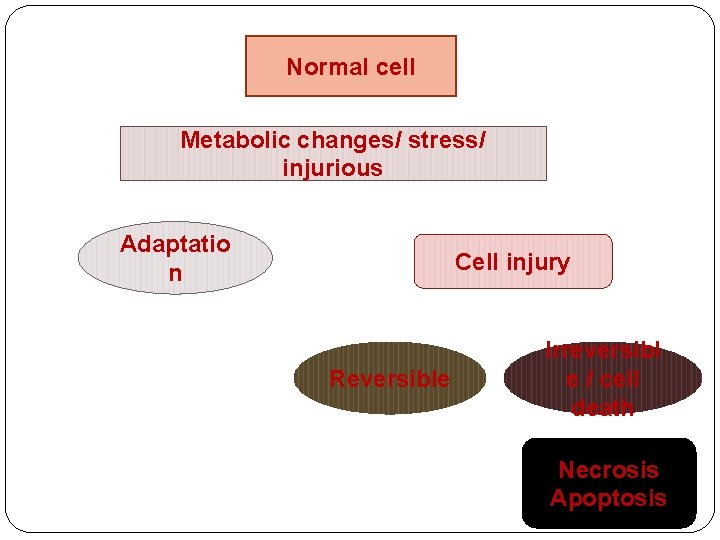
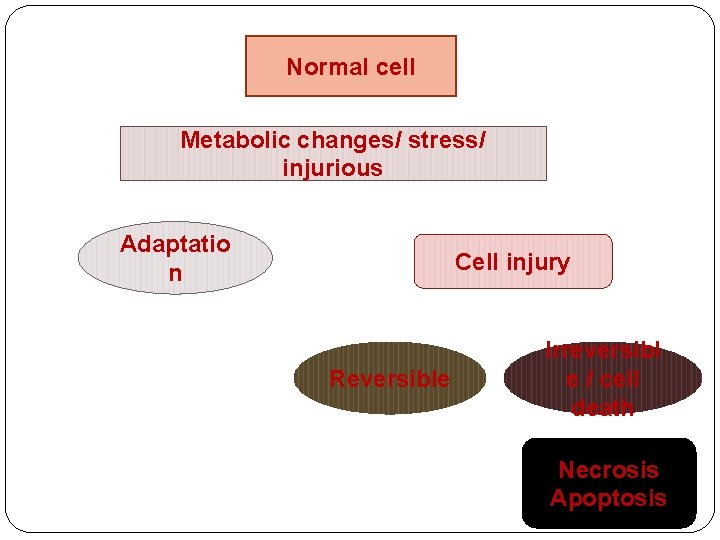
Normal cell Metabolic changes/ stress/ injurious Adaptatio n Cell injury Reversible Irreversibl e / cell death Necrosis Apoptosis
Adaptation response: v Adaptations are reversible changes in the size, number, phenotype, metabolic activity, or functions of cells in response to changes in their environment Ø Hypertrophy Ø Hyperplasia Ø Atrophy Ø Metaplasia
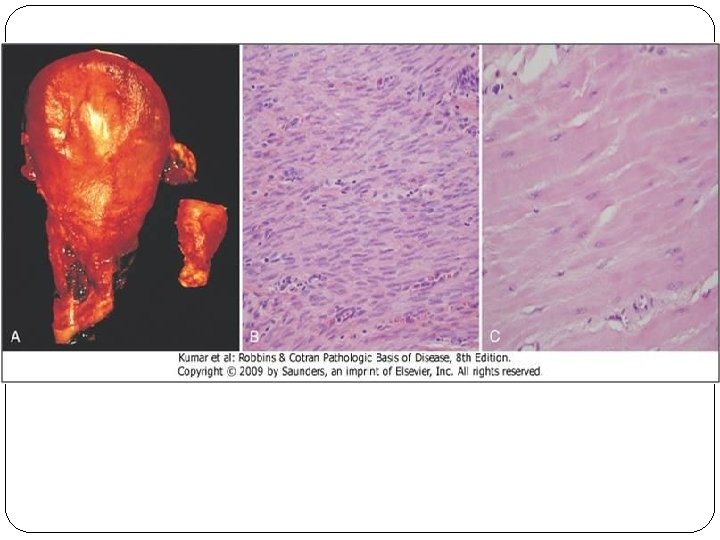
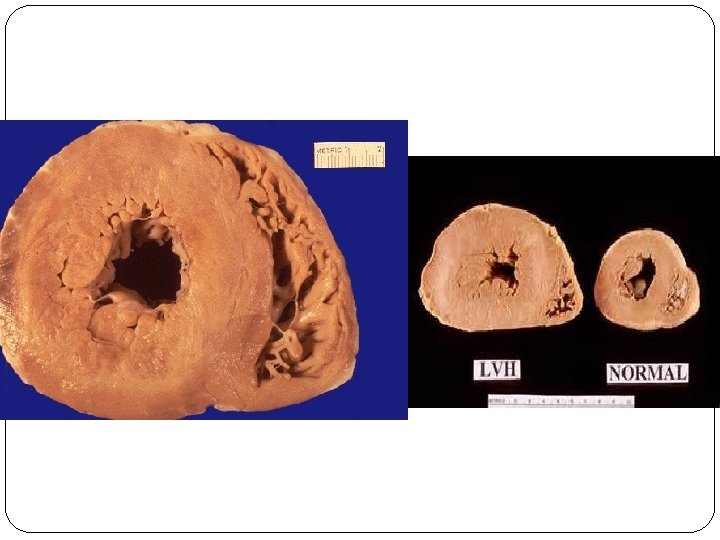
Hypertrophy �Hypertrophy refers to an increase in the size of cells, resulting in an increase in the size of the organ. �The increased size of the cells is due to the synthesis of more proteins and cell organelles. �Hypertrophy can be physiologic or pathologic. �Occurs as a response to increased functional demand or by stimulation by hormones and growth factors.
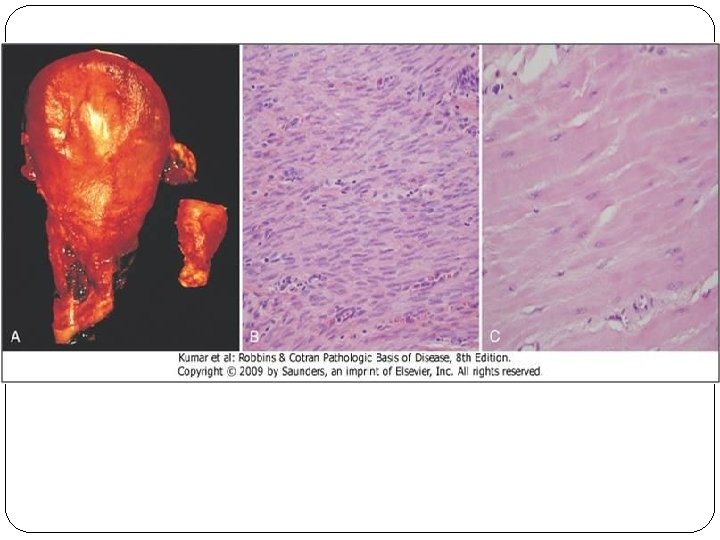
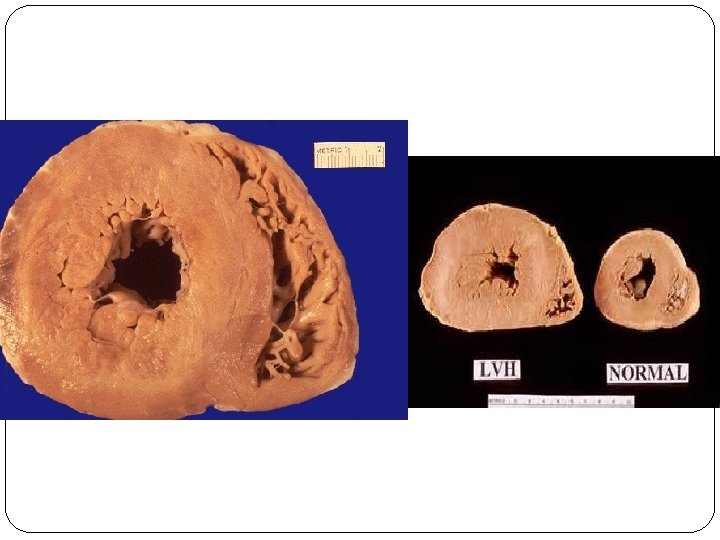
�Mechanism: activation of cell receptors, gens, growth factors leading to synthesis of proteins and cell organelles. �In the heart, the stimulus for hypertrophy is usually chronic hemodynamic overload, resulting from either hypertension or faulty valves. �The massive physiologic growth of the uterus during pregnancy due to hormone-induced increase in the size of an organ that results mainly from hypertrophy of muscle fibers.
Hyperplasia �Hyperplasia is an increase in the number of cells in an organ or tissue, usually resulting in increased mass of the organ or tissue. �Hyperplasia can be physiologic or pathologic. �The same triggers for hypertrophy; Hyperplasia takes place if the cell population can devide.
Ø Physiologic hyperplasia: ü hormonal hyperplasia ( e. g. proliferation of the glandular epithelium of the female breast at puberty and during pregnancy, usually accompanied by enlargement (hypertrophy) of the glandular epithelial cells). ü Compensatory hyperplasia, which increases tissue mass after damage or partial resection.
Ø Pathologic hyperplasia : caused by excesses of hormones or growth factors acting on target cells. ( e. g. Endometrial hyperplasia is an example of abnormal hormone-induced hyperplasia ; Hyperplasia is a characteristic response to certain viral infections, such as papillomaviruses, which cause skin warts and several mucosal lesions composed of masses of hyperplastic epithelium. growth factors produced by viral genes or by infected cells may stimulate cellular proliferation ).
�Mechanism: Hyperplasia is the result of growth factor–driven proliferation of mature cells and, in some cases, by increased output of new cells from tissue stem cells.
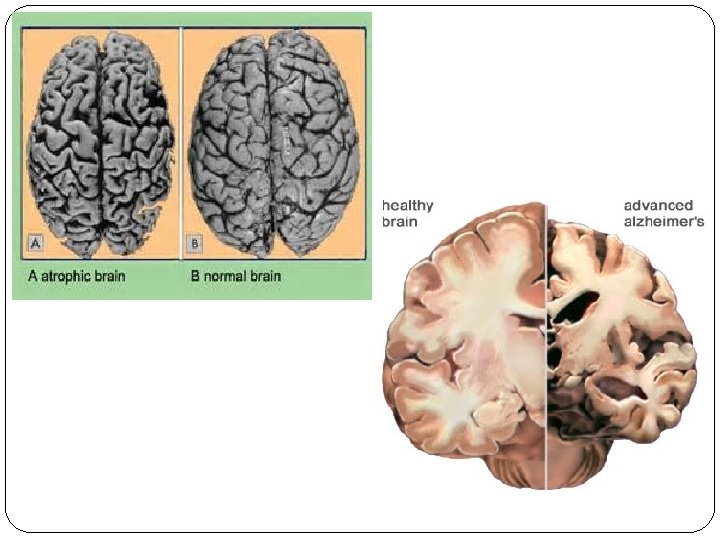
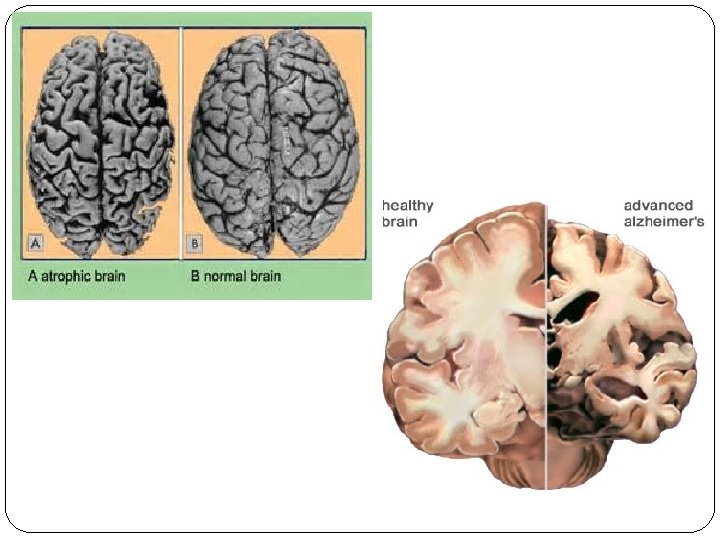
Atrophy �Atrophy is reduced size of an organ or tissue resulting from a decrease in cell size and number. �Atrophy can be physiologic or pathologic. Physiologic atrophy is common during normal development, such as the notochord and thyroglossal duct, undergo atrophy during fetal development.
�Pathologic atrophy depends on the underlying cause: ü Decreased workload (atrophy of disuse). ü Loss of innervation (denervation atrophy). ü Diminished blood supply. ü Inadequate nutrition. ü Loss of endocrine stimulation. ü Pressure.
Mechanisms of Atrophy �Atrophied cells had decrease in cell size and organelles, which may reduce the metabolic needs of the cell sufficiently to permit its survival. �Atrophy results from decreased protein synthesis and increased protein degradation in cells (ubiquitin-proteasome pathway). � Protein synthesis decreases because of reduced metabolic activity.
�atrophy is also accompanied by increased autophagy, with resulting increases in the number of autophagic vacuoles. � Autophagy (“self eating”) is the process in which the starved cell eats its own components in an attempt to find nutrients and survive.
Metaplasia �Metaplasia is a reversible change in which one differentiated cell type (epithelial or mesenchymal) is replaced by another cell type. � It represent an adaptive substitution of cells that are sensitive to stress by cell types better able to withstand the stress.
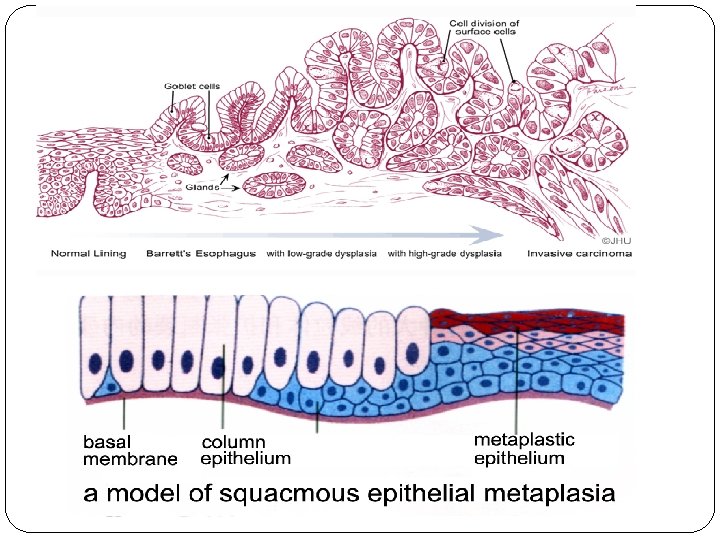
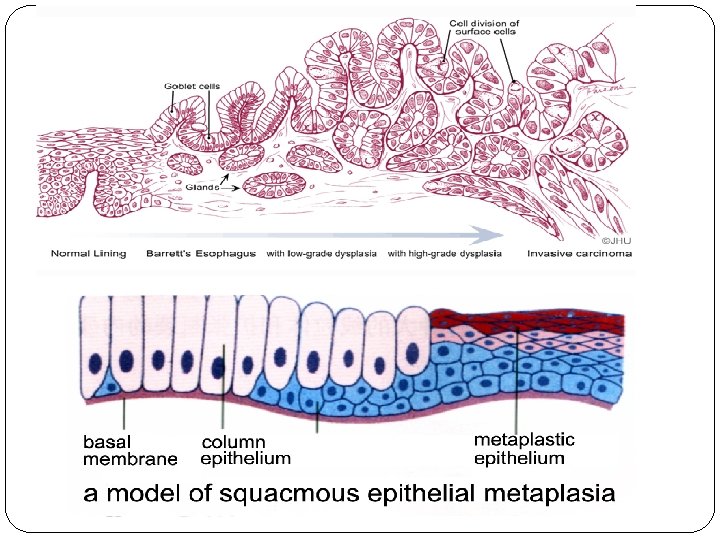
�The most common epithelial metaplasia is columnar to squamous, as occurs in the respiratory tract in response to chronic irritation in cigarette smokers. �Metaplasia from squamous to columnar type may also occur, as in Barrett esophagus.
�Metaplasia does not result from a change in the phenotype of an already differentiated cell type; instead it is the result of a reprogramming of stem cells that are known to exist in normal tissues, or of undifferentiated mesenchymal cells present in connective tissue.
Cell injury v Cell injury results when cells are stressed so severely that they are no longer able to adapt. v The injury depend on: type of stress, severity, type of cell/tissue affected. (e. g. neuron are more susceptible to ischemic injury than skeletal muscle).
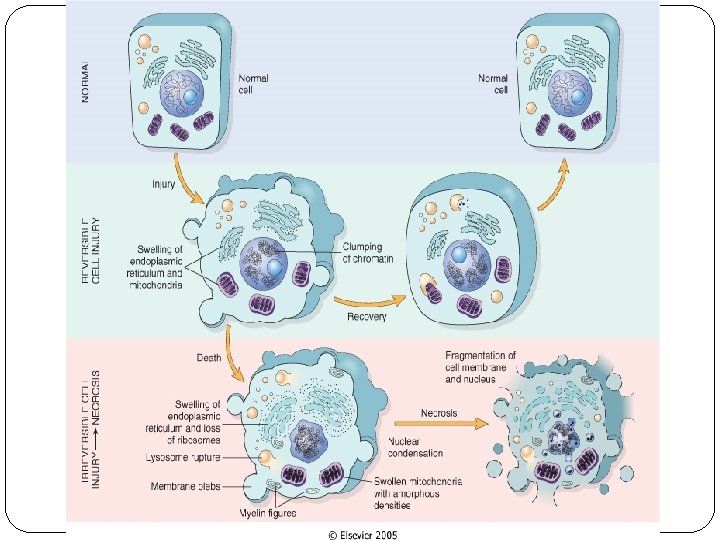
Reversible cell injury � In mild forms of injury, the functional and morphologic changes are reversible. � The hallmarks of reversible injury are reduced oxidative phosphorylation with resultant depletion of energy stores in the form of adenosine triphosphate (ATP), and cellular swelling caused by changes in ion concentrations and water influx.
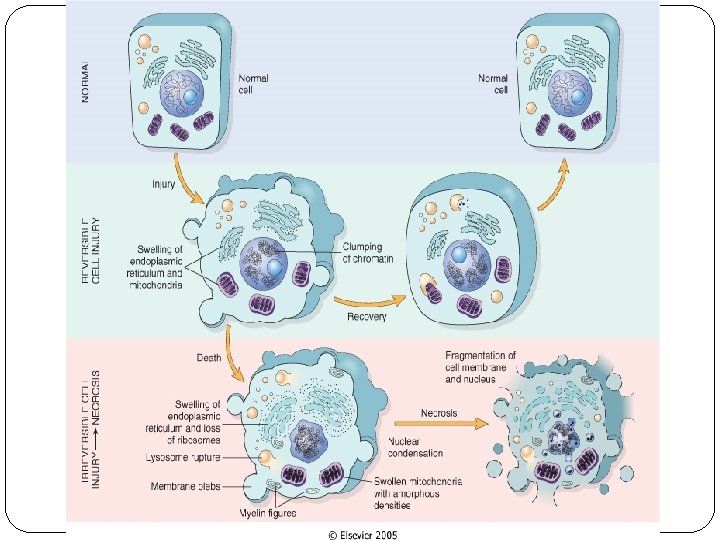
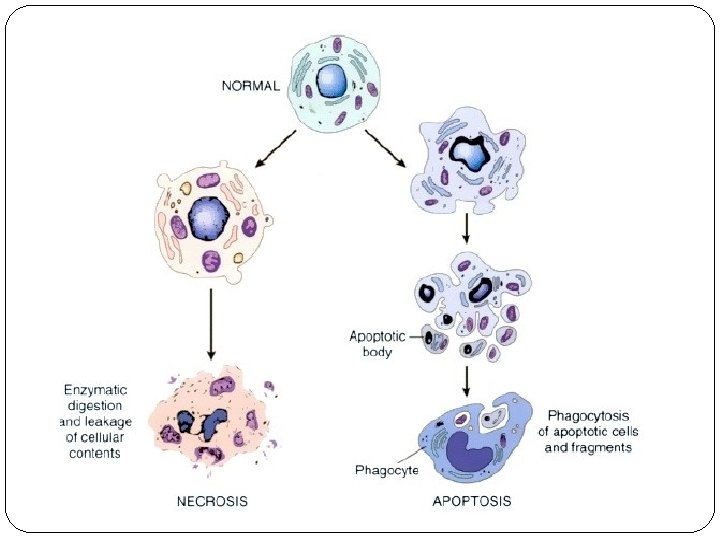
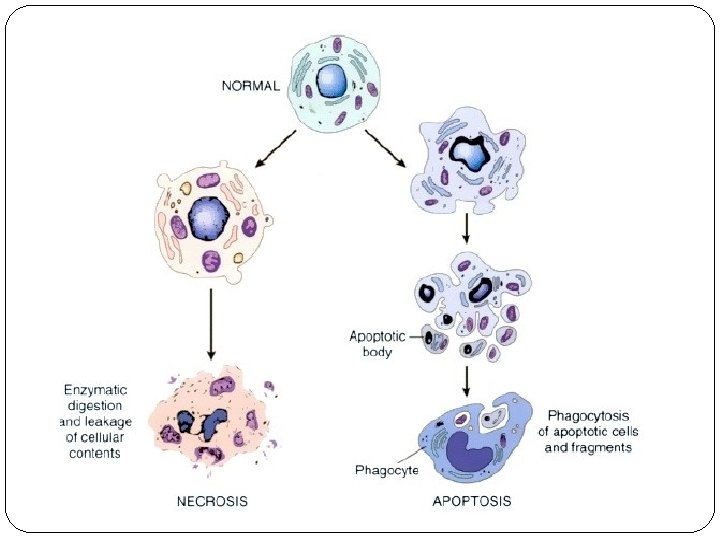
Cell death � When damage to membranes is severe, lysosomal enzymes enter the cytoplasm and digest the cell, and cellular contents leak out, resulting in necrosis. � In situations when the cell's DNA or proteins are damaged beyond repair, the cell kills itself by apoptosis, a form of cell death that is characterized by nuclear dissolution, fragmentation of the cell without complete loss of membrane integrity, and rapid removal of the cellular debris. � Whereas necrosis is always a pathologic process, apoptosis serves many normal functions and is not necessarily associated with cell injury.
Causes of cell injury: �The causes of cell injury are classified as exogenous or endogenous, it can occur due to the following factors: ü Excessive or prolonged normal stimuli (e. g hormones or growth factors). ü Action of toxins that inhibit the vital cell functions (e. g. oxidative phosphorylation or protein synthesis). ü Deficiency of oxygen and /or essential nutrients and metabolites.
Causes of Cell Injury �Oxygen Deprivation (Hypoxia). �Physical Agents �Chemical Agents and Drugs �Infectious Agents �Immunologic Reactions �Nutritional Imbalances �Genetic Derangements
�Hypoxia is the most important cause of cell injury. �Hypoxia is a relative deficiency of oxygen. �It may result from reduced supply or increased demand. �Complete block in the oxygen supply is called anoxia.
Causes of hypoxia ü Reduced blood flow (celled ischemia) ü Inadequate oxygenation of the blood due to cardiorespiratory failure. ü Decreased oxygen-carrying capacity of the blood, as in anemia or carbon monoxide poisoning (producing a stable carbon monoxyhemoglobin that blocks oxygen carriage). ü Severe blood loss.
�Exogenous causes include physical, chemical and biological factors, e. g heat, cold, toxins, drugs, viruses and bacteria. �Endogenous causes include gentic defects, metabolites, hormones, cytokines, and other bioactive substances.
Reversible injury is characterized by: ü generalized swelling of the cell and its organelles ü blebbing of the plasma membrane ü detachment of ribosomes from the ER ü clumping of nuclear chromatin. ü These morphologic changes are associated with decreased generation of ATP, loss of cell membrane integrity, defects in protein synthesis, cytoskeletal damage, and DNA damage.
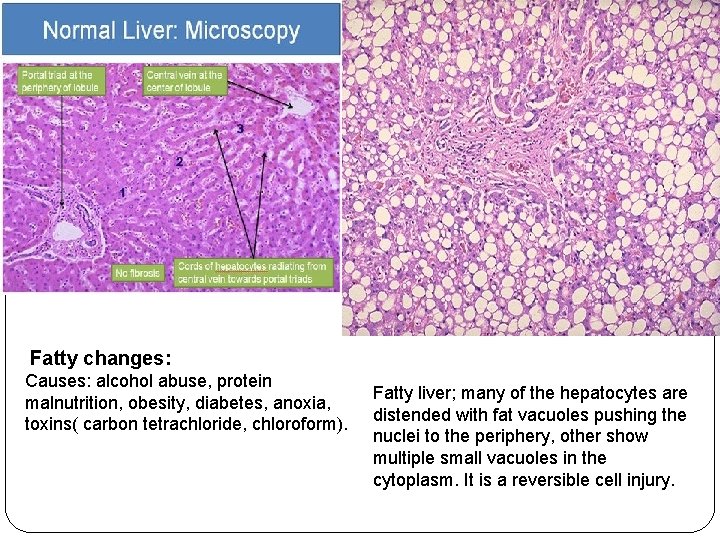
Two features of reversible cell injury can be recognized under the light microscope: Ø Cellular swelling appears whenever cells are incapable of maintaining ionic and fluid homeostasis and is the result of failure of energy-dependent ion pumps in the plasma membrane. Ø Fatty change occurs in hypoxic injury and various forms of toxic or metabolic injury. It is manifested by the appearance of lipid vacuoles in the cytoplasm. It is seen mainly in cells involved in and dependent on fat metabolism, such as hepatocytes and myocardial cells.
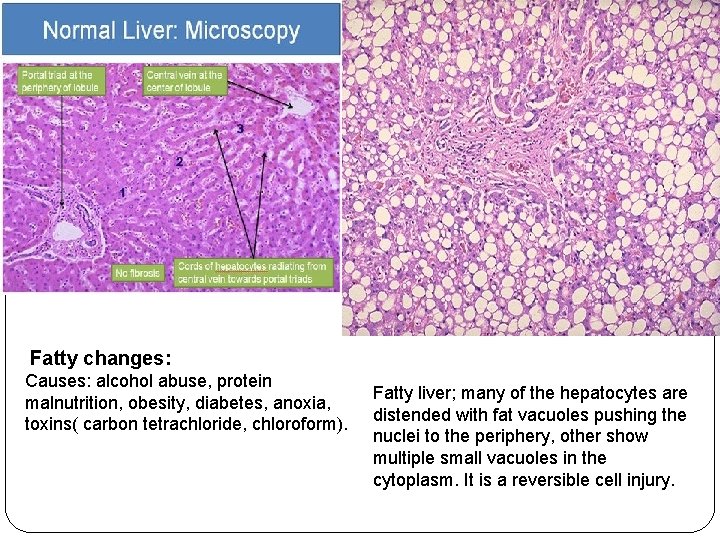
Fatty changes: Causes: alcohol abuse, protein malnutrition, obesity, diabetes, anoxia, toxins( carbon tetrachloride, chloroform). Fatty liver; many of the hepatocytes are distended with fat vacuoles pushing the nuclei to the periphery, other show multiple small vacuoles in the cytoplasm. It is a reversible cell injury.
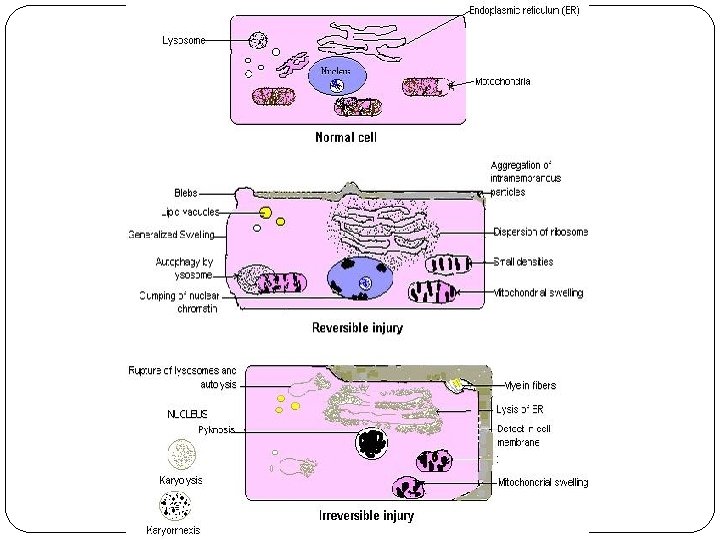
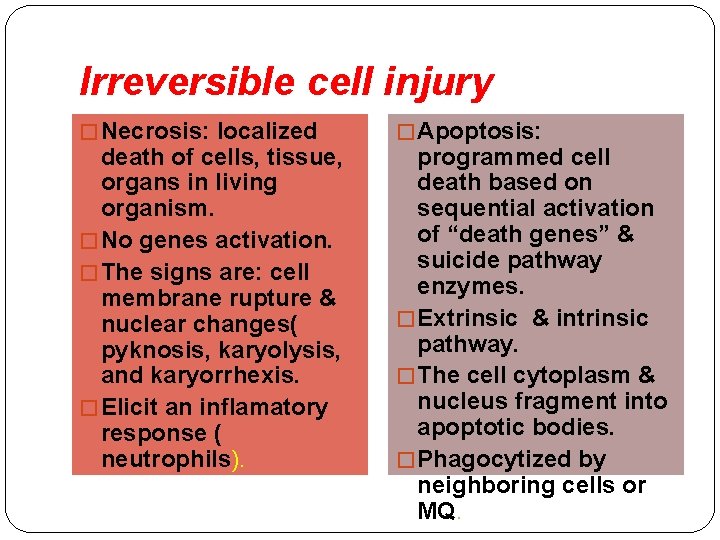
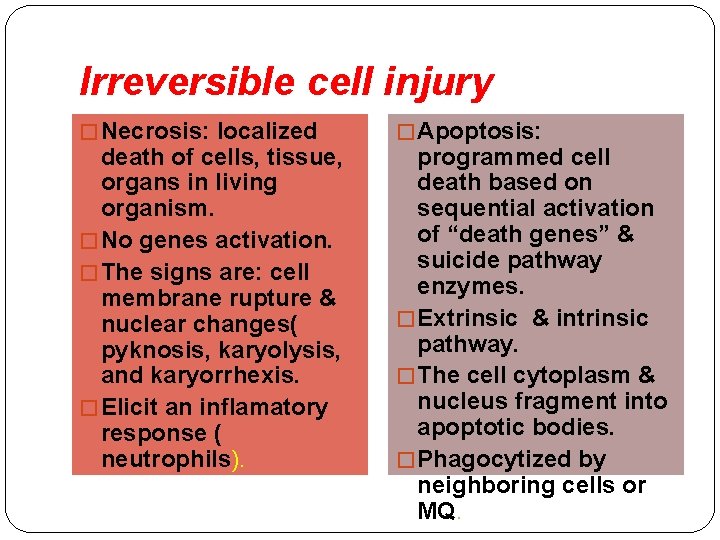
Irreversible cell injury � Necrosis: localized death of cells, tissue, organs in living organism. � No genes activation. � The signs are: cell membrane rupture & nuclear changes( pyknosis, karyolysis, and karyorrhexis. � Elicit an inflamatory response ( neutrophils). � Apoptosis: programmed cell death based on sequential activation of “death genes” & suicide pathway enzymes. � Extrinsic & intrinsic pathway. � The cell cytoplasm & nucleus fragment into apoptotic bodies. � Phagocytized by neighboring cells or MQ.
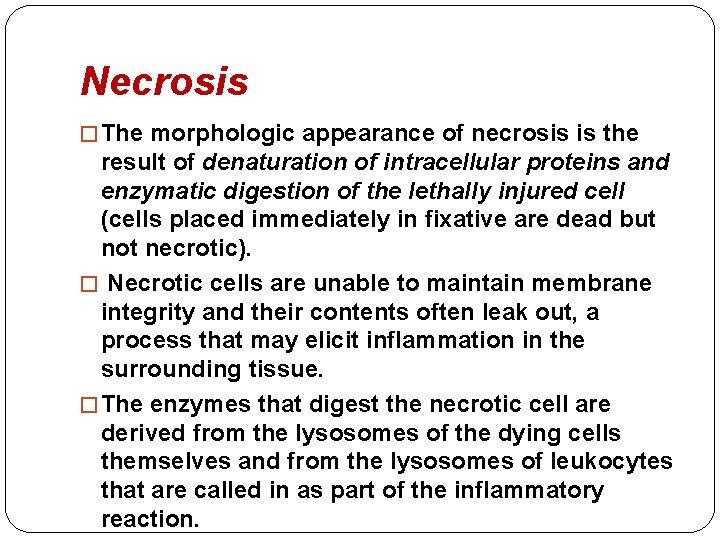
Necrosis � The morphologic appearance of necrosis is the result of denaturation of intracellular proteins and enzymatic digestion of the lethally injured cell (cells placed immediately in fixative are dead but not necrotic). � Necrotic cells are unable to maintain membrane integrity and their contents often leak out, a process that may elicit inflammation in the surrounding tissue. � The enzymes that digest the necrotic cell are derived from the lysosomes of the dying cells themselves and from the lysosomes of leukocytes that are called in as part of the inflammatory reaction.
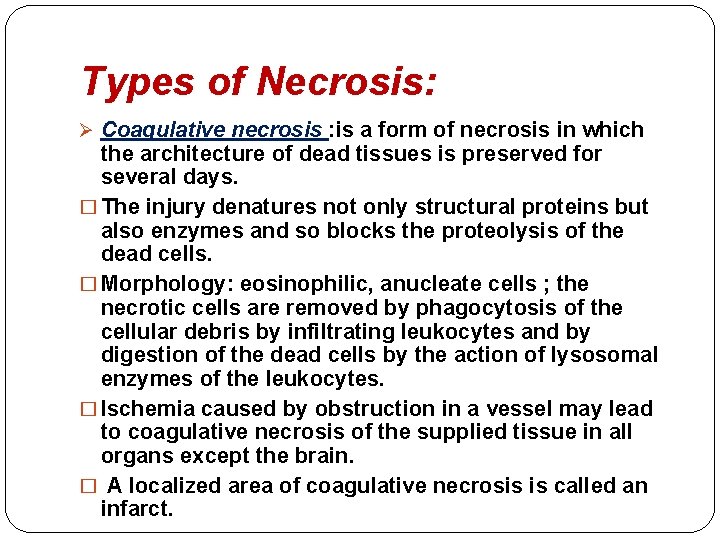
Types of Necrosis: Ø Coagulative necrosis : is a form of necrosis in which the architecture of dead tissues is preserved for several days. � The injury denatures not only structural proteins but also enzymes and so blocks the proteolysis of the dead cells. � Morphology: eosinophilic, anucleate cells ; the necrotic cells are removed by phagocytosis of the cellular debris by infiltrating leukocytes and by digestion of the dead cells by the action of lysosomal enzymes of the leukocytes. � Ischemia caused by obstruction in a vessel may lead to coagulative necrosis of the supplied tissue in all organs except the brain. � A localized area of coagulative necrosis is called an infarct.
Ø Liquefactive necrosis: is characterized by digestion of the dead cells, resulting in transformation of the tissue into a liquid viscous mass. � It is seen in focal bacterial or , fungal infections, because microbes stimulate the accumulation of leukocytes and the liberation of enzymes from these cells. � The necrotic material is frequently creamy yellow because of the presence of dead leukocytes and is called pus. � hypoxic death of cells within the central nervous system often manifests as liquefactive necrosis.
Ø Gangrenous necrosis : is not a specific pattern of cell death, but the term is commonly used in clinical practice. � It is usually applied to a limb, generally the lower leg, that has lost its blood supply and has undergone necrosis (typically coagulative necrosis) involving multiple tissue planes. When bacterial infection is superimposed there is more liquefactive necrosis because of the actions of degradative enzymes in the bacteria and the attracted leukocytes.
Ø Caseous necrosis : is used most often in foci of tuberculous infection. �The term “caseous” (cheeselike) is derived from the friable white appearance of the area of necrosis. �On microscopic examination, the necrotic area appears as a collection of fragmented or lysed cells and amorphous granular debris enclosed within a distinctive inflammatory border; this appearance is characteristic of a focus of inflammation known as a granuloma.
Ø Fat necrosis : it refers to focal areas of fat destruction, typically resulting from release of activated pancreatic lipases into the substance of the pancreas and the peritoneal cavity. �The released lipases split the triglyceride esters contained within fat cells. �The fatty acids, combine with calcium to produce grossly visible chalky-white areas (fat saponification), which enable the surgeon and the pathologist to identify the lesions.
Ø Fibrinoid necrosis is a special form of necrosis usually seen in immune reactions involving blood vessels.
Apoptosis �Apoptosis is a pathway of cell death that is induced by a tightly regulated suicide program in which cells destined to die activate enzymes that degrade the cells' own nuclear DNA and nuclear and cytoplasmic proteins.
�Apoptotic cells break up into fragments, called apoptotic bodies, which contain portions of the cytoplasm and nucleus. � The plasma membrane of the apoptotic cell and bodies remains intact, but its structure is altered in such a way that these become “tasty” targets for phagocytes.
Morphology of apoptosis ü Cell shrinkage: The cell is smaller in size; the cytoplasm is dense and the organelles are more tightly packed. ü Chromatin condensation: This is the most characteristic feature of apoptosis; The chromatin aggregates peripherally, under the nuclear membrane, into dense masses of various shapes and sizes ; The nucleus itself may break up, producing two or more fragments. ü Formation of cytoplasmic blebs and apoptotic bodies. ü Phagocytosis of apoptotic cells or cell bodies, usually by macrophages.
Ø Apoptosis regulated by genes: �bcl 2 ( inhibit apoptosis): prevent release of cytochrome c from the mitochondria. �P 53 ( stimulate apoptosis): elevated by DNA injury and arrests the cell cycle. �Apoptosis Induced By the TNF Receptor Family.
Ø Mechanism: � mediated by cascade of caspase. �Caspase digest nuclear and cytoskeletal proteins, and activate endonuclease.