PATHOLOGY Degenerative changes in the lumbar spine disc
PATHOLOGY Degenerative changes in the lumbar spine disc degeneration vertebral compression deformities ligamentous laxity deterioration of facet joint cartilage May cause instability and subluxation of one vertebra on another (degenerative spondylolisthesis)

Anterolisthesis at L 4 -L 5
PATHOLOGY Backward slippage (retrolisthesis) is generally believed to be asymptomatic and of little clinical significance. Forward slippage (anterolisthesis) may result in narrowing of vertebral canal and neural foramina (spinal stenosis) leading to development of chronic back pain (with or without leg pain). Compression of L 5 spinal nerve may be involved.
PATHOLOGY When LS joint is particularly stable, L 4 and L 5 are more vulnerable to stress forces. If degenerative changes have occurred, anterolisthesis at L 4 is more likely. Clinical symptoms associated with anterior subluxation at L 4 -L 5 at L 3 -L 4 80% 10 -20%
PATHOLOGY Spinal stenosis symptoms: back pain progressing to leg pain functional independence deteriorates reduced ability to walk reduced ability to carry out ADLs Symptoms often episodic, no natural resolution over time
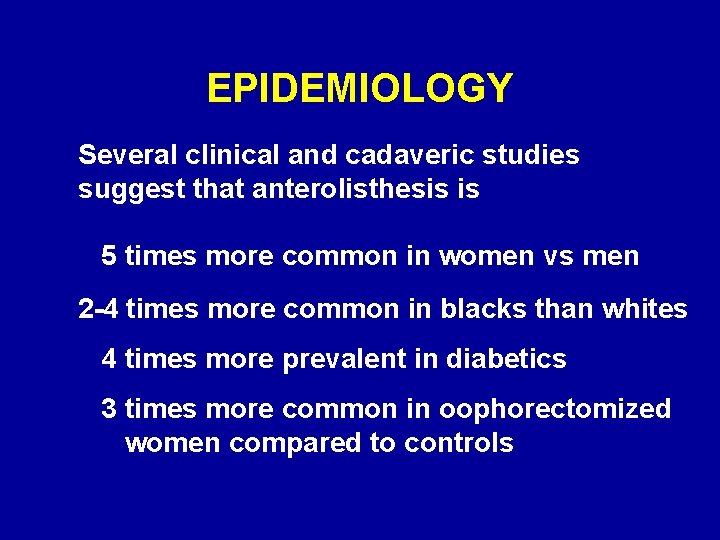
EPIDEMIOLOGY Several clinical and cadaveric studies suggest that anterolisthesis is 5 times more common in women vs men 2 -4 times more common in blacks than whites 4 times more prevalent in diabetics 3 times more common in oophorectomized women compared to controls
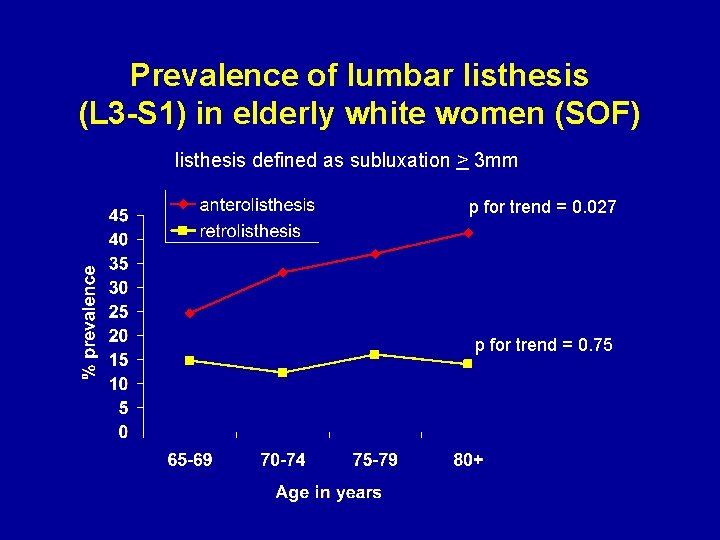
Prevalence of lumbar listhesis (L 3 -S 1) in elderly white women (SOF) listhesis defined as subluxation > 3 mm p for trend = 0. 027 p for trend = 0. 75
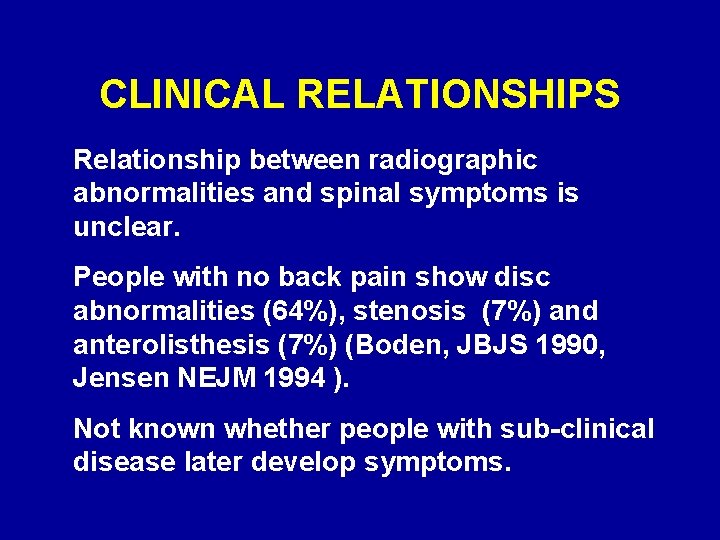
CLINICAL RELATIONSHIPS Relationship between radiographic abnormalities and spinal symptoms is unclear. People with no back pain show disc abnormalities (64%), stenosis (7%) and anterolisthesis (7%) (Boden, JBJS 1990, Jensen NEJM 1994 ). Not known whether people with sub-clinical disease later develop symptoms.
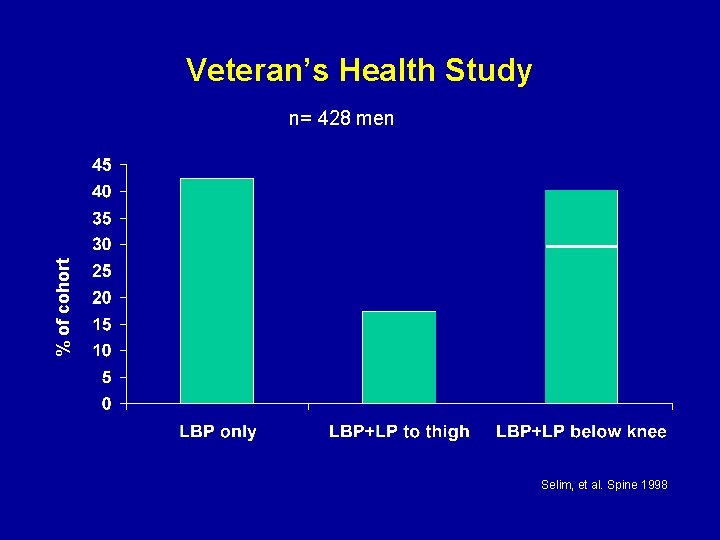
Veteran’s Health Study % of cohort n= 428 men Selim, et al. Spine 1998
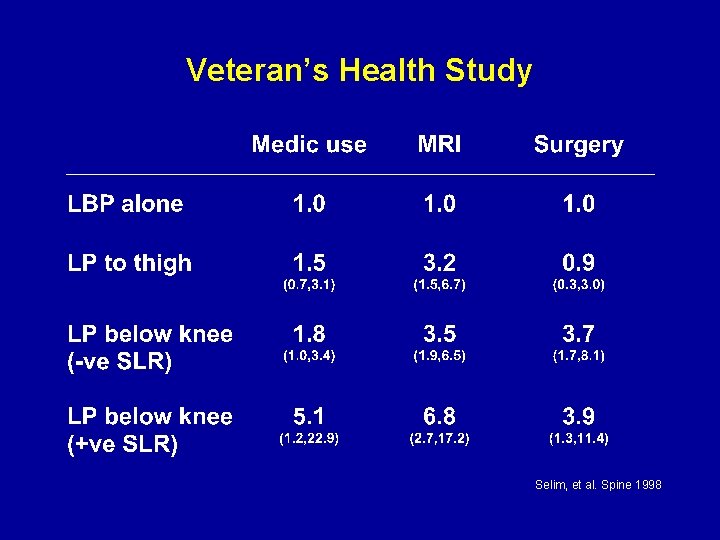
Veteran’s Health Study Selim, et al. Spine 1998
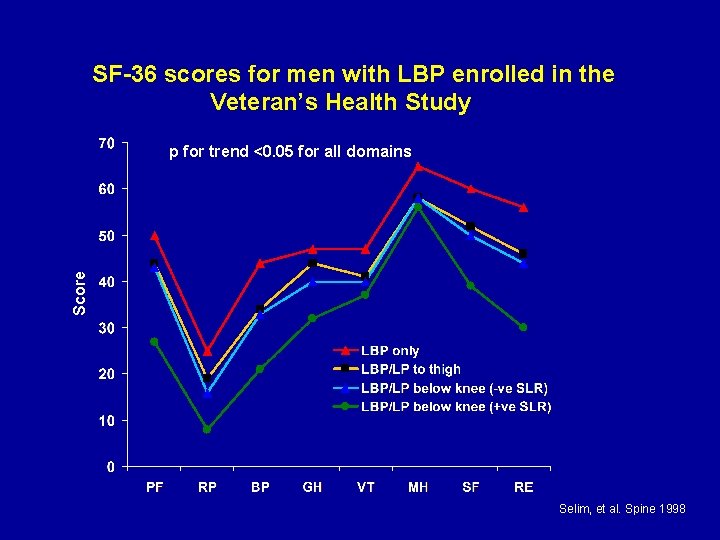
SF-36 scores for men with LBP enrolled in the Veteran’s Health Study Score p for trend <0. 05 for all domains Selim, et al. Spine 1998
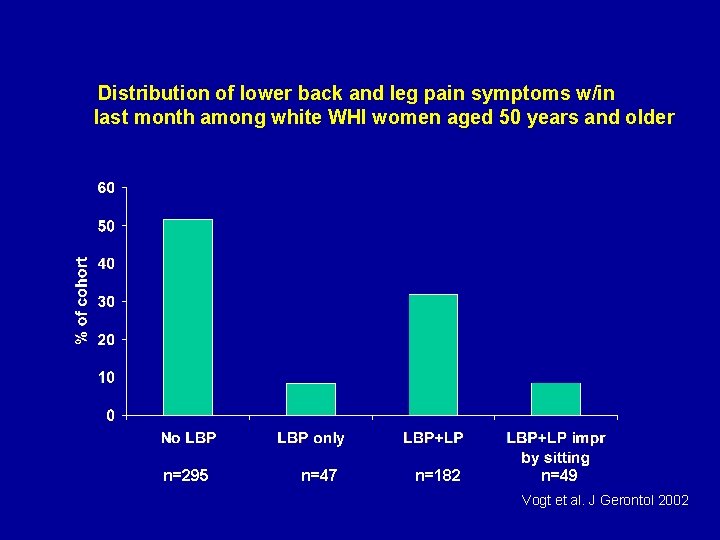
Distribution of lower back and leg pain symptoms w/in last month among white WHI women aged 50 years and older n=295 n=47 n=182 n=49 Vogt et al. J Gerontol 2002
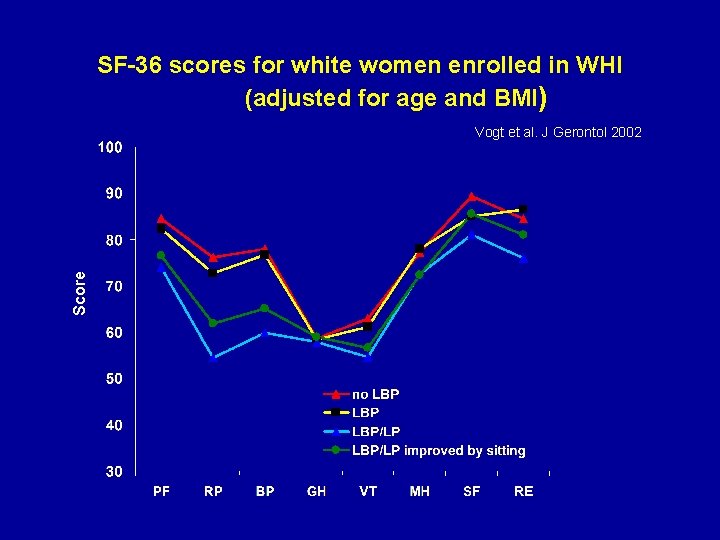
SF-36 scores for white women enrolled in WHI (adjusted for age and BMI) Score Vogt et al. J Gerontol 2002
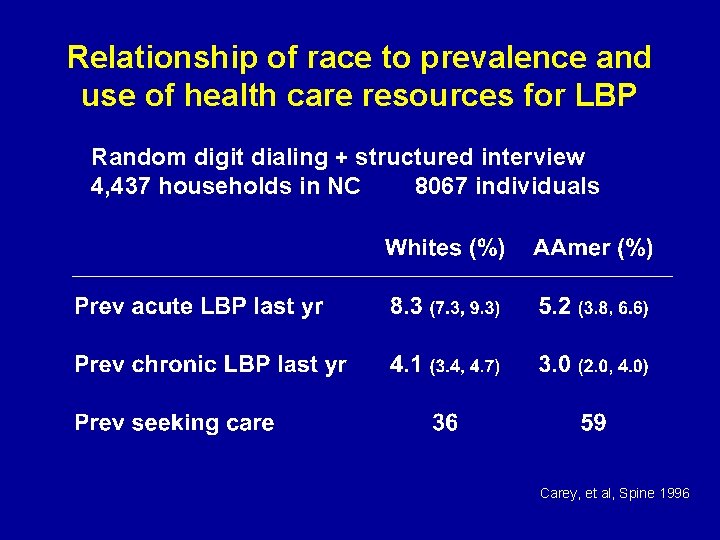
Relationship of race to prevalence and use of health care resources for LBP Random digit dialing + structured interview 4, 437 households in NC 8067 individuals Carey, et al, Spine 1996
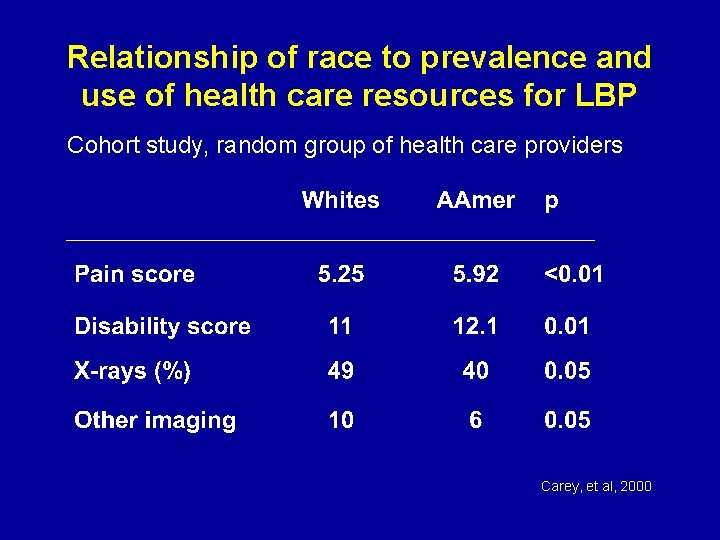
Relationship of race to prevalence and use of health care resources for LBP Cohort study, random group of health care providers Carey, et al, 2000
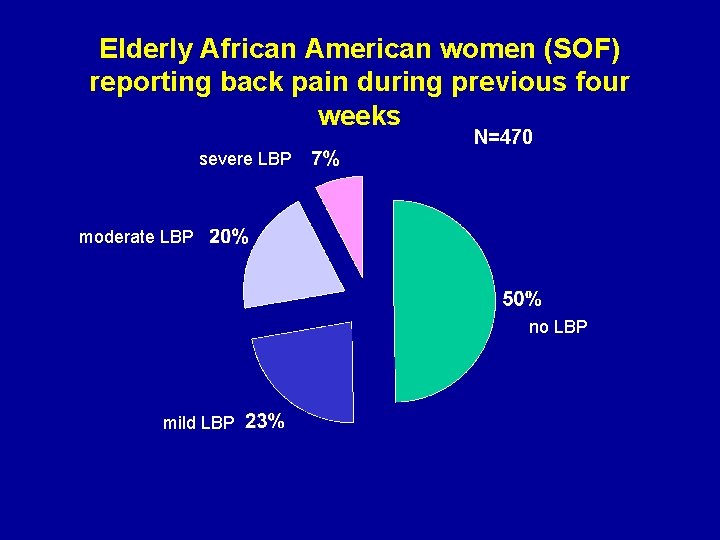
Elderly African American women (SOF) reporting back pain during previous four weeks N=470 severe LBP moderate LBP no LBP mild LBP
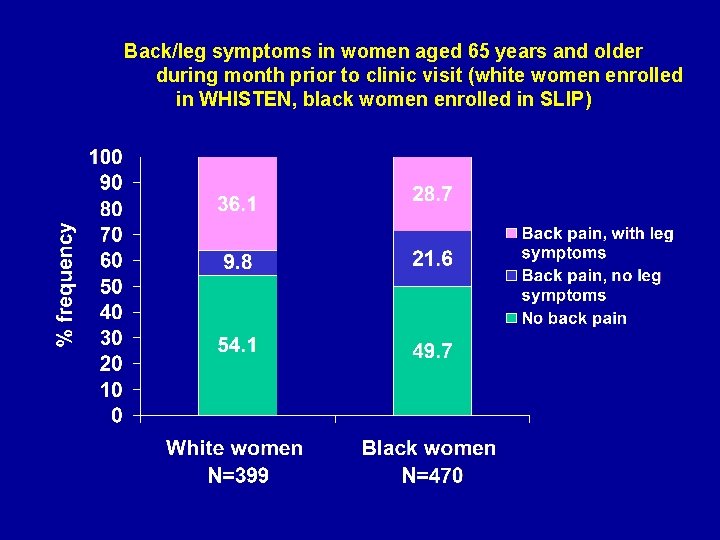
Back/leg symptoms in women aged 65 years and older during month prior to clinic visit (white women enrolled in WHISTEN, black women enrolled in SLIP)
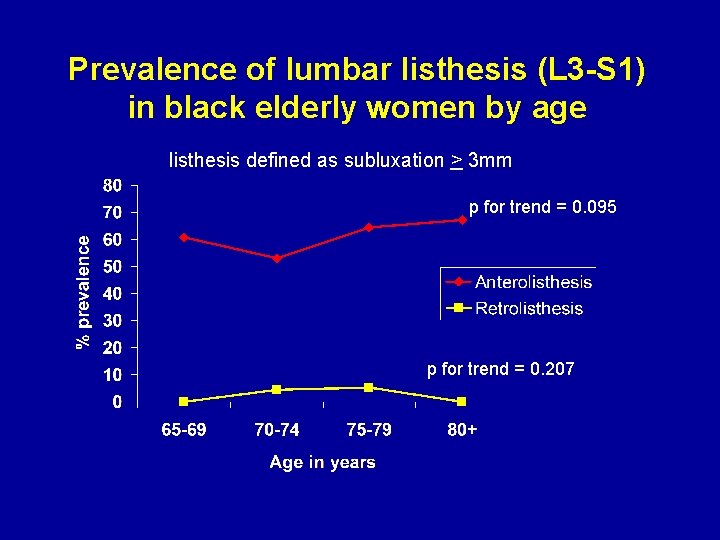
Prevalence of lumbar listhesis (L 3 -S 1) in black elderly women by age listhesis defined as subluxation > 3 mm p for trend = 0. 095 p for trend = 0. 207
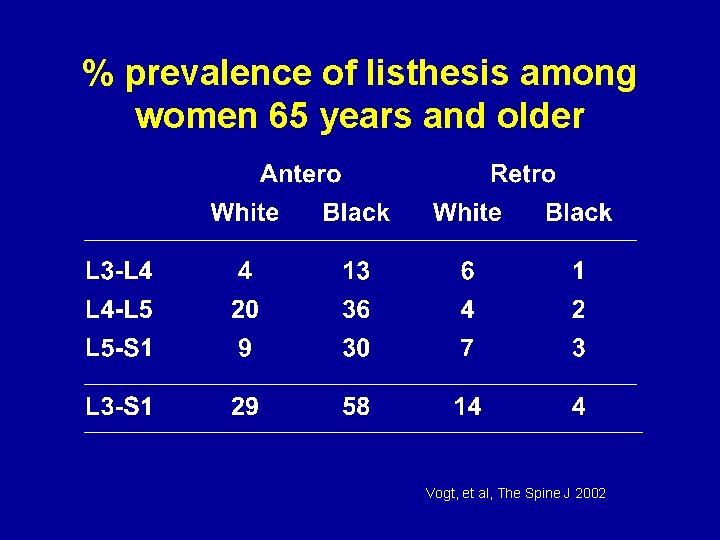
% prevalence of listhesis among women 65 years and older Vogt, et al, The Spine J 2002
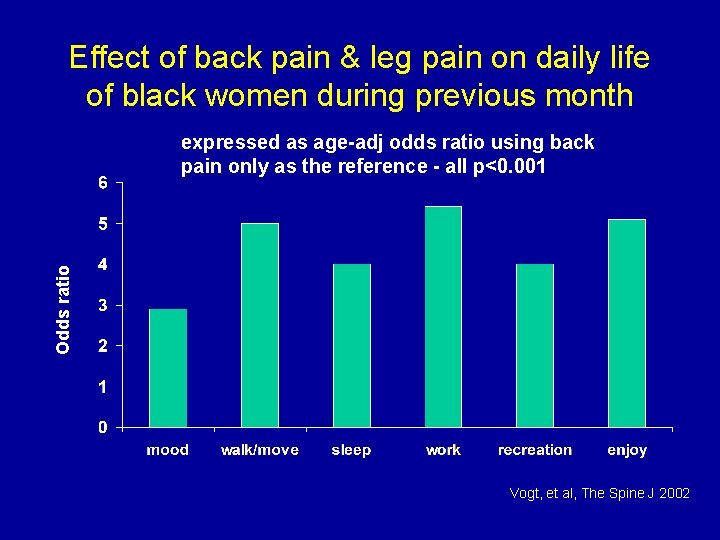
Effect of back pain & leg pain on daily life of black women during previous month Odds ratio expressed as age-adj odds ratio using back pain only as the reference - all p<0. 001 Vogt, et al, The Spine J 2002
PREVENTION Because most people experience LBP during their lifetime, the distinction between primary and secondary prevention is blurred. • which interventions can prevent occurrence of LBP? • which interventions can prevent development of chronic LBP?
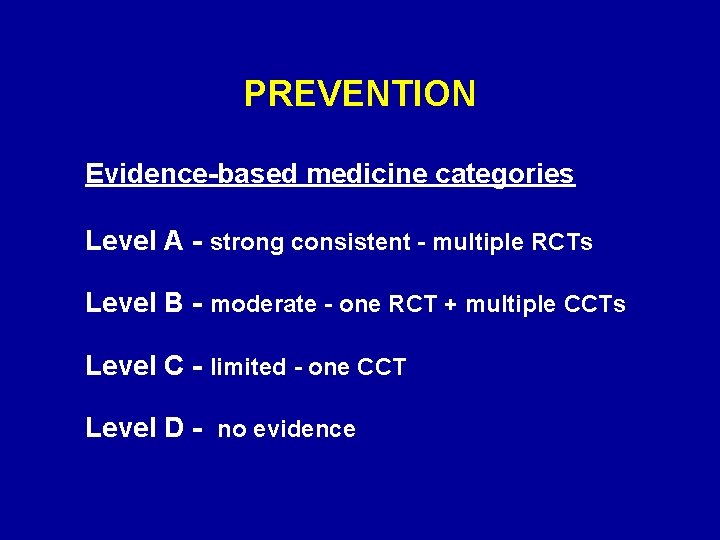
PREVENTION Evidence-based medicine categories Level A - strong consistent - multiple RCTs Level B - moderate - one RCT + multiple CCTs Level C - limited - one CCT Level D - no evidence
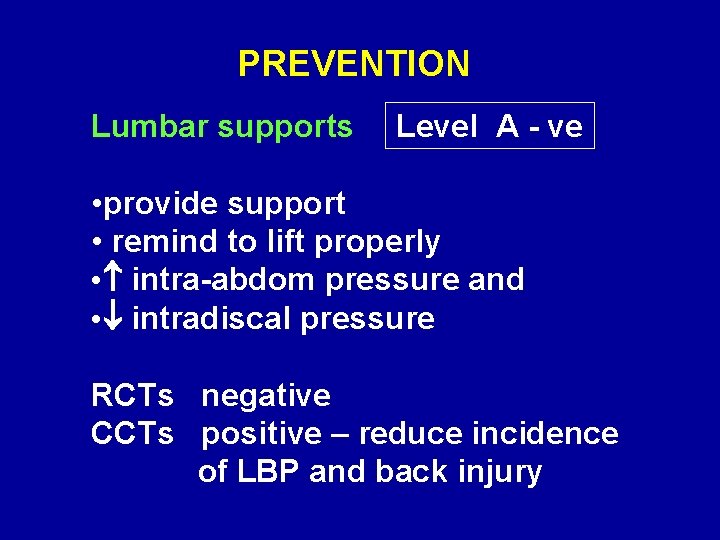
PREVENTION Lumbar supports Level A - ve • provide support • remind to lift properly • intra-abdom pressure and • intradiscal pressure RCTs negative CCTs positive – reduce incidence of LBP and back injury
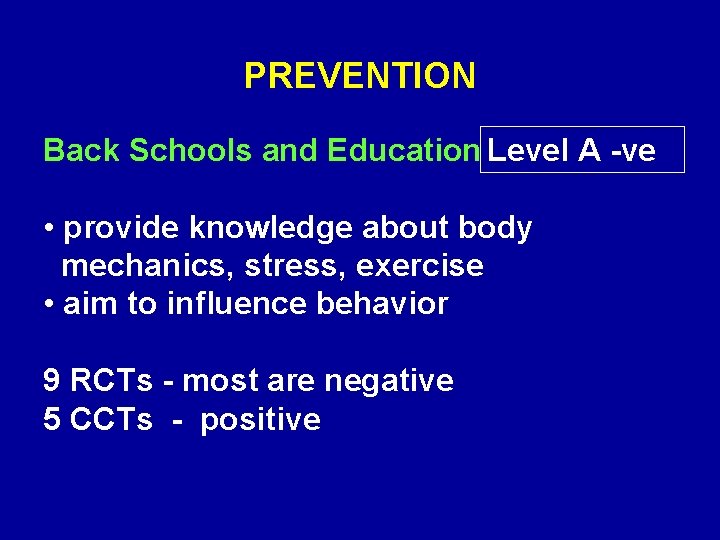
PREVENTION Back Schools and Education Level A -ve • provide knowledge about body mechanics, stress, exercise • aim to influence behavior 9 RCTs - most are negative 5 CCTs - positive
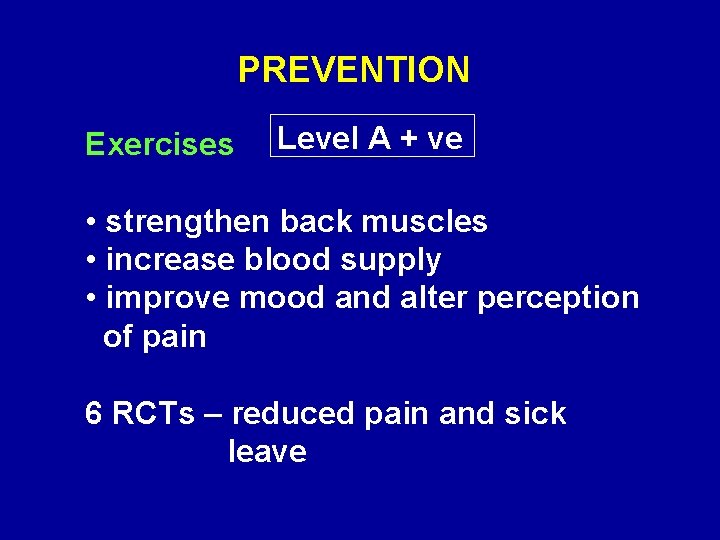
PREVENTION Exercises Level A + ve • strengthen back muscles • increase blood supply • improve mood and alter perception of pain 6 RCTs – reduced pain and sick leave
PREVENTION Ergonomics Level D - ve • job related interventions No RCTs or CCTs
PREVENTION Risk Factor Modification Level D - ve • individual (weight, strength, smoking) • biomechanical (lifting, posture) • psychosocial (job control, job dissatisfaction, depression) No RCTs or CCTs
Review of 47 epidemiologic studies concluded that smoking may be a ‘weak risk indicator and not a cause of low back pain’ Le -Bouef-Yde Spine 1999 Smoking may have a systemic effect on the musculoskeletal system - associated with generalized pain. Biological basis unknown - neuroendocrine effect?
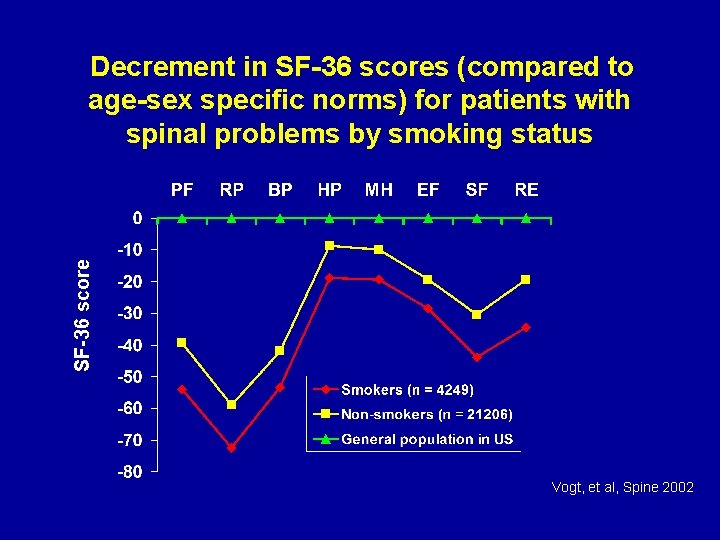
SF-36 score Decrement in SF-36 scores (compared to age-sex specific norms) for patients with spinal problems by smoking status Vogt, et al, Spine 2002
PREVENTION Currently only exercise seems to be helpful in prevention of LBP. Consistent evidence – Level A. Linton, van Tulder, Spine 2001
PREVENTION Why the disappointing results? • small studies, low power, short follow-up, variation in intervention, varying outcome • natural course of back pain, hard to define and categorize, multi-factorial causation • single modal programs studied mostly, maybe multi-dimensional approach needed • timing, compliance
- Slides: 32