Patent Ductus Arteriosus Incidence of PDA l Closure

- Slides: 13

Patent Ductus Arteriosus
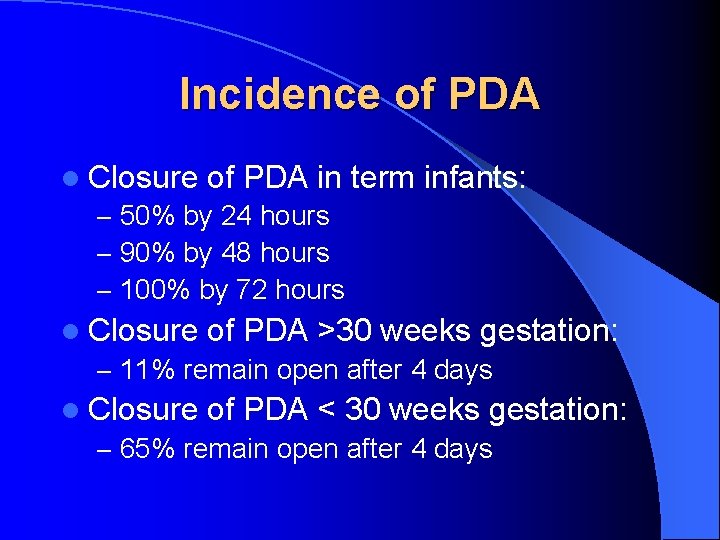
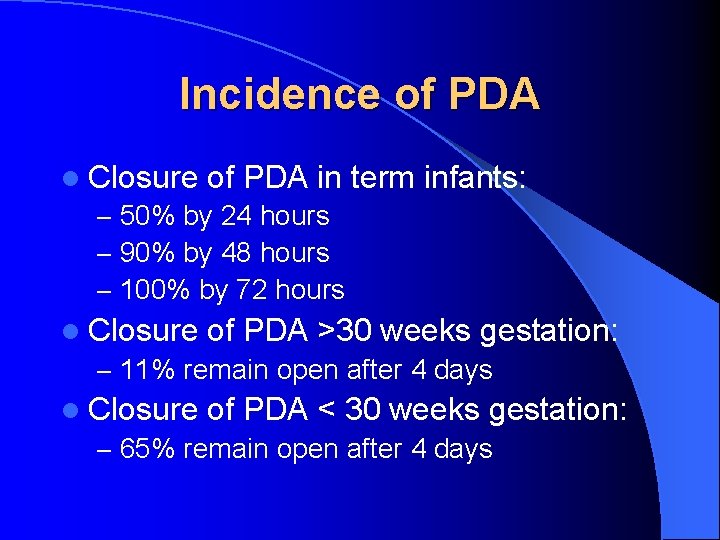
Incidence of PDA l Closure of PDA in term – 50% by 24 hours – 90% by 48 hours – 100% by 72 hours infants: l Closure of PDA >30 weeks gestation: – 11% remain open after 4 days l Closure of PDA < 30 weeks gestation: – 65% remain open after 4 days
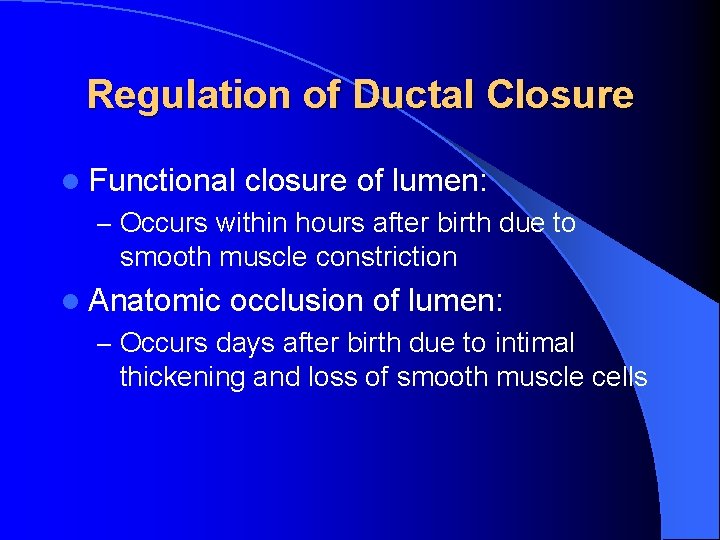
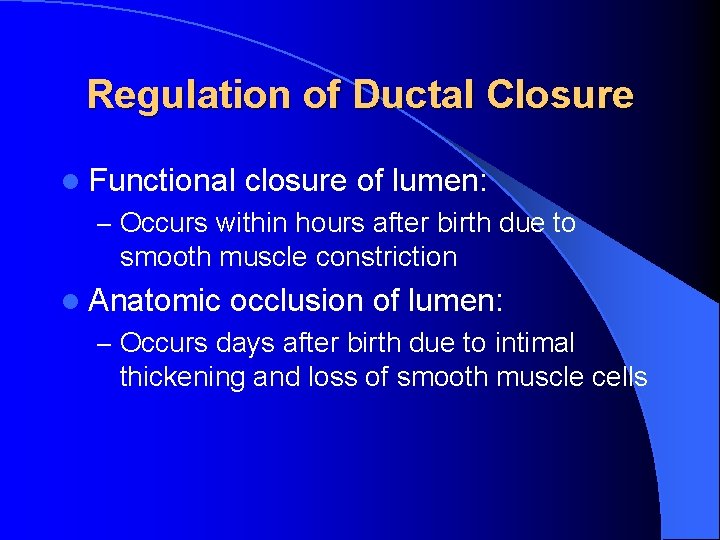
Regulation of Ductal Closure l Functional closure of lumen: – Occurs within hours after birth due to smooth muscle constriction l Anatomic occlusion of lumen: – Occurs days after birth due to intimal thickening and loss of smooth muscle cells
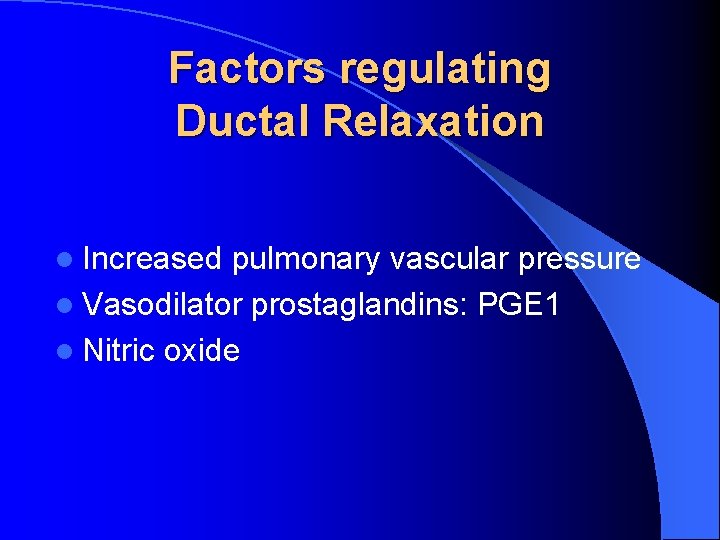
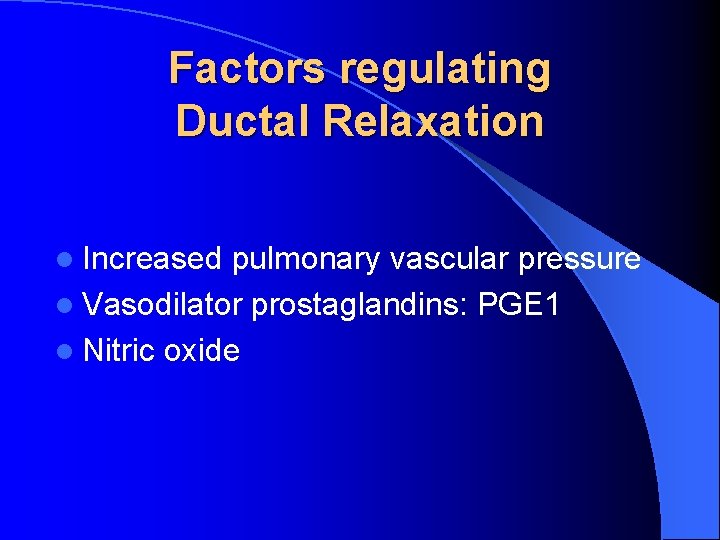
Factors regulating Ductal Relaxation l Increased pulmonary vascular pressure l Vasodilator prostaglandins: PGE 1 l Nitric oxide
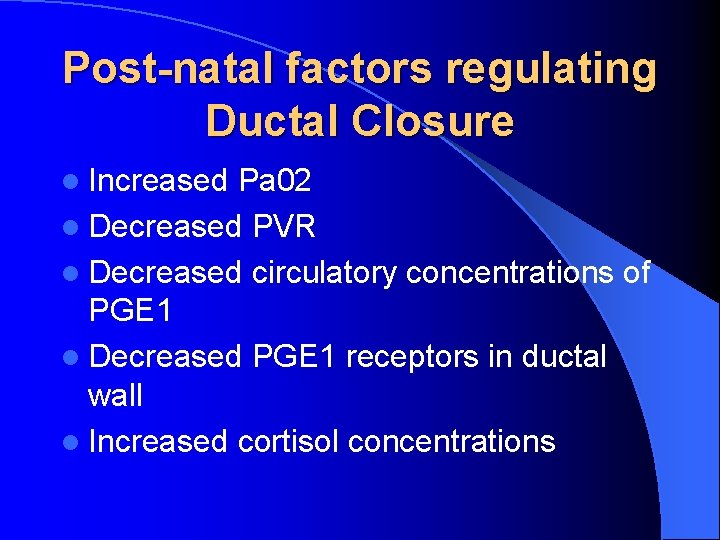
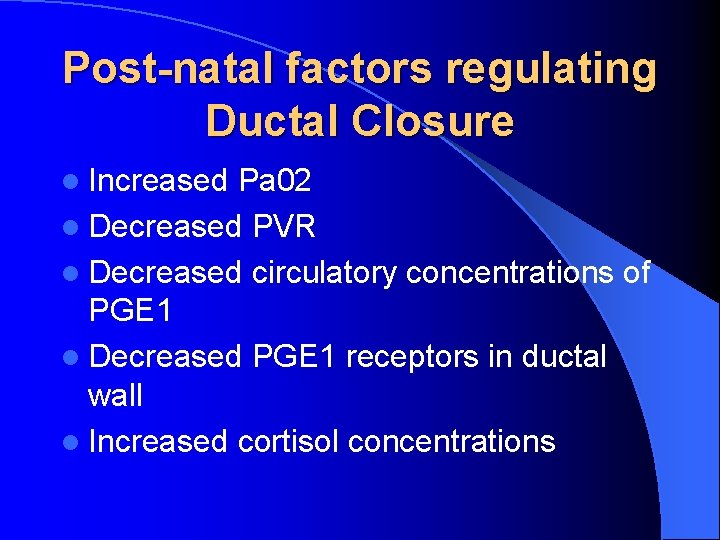
Post-natal factors regulating Ductal Closure l Increased Pa 02 l Decreased PVR l Decreased circulatory concentrations of PGE 1 l Decreased PGE 1 receptors in ductal wall l Increased cortisol concentrations
Factors Restricting Ductal Closure in Preemies l Decreased intrinsic smooth muscle tone l Higher circulating PGE 1 concentrations l Increased sensitivity to vasodilatory effects of PGE 1 and NO
Hemodynamic and Pulmonary Consequences of PDA l Left to right shunt: increased pulmonary venous pressure, increased pulmonary edema l Decreased blood flow to skin, bone, muscle, GI tract, and kidneys l Rapid increase in pulmonary blood flow leading to pulmonary hemorrhage (risk of surfactant administration)
Treatment l Indocin prophlaxis l Treatment indocin: closure in 85% patients l Surgical ligation
Complications of PDA l BPD l NEC l Feeding intolerance
Risks of Indocin Use l Decreased mesenteric, renal, and cerebral blood flow l Oliguria, dilutional hyponatremia l Isolated intestinal perforation (increased risk when combined with postnatal steroids) l NEC?
Contraindications to Indocin Use l NEC l Renal failure l Bleeding disorders and severe thrombocytopenia l Hemodynamically insignificant PDA
Clinical diagnosis l Systolic heart murmur, though may be absent l Hyperdynamic precordium l Bounding peripheral pulses l Wide pulse pressure l Worsening respiratory status
Indocin Prophylaxis l Decreases symptomatic PDA and the need for surgical ligation l Decreases Grade III and IV IVH l No change in short or long term mortality l No difference in rates of NEC l Long term neurodevelopmental outcome is not adversely affected