Patellar Dislocation What is Patellar Dislocation The cause

- Slides: 8
Patellar Dislocation
What is Patellar Dislocation? The cause: • Patients with normal anatomy and had a traumatic event. -OR • Patients with predisposing anatomy and a history of subluxation without a traumatic event.
How to Diagnosis: Refer for Imaging • Although some patellar dislocations will be obvious a complete evaluation of the suspected patellar dislocation must include basic imaging. • An MRI is particularly useful in order to determine the best intervention strategy by exposing the affected tissues. In the presence of osteochondral injury, loose bodies, or NPFL injury may point the surgeon toward a operative treatment.
Nonoperative treatment • Traditionally, implication for 3 to 6 weeks. • Today treatment with early mobilization • However, Lerason and Leuridsen predicted the chance of recurrence with 6 years is 53% after following 79 acute patellar dislocations. Other studies show similar results.
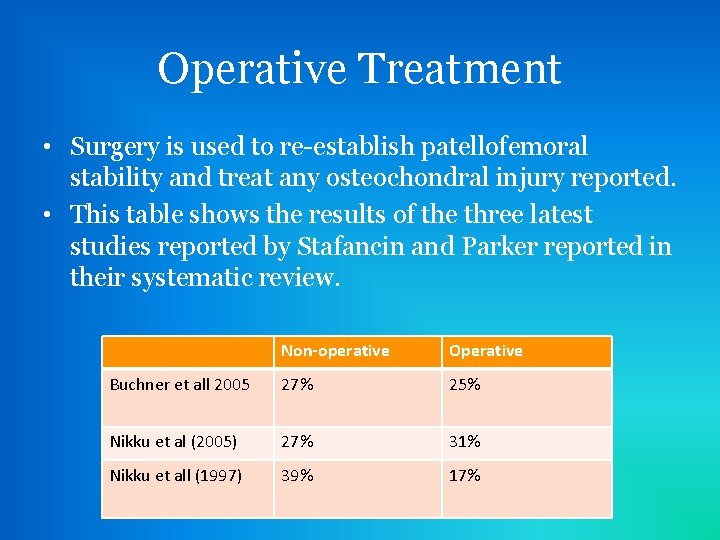
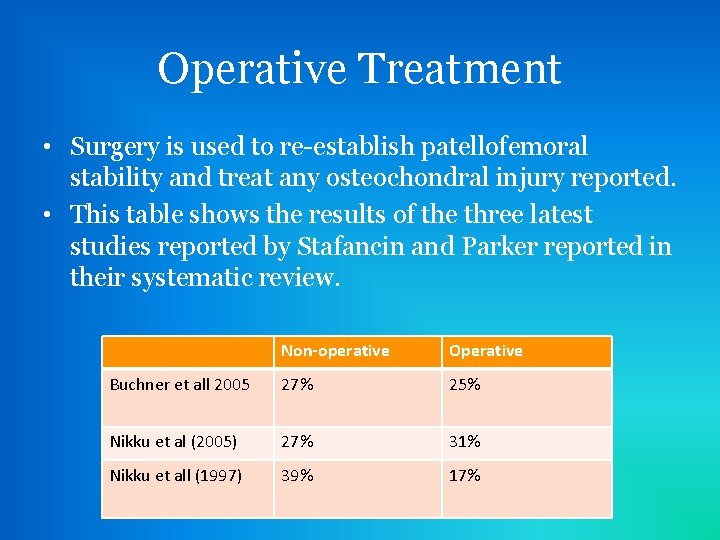
Operative Treatment • Surgery is used to re-establish patellofemoral stability and treat any osteochondral injury reported. • This table shows the results of the three latest studies reported by Stafancin and Parker reported in their systematic review. Non-operative Operative Buchner et all 2005 27% 25% Nikku et al (2005) 27% 31% Nikku et all (1997) 39% 17%

Treatment Post Surgery • Structured rehabilitation is essential for optimal recovery despite treatment method. • An individualized treatment plan should be developed for each patient. • Immobilization in extension for first 10 -14 days. • Examination should include palpation for defect in the medial retinaculum. • Advance weight bearing and regain both AROM & PROM. • Start with closed chin strength training and proprioceptive exercises and advance to sport specific training.
When they can return to Play? • Subjective – No pain, swelling, or sensation of instability • Objectively – No effusion tenderness or apprehension – Full range of motion without pain – Quadriceps strength should be at least 80% of the contralateral side – Running and cutting can be performed without symptoms
Reference De. Lee: De. Lee and Drez's Orthopaedic Sports Medicine, 3 rd ed. Copyright © 2009 Saunders, An Imprint of Elsevier