Partile lever resectie gaat gepaard met een postoperatieve




- Slides: 48
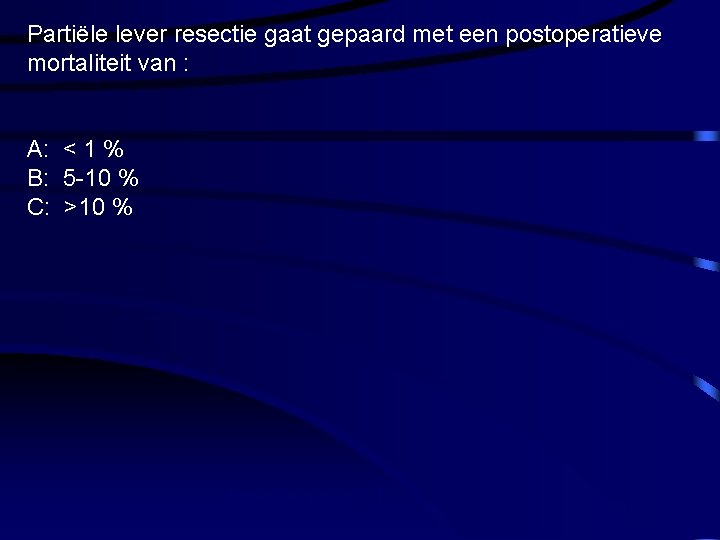
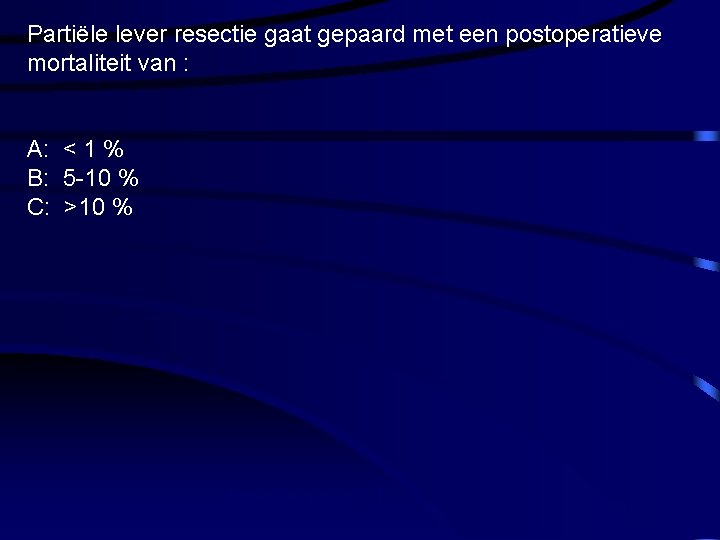
Partiële lever resectie gaat gepaard met een postoperatieve mortaliteit van : A: < 1 % B: 5 -10 % C: >10 % Hersenmetastasen CT
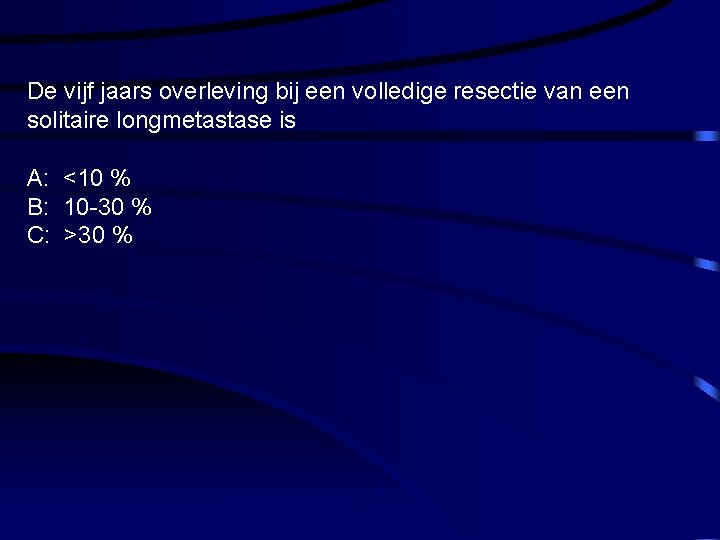
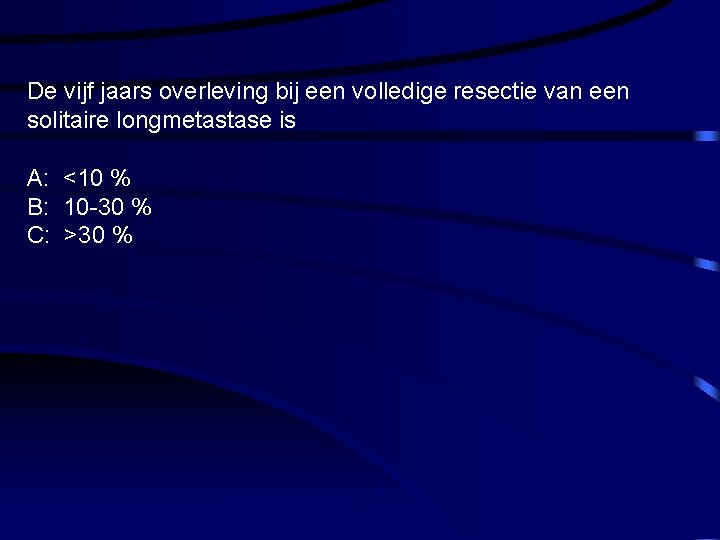
De vijf jaars overleving bij een volledige resectie van een solitaire longmetastase is A: <10 % B: 10 -30 % C: >30 % Hersenmetastasen CT
LOKALE BEHANDELING VAN DE OLIGOGEMETASTASEERDE PATIENTE Prof Herman Depypere, Dr A Dierickx, Drs C Vertriest, prof R Vandenbroecke, prof Troisy, prof Cocquyt Breast and Menopause Clinic, University Hospital, Gent, Belgium
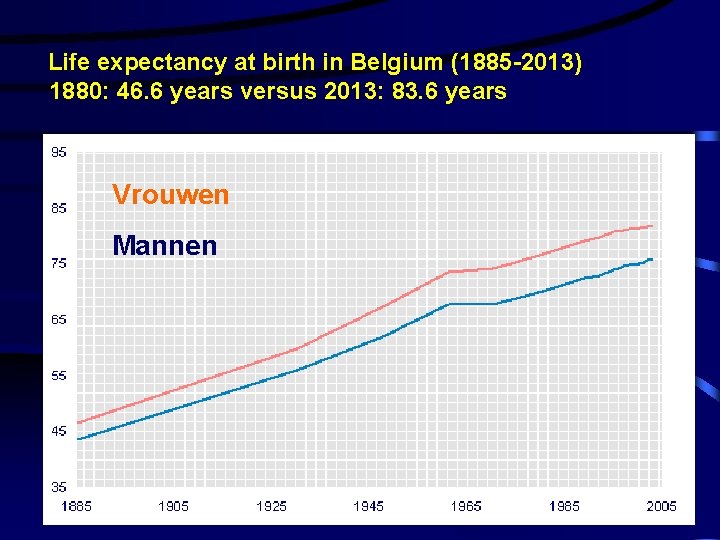
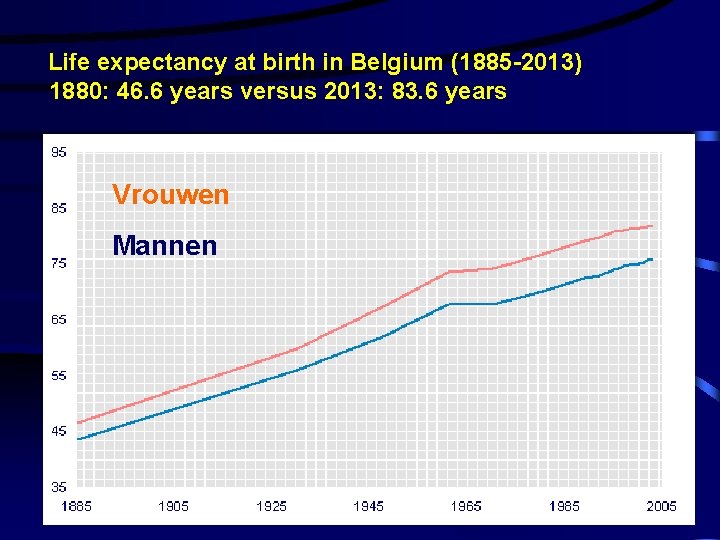
Life expectancy at birth in Belgium (1885 -2013) 1880: 46. 6 years versus 2013: 83. 6 years Vrouwen Mannen 4
biomedische les hormonen en kanker 2012 - Prof Depypere -Prof Bracke 5
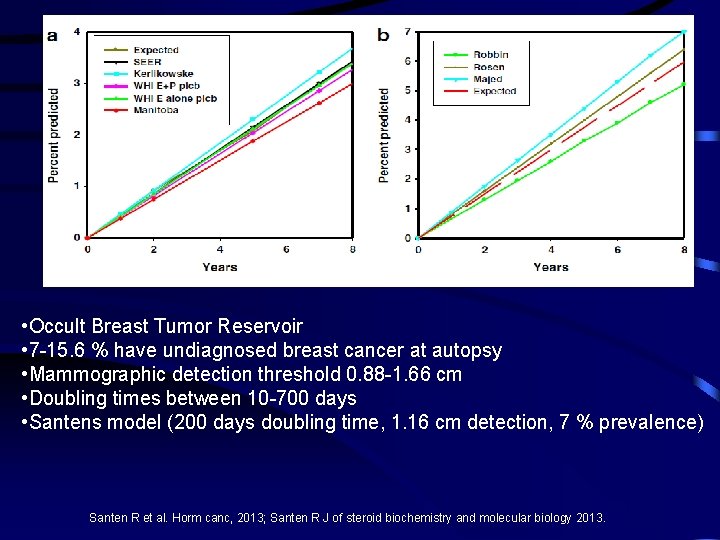
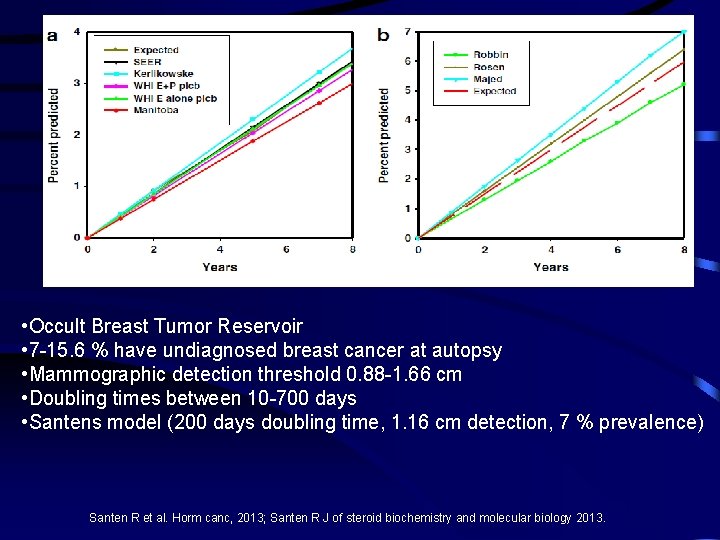
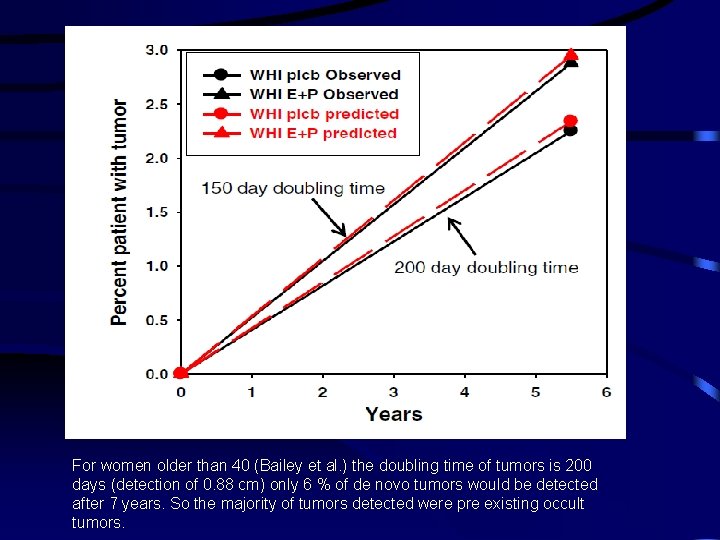
• Occult Breast Tumor Reservoir • 7 -15. 6 % have undiagnosed breast cancer at autopsy • Mammographic detection threshold 0. 88 -1. 66 cm • Doubling times between 10 -700 days • Santens model (200 days doubling time, 1. 16 cm detection, 7 % prevalence) Santen R et al. Horm canc, 2013; Santen R J of steroid biochemistry and molecular biology 2013.
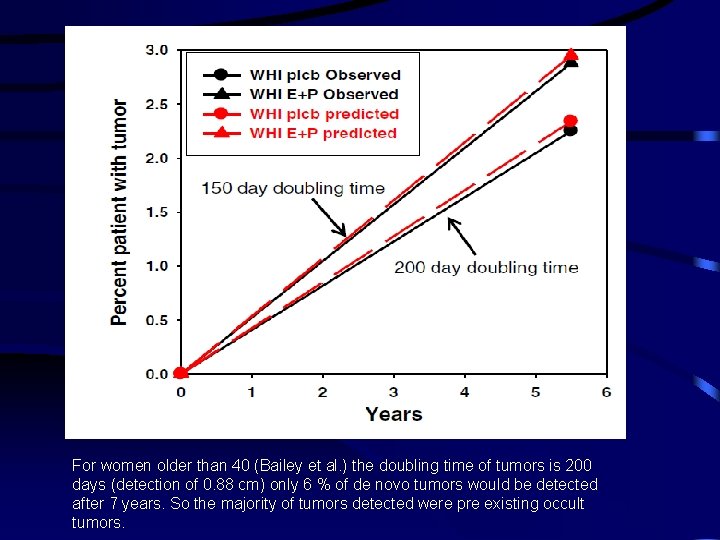
For women older than 40 (Bailey et al. ) the doubling time of tumors is 200 days (detection of 0. 88 cm) only 6 % of de novo tumors would be detected after 7 years. So the majority of tumors detected were pre existing occult tumors.
CANCER PROGRESSION Tumor/Invasion- promotor and -suppressor genes Metastasic promotor genes? early?
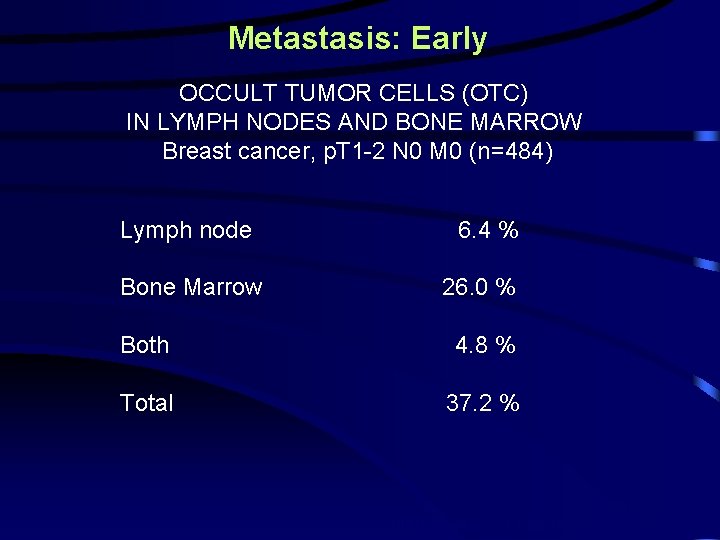
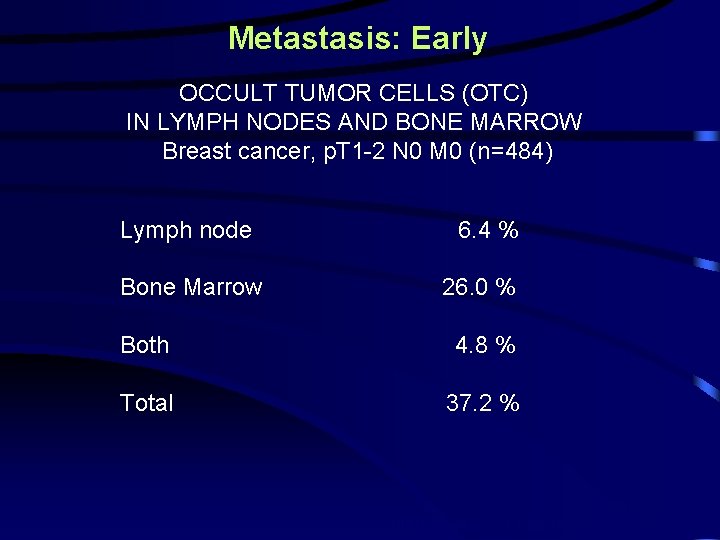
Metastasis: Early OCCULT TUMOR CELLS (OTC) IN LYMPH NODES AND BONE MARROW Breast cancer, p. T 1 -2 N 0 M 0 (n=484) Lymph node Bone Marrow 6. 4 % 26. 0 % Both 4. 8 % Total 37. 2 % Gerber et al. , J Clin Oncol 19: 960. 2001
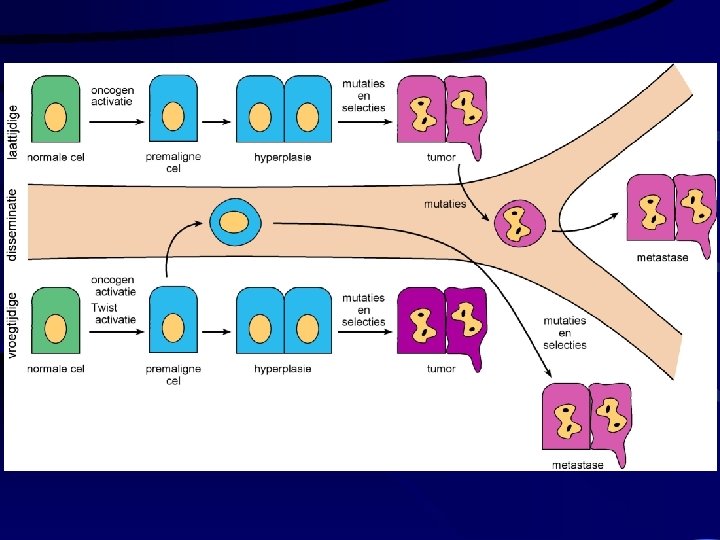
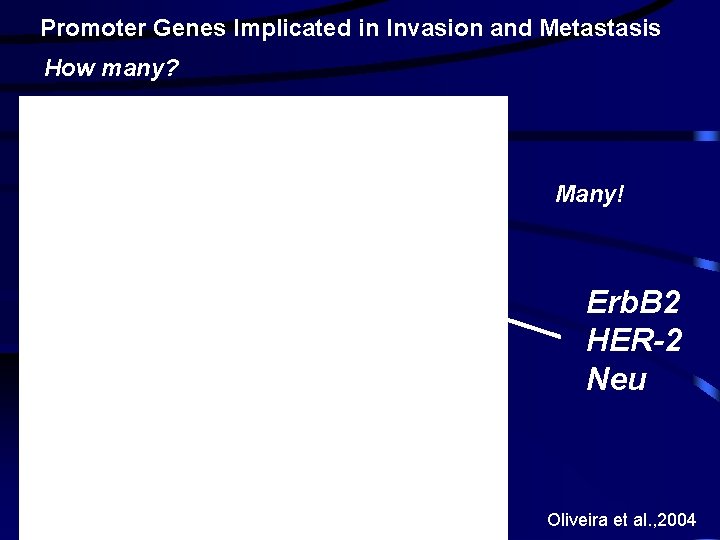
Promoter Genes Implicated in Invasion and Metastasis How many? Many! Erb. B 2 HER-2 Neu Oliveira et al. , 2004
1991
2005
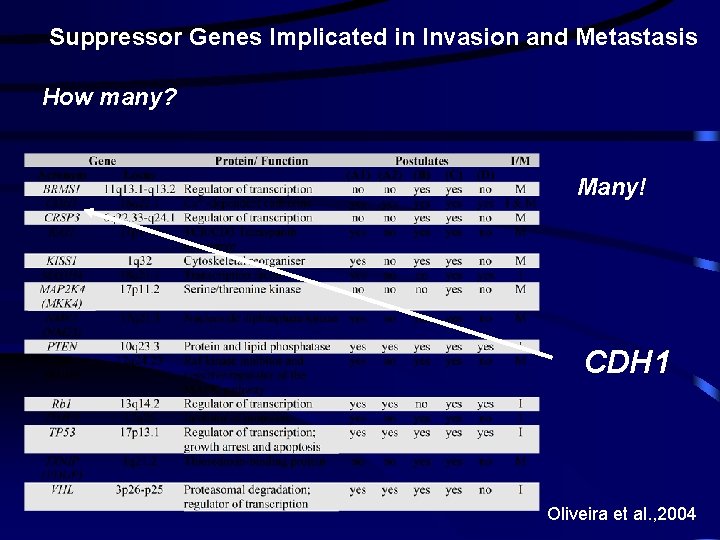
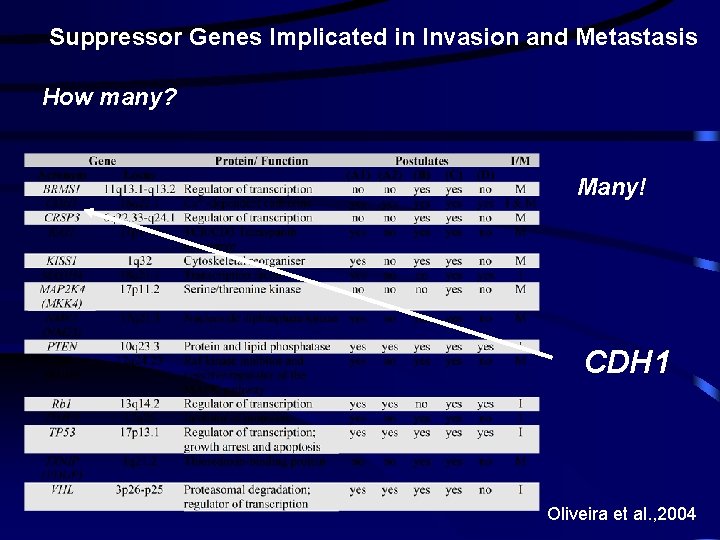
Suppressor Genes Implicated in Invasion and Metastasis How many? Many! CDH 1 Oliveira et al. , 2004
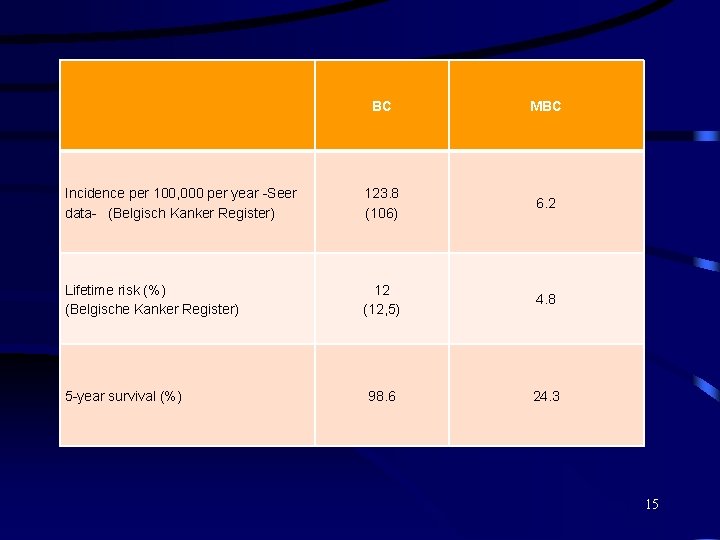
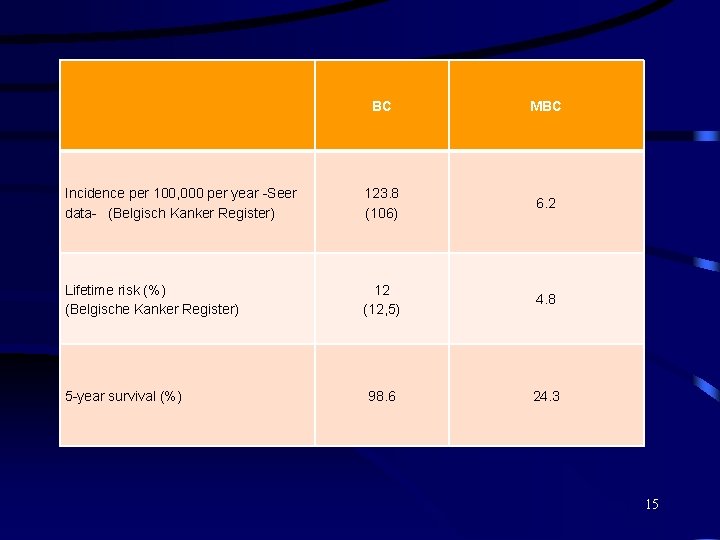
BC MBC Incidence per 100, 000 per year -Seer data- (Belgisch Kanker Register) 123. 8 (106) 6. 2 Lifetime risk (%) (Belgische Kanker Register) 12 (12, 5) 4. 8 98. 6 24. 3 5 -year survival (%) 15

MBC up till now considered as uncurable disease and treated with chemo/hormonal/immuno/radiotherapy. Aim palliation and prolongation of live. Surgery was used for palliation in symptomatic patients with bone or brain metastasis or to prevent fractures in bonemetastasis. Metastasectomy has been successfully in patients with colorectal cancer, osteosarcoma, renalcel cancer, melanoma and germcel cancer.
Currently, candidates for resection/treatment of metastatic locations are: 1. Patients with oligometastasis 2. Patients with metastasis that respond well on systemic therapy 3. Resectable location/tissue
Livermetastasis 1. 2. 3. 4. Echography ct scan/pet scan Mri biopsy

Echografie lever
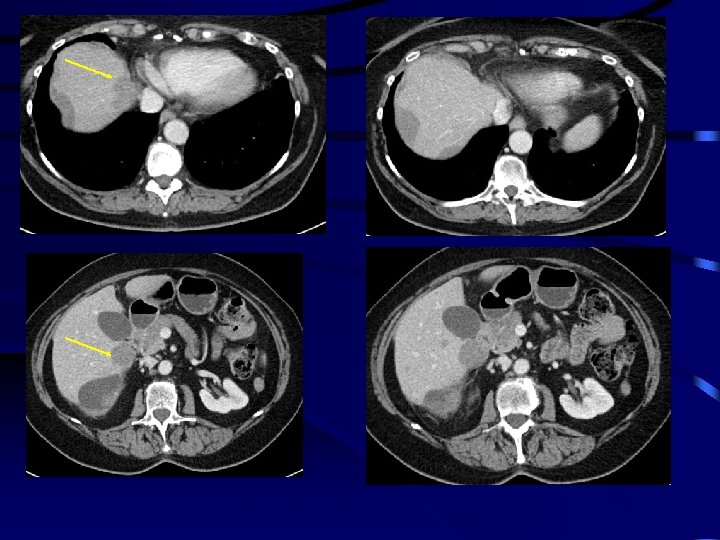
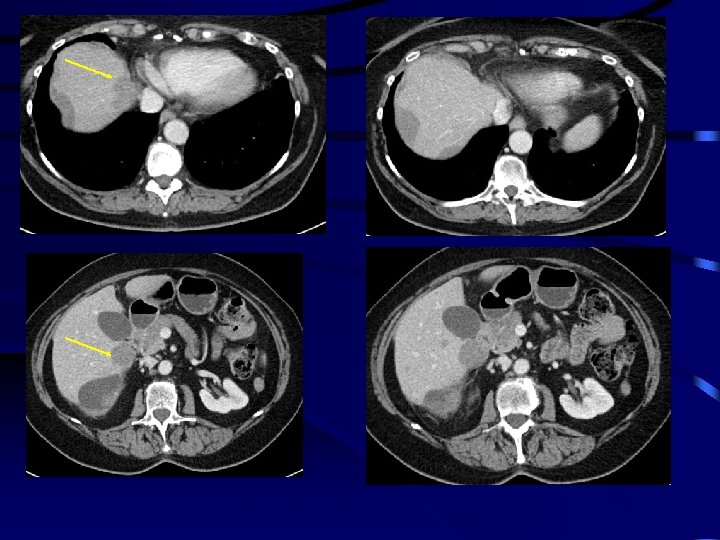
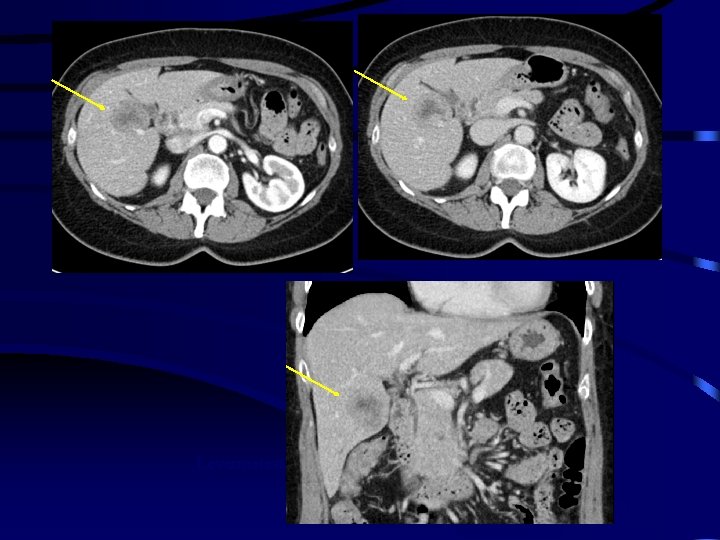
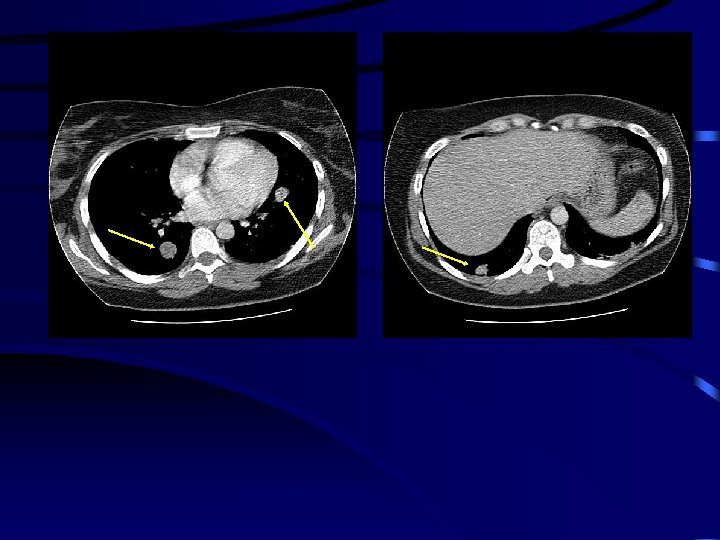
Levermetastasen CT
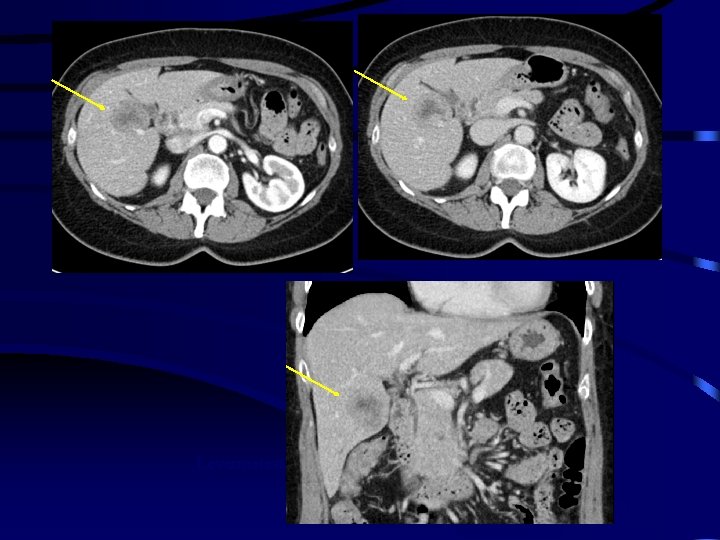
Levermetastase van mammaca
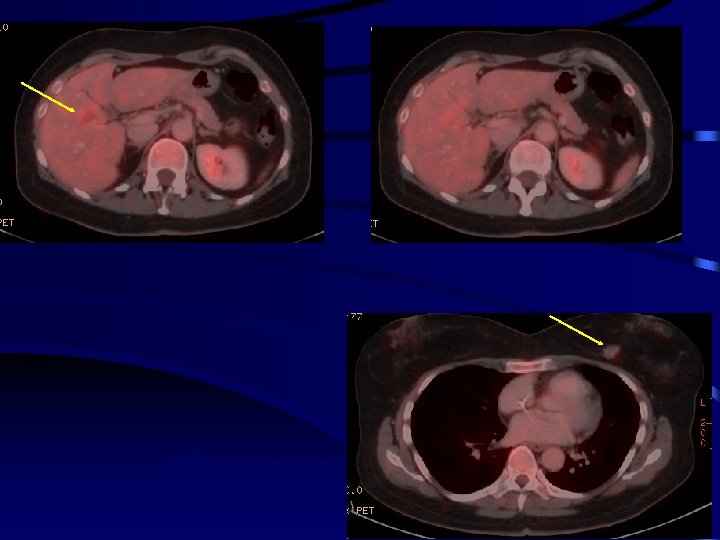
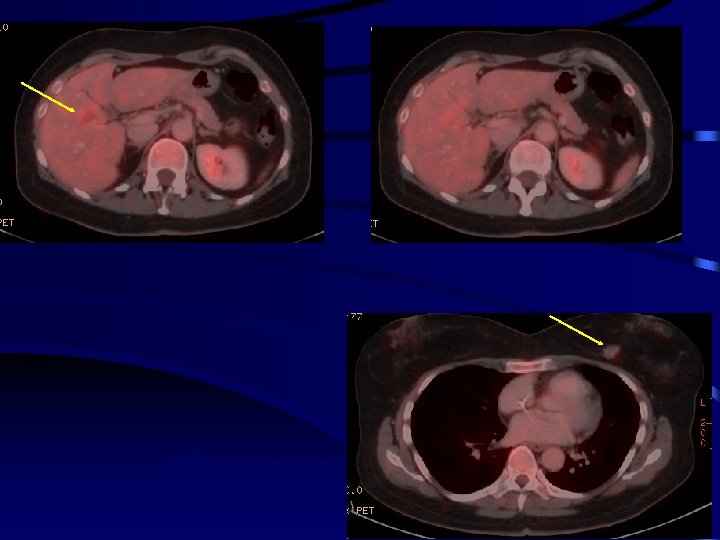
PETCT borsttumor en levermetastase
Studies report a median survival of MBC patients after liver metastasectomy between 27 and 63 months. Postoperative mortality is 0 %. Ideal candidate for resection of livermetastase(s)s of breast cancer: 1. 2. 3. 4. 5. 6. 7. 8. Young age Hormone sensitive breast cancer DFI ≥ 1 year Good preoperative respons on chemotherapy < 4 liver metastases Normal liverfunction tests no extrahepatic disease (except bone metastases) RO resection
lungmetastasis Rx thorax Ct scan biopsy
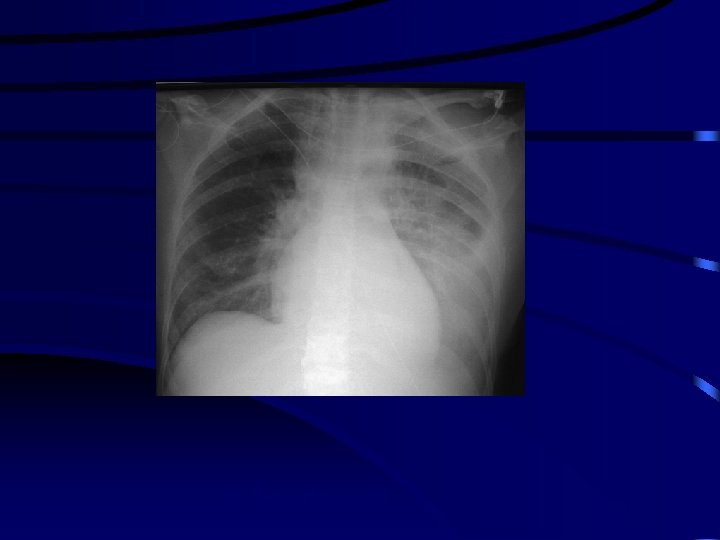
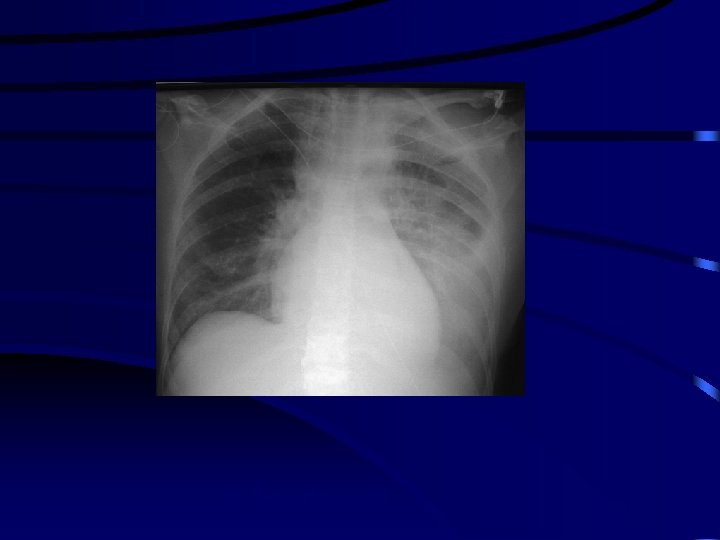
RX thorax pleuravocht
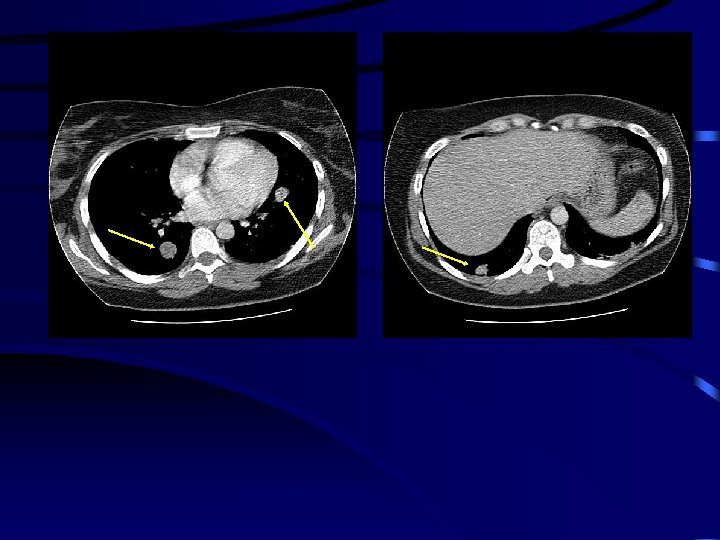
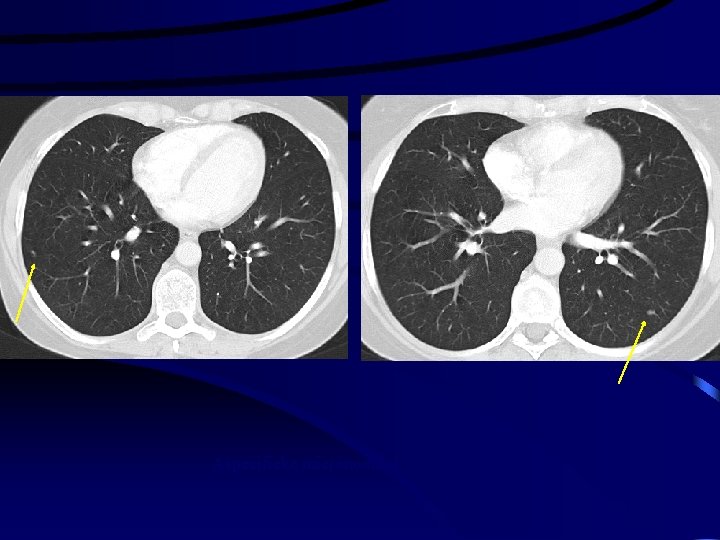
CT longmetastasen
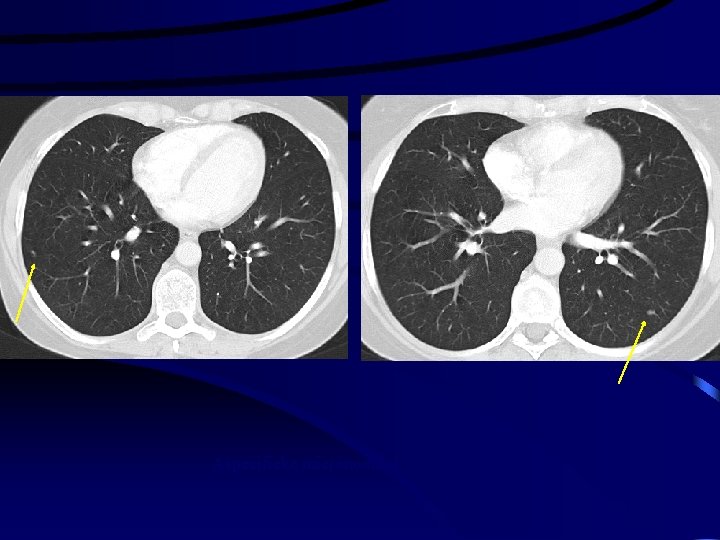
Aspecifieke micronodules
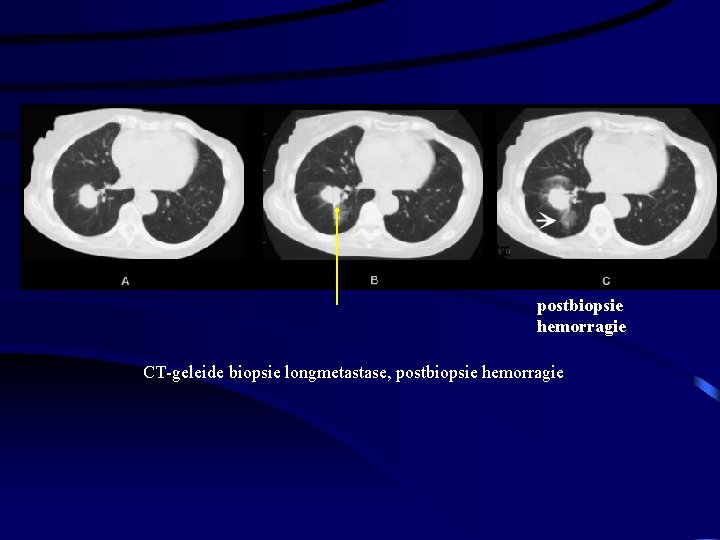
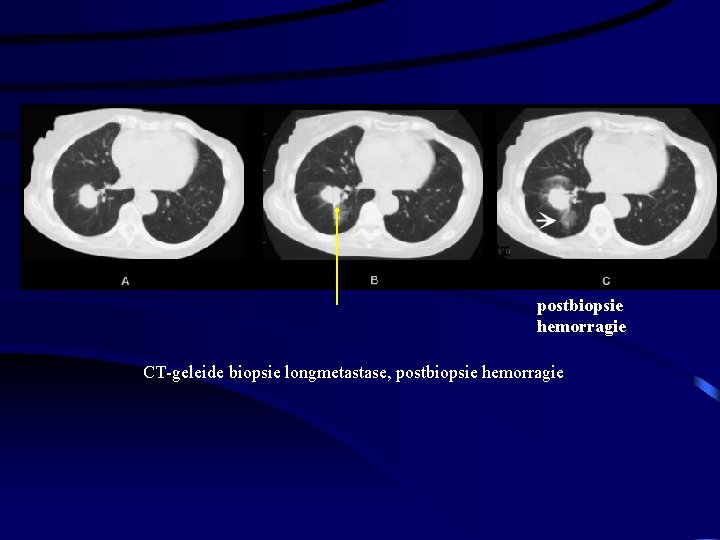
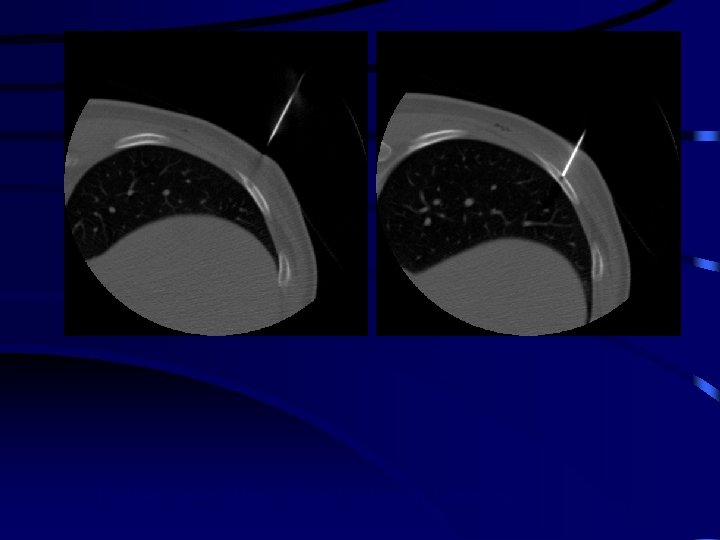
postbiopsie hemorragie CT-geleide biopsie longmetastase, postbiopsie hemorragie
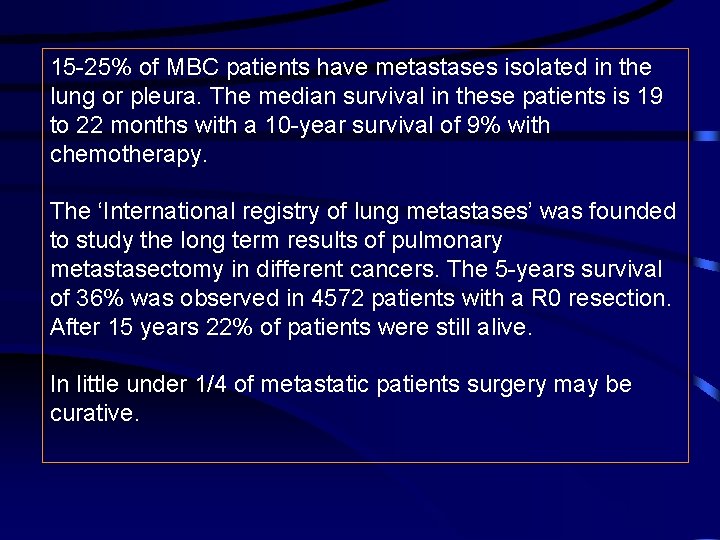
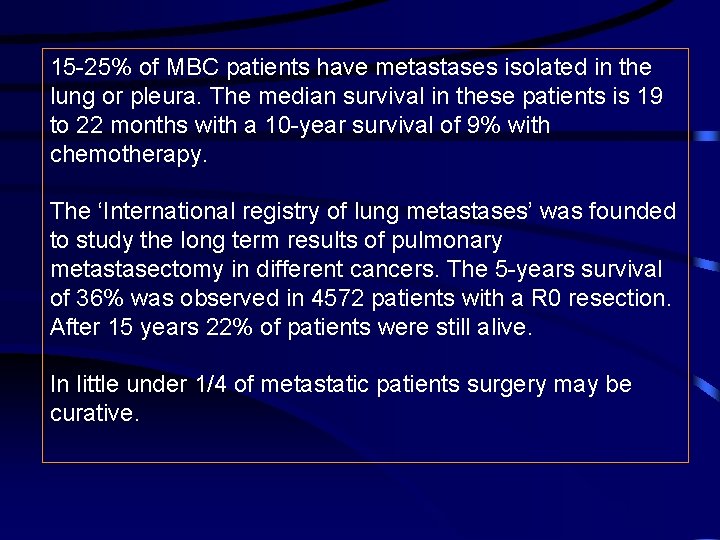
15 -25% of MBC patients have metastases isolated in the lung or pleura. The median survival in these patients is 19 to 22 months with a 10 -year survival of 9% with chemotherapy. The ‘International registry of lung metastases’ was founded to study the long term results of pulmonary metastasectomy in different cancers. The 5 -years survival of 36% was observed in 4572 patients with a R 0 resection. After 15 years 22% of patients were still alive. In little under 1/4 of metastatic patients surgery may be curative.
Ideal candidates for resection of longmetastases in breast cancer are: 1. 2. 3. 4. DFI≥ 36 months R 0 resection number (<2) Size (<3 cm)
Meimarakis et al. (2013) performed a prospective trial in 81 MBC patients who underwent a ressection of longmetastasis. In their study other factors were included: size of metastase (mediane survival if metastase <3 cm: 103. 4 months versus 39. 1 months if >3 cm) hormone receptor positivity (median survival if positive 127 months versus 27 months if negative Reported mortality after resection of lung metastasis is 01% , the morbidity is 0 -13% in different studies. Hersenmetastasen CT
In instances of recurrence: resect again
Bone metastases Palliative setting : main indication Avoid fracture Releave of pain Survival influence Cure ?
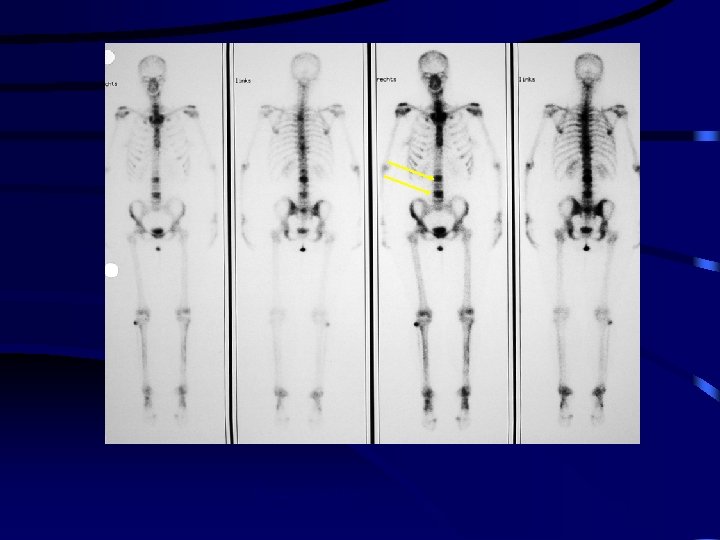
Bone metastasis BONE SCAN RX BONE MR
Botmetastasen van ovariumcarcinoom
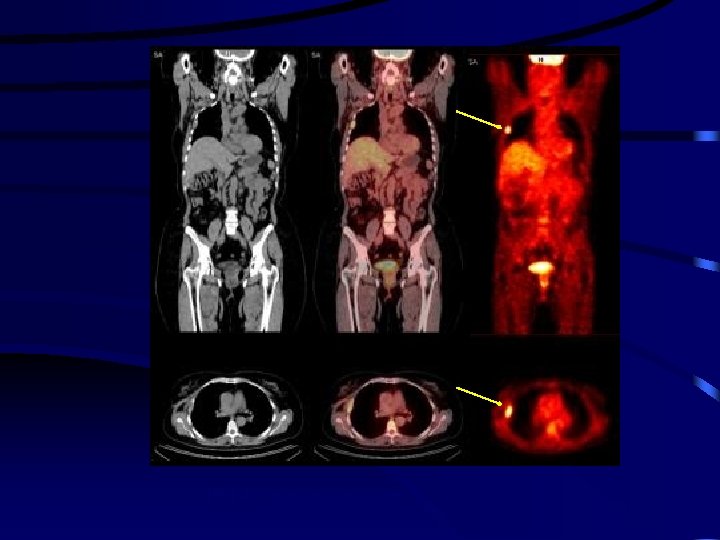
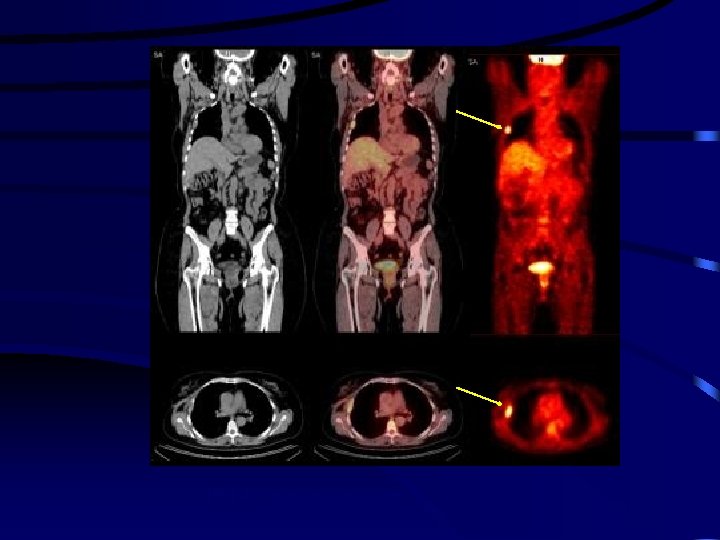
PET-CT mammacarcinoom

RX en MR botmetastasen
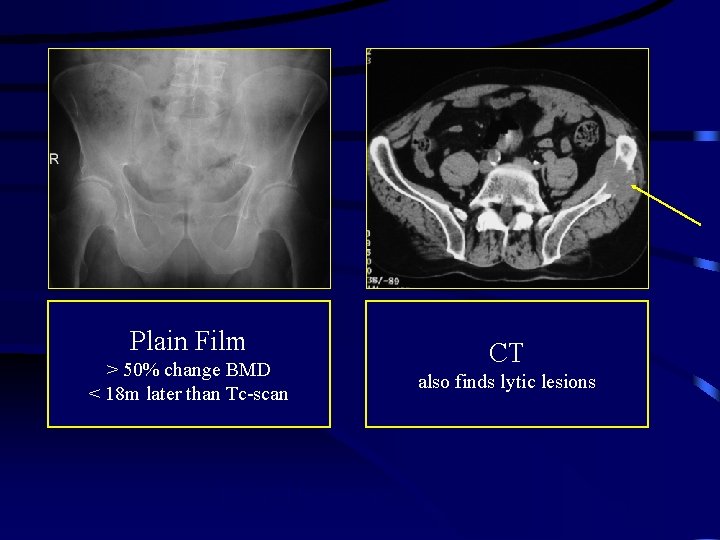
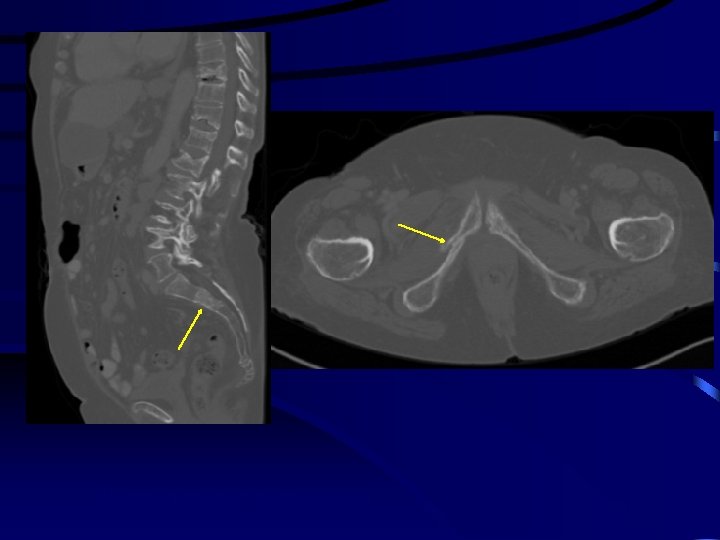
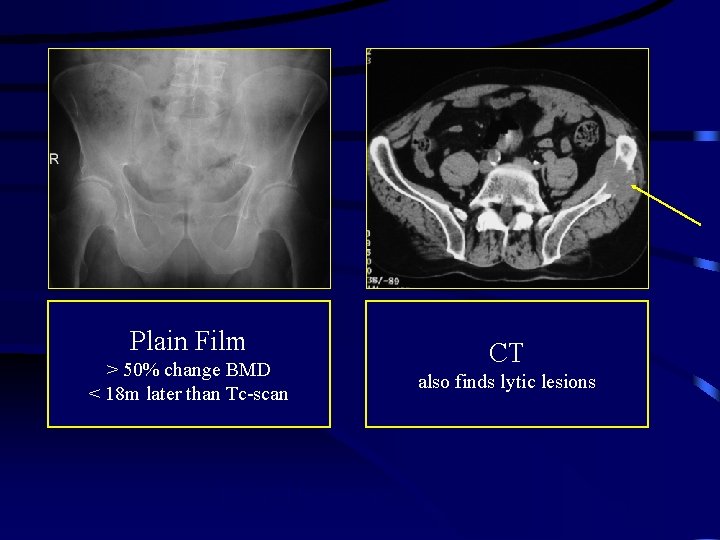
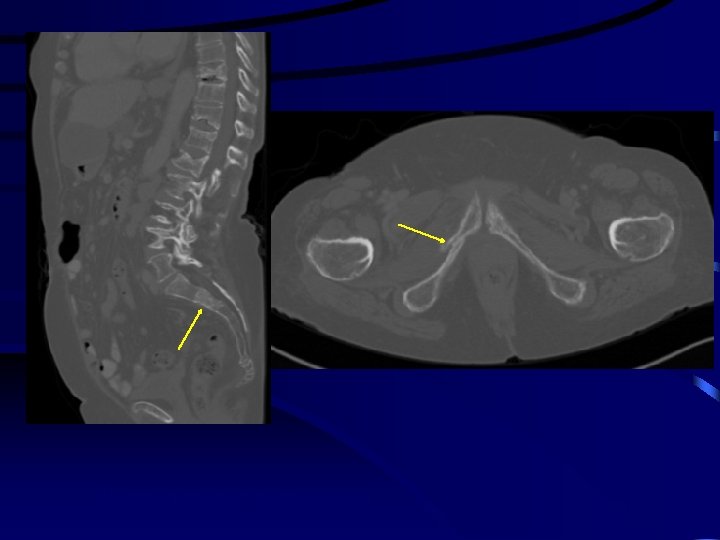
Plain Film > 50% change BMD < 18 m later than Tc-scan RX en CT botmetastase CT also finds lytic lesions
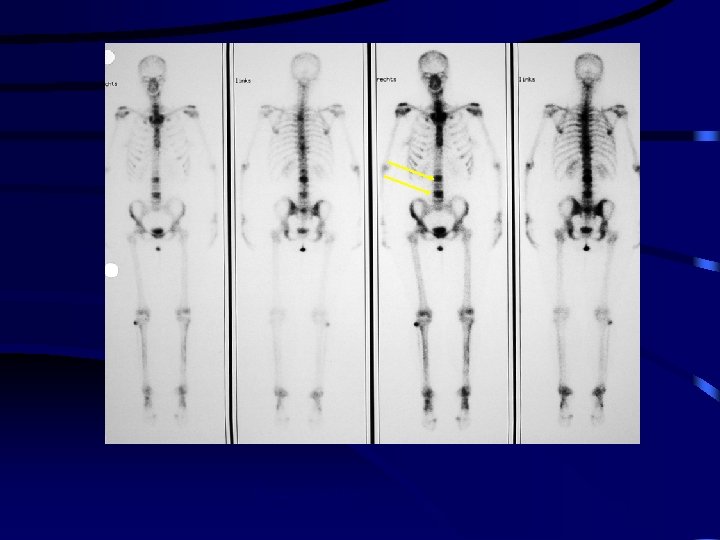
Botscintigrafie
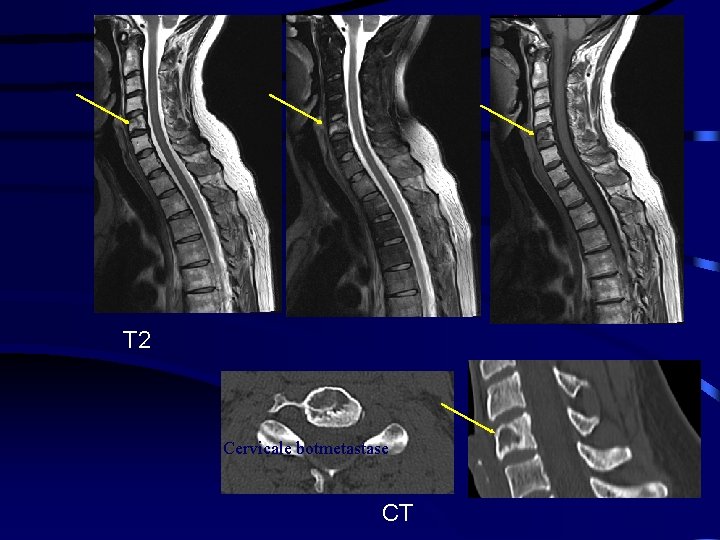
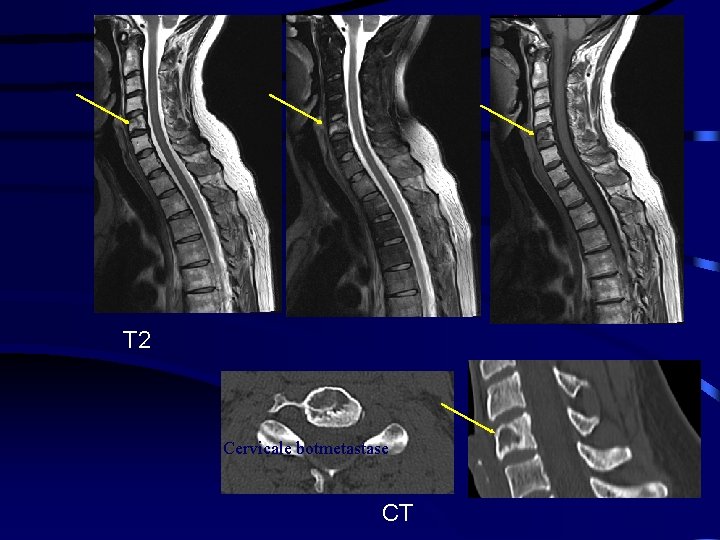
T 2 Cervicale botmetastase CT
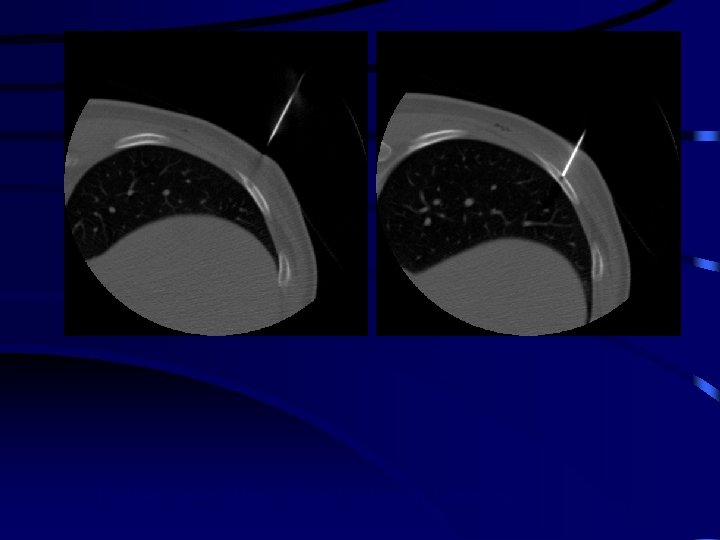
CT geleide biopsie ribletsel, hotspot op botscan, bij mammaca

CT-geleide biopsie lytisch botletsel pathologische fractuur
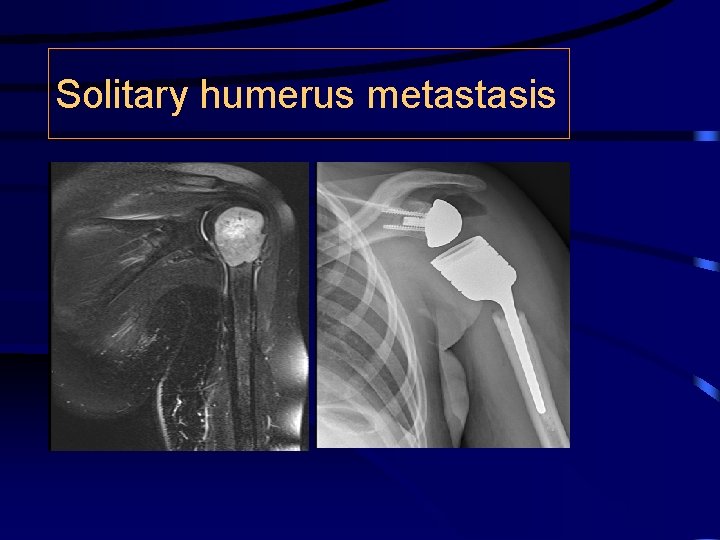
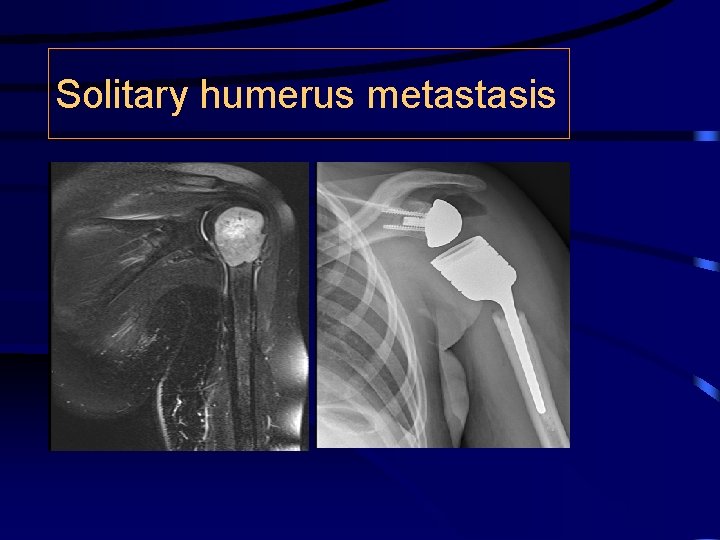
Solitary humerus metastasis
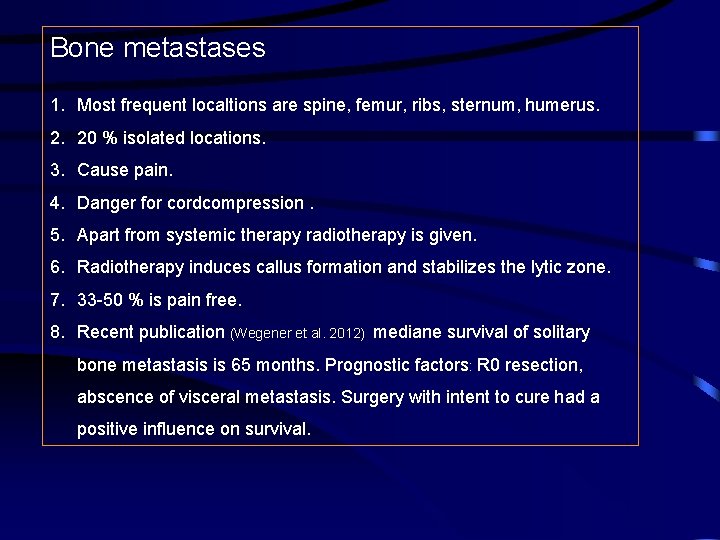
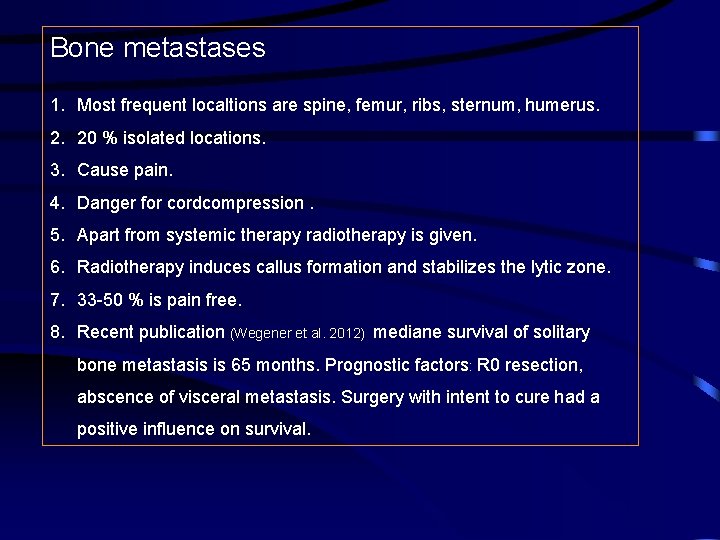
Bone metastases 1. Most frequent localtions are spine, femur, ribs, sternum, humerus. 2. 20 % isolated locations. 3. Cause pain. 4. Danger for cordcompression. 5. Apart from systemic therapy radiotherapy is given. 6. Radiotherapy induces callus formation and stabilizes the lytic zone. 7. 33 -50 % is pain free. 8. Recent publication (Wegener et al. 2012) mediane survival of solitary bone metastasis is 65 months. Prognostic factors: R 0 resection, abscence of visceral metastasis. Surgery with intent to cure had a positive influence on survival.
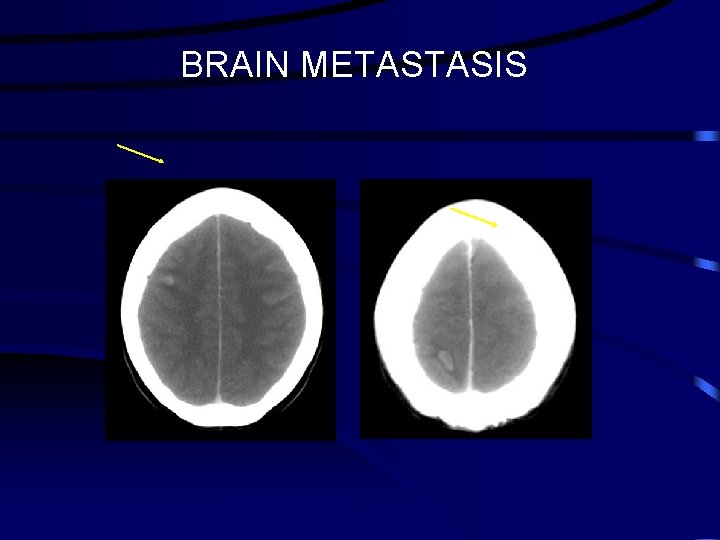
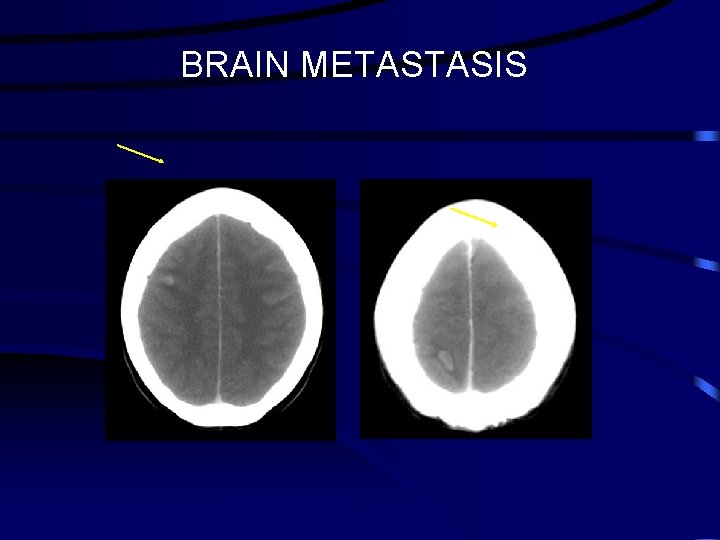
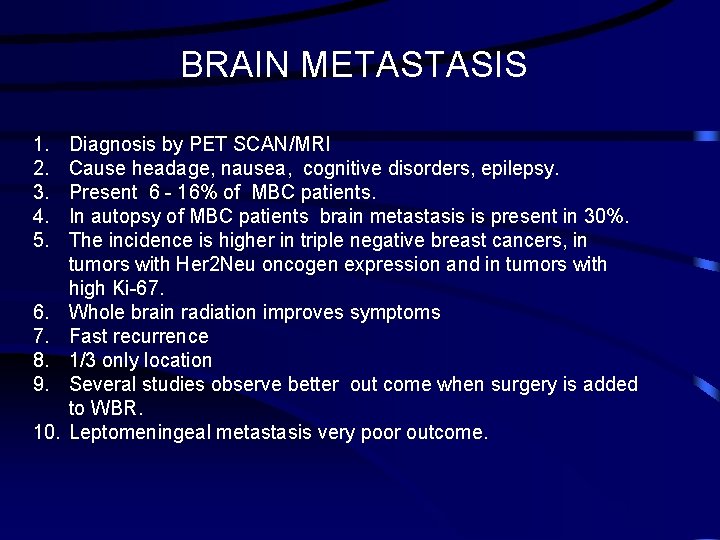
BRAIN METASTASIS Hersenmetastasen CT
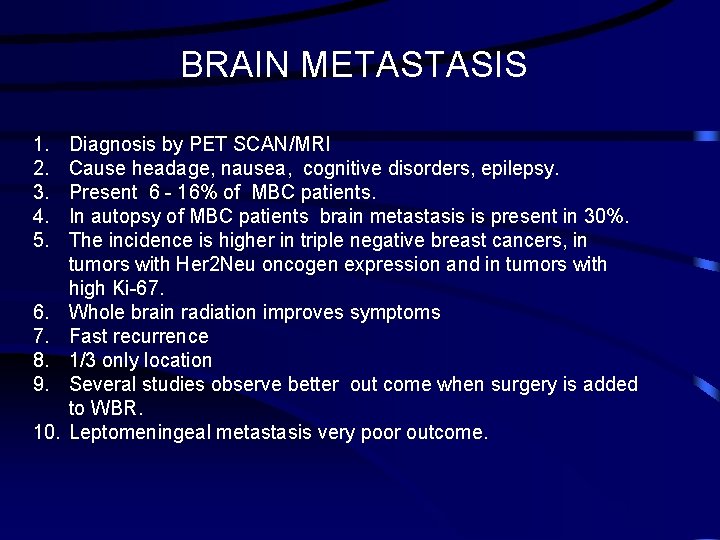
BRAIN METASTASIS 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Diagnosis by PET SCAN/MRI Cause headage, nausea, cognitive disorders, epilepsy. Present 6 - 16% of MBC patients. In autopsy of MBC patients brain metastasis is present in 30%. The incidence is higher in triple negative breast cancers, in tumors with Her 2 Neu oncogen expression and in tumors with high Ki-67. Whole brain radiation improves symptoms Fast recurrence 1/3 only location Several studies observe better out come when surgery is added to WBR. Leptomeningeal metastasis very poor outcome.
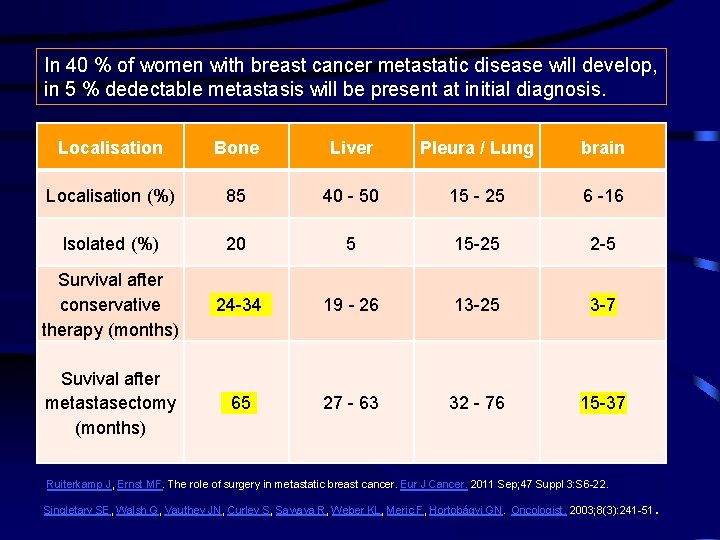
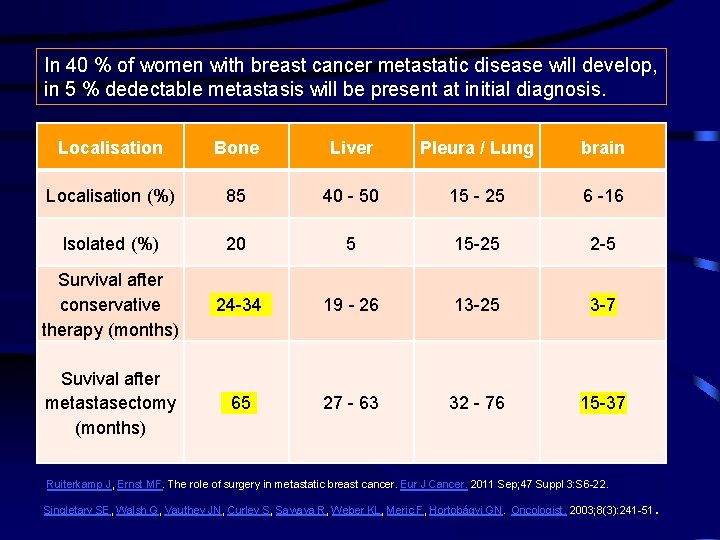
In 40 % of women with breast cancer metastatic disease will develop, in 5 % dedectable metastasis will be present at initial diagnosis. Localisation Bone Liver Pleura / Lung brain Localisation (%) 85 40 - 50 15 - 25 6 -16 Isolated (%) 20 5 15 -25 2 -5 Survival after conservative therapy (months) 24 -34 19 - 26 13 -25 3 -7 Suvival after metastasectomy (months) 65 27 - 63 32 - 76 15 -37 Ruiterkamp J, Ernst MF. The role of surgery in metastatic breast cancer. Eur J Cancer. 2011 Sep; 47 Suppl 3: S 6 -22. . Singletary SE, Walsh G, Vauthey JN, Curley S, Sawaya R, Weber KL, Meric F, Hortobágyi GN. Oncologist. 2003; 8(3): 241 -51