Part I Digestion absorption and transport of carbohydrates
Part I Digestion, absorption and transport of carbohydrates
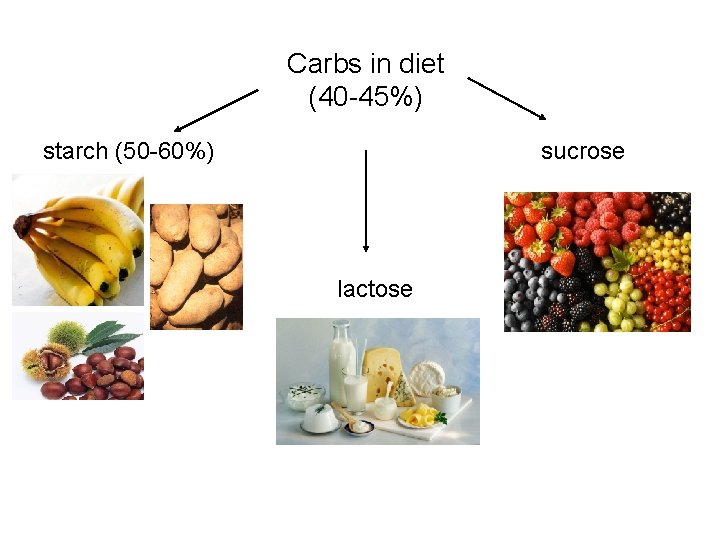
Carbs in diet (40 -45%) starch (50 -60%) sucrose lactose
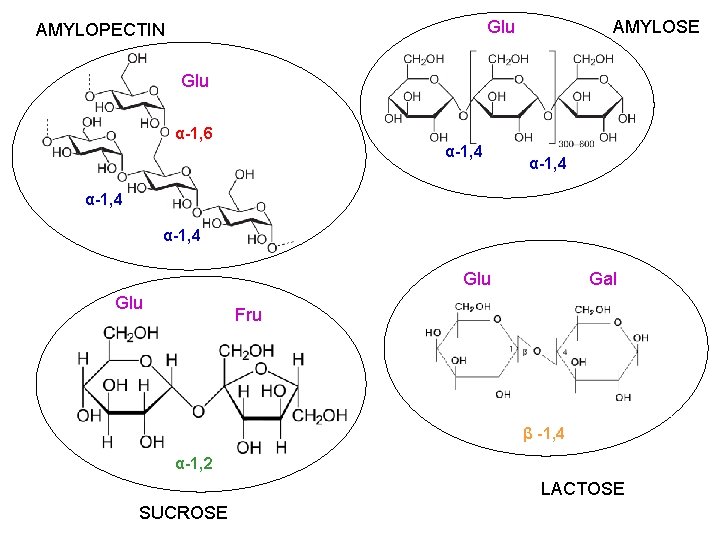
Glu AMYLOPECTIN AMYLOSE Glu α-1, 6 α-1, 4 Glu sgzusui Gal Fru β -1, 4 α-1, 2 LACTOSE SUCROSE

Digestion of starch

α-amylase (salivary) HCl α-amylase (pancreatic) HCO 3 - starch lactose sucrose α-dextrins sucrose sucrase glucose fructose lactase glucose galactose tri- and disaccharides maltose, isomaltose maltase isomaltase glucose fiber non-digested CH
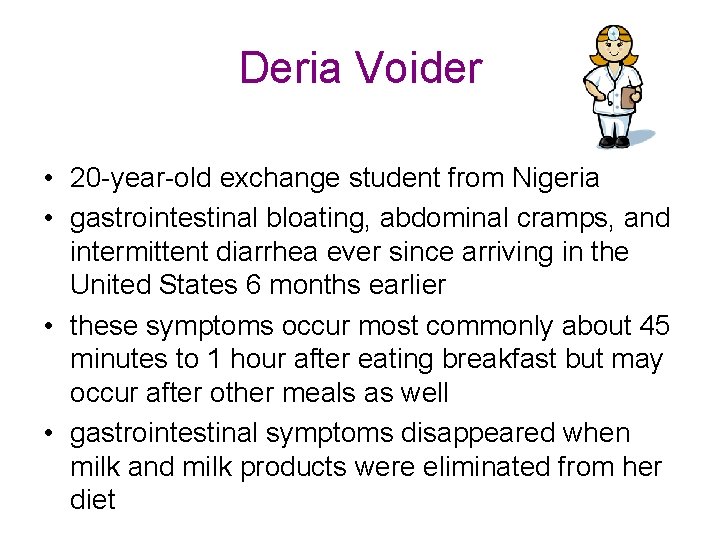
Deria Voider • 20 -year-old exchange student from Nigeria • gastrointestinal bloating, abdominal cramps, and intermittent diarrhea ever since arriving in the United States 6 months earlier • these symptoms occur most commonly about 45 minutes to 1 hour after eating breakfast but may occur after other meals as well • gastrointestinal symptoms disappeared when milk and milk products were eliminated from her diet
Ann Sulin • Fasting and postprandial blood glucose levels are frequently above the normal range in spite of good compliance with insulin therapy • Her physician has referred to a dietician skilled in training diabetic patients in the successful application of appropriate diabetic diet • She is asked to incorporate foods containing fiber in her diet, such as whole grains (e. g. wheat, oat, corn), legumes (e. g. peas, beans, lentils), tubers (e. g. potatoes, peanut) and fruit
Nona Melos • • 7 -month-old baby girl, the second child born to unrelated parents Her mother had a healthy, full-term pregnancy, and Nona’s birth weight was normal She did not respond well to breast feeding and was changed entirely to a formula based on cow’s milk at 4 weeks Between 7 and 12 weeks of age, she was admitted to the hospital twice with a history of screaming after feeding, but was discharged after observation without a specific diagnosis Elimination of cow’s milk from her diet did not relieve her symptoms; Nona’s mother reported that the screaming bouts were worse after Nona drank juice and that Nona frequently had gas and a distended abdomen At 7 months she was still thriving (weight above 97 th percentile) with no abnormal findings on physical examination. Stool sample had a p. H of 5 and gave a positive test for sugar Hydrogen breath test was recommended
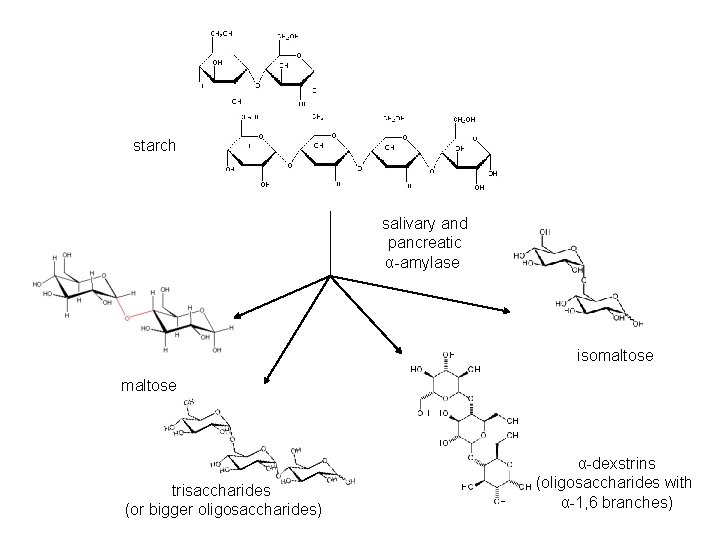
starch salivary and pancreatic α-amylase isomaltose trisaccharides (or bigger oligosaccharides) α-dexstrins (oligosaccharides with α-1, 6 branches)
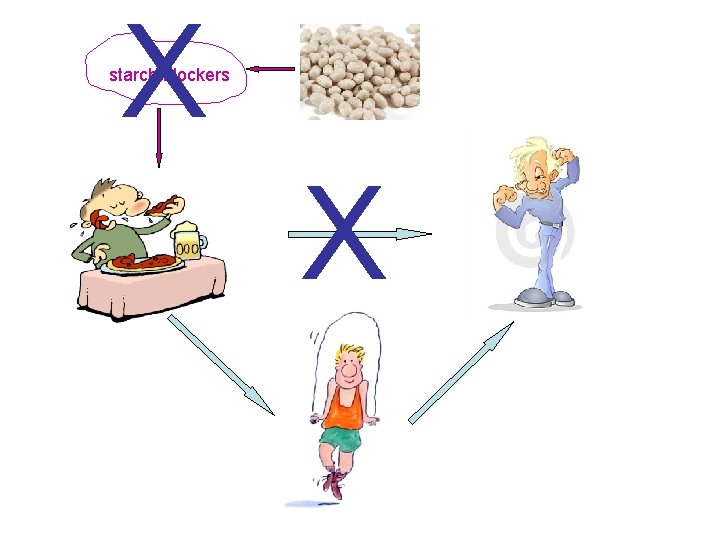
X starch blockers X
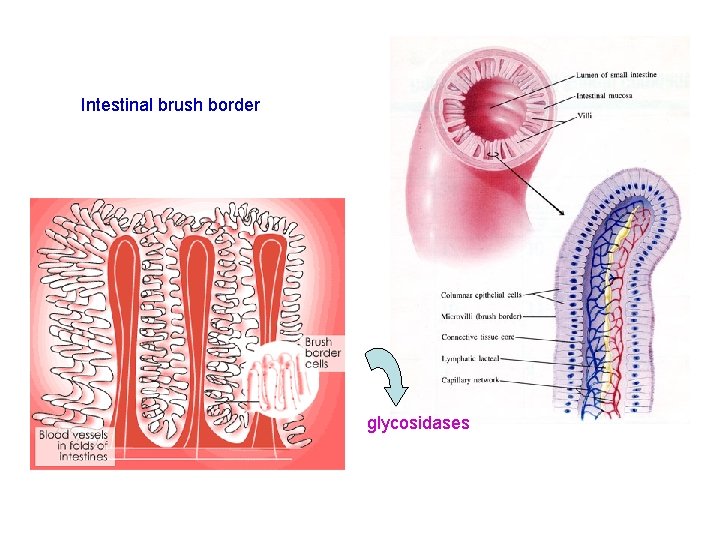
Intestinal brush border glycosidases
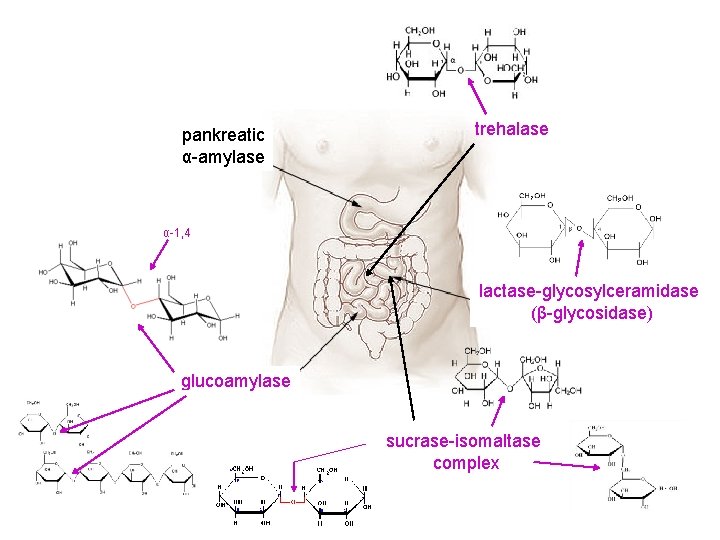
pankreatic α-amylase trehalase jgjhgjh α-1, 4 lactase-glycosylceramidase (β-glycosidase) glucoamylase sucrase-isomaltase complex
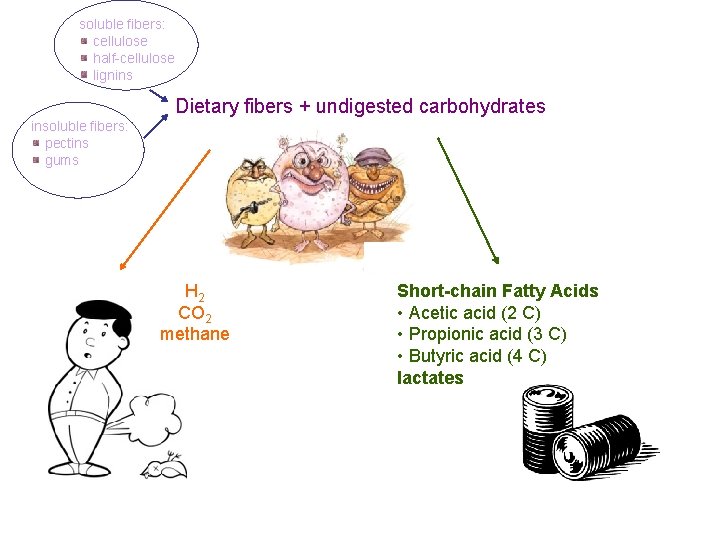
soluble fibers: cellulose half-cellulose lignins Dietary fibers + undigested carbohydrates insoluble fibers: pectins gums jhkjhkjhk H 2 CO 2 methane Short-chain Fatty Acids • Acetic acid (2 C) • Propionic acid (3 C) • Butyric acid (4 C) lactates
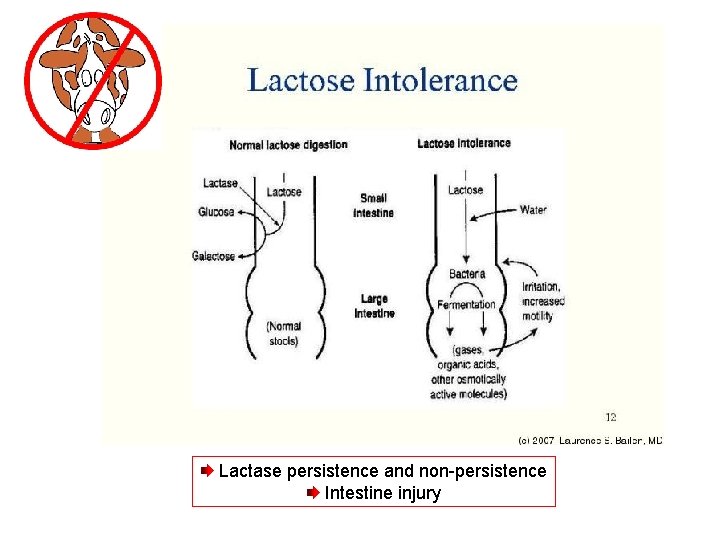
Lactase persistence and non-persistence Intestine injury
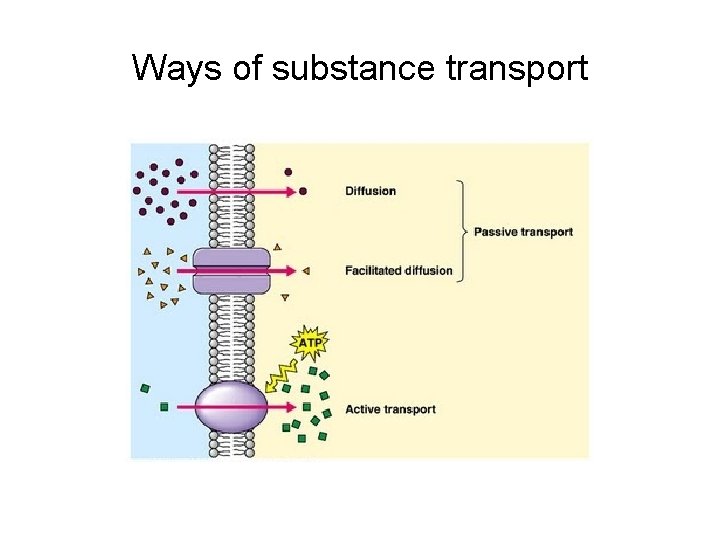
Ways of substance transport
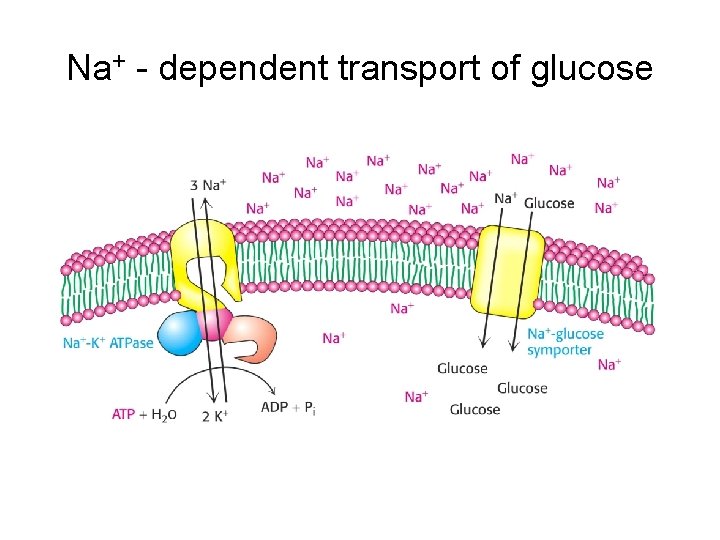
Na+ - dependent transport of glucose

Facilitated diffusion of glucose
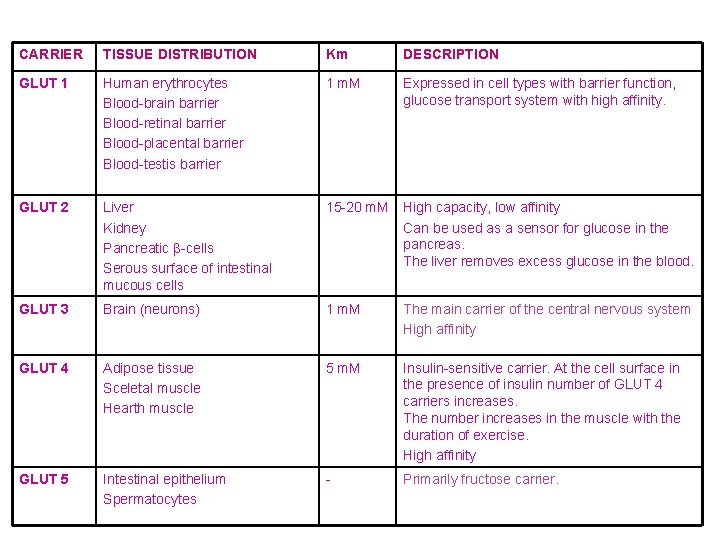
CARRIER TISSUE DISTRIBUTION Km DESCRIPTION GLUT 1 Human erythrocytes Blood-brain barrier Blood-retinal barrier Blood-placental barrier Blood-testis barrier 1 m. M Expressed in cell types with barrier function, glucose transport system with high affinity. GLUT 2 Liver Kidney Pancreatic β-cells Serous surface of intestinal mucous cells 15 -20 m. M High capacity, low affinity Can be used as a sensor for glucose in the pancreas. The liver removes excess glucose in the blood. GLUT 3 Brain (neurons) 1 m. M The main carrier of the central nervous system High affinity GLUT 4 Adipose tissue Sceletal muscle Hearth muscle 5 m. M Insulin-sensitive carrier. At the cell surface in the presence of insulin number of GLUT 4 carriers increases. The number increases in the muscle with the duration of exercise. High affinity GLUT 5 Intestinal epithelium Spermatocytes - Primarily fructose carrier.
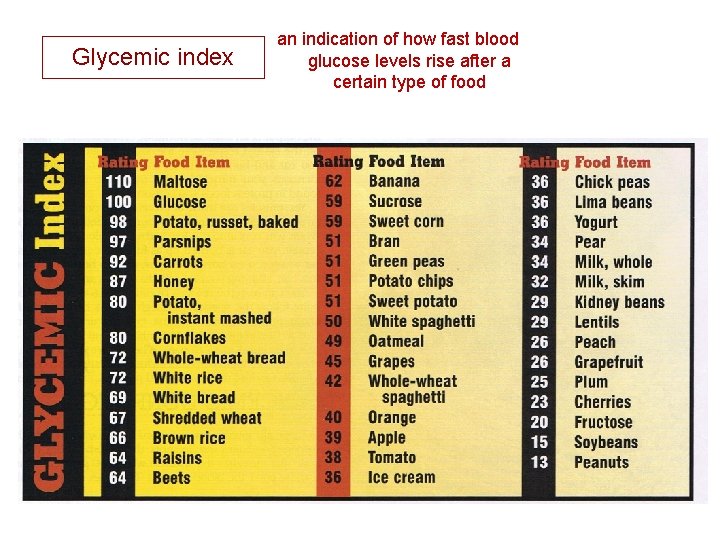
Glycemic index an indication of how fast blood glucose levels rise after a certain type of food
Clinical cases • Deria Voider Lactose intolerance • Ann Sulin Hyperglycemia caused with lack of circulating, active insulin • Nona Melos Fructose intolerance
Part II Lysosomal storage diseases. Gaucher disease
• Lysosomal storage diseases is the group of around 40 rare inherited metabolic disorders caused as a result of defects in the function of lysosomes • Most often the cause of the disease is a lack of a single enzyme required to metabolize lipids, glycoproteins and mucopolysaccharides
• Lysosom is recyclable place in the cell because it translates "unwanted material" into compounds that cells can use by specific enzymes. • When the enzyme is missing, the molecule supposed to degrade and re-use accumulates in the cell. membrane enzyme complex
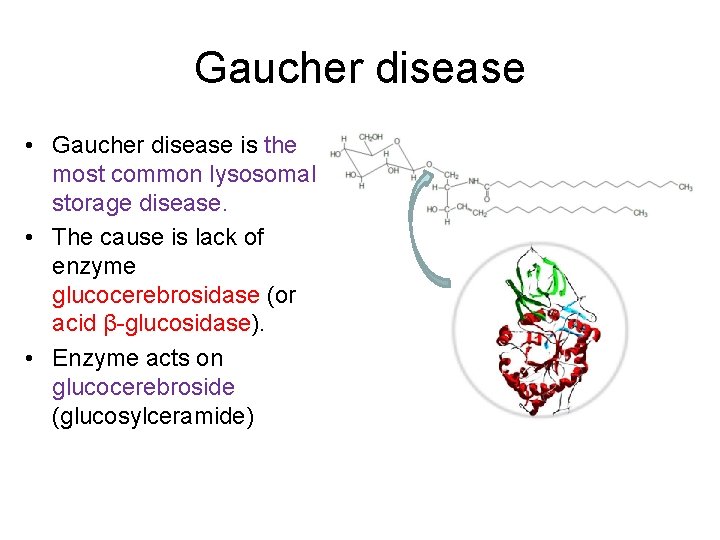
Gaucher disease • Gaucher disease is the most common lysosomal storage disease. • The cause is lack of enzyme glucocerebrosidase (or acid β-glucosidase). • Enzyme acts on glucocerebroside (glucosylceramide)
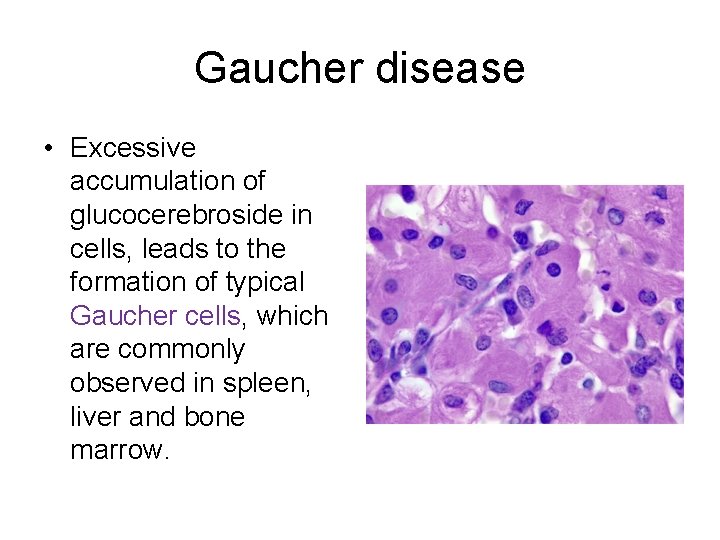
Gaucher disease • Excessive accumulation of glucocerebroside in cells, leads to the formation of typical Gaucher cells, which are commonly observed in spleen, liver and bone marrow.
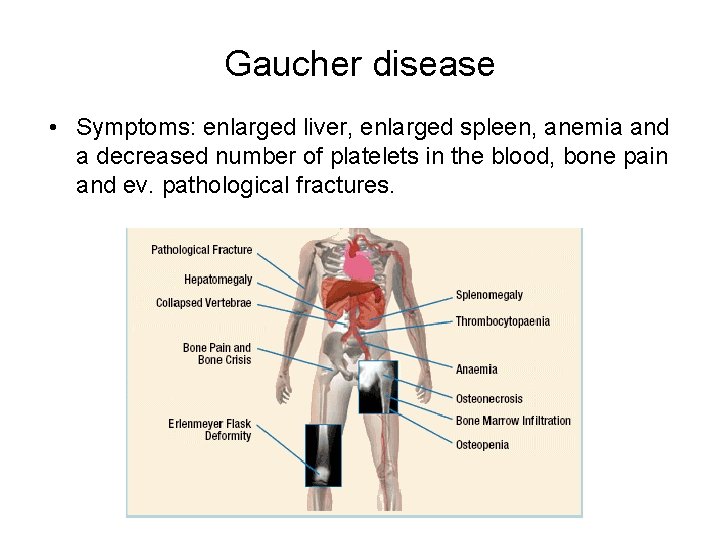
Gaucher disease • Symptoms: enlarged liver, enlarged spleen, anemia and a decreased number of platelets in the blood, bone pain and ev. pathological fractures.
Gaucher disease • The course of disease is different, some patients are already at an early age dependent on wheelchair while in other patients the disease has a slower flow, but progressively worse over the years. • The disease is in an advanced stage extremely difficult and can lead to disability, and in some cases is fatal if untreated with timely treatment.
Other lysosomal storage diseases • Tay-Sachs, Niemann-Pick, Fabry, Krabe, Pompe. . . .
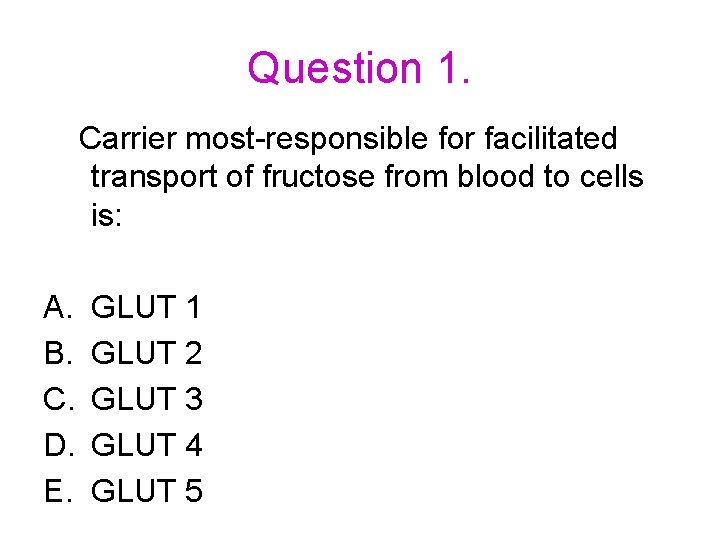
Question 1. Carrier most-responsible for facilitated transport of fructose from blood to cells is: A. B. C. D. E. GLUT 1 GLUT 2 GLUT 3 GLUT 4 GLUT 5
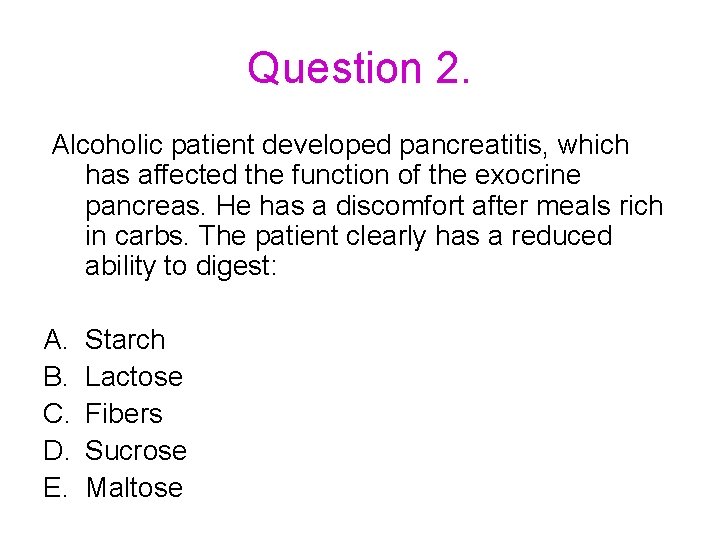
Question 2. Alcoholic patient developed pancreatitis, which has affected the function of the exocrine pancreas. He has a discomfort after meals rich in carbs. The patient clearly has a reduced ability to digest: A. B. C. D. E. Starch Lactose Fibers Sucrose Maltose
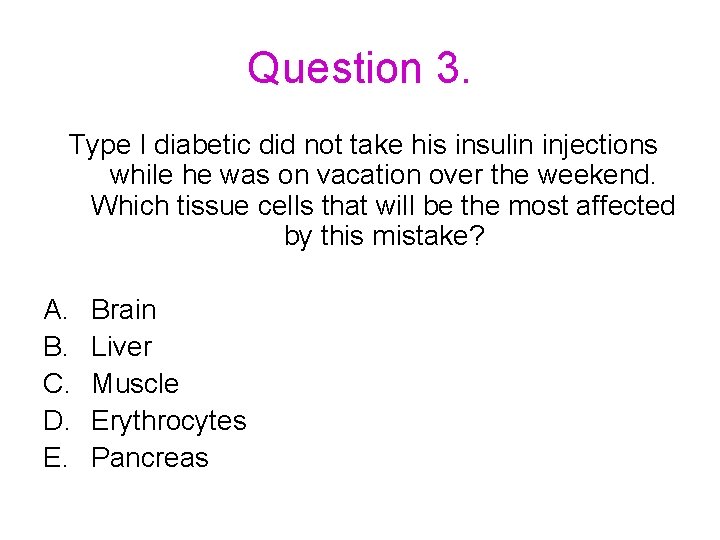
Question 3. Type I diabetic did not take his insulin injections while he was on vacation over the weekend. Which tissue cells that will be the most affected by this mistake? A. B. C. D. E. Brain Liver Muscle Erythrocytes Pancreas
Question 4. After taking a piece of cake that contains flour, milk and sucrose as primary ingredients, the main products of carbs entering the blood are: A. B. C. D. E. Glucose Fructose and galactose Galactose and glucose Fructose and glucose Glucose, galactose and fructose
Question 5. The patient has a genetic disorder that causes the intestinal epithelial cells to produce disaccharidases with significantly less activity than normal. Compared to a normal person, after a glass of milk and oatmeal sweetened with sugar cube, this patient would have higher levels of: A. B. C. D. E. Maltose, sucrose and lactose in stool Starch in stool Galactose and fructose in blood Glycogen in muscle Insulin in blood
- Slides: 33