Part 3 B Endobronchial Brushing volume 1 Strategy
Part 3 B: Endobronchial Brushing volume 1 Strategy and Planning Execution Bronchoscopy International BI 1
When to perform endobronchial brushing n n Visible airway mucosal abnormalities Visible airway nodules or masses In case of suspected sarcoidosis (even if airway mucosa appears normal) In case of abnormal autofluorescence to diagnose intraepithelial lesions (dysplasia, metaplasia, carcinoma in-situ) BI 2
Training is essential in order to Learn proper techniques and indications n Avoid procedure-related complications. n Learn to protect the equipment and the patient n To obtain adequate tissue for diagnosis n To avoid damaging the working channel n To avoid excess patient discomfort (cough, anxiety, shortness of breath). n To avoid bleeding, that might also prompt cough and patient agitation. n BI 3
Q 1: Optimal endobronchial brushing samples requires correct processing BI 4
Q 8: Optimal endobronchial brushing samples requires correct processing BI 5
TRUE. Brushing samples must be processed correctly and according to the needs and preferences of your institution’s cytology and microbiology laboratories. n Other ways to potentially increase diagnostic yield include n n Using brushes with longer bristles Brushing vigorously and for a longer period of time. Making sure that all parts of the brush are in contact with the mucosal abnormality. Using the pirouette technique (rotation) in combination with long-axis motion. BI 6
Bronchial brushing: n n Originally done under fluoroscopy without bronchoscopy Common indications: n n Visible endobronchial tumors or mucosal abnormality Peripheral tumors (+/- fluoroscopy) Peripheral infection – pneumonia, abscess, cavity Brush samples larger surface area of lesion BI 7
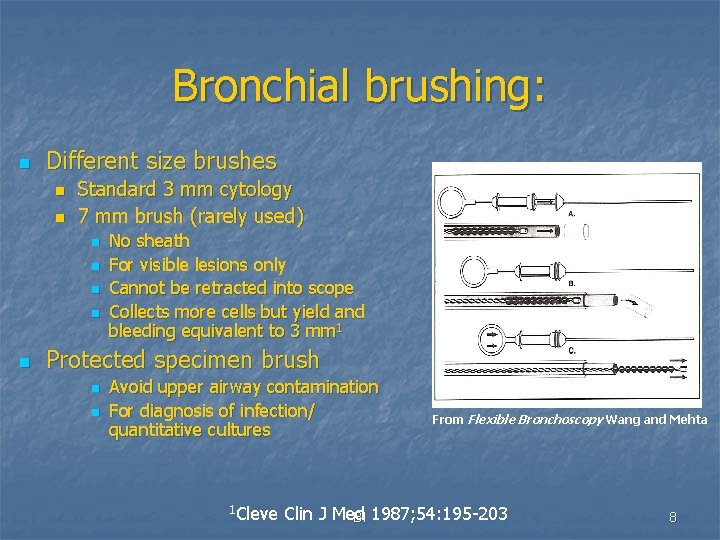
Bronchial brushing: n Different size brushes n n Standard 3 mm cytology 7 mm brush (rarely used) n n n No sheath For visible lesions only Cannot be retracted into scope Collects more cells but yield and bleeding equivalent to 3 mm 1 Protected specimen brush n n Avoid upper airway contamination For diagnosis of infection/ quantitative cultures 1 Cleve From Flexible Bronchoscopy Wang and Mehta Clin J Med BI 1987; 54: 195 -203 8
Bronchial brushing: n Technique: Advance catheter into desired segment – then extend brush (up to 5 cm) n Make sure brush extension doesn’t push back the scope or catheter n Move back and forth over the visible lesion or blindly in distal airway (5 -10 times) +/rotation n Cells collected in brush bristles n BI 9
Bronchial brushing: n Yield: 94% endoscopically visible/peripheral 78%1 n 92% central and peripheral with fluoro 2 n 77% endoscopically visible/20% peripheral with fluoro 3 n 1 CHEST 1 Am 1973; 63: 889 -892 Rev Respir Dis 1974; 109: 63 -66 2 CHEST 1974; 65: 616 -619 3 CHEST 1976; 69: 752 -757 BI 10
Bronchial brushing: n Complications: Bleeding n Pneumothorax n BI 11
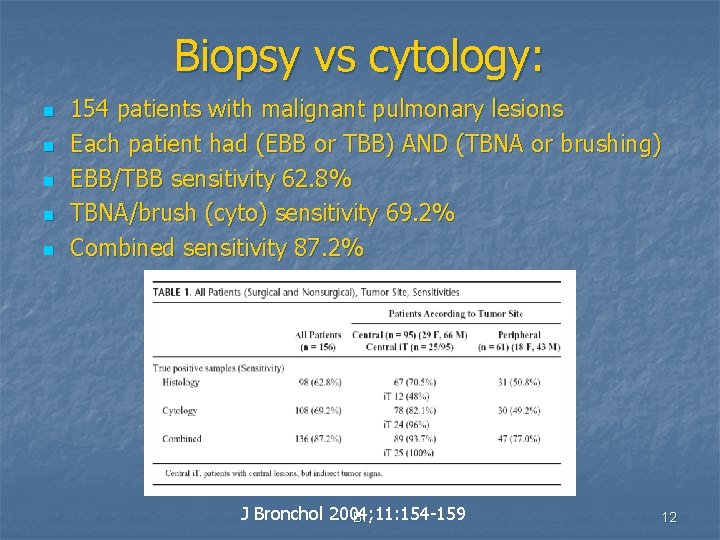
Biopsy vs cytology: n n n 154 patients with malignant pulmonary lesions Each patient had (EBB or TBB) AND (TBNA or brushing) EBB/TBB sensitivity 62. 8% TBNA/brush (cyto) sensitivity 69. 2% Combined sensitivity 87. 2% J Bronchol 2004; 11: 154 -159 BI 12
Additional literature: BI J Bronchol 2004; 11: 154 -159 13
Endobronchial Brushing n n n Brush samples large area of mucosal abnormality May be done under direct visualization, or with fluoroscopic guidance Brushes may be bare of within a covering sheath Brush Video BI 14
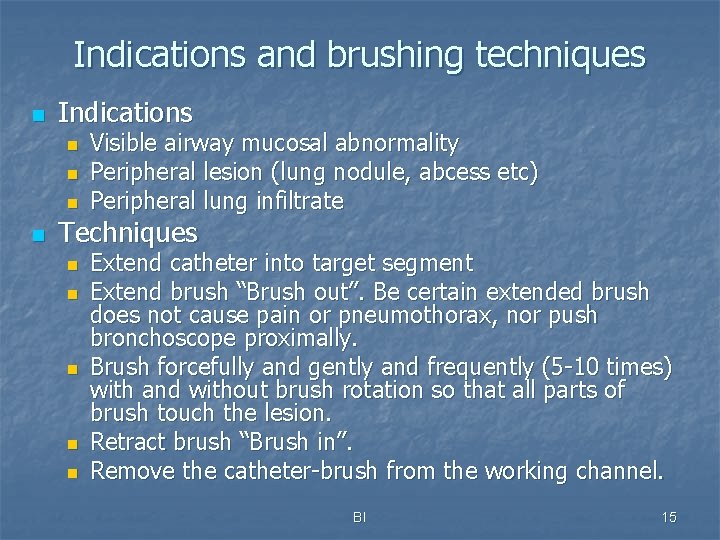
Indications and brushing techniques n Indications n n Visible airway mucosal abnormality Peripheral lesion (lung nodule, abcess etc) Peripheral lung infiltrate Techniques n n n Extend catheter into target segment Extend brush “Brush out”. Be certain extended brush does not cause pain or pneumothorax, nor push bronchoscope proximally. Brush forcefully and gently and frequently (5 -10 times) with and without brush rotation so that all parts of brush touch the lesion. Retract brush “Brush in”. Remove the catheter-brush from the working channel. BI 15
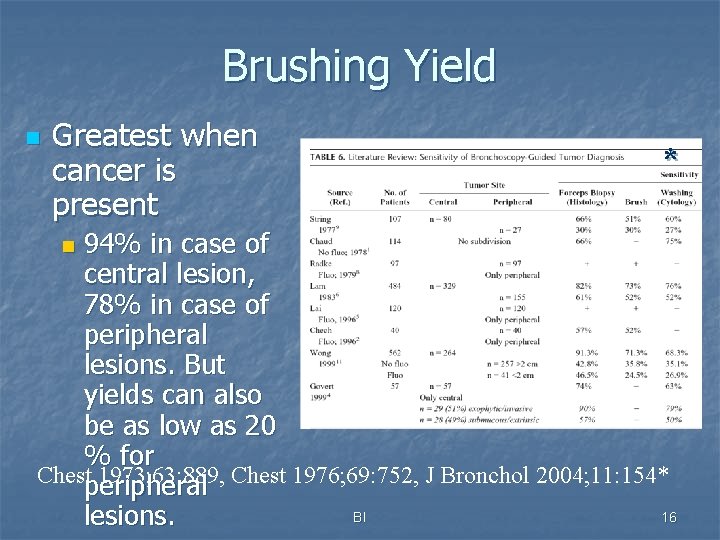
Brushing Yield n Greatest when cancer is present * 94% in case of central lesion, 78% in case of peripheral lesions. But yields can also be as low as 20 % for Chest 1973; 63: 889, Chest 1976; 69: 752, J Bronchol 2004; 11: 154* peripheral BI 16 lesions. n
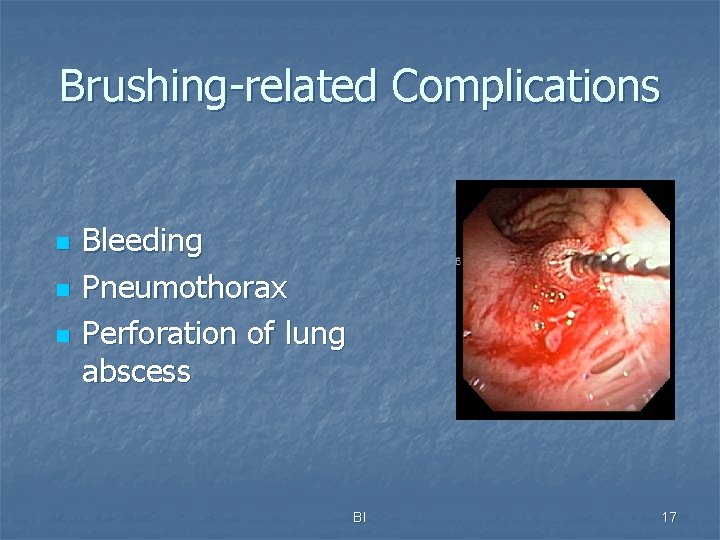
Brushing-related Complications n n n Bleeding Pneumothorax Perforation of lung abscess BI 17
Bleeding risk if Thrombocytopenia: <50, 000 n n n Risk of bleeding: 0 -26% (TBBx, post transfusion) (1) Brushing with mean platelet count of 30, 000: Bleed: 16% , Death: 4% (2) What to do? Transfuse 6 packs before & during bronchoscopy, no need to recheck platelets (3) n Platelet half-life 6 hours! (1) Weiss S, Chest, 1993; 104: 1025 (2) Papin T, Chest, 1985; 88: 54 (3)Wahidi M, Respiration 2005; 72: 285 BI 18
Combined procedures have greatest yield for malignancy n Arch Bronchoneumol. 2006; 42(6): 278 -82 n 75 patients underwent bronchial washing before (pre) and after (post) endobronchial biopsy and brushing BI 19
This presentation is part of a comprehensive curriculum for Flexible Bronchoscopy. Our goals are to help health care workers become better at what they do, and to decrease the burden of procedurerelated training on patients. BI 20
Step by Step© Bronchoscopy. org BRONCHATLAS© BI 21
All efforts are made by Bronchoscopy International to maintain currency of online information. All published multimedia slide shows, streaming videos, and essays can be cited for reference as: Bronchoscopy International: Art of Bronchoscopy, an Electronic On. Line Multimedia Slide Presentation. http: //www. Bronchoscopy. org/Art of Bronchoscopy/htm. Published 2007 (Please add “Date Accessed”). Thank you BI 22
Prepared with the expert assistance of Udaya Prakash M. D. (Mayo Clinic, USA), and Atul Mehta M. D. (Cleveland Clinic, USA), and Wes Shepherd M. D. (Virginia Commonwealth University, USA) www. bronchoscopy. org BI 23
- Slides: 23