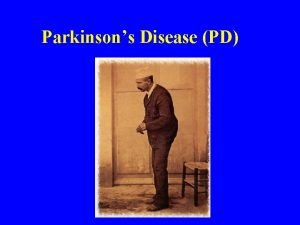
PARKINSONS DISEASE DEFINITION A chronic progressive disease of




- Slides: 51

PARKINSON’S DISEASE
DEFINITION �A chronic, progressive disease of the nervous system due to degeneration of dopamineproducing cells in the substantia nigra characterized by rigidity, bradykinesia, resting tremor, and postural instability
Other names: � Paralysis agitans � True PD � Idiopathic Parkinson’s disease � Shaking palsy
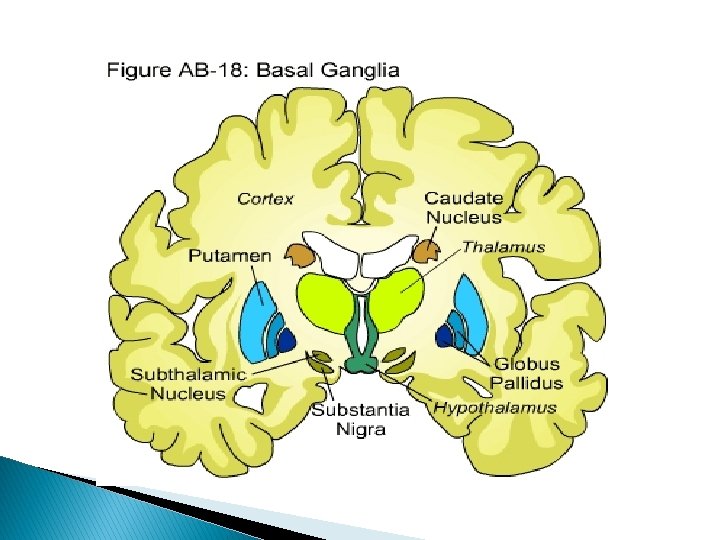
Anatomy Extrapyramidal system – eliminates unwanted movements for smooth voluntary motor activity 1. Basal ganglia 2. Subthalamic nucleus 3. Substantia nigra 4. Reticular formation 5. Red nucleus
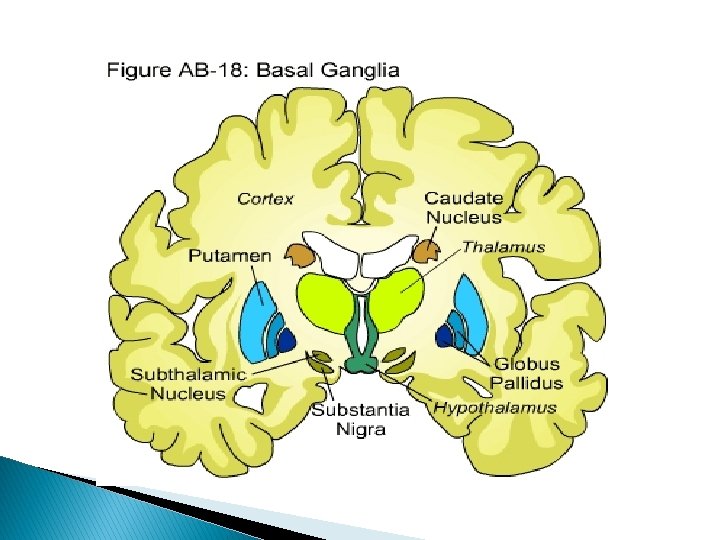
Cell bodies in the basal ganglia 1. Putamen 2. Globus pallidus – regulates muscle tone 3. Caudate nucleus - coordination Striatum/Neostriatum (controls large subconscious movements) = caudate nucleus + putamen Paleostriatum/Pallidum = globus pallidus Lenticular nucleus = globus pallidus + putamen Corpus striatum = lenticular nucleus + caudate nucleus
Dopamine – main inhibitory neurotransmitter from the basal ganglia Acetylcholine – main excitatory neurotransmitter within the corpus striatum Circuit involved in PD: Striatum Substantia Nigra Thalamus Cerebral Cortex
EPIDEMIOLOGY � 58 -62 �M y/o – mean age of onset >F � Kyphosis – most common postural deformity � Pneumonia – one of the leading causes of death
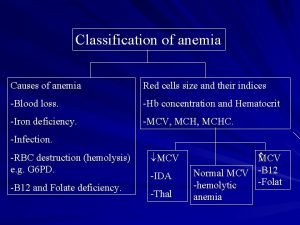
ETIOLOGY 1. 2. 3. Parkinsonism – a group of disorders that produce abnormalities of the basal ganglia function Primary parkinsonism – most common cause Secondary parkinsonism – results from a number of different causes Parkinson-plus syndromes – conditions with symptoms of multiple system degeneration
Primary parkinsonism Parkinson’s disease – Idiopathic parkinson’s disease �True PD, paralysis agitans, shaking palsy �Groups: �Postural instability gait disturbed �Tremor predominant
Secondary parkinsonism 1. Post-infectious parkinsonism – caused by viral infection �Encephalitis lethargica – “sleeping sickness” �Presence of headache and drowsiness progressing to coma �Cryptococcal meningitis – inflammation of meninges caused by Cryptococcus 2. Toxic parkinsonism – from industrial poisons and chemicals �Manganese – most common �Synthetic heroin – causes severe parkinsonism
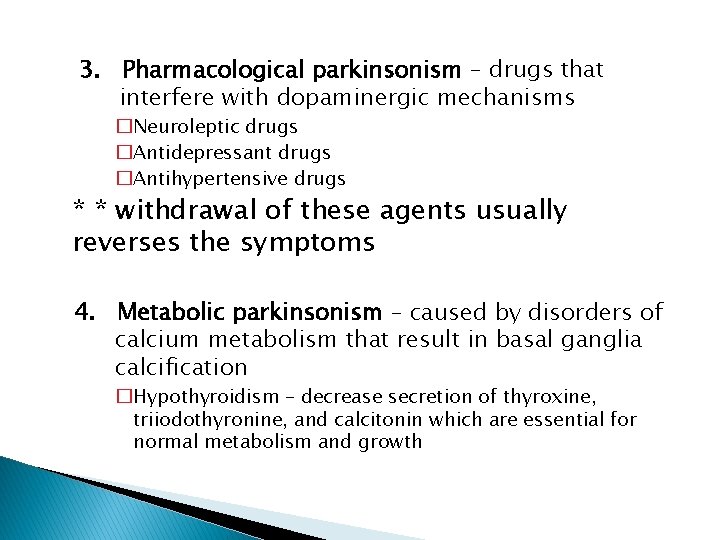
3. Pharmacological parkinsonism – drugs that interfere with dopaminergic mechanisms �Neuroleptic drugs �Antidepressant drugs �Antihypertensive drugs * * withdrawal of these agents usually reverses the symptoms 4. Metabolic parkinsonism – caused by disorders of calcium metabolism that result in basal ganglia calcification �Hypothyroidism – decrease secretion of thyroxine, triiodothyronine, and calcitonin which are essential for normal metabolism and growth
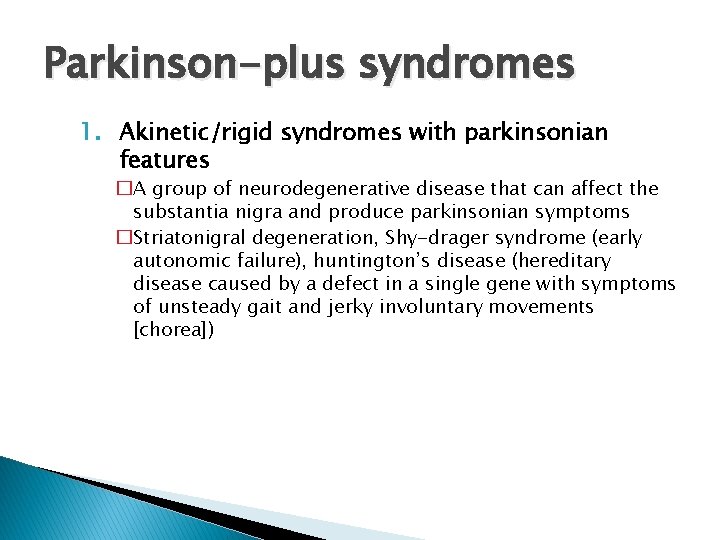
Parkinson-plus syndromes 1. Akinetic/rigid syndromes with parkinsonian features �A group of neurodegenerative disease that can affect the substantia nigra and produce parkinsonian symptoms �Striatonigral degeneration, Shy-drager syndrome (early autonomic failure), huntington’s disease (hereditary disease caused by a defect in a single gene with symptoms of unsteady gait and jerky involuntary movements [chorea])
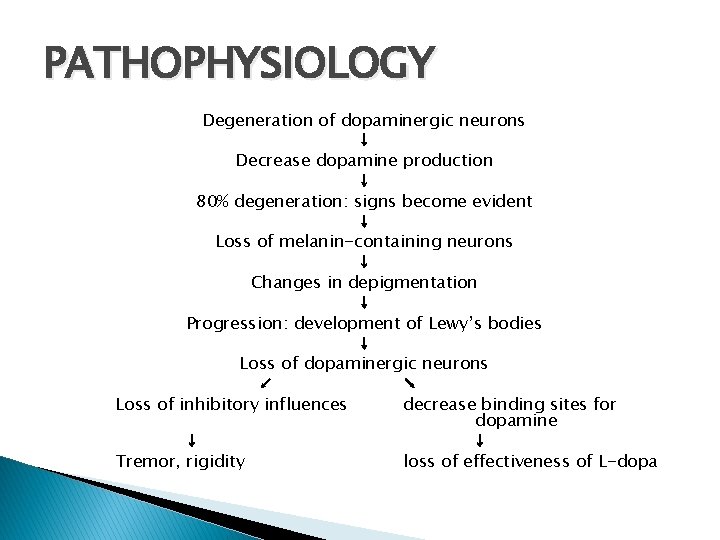
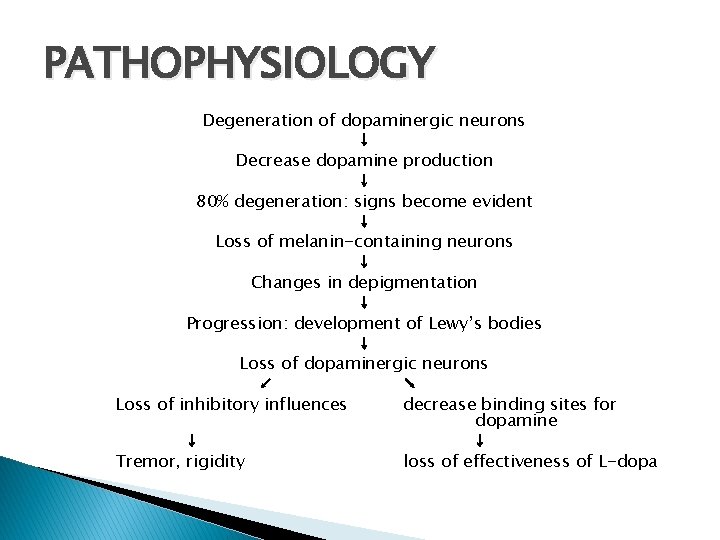
PATHOPHYSIOLOGY Degeneration of dopaminergic neurons ↓ Decrease dopamine production ↓ 80% degeneration: signs become evident ↓ Loss of melanin-containing neurons ↓ Changes in depigmentation ↓ Progression: development of Lewy’s bodies ↓ Loss of dopaminergic neurons ↙ ↘ Loss of inhibitory influences decrease binding sites for dopamine ↓ ↓ Tremor, rigidity loss of effectiveness of L-dopa
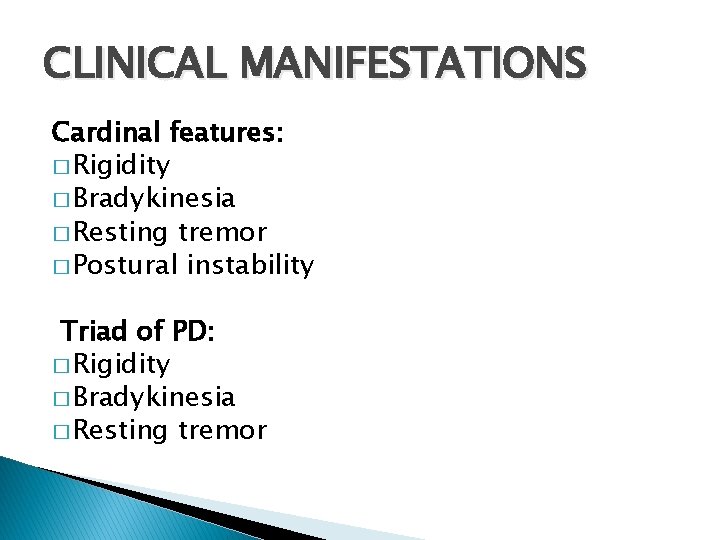
CLINICAL MANIFESTATIONS Cardinal features: � Rigidity � Bradykinesia � Resting tremor � Postural instability Triad of PD: � Rigidity � Bradykinesia � Resting tremor
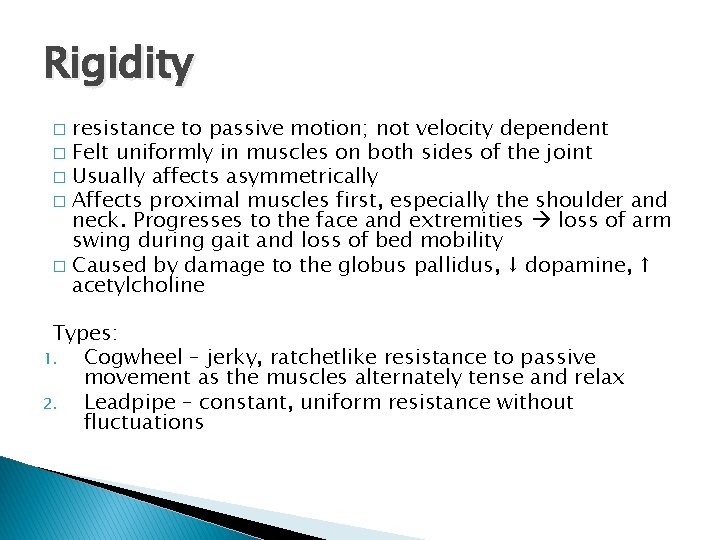
Rigidity resistance to passive motion; not velocity dependent � Felt uniformly in muscles on both sides of the joint � Usually affects asymmetrically � Affects proximal muscles first, especially the shoulder and neck. Progresses to the face and extremities loss of arm swing during gait and loss of bed mobility � Caused by damage to the globus pallidus, ↓ dopamine, ↑ acetylcholine � Types: 1. Cogwheel – jerky, ratchetlike resistance to passive movement as the muscles alternately tense and relax 2. Leadpipe – constant, uniform resistance without fluctuations
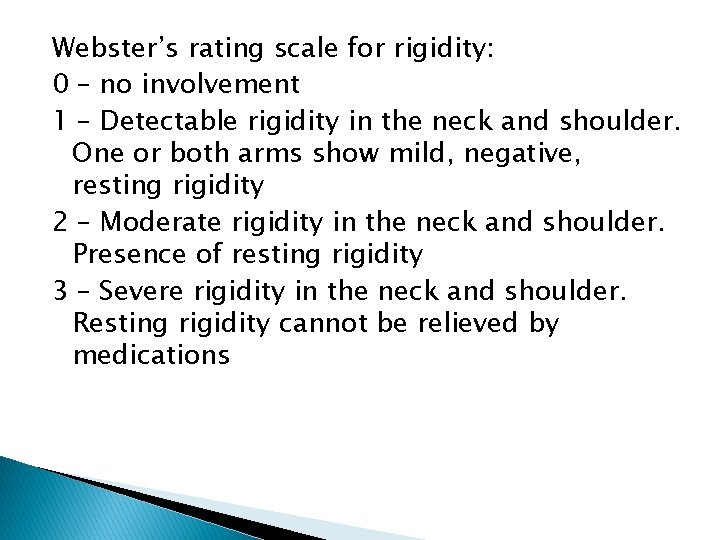
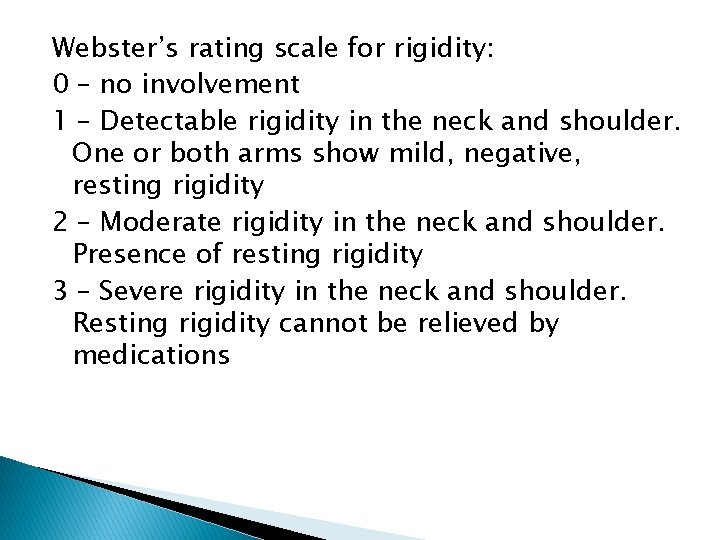
Webster’s rating scale for rigidity: 0 – no involvement 1 – Detectable rigidity in the neck and shoulder. One or both arms show mild, negative, resting rigidity 2 – Moderate rigidity in the neck and shoulder. Presence of resting rigidity 3 – Severe rigidity in the neck and shoulder. Resting rigidity cannot be relieved by medications
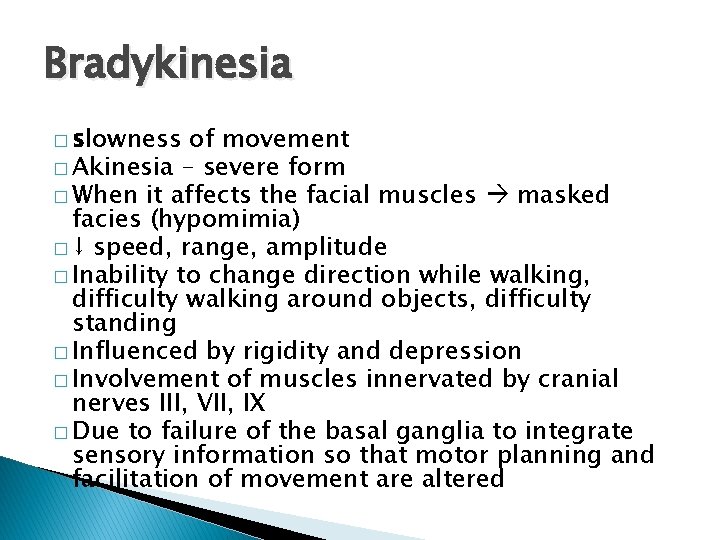
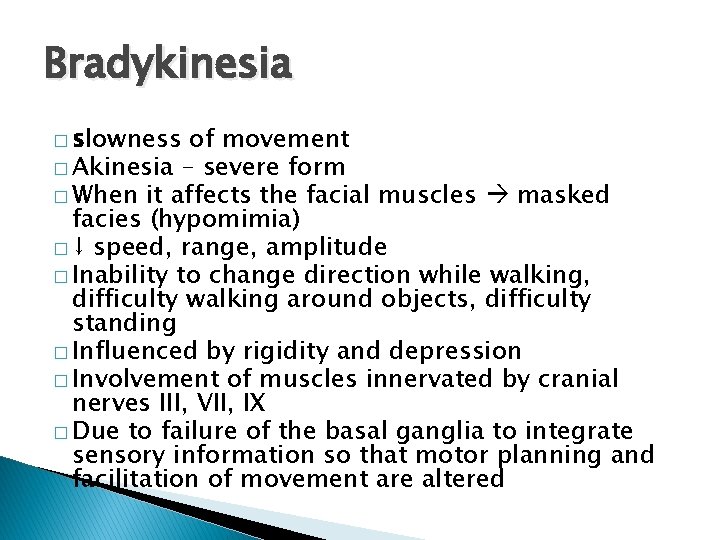
Bradykinesia � slowness of movement � Akinesia – severe form � When it affects the facial muscles masked facies (hypomimia) � ↓ speed, range, amplitude � Inability to change direction while walking, difficulty walking around objects, difficulty standing � Influenced by rigidity and depression � Involvement of muscles innervated by cranial nerves III, VII, IX � Due to failure of the basal ganglia to integrate sensory information so that motor planning and facilitation of movement are altered
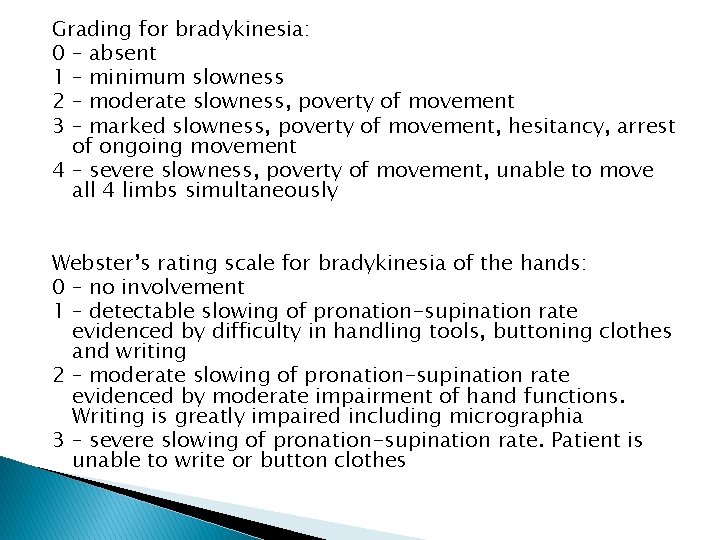
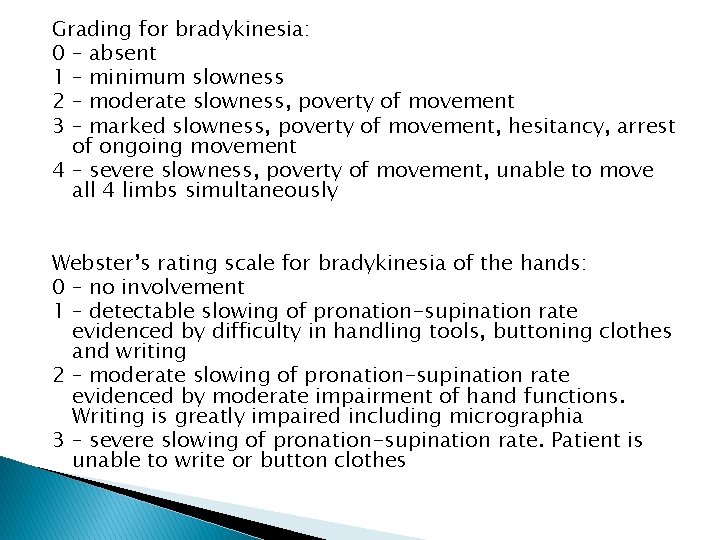
Grading for bradykinesia: 0 – absent 1 – minimum slowness 2 – moderate slowness, poverty of movement 3 – marked slowness, poverty of movement, hesitancy, arrest of ongoing movement 4 – severe slowness, poverty of movement, unable to move all 4 limbs simultaneously Webster’s rating scale for bradykinesia of the hands: 0 – no involvement 1 – detectable slowing of pronation-supination rate evidenced by difficulty in handling tools, buttoning clothes and writing 2 – moderate slowing of pronation-supination rate evidenced by moderate impairment of hand functions. Writing is greatly impaired including micrographia 3 – severe slowing of pronation-supination rate. Patient is unable to write or button clothes
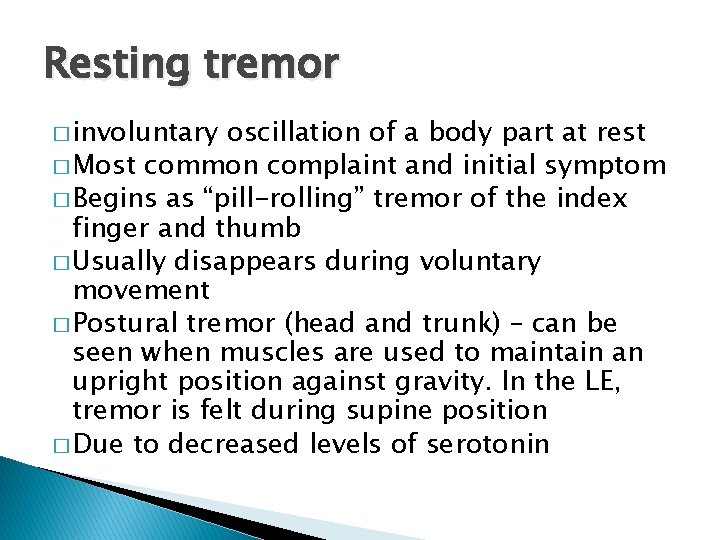
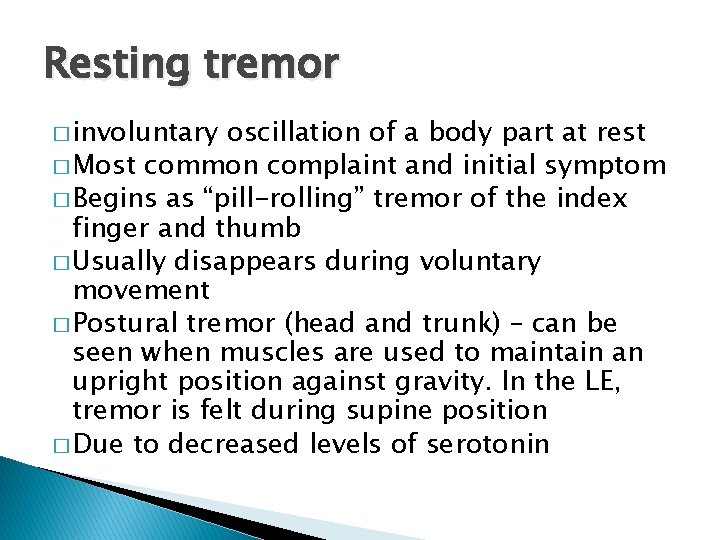
Resting tremor � involuntary oscillation of a body part at rest � Most common complaint and initial symptom � Begins as “pill-rolling” tremor of the index finger and thumb � Usually disappears during voluntary movement � Postural tremor (head and trunk) – can be seen when muscles are used to maintain an upright position against gravity. In the LE, tremor is felt during supine position � Due to decreased levels of serotonin
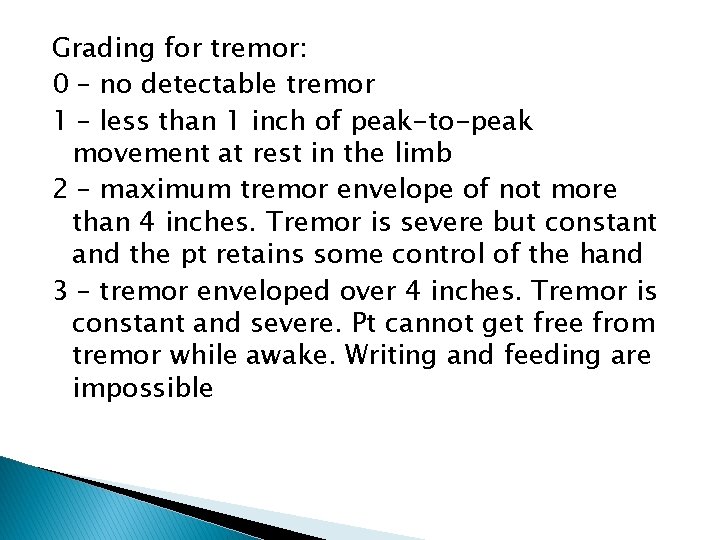
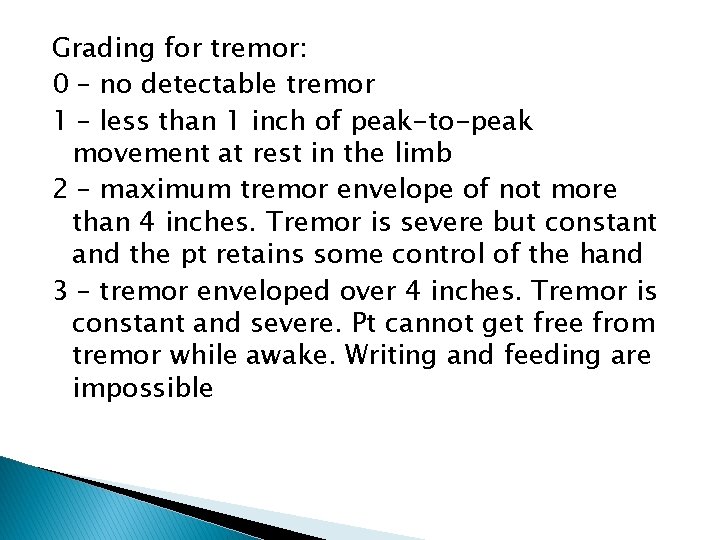
Grading for tremor: 0 – no detectable tremor 1 – less than 1 inch of peak-to-peak movement at rest in the limb 2 – maximum tremor envelope of not more than 4 inches. Tremor is severe but constant and the pt retains some control of the hand 3 – tremor enveloped over 4 inches. Tremor is constant and severe. Pt cannot get free from tremor while awake. Writing and feeding are impossible
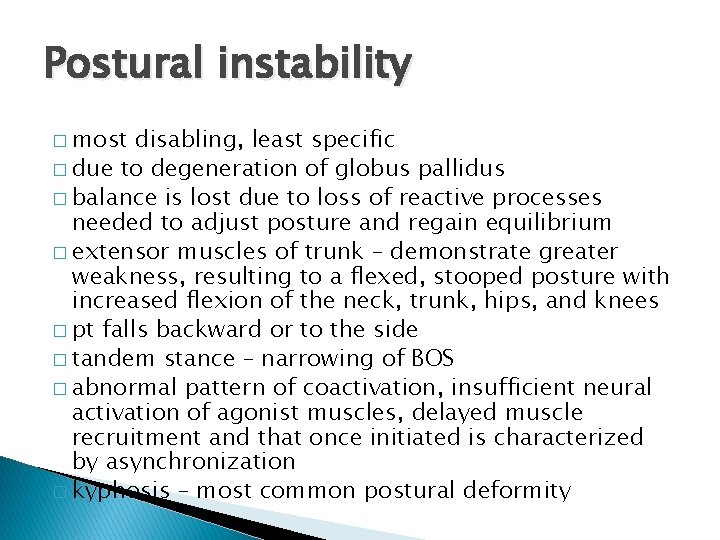
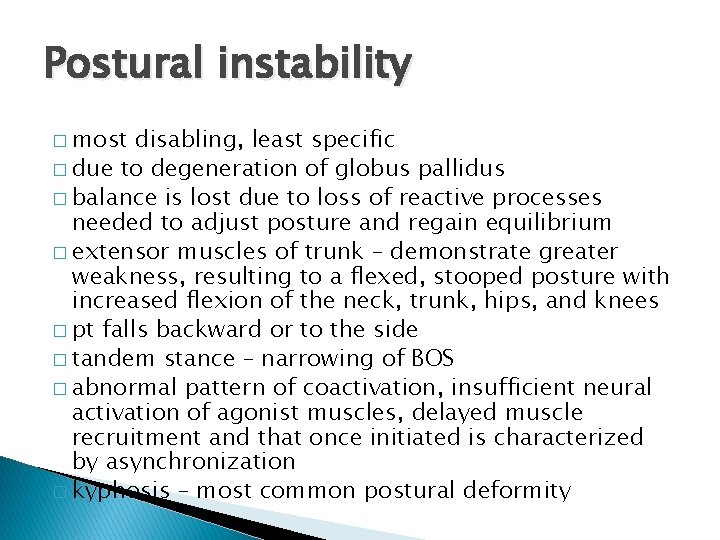
Postural instability � most disabling, least specific � due to degeneration of globus pallidus � balance is lost due to loss of reactive processes needed to adjust posture and regain equilibrium � extensor muscles of trunk – demonstrate greater weakness, resulting to a flexed, stooped posture with increased flexion of the neck, trunk, hips, and knees � pt falls backward or to the side � tandem stance – narrowing of BOS � abnormal pattern of coactivation, insufficient neural activation of agonist muscles, delayed muscle recruitment and that once initiated is characterized by asynchronization � kyphosis – most common postural deformity
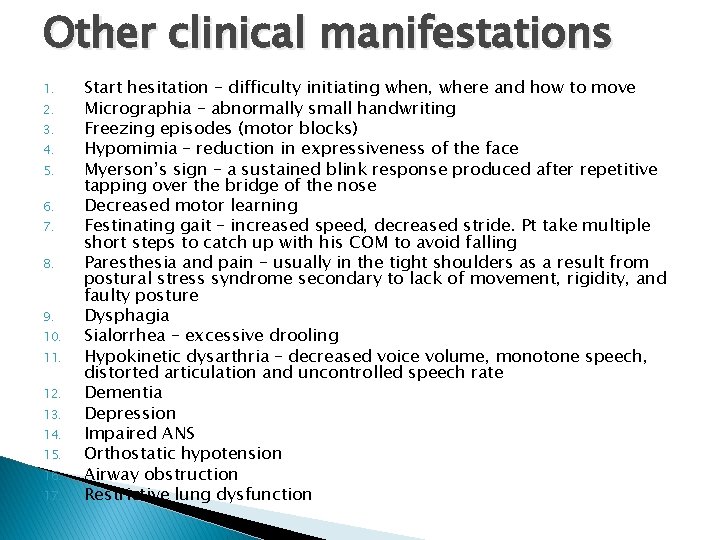
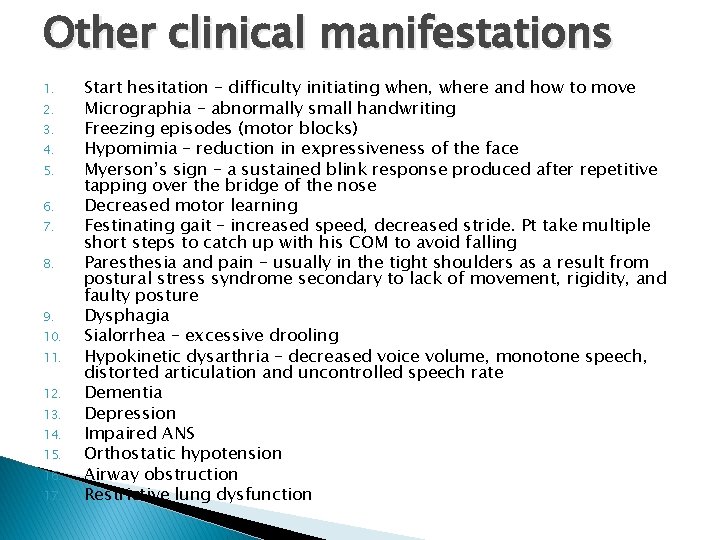
Other clinical manifestations 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. Start hesitation – difficulty initiating when, where and how to move Micrographia – abnormally small handwriting Freezing episodes (motor blocks) Hypomimia – reduction in expressiveness of the face Myerson’s sign – a sustained blink response produced after repetitive tapping over the bridge of the nose Decreased motor learning Festinating gait – increased speed, decreased stride. Pt take multiple short steps to catch up with his COM to avoid falling Paresthesia and pain – usually in the tight shoulders as a result from postural stress syndrome secondary to lack of movement, rigidity, and faulty posture Dysphagia Sialorrhea – excessive drooling Hypokinetic dysarthria – decreased voice volume, monotone speech, distorted articulation and uncontrolled speech rate Dementia Depression Impaired ANS Orthostatic hypotension Airway obstruction Restrictive lung dysfunction
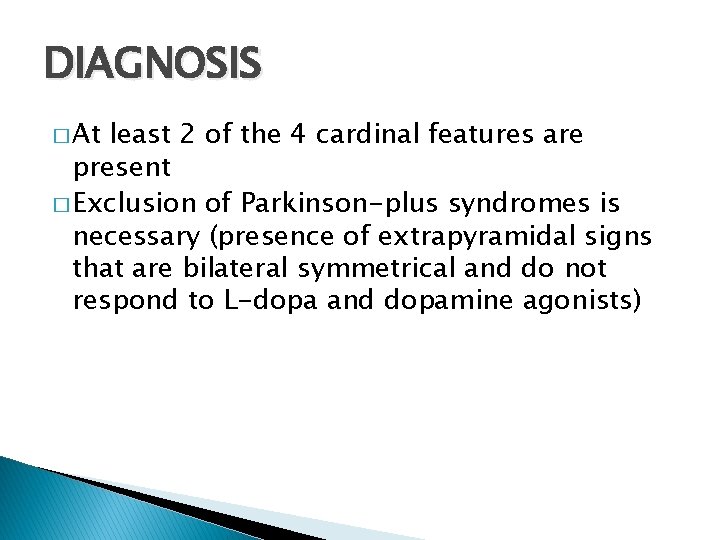
DIAGNOSIS � At least 2 of the 4 cardinal features are present � Exclusion of Parkinson-plus syndromes is necessary (presence of extrapyramidal signs that are bilateral symmetrical and do not respond to L-dopa and dopamine agonists)
Tools 1. 2. 3. MRI Positron emission tomography Single-photon emission computerized tomography
PT Dx 1. 2. 3. 4. 5. 6. Presence of tremor, festinating gait, flexed stooped posture, expressionless face, rigidity, babinski reflex, hyperreflexia, micrographia Loss of hip and knee extension, ankle dorsiflexion, shoulder flexion, elbow extension, dorsal spine and neck extension, and axial rotation during ROM Slow movement Excessive drooling or sweating Tonal changes in the shoulder and neck, trunk and extremities Rapid, monotonous, low volume with poor articulation in speech
Pharmacology Levodopa (L-dopa) – mainstay of symptomatic treatment ◦ A metabolic precursor of dopamine that is able to cross the BBB and raise the level of striatal dopamine in the BG ◦ Commonly administered with CARBIDOPA, which allows a higher percentage of L-dopa to enter the CNS ◦ L-dopa is usually metabolized before reaching the brain ◦ SINEMET – most common carbidopa/L-dopa medication; alleviates bradykinesia and rigidity, less effect on tremor Selegiline – delays the primary endpoint at which pts need to start taking L-dopa ◦ Monoamine oxidase inhibitor (drug class) ◦ Once L-dopa therapy is started, selegiline in combination permits a lower dose to be used
Dopamine agonists – act directly on the postsynaptic dopamine receptors ◦ Example: bromocriptine ◦ Reduces rigidity and bradykinesia Anticholinergics – used in early, untreated PD ◦ Block cholinergic function and have the most benefit moderating tremor and rigidity ◦ Examples: trihexyphenidyl, bentropin
Surgical management Indications: 1. pts with advanced PD who respond poorly to medications 2. pts who experience complications related to pharmacotherapy
� Stereotactic brain surgery – surgical lesioning of the ◦ Pallidotomy – producing a destructive lesion in the sensorimotor portion of the globus pallidus internus which produces excessive GPi inhibitory activity that results in tonic thalamic hypoactivity; indicated for rigidity and tremor ◦ Thalamotomy – producing a destructive lesion within the ventral intermediate nucleus of the thalamus; reduces longstanding tremor, improvement of rigidity � Deep brain stimulation – implantation of electrodes into the brain where they block nerve signals that cause symptoms � Neural transplantation – transplantation of cells capable of surviving and delivering dopamine into the striatum of pts with advanced PD; stem cells? ? ?
PROGNOSIS � Hoehn and Yahr Classification of Disability Stage I - Minimal or absent; unilateral if present ◦ ◦ Tremor of 1 limb Decreased arm swing Micrographia hypophonia
Stage II - Minimal bilateral or midline involvement; balance not impaired ◦ ◦ Sx’s evident in Stage I, plus Bradykinesia Stoop posture Shuffling gait
Stage III - Impaired righting reflex; unsteadiness when turning or rising from the chair; some activities are restricted but pt is independent ◦ Sx’s evident in Stages I & II, plus ◦ Pronounced gait disturbance ◦ Moderate general disability
Stage IV - All symptoms present and severe; standing and walking possible only with assistance ◦ Sx’s evident in Stages I, II & III, plus ◦ Significant disability
Stage V - Confined to bed or wheelchair ◦ Sx’x evident in Stages I, III & IV, plus ◦ Complete invalidism
Positive prognostic features: 1. Early tremor 2. Rigidity 3. Family history Negative prognostic features: 1. Bradykinesia 2. Akinesia 3. Postural instability 4. Gait difficulties 5. Cognitive defects 6. Late age of onset
PT Mx Relaxation techniques � A rocking chair is a good tool for pt relaxation � Rhythmic initiation � Jacobson’s progressive relaxation techniques – contract-relax � Lower trunk rotation with the pt hook-lying – to relax trunkal rigidity
ROM and mobility exercises � ROM should focus on strengthening the weak extensor muscles and stretch the tight flexor muscles � Prone-on-elbows and prone-on-extension – improve thoracic extension � PJM – to decrease tightness of joint capsule � Bilateral symmetrical D 2 flexion pattern – activates extensors in order to straighten the spine � Standing balance with rhythmic stabilization
Breathing exercises – emphasis on diaphragmatic breathing Clinical restorator – for conditioning Gait training ◦ Lengthen stride, widen the BOS ◦ Increase contralateral trunk movement and arm swing ◦ Place markers or blocks to help encourage the pt to widen the stride and avoid shuffling the feet PRE’s US – over the tight structures especially the shoulder HMP FES – emphasis on weak extensor muscles HEP – walking exercise
OTHER MOVEMENT DISORDERS
Huntington’s disease Relentless, progressive, adult-onset, autosomal dominant disorder that is associated with cell loss within a specific subset of neurons in the caudate nucleus and putamen � Cardinal features: involuntary movements, dementia, and behavioural changes � Clinical onset usually 30 -50 years of age, fatal outcome usually within 15 -20 years � Caused by mutant huntingtin � Pneumonia and cardiovascular changes – most common primary causes of mortality � Depression – most common psychological dysfunction � Hallmark: Chorea – excessive abrupt irregular spontaneous involuntary movements � Westphal variant: hypokinesia and rigidity � Chorea does not respond to physical therapy �

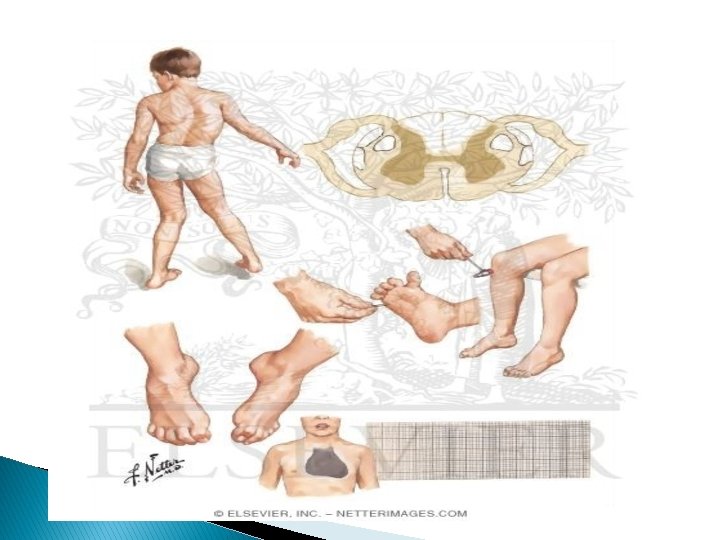
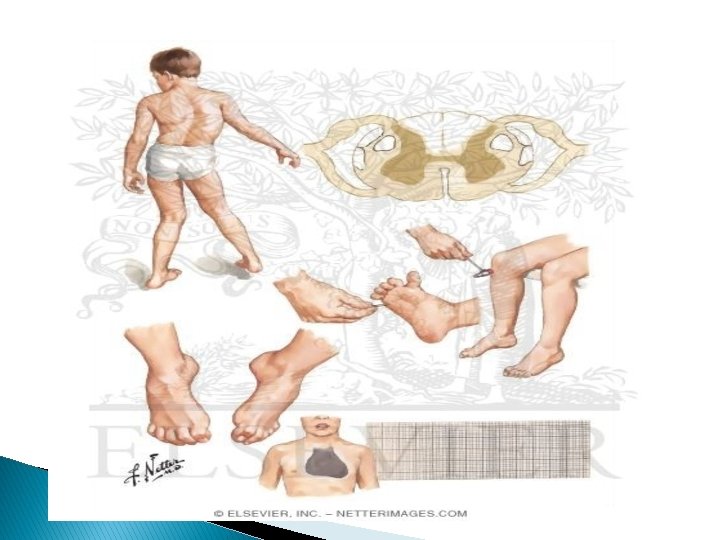
Hereditary ataxias � can result from disorders of the cerebellum or its connections � Friedreich ataxia – most common syndrome. It is a progressive disorder with the presentation of limb and gait ataxia with diminished muscle stretch reflexes, joint position sense, and vibratory appreciation
Hereditary spastic paraparesis �a group of inherited disorders in which the primary symptoms are progressive bilateral lower extremity spasticity and weakness caused by axonal degeneration in the spinal cord, maximally in the corticospinal tracts and the dorsal column fibers � Other names: familial spastic paraplegia, Strumpell. Lorrain syndrome � Progressive difficulty walking – classic presenting symptom � Cardinal features: symmetric lower extremity spastic paresis, extensor plantar responses � Tx: cold application, manual stretching techniques, splinting, serial casting, posture and body mechanics training, aerobic conditioning, and gait and dynamic balance training
Dystonia � movement disorder characterized by muscle contraction resulting in twisting, turning, and posturing as a result of sustained cocontraction of the agonist and antagonist � Tx: massage, slow stretching, US, gait training and mobility

Tourette syndrome �a constellation of symptoms including tic disorders and comorbid neurobehavioral problems � Tics – involuntary, sudden, rapid, repetitive, non-rythmic, stereotyped movements or vocalizations �Commonly involves the face, head and shoulders (sniffing, blinking, frowning, shoulder shrugging, head thrusting)

 Parkinsons disease hereditory
Parkinsons disease hereditory Parkinsons disease
Parkinsons disease Shy drager syndrome
Shy drager syndrome Is parkinsons hereditery
Is parkinsons hereditery Amantadin
Amantadin Mb behcet wikipedia
Mb behcet wikipedia Chronic granulomatous disease
Chronic granulomatous disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Jewish chronic disease hospital
Jewish chronic disease hospital Chronic kidney disease near atwater
Chronic kidney disease near atwater Dcld vs cld
Dcld vs cld Carlee oakley
Carlee oakley Stigmata of chronic liver disease
Stigmata of chronic liver disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Kate lorig chronic disease self-management
Kate lorig chronic disease self-management Wagner model of chronic disease management
Wagner model of chronic disease management Chronic disease
Chronic disease Stage 3 liver disease
Stage 3 liver disease Chronic disease
Chronic disease Pictures of lungs with copd
Pictures of lungs with copd Vijaya's echo criteria
Vijaya's echo criteria Present progressive passive
Present progressive passive Affirmative past progressive
Affirmative past progressive Past perfect past perfect progressive
Past perfect past perfect progressive Schizophrenia relapse
Schizophrenia relapse Progressive disease
Progressive disease Definition of chronic toxicity
Definition of chronic toxicity Chronic care model definition
Chronic care model definition Definition of chronic toxicity
Definition of chronic toxicity Chronic pain definition
Chronic pain definition Bharathi viswanathan
Bharathi viswanathan Angioectasia icd 10
Angioectasia icd 10 Flinders model of chronic care self-management limitations
Flinders model of chronic care self-management limitations Earthy look in chronic renal failure
Earthy look in chronic renal failure Pulpitis classification
Pulpitis classification Chronic blood loss
Chronic blood loss Cholecystitis pathogenesis
Cholecystitis pathogenesis Fibromyalgia vs chronic fatigue
Fibromyalgia vs chronic fatigue Pulpitis classification
Pulpitis classification Acute inflammation definition
Acute inflammation definition Prescriptive screening vs prospective
Prescriptive screening vs prospective Hemolysis ldh haptoglobin
Hemolysis ldh haptoglobin Chronic unease in the workplace
Chronic unease in the workplace Chronic calculous cholecystitis
Chronic calculous cholecystitis Chronic blood loss
Chronic blood loss Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Acute subacute chronic
Acute subacute chronic Hetrotropia
Hetrotropia Chronic gout
Chronic gout Chronic blood loss
Chronic blood loss Turban epiglottis meaning
Turban epiglottis meaning Gastritis type a
Gastritis type a