Parenteral Nutrition in Critical Illness Judy WONG Dietitian



- Slides: 57
Parenteral Nutrition in Critical Illness Judy WONG Dietitian PMH
Overview What is parenteral nutrition Selection Criteria of parenteral nutrition Parenteral nutrition access Requirements of critically ill patients Refeeding Syndrome Parenteral Nutrition formulations & How to choose Case Study
What is Parenteral Nutrition Parenteral nutrition refers to the infusion of intravenous nutrition formula into the bloodstream DAA, 2011
Selection Criteria for Parenteral Nutrition Should be used in patients who are or will become malnourished, and Who do not have sufficient gastrointestinal function to be able to restore / maintain nutritional status Mc. Clave et al. , 2009
Access of parenteral nutrition
Access of parenteral nutrition Central parenteral nutrition (CPN) To large, high blood flow vein (e. g. superior vena cava) For long term parenteral nutrition Central Parenteral Nutrition solution osmolarity can be > 900 m. Osm/L More suitable for volume-sensitive patients (e. g. patients with heart, renal or liver problem)
Access of parenteral nutrition Peripheral parenteral nutrition (PPN) Catheter tip placement in a small vein (e. g. forearm) Peripherall. Parenteral Nutrition solution osmolarity < 900 m. Osm/L Usually do not fully meet nutrition requirements Use as: Supplemental feeding Transition to oral/enteral feeding Temporary PN when central access has not been initiated
Requirements of critically ill patients Energy requirement Macronutrient requirements Micronutrient requirements
Requirements during metabolic stress Adequate energy is essential for metabolically stressed patients Avoidance of overfeeding in the critically ill patients is important Excess calories can result in complications: hyperglycaemia hepatic steatosis excess CO 2 production (exacerbate respiratory insufficiency / prolong weaning from mechanical ventilation) Krause’s, 2012
How much energy should critically ill patients receive? ESPEN Guidelines 2009: “as close as possible to the energy expenditure in order to decrease negative energy balance” (Grade B); “in the absence of indirect calorimetry, ICU patients should receive 25 kcal/kg/day increasing to target over the next 2 -3 days” (Grade C) Singer P et al (2009)
Calculations of requirement Estimation of energy requirement = Basal Metabolic Rate (BMR) + Activity Factor + Stress Factor
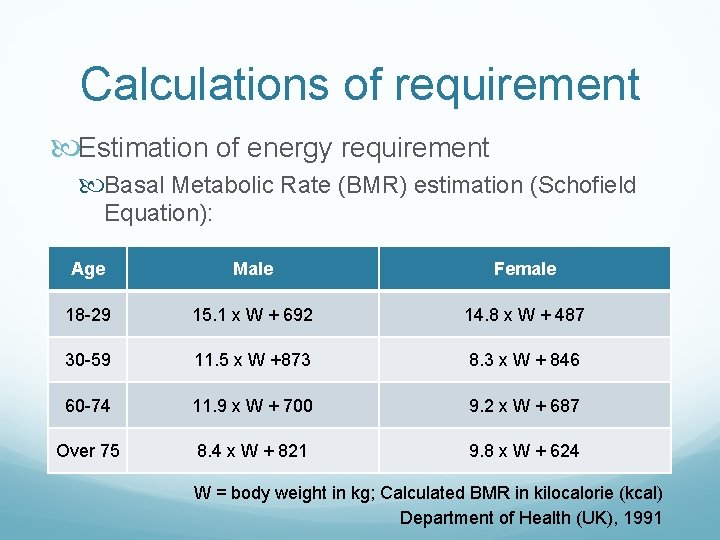
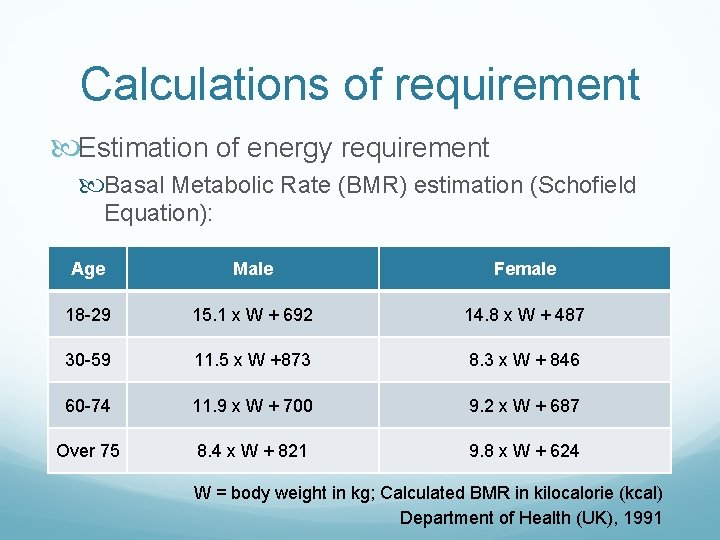
Calculations of requirement Estimation of energy requirement Basal Metabolic Rate (BMR) estimation (Schofield Equation): Age Male Female 18 -29 15. 1 x W + 692 14. 8 x W + 487 30 -59 11. 5 x W +873 8. 3 x W + 846 60 -74 11. 9 x W + 700 9. 2 x W + 687 Over 75 8. 4 x W + 821 9. 8 x W + 624 W = body weight in kg; Calculated BMR in kilocalorie (kcal) Department of Health (UK), 1991
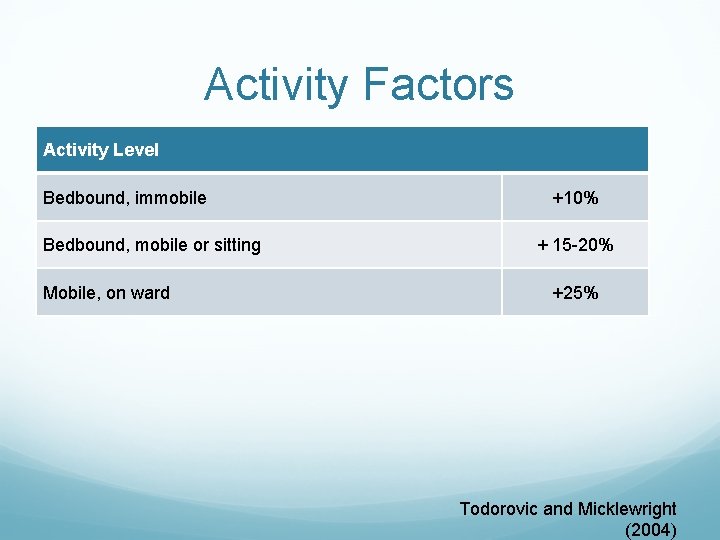
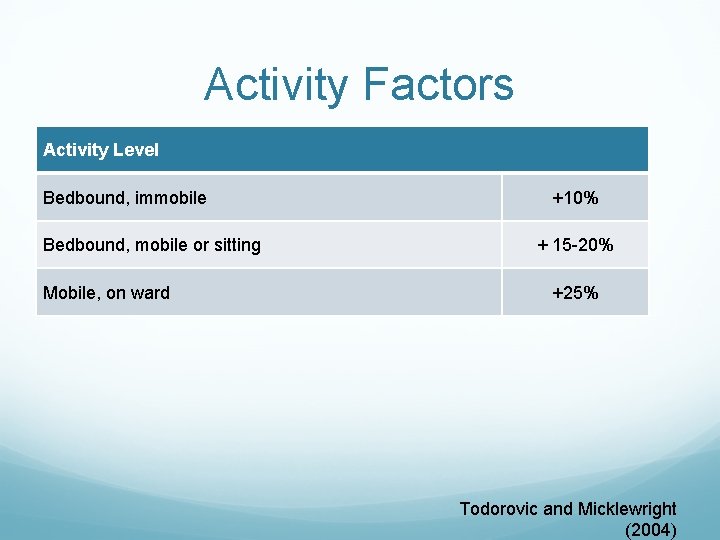
Activity Factors Activity Level Bedbound, immobile Bedbound, mobile or sitting Mobile, on ward +10% + 15 -20% +25% Todorovic and Micklewright (2004)
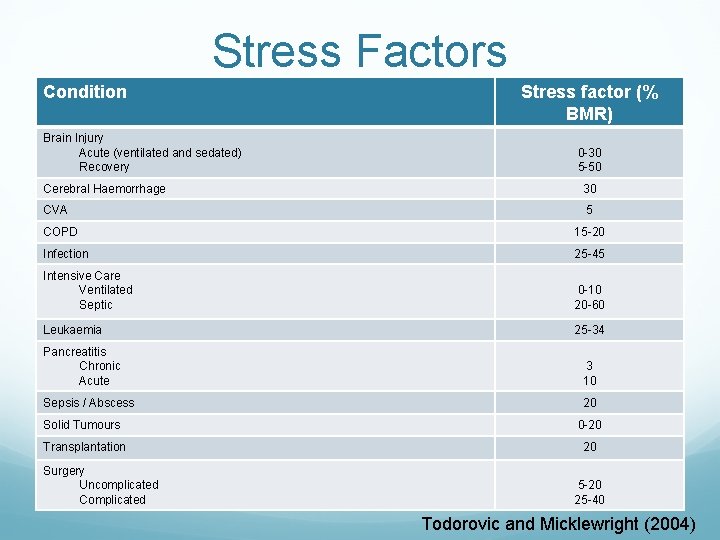
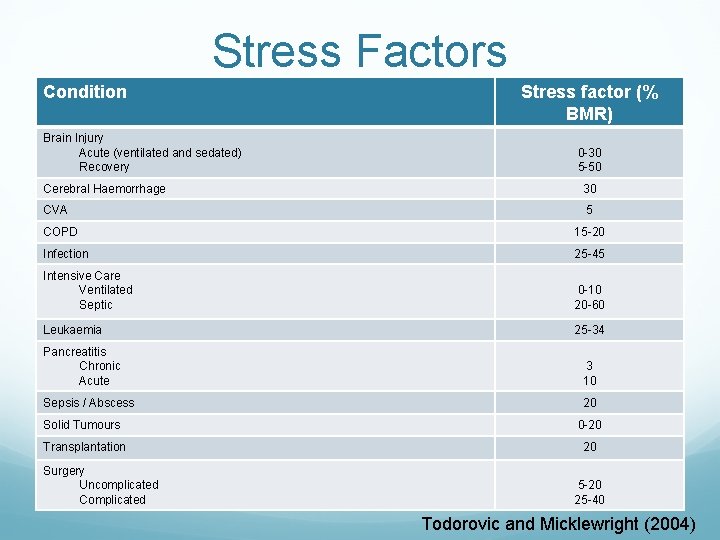
Stress Factors Condition Brain Injury Acute (ventilated and sedated) Recovery Stress factor (% BMR) 0 -30 5 -50 Cerebral Haemorrhage 30 CVA 5 COPD 15 -20 Infection 25 -45 Intensive Care Ventilated Septic 0 -10 20 -60 Leukaemia 25 -34 Pancreatitis Chronic Acute 3 10 Sepsis / Abscess 20 Solid Tumours 0 -20 Transplantation 20 Surgery Uncomplicated Complicated 5 -20 25 -40 Todorovic and Micklewright (2004)
Macronutrients Requirements
Macronutrient requirements Protein depending on the baseline nutritional status, degree of injury and metabolic demand, or any abnormal losses (e. g. open wound or burned skin) Varies between 0. 9 -1. 5 g/kg/day for various conditions Krause’s, 2012
Macronutrient requirements Carbohydrate Ensures that protein is not catabolised for energy during metabolism Excessive administration: hyperglycaemia hepatic abnormalities ventilatory drives Maximum infusion rate of carbohydrate: <5 mg/minute/kg body weight DAA, 2011
Macronutrient requirements Fat ~ 10% of calories/day from fat provide 2% to 4% of calories from linoleic acid (LA) in order to prevent Essential Fatty Acid Deficiency Soybean and safflower oils: rich sources of LA LA: pro-inflammatory & immunosuppressive Maximum infusion rate of fat: <0. 11 g/hour/kg body weight DAA, 2011
Micronutrient Requirements
Micronutrient requirements Ready-made Parenteral Nutritional Products are free of vitamins and trace elements The addition of vitamins and trace elements are always required ESPEN Guidelines 2009; Casaer & Van den Berghe, 2014
Micronutrients Vitamins and trace elements addition via the addition of: Soluvit® N Vitalipid N® Adult Addamel® N
Soluvit® N provide the daily requirement of water-soluble vitamins A vial (10 ml) = normal daily requirement of water-soluble vitamins Fresenius Kabi
Vitalipid N® Adult meet the daily requirement of the fat-soluble vitamins A, D 2, E and K 1 in adults & children aged 11 years or older One ampoule (10 ml) = daily intake of fat-soluble vitamins Contraindications: hypersensitivity to egg protein / soybean / peanut protein Fresenius Kabi
Addamel® N covers basal or moderately trace elements needs The recommended daily does for adult patients with basal or moderately elevated needs is 10 ml (one ampoule) Contraindications: in patients with blocked bile flow, and manganese levels must be checked if treatment lasts > 4 weeks Fresenius Kabi
Refeeding Syndrome
Refeeding Syndrome 1. What is refeeding syndrome? A metabolic disorder as a consequence of too aggressive administration of nutrition after a prolonged inadequate nutrition supply Characterized by hypophosphataemia, hypomagnesiumaemia and hypokalaemia; with excessive sodium and fluid retention May cause potentially lethal electrolye flucatuations involving metabolic, haemodynamic & neuromuscular problems Stanga, Z et al (2008) Krause’s (2012) Mehanna et al (2008)
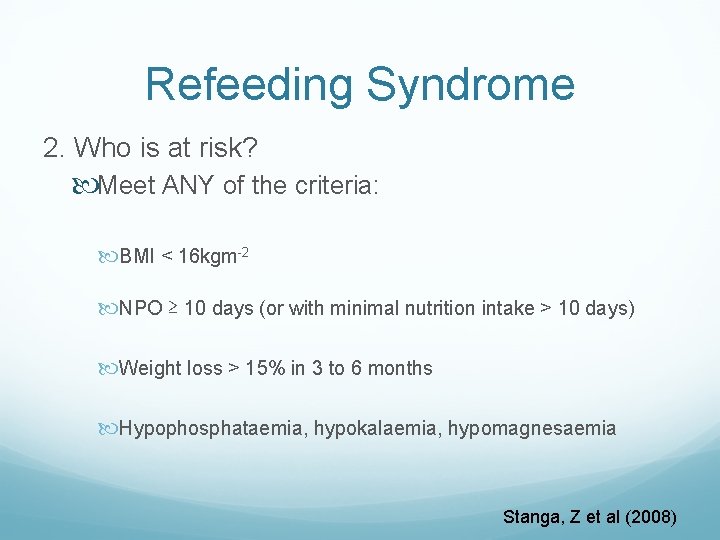
Refeeding Syndrome 2. Who is at risk? Meet ANY of the criteria: BMI < 16 kgm-2 NPO ≥ 10 days (or with minimal nutrition intake > 10 days) Weight loss > 15% in 3 to 6 months Hypophosphataemia, hypokalaemia, hypomagnesaemia Stanga, Z et al (2008)
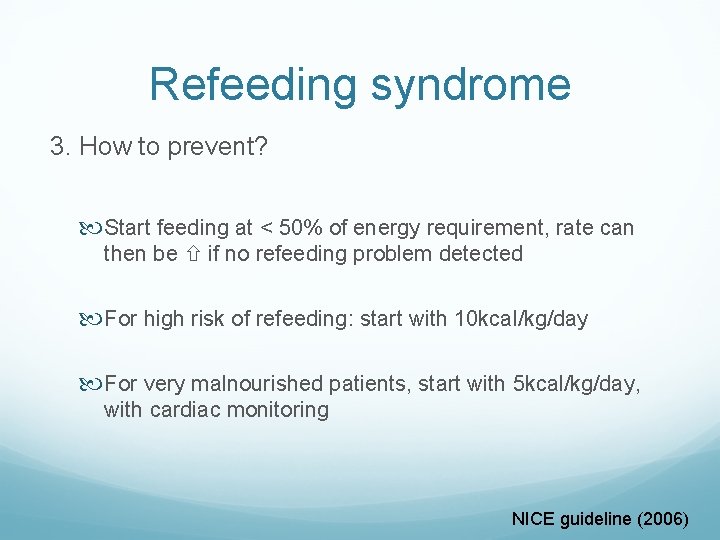
Refeeding syndrome 3. How to prevent? Start feeding at < 50% of energy requirement, rate can then be if no refeeding problem detected For high risk of refeeding: start with 10 kcal/kg/day For very malnourished patients, start with 5 kcal/kg/day, with cardiac monitoring NICE guideline (2006)
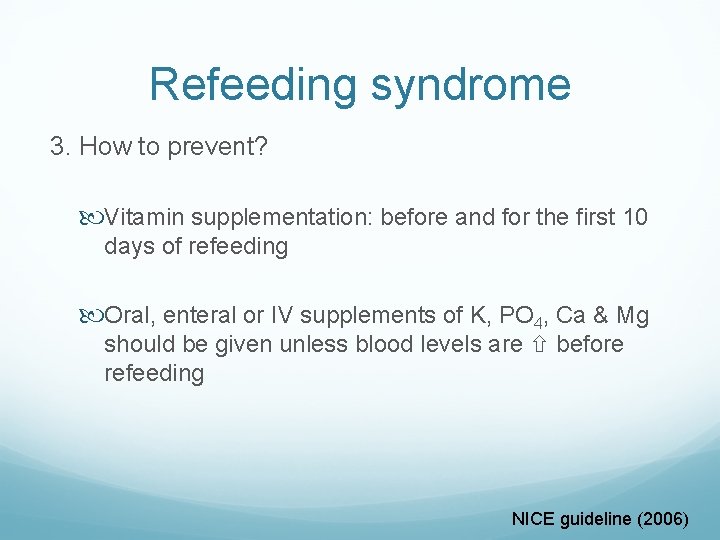
Refeeding syndrome 3. How to prevent? Vitamin supplementation: before and for the first 10 days of refeeding Oral, enteral or IV supplements of K, PO 4, Ca & Mg should be given unless blood levels are before refeeding NICE guideline (2006)

PN formulations
Currently available formulations in PMH
PN Formulations Besides carbohydrate and protein content varies, type of fat emulsions used also differ Most commonly used is soybean oil based fat emulsion Alternatively fat emulsions: Soybean oil + MCT Soybean oil + Olive Oil Fish oil other multi-lipids (a mixture of soy, MCT, olive and fish oil) DAA, 2011 ASPEN Position Paper, 2012
Soybean oil Examples: Kabiven Central, Kabiven Peripheral The most commonly used fat emulsion type Linoleic Acid (LA, n-6) comprise a 50% of total fatty acid profile Alpha Linolenic Acid (ALA, n-3) about 10% of total fatty acid profile omega 6 content drawback due to its pro-inflammatory potential ASPEN Position Paper (2012)
Soybean oil + MCT Examples: Nutriflex Lipid Special, Nutriflex Lipid Plus Soybean oil : MCT = 50 : 50 MCT: readily oxidizable Safe source of lipid pro-inflammatory properties
Soybean oil + Olive oil Examples: Oliclinomel Olive oil : soybean oil = 80 : 20 the content of omega 6 in formulation by ~ 75% Higher vitamin E content for its anti-oxidating properties ASPEN Position Paper (2012)
Multi-lipids Examples: SMOF Kabiven A mixture of soybean oil, MCT, olive oil and fish oil in a ratio of 30 : 10 Fish Oil: rich in omega 3 (anti-inflammatory properties) ASPEN Position Paper (2012)
How to choose?
How to choose? 1. Based on calculated energy / protein requirements 2. Disease Specific: Renal / Cardiac diseases Vs Fluid content of PN BGA / p. CO 2 Vs CHO content
Initiation of parenteral nutrition
Initiation of Parenteral Nutrition 1. Ensure the selected formulation is compatible with the route of parenteral nutrition (central / peripheral) 2. Choice of parenteral nutrition regimen Continuous PN (Q 24 H) Cyclic / intermittent (Q 16 H/Q 12 H) 3. Ensure final infusion rate DOES NOT exceed the maximum infusion rate for fat and CHO
Case Study
Case Study Background Information KC, 57 year-old male, admitted to PMH on 5 Aug 2013 Admission Diagnosis: Malnutrition Past Medical History: HT, anaemia, Ca cardia with oseophagogastrectomy, short bowel syndrome, CHB Relevant Medications: Aminoleban EN (1 sachet), Entecavir, Vitamin K 1, Slow K, Vitamin B complex
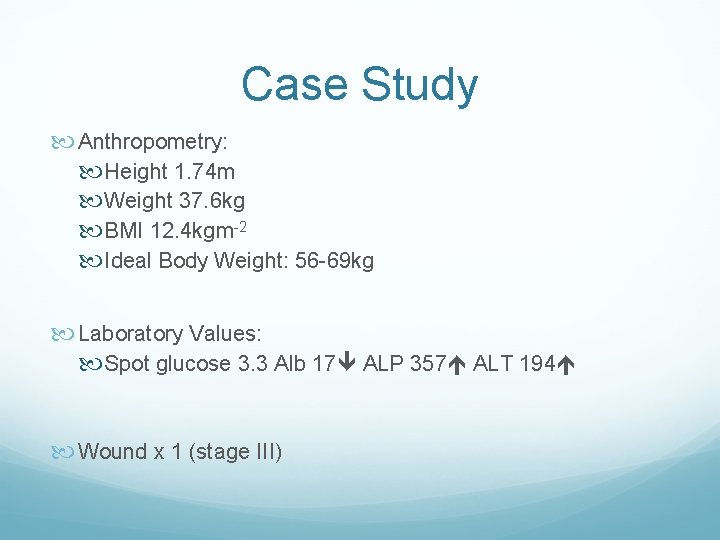
Case Study Anthropometry: Height 1. 74 m Weight 37. 6 kg BMI 12. 4 kgm-2 Ideal Body Weight: 56 -69 kg Laboratory Values: Spot glucose 3. 3 Alb 17 ALP 357 ALT 194 Wound x 1 (stage III)
Case Study Estimated energy requirement: ~ 2000 -2100 kcal (bedbound + weight ) Estimated protein requirement: ~56 -69 g per day Route of nutrition: 1. Oral (as much as tolerated) 2. Peripheral parenteral nutrition
Case Study 1. Formula selection: Peripheral access = Kabiven Peripheral Plan to start with small infusion rate and grade up as tolerated
Case Study 2. Starting PN: 30 ml/hr x 16 hrs Kabiven Peripheral (+ Addamel N / Vitalipid N Adult / Soluvit N) (~333 kcal, 11 g protein) Gradually stepped up to 100 ml/hr x 16 hrs (~1167 kcal, 37 g protein) (Note: Maximum infusion rate: < 139 ml/hr for 37. 6 kg)
One Month later (5 Sept 2013)
One month later Laboratory values: Spot glu 5. 7, Alb 13 , ALP/ALT normal Wound healed Oral intake: ~200 ml/meal Stool: BOx 1 per day PICC (central line) to be inserted the next day
One month later PN consideration: 1. To central formula (for more nutrition to meet requirement) 2. Per case MO, patient cannot tolerate excessive volume Nutriflex Lipid Special (1250 ml/1475 kcal/72 g protein)
One month later Recommendation: 1. Nutriflex Lipid Special (+ Addamel N / Vitalipid N Adult / Soluvit N) 2. Start with 20 ml/hr x 24 hr, gradually step up to 52 ml/hr x 24 hr (~1475 kcal, 72 g protein)
10 months since first admission

10 months later Date Weight (kg) BMI (kgm-2) 6/8/2013 37. 6 12. 4 11/12/2013 41. 2 13. 6 15/1/2014 44. 9 14. 8 22/1/2014 46 15. 2 29/1/2014 48. 1 15. 9 5/2/2014 48. 4 16. 0 11/2/2014 48. 8 16. 1 26/2/2014 49 16. 2 17/3/2014 50 16. 5 24/3/2014 50. 8 16. 8 31/3/2014 51 16. 8 3/6/2014 54. 5 kg 18. 0
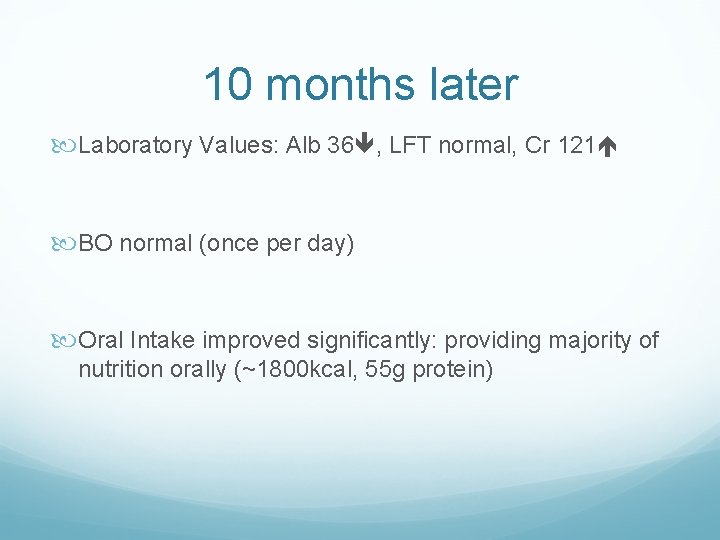
10 months later Laboratory Values: Alb 36 , LFT normal, Cr 121 BO normal (once per day) Oral Intake improved significantly: providing majority of nutrition orally (~1800 kcal, 55 g protein)
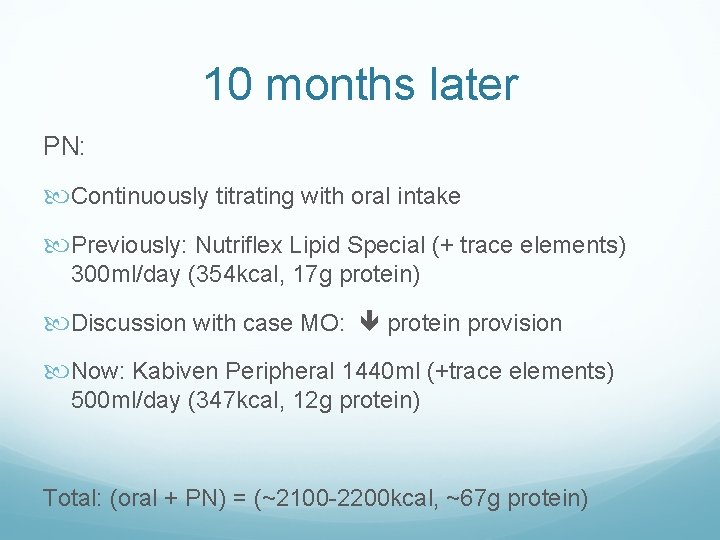
10 months later PN: Continuously titrating with oral intake Previously: Nutriflex Lipid Special (+ trace elements) 300 ml/day (354 kcal, 17 g protein) Discussion with case MO: protein provision Now: Kabiven Peripheral 1440 ml (+trace elements) 500 ml/day (347 kcal, 12 g protein) Total: (oral + PN) = (~2100 -2200 kcal, ~67 g protein)

Q & A Session
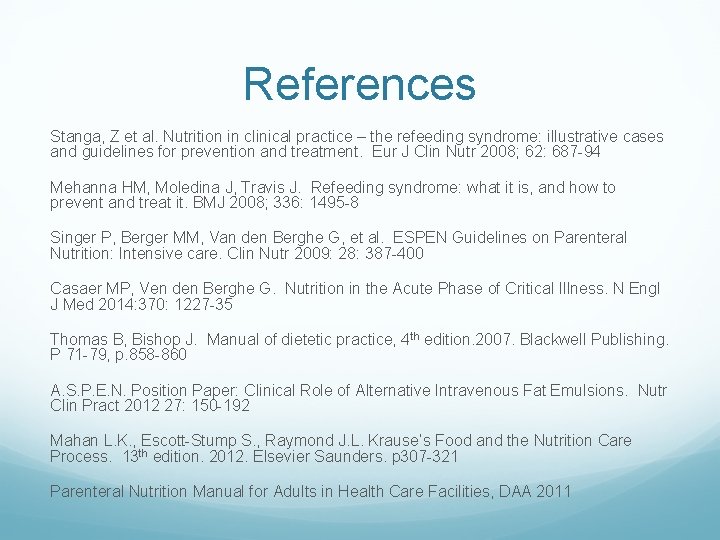
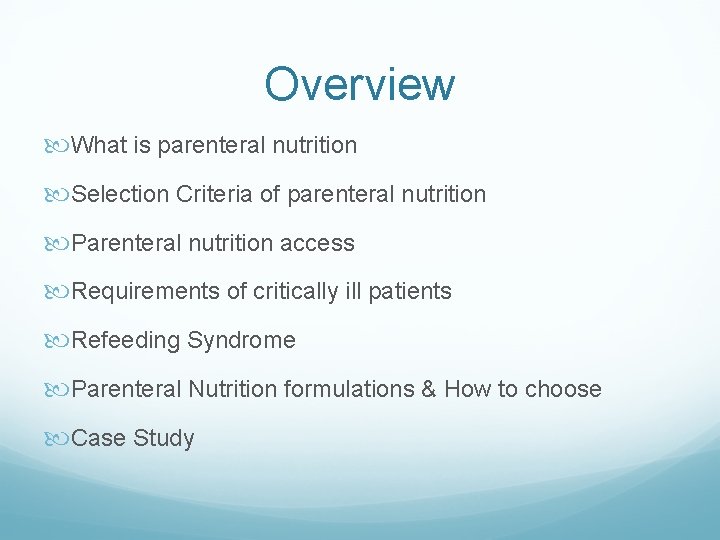
References Stanga, Z et al. Nutrition in clinical practice – the refeeding syndrome: illustrative cases and guidelines for prevention and treatment. Eur J Clin Nutr 2008; 62: 687 -94 Mehanna HM, Moledina J, Travis J. Refeeding syndrome: what it is, and how to prevent and treat it. BMJ 2008; 336: 1495 -8 Singer P, Berger MM, Van den Berghe G, et al. ESPEN Guidelines on Parenteral Nutrition: Intensive care. Clin Nutr 2009: 28: 387 -400 Casaer MP, Ven den Berghe G. Nutrition in the Acute Phase of Critical Illness. N Engl J Med 2014: 370: 1227 -35 Thomas B, Bishop J. Manual of dietetic practice, 4 th edition. 2007. Blackwell Publishing. P 71 -79, p. 858 -860 A. S. P. E. N. Position Paper: Clinical Role of Alternative Intravenous Fat Emulsions. Nutr Clin Pract 2012 27: 150 -192 Mahan L. K. , Escott-Stump S. , Raymond J. L. Krause’s Food and the Nutrition Care Process. 13 th edition. 2012. Elsevier Saunders. p 307 -321 Parenteral Nutrition Manual for Adults in Health Care Facilities, DAA 2011
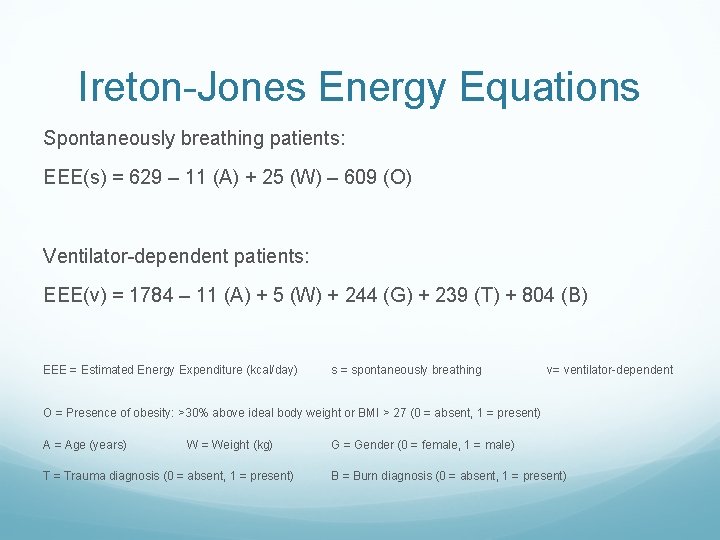
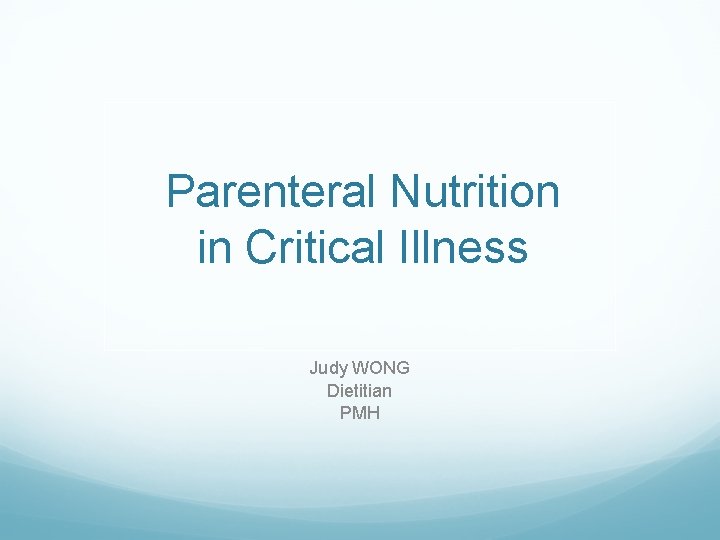
Ireton-Jones Energy Equations Spontaneously breathing patients: EEE(s) = 629 – 11 (A) + 25 (W) – 609 (O) Ventilator-dependent patients: EEE(v) = 1784 – 11 (A) + 5 (W) + 244 (G) + 239 (T) + 804 (B) EEE = Estimated Energy Expenditure (kcal/day) s = spontaneously breathing v= ventilator-dependent O = Presence of obesity: >30% above ideal body weight or BMI > 27 (0 = absent, 1 = present) A = Age (years) W = Weight (kg) T = Trauma diagnosis (0 = absent, 1 = present) G = Gender (0 = female, 1 = male) B = Burn diagnosis (0 = absent, 1 = present)