Parenteral Medications and Sterile Fluids Injections are sterile








- Slides: 30

Parenteral Medications and Sterile Fluids
Injections are sterile, pyrogen-free preparations intended to be administered parenterally. l The term parenteral refers to the injectable routes of administration. l Greek words para and enteron mean outside of the intestine. l It denotes routes of administration other than the oral route. l
Injections… cont. l l l Rapid drug action is desired Emergency situations The patient is uncooperative The patient is unconscious Unable to accept or tolerate mediations by oral route The drug is ineffective by other routes

Injections… cont. l l l l l Joints = intra-articular Joint fluid area = intrasynovial Spinal column = intraspinal Refer to page 287 Spinal fluid = intrathecal Arteries = intra-arterial Heart = intracardic Vein = intravenous (I. V. ) Muscle = intramuscular (I. M. ) Into the skin = intradermal (I. D. ) Under the skin = subcutaneous (S. C. , Sub-Q, S. Q. )
Intravenous Route l Once the drug is administered intravenously, it cannot be retrieved. l In the case of an adverse reaction to the drug, for instance, the drug cannot be easily removed from the circulation as it could, for example, by the induction of vomiting following the oral administration of the same drug.
Intravenous Route … cont. l Not only are the injectable solutions sterile, the syringes and needles employed must also be sterilized and the entrance must be disinfected to reduce the chance of carrying bacteria from the skin into the blood via the needle.

Intravenous Route … cont. l l l The main hazard of intravenous infusion is the possibility of thrombus formation induced by the touching of the wall of the vein by catheter or needle. Thrombi are more likely to occur when the infusion solution is of an irritating nature to biological tissues. A thrombus is a blood clot formed within the blood vessel or (heart) due to a slowing of the circulation or to an alteration of the blood or vessel wall. Once such a clot circulated, it becomes embolus, carried by the blood stream until it lodges in a blood vessel, obstructing it, and resulting in a blockage or occlusion known as embolism. Such an obstruction may be of a critical hazard to the patient, depending upon the site and severity of the obstruction.
Intramuscular Route l l l I. M. injections of drugs provide drug effects that are less rapid, but generally of greater duration than those obtained from intravenous administration. Aqueous or oleaginous solutions or suspensions of drug substances may be administered intramuscularly. I. M. injections are performed deep into the skeletal muscles, and the point of injection should be as far as possible from major nerves and blood vessels to prevent any possible injuries to the patient. In adult, the upper outer quadrant of the gluteus maximus is the most frequently used site for I. M. In infants and young children, the deltoid muscles of the upper arm is preferred.

Deltoid muscles Gluteus maximus Long acting drugs are commonly referred to as “DEPOT” preparations

Subcutaneous Route l It is utilized for the injection of small amounts of medication. l The site of injection is rotated when injections are frequently given. l Insulin is an example of drugs given by such route.
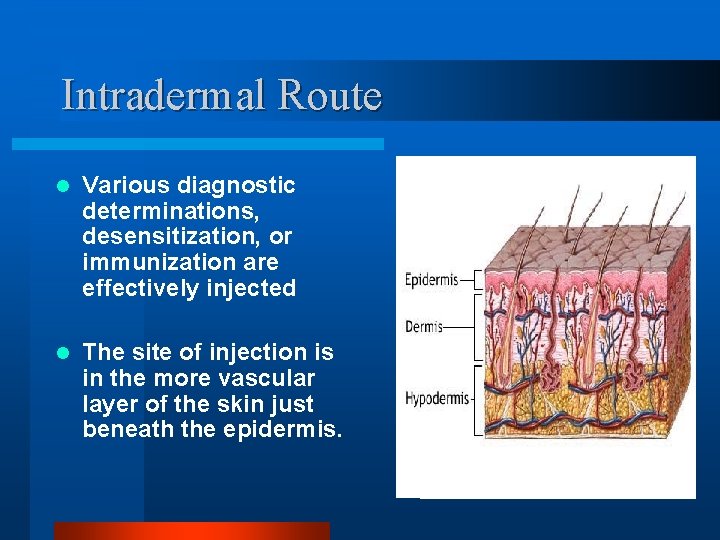
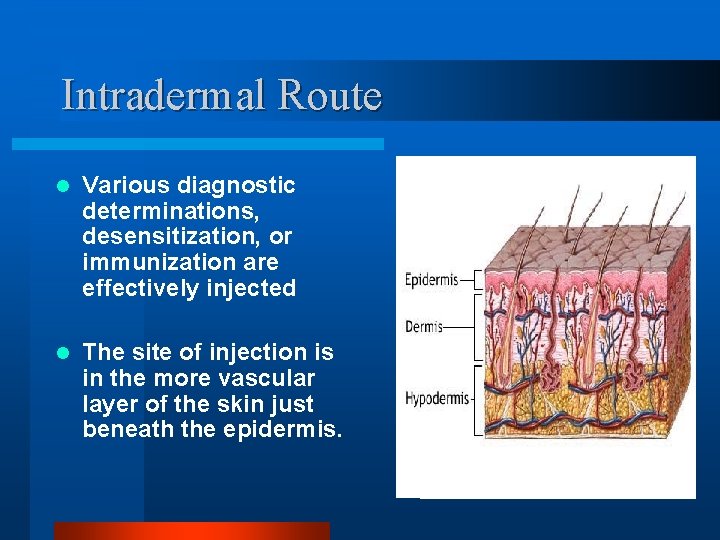
Intradermal Route l Various diagnostic determinations, desensitization, or immunization are effectively injected l The site of injection is in the more vascular layer of the skin just beneath the epidermis.
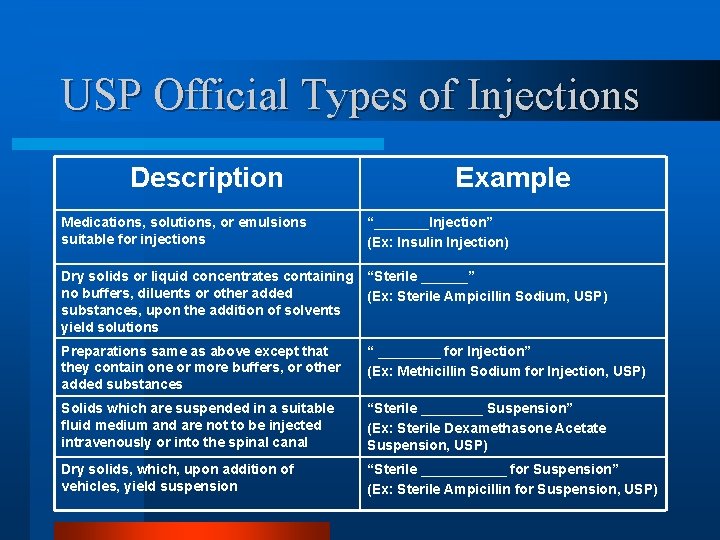
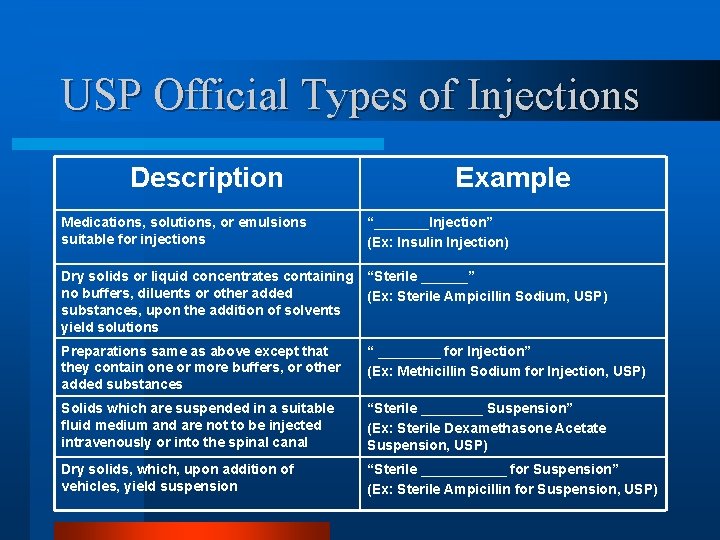
USP Official Types of Injections Description Medications, solutions, or emulsions suitable for injections Example “_______Injection” (Ex: Insulin Injection) Dry solids or liquid concentrates containing “Sterile ______” no buffers, diluents or other added (Ex: Sterile Ampicillin Sodium, USP) substances, upon the addition of solvents yield solutions Preparations same as above except that they contain one or more buffers, or other added substances “ ____ for Injection” (Ex: Methicillin Sodium for Injection, USP) Solids which are suspended in a suitable fluid medium and are not to be injected intravenously or into the spinal canal “Sterile ____ Suspension” (Ex: Sterile Dexamethasone Acetate Suspension, USP) Dry solids, which, upon addition of vehicles, yield suspension “Sterile ______ for Suspension” (Ex: Sterile Ampicillin for Suspension, USP)

Solvents and Vehicles for Injections Water for Injection • Purified by distillation or by reverse osmosis • May not contain added substances • Although water for injection is not required to be sterile, it must be pyrogen free • It is intended to be used in the manufacture of injectable products which are to be sterilized after preparation. • It should be stored in tight containers • It should be used within 24 hours following its collection
Solvents and Vehicles for Injections…cont. Sterile Water for Injection • It has been sterilized and packaged in single dose containers • It must be pyrogen free and may not contain an antimicrobial agents or other added substance • This water is intended to be used as a solvent, vehicle or diluent for already sterilized and packaged injectable medications.
Solvents and Vehicles for Injections…cont. Bacteriostatic Water for Injection, USP • It is a sterile water • It contains one or more antimicrobial agents • It is packaged in prefilled syringe or in vials • The container label must state the name and proportion of the antimicrobial agent(s) present

Solvents and Vehicles for Injections…cont. Bacteriostatic Water for Injection, USP …cont. • The presence of the bacteriostatic agent gives the flexibility for multiple dose vials • Because of the presence of antimicrobial agents, the water must only be used in parenterals that are administered in small volumes • In using bacteriostatic water for injection, the compatibility of the bacteriostatic agent(s) present with the particular medicinal agent being dissolved or suspended must be considered
Solvents and Vehicles for Injections…cont. Sodium Chloride Injection, USP • It is a sterile isotonic solution of sodium chloride in water for injection • It contains no antimicrobial agents • The solution may be used as a sterile vehicle in preparing solutions or suspensions of drugs for parenteral administration

Solvents and Vehicles for Injections…cont. Bacteriostatic Sodium Chloride Injection, USP • It is a sterile isotonic solution of sodium chloride in water for injection • It contains one or more antimicrobial agents • Sodium chloride is present at 0. 9% concentration to render the solution isotonic
Solvents and Vehicles for Injections…cont. Ringer’s Injection, USP • It is a sterile solution of sodium chloride, potassium chloride and calcium chloride in water for injection • The three solutions are present in concentrations similar to that found in physiologic fluids • The solution is used as a vehicle for other drugs, or alone as an electrolyte replenisher and fluid extender
Solvents and Vehicles for Injections…cont. Lactate Ringer’s Injection, USP • It has different quantities of the same three salts (sodium chloride, potassium chloride and calcium chloride) in Ringer’s injection and contains sodium lactate. • This injection is a fluid and electrolyte replenisher and a systemic alkalizer.
Solvents and Vehicles for Injections…cont. Nonaqueous Vehicles • Although an aqueous vehicle is generally preferred for an injection, its use may be precluded in a formulation due to the limited water solubility of a medicinal substance or its susceptibility to hydrolysis.
Solvents and Vehicles for Injections…cont. The selected Vehicles 1. Nonirritating 2. Non toxic 3. Non-sensitizing 4. Must no exert pharmacological activity 5. It must not affect the activity of medicinal agents 6. Physically and chemically stable at various p. H levels. 7. Its viscosity must be such as to allow ease of injection (syringeability) 8. Its fluidity must be maintained over a wide temperature 9. Its boiling point must be sufficiently enough to permit heat sterilization
Solvents and Vehicles for Injections…cont. Examples of the non aqueous vehicles 1. Vegetable oils 2. Glycerin 3. Polyethylene glycol 4. Propylene glycol 5. Alcohol 6. Other agents (ethyl oleate, isopropyl myristate …. etc.
Solvents and Vehicles for Injections…cont. Note: 1. USP specifies restrictions on the use of fixed vegetable oils which may be employed in parenteral products. For one thing, they must remain clear when cooled to 10 °C to ensure the stability and clarity of the injectable product upon storage under refrigeration. 2. The oils must not contain mineral oil or paraffin, as these materials are not absorbed by body tissues. 3. Some patients exhibit allergic reactions to specific oils. Thus, when vegetable oils are used, the label must state the specific oil present. 4. The most commonly used fixed oils in injection are corn, cottonseed oil, peanut oil, and sesame oil. Castor oil and olive oil have been used on occasion.
Solvents and Vehicles for Injections…cont. Added substances: 1. Antibacterial preservatives 2. Buffers 3. Solubilizers 4. Antioxidants
Total Parenteral Nutrition (TPN)
TPN l Energy substrates l Carbohydrate l Protein l Lipid l Fluid and electrolyte requirements l Vitamin requirements
TPN l l l Determining whether a patient is a suitable candidate for nutrition support requires a careful clinical evaluation guided by the general principles. This decision requires consideration of the following questions: Will this patient be unable to eat or attain adequate enteral intake within 5 to 7 days? Is an extended period of functional postoperative starvation likely in this patient? Is there clear evidence of clinical markers for ongoing metabolic stress (e. g. , ventilator dependency, fever, sepsis) requiring additional calories to support an ongoing injury response? Was this patient previously malnourished, suggesting that a period of nutrition support may be beneficial in the hypermetabolic phase of illness, stress, operation, and recovery?
General Considerations for the Administration of Total Parenteral Nutrition l l l l When writing or reviewing TPN orders, the physician must consider a number of factors. These factors include: Volume status of the patient. Energy requirements to sustain the patient’s response to illness, injury, sepsis, or infection. Fulfillment of caloric needs by glucose, lipid, and protein substrates. Electrolyte, vitamin, and other micronutrient requirements. Concurrent illnesses. Presence of associated enteral access.
Other Parenteral Products or Formulations l Biologics: refers to such pharmaceutical products as vaccines, toxins, toxoids, blood derivatives, …etc l Most biologics are stored in a refrigerator at between 2 °C to 8 °C, and freezing is avoided
 Insidan region jh
Insidan region jh Sterile vs non sterile compounding
Sterile vs non sterile compounding Parts of syringe
Parts of syringe Circular flow of income injections and withdrawals
Circular flow of income injections and withdrawals Chapter 11 medications and drugs
Chapter 11 medications and drugs Chalzion
Chalzion Glutathione injection in dubai
Glutathione injection in dubai Masseter boto
Masseter boto Jawline filler dubai
Jawline filler dubai Glutathione injections in dubai
Glutathione injections in dubai Gow gates
Gow gates Skin whitening injection in dubai
Skin whitening injection in dubai Needle sizes for injections
Needle sizes for injections Nasopalatine nerve block
Nasopalatine nerve block Common pediatric medications
Common pediatric medications Tuohy needle sizes
Tuohy needle sizes Hepatitis d
Hepatitis d List of high-alert medications jci
List of high-alert medications jci Mock code steps
Mock code steps 5 rights of medication
5 rights of medication Drug distribution system in hospital pharmacy
Drug distribution system in hospital pharmacy Chapter 30 administering medications
Chapter 30 administering medications Medications
Medications Debbie norrie
Debbie norrie Medication reconciled meaning
Medication reconciled meaning High risk medications
High risk medications Chapter 30 administering medications
Chapter 30 administering medications Peripheral nervous system medications
Peripheral nervous system medications Solids liquids and gases section 2 properties of fluids
Solids liquids and gases section 2 properties of fluids Compressible and incompressible fluids
Compressible and incompressible fluids Australian standards for texture modified foods and fluids
Australian standards for texture modified foods and fluids