Parastomal hernia Dr Chan Wai Hei Arthur Queen


- Slides: 38
Parastomal hernia Dr Chan Wai Hei, Arthur Queen Elizabth Hospital
Overview § Background § Classification § Risk factors § Clinical presentation & Complications requiring surgical intervention § Management § Prevention
Definition § A parastomal hernia (PSH) is a type of incisional hernia that occurs at the site of stoma or immediately adjacent to the stoma § The most common late complication of a permanent stoma
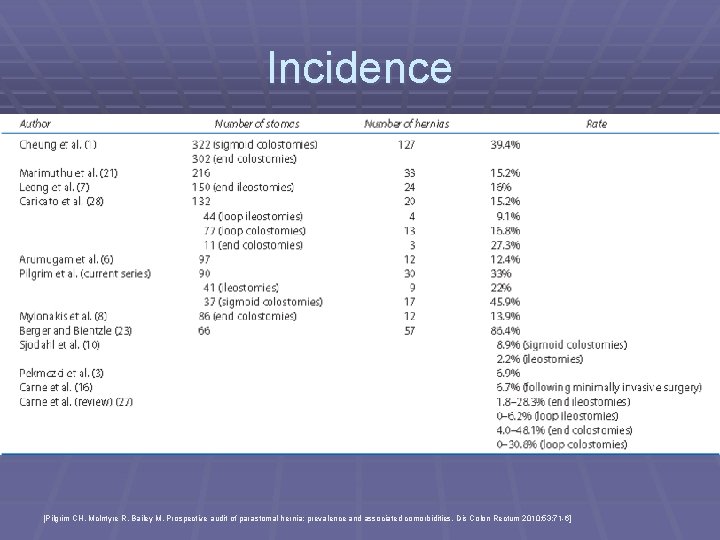
Incidence § Variable incidence reported in literature § Incidence increases with time § Most occur within 2 years of stoma formation § Some believe that it is an inevitable consequence of stoma formation
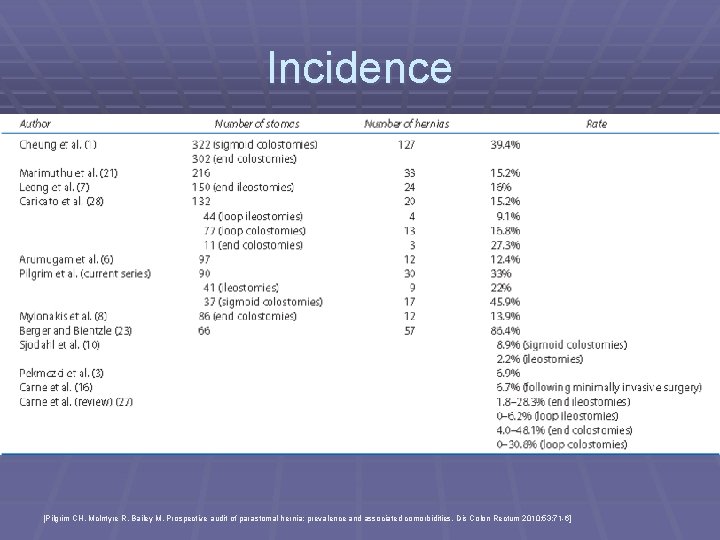
Incidence [Pilgrim CH, Mc. Intyre R, Bailey M. Prospective audit of parastomal hernia: prevalence and associated comorbidities. Dis Colon Rectum 2010; 53: 71 -6]
Incidence § Literature review by Carne et al. § 1. 8 -28. 3% in end ileostomies § 0 -6. 2% in loop ileostomies § 4. 0 -48. 1% in end colostomies § 0 -30. 8% in loop colostomies [Carne PW, Robertson GM, Frizelle FA. Parastomal hernia. Br J Surg 2003; 90: 784 -93]
Classification § Traditional § Radiological
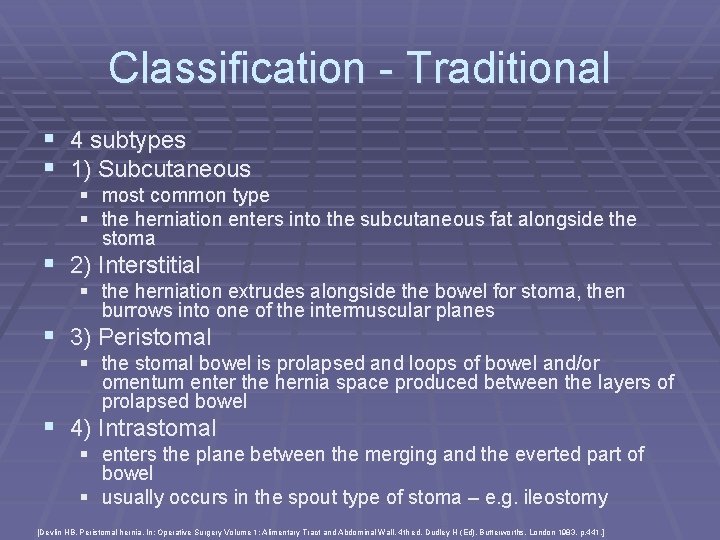
Classification - Traditional § 4 subtypes § 1) Subcutaneous § most common type § the herniation enters into the subcutaneous fat alongside the stoma § 2) Interstitial § the herniation extrudes alongside the bowel for stoma, then burrows into one of the intermuscular planes § 3) Peristomal § the stomal bowel is prolapsed and loops of bowel and/or omentum enter the hernia space produced between the layers of prolapsed bowel § 4) Intrastomal § enters the plane between the merging and the everted part of bowel § usually occurs in the spout type of stoma – e. g. ileostomy [Devlin HB. Peristomal hernia. In: Operative Surgery Volume 1: Alimentary Tract and Abdominal Wall, 4 th ed, Dudley H (Ed), Butterworths, London 1983. p. 441. ]
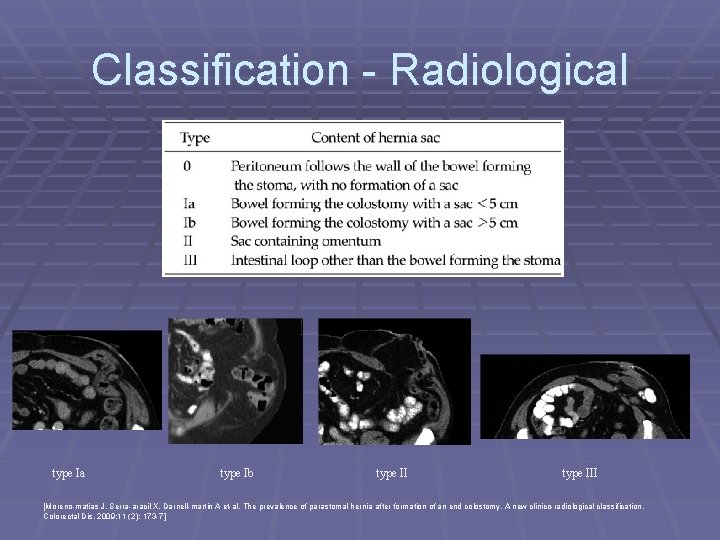
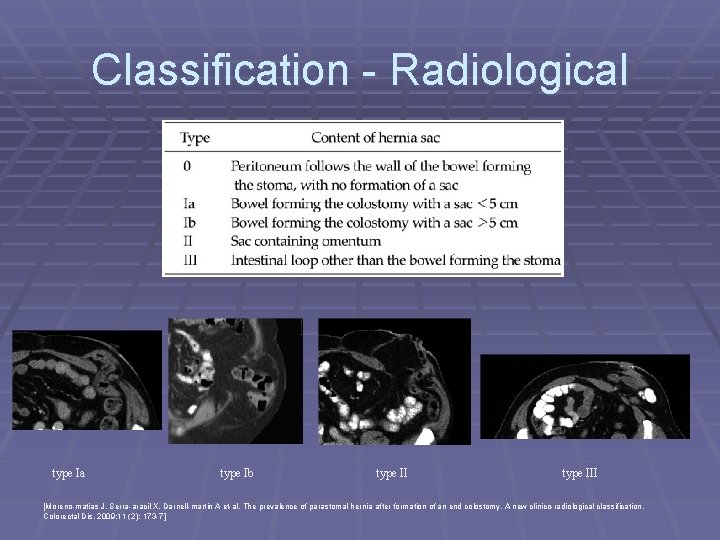
Classification - Radiological type Ia type Ib type III [Moreno-matias J, Serra-aracil X, Darnell-martin A et-al. The prevalence of parastomal hernia after formation of an end colostomy. A new clinico-radiological classification. Colorectal Dis. 2009; 11 (2): 173 -7]
Risk factors § Patient-related § Surgery-related
Patient-related risk factors § Age § Obesity (>30 kg/m 2) and waist circumference § § § (>100 cm) Poor nutritional status Increased intraabdominal pressure (COAD, constipation, BPH, ascites, etc) Connective tissue disorders Immunosuppressive drugs (e. g. corticosteroids) Other disease predispose to wound infection (e. g. DM) Other underlying diseases (e. g. IBD, malignancy)
Surgery-related risk factors § Emergency construction of stoma § Stoma lateral to rectus muscle § Diameter of trephine § defect >3 cm was found to be associated with a higher incidence of herniation, independent of stoma type § currently few data to base advice about the appropriate size of abd wall opening § suggestions of not more than 2. 5 cm had been made § smallest opening that allows the creation of a viable stoma without ischaemia appears to be the best guide § Closure of lateral space § Stoma fixation to fascia § Intraperitoneal or extraperitoneal approach
Clinical presentation § Vary from asymptomatic to life-threatening § § strangulation Typically – bulge at the site of or adjacent to the stoma, with or without pain Mild abd discomfort, intermittent colic, distention, nausea & vomiting, diarrhoea, constipation and a reducible hernia Physical examination – on lying down and standing with valsalva Digital examination enables the fascial aperture and parastomal tissues to be assessed
Complications requiring surgery § § Literature reported a range of 11%-70% Local data: ~32% require surgical intervention Urgent surgery for strangulation of an irreducible hernia Following signs & symptoms can be repaired electively § § § increasing size intermitted bowel obstructions chronic abdominal pain related to PSH ill-fitting appliance and leakage peristomal skin breakdown other stoma complications
Management § Conservative § Surgery § § Closure of stoma Direct fascial repair Relocation Mesh repair § Different location § Lap vs open § Laparoscopic techniques § Prevention
Direct fascial repair § Reduce size of hernia defect by reapproximating the fascial edges of trephine with sutures § Advantage § § simple technique avoids laparotomy low complication rate in elective operation may have a role when there is a strong desire to avoid mesh or more major surgery § Disadvantage § excessive tension and subsequent failure in large fascial defect § high recurrence rate – reported in various literature to be 46100%
Relocation § This approach avoided because the new stoma at new site is associated with the same high risk of hernia formation § Some authors reported a lower recurrence rate after relocation to other side of abdominal wall than relocation on the same side of abdomen § Advantage § § § useful if the current stoma position unsatisfactory can be done with or without laparotomy lower recurrence rate than direct fascial repair § § local recurrence rate reported in literature ~36. 3% (range up to 76. 2%) not feasible if patient has multiple previous scars risk of incisional hernia at the site of the original stoma or midline wound more risk of morbidity if require laparotomy § Disadvantage [Carne PW, Robertson GM, Frizelle FA. Parastomal hernia. Br J Surg 2003; 90: 784 -93]
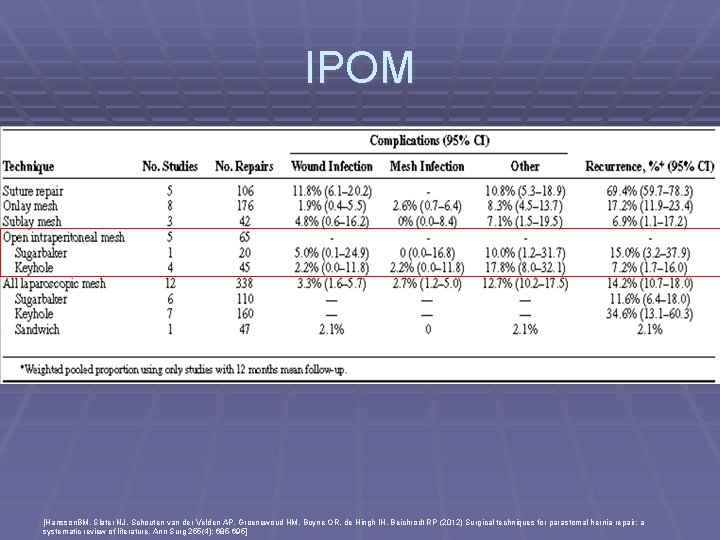
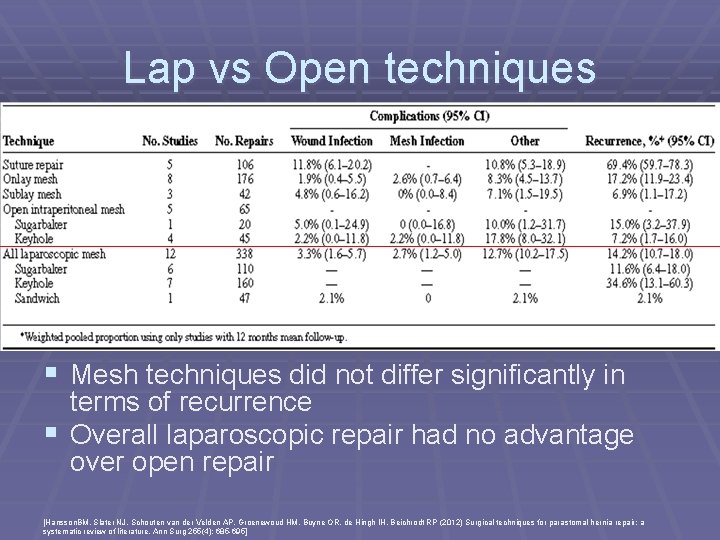
Mesh repair § Overall recurrence rates after mesh repair vary between 6. 9 -17. 8% (depending on technique and placement of mesh) § Overall mesh infection rate 2. 4% § Risk of mesh infection did not differ between mesh techniques [Hansson. BM, Slater NJ, Schouten van der Velden AP, Groenewoud HM, Buyne OR, de Hingh IH, Beichrodt RP (2012) Surgical techniques for parastomal hernia repair: a systematic review of literature. Ann Surg 255(4): 685 -695]
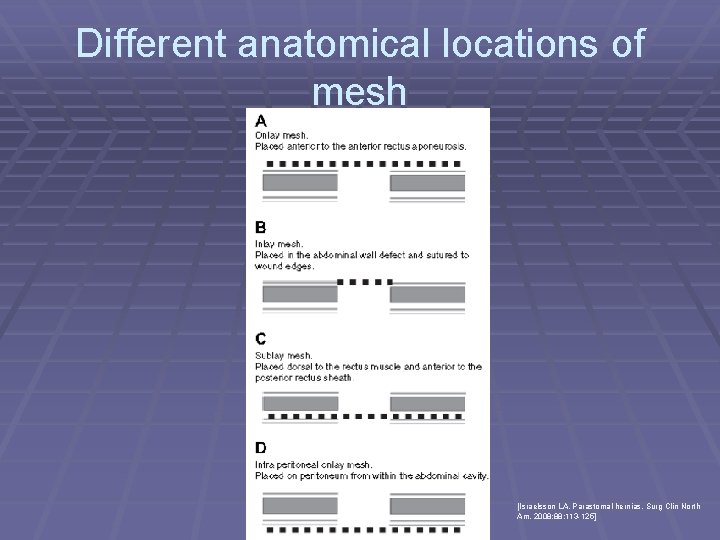
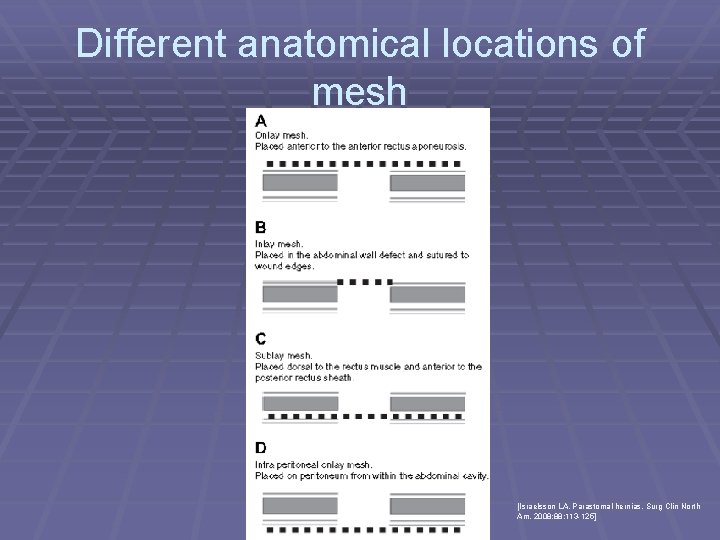
Different anatomical locations of mesh [Israelsson LA. Parastomal hernias. Surg Clin North Am. 2008; 88: 113 -125]
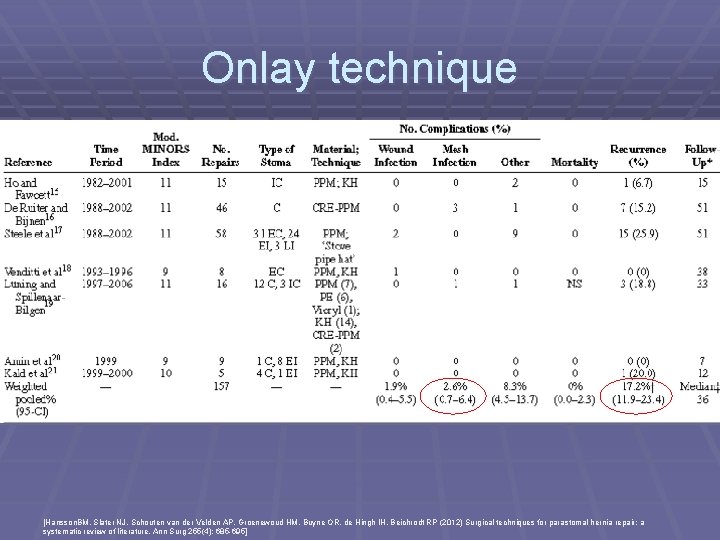
Onlay technique § First described by Rosin and Bonardi in 1977 § Mesh placed subcutaneously and fixed onto the anterior rectus § § § aponeurosis Prefascial plane was entered through a lateral parastomal incision After reduction of hernia sac, the fascial opening was narrowed with sutures and mesh was placed to reinforce the suture repair Advantage: § more straight forward surgical technique involving a mesh § avoids intra-abdominal dissection § Disadvantage § associated with higher risk of contamination & sepsis than sublay technique § extensive dissection of subcutaneous tissue § predisposes to haematoma / seroma formation § undermining is a risk for ischaemic injury to skin => impair wound healing § intraabdominal pressure may lead to detachment of mesh resulting in recurrence
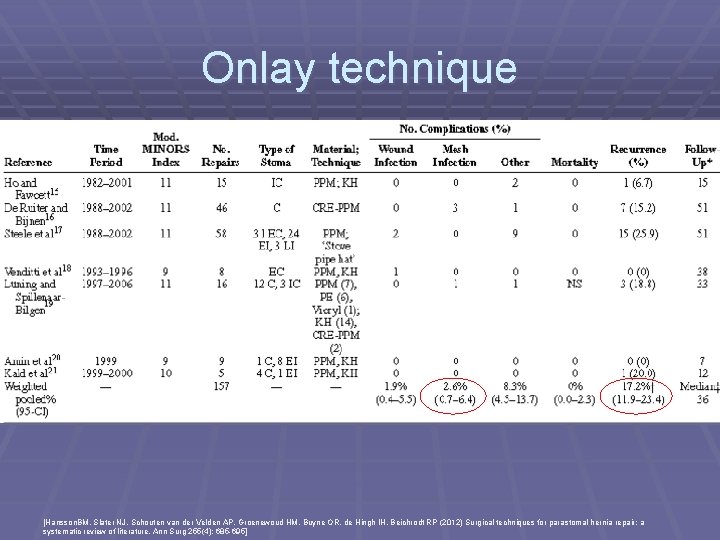
Onlay technique [Hansson. BM, Slater NJ, Schouten van der Velden AP, Groenewoud HM, Buyne OR, de Hingh IH, Beichrodt RP (2012) Surgical techniques for parastomal hernia repair: a systematic review of literature. Ann Surg 255(4): 685 -695]
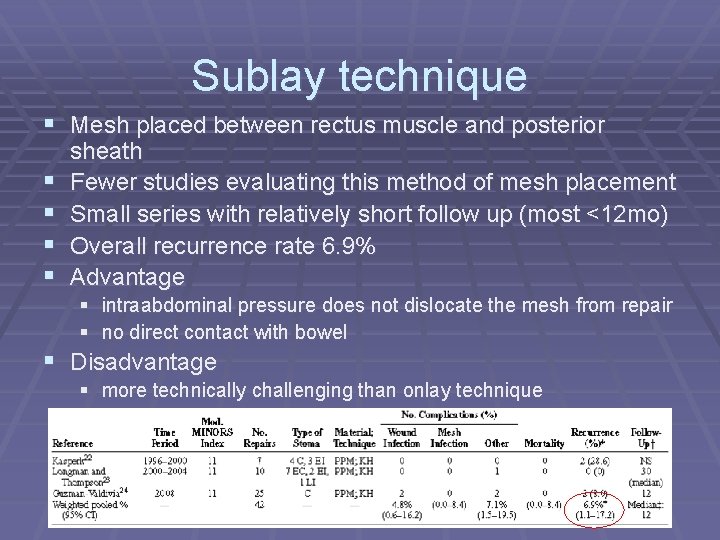
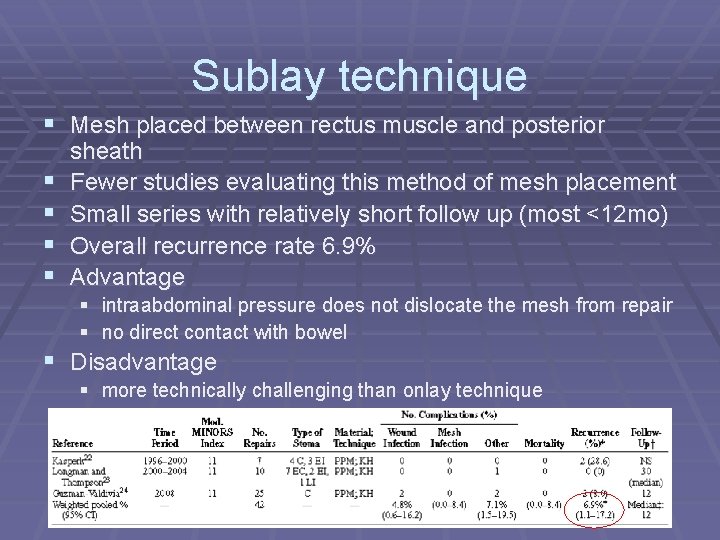
Sublay technique § Mesh placed between rectus muscle and posterior § § sheath Fewer studies evaluating this method of mesh placement Small series with relatively short follow up (most <12 mo) Overall recurrence rate 6. 9% Advantage § intraabdominal pressure does not dislocate the mesh from repair § no direct contact with bowel § Disadvantage § more technically challenging than onlay technique
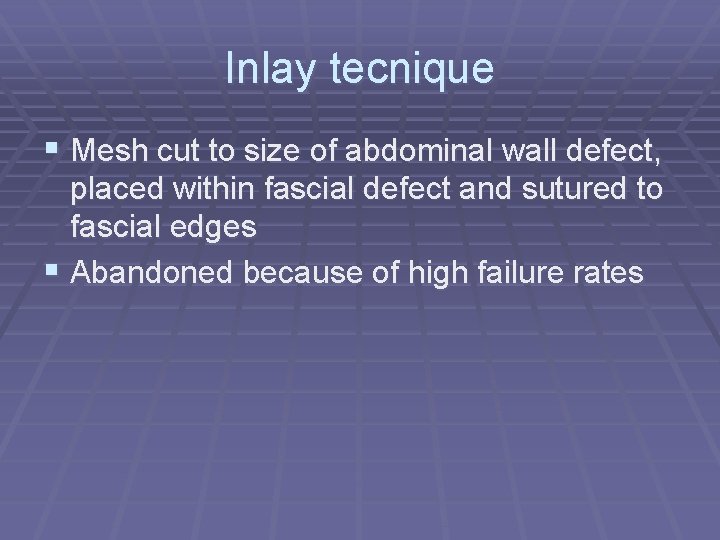
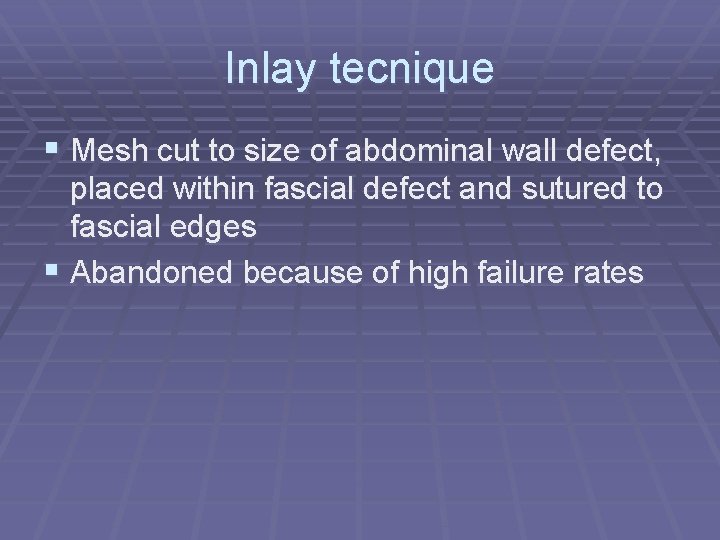
Inlay tecnique § Mesh cut to size of abdominal wall defect, placed within fascial defect and sutured to fascial edges § Abandoned because of high failure rates
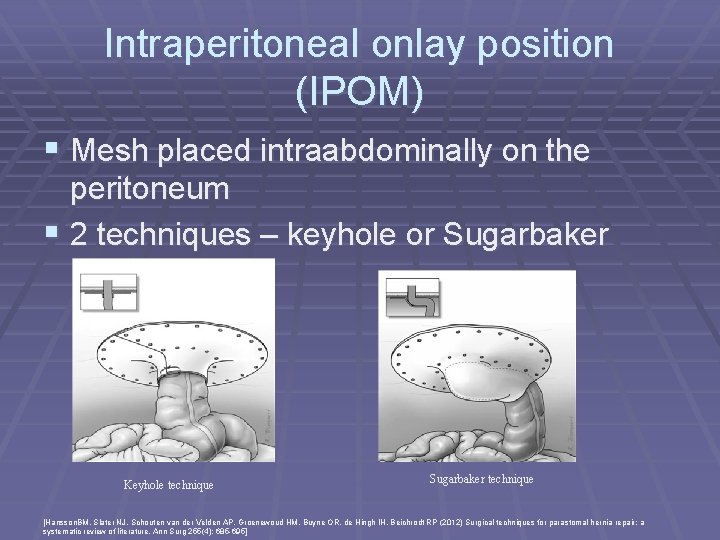
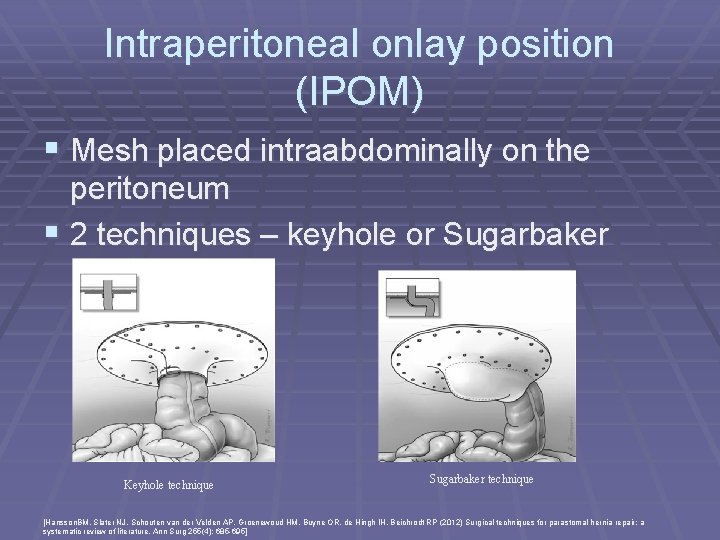
Intraperitoneal onlay position (IPOM) § Mesh placed intraabdominally on the peritoneum § 2 techniques – keyhole or Sugarbaker Keyhole technique Sugarbaker technique [Hansson. BM, Slater NJ, Schouten van der Velden AP, Groenewoud HM, Buyne OR, de Hingh IH, Beichrodt RP (2012) Surgical techniques for parastomal hernia repair: a systematic review of literature. Ann Surg 255(4): 685 -695]
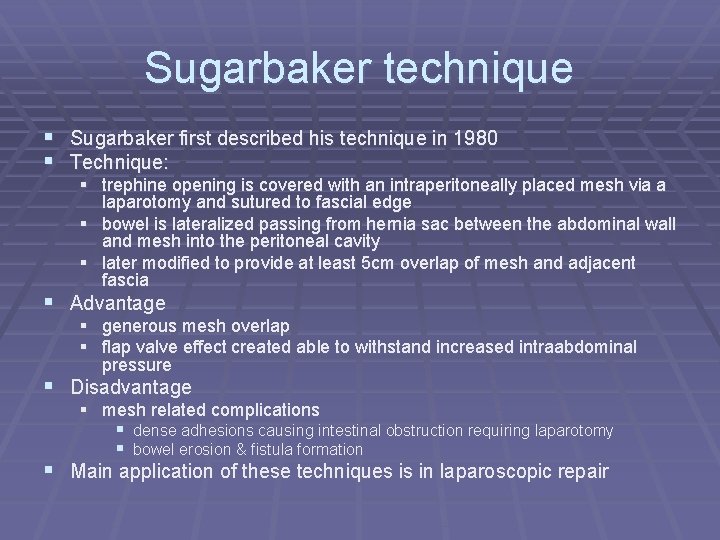
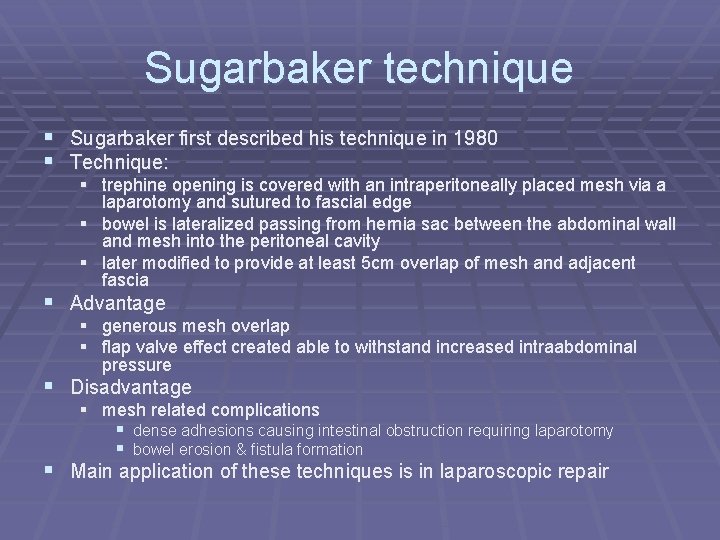
Sugarbaker technique § Sugarbaker first described his technique in 1980 § Technique: § trephine opening is covered with an intraperitoneally placed mesh via a laparotomy and sutured to fascial edge § bowel is lateralized passing from hernia sac between the abdominal wall and mesh into the peritoneal cavity § later modified to provide at least 5 cm overlap of mesh and adjacent fascia § Advantage § generous mesh overlap § flap valve effect created able to withstand increased intraabdominal pressure § Disadvantage § mesh related complications § dense adhesions causing intestinal obstruction requiring laparotomy § bowel erosion & fistula formation § Main application of these techniques is in laparoscopic repair
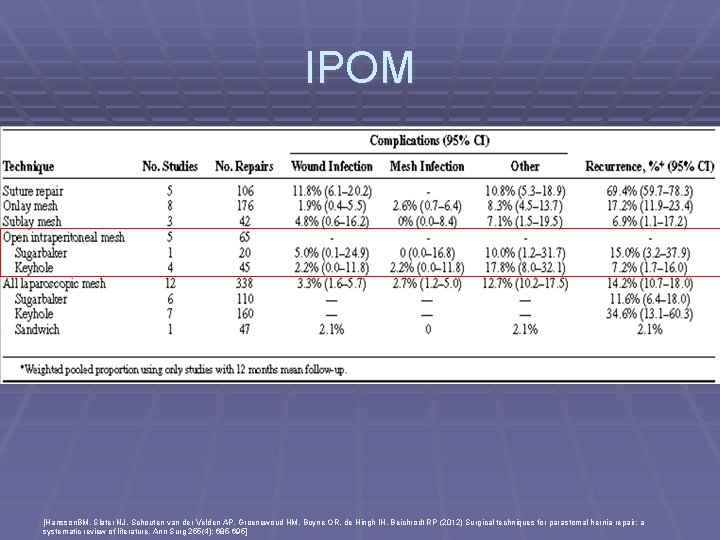
IPOM [Hansson. BM, Slater NJ, Schouten van der Velden AP, Groenewoud HM, Buyne OR, de Hingh IH, Beichrodt RP (2012) Surgical techniques for parastomal hernia repair: a systematic review of literature. Ann Surg 255(4): 685 -695]

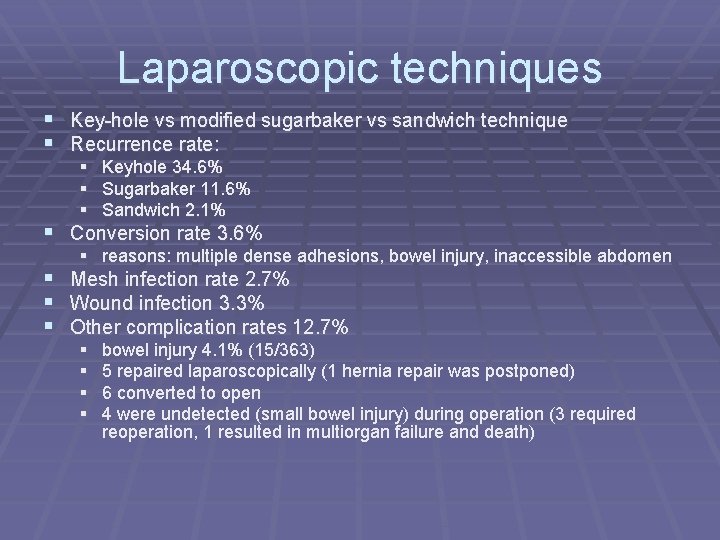
Laparscopic techniques § Key-hole vs modified sugarbaker vs sandwich technique § Potential advantages § minimal additional injury to abdominal wall which is already at risk of herniation § better view of defect allowing more precise repair and reinforcement with a mesh § concomitant incisional hernia repair § faster postop recovery and decreased postop pain § Sandwich technique [Berger D, Bientzle M. Polyvinylidene fluoride: a suitable mesh material for laparoscopic incisional and parastomal hernia repair. A prospective, observational study with 344 patients. Hernia. 2009; 13: 167 -172. ]
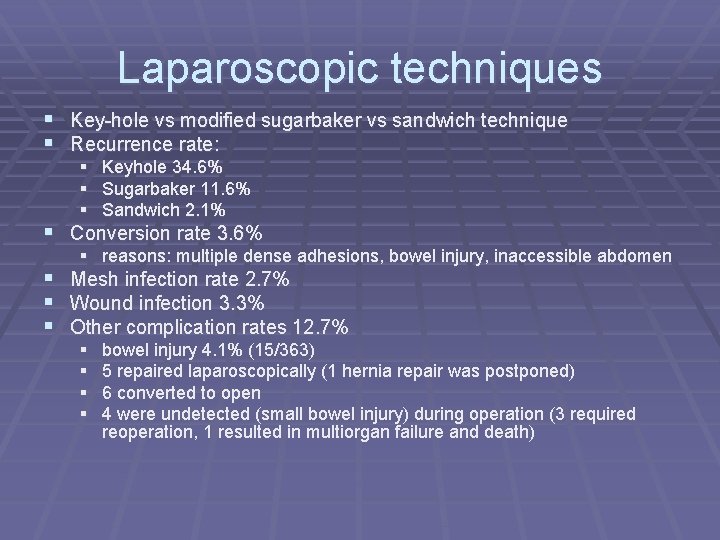
Laparoscopic techniques § Key-hole vs modified sugarbaker vs sandwich technique § Recurrence rate: § Keyhole 34. 6% § Sugarbaker 11. 6% § Sandwich 2. 1% § Conversion rate 3. 6% § reasons: multiple dense adhesions, bowel injury, inaccessible abdomen § Mesh infection rate 2. 7% § Wound infection 3. 3% § Other complication rates 12. 7% § § bowel injury 4. 1% (15/363) 5 repaired laparoscopically (1 hernia repair was postponed) 6 converted to open 4 were undetected (small bowel injury) during operation (3 required reoperation, 1 resulted in multiorgan failure and death)
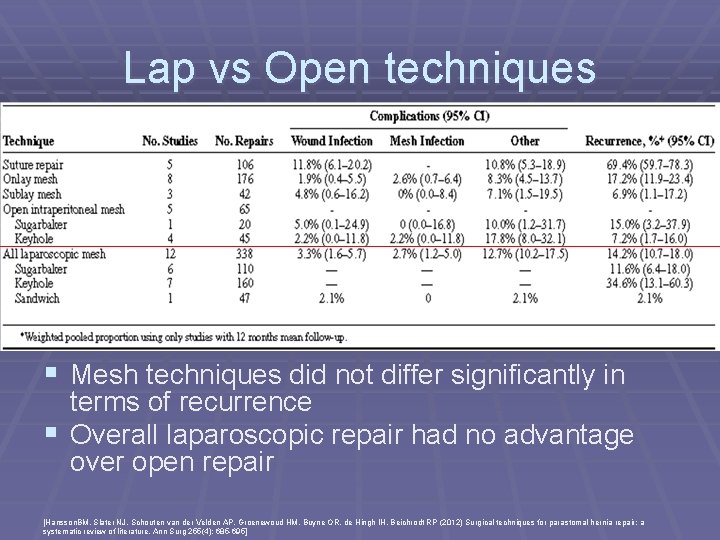
Lap vs Open techniques § Mesh techniques did not differ significantly in terms of recurrence § Overall laparoscopic repair had no advantage over open repair [Hansson. BM, Slater NJ, Schouten van der Velden AP, Groenewoud HM, Buyne OR, de Hingh IH, Beichrodt RP (2012) Surgical techniques for parastomal hernia repair: a systematic review of literature. Ann Surg 255(4): 685 -695]
Prevention § High incidence of parastomal hernia together with unsatisfactory results of its repair and morbidity associated with operation lead to emphasis on prevention § Prevention strategies § surgical techniques § prophylactic mesh insertion
Surgical techniques in prevention § Through or lateral rectus abdominis § only retrospective studies found lower rate of PSH with stomas formed through the rectus muscle § nonetheless probably wise to bring out stoma throught rectus abdominis ms as this is not associated with any disadvantage § § Fascial fixation Closure of lateral space Trephine size Extraperitoneal route for stoma construction
Extraperitoneal route for permanent colostomy § Few studies had shown that extraperitoneal approach can achieve lower risk of herniation than transperitoneal route § Potential disadvantage § longer operative time § may need mobilization of splenic flexure for extra length § Goligher first published the formation of extraperitoneal colostomy in 1958 § extraperitoneal route provides an oblique passage of bowel and eliminate the lateral peritoneal space without using suture § attempt to reduce risk of postop small bowel obstruction due to internal herniation into lateral peritoneal space and reduce parastomal hernia § Since then, subsequent studies have been published with inconsistent results § Only 2 retrospective studies found extraperitoneal colostomy construction was associated with a lower rate of parastomal herniation than intraperitoneal route § most studies were observational retrospective studies with small numbers of patients undergoing extraperitoneal colostomy and follow up period was not mentioned § Studies of highter quality, including RCTS with larger no. of patients are needed
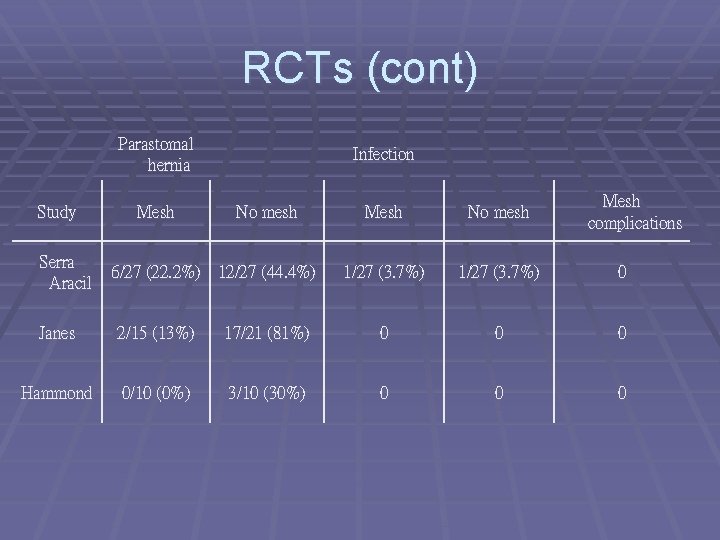
Prophylactic mesh insertion § Bayer and colleagues first described mesh insertion at § § § the time of primary stoma formation in 1986 Since then many observational studies confirmed the safety and effectiveness of prophylactic mesh insertion with low morbidity Three RCTs (2008 -2009) have shown that prophylactic mesh in sublay position is associated with reduction in parastomal hernia when compared with standard stoma formation Systematic review including the three RCTs found a statistically significant difference in the incidence of PSH in the mesh gp 12. 5% and in the no-mesh gp 53%, but no difference in morbidity [Shabbir J, Chaudhary BN, Dawson R. A systematic review on the use of prophylactic mesh during primary stoma formation to prevent parastomal hernia formation. Colorectal Dis 2012; 14(8): 931 -6. ]
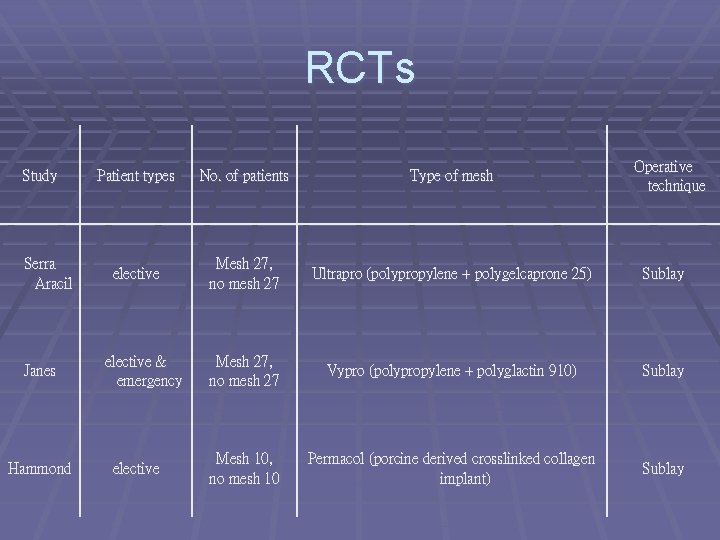
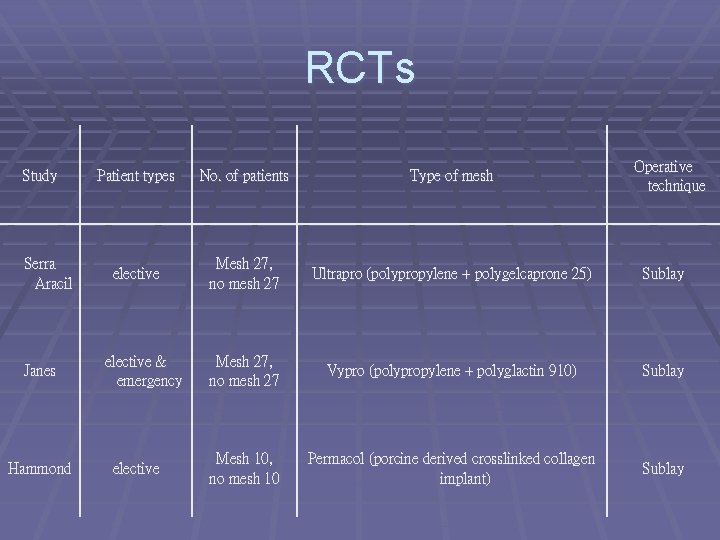
RCTs Study Serra Aracil Janes Hammond Operative technique Patient types No. of patients Type of mesh elective Mesh 27, no mesh 27 Ultrapro (polypropylene + polygelcaprone 25) Sublay Mesh 27, no mesh 27 Vypro (polypropylene + polyglactin 910) Sublay Mesh 10, no mesh 10 Permacol (porcine derived crosslinked collagen implant) Sublay elective & emergency elective
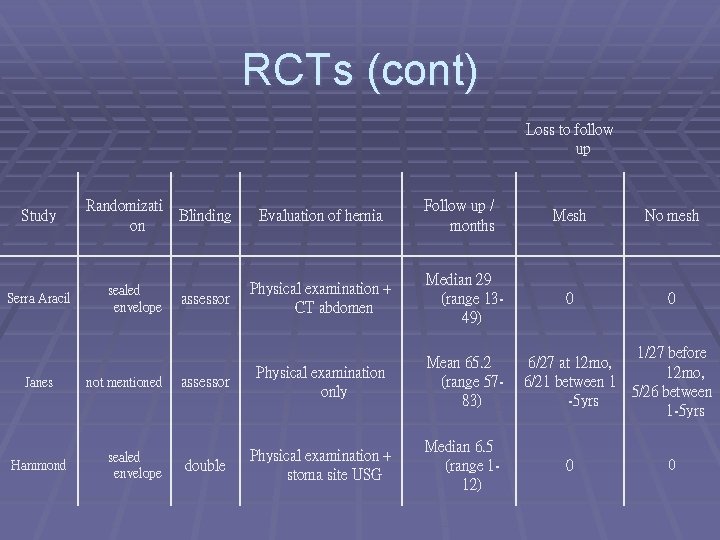
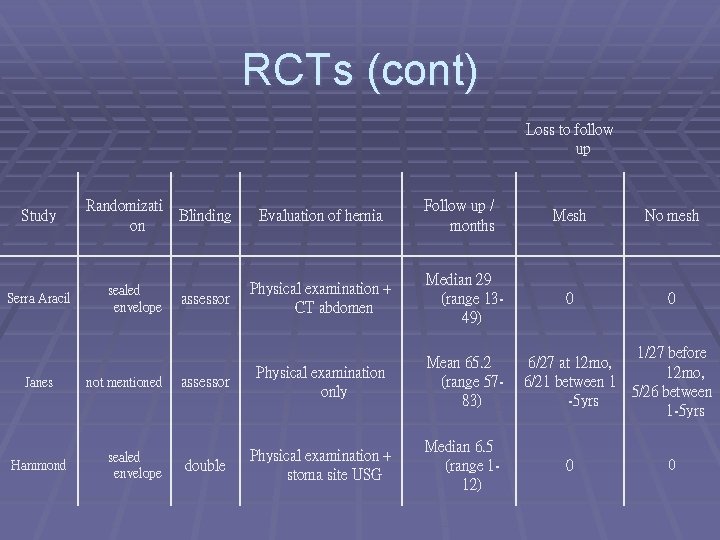
RCTs (cont) Loss to follow up Study Serra Aracil Janes Hammond Randomizati on sealed envelope not mentioned sealed envelope Follow up / months Blinding Evaluation of hernia assessor Physical examination + CT abdomen Median 29 (range 1349) assessor Physical examination only Mean 65. 2 (range 5783) double Physical examination + stoma site USG Median 6. 5 (range 112) Mesh No mesh 0 0 1/27 before 6/27 at 12 mo, 6/21 between 1 5/26 between -5 yrs 1 -5 yrs 0 0
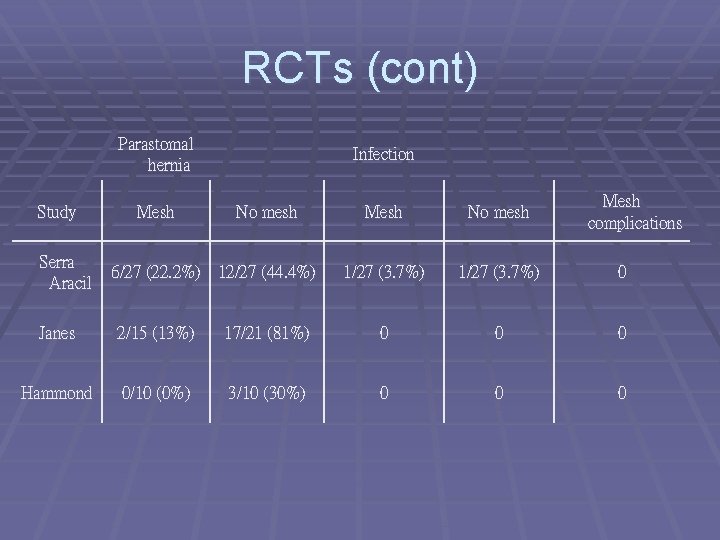
RCTs (cont) Parastomal hernia Study Serra Aracil Mesh Infection No mesh 6/27 (22. 2%) 12/27 (44. 4%) Mesh complications Mesh No mesh 1/27 (3. 7%) 0 Janes 2/15 (13%) 17/21 (81%) 0 0 0 Hammond 0/10 (0%) 3/10 (30%) 0 0 0
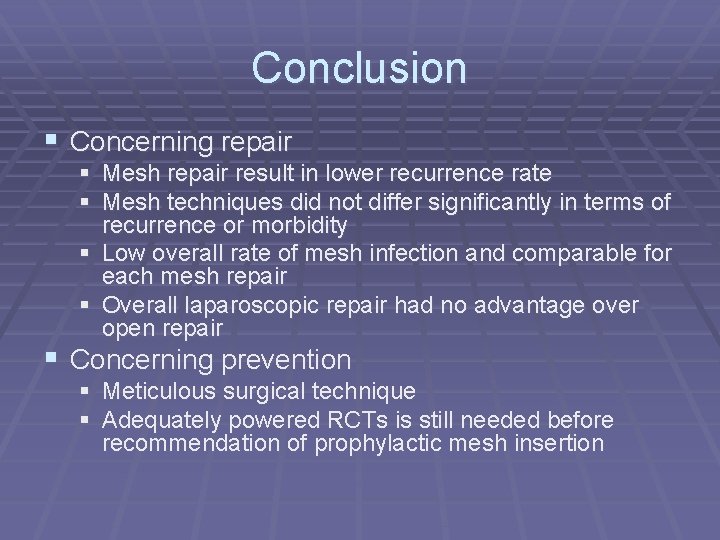
Conclusion § Concerning repair § Mesh repair result in lower recurrence rate § Mesh techniques did not differ significantly in terms of recurrence or morbidity § Low overall rate of mesh infection and comparable for each mesh repair § Overall laparoscopic repair had no advantage over open repair § Concerning prevention § Meticulous surgical technique § Adequately powered RCTs is still needed before recommendation of prophylactic mesh insertion

Discussion