PARAMOUNT ADVANTAGE MEDICAID New Electronic Claims System Webinar

PARAMOUNT ADVANTAGE MEDICAID New Electronic Claims System Webinar
Agenda • Paramount Overview • New Electronic Claims System • • • Member ID card Claims editing Explanation of Payment (EOP) Provider portal claim status Provider registration with Ohio Department of Medicaid (ODM) • Additional information
WHO WE ARE • Paramount Insurance Company became a wholly owned and operated affiliate of Pro. Medica in 1992 • Offers six product lines for individuals and employers across six Midwest states • 601, 000+ unique members


MEDICAID Ranked #1 in the following Pay 25+ years of Medicaid coverage for Performance metrics 54 county service area 215, 000+ covered lives* • Follow-up after 18+ years of NCQA accreditation hospitalization for mental Rated top Medicaid health illness insurance plan in Ohio for 2019 • Postpartum care and 2020 by NCQA • Controlling high blood • Achieving 4. 0 out of 5 pressure overall rating Non-profit Ranked #2 overall for Pay for Performance metrics • Achieving 61. 8% amongst Ohio MCPs *215, 000 covered lives as of 12/31/19
New Electronic Claims System • Presenters • Lisa Ash, Provider Relations Representative • Tanya Curtland, Director, Provider Services • Freda Hogan, Vice President, Provider Operations • How to ask questions during the presentation • Chat feature
New Electronic Claims System Health. Rules Payor by Health. Edge is a next-generation core administrative processing system. • System Go Live: June 1, 2021 • Medicaid product line only. All other product lines will go live in 2022. • For questions: • Contact your Provider Relations representative or email providerrelations. paramount@promedica. org. • Visit Paramount’s website for more information: • www. paramounthealthcare. com/services/providers/provider-news
New Electronic Claims System What makes Health. Rules Payor different from the electronic claims system Paramount uses today? • Automatic Claims Processing: Improvement of 15% in auto adjudication of claims. • Versioning: Records are never archived or deleted, when changes occur a new version of the record is created. • Automatic Re-Processing: When a new version is created, which would alter the results of adjudication, the system automatically re-processes any claim impacted.
Member ID Information • Health. Rules Payor member ID will be all numerical and 11 digits. Example 10000000121. • A 0000 -01 legacy (current) member ID number will remain active for 2 -year run out period. • Legacy member “A 00” ID number may be used to submit claims or real-time eligibility (RTE) requests after June 1, 2021. When doing so, the Health. Rules Payor member ID will be included on the explanation of payment (EOP) and RTE response. • Legacy member “A 00” ID must be used for services prior to June 1, 2021. This includes any resubmission (for services prior to June 1, 2021) that may be required after June 1, 2021. The current electronic claim system will reject any claims submitted with the Health. Rules Payor member ID. • Health. Rules Payor member ID cards for existing membership will be mailed to members over a 4 -6 week period beginning early June. New members effective June 1, 2021, or after will receive their card immediately.
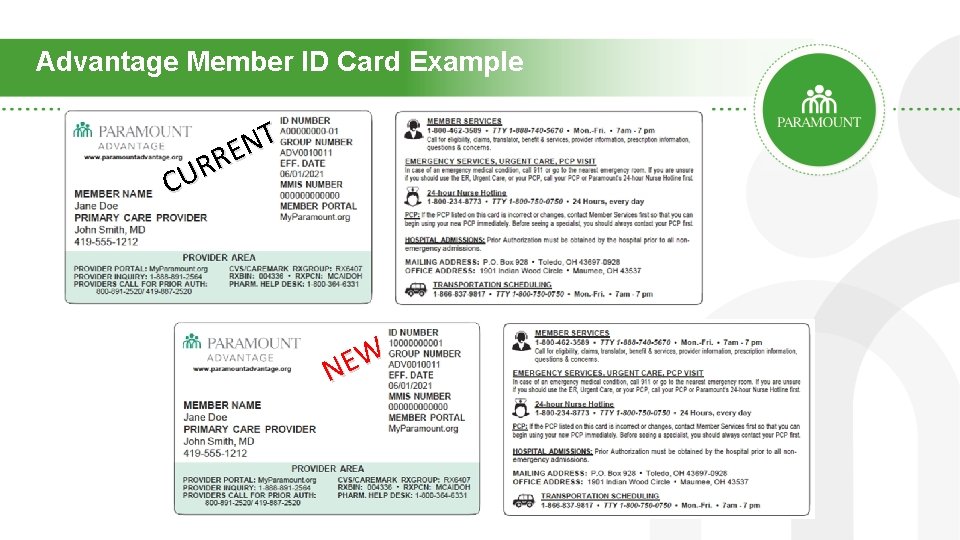
Advantage Member ID Card Example T N E R R U C W E N
Claims Editing Process • Enhancing existing, internally developed claims editing processes, which we use to administer reimbursement policy and claim edit rules, by passing claims through Optum Claims Edit System® (CES). CES uses the following sources for edits: • National Correct Coding Initiative (NCCI) edits, including Medically Unlikely Edits (MUEs) • Federal Register (The Daily Journal of the U. S Government that contains agency rules, proposed rules and public notices) • Medicare publications • Local and National Coverage Determinations (LCDs/NCDs) • Outpatient Code Editor (OCE) • Medicare Code Editor (MCE) • Center for Medicare and Medicaid (CMS) • Ohio Department of Medicaid (ODM)
Claims Editing Process • CES will replace Change Healthcare Claim Check to automatically review and catch errors, omissions and questionable coding. • The end result: Streamlined claims, reduced reimbursement errors and improved payment integrity. • All edits are transparent, and you will be able to look up specific claims and see both edits and sourced citations.
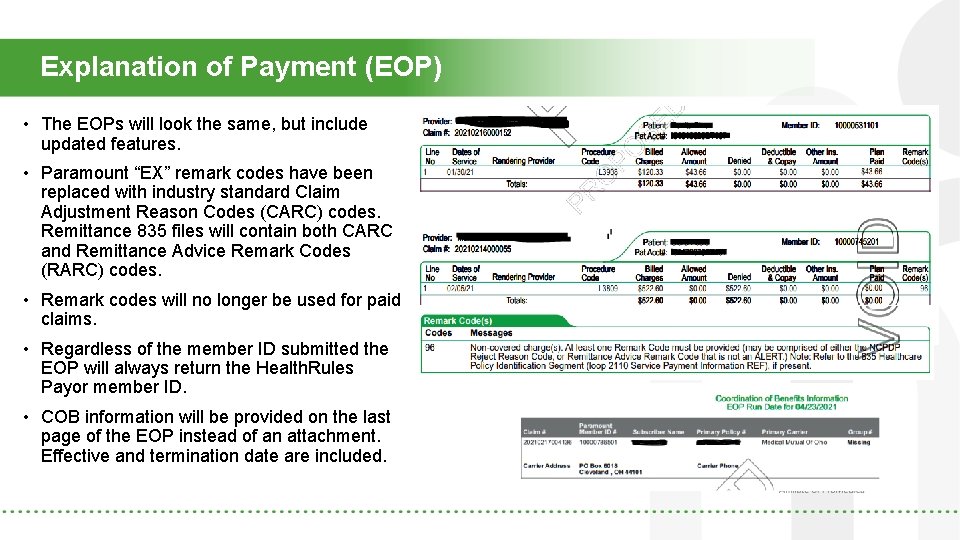
Explanation of Payment (EOP) • The EOPs will look the same, but include updated features. • Paramount “EX” remark codes have been replaced with industry standard Claim Adjustment Reason Codes (CARC) codes. Remittance 835 files will contain both CARC and Remittance Advice Remark Codes (RARC) codes. • Remark codes will no longer be used for paid claims. • Regardless of the member ID submitted the EOP will always return the Health. Rules Payor member ID. • COB information will be provided on the last page of the EOP instead of an attachment. Effective and termination date are included.
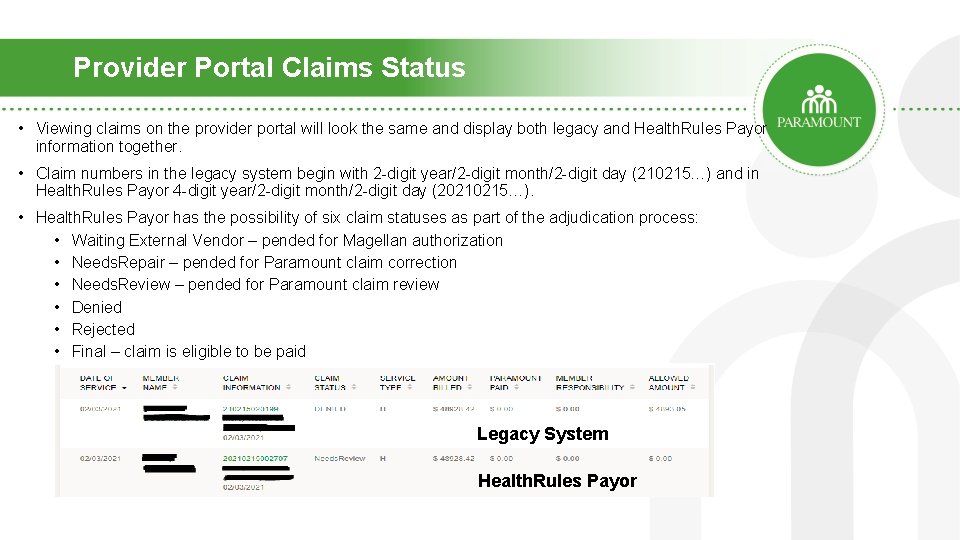
Provider Portal Claims Status • Viewing claims on the provider portal will look the same and display both legacy and Health. Rules Payor information together. • Claim numbers in the legacy system begin with 2 -digit year/2 -digit month/2 -digit day (210215…) and in Health. Rules Payor 4 -digit year/2 -digit month/2 -digit day (20210215…). • Health. Rules Payor has the possibility of six claim statuses as part of the adjudication process: • Waiting External Vendor – pended for Magellan authorization • Needs. Repair – pended for Paramount claim correction • Needs. Review – pended for Paramount claim review • Denied • Rejected • Final – claim is eligible to be paid Legacy System Health. Rules Payor
Additional Information • Claims will continue loading overnight in batch format. • Payables will continue to be generated on Monday, Wednesday and Friday. • No changes required with clearinghouse. • ODM Enrollment Status – claims will deny if the provider (based on billing NPI) is not registered with ODM. Below is the CARC denial message that will be returned on the EOP. • B 7 – This provider was not certified/eligible to be paid for this procedure/service on this date of service. Usage: Refer to the 835 Healthcare Policy identification Segment (loop 2110 Service Payment Information REF), if present. • Claims submitted from an Optometrist (routine and medical) will deny in Health. Rules Payor to submit the claim to Eye. Quest. • The billing information for Eye. Quest will be provided: Eye. Quest, PO Box 527, Thiensville, WI 53092.
Additional Information • As a reminder, Paramount will follow reimbursement policy RM-012 Anesthesia Rounding. • Paramount will now be following CMS guidelines for time unit rounding. Time spent performing anesthesia services is reported in one-minute increments and noted in the unit’s field. Do not estimate the time or round up or down inappropriately. To calculate reimbursement for time, the number of minutes reported is divided by 15 (minutes) and rounded up to the next tenth to provide a unit of measure. Example: 61 minutes divided by 15 = 4. 0666 units. Reimbursement for time will be rounded to 4. 1 units instead of using a whole 5 unit of measure. • Credentialing – Health. Rules Payor matches claims to providers utilizing the provider’s National Provider Identifier (NPI). If you have not sent us this information in the past, please send an updated roster noting the billing NPI(s) for each practitioner.
Resources • Today’s webinar is being recorded • Q&A will be sent to all participants and posted on our website For questions: • Call Provider Inquiry at 888 -891 -2564. • Contact your Provider Relations representative or email providerrelations. paramount@promedica. org. • Visit Paramount’s website for more information: • www. paramounthealthcare. com/services/providers/provider-news
Thank you! On behalf of the entire Paramount team, thank you for joining today. We look forward to the launch of our new electronic claims processing system!
- Slides: 18