Paramount Advantage CentralSoutheast Region Transition Plan Welcome Randy






- Slides: 30

Paramount Advantage Central/Southeast Region Transition Plan
Welcome Randy Runyon, CEO, OACHC
Agenda Tim Petee, Director, Regional Operations

Thank you

Meet our Panel • Webinar Moderator: Tim Petee, Director, Regional Operations • David Bishop, Manager, Provider Relations • Cresta Montgomery, RN, Manager, Behavioral Health Care Management • Dale Ocheske, Administrative Director, Medicaid Operations • Anita Patel, Regional Director, Case Management • Brandon Urso, Operations Manager, Utilization Management
Agenda 1. 2. 3. 4. 5. Scaling back service area Transitioning members to new plans Plan for transitioning high-priority members Special concerns for providers Accepting new members in west and northeast regions 6. Panel Q&A
Scaling Back Service Area Dale Ocheske, Administrative Director, Medicaid Operations

Scaling Back Service Area Paramount made the difficult decision to withdraw from the central/southeast region.
Scaling Back Service Area What does this mean for our central/southeast members? • All will be enrolled in a new plan by June 1, 2020. • No one will go without coverage. • No one eligible for Medicaid will lose benefits.
Transitioning Members to New Plans Dale Ocheske, Administrative Director, Medicaid Operations
Transitioning Members to New Plans • From now until April 30, 2020, members can select their new plans. • To select a plan, members can: – Call the Medicaid Hotline at 800 -324 -8680. – Visit www. ohiomh. com. • New plans will be effective the first day of the following month.
Transitioning Members to New Plans • For those who do not select a new plan before April 30, 2020, ODM will assign one for them. • Once assigned, ODM will send members written communication notifying them of their new plan. • New plans will be effective June 1, 2020.
Transitioning Members to New Plans Until the effective date of the new plan, members can continue to: • Use their Paramount health insurance. • See their current health care providers.
Transitioning Members to New Plans How to help patients • Reassure them that they are not losing their benefits. • Help them understand the timeline. • When picking a new plan, remind patients to: – Compare benefits and special programs. – Make sure their providers are in network. – Contact the Medicaid Hotline to learn about each plan.
Transitioning Members to New Plans Contact information: Medicaid Hotline • Call 800 -324 -8680 – Monday through Friday, 7 a. m. to 8 p. m. – Saturdays, 8 a. m. to 5 p. m. • Visit www. ohiomh. com

Transitioning Members to New Plans Contact information: Paramount Member Services Department • Call toll free at 1 -800 -462 -3589. Choose option No. 2. • TTY users call toll free 1 -888 -740 -5670. • Use live chat at www. paramounthealthcare. com Monday through Friday, 9 a. m. – 4 p. m. • Log on to the member portal at www. myparamount. org 24 hours a day, seven days a week. • The team is available Monday – Friday, 7 a. m. – 7 p. m.
Plan for Transitioning High-Priority Members Anita Patel, Regional Director, Case Management
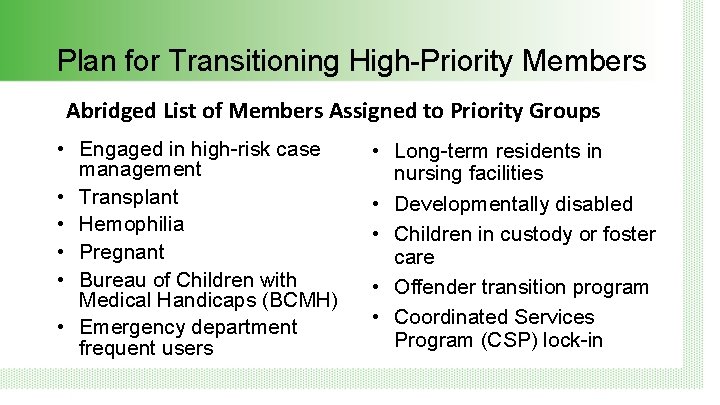
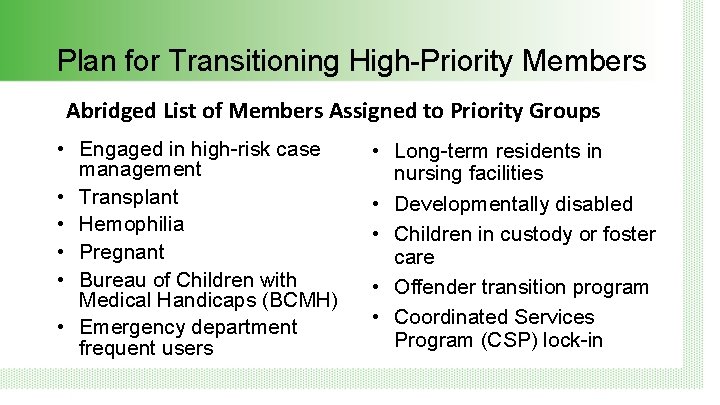
Plan for Transitioning High-Priority Members Abridged List of Members Assigned to Priority Groups • Engaged in high-risk case management • Transplant • Hemophilia • Pregnant • Bureau of Children with Medical Handicaps (BCMH) • Emergency department frequent users • Long-term residents in nursing facilities • Developmentally disabled • Children in custody or foster care • Offender transition program • Coordinated Services Program (CSP) lock-in
Plan for Transitioning High-Priority Members Outreach to Members • Case managers (CM) are making every effort to reach out to members who are identified as being part of a high -priority population. – – Inform members of Paramount’s exit from the central/southeast region. Offer to facilitate a three-way call with member, Medicaid Hotline and Paramount CM to assist member with choosing a new plan.
Plan for Transitioning High-Priority Members Outreach to New Health Plans • To ensure members using case management services experience a smooth transition to their new plan, each month, Paramount: – – Identifies the members who have selected a new plan and who also use case management services. Conducts meetings with each plan to review key clinical information and case management needs of identified members.
Special Concerns for Providers David Bishop, Manager, Provider Relations Brandon Urso, Manager, Utilization Management
Special Concerns for Providers • Still part of Paramount network. Paramount is not terming any provider contracts. • Paramount Medicaid providers continue to be eligible to see Paramount members no matter where their practice is located.
Special Concerns for Providers Pre-certifications All services that have been authorized by Paramount will be honored by the member’s new managed care plan through the approved time period.
Special Concerns for Providers Comprehensive primary care (CPC) practices • One of the other four Medicaid plans will take over Paramount’s role as lead managed care plan for CPC practices in the central/southeast region. • No new practices were assigned to Paramount in 2020.
Accepting New Members in West and Northeast Regions Dale Ocheske, Administrative Director, Medicaid Operations
Accepting New Members in West and Northeast Regions • Newly Medicaid-eligible Ohioans are now being assigned to Paramount. • Newly assigned Medicaid members have 90 days to change plans, if they choose, by: – Calling Medicaid Hotline at 800 -324 -8680. – Visiting www. ohiomh. com.

Questions and Answers Tim Petee, Moderator Paramount Panel
Wrap Up Tim Petee, Moderator
Wrap Up • OACHC will post this recording to their website for your reference • Watch your email for this Power. Point, written answers to the questions asked today, and other materials.
Thank you for your participation