Paramedic Inter Facility Transfer Training Section 1 PIFT



- Slides: 49

Paramedic Inter Facility Transfer Training Section 1 PIFT Overview

Paramedic Inter Facility Transfer
Interfacility Transfer – Interfacility transfer means the transfer of a patient from one health care facility (hospital, rehab, nursing home, etc. ) to another.
Interfacility Transfer – Interfacility transfers are done every day within the normal scope of practice as defined by Maine EMS rules
Interfacility Transfer – Examples: • EMT-B transfers a patient with a saline lock • EMT-P transfers a patient on a Fentanyl drip
Interfacility Transfer If the normal scope of practice is not exceeded, then no further assistance or special circumstance is needed As long as the patient is otherwise stable
Interfacility Transfer – Occasionally, the needs of the patient exceed the capabilities and scope of practice of the EMS provider - Examples: • A stable patient on an Amiodarone drip • A 26 week pregnant female in active labor
Interfacility Transfer Under normal circumstances these patients would require hospital staff to accompany the crew in transport
Interfacility Transfer The RN would be part of the team, but hold ultimate responsibility for administering and monitoring the “non. EMS” medications, devices and treatments.
PIFT Program • Developed in 1990’s to address concerns of hospitals • Hospitals concerned with having to send staff on inter facility transfers • They believed stable patients who had medications running that were outside the normal standard of care could be transported by paramedics alone
PIFT Program • MDPB determined that there are many situations where properly trained paramedics can safely transport patients who are receiving medications that are outside the identified paramedic standard of care.
PIFT Training • Expanded the paramedic standard of care in the interfacility setting only. • Allowed paramedics in specific circumstances to control and administer a new list of medications and monitor and troubleshoot a variety of patient care devices.
PIFT Training • The trouble is the list kept expanding…
PIFT Training • In 2006 the MDPB updated the program to make it more universal. – Medication classifications instead of a list • The sticking point has always been patient stability.
Current PIFT Parameters • Paramedics who have completed the inter facility transport program may (in a PIFT Setting): – Transport medications established by the normal standard of care – And transport the following additional classifications of medications:
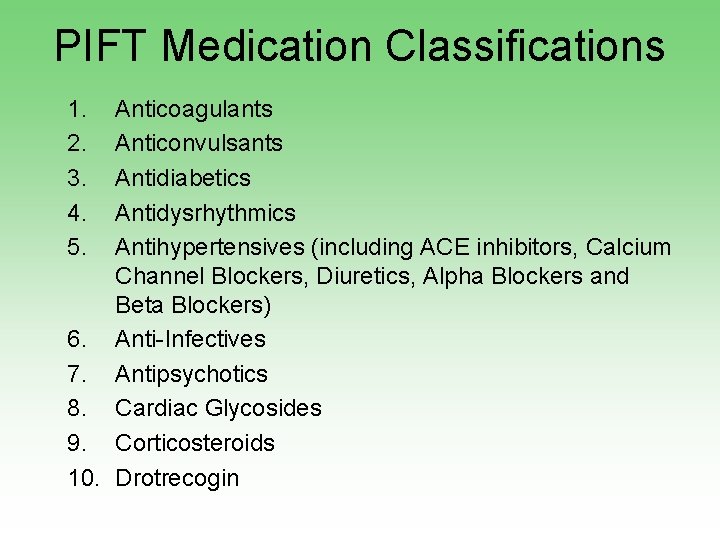
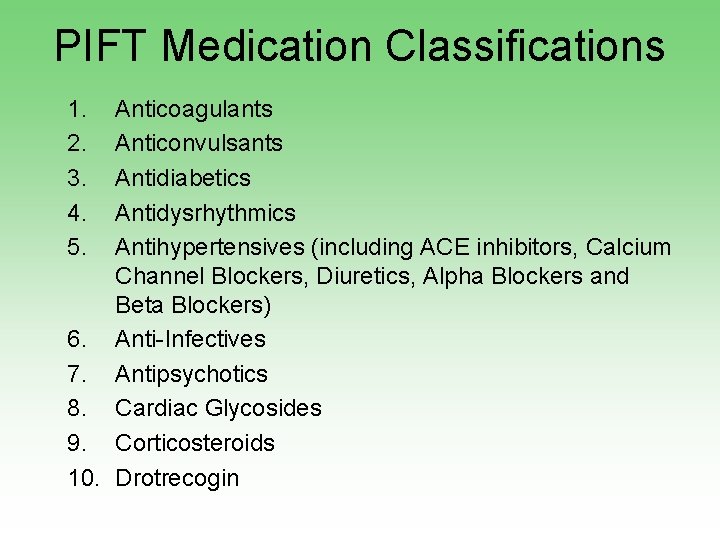
PIFT Medication Classifications 1. 2. 3. 4. 5. Anticoagulants Anticonvulsants Antidiabetics Antidysrhythmics Antihypertensives (including ACE inhibitors, Calcium Channel Blockers, Diuretics, Alpha Blockers and Beta Blockers) 6. Anti-Infectives 7. Antipsychotics 8. Cardiac Glycosides 9. Corticosteroids 10. Drotrecogin
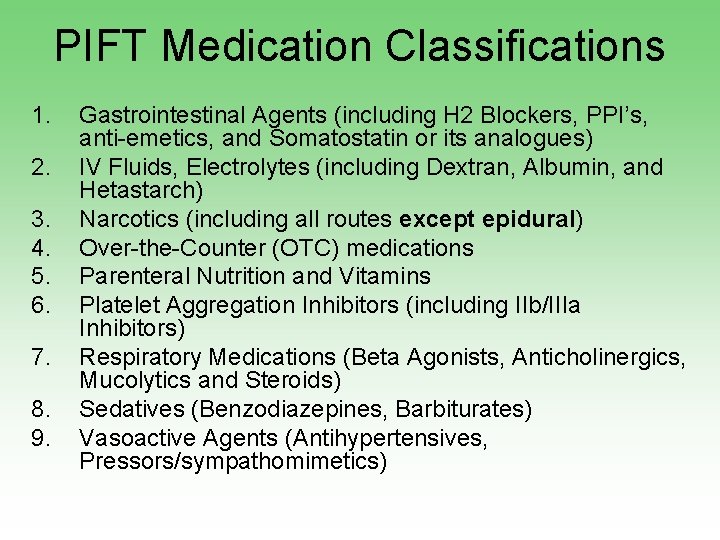
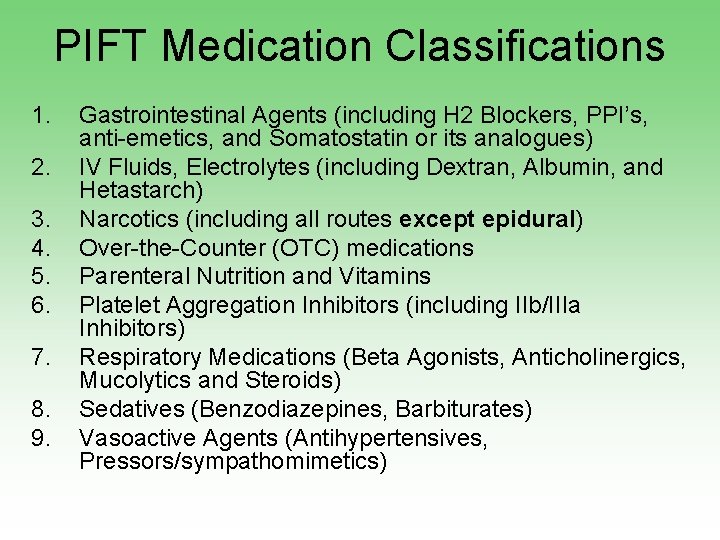
PIFT Medication Classifications 1. 2. 3. 4. 5. 6. 7. 8. 9. Gastrointestinal Agents (including H 2 Blockers, PPI’s, anti-emetics, and Somatostatin or its analogues) IV Fluids, Electrolytes (including Dextran, Albumin, and Hetastarch) Narcotics (including all routes except epidural) Over-the-Counter (OTC) medications Parenteral Nutrition and Vitamins Platelet Aggregation Inhibitors (including IIb/IIIa Inhibitors) Respiratory Medications (Beta Agonists, Anticholinergics, Mucolytics and Steroids) Sedatives (Benzodiazepines, Barbiturates) Vasoactive Agents (Antihypertensives, Pressors/sympathomimetics)
PIFT Medication Classifications o Paramedics may actually be administering some of these medications as required by the patient condition and allowed by physician order and training. o Paramedics may transport patients with central lines as long as the medications running are contained on this list.
The MDPB defined very specific limitations for PIFT transfers
PIFT Limitations • PIFT Transfers are limited to PIFT trained paramedics – In order to be eligible to participate in a PIFT transfer, the provider must be a paramedic who has attended a new, updated PIFT training.
PIFT Limitations • Expanded protocols are limited to the “interfacility transfer setting” – Interfacility transfer setting means the transfer of a patient from one health care facility (hospital) to another. – PIFT trained paramedics are not allowed to use expanded protocols in any setting other than a PIFT transfer.
PIFT Limitations • Services must also be permitted through MEMS as a “PIFT Service” • More on this later…
Stability
Stability • To be eligible for a PIFT transfer, a patient must be “stable. ”
Stability • “A patient is considered “stable” when there is no foreseeable likelihood of material deterioration in the condition of the patient as a result of or during the transport. ” Maine EMS Medical Directions and Practice Board 2006
Stability Assessment of stability will require: • Hemodynamic and neurologic signs which have demonstrated no deterioration from the acute presentation of the patient, or are within acceptable limits of variation on existing therapy and…. Maine EMS Medical Directions and Practice Board 2006
Stability …may be reasonably predicted to remain so during the transport without the need for further adjustments to such therapy… Maine EMS Medical Directions and Practice Board 2006
Stability The pathophysiology of the patient’s acute condition is known to favorably respond to therapeutic interventions which have been undertaken at the sending hospital Maine EMS Medical Directions and Practice Board 2006
Stability • Patient reports and detailed physician orders are critical components of a stability decision
Stability • The PIFT paramedic must have: – A detailed understanding of the patient history as it relates to this current treatment plan – Additional relevant patient history – Physician instructions for managing patient change during transport.
The final decision on whether the patient can be transported under the PIFT program will be made by the transporting paramedic
There are many inter facility transfers that will not be eligible for PIFT and therefore must utilize hospital staff
Non-PIFT Situations • • • Patients who are not stable according to the definition listed previously. Patients who are on medications or equipment that is not included in the PIFT program. Situations where the paramedic is not comfortable transporting without additional hospital personnel
Bottom Line A safe and effective inter facility transport requires the use of adequately trained personnel utilizing appropriate equipment for the management of the patient
PIFT Transfers
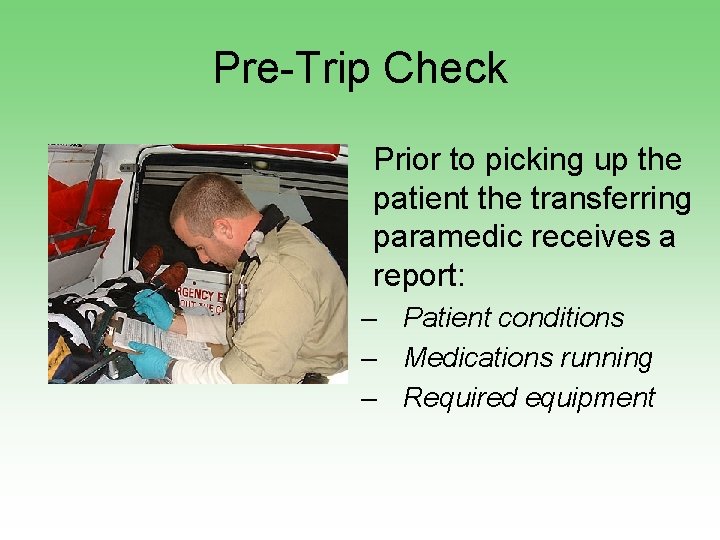
Pre-Trip Check • Prior to picking up the patient the transferring paramedic receives a report: – Patient conditions – Medications running – Required equipment
Pre-Trip Check § Paramedic conducts a pre-trip inventory ü Appropriate equipment ü Gas levels ü Resources
Pre-Trip Check • Paramedic reviews operation of any required equipment to ensure proper familiarity with operation.
Pre-Trip Check • Paramedic reviews unfamiliar medications – – – Mechanism of action Indications Contraindications Precautions Side Effects/Untoward effects – Potential complications

Patient Deterioration
Patient Deterioration • Patient must be regularly re-assessed in order to identify changes in patient condition as soon as possible.
Patient Deterioration • Paramedics must be acutely aware of specific physician orders and the medications that are being administered
Patient Deterioration • What are the orders? • What medications need to be given to prevent deterioration? • Are there medications to be given in the event of deterioration?
Patient Deterioration • If changes in the patient are dramatic, the paramedic should attempt to contact medical control – 1 st choice = Sending physician/facility – 2 nd choice = Receiving physician/facility – 3 rd choice = Diversion/3 rd party physician
Patient Deterioration • In extreme circumstances, the paramedic may consider discontinuing the medication and utilize existing MEMS protocols to manage the patient.
Patient Deterioration • The transporting crew should also consider diverting to the closest hospital with an emergency department for assistance.
Report to Receiving Facility • The Paramedic is a key part of the patient care team and must take responsibility for continuing the communication link that passes critical patient information between caregivers.
Report to Receiving Facility • Information that should be passed along to the receiving facility include: – – History received from the sending facility Assessment findings during transport Patient general condition Treatments administered and/or altered during transport – Patient response to treatments or changes.
Summary • PIFT enables paramedics to broaden their scope of practice during interfacilty transfers • Not all interfacility transfers will qualify for PIFT • PIFT has rigid parameters including a stability assessment • Appropriate transport decisions must be made • Good judgment is an ongoing requirement