Papillary Muscle Approximation versus Undersizing Restrictive Annuloplasty Alone


- Slides: 20

Papillary Muscle Approximation versus Undersizing Restrictive Annuloplasty Alone for Severe Ischemic Mitral Regurgitation: a Randomized Clinical Trial Francesco Nappi, Cristiano Spadaccio, Antonio Nenna, Mario Lusini, Christophe Acar, Massimo Chello Antonio Nenna, MD Department of Cardiovascular Surgery Università Campus Bio-Medico di Roma, Rome, Italy a. nenna@unicampus. it francesconappi 2@gmail. com American College of Cardiology 2016, 65 th Annual Scientific Session ACC. 16, April. CAMPUS 2 -4 2016, Chicago, UNIVERSITA' BIO-MEDICO DI ROMAUSA Via Álvaro del Portillo, 21 - 00128 Roma - Italia www. unicampus. it
ISCHEMIC MITRAL REGURGITATION Ischemic mitral regurgitation (IMR) is a consequence of myocardial ischemia which results in geometrical disturbance of mitral valve due to papillary muscle injury and displacement, favoring impaired leaflet coaptation. The incidence of IMR among patients with myocardial infarction is up to 39% (1, 6 – 2, 8 million patients in the US) Functional regurgitation imbalance closing forces VS tethering forces Circulation 1997; 96: 827 -33. Circulation 2001; 103: 1759 -64. Am J Cardiol 2002; 89: 315 -8
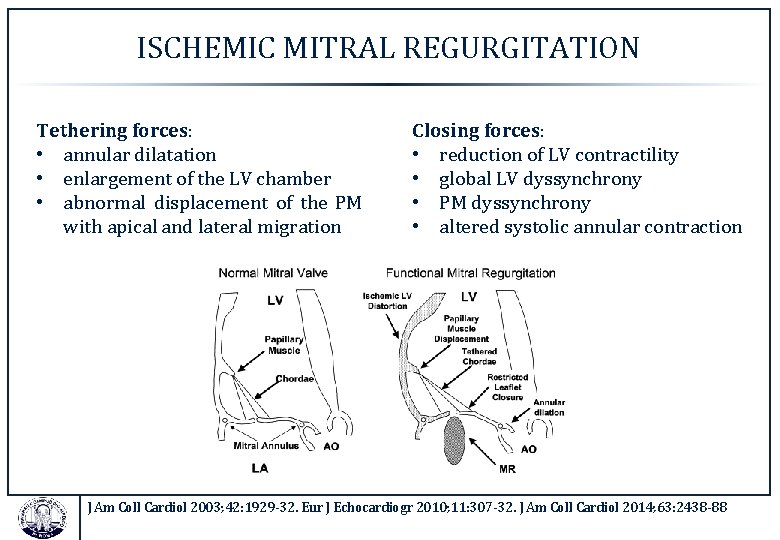
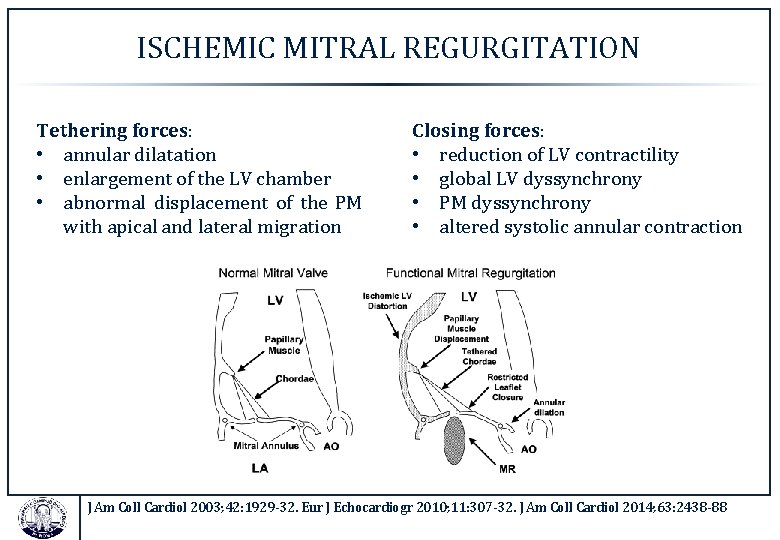
ISCHEMIC MITRAL REGURGITATION Tethering forces: • annular dilatation • enlargement of the LV chamber • abnormal displacement of the PM with apical and lateral migration Closing forces: • reduction of LV contractility • global LV dyssynchrony • PM dyssynchrony • altered systolic annular contraction J Am Coll Cardiol 2003; 42: 1929 -32. Eur J Echocardiogr 2010; 11: 307 -32. J Am Coll Cardiol 2014; 63: 2438 -88
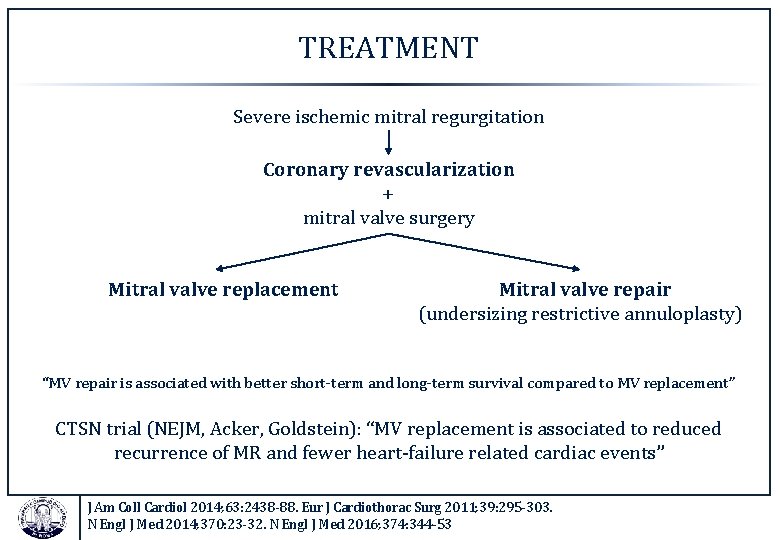
TREATMENT Severe ischemic mitral regurgitation Coronary revascularization + mitral valve surgery Mitral valve replacement Mitral valve repair (undersizing restrictive annuloplasty) “MV repair is associated with better short-term and long-term survival compared to MV replacement” CTSN trial (NEJM, Acker, Goldstein): “MV replacement is associated to reduced recurrence of MR and fewer heart-failure related cardiac events” J Am Coll Cardiol 2014; 63: 2438 -88. Eur J Cardiothorac Surg 2011; 39: 295 -303. N Engl J Med 2014; 370: 23 -32. N Engl J Med 2016; 374: 344 -53
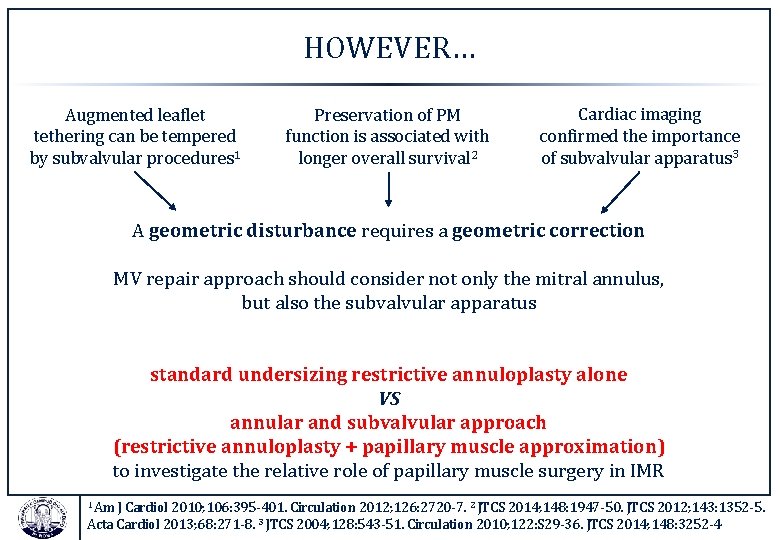
HOWEVER… Augmented leaflet tethering can be tempered by subvalvular procedures 1 Preservation of PM function is associated with longer overall survival 2 Cardiac imaging confirmed the importance of subvalvular apparatus 3 A geometric disturbance requires a geometric correction MV repair approach should consider not only the mitral annulus, but also the subvalvular apparatus standard undersizing restrictive annuloplasty alone VS annular and subvalvular approach (restrictive annuloplasty + papillary muscle approximation) to investigate the relative role of papillary muscle surgery in IMR 1 Am J Cardiol 2010; 106: 395 -401. Circulation 2012; 126: 2720 -7. 2 JTCS 2014; 148: 1947 -50. JTCS 2012; 143: 1352 -5. Acta Cardiol 2013; 68: 271 -8. 3 JTCS 2004; 128: 543 -51. Circulation 2010; 122: S 29 -36. JTCS 2014; 148: 3252 -4
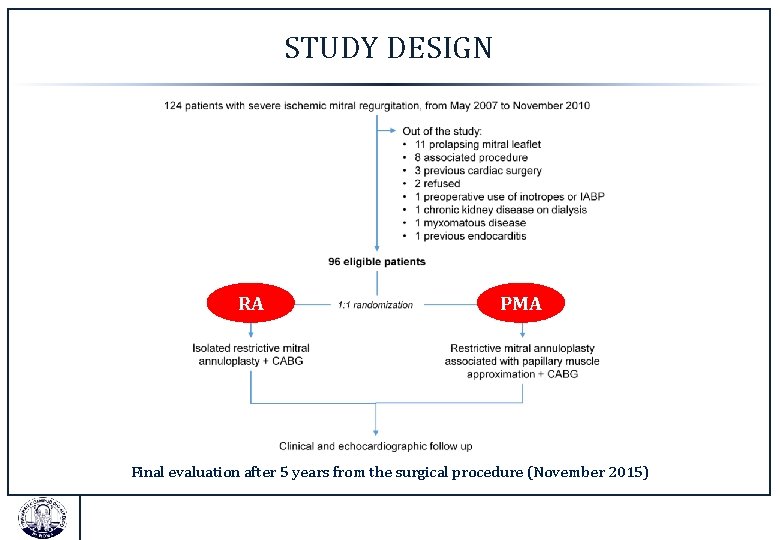
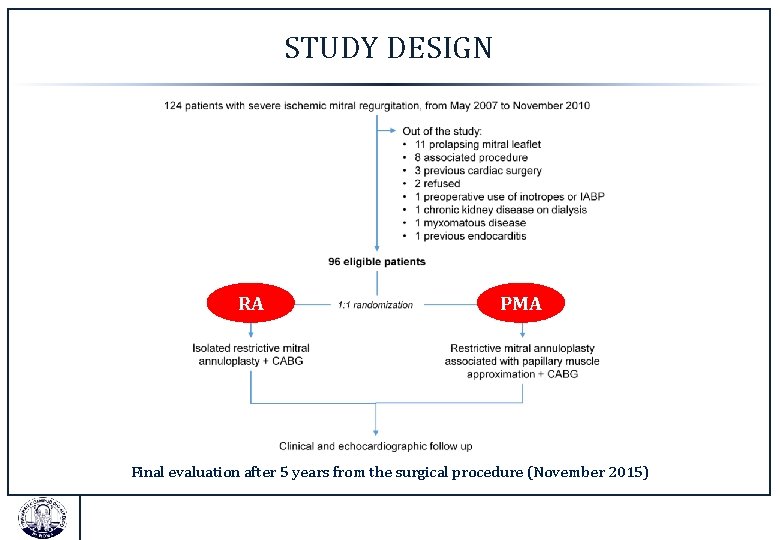
STUDY DESIGN RA PMA Final evaluation after 5 years from the surgical procedure (November 2015)
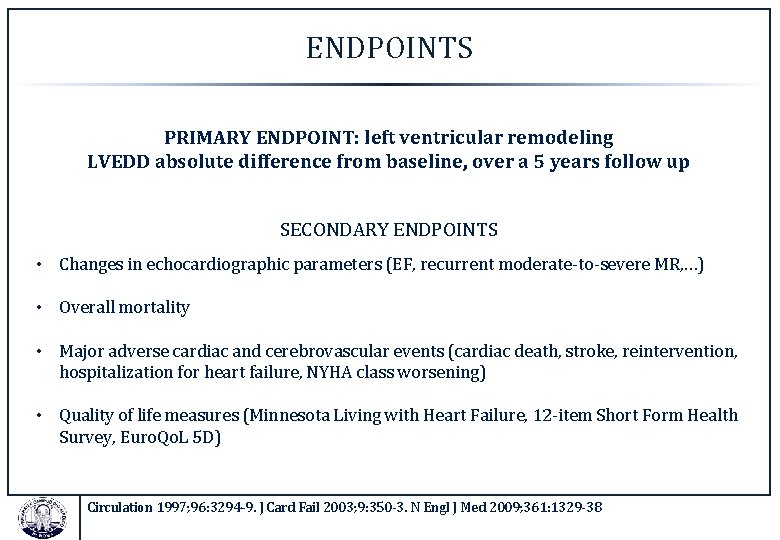
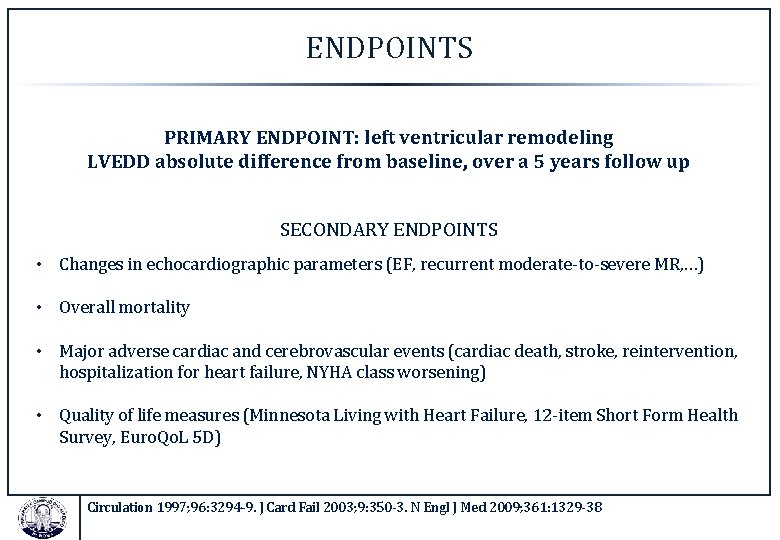
ENDPOINTS PRIMARY ENDPOINT: left ventricular remodeling LVEDD absolute difference from baseline, over a 5 years follow up SECONDARY ENDPOINTS • Changes in echocardiographic parameters (EF, recurrent moderate-to-severe MR, …) • Overall mortality • Major adverse cardiac and cerebrovascular events (cardiac death, stroke, reintervention, hospitalization for heart failure, NYHA class worsening) • Quality of life measures (Minnesota Living with Heart Failure, 12 -item Short Form Health Survey, Euro. Qo. L 5 D) Circulation 1997; 96: 3294 -9. J Card Fail 2003; 9: 350 -3. N Engl J Med 2009; 361: 1329 -38
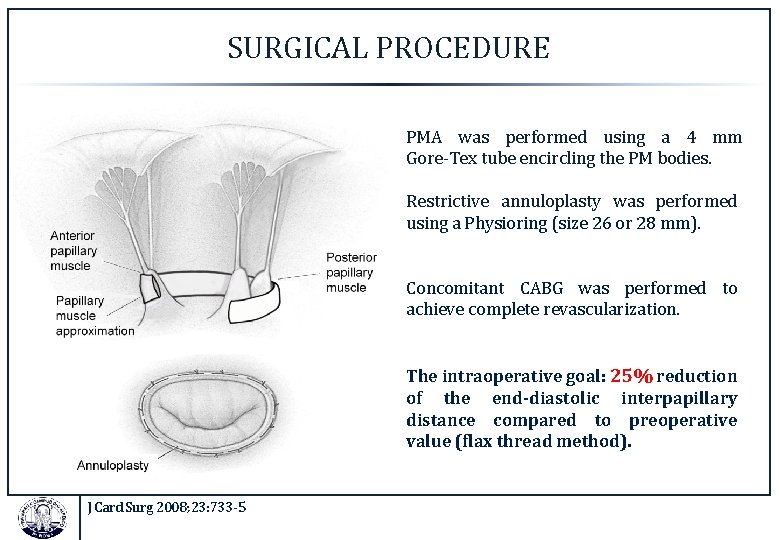
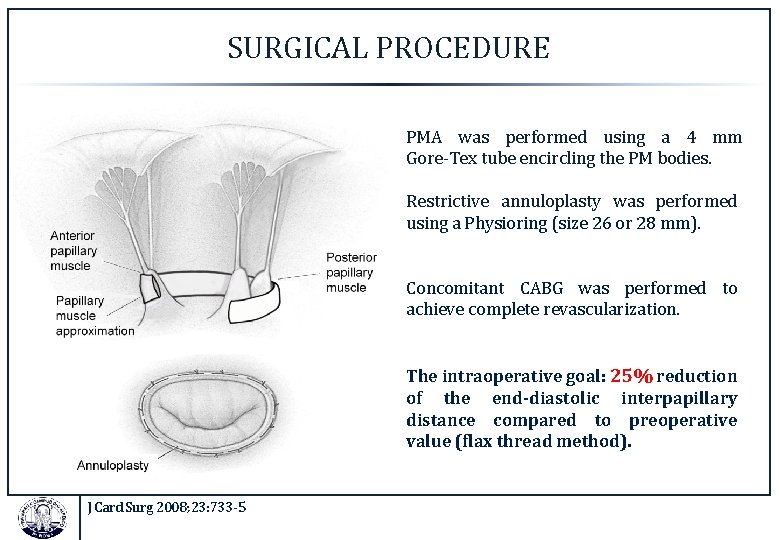
SURGICAL PROCEDURE PMA was performed using a 4 mm Gore-Tex tube encircling the PM bodies. Restrictive annuloplasty was performed using a Physioring (size 26 or 28 mm). Concomitant CABG was performed to achieve complete revascularization. The intraoperative goal: 25% reduction of the end-diastolic interpapillary distance compared to preoperative value (flax thread method). J Card Surg 2008; 23: 733 -5
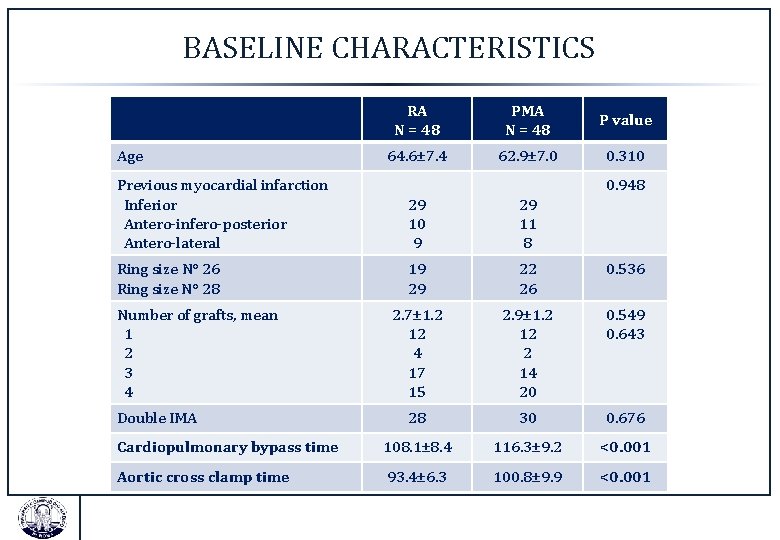
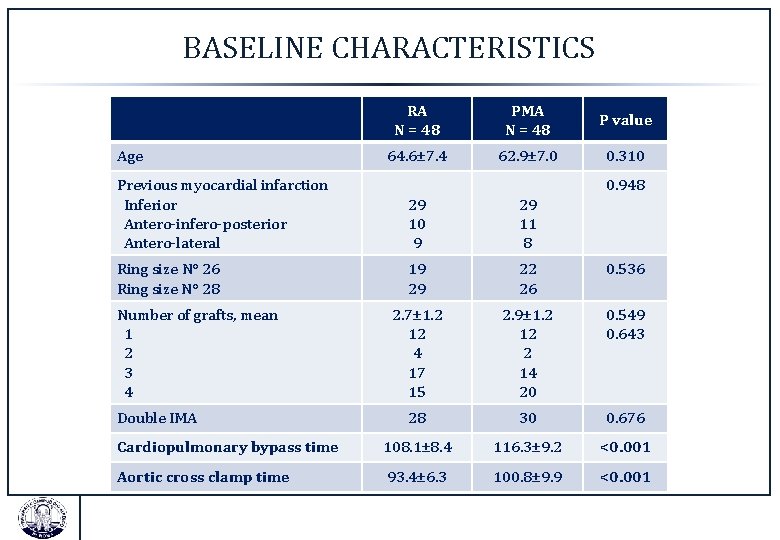
BASELINE CHARACTERISTICS Age RA N = 48 PMA N = 48 P value 64. 6± 7. 4 62. 9± 7. 0 0. 310 Previous myocardial infarction Inferior Antero-infero-posterior Antero-lateral 29 10 9 29 11 8 Ring size N° 26 Ring size N° 28 19 29 22 26 0. 536 2. 7± 1. 2 12 4 17 15 2. 9± 1. 2 12 2 14 20 0. 549 0. 643 28 30 0. 676 Cardiopulmonary bypass time 108. 1± 8. 4 116. 3± 9. 2 <0. 001 Aortic cross clamp time 93. 4± 6. 3 100. 8± 9. 9 <0. 001 Number of grafts, mean 1 2 3 4 Double IMA 0. 948
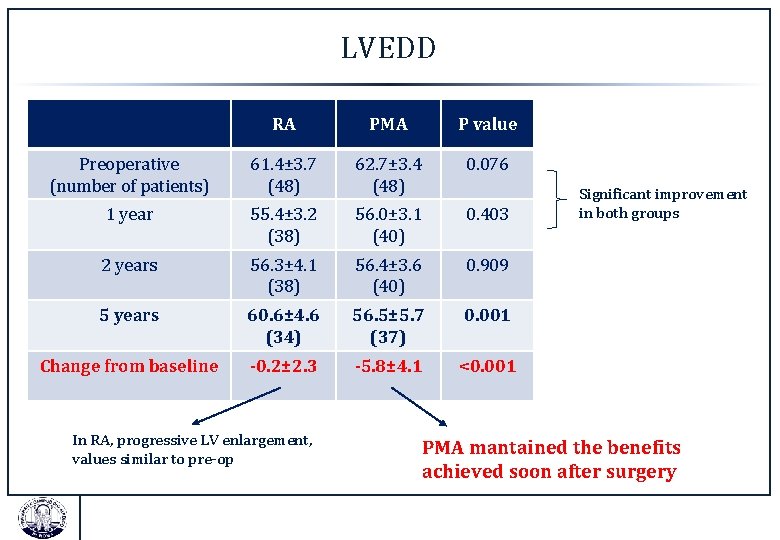
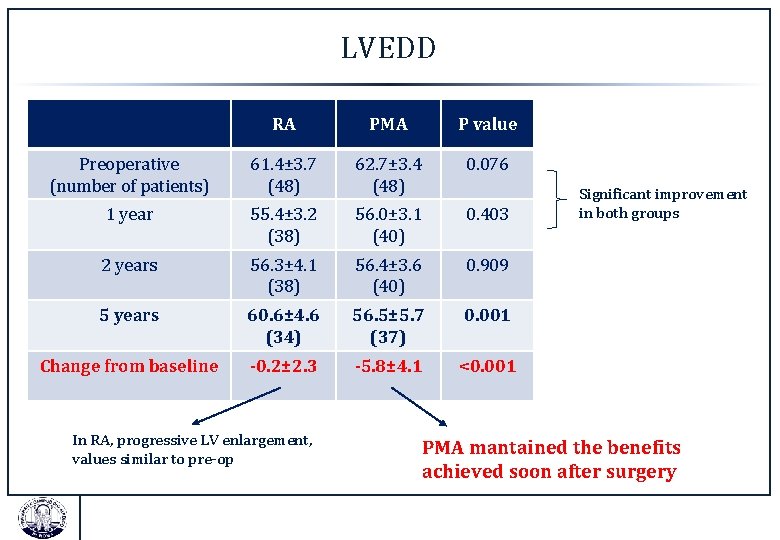
LVEDD RA PMA P value Preoperative (number of patients) 61. 4± 3. 7 (48) 62. 7± 3. 4 (48) 0. 076 1 year 55. 4± 3. 2 (38) 56. 0± 3. 1 (40) 0. 403 2 years 56. 3± 4. 1 (38) 56. 4± 3. 6 (40) 0. 909 5 years 60. 6± 4. 6 (34) 56. 5± 5. 7 (37) 0. 001 Change from baseline -0. 2± 2. 3 -5. 8± 4. 1 <0. 001 In RA, progressive LV enlargement, values similar to pre-op Significant improvement in both groups PMA mantained the benefits achieved soon after surgery
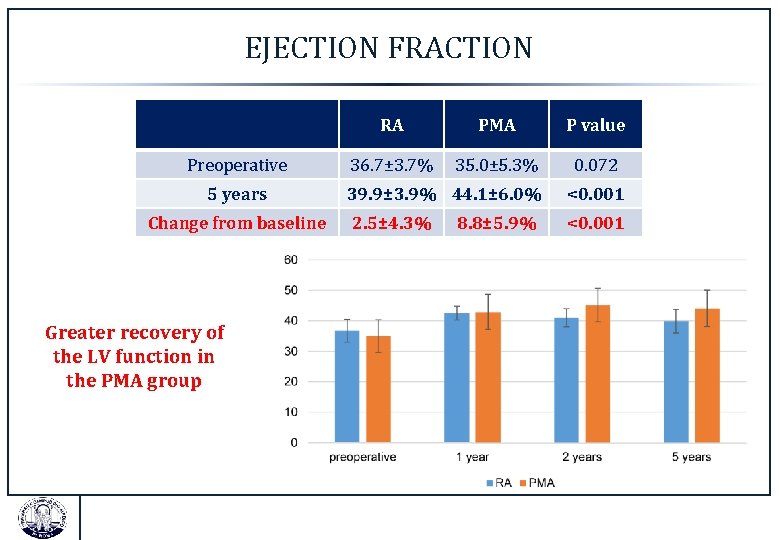
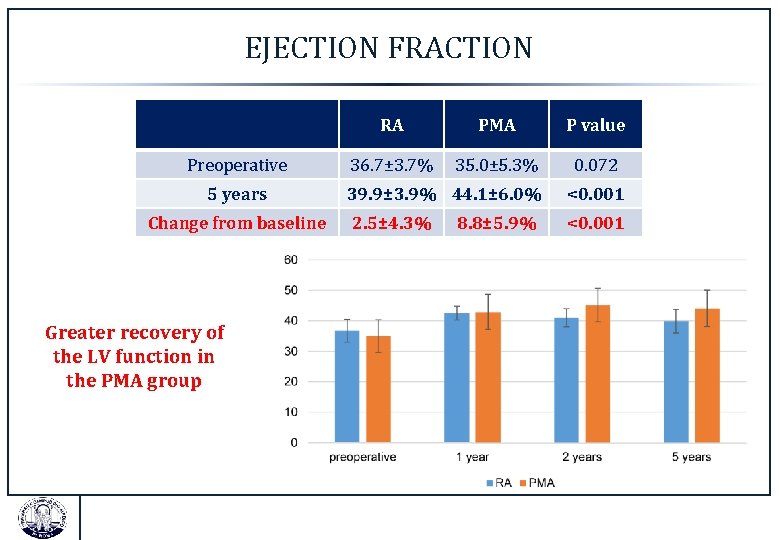
EJECTION FRACTION Preoperative 5 years Change from baseline Greater recovery of the LV function in the PMA group RA PMA P value 36. 7± 3. 7% 35. 0± 5. 3% 0. 072 39. 9± 3. 9% 44. 1± 6. 0% <0. 001 2. 5± 4. 3% <0. 001 8. 8± 5. 9%
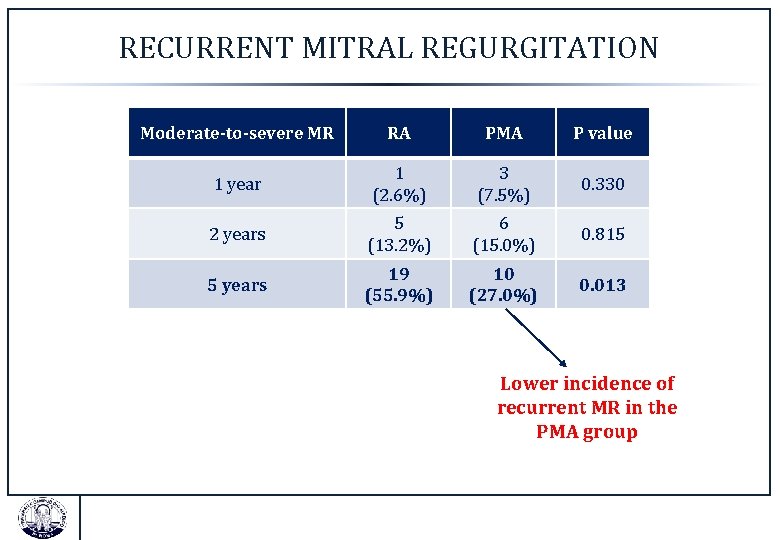
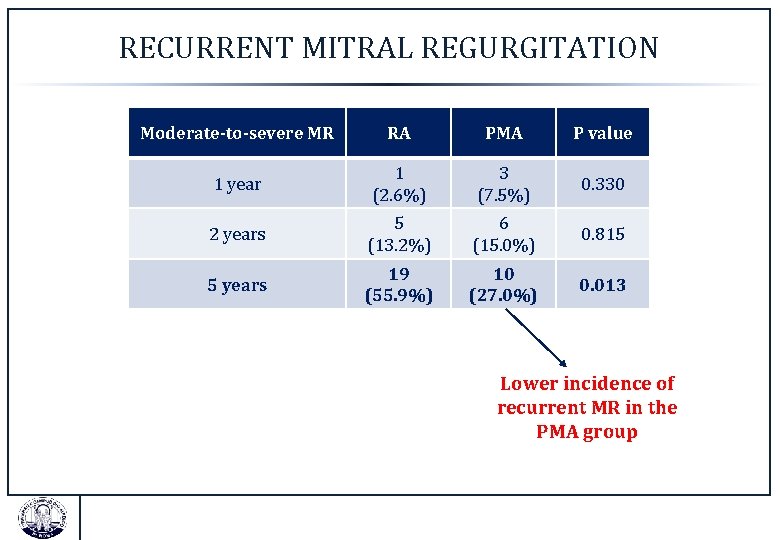
RECURRENT MITRAL REGURGITATION Moderate-to-severe MR RA PMA P value 1 year 1 (2. 6%) 3 (7. 5%) 0. 330 2 years 5 (13. 2%) 6 (15. 0%) 0. 815 5 years 19 (55. 9%) 10 (27. 0%) 0. 013 Lower incidence of recurrent MR in the PMA group
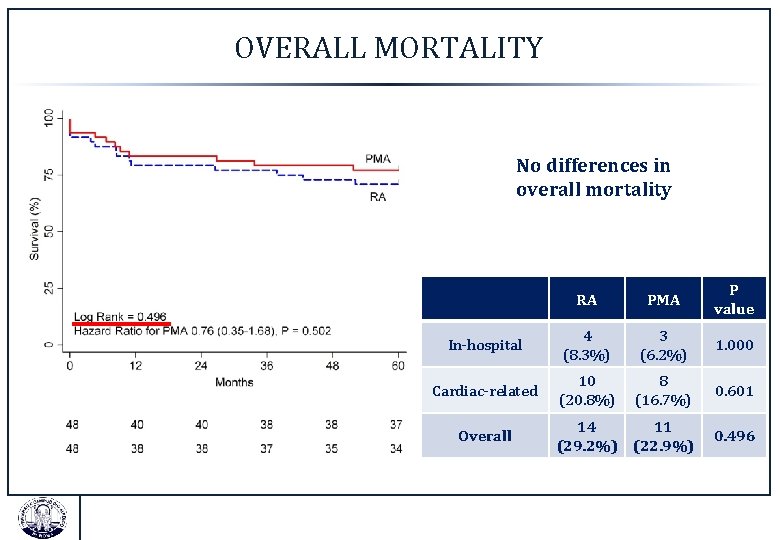
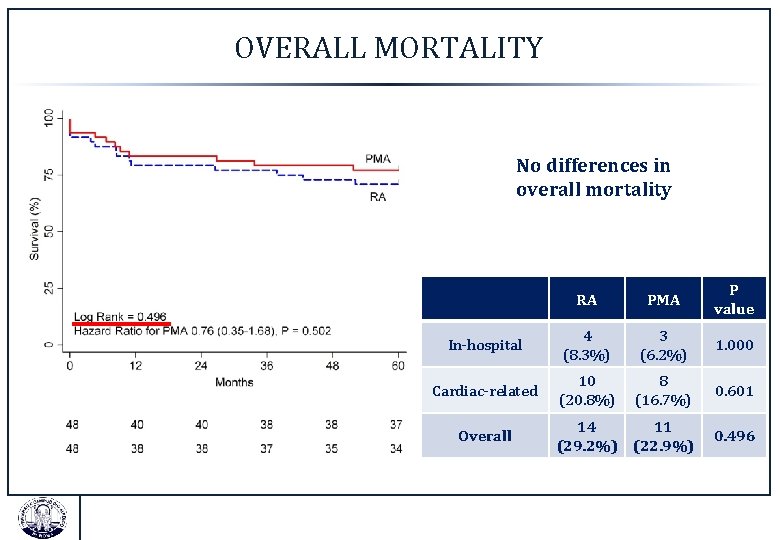
OVERALL MORTALITY No differences in overall mortality RA PMA P value In-hospital 4 (8. 3%) 3 (6. 2%) 1. 000 Cardiac-related 10 (20. 8%) 8 (16. 7%) 0. 601 14 11 (29. 2%) (22. 9%) 0. 496 Overall
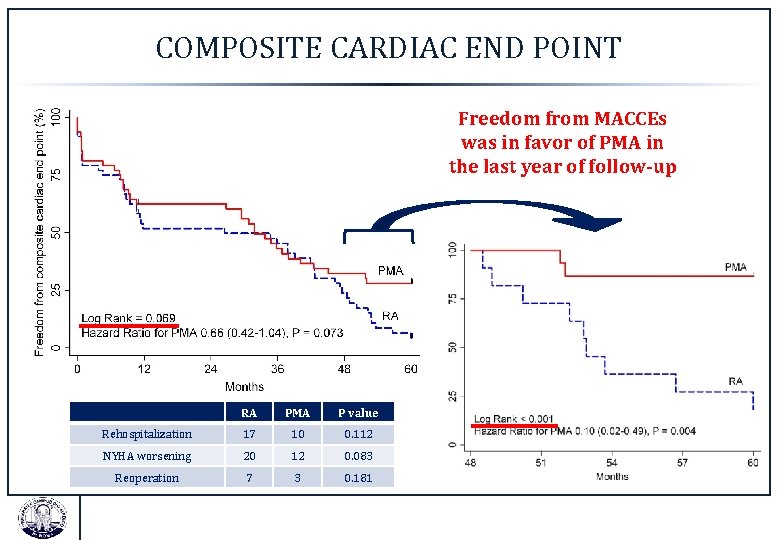
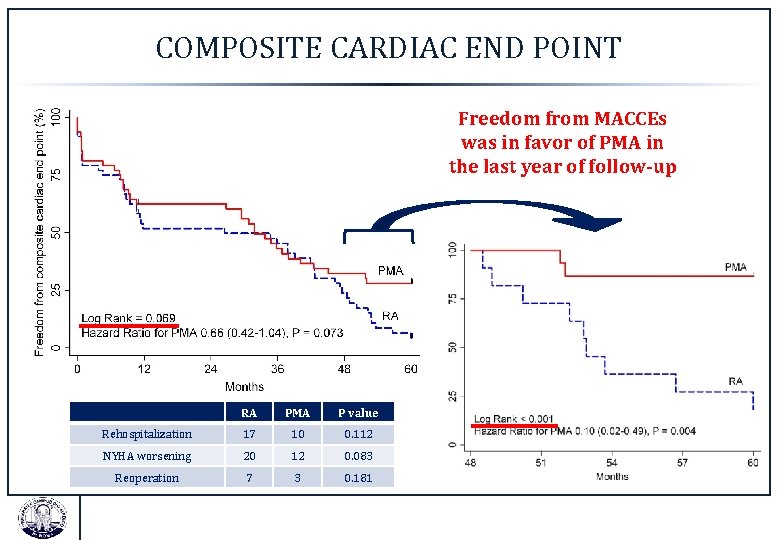
COMPOSITE CARDIAC END POINT Freedom from MACCEs was in favor of PMA in the last year of follow-up RA PMA P value Rehospitalization 17 10 0. 112 NYHA worsening 20 12 0. 083 Reoperation 7 3 0. 181
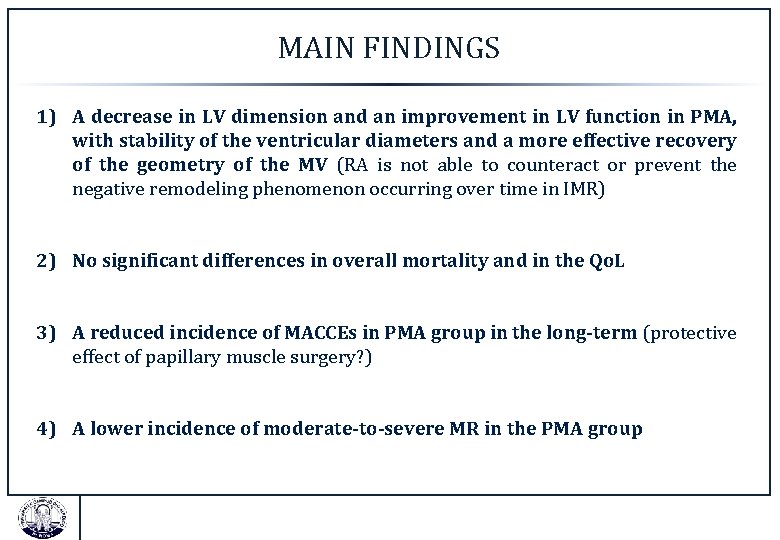
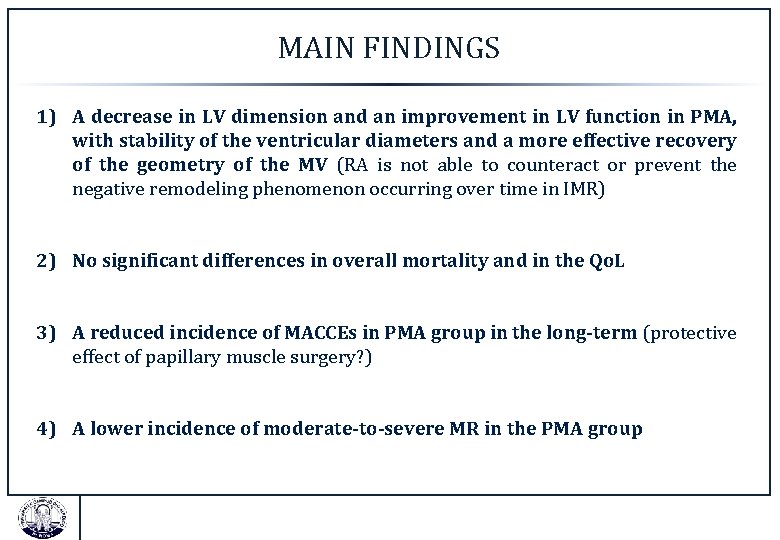
MAIN FINDINGS 1) A decrease in LV dimension and an improvement in LV function in PMA, with stability of the ventricular diameters and a more effective recovery of the geometry of the MV (RA is not able to counteract or prevent the negative remodeling phenomenon occurring over time in IMR) 2) No significant differences in overall mortality and in the Qo. L 3) A reduced incidence of MACCEs in PMA group in the long-term (protective effect of papillary muscle surgery? ) 4) A lower incidence of moderate-to-severe MR in the PMA group
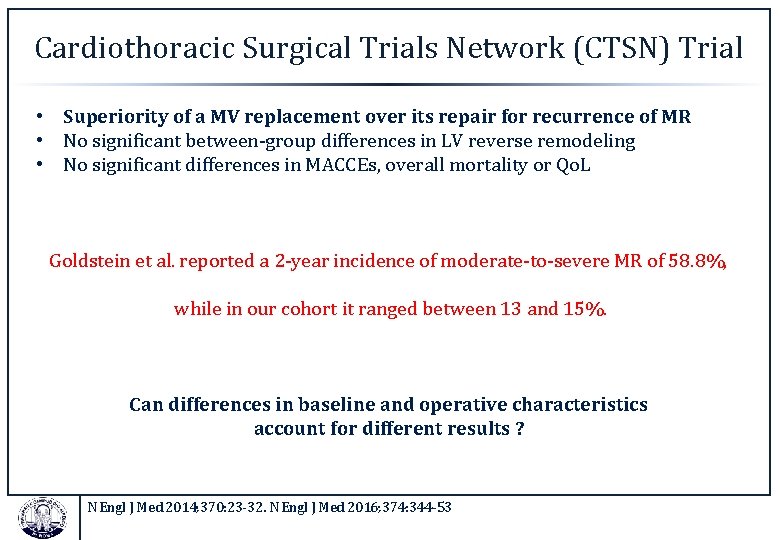
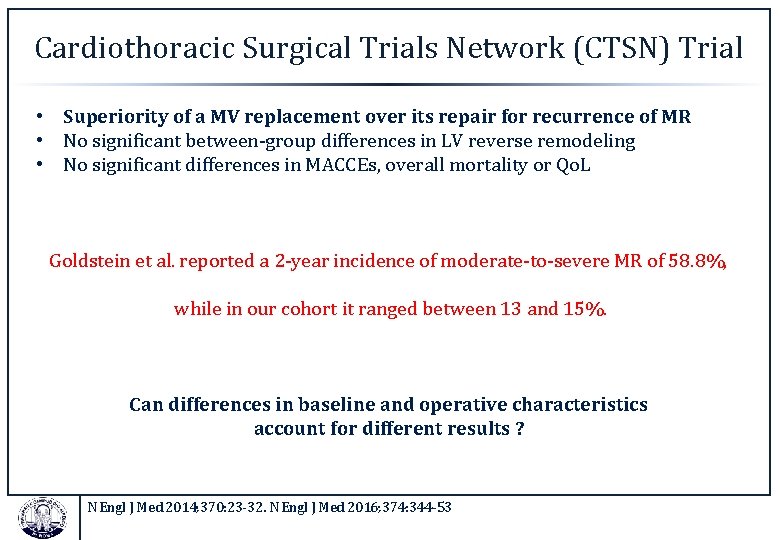
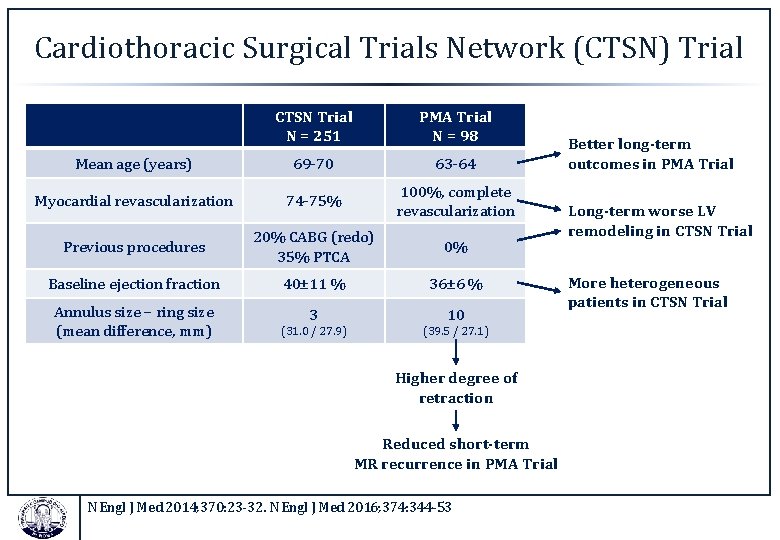
Cardiothoracic Surgical Trials Network (CTSN) Trial • Superiority of a MV replacement over its repair for recurrence of MR • No significant between-group differences in LV reverse remodeling • No significant differences in MACCEs, overall mortality or Qo. L Goldstein et al. reported a 2 -year incidence of moderate-to-severe MR of 58. 8%, while in our cohort it ranged between 13 and 15%. Can differences in baseline and operative characteristics account for different results ? N Engl J Med 2014; 370: 23 -32. N Engl J Med 2016; 374: 344 -53
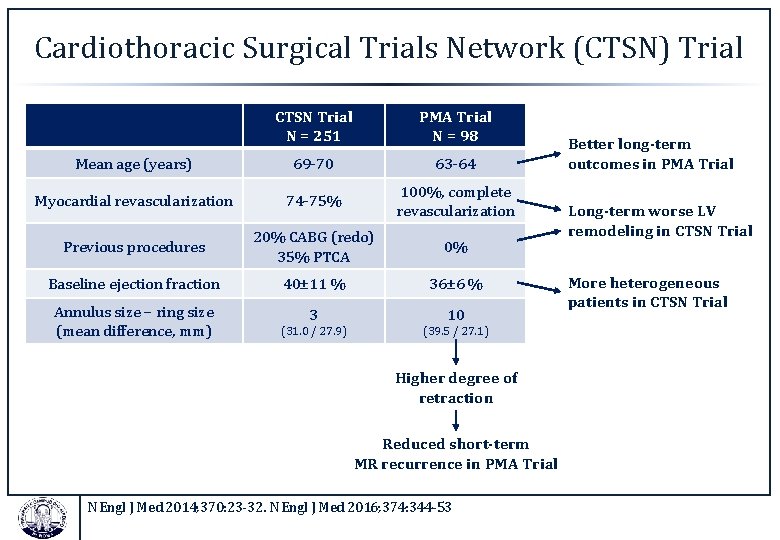
Cardiothoracic Surgical Trials Network (CTSN) Trial CTSN Trial N = 251 PMA Trial N = 98 Mean age (years) 69 -70 63 -64 Myocardial revascularization 74 -75% 100%, complete revascularization Previous procedures 20% CABG (redo) 35% PTCA 0% Baseline ejection fraction 40± 11 % 36± 6 % Annulus size – ring size (mean difference, mm) 3 10 (31. 0 / 27. 9) (39. 5 / 27. 1) Higher degree of retraction Reduced short-term MR recurrence in PMA Trial N Engl J Med 2014; 370: 23 -32. N Engl J Med 2016; 374: 344 -53 Better long-term outcomes in PMA Trial Long-term worse LV remodeling in CTSN Trial More heterogeneous patients in CTSN Trial
CONCLUSION The “Achilles heel” of MV repair in IMR is the long-term adverse LV remodeling, which influences the geometrical relationships within the ventricle and the equilibrium between forces. Papillary muscle surgery together with complete myocardial revascularization can address these issues improving the general negative outcomes of this procedure. Direct comparison of a “complete” MV repair strategy, including papillary muscle surgery, versus chordal-sparing mitral replacement should be advocated to define the best treatment in IMR
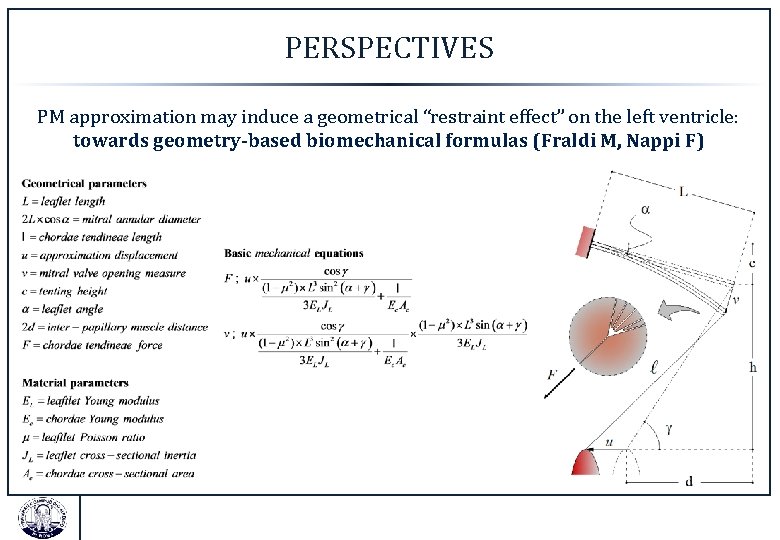
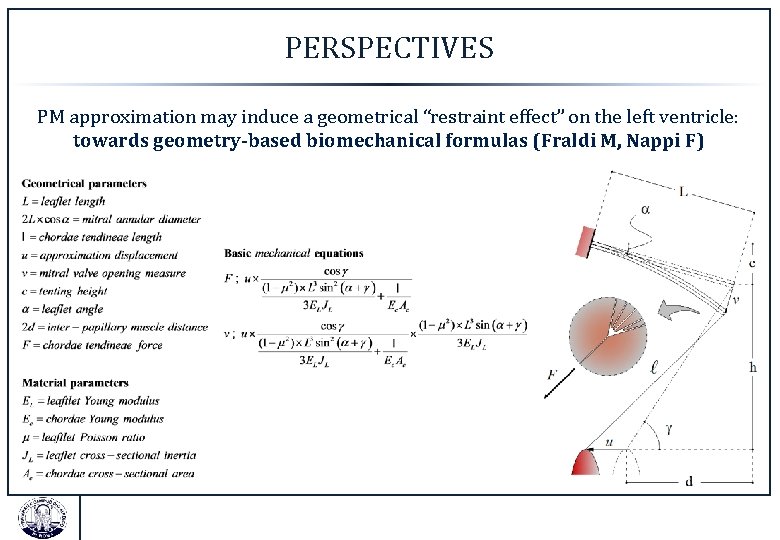
PERSPECTIVES PM approximation may induce a geometrical “restraint effect” on the left ventricle: towards geometry-based biomechanical formulas (Fraldi M, Nappi F)

Grazie per l’attenzione ! ( Thank You for Your attention ! )