Pap smears and Cultures Maria Horvat MD FACOG








- Slides: 37
Pap smears and Cultures Maria Horvat, MD, FACOG
Objectives Know how and when to perform Pap smear Know how and when to perform cultures
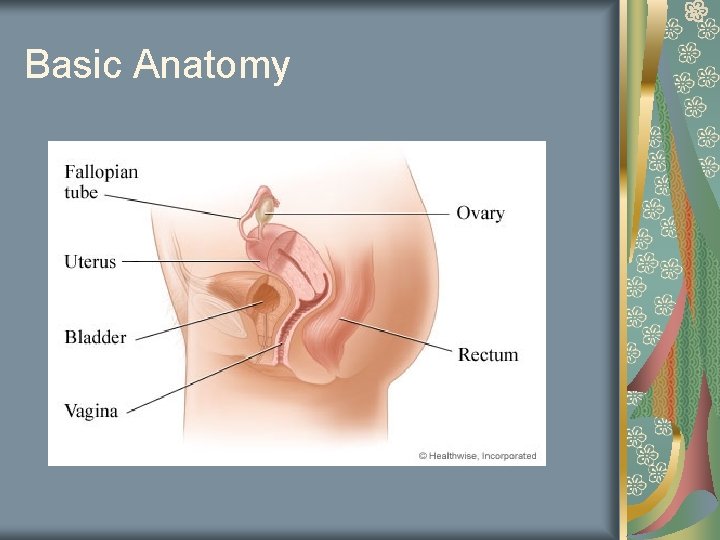
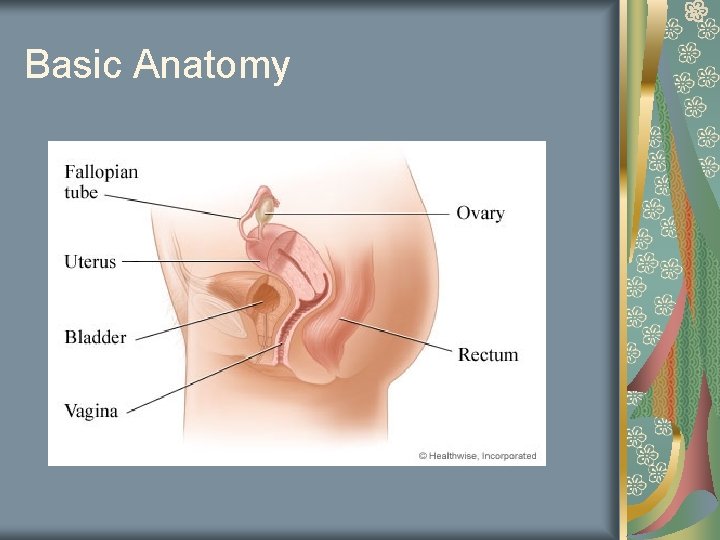
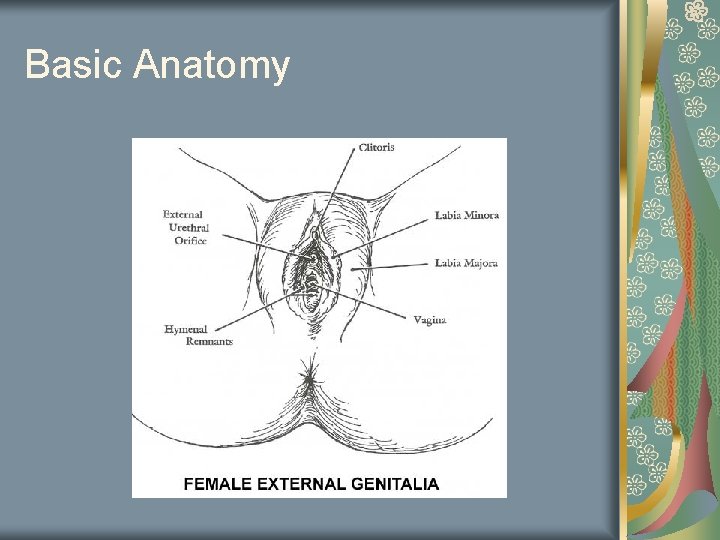
Basic Anatomy

Basic Anatomy
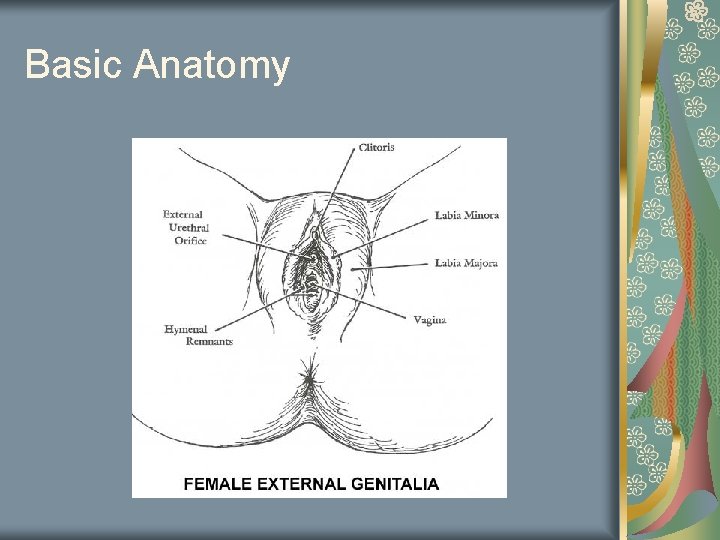
Basic Anatomy
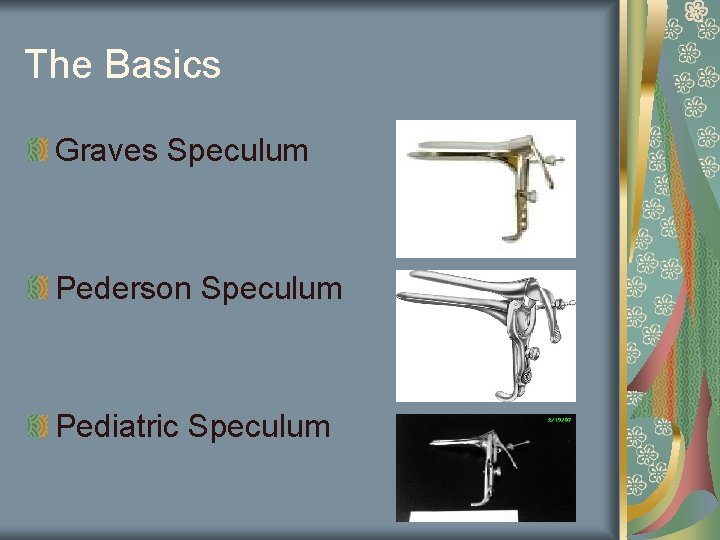
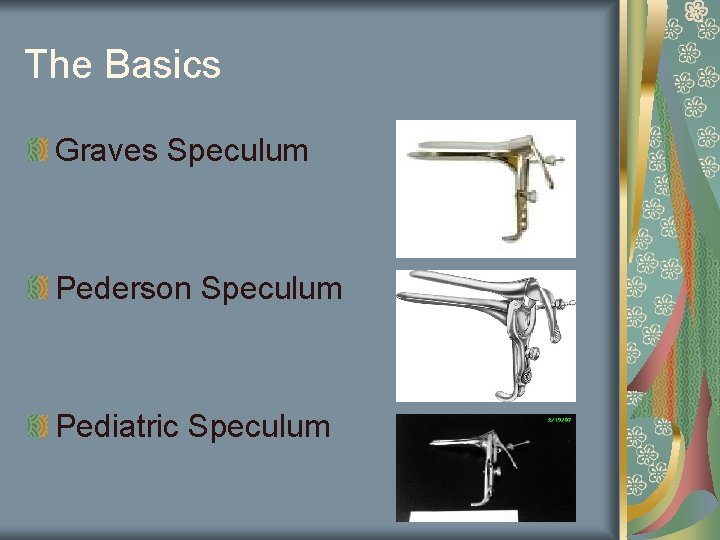
The Basics Graves Speculum Pederson Speculum Pediatric Speculum
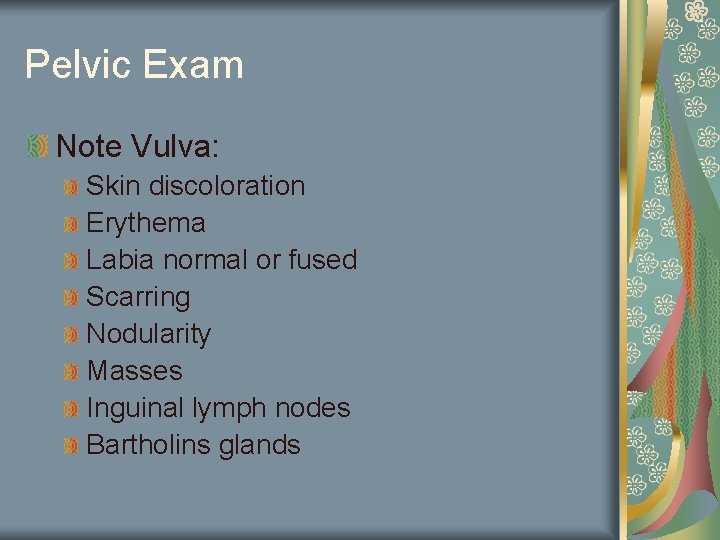
Pelvic Exam Note Vulva: Skin discoloration Erythema Labia normal or fused Scarring Nodularity Masses Inguinal lymph nodes Bartholins glands
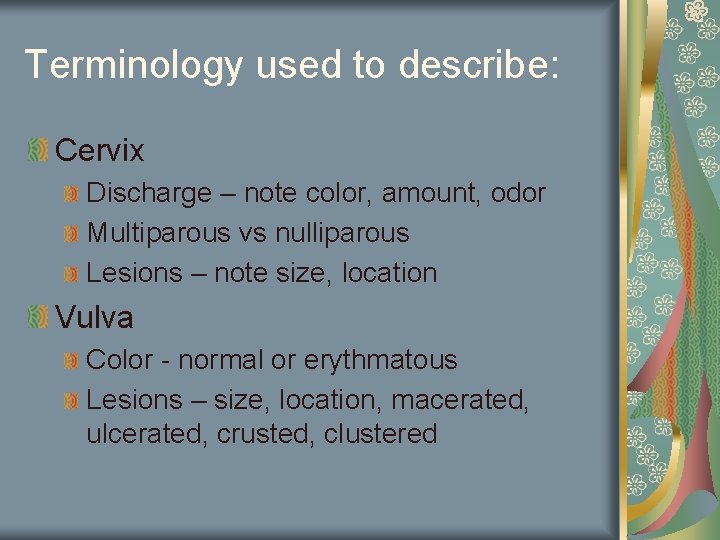
Terminology used to describe: Cervix Discharge – note color, amount, odor Multiparous vs nulliparous Lesions – note size, location Vulva Color - normal or erythmatous Lesions – size, location, macerated, ulcerated, crusted, clustered
To perform Pap: Pick appropriate speculum Warm speculum with water Neutral touch on inner thigh Introduce speculum Note color, odor, amount of discharge Wipe away excess mucous Perform Pap Perform cultures
Tips: Correct positioning Have Pap and cultures ready Correct speculum size Medical assistant chaperone especially for males Litmus ph paper ready

Thin prep: Liquid based More effective in detecting LSIL’s and more severe lesions Use spatula and brush Conventional Pap Slide Must be fixed in timely manner Sensitivity 50%
Current recommendations on Pap and cultures 1 st Pap within 3 years of 1 st sexual intercourse By the age of 21 if no sexual activity Annual Pap when women are into their 20’s Pap and Gonorrhea/Chlamydia culture for sexually active females until age 2 At age 30 if you have 3 consecutive normal pap tests or recent pap and HPV is negative – can space out to q 2 -3 years
Recommendations are always changing ACS APGO (Association of Professors of Gynecology and Obstetrics) ACOG American college of Physicians
There always variations Post-menopause: Some guidelines require – no pap ACOG still advocates periodic pap q 3 -5 years Patient has had a hysterectomy If for benign reason pap may be performed q 35 years Yearly if: Cervix present History of abnormal paps History of gyne cancer History of DES exposure History of cervical cancer Smoking (increases chances of vaginal cancer)

Risk factors for cervical dysplasia Sexual activity at early age Multiple partners History of abnormal pap’s Smoking History of STD’s Immune status (HIV, chemotherapy) HPV infection Alcoholism Poor diet
Remember! Any obvious lesion needs to be biopsied!
Infection Herpes Trichomonas Gonorrhea Chlamydia Bacterial Vaginosis Yeast Vaginitis Syphilis
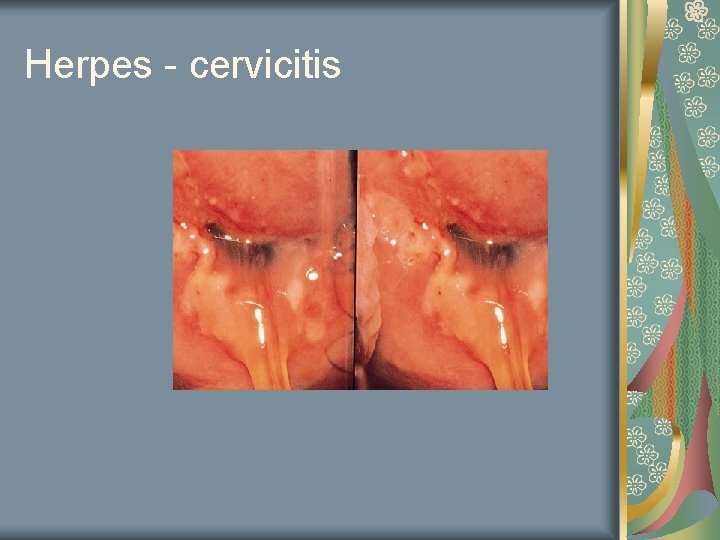
Herpes Painful vulvar lesion Clusters with a superficial crust 10 – 20% cultures give false negative 22% of adults have antibodies Other associated symptoms Pain, fever, headaches, malaise, itching, tingling Tends to be recurrent
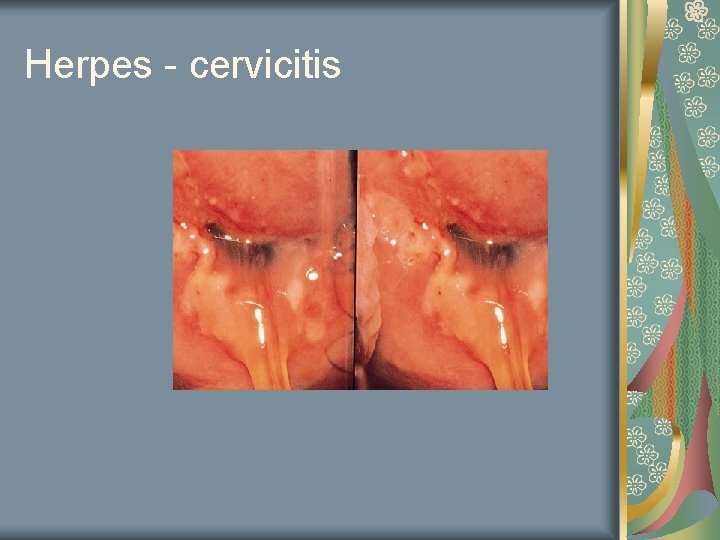
Herpes - cervicitis

Herpes - vulva
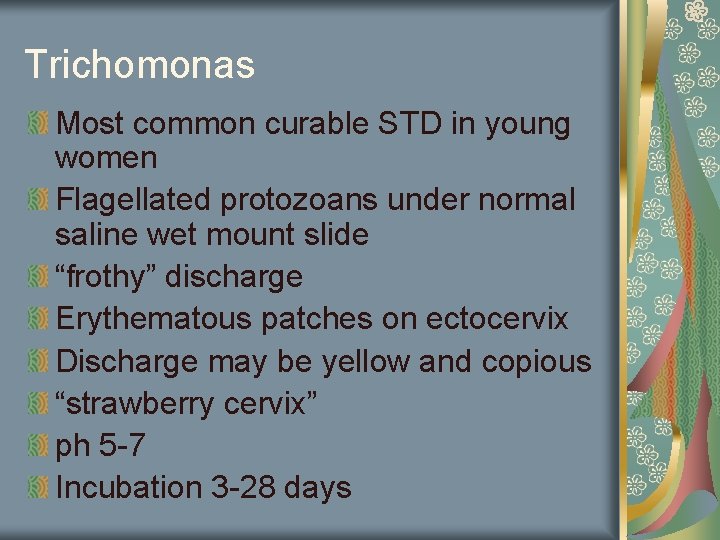
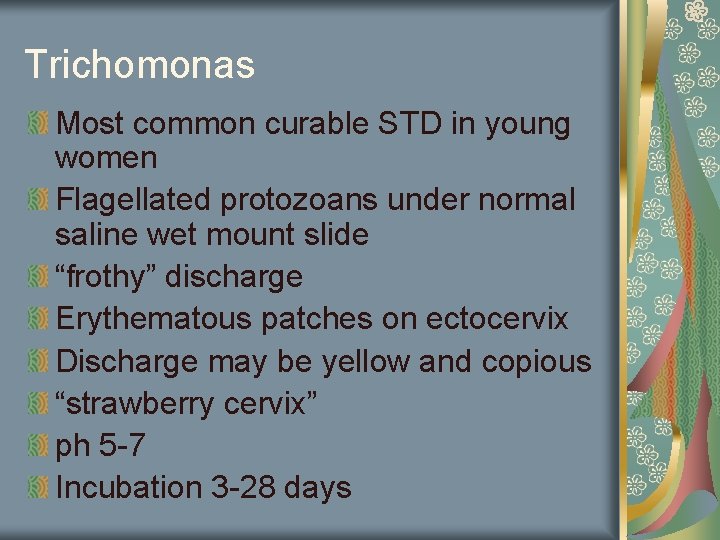
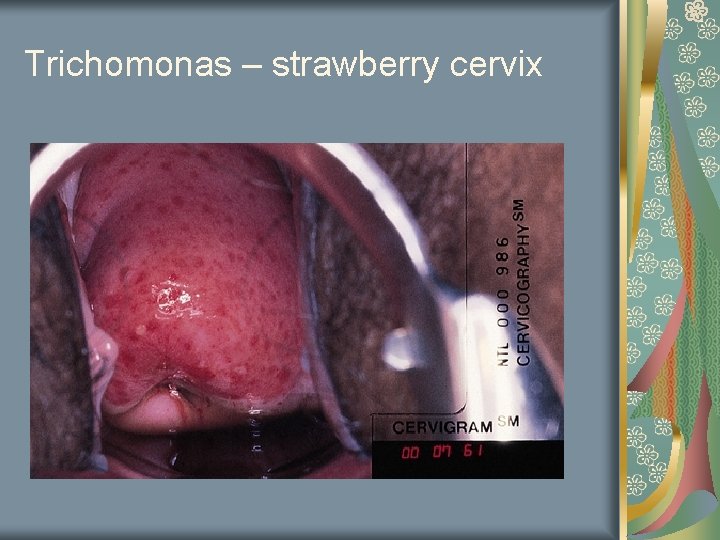
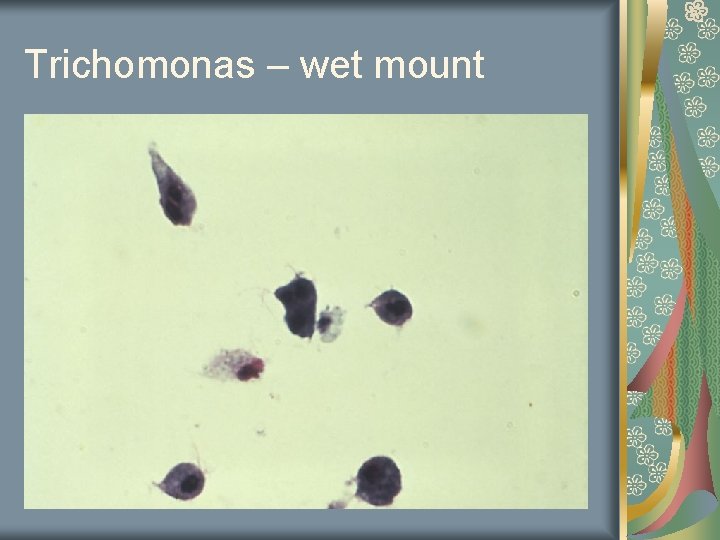
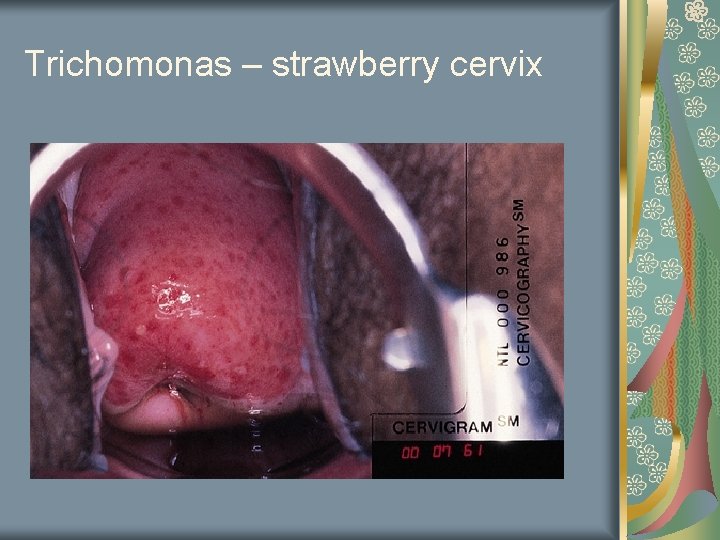
Trichomonas Most common curable STD in young women Flagellated protozoans under normal saline wet mount slide “frothy” discharge Erythematous patches on ectocervix Discharge may be yellow and copious “strawberry cervix” ph 5 -7 Incubation 3 -28 days
Trichomonas – strawberry cervix
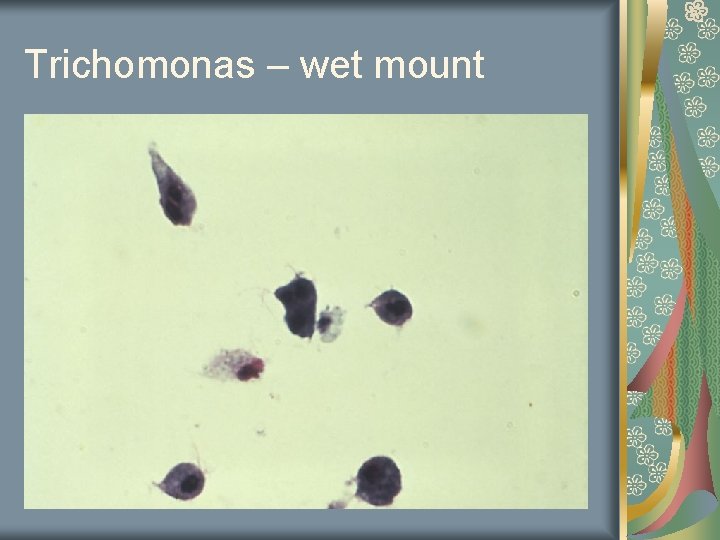
Trichomonas – wet mount
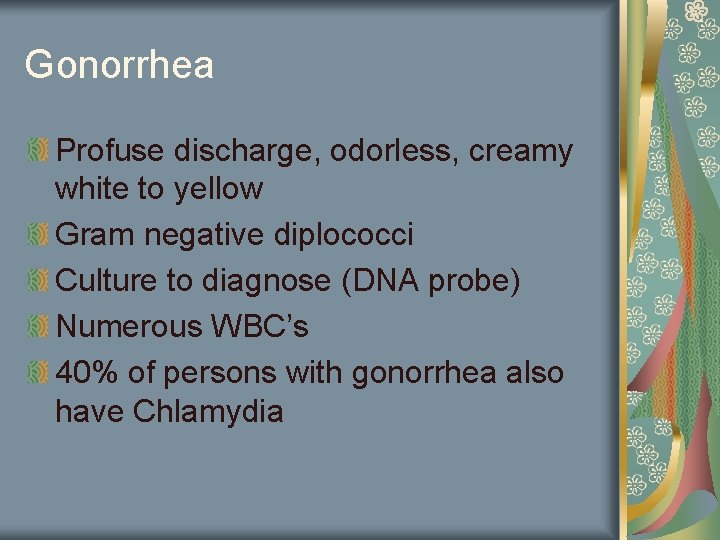
Gonorrhea Profuse discharge, odorless, creamy white to yellow Gram negative diplococci Culture to diagnose (DNA probe) Numerous WBC’s 40% of persons with gonorrhea also have Chlamydia

Gonococcal cervicitis
Chlamydia Mucopurulent discharge 60% Intracellular parasite Most prevalent venereal disease in US Post coital bleeding 8% are asymptomatic

Chlamydia cervicitis
Bacterial Vaginitis Patient complains of fishy odor or general vaginal discomfort Diagnose by saline wet mount ph>4. 5 Positive whiff test Clue cells (bacteria cling to edge of epithelial cells) Caused by decreased hydrogen peroxide producing lactobacilli and increased gardnerella

Bacterial Vaginitis – Clue Cells
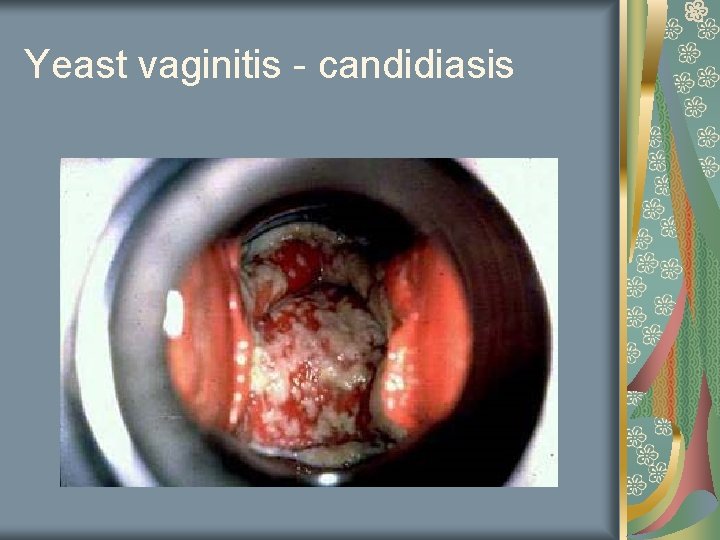
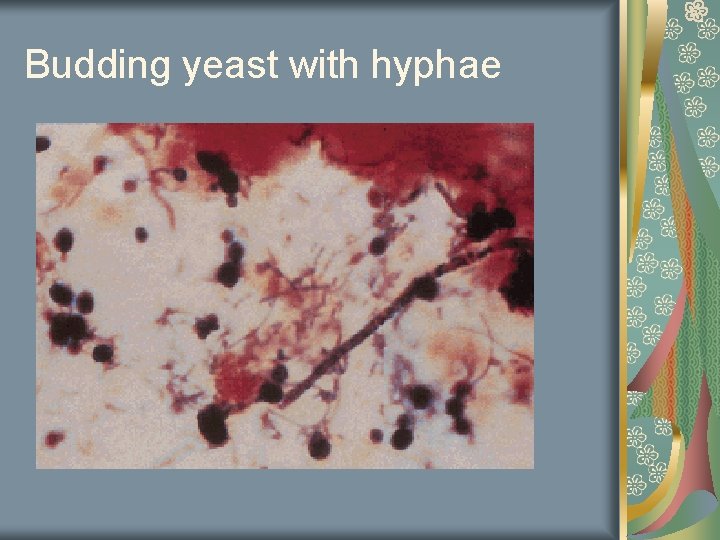
Yeast Vaginitis KOH slide Budding yeast with hyphea Erythmatous vagina White discharge
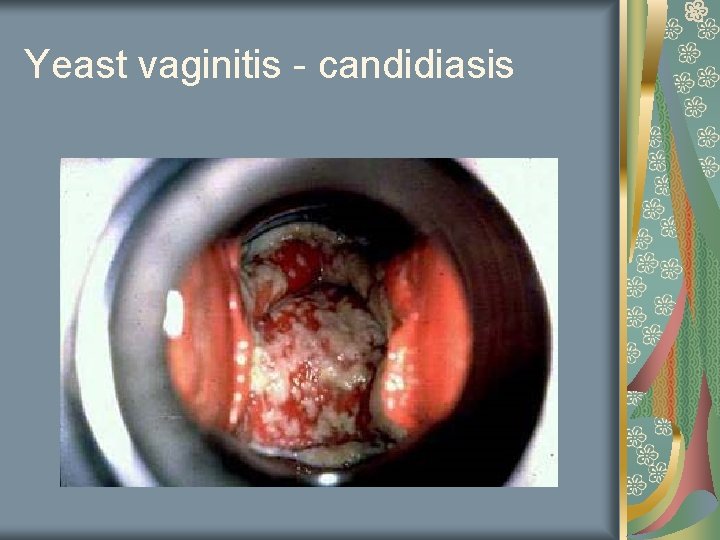
Yeast vaginitis - candidiasis
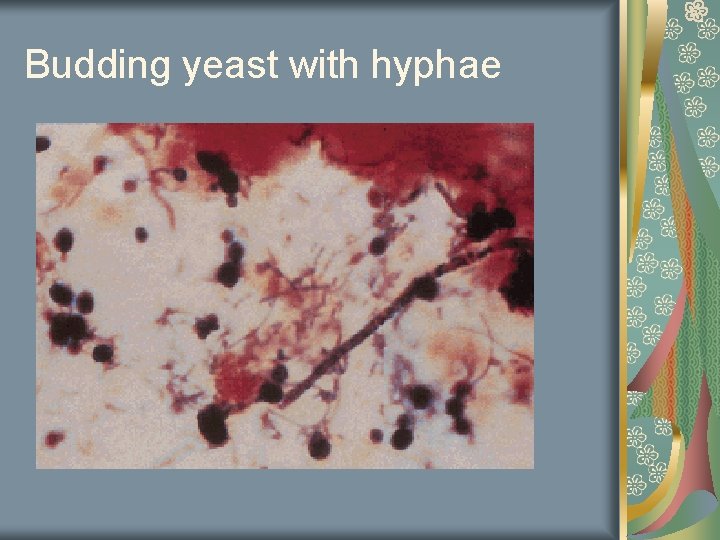
Budding yeast with hyphae
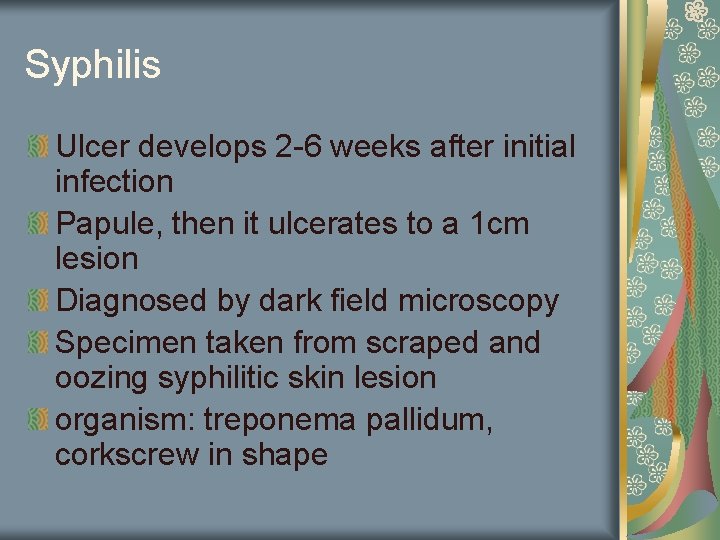
Syphilis Ulcer develops 2 -6 weeks after initial infection Papule, then it ulcerates to a 1 cm lesion Diagnosed by dark field microscopy Specimen taken from scraped and oozing syphilitic skin lesion organism: treponema pallidum, corkscrew in shape

Primary syphilitic lesion
Other recommendations Pap test as previously discussed Annual breast exam Baseline mammogram at age 35 -40 Annual mammogram starting at age 40 Annual pelvic exam Annual rectal, heme-occult starting at age 50 Dexa screen q 2 -3 years Colonoscopy q 10 years starting at age 50
References www. chups. jussieu. fr/polys/gyneco/sy philis. jpg www. kcom. edu www. usc. edu www. images. md commons. wikimedia. org/wiki/Imag e: Trichomonas
 Maria horvat md
Maria horvat md Spiritual organization
Spiritual organization Unacceptable blood smears
Unacceptable blood smears Unacceptable blood smears
Unacceptable blood smears Blood smear practical
Blood smear practical Unacceptable blood smears
Unacceptable blood smears Iva horvat radman
Iva horvat radman 4 velika proroka
4 velika proroka Lara horvat
Lara horvat Ivor horvat
Ivor horvat Adenozil kobalamin
Adenozil kobalamin Intermediarno
Intermediarno Anulociti
Anulociti Marina horvat pavlic
Marina horvat pavlic Jelena horvat
Jelena horvat Maria felicia de jesús sacramentado maría teresa arminda
Maria felicia de jesús sacramentado maría teresa arminda Examining social life
Examining social life Recreational activities across cultures and genders
Recreational activities across cultures and genders Chapter 20:12 measuring specific gravity
Chapter 20:12 measuring specific gravity Japan indulgence vs restraint
Japan indulgence vs restraint Atakapans
Atakapans What aspects of minoan culture did the mycenaeans adopt
What aspects of minoan culture did the mycenaeans adopt Cultures and organizations software of the mind
Cultures and organizations software of the mind School of languages cultures and societies
School of languages cultures and societies The stone ages and early cultures
The stone ages and early cultures Abnormal pap and colposcopy
Abnormal pap and colposcopy Subcultures
Subcultures Which cultures believe in reincarnation
Which cultures believe in reincarnation In what ways did neighboring cultures influence japan?
In what ways did neighboring cultures influence japan? Religions that believe in reincarnation
Religions that believe in reincarnation Slidetodoc.com
Slidetodoc.com Which cultures believe in reincarnation
Which cultures believe in reincarnation Small culture
Small culture Taste different cultures
Taste different cultures What is culture
What is culture Individualistic culture vs. collectivist culture
Individualistic culture vs. collectivist culture Collectivistic cultures
Collectivistic cultures Which cultures believe in reincarnation
Which cultures believe in reincarnation