Pancytopenia and Aplastic Anemia Pancytopenia Definition The simultaneous






- Slides: 33
Pancytopenia and Aplastic Anemia

Pancytopenia : Definition • The simultaneous presence of – Anemia – Leukopenia – Thrombocytopenia • Hb< 11. 5 g/d. L (adult females), < 13. 5 g/d. L (adult males) • WBC < 4 x 10^9/L (4000/mm 3) • Plt. < 150 x 10^9/L (150. 000/mm 3 )
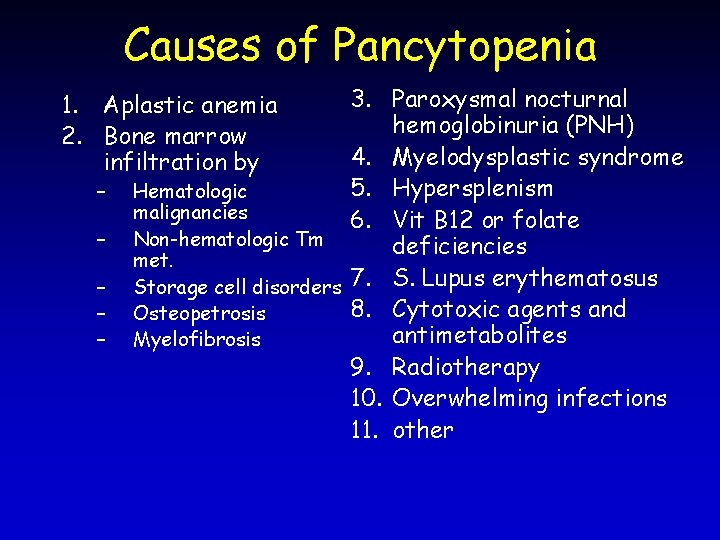
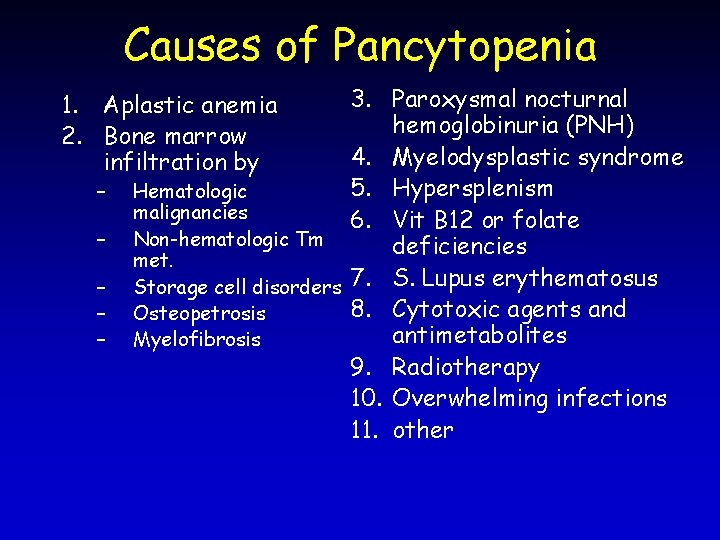
Causes of Pancytopenia 3. Paroxysmal nocturnal hemoglobinuria (PNH) 4. Myelodysplastic syndrome 5. Hypersplenism Hematologic malignancies 6. Vit B 12 or folate Non-hematologic Tm deficiencies met. Storage cell disorders 7. S. Lupus erythematosus 8. Cytotoxic agents and Osteopetrosis antimetabolites Myelofibrosis 9. Radiotherapy 10. Overwhelming infections 11. other 1. Aplastic anemia 2. Bone marrow infiltration by – – –
Clinical features • Related to – Pancytopenia Or – Underlying condition/disease
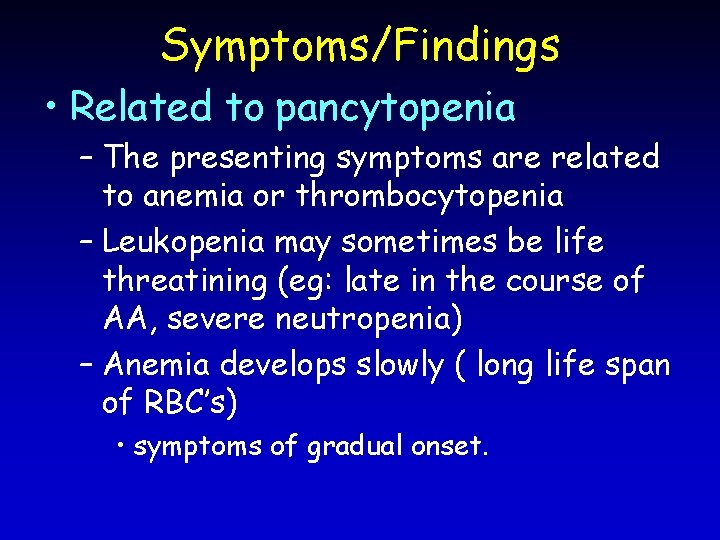
Symptoms/Findings • Related to pancytopenia – The presenting symptoms are related to anemia or thrombocytopenia – Leukopenia may sometimes be life threatining (eg: late in the course of AA, severe neutropenia) – Anemia develops slowly ( long life span of RBC’s) • symptoms of gradual onset.

Symptoms/Findings • Related to pancytopenia – Thrombocytopenic type bleeding may occur and – severity depends on the plt. number. eg: spontaneous bleeding indicates plt<20. 000/mm 3 – Infections are related to neutropenia , with severity depending on the decrease in neutrophyl counts.
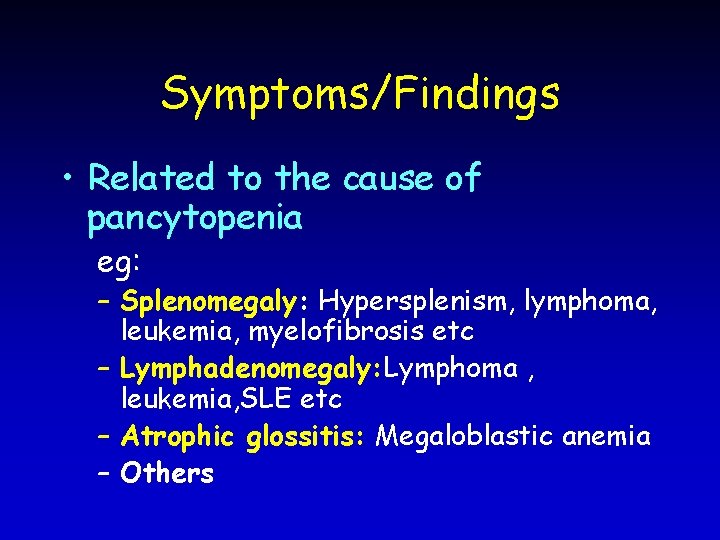
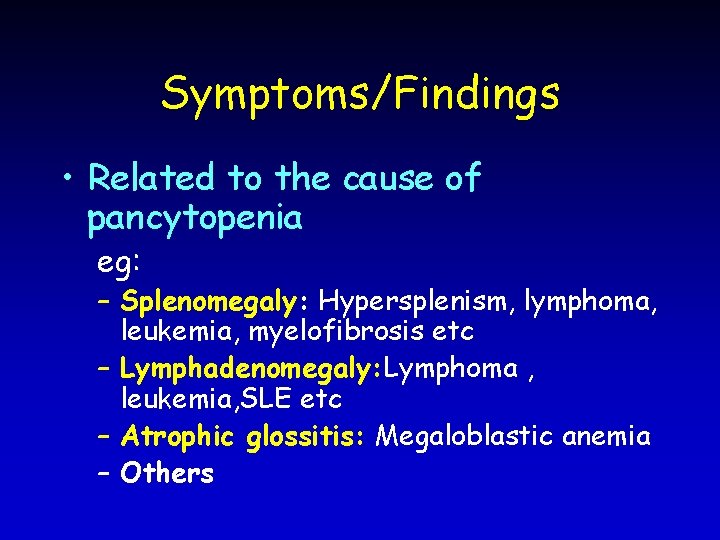
Symptoms/Findings • Related to the cause of pancytopenia eg: – Splenomegaly: Hypersplenism, lymphoma, leukemia, myelofibrosis etc – Lymphadenomegaly: Lymphoma , leukemia, SLE etc – Atrophic glossitis: Megaloblastic anemia – Others
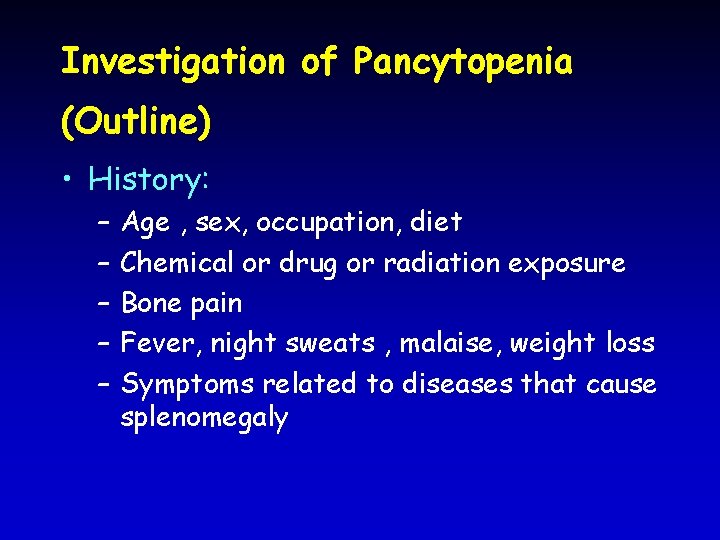
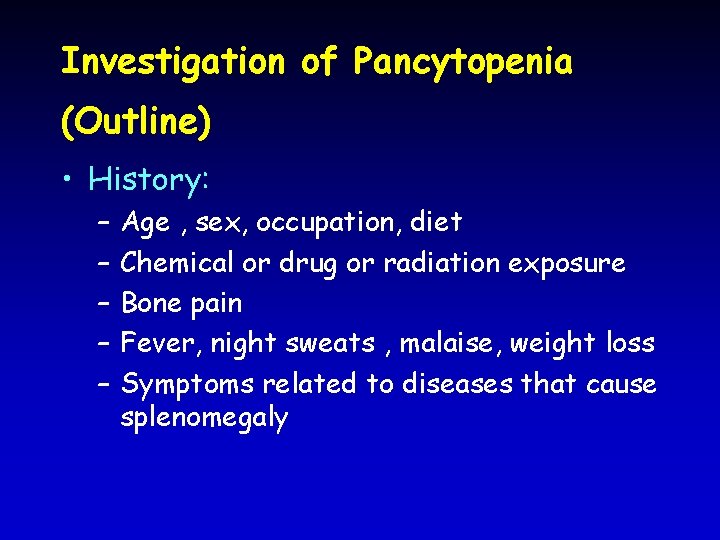
Investigation of Pancytopenia (Outline) • History: – – – Age , sex, occupation, diet Chemical or drug or radiation exposure Bone pain Fever, night sweats , malaise, weight loss Symptoms related to diseases that cause splenomegaly
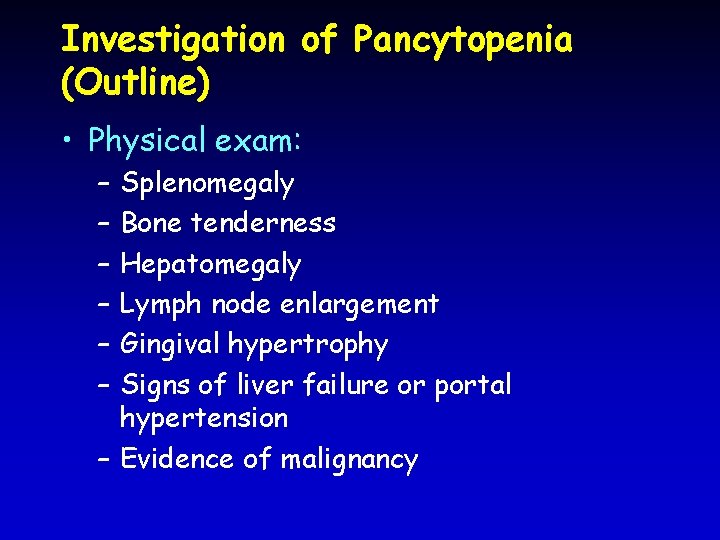
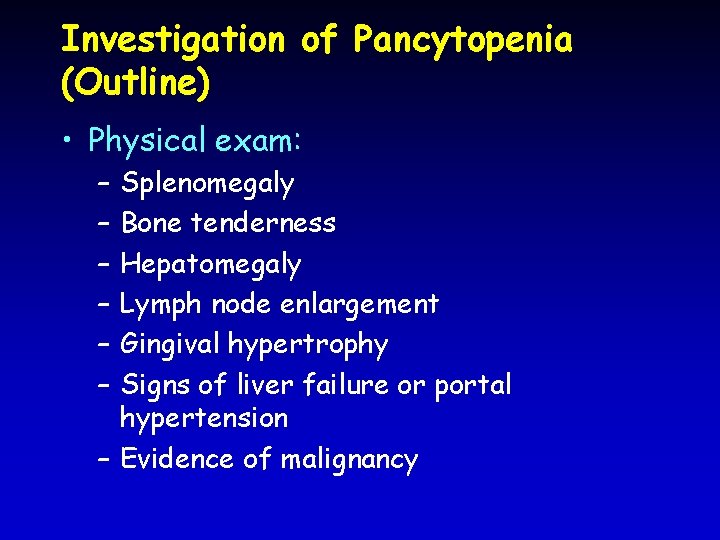
Investigation of Pancytopenia (Outline) • Physical exam: – – – Splenomegaly Bone tenderness Hepatomegaly Lymph node enlargement Gingival hypertrophy Signs of liver failure or portal hypertension – Evidence of malignancy
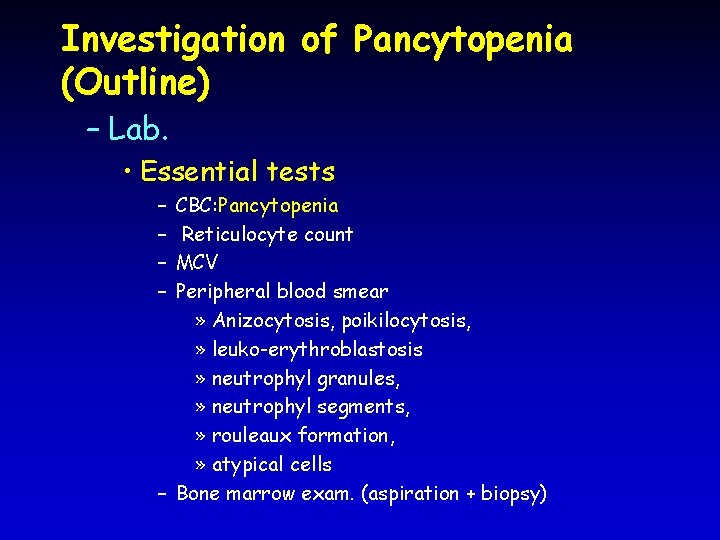
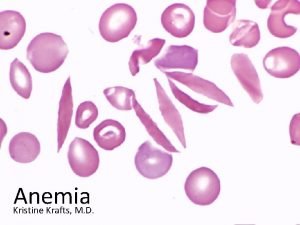
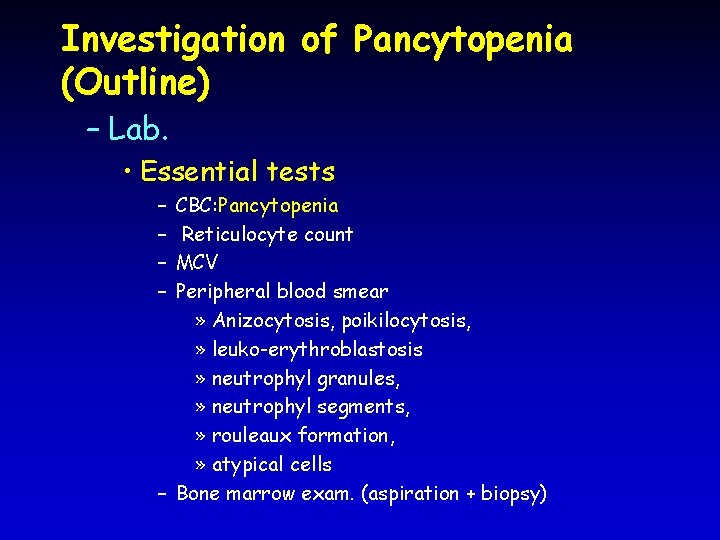
Investigation of Pancytopenia (Outline) – Lab. • Essential tests – – CBC: Pancytopenia Reticulocyte count MCV Peripheral blood smear » Anizocytosis, poikilocytosis, » leuko-erythroblastosis » neutrophyl granules, » neutrophyl segments, » rouleaux formation, » atypical cells – Bone marrow exam. (aspiration + biopsy)

Investigation of Pancytopenia (Outline) • Lab: – Further investigations when required • • • X-Rays: Bone, chest etc Alk. Phosp, acid. Phosp Serum protein electrophoresis Anti-DNA, FANA, etc Urinary proteins (Bence-Jones) Lymph node or other biopsies
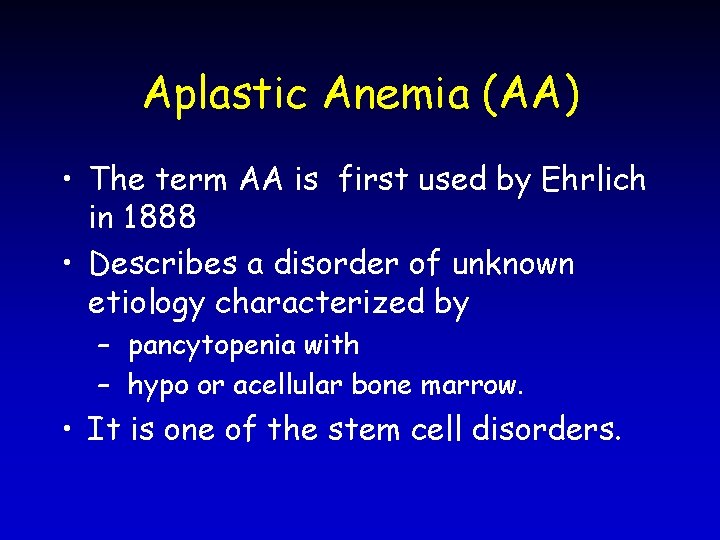
Aplastic Anemia (AA) • The term AA is first used by Ehrlich in 1888 • Describes a disorder of unknown etiology characterized by – pancytopenia with – hypo or acellular bone marrow. • It is one of the stem cell disorders.

Classification of AA I-Inherited AA – Fanconi’s anemia: • Autosomal. recessive inheritance • Skeletal and renal defects • Hyperpigmentation • Small stature • Hypogonadism • Chromosomal changes – Familial AA (non-Fanconi) • Familial but without features of Fanconi’s anemia – Dyskeratosis congenita • Skin, nail and hair abnormalities • Telangiectasia • Alopecia • Abnormal sweating • Mental retardation • Growth failure and hypogonadism – Shwachman–Diamond syndrome
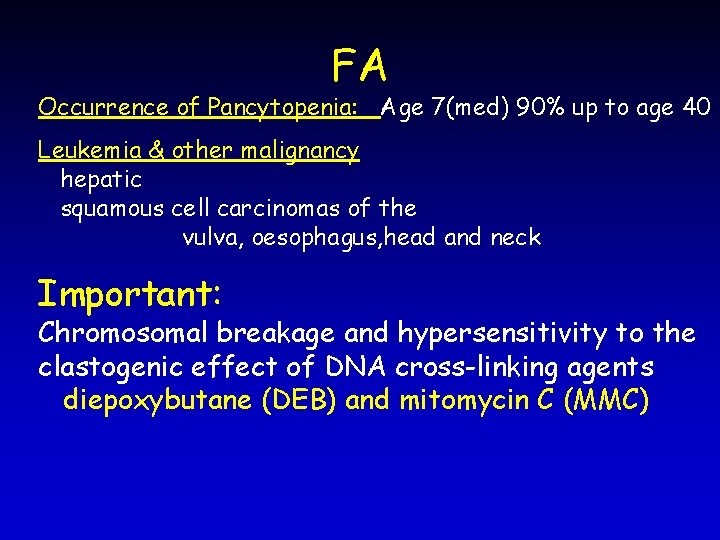
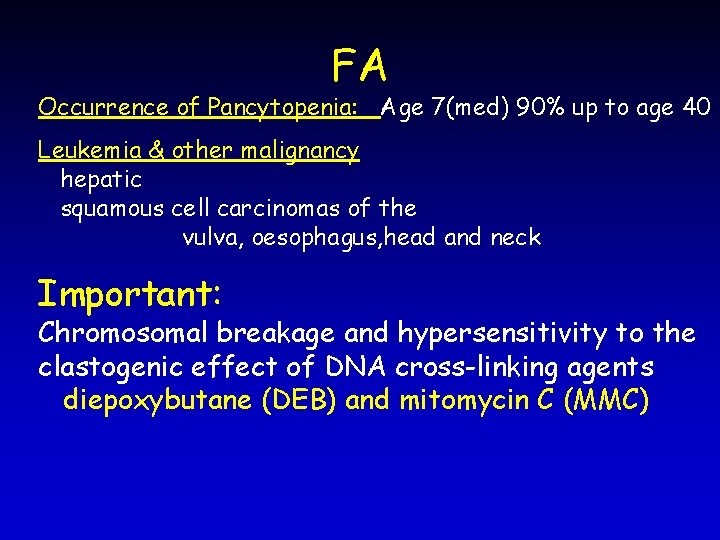
FA Occurrence of Pancytopenia: Age 7(med) 90% up to age 40 Leukemia & other malignancy hepatic squamous cell carcinomas of the vulva, oesophagus, head and neck Important: Chromosomal breakage and hypersensitivity to the clastogenic effect of DNA cross-linking agents diepoxybutane (DEB) and mitomycin C (MMC)
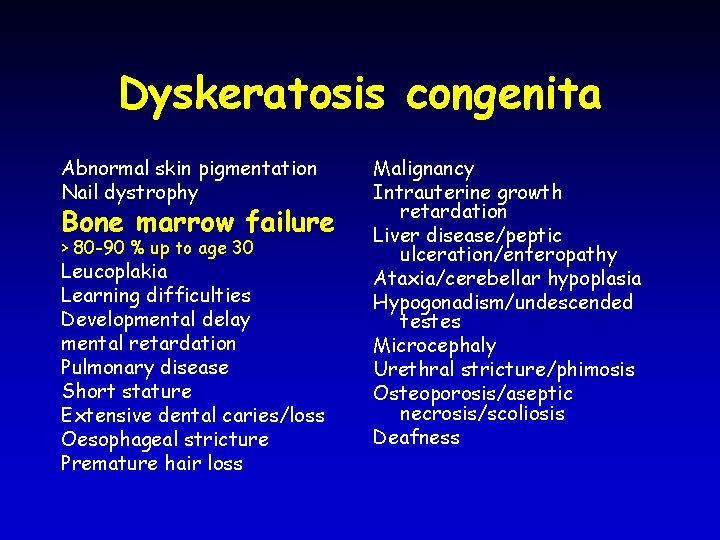
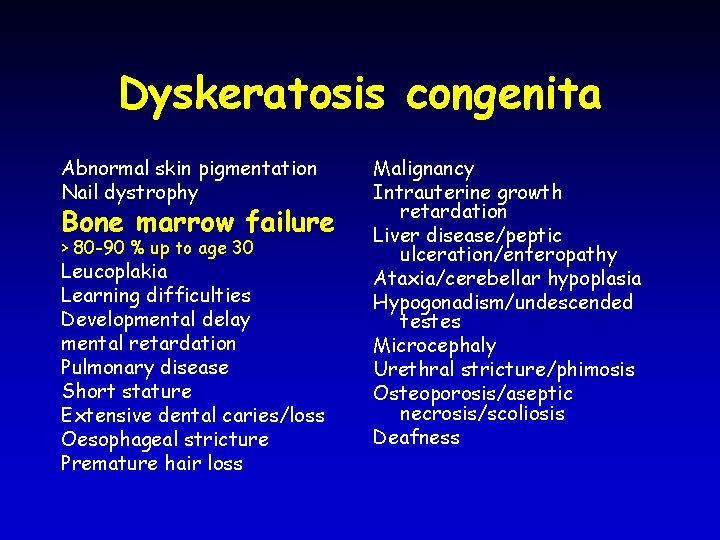
Dyskeratosis congenita Abnormal skin pigmentation Nail dystrophy Bone marrow failure > 80 -90 % up to age 30 Leucoplakia Learning difficulties Developmental delay mental retardation Pulmonary disease Short stature Extensive dental caries/loss Oesophageal stricture Premature hair loss Malignancy Intrauterine growth retardation Liver disease/peptic ulceration/enteropathy Ataxia/cerebellar hypoplasia Hypogonadism/undescended testes Microcephaly Urethral stricture/phimosis Osteoporosis/aseptic necrosis/scoliosis Deafness
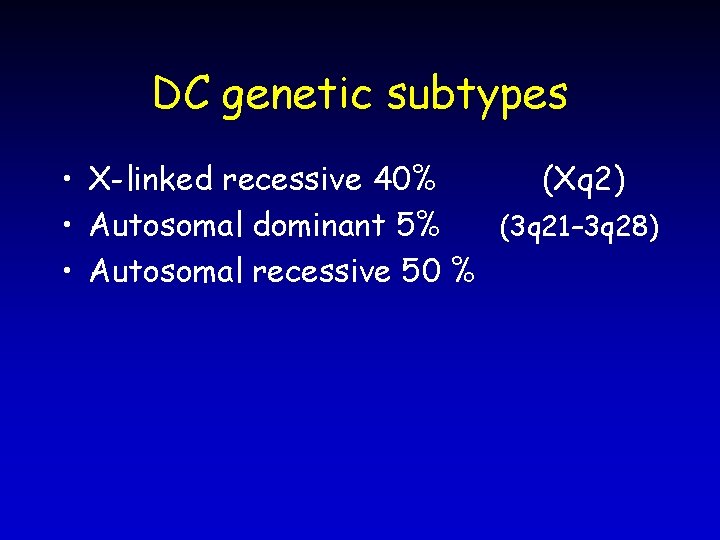
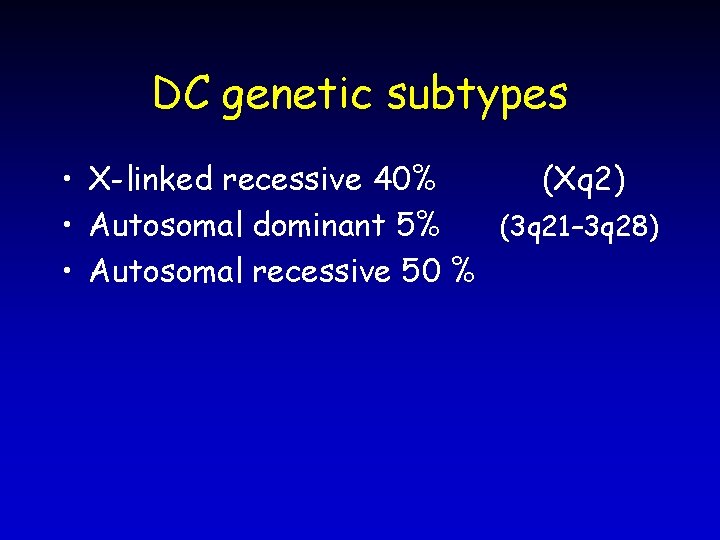
DC genetic subtypes • X-linked recessive 40% (Xq 2) • Autosomal dominant 5% (3 q 21– 3 q 28) • Autosomal recessive 50 %
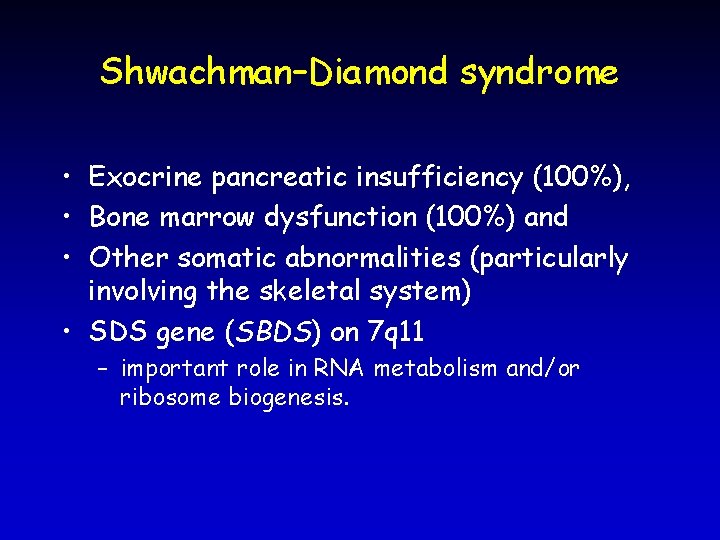
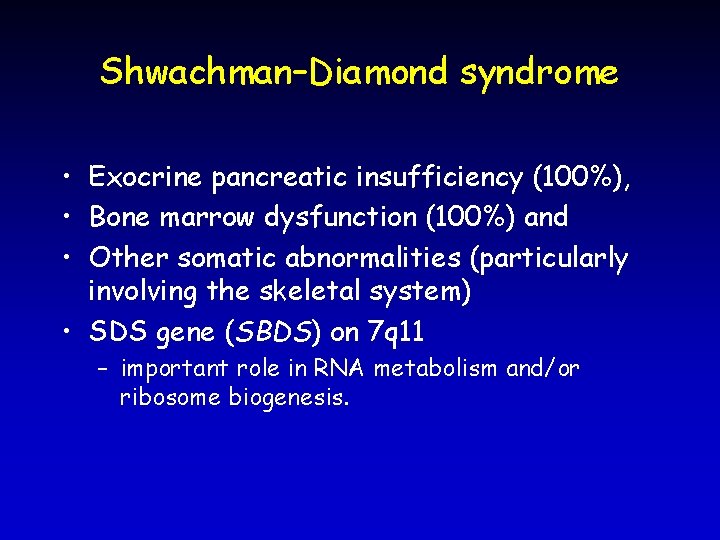
Shwachman–Diamond syndrome • Exocrine pancreatic insufficiency (100%), • Bone marrow dysfunction (100%) and • Other somatic abnormalities (particularly involving the skeletal system) • SDS gene (SBDS) on 7 q 11 – important role in RNA metabolism and/or ribosome biogenesis.
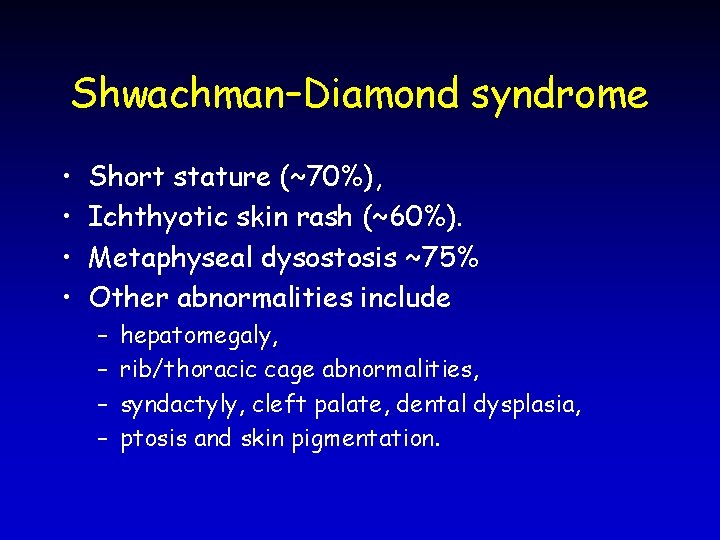
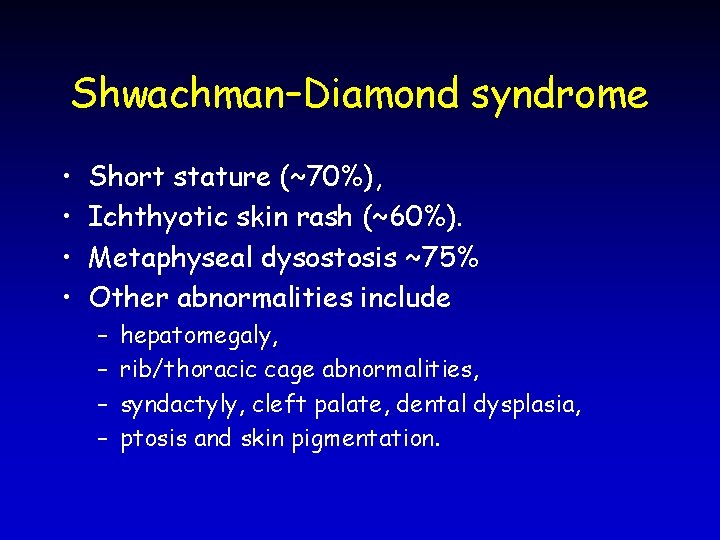
Shwachman–Diamond syndrome • • Short stature (~70%), Ichthyotic skin rash (~60%). Metaphyseal dysostosis ~75% Other abnormalities include – – hepatomegaly, rib/thoracic cage abnormalities, syndactyly, cleft palate, dental dysplasia, ptosis and skin pigmentation.
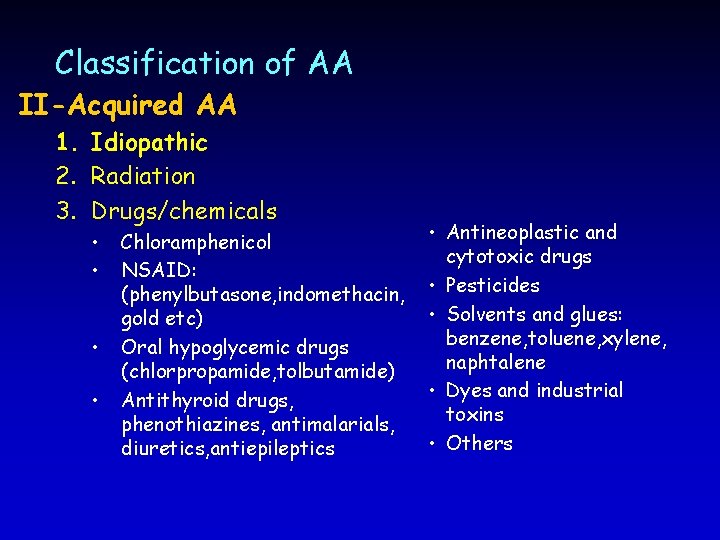
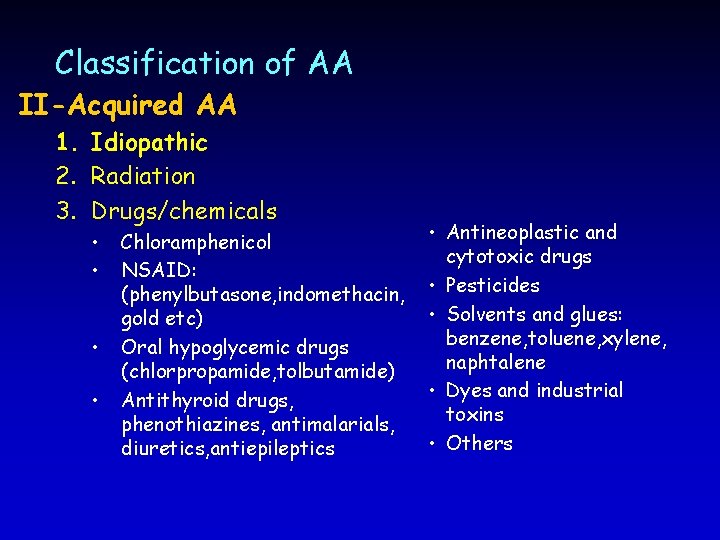
Classification of AA II-Acquired AA 1. Idiopathic 2. Radiation 3. Drugs/chemicals • • Chloramphenicol NSAID: (phenylbutasone, indomethacin, gold etc) Oral hypoglycemic drugs (chlorpropamide, tolbutamide) Antithyroid drugs, phenothiazines, antimalarials, diuretics, antiepileptics • Antineoplastic and cytotoxic drugs • Pesticides • Solvents and glues: benzene, toluene, xylene, naphtalene • Dyes and industrial toxins • Others
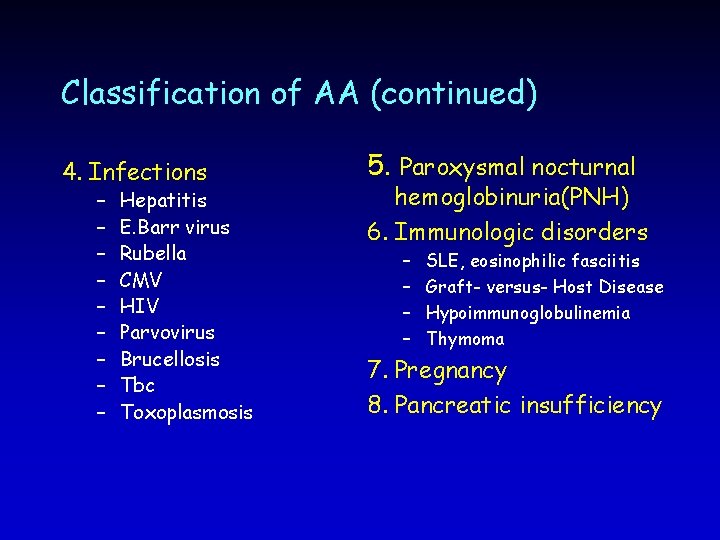
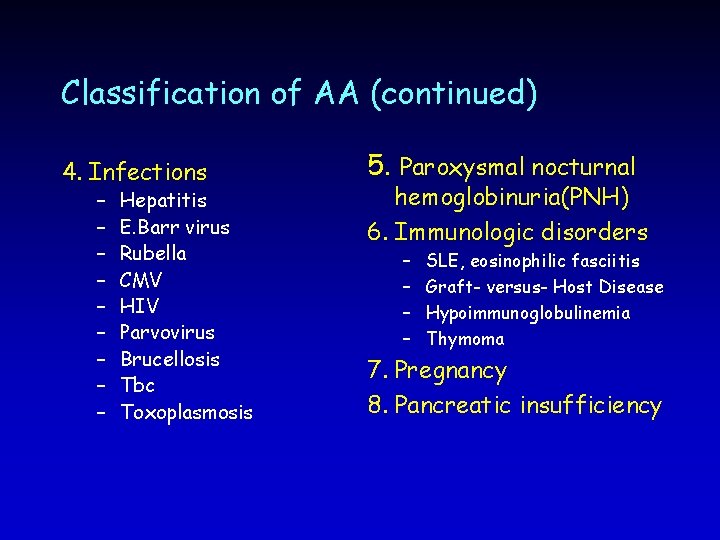
Classification of AA (continued) 4. Infections – – – – – Hepatitis E. Barr virus Rubella CMV HIV Parvovirus Brucellosis Tbc Toxoplasmosis 5. Paroxysmal nocturnal hemoglobinuria(PNH) 6. Immunologic disorders – – SLE, eosinophilic fasciitis Graft- versus- Host Disease Hypoimmunoglobulinemia Thymoma 7. Pregnancy 8. Pancreatic insufficiency
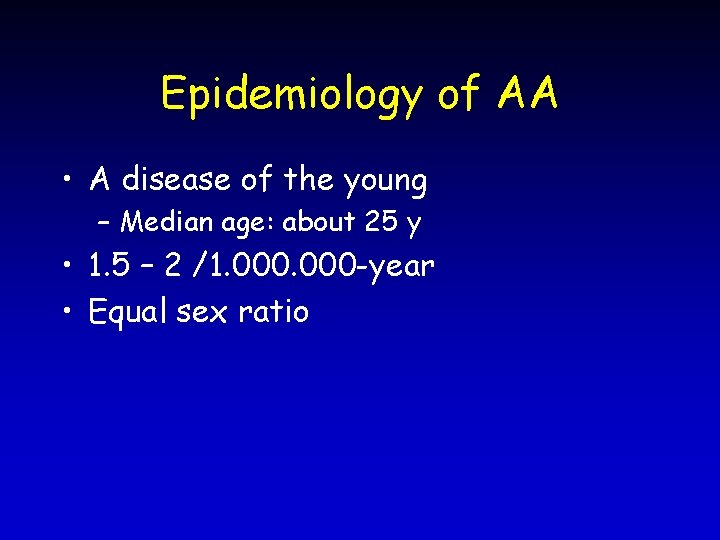
Epidemiology of AA • A disease of the young – Median age: about 25 y • 1. 5 – 2 /1. 000 -year • Equal sex ratio
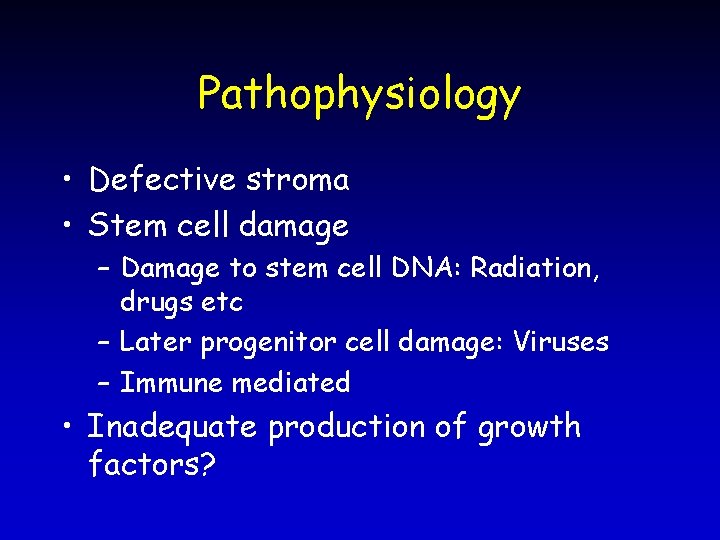
Pathophysiology • Defective stroma • Stem cell damage – Damage to stem cell DNA: Radiation, drugs etc – Later progenitor cell damage: Viruses – Immune mediated • Inadequate production of growth factors?
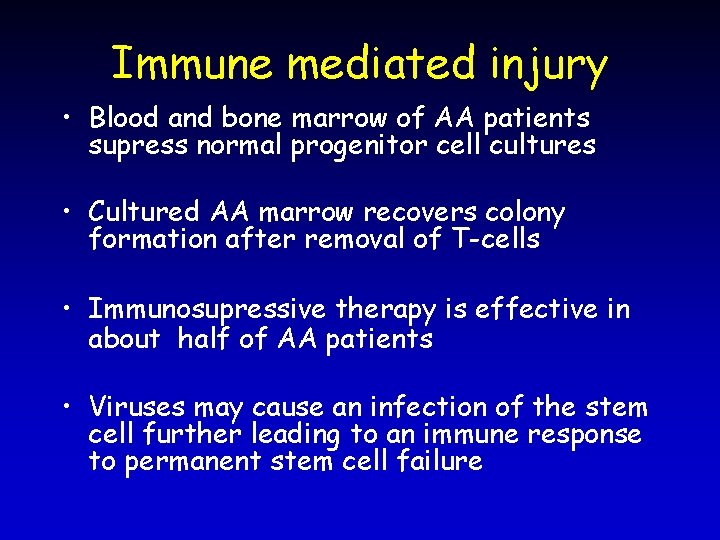
Immune mediated injury • Blood and bone marrow of AA patients supress normal progenitor cell cultures • Cultured AA marrow recovers colony formation after removal of T-cells • Immunosupressive therapy is effective in about half of AA patients • Viruses may cause an infection of the stem cell further leading to an immune response to permanent stem cell failure

Clinical Features of AA • History: – – Bleeding Symptoms of anemia Infections Drugs, chemicals or other etiologically important exposures have to be questioned.
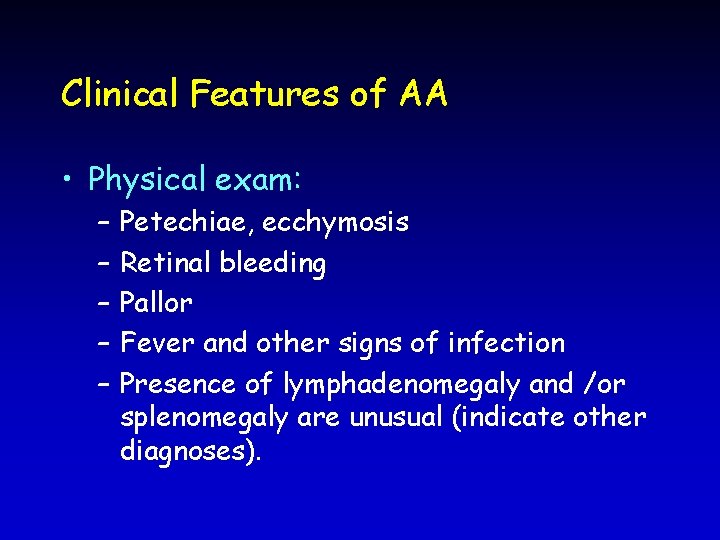
Clinical Features of AA • Physical exam: – – – Petechiae, ecchymosis Retinal bleeding Pallor Fever and other signs of infection Presence of lymphadenomegaly and /or splenomegaly are unusual (indicate other diagnoses).
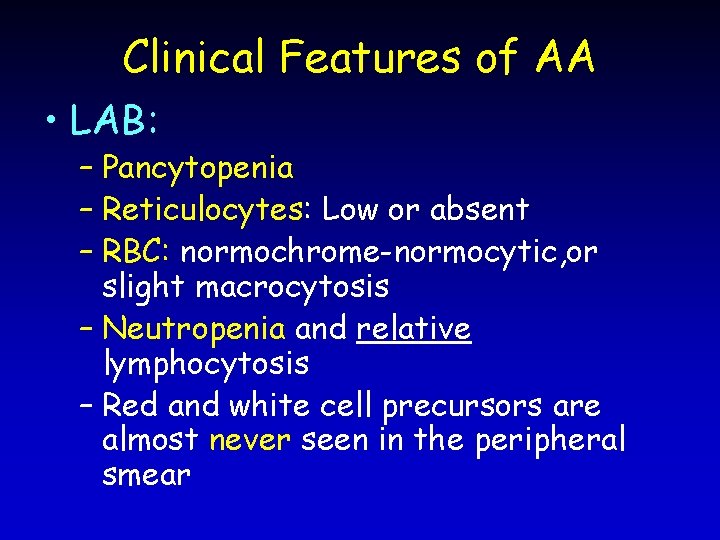
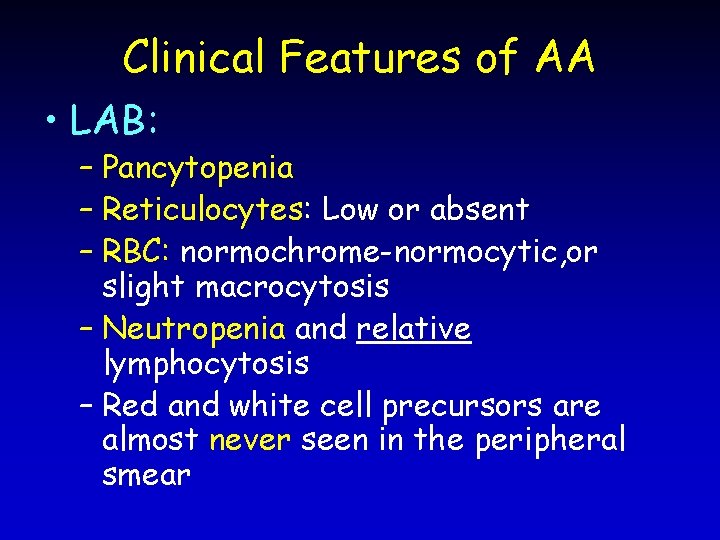
Clinical Features of AA • LAB: – Pancytopenia – Reticulocytes: Low or absent – RBC: normochrome-normocytic, or slight macrocytosis – Neutropenia and relative lymphocytosis – Red and white cell precursors are almost never seen in the peripheral smear
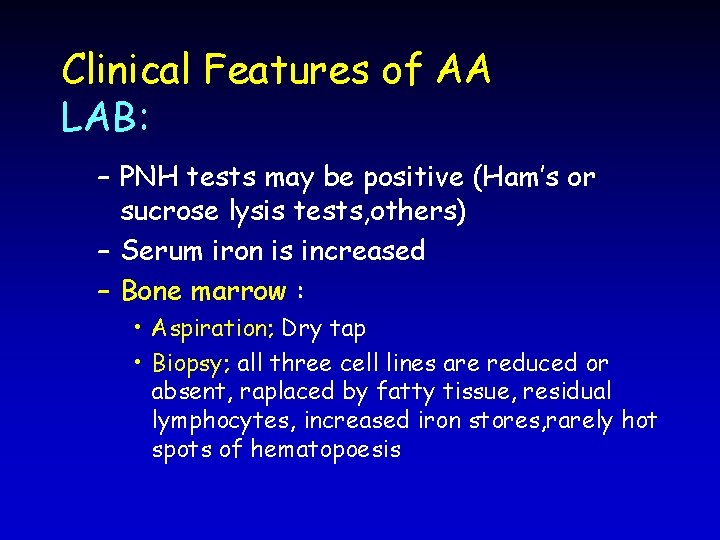
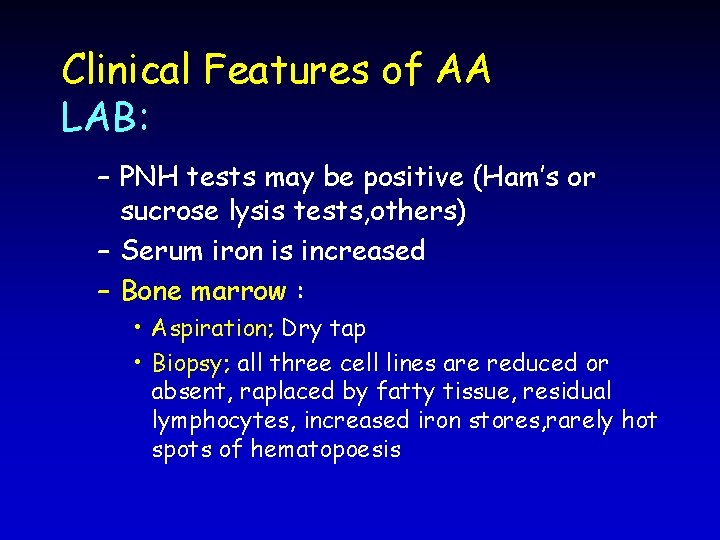
Clinical Features of AA LAB: – PNH tests may be positive (Ham’s or sucrose lysis tests, others) – Serum iron is increased – Bone marrow : • Aspiration; Dry tap • Biopsy; all three cell lines are reduced or absent, raplaced by fatty tissue, residual lymphocytes, increased iron stores, rarely hot spots of hematopoesis

Course and prognosis of AA • • • Definition of severe aplastic anaemia: 1 -hypocellular bone marrow 2 -neutrophils <500/mm 3 3 -platelets<20. 000/mm 3 4 -reticulocytes<20. 000/mm 3 (<%1) Survival in severe disease is about 1 year if it is treated with transfusions only. Very severe AA: Severe AA criteria + Neutrophils: < 200/mm 3
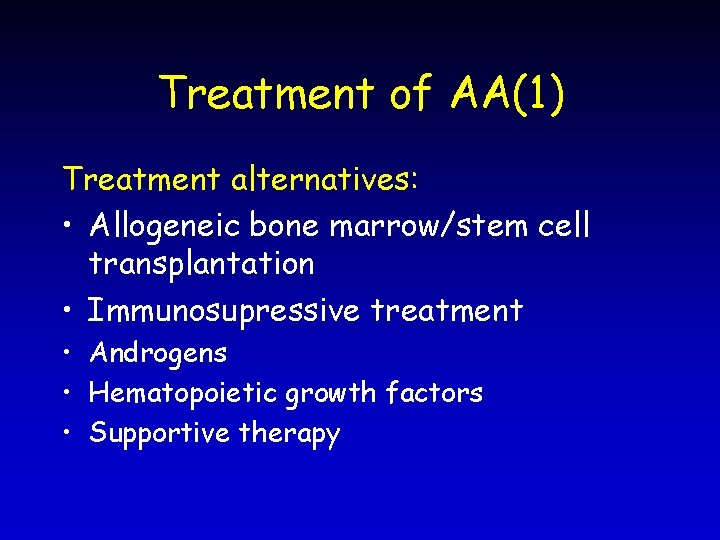
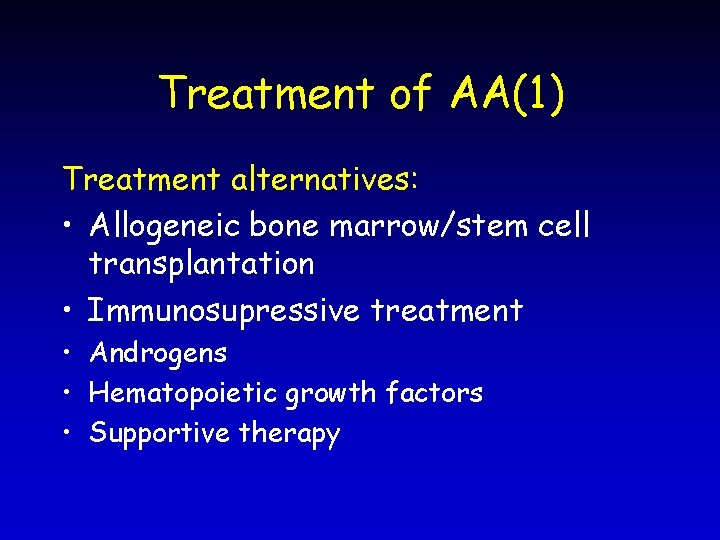
Treatment of AA(1) Treatment alternatives: • Allogeneic bone marrow/stem cell transplantation • Immunosupressive treatment • Androgens • Hematopoietic growth factors • Supportive therapy
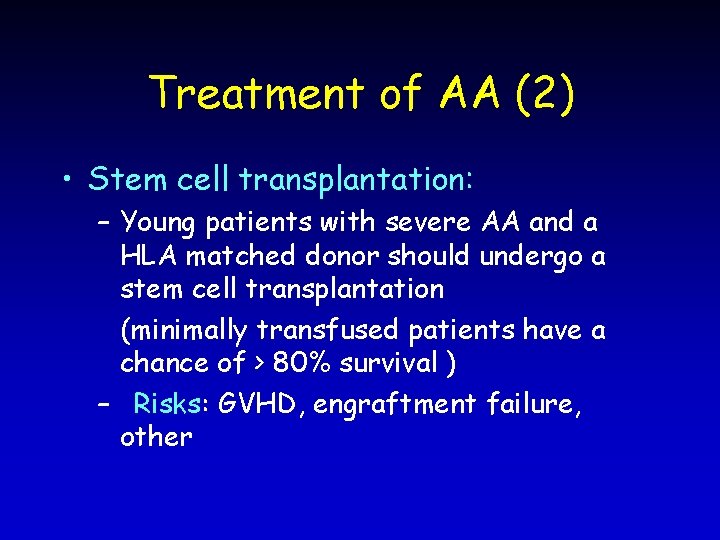
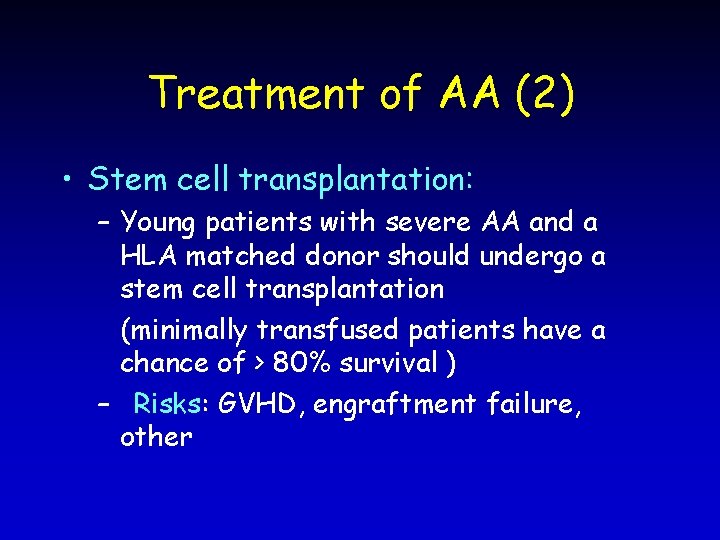
Treatment of AA (2) • Stem cell transplantation: – Young patients with severe AA and a HLA matched donor should undergo a stem cell transplantation (minimally transfused patients have a chance of > 80% survival ) – Risks: GVHD, engraftment failure, other
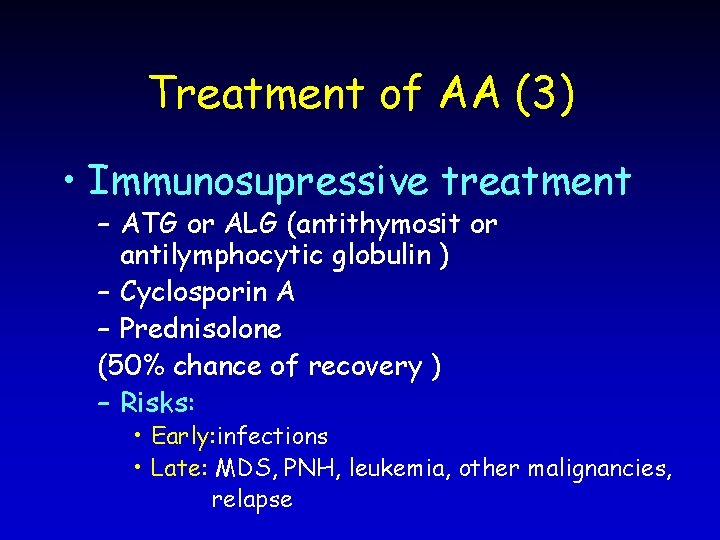
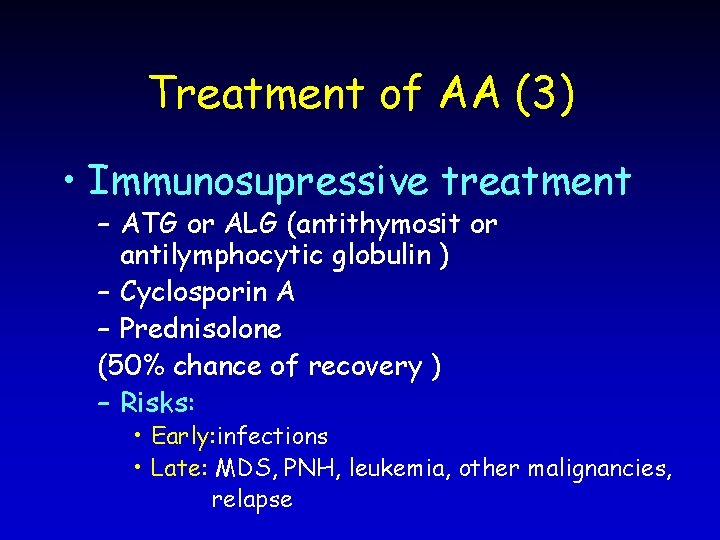
Treatment of AA (3) • Immunosupressive treatment – ATG or ALG (antithymosit or antilymphocytic globulin ) – Cyclosporin A – Prednisolone (50% chance of recovery ) – Risks: • Early: infections • Late: MDS, PNH, leukemia, other malignancies, relapse
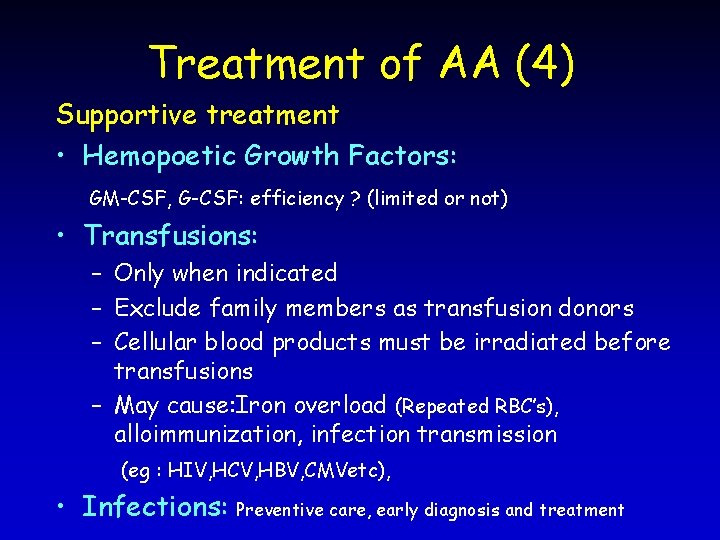
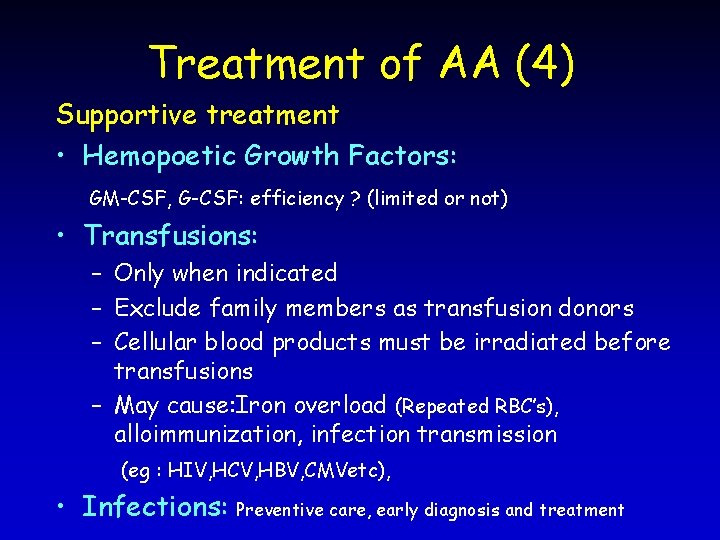
Treatment of AA (4) Supportive treatment • Hemopoetic Growth Factors: GM-CSF, G-CSF: efficiency ? (limited or not) • Transfusions: – Only when indicated – Exclude family members as transfusion donors – Cellular blood products must be irradiated before transfusions – May cause: Iron overload (Repeated RBC’s), alloimmunization, infection transmission (eg : HIV, HCV, HBV, CMVetc), • Infections: Preventive care, early diagnosis and treatment
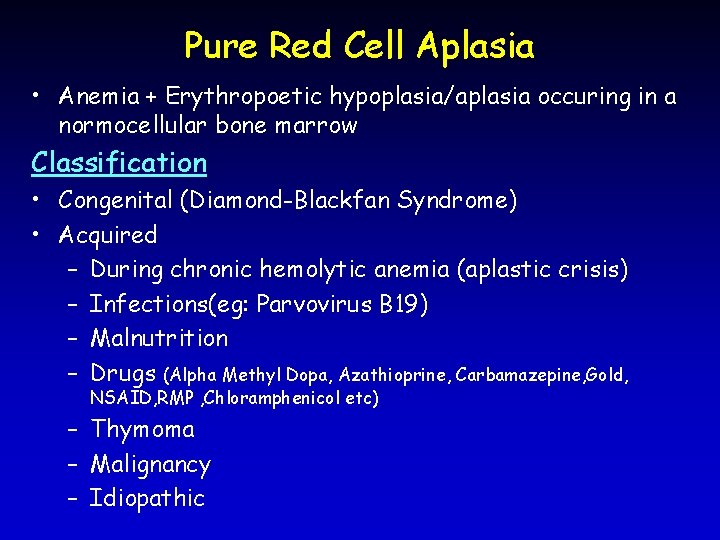
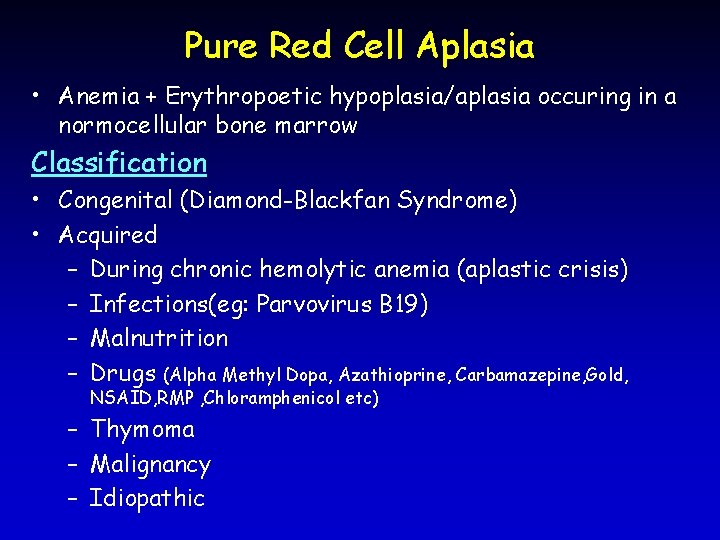
Pure Red Cell Aplasia • Anemia + Erythropoetic hypoplasia/aplasia occuring in a normocellular bone marrow Classification • Congenital (Diamond-Blackfan Syndrome) • Acquired – During chronic hemolytic anemia (aplastic crisis) – Infections(eg: Parvovirus B 19) – Malnutrition – Drugs (Alpha Methyl Dopa, Azathioprine, Carbamazepine, Gold, NSAID, RMP , Chloramphenicol etc) – Thymoma – Malignancy – Idiopathic
 Pansitopenia adalah
Pansitopenia adalah Pathophysiology of aplastic anemia
Pathophysiology of aplastic anemia Thalassemia
Thalassemia Aplastic anemia
Aplastic anemia Pancytopenia causes
Pancytopenia causes Pernicious anemia vs megaloblastic anemia
Pernicious anemia vs megaloblastic anemia Investigation of megaloblastic anemia
Investigation of megaloblastic anemia Lesch nyhan syndrome
Lesch nyhan syndrome Sickle cell anemia lab values
Sickle cell anemia lab values Pancytopenia
Pancytopenia Simultaneous translation definition
Simultaneous translation definition Substitution method simultaneous equations
Substitution method simultaneous equations Simultaneous grinding and drying
Simultaneous grinding and drying Simultaneous heat and mass transfer
Simultaneous heat and mass transfer Example of simultaneous integration
Example of simultaneous integration Persamaan diferensial simultan
Persamaan diferensial simultan Contoh persamaan simultan
Contoh persamaan simultan How to solve non linear simultaneous equations
How to solve non linear simultaneous equations Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Thang điểm glasgow
Thang điểm glasgow Chúa sống lại
Chúa sống lại Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Phép trừ bù
Phép trừ bù độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới