Pancreatitis Gail Lupica Ph D RN CNE Nursing



- Slides: 28
Pancreatitis Gail Lupica Ph. D, RN, CNE Nursing 211
Objectives • Implement and evaluate an appropriate plan of care for your patient with Acute Pancreatitis • Compare and contrast Chronic Pancreatitis to Acute Pancreatitis on the basis of etiology, pathophysiology, clinical manifestations, laboratory data, nursing/collaborative care (including patient teaching points)
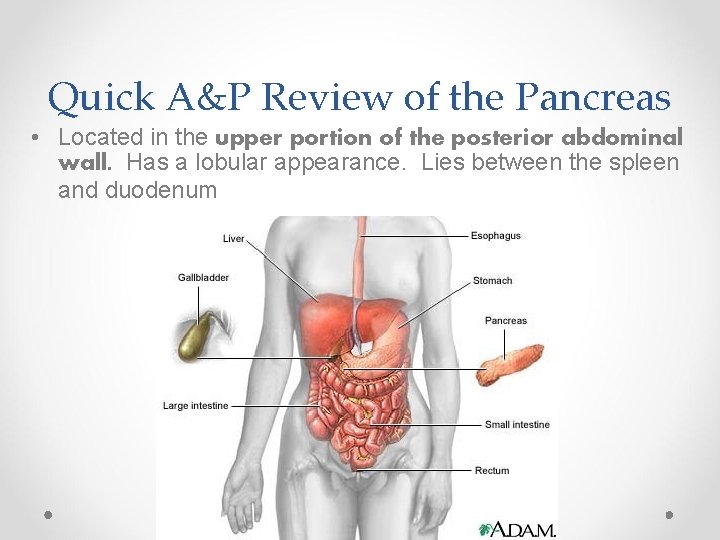
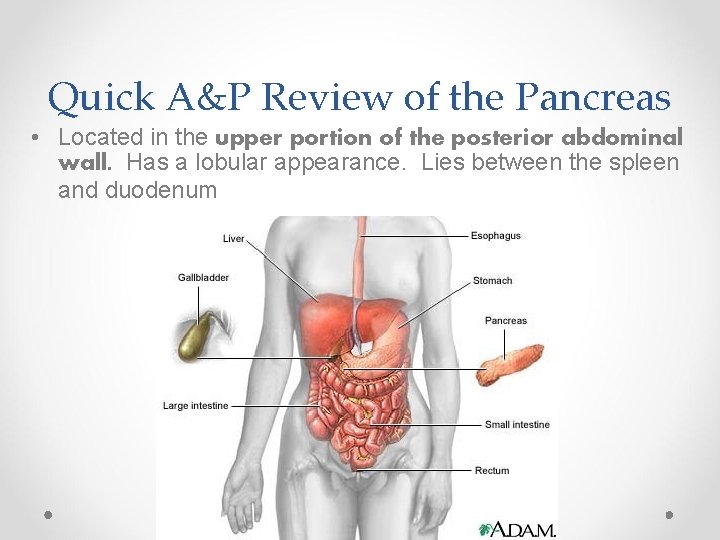
Quick A&P Review of the Pancreas • Located in the upper portion of the posterior abdominal wall. Has a lobular appearance. Lies between the spleen and duodenum
Quick A&P Review • The pancreas secretes digestive enzymes (exocrine function) and the hormones insulin and glucagon (endocrine functions). • Hormones are secreted by the Islet Cells o Digestive Enzymes that it secretes are: o Amylase – breaks down carbohydrates into maltose and dextrins o Lipase – breaks down fats into glycerol and fatty acids o Protease – breaks down peptides into proteins and amino acids
Etiology and Pathophysiology pancreatitis • Primary Etiologic factors: o alcoholism (may cause edema of duodenum and spasm of sphincter of Oddi) o biliary tract disease (gallstones block bile going into the duodenum causing it to back up into the pancreas resulting in cellular injury). • Other causes o Trauma, viral infections (mumps, coxsackievirus), penetrating duodenal ulcers, drugs, metabolic disorders, etc.
Etiology and Pathophysiology • auto-digestion of the pancreas. • Etiological Factors resulting in auto-digestion Activation of pancreatic enzymes in the pancreas rather than Intestine
The Process of Autodigestion • Normally, digestive enzymes are activated in the duodenum. In pancreatitis, the enzymes are activated in the pancreas o This process is not entirely known, but may be the result of the reflux of bile acids into the pancreatic ducts via the sphincter of Oddi
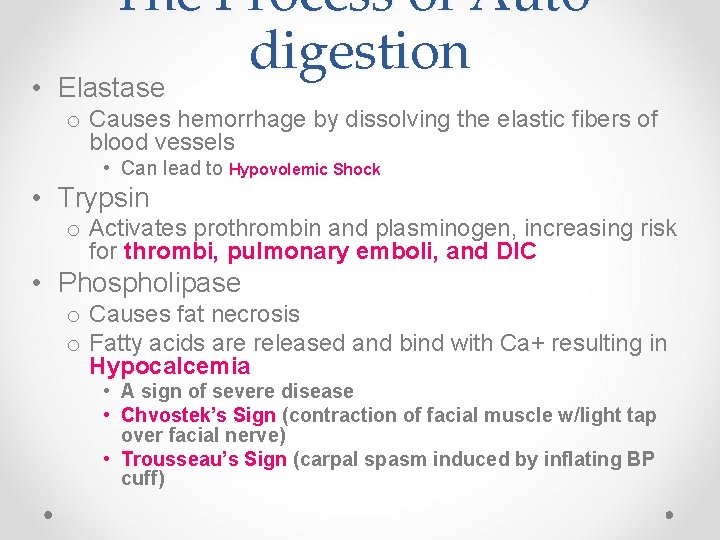
The Process of Autodigestion • Elastase o Causes hemorrhage by dissolving the elastic fibers of blood vessels • Can lead to Hypovolemic Shock • Trypsin o Activates prothrombin and plasminogen, increasing risk for thrombi, pulmonary emboli, and DIC • Phospholipase o Causes fat necrosis o Fatty acids are released and bind with Ca+ resulting in Hypocalcemia • A sign of severe disease • Chvostek’s Sign (contraction of facial muscle w/light tap over facial nerve) • Trousseau’s Sign (carpal spasm induced by inflating BP cuff)
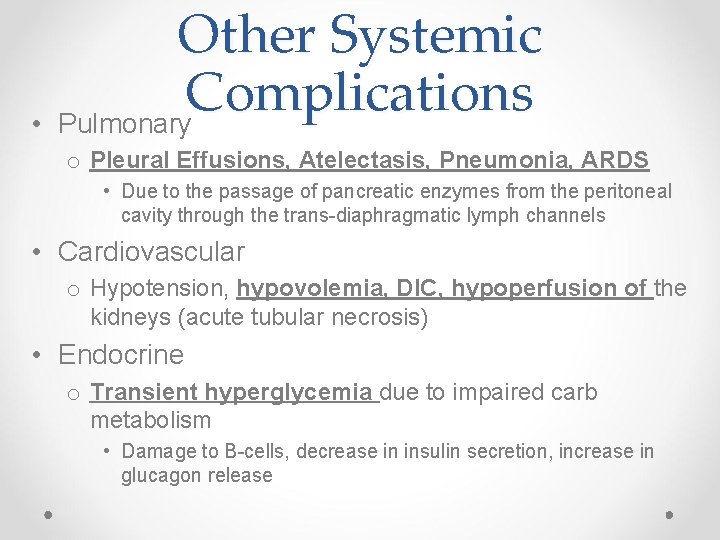
• Other Systemic Complications Pulmonary o Pleural Effusions, Atelectasis, Pneumonia, ARDS • Due to the passage of pancreatic enzymes from the peritoneal cavity through the trans-diaphragmatic lymph channels • Cardiovascular o Hypotension, hypovolemia, DIC, hypoperfusion of the kidneys (acute tubular necrosis) • Endocrine o Transient hyperglycemia due to impaired carb metabolism • Damage to B-cells, decrease in insulin secretion, increase in glucagon release
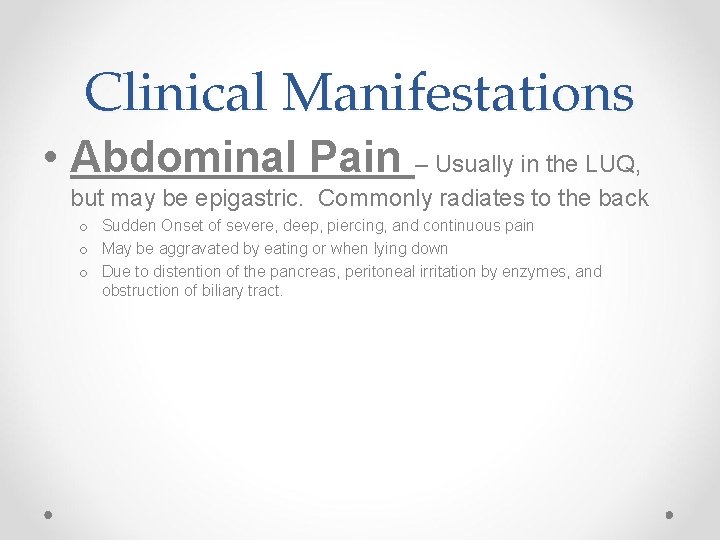
Clinical Manifestations • Abdominal Pain – Usually in the LUQ, but may be epigastric. Commonly radiates to the back o Sudden Onset of severe, deep, piercing, and continuous pain o May be aggravated by eating or when lying down o Due to distention of the pancreas, peritoneal irritation by enzymes, and obstruction of biliary tract.
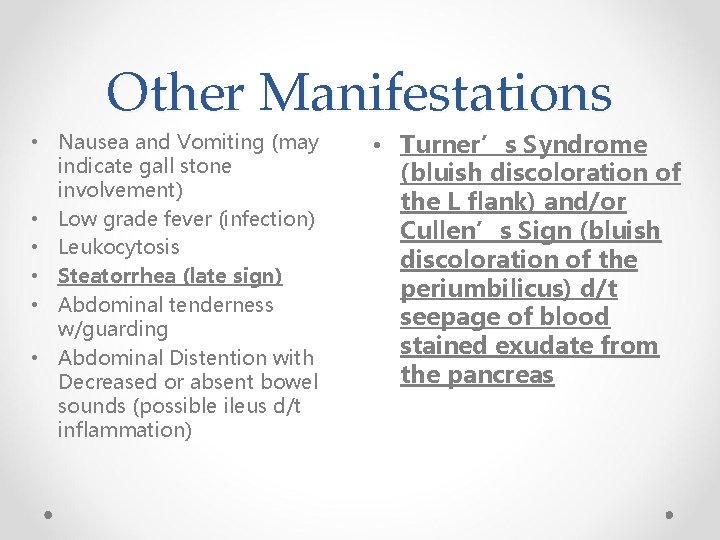
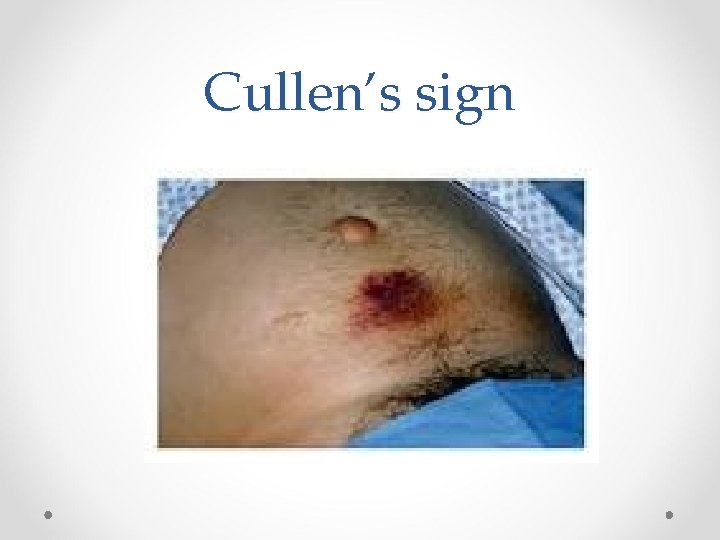
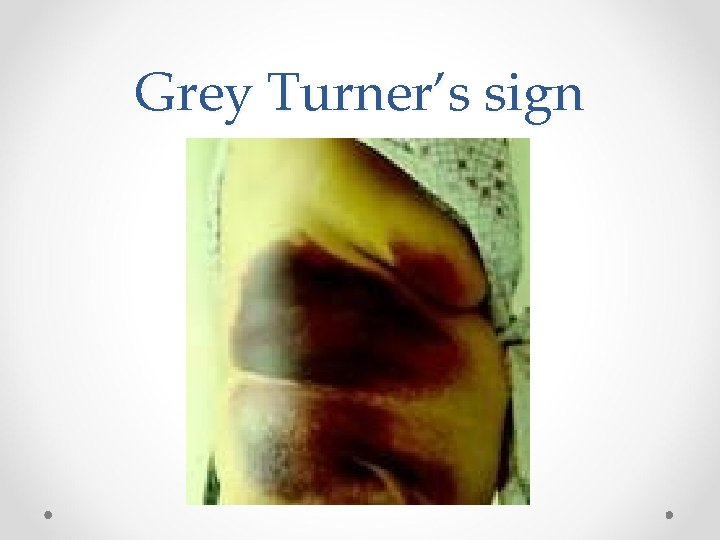
Other Manifestations • Nausea and Vomiting (may indicate gall stone involvement) • Low grade fever (infection) • Leukocytosis • Steatorrhea (late sign) • Abdominal tenderness w/guarding • Abdominal Distention with Decreased or absent bowel sounds (possible ileus d/t inflammation) • Turner’s Syndrome (bluish discoloration of the L flank) and/or Cullen’s Sign (bluish discoloration of the periumbilicus) d/t seepage of blood stained exudate from the pancreas
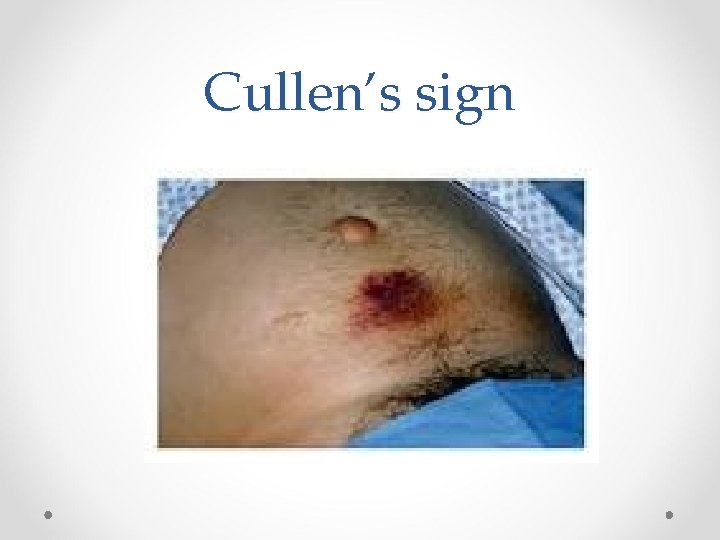
Cullen’s sign

Cullen’s sign

Cullen’s sign
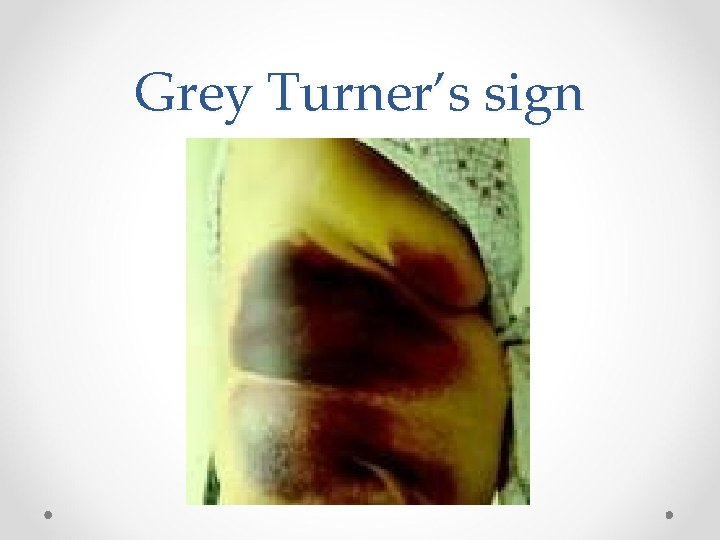
Grey Turner’s sign

Turner’s sign
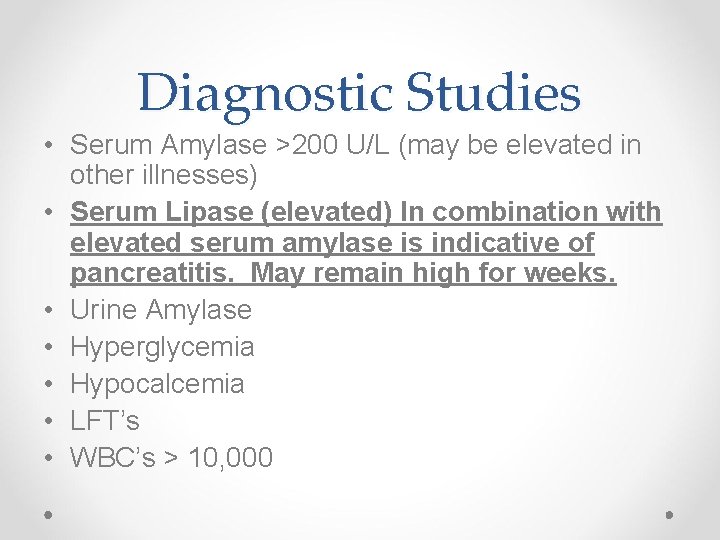
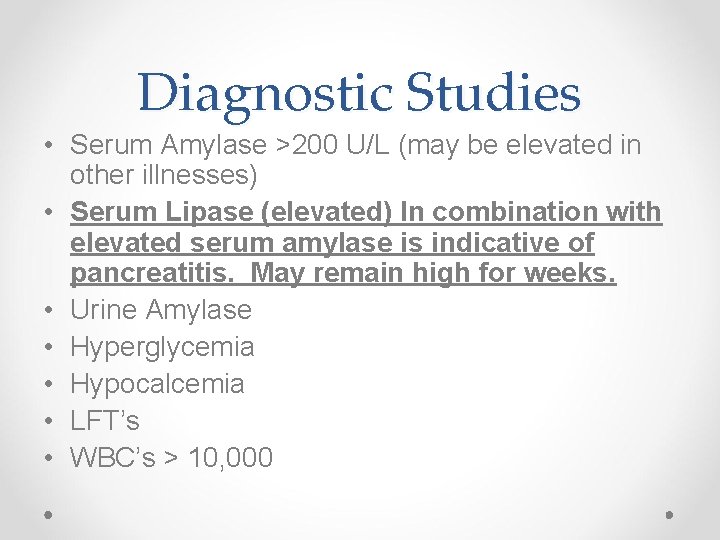
Diagnostic Studies • Serum Amylase >200 U/L (may be elevated in other illnesses) • Serum Lipase (elevated) In combination with elevated serum amylase is indicative of pancreatitis. May remain high for weeks. • Urine Amylase • Hyperglycemia • Hypocalcemia • LFT’s • WBC’s > 10, 000
Diagnostic Studies • Radiology studies o Ultrasound o CT o X-ray (chest and abdomen) o MRI o ERCP (Endoscopic retrograde cholangiopancreatography)
• • • Care Plan Pain Control (Demerol vs Morphine? ? ? ) NCLEX does NOT want you to give MSO 4 Anti-spasmodic, Antacids, Tagamet, Prilosec Albumin/plasma volume expanders (shock) Lactated Ringer’s/Electrolytes Vasoactive drugs for hypotension (to increase SVR, i. e. Dopamine) Reduce/suppress pancreatic enzymes and decrease pancreatic stimulation o NPO o NG to suction (reduce vomiting, gastric distention, prevention of acidic contents into duodenum)
Care Plan • What do you think needs to be done for severe respiratory and circulatory complications?
Care Plan • Surgery o If gallstones present o Abscess o Acute Pseudocyst • May perform percutaneous drainage o Severe Peritonitis
Care Plan Nutritional • Nutritional Therapy o Initially NPO, followed by small, frequent feedings o High Carb (least stimulating to pancreas) o Bland (decreased stimulants such as caffeine or alcohol) o Fat-soluble vitamin supplements o Possible TPN if severe nutritional deficiencies exist
Chronic Pancreatitis • A progress destruction of the pancreas with fibrotic replacement of pancreatic tissue. Strictures and calcifications may also occur. • Two Primary Types o Chronic Obstructive Pancreatitis o Chronic Calcifying Pancreatitis
Chronic Obstructive Pancreatitis • Associated with biliary disease • Often caused by inflammation of the sphincter of Oddi, associated with cholelithiasis. • Cancer can also be a cause of obstructive pancreatitis
Chronic Calcifying Pancreatitis • Inflammation and sclerosis in the pancreas and around the pancreatic duct. Also called alcohol-induced pancreatitis • Ducts are obstructed with protein followed by fibrosis and glandular atrophy. • Pseudocysts and abscesses commonly develop
Clinical Manifestationschronic • Abdominal Pain, usually chronic, but may have acute episodes o Described as heavy, gnawing feeling or cramping • May experience malabsorption with weight loss, constipation, mild jaundice, dark urine, diabetes, steatorrhea.
Diagnostic Studies • May or may not have elevated serum amylase/lipase. • May have increased serum bilirubin and alkaline phosphate • Mild Leukocytosis and elevated ESR • Use the Secretin stimulation test to assess pancreatic function o Secretin stimulates bicarbonate secretion o Decreased bicarbonate secretions indicate chronic pancreatitis • Hyperglycemia • Steatorrhea
Care Plan • Prevention of “attacks” • Diet – low fat, high carb • Pancreatic Enzyme replacement o Pancreatin, Pancrealipase o Bile salts to absorb fat-soluble vitamins • Blood sugar control • Eliminate alcohol