Pancreatic cancer Pathology l Exocrine l Solid Infiltrating





- Slides: 41
Pancreatic cancer
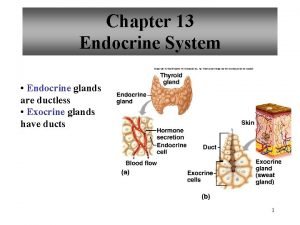
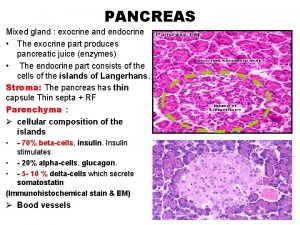
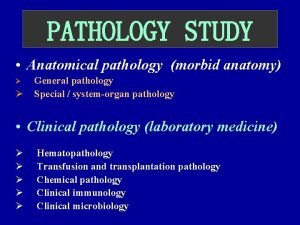
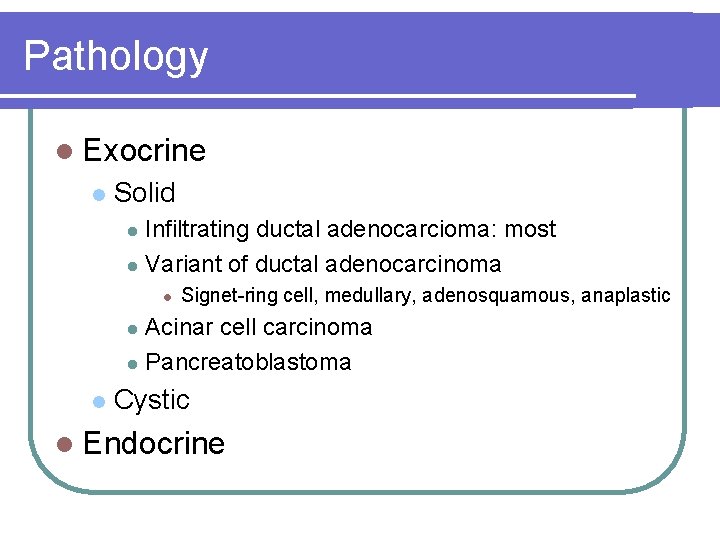
Pathology l Exocrine l Solid Infiltrating ductal adenocarcioma: most l Variant of ductal adenocarcinoma l l Signet-ring cell, medullary, adenosquamous, anaplastic Acinar cell carcinoma l Pancreatoblastoma l l Cystic l Endocrine
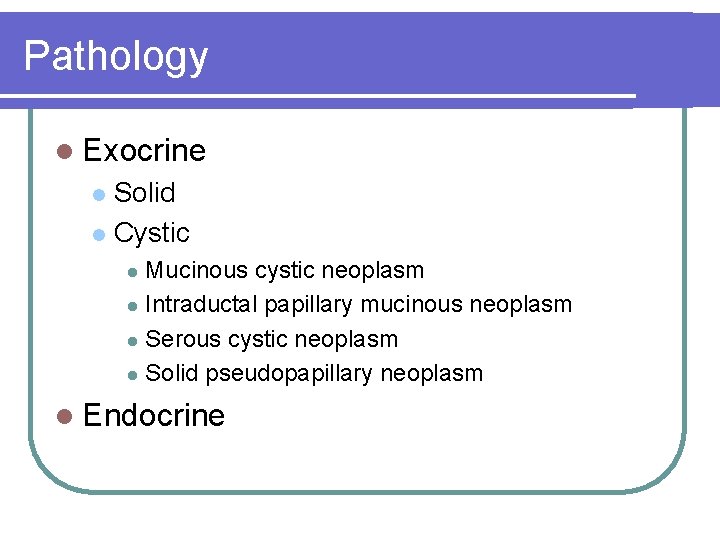
Pathology l Exocrine Solid l Cystic l Mucinous cystic neoplasm l Intraductal papillary mucinous neoplasm l Serous cystic neoplasm l Solid pseudopapillary neoplasm l l Endocrine
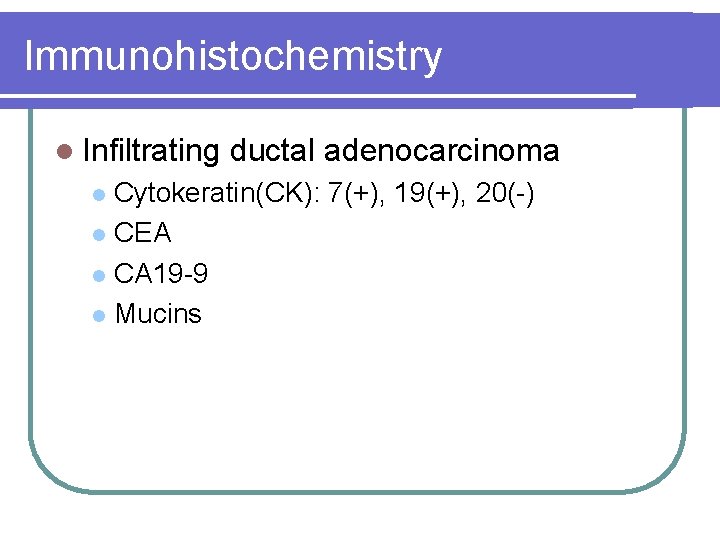
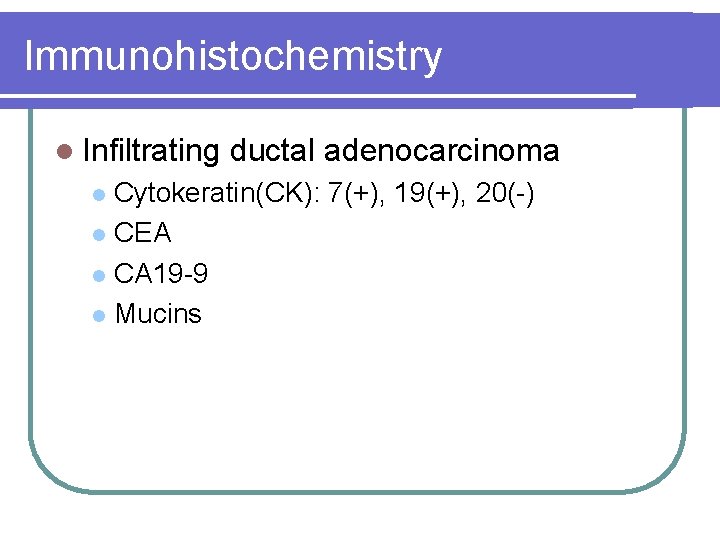
Immunohistochemistry l Infiltrating ductal adenocarcinoma Cytokeratin(CK): 7(+), 19(+), 20(-) l CEA l CA 19 -9 l Mucins l
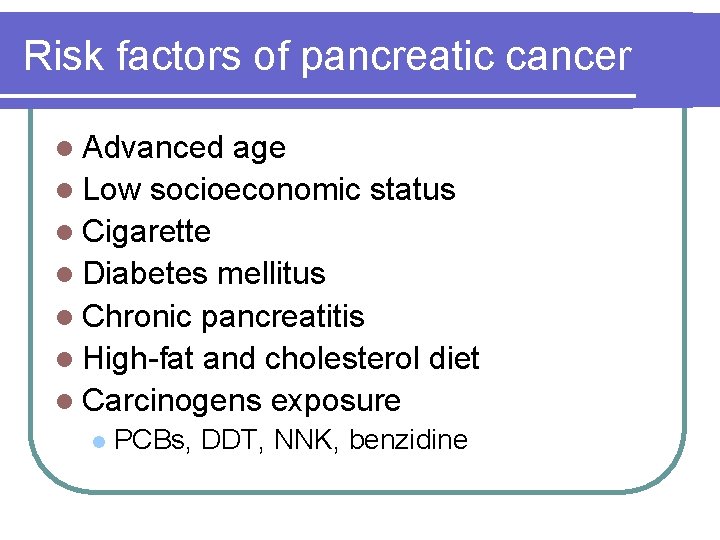
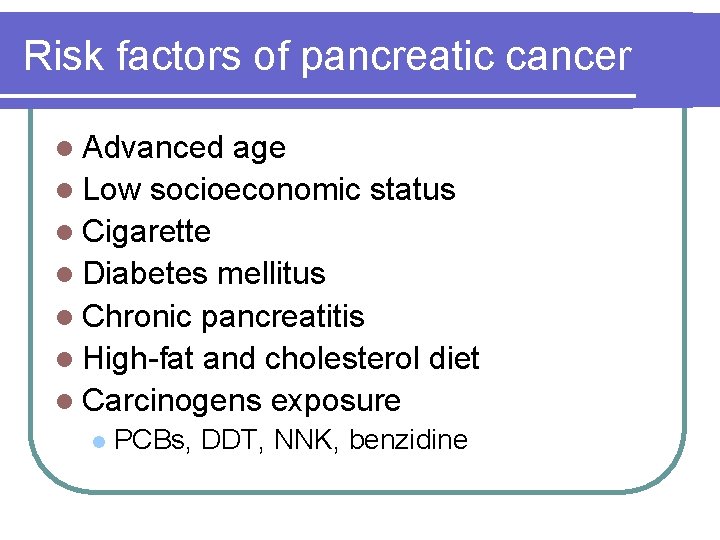
Risk factors of pancreatic cancer l Advanced age l Low socioeconomic status l Cigarette l Diabetes mellitus l Chronic pancreatitis l High-fat and cholesterol diet l Carcinogens exposure l PCBs, DDT, NNK, benzidine
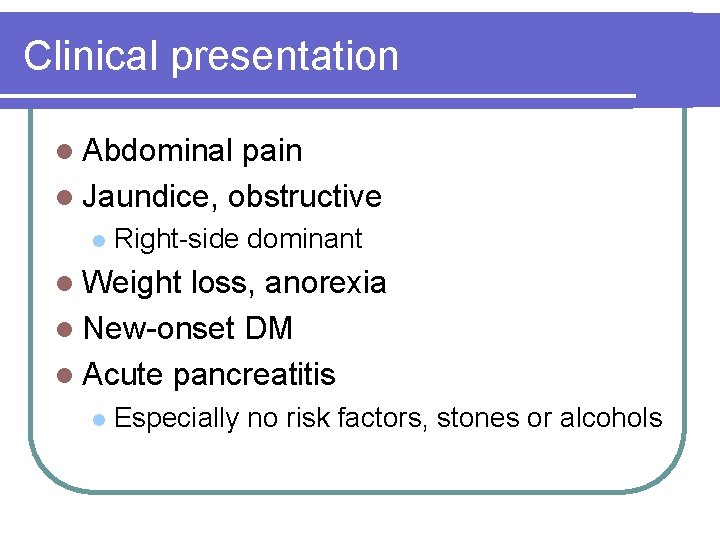
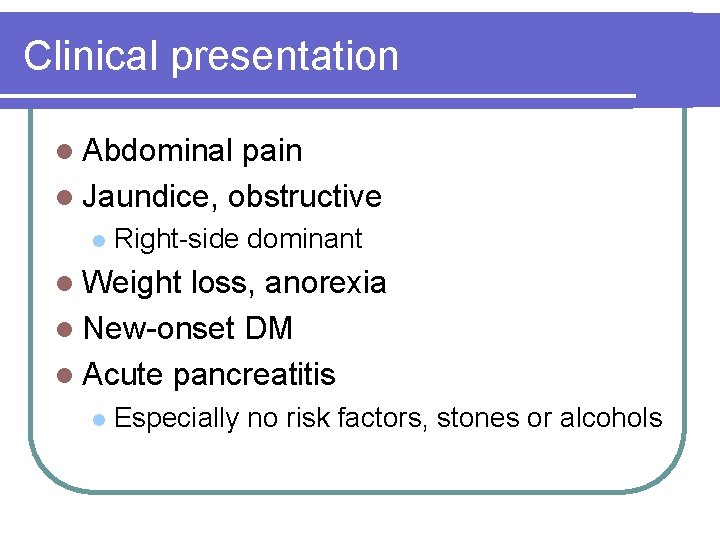
Clinical presentation l Abdominal pain l Jaundice, obstructive l Right-side dominant l Weight loss, anorexia l New-onset DM l Acute pancreatitis l Especially no risk factors, stones or alcohols
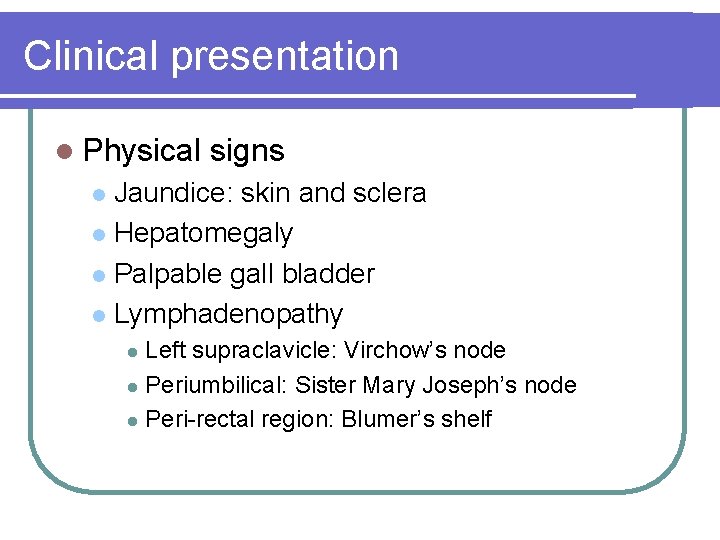
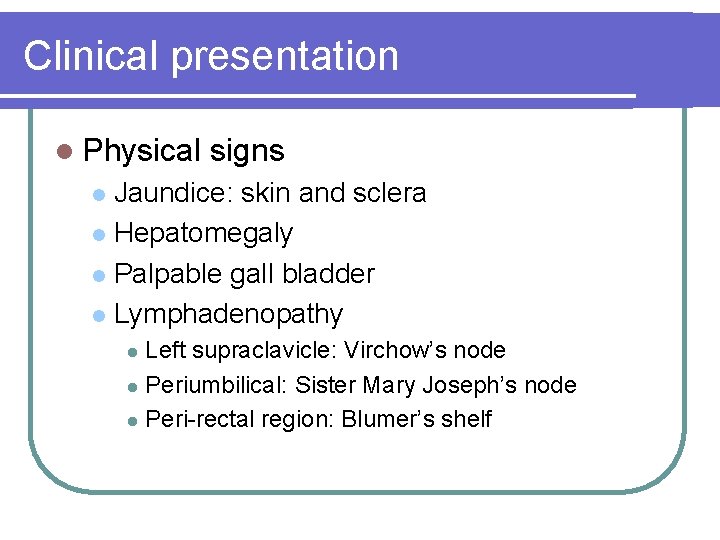
Clinical presentation l Physical signs Jaundice: skin and sclera l Hepatomegaly l Palpable gall bladder l Lymphadenopathy l Left supraclavicle: Virchow’s node l Periumbilical: Sister Mary Joseph’s node l Peri-rectal region: Blumer’s shelf l
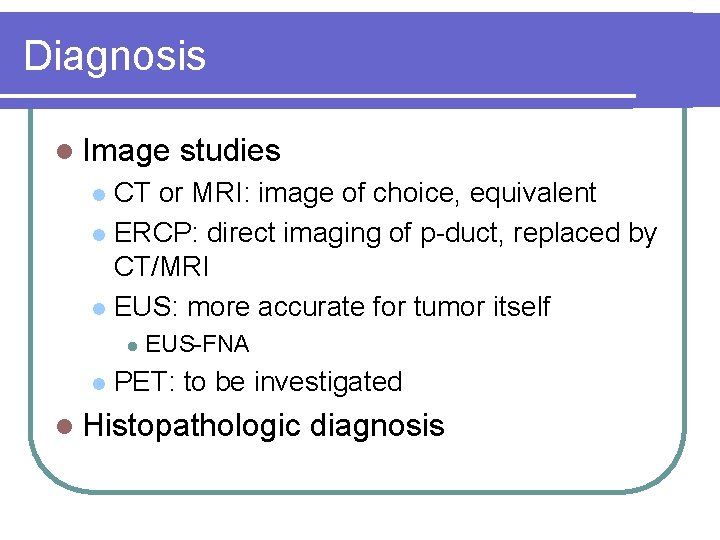
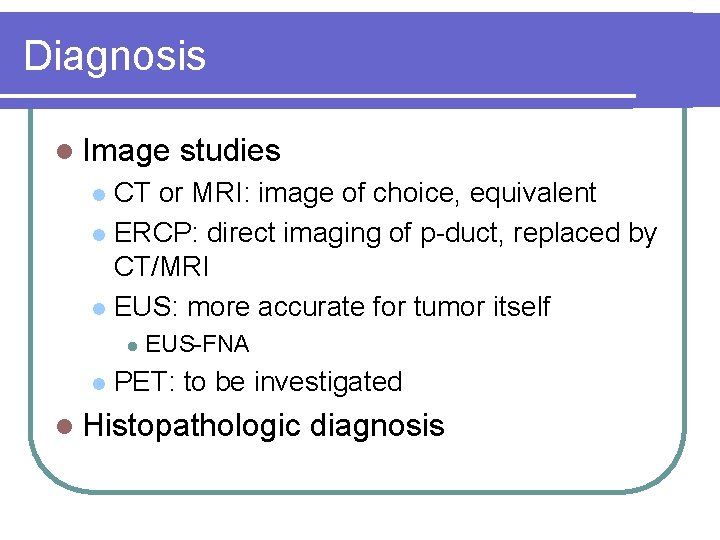
Diagnosis l Image studies CT or MRI: image of choice, equivalent l ERCP: direct imaging of p-duct, replaced by CT/MRI l EUS: more accurate for tumor itself l l l EUS-FNA PET: to be investigated l Histopathologic diagnosis
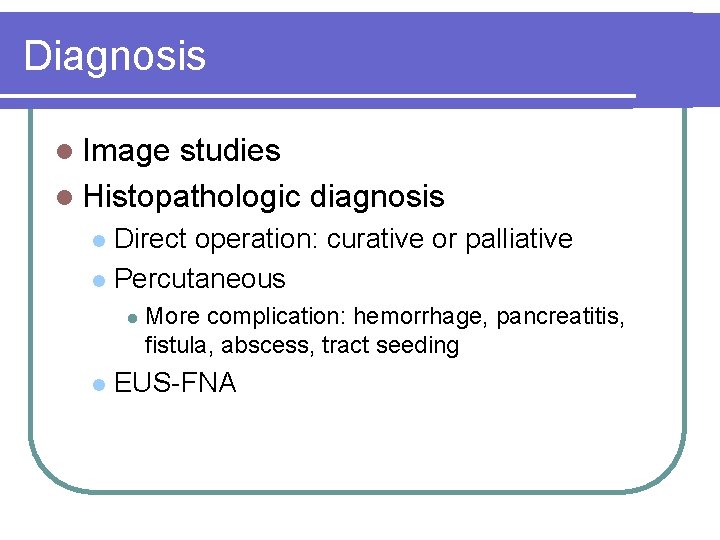
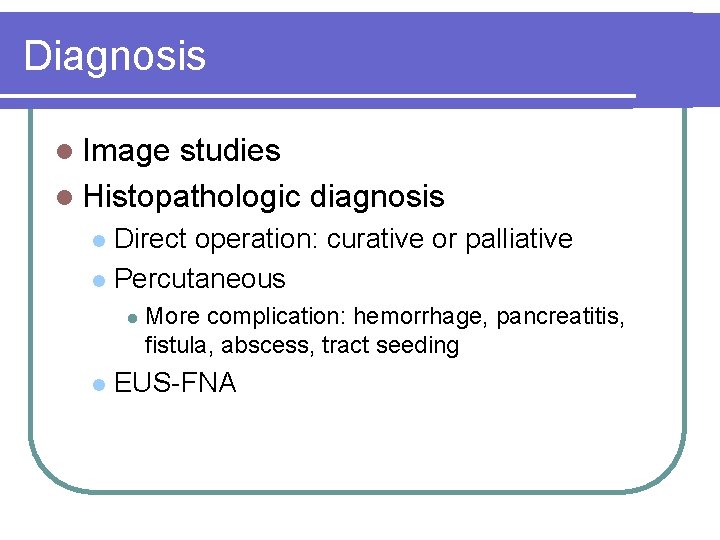
Diagnosis l Image studies l Histopathologic diagnosis Direct operation: curative or palliative l Percutaneous l l l More complication: hemorrhage, pancreatitis, fistula, abscess, tract seeding EUS-FNA
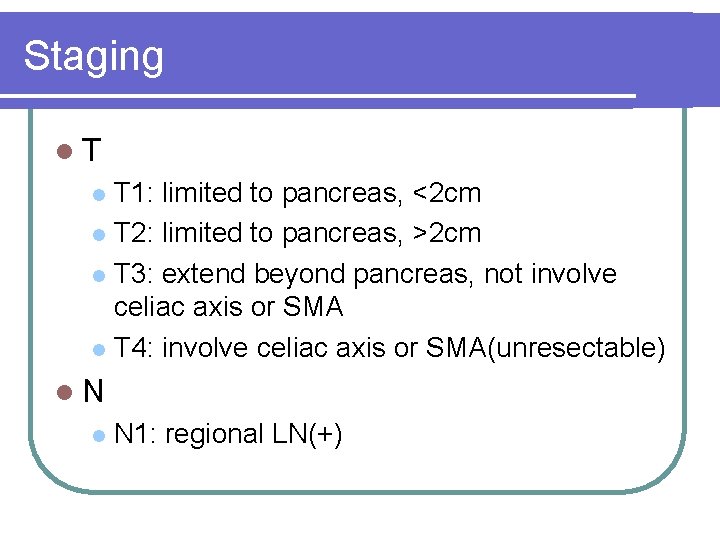
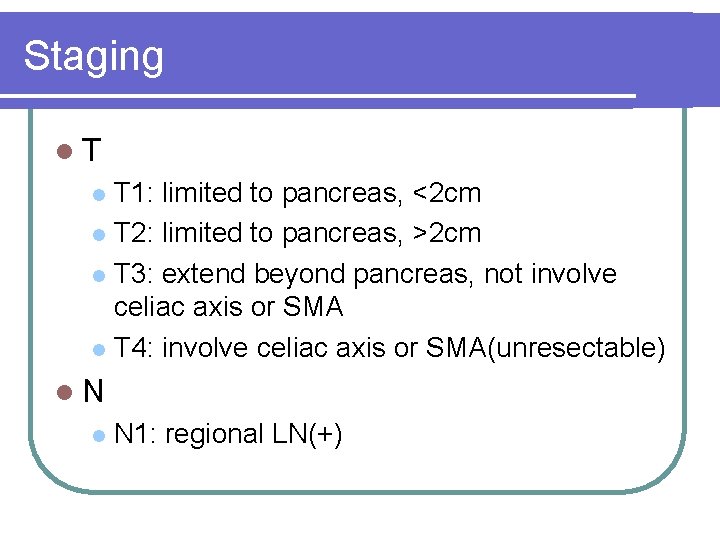
Staging l. T T 1: limited to pancreas, <2 cm l T 2: limited to pancreas, >2 cm l T 3: extend beyond pancreas, not involve celiac axis or SMA l T 4: involve celiac axis or SMA(unresectable) l l. N l N 1: regional LN(+)
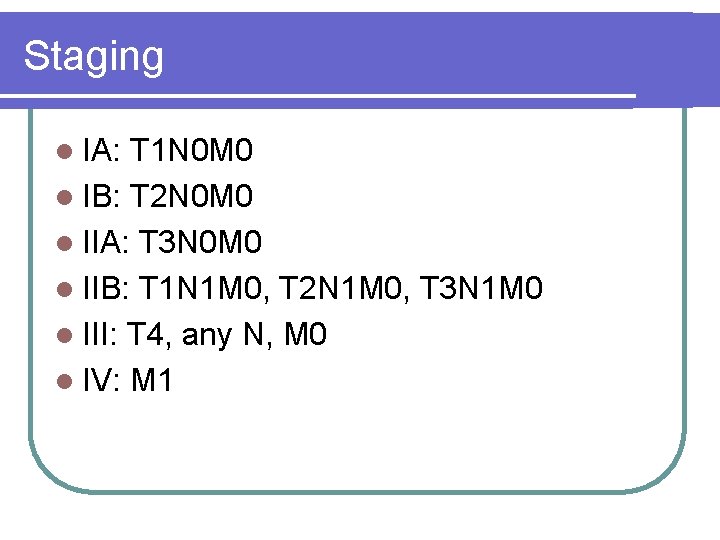
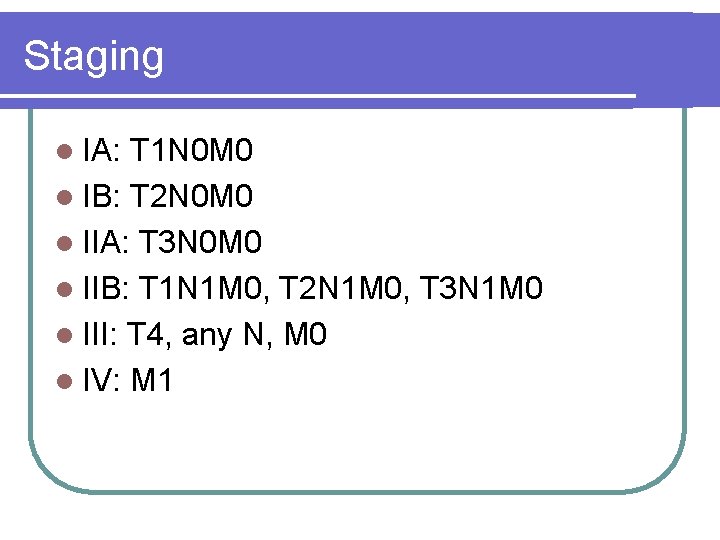
Staging l IA: T 1 N 0 M 0 l IB: T 2 N 0 M 0 l IIA: T 3 N 0 M 0 l IIB: T 1 N 1 M 0, T 2 N 1 M 0, T 3 N 1 M 0 l III: T 4, any N, M 0 l IV: M 1
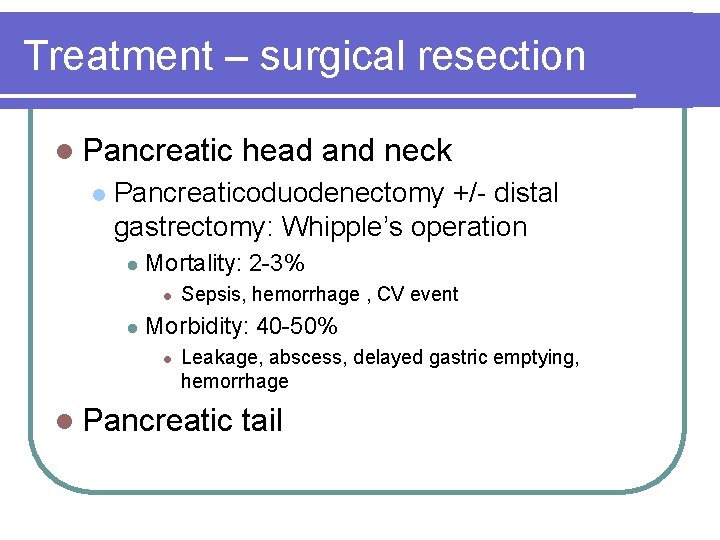
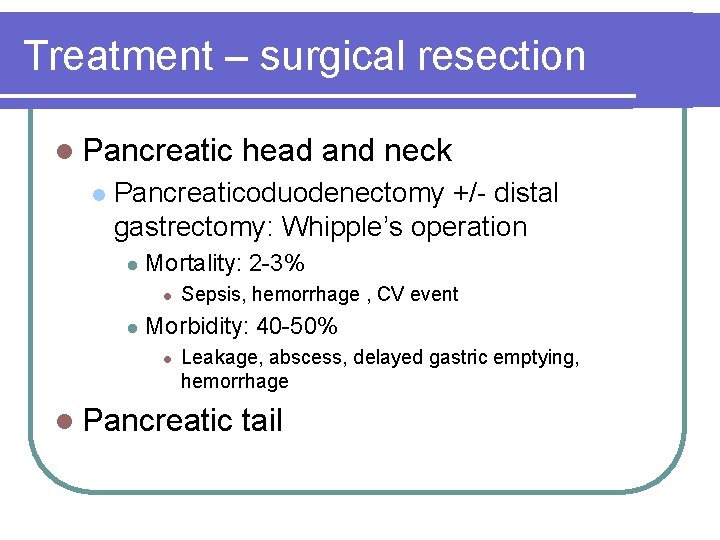
Treatment – surgical resection l Pancreatic l head and neck Pancreaticoduodenectomy +/- distal gastrectomy: Whipple’s operation l Mortality: 2 -3% l l Sepsis, hemorrhage , CV event Morbidity: 40 -50% l Leakage, abscess, delayed gastric emptying, hemorrhage l Pancreatic tail

Treatment – surgical resection l Pancreatic head and neck l Pancreatic tail l No obstructive jaundice in early state l l Tend to be larger, usually metastasis at dx Distal pancreatectomy
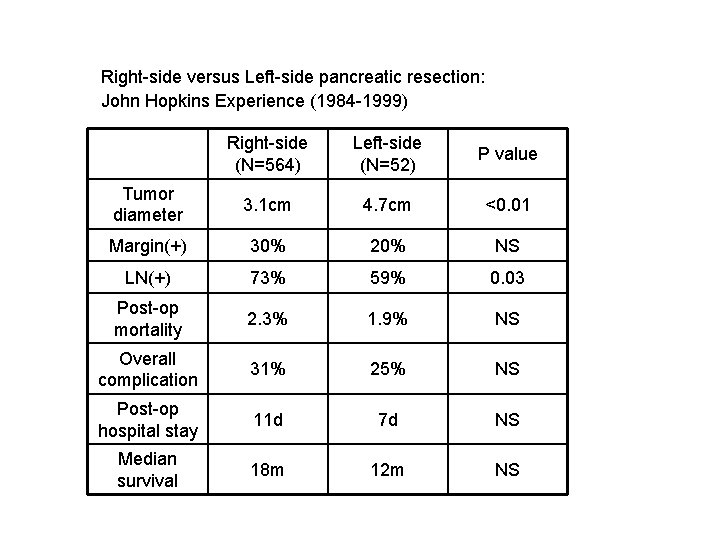
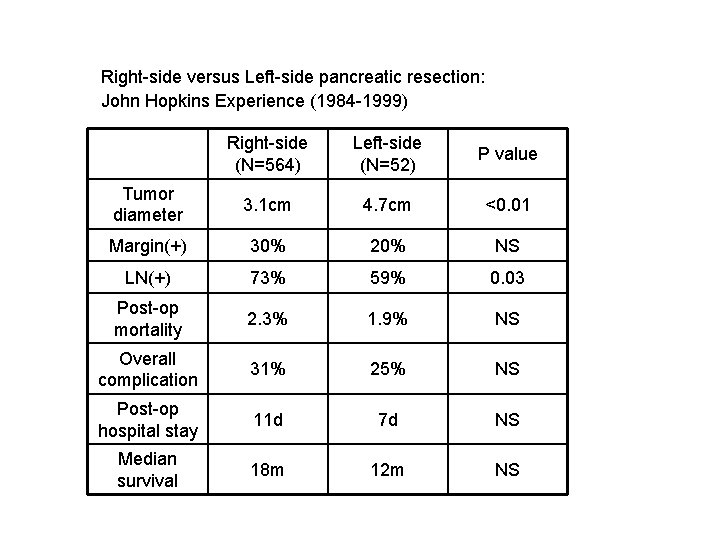
Right-side versus Left-side pancreatic resection: John Hopkins Experience (1984 -1999) Right-side (N=564) Left-side (N=52) P value Tumor diameter 3. 1 cm 4. 7 cm <0. 01 Margin(+) 30% 20% NS LN(+) 73% 59% 0. 03 Post-op mortality 2. 3% 1. 9% NS Overall complication 31% 25% NS Post-op hospital stay 11 d 7 d NS Median survival 18 m 12 m NS
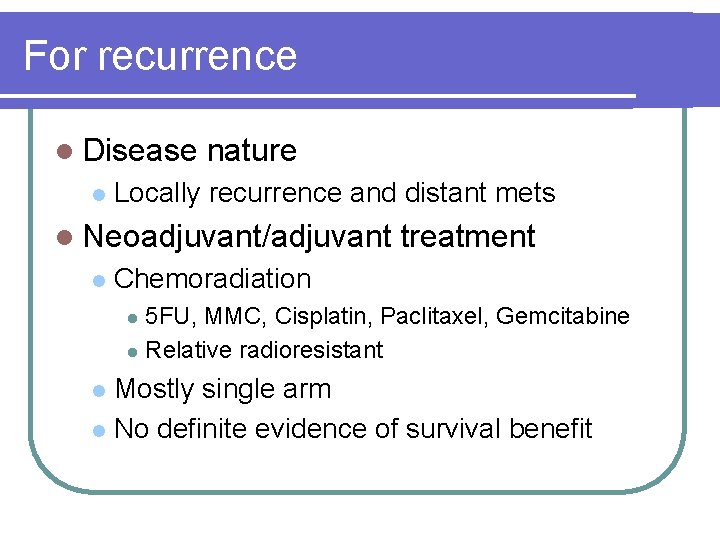
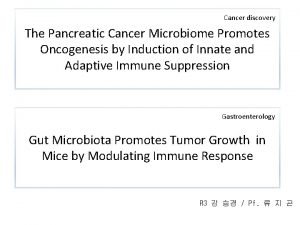
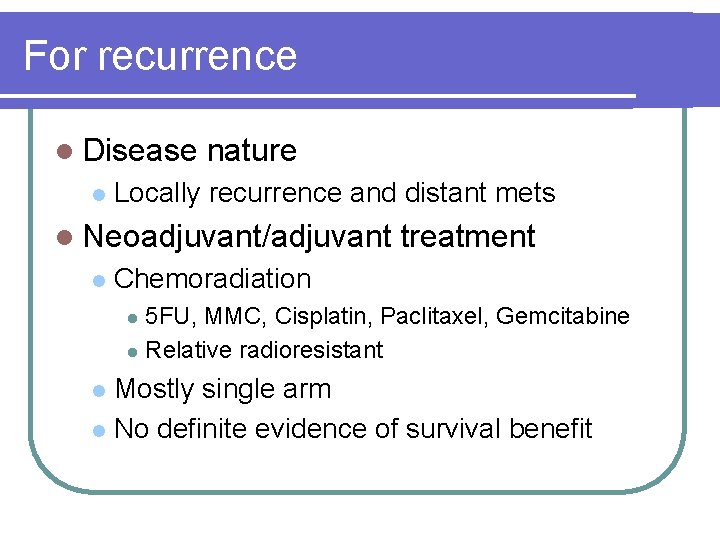
For recurrence l Disease l nature Locally recurrence and distant mets l Neoadjuvant/adjuvant l treatment Chemoradiation 5 FU, MMC, Cisplatin, Paclitaxel, Gemcitabine l Relative radioresistant l Mostly single arm l No definite evidence of survival benefit l
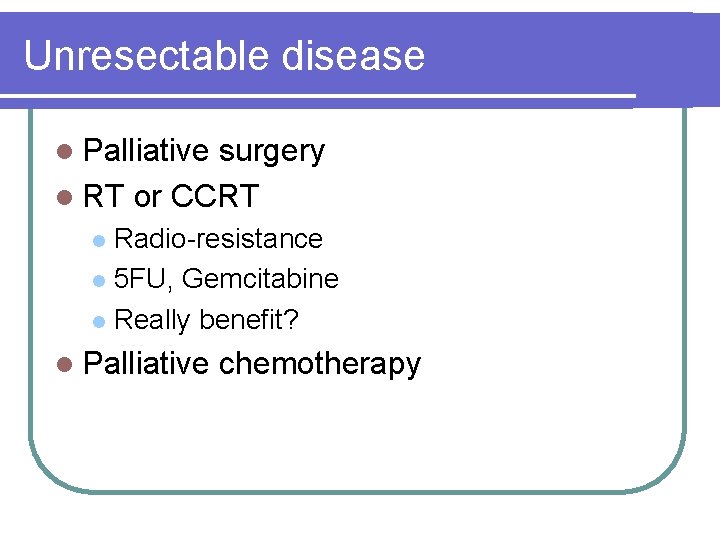
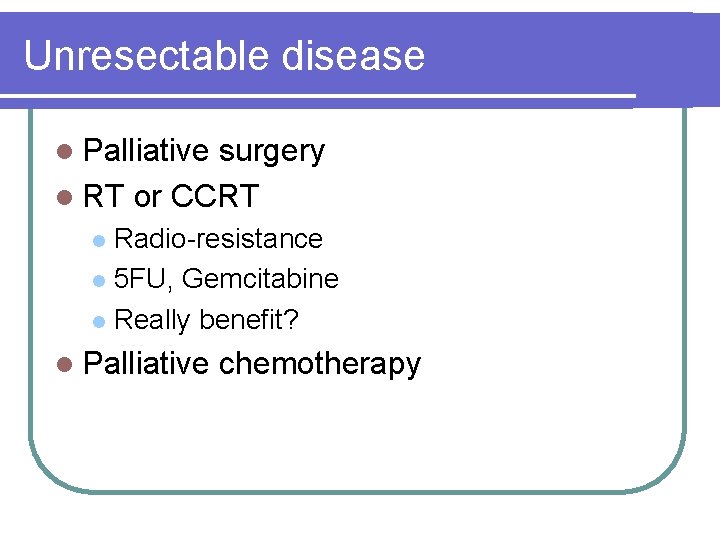
Unresectable disease l Palliative surgery l RT or CCRT Radio-resistance l 5 FU, Gemcitabine l Really benefit? l l Palliative chemotherapy

Palliative surgery l Obstructive jaundice l Duodenal obstruction Hepaticojejunostomy l Choledochoduodenostomy l Cholecystojejunostomy l l Pain l relief Neurolysis
Systemic chemotherapy l Problems Highly resistant to chemotherapy l Usually poor performance l l Pain, N/V, cachexia, weakness Impaired liver function l Usually lack of measurable lesions l l Variation in phase II studies
Chemotherapy – historical l 5 -FU l is cornerstone Combination with Adramycin, mitomycin: FAM l Cyc, MTX, Vincristine, Mitomycin l Epirubicin, cisplatin, carboplatin, Ara-C High response rate in phase II : 40% Not confirmed in phase III l l Combination not better than 5 FU alone
Gemcitabine l Well-tolerated agent l Phase III study, Gemzar vs. 5 -FU Response rate: 5. 4% vs. 0% l Survival: 5. 65 m vs. 4. 41 m (p=0. 0025) l Clinical benefit: 23. 8% vs. 4. 8 l l l Pain, performance status, weight gain Toxicity similar with 5 -FU l Gemcitabine superior to 5 -FU

Gemcitabine-based combination
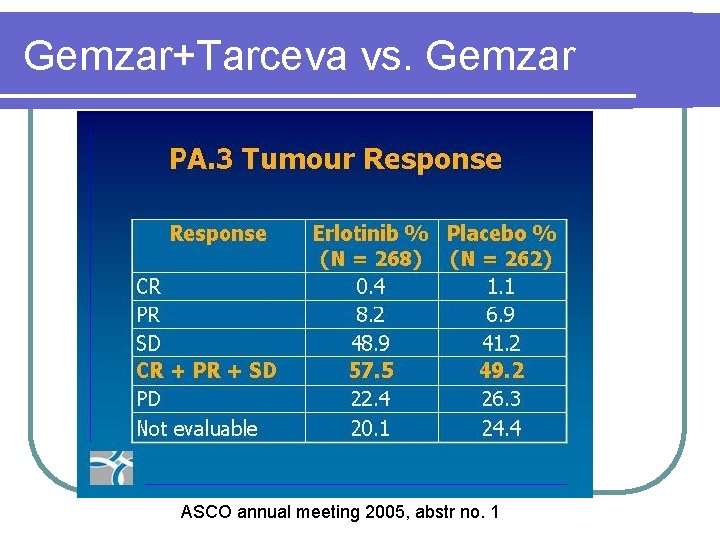
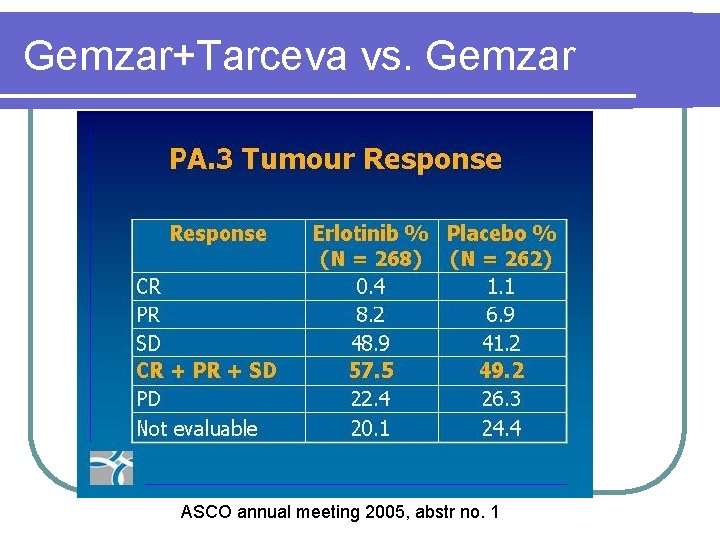
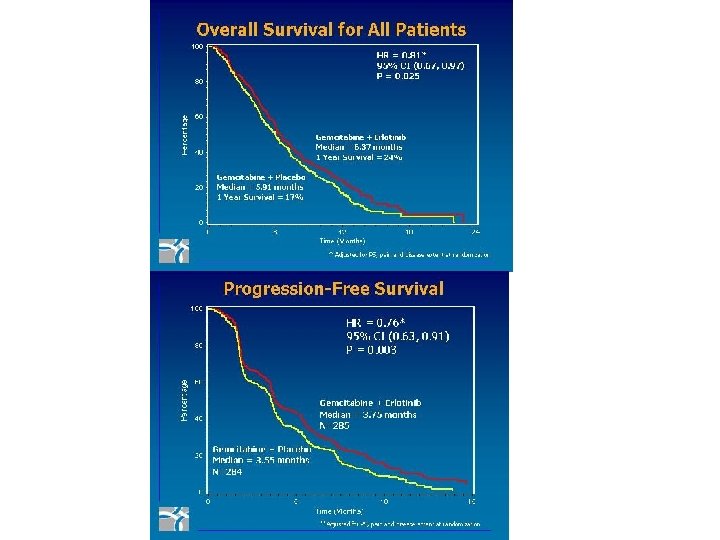
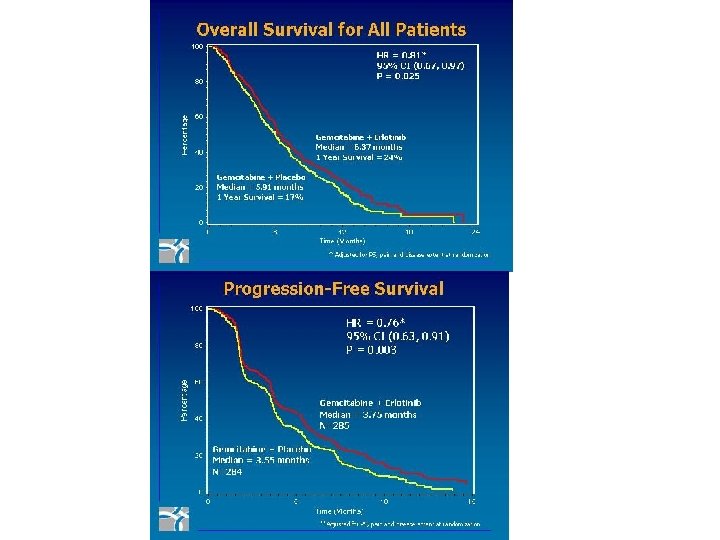
Gemzar+Tarceva vs. Gemzar ASCO annual meeting 2005, abstr no. 1
Biliary tract cancer

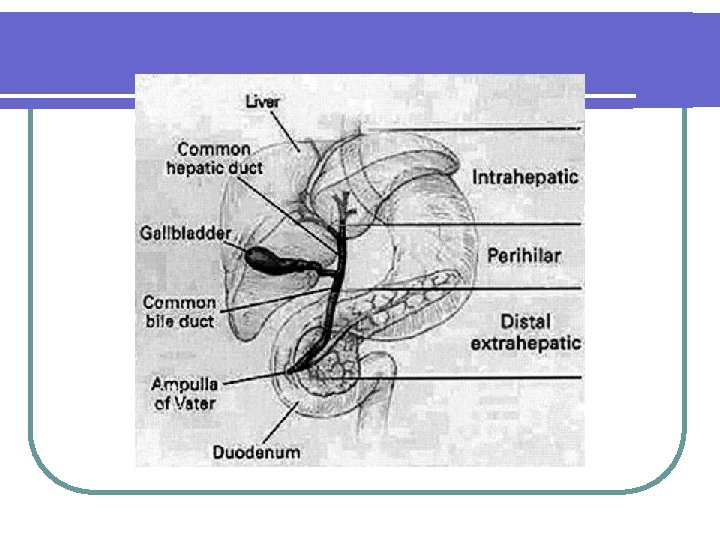
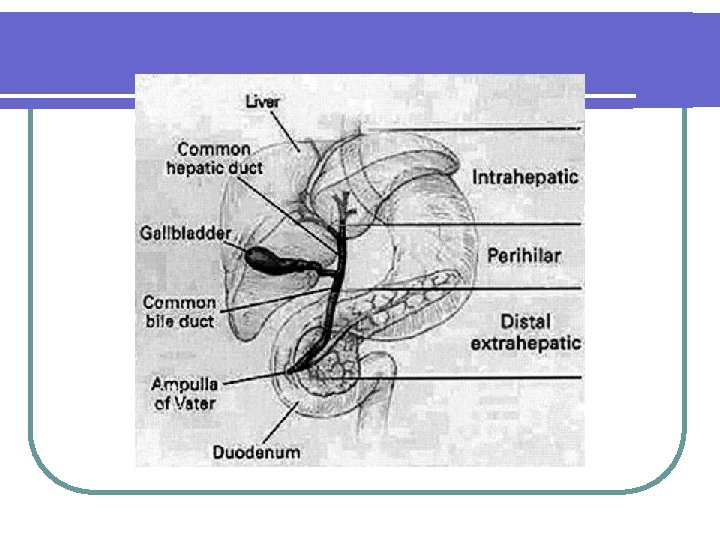
Classification l Cholangiocarcinoma l All tumors arise from bile duct epithelium l Mostly adenocarcinoma Intrahepatic (6%) l Hilum (67%): Klaskin’s tumor l Distal extrahepatic (27%) l Gall bladder l
Epidemiology l Old age: median 65 year-old l Slightly more in men l Uncommon cancer l Uncertain nature course and treatment

Risk factors l Chronic inflammation Primary sclerosing cholangitis : autoimmune l Choledochal cyst : congenital l Parasite l Stone : maybe l Repeat inflammation, stricture l Young age-onset l l Carcinogens
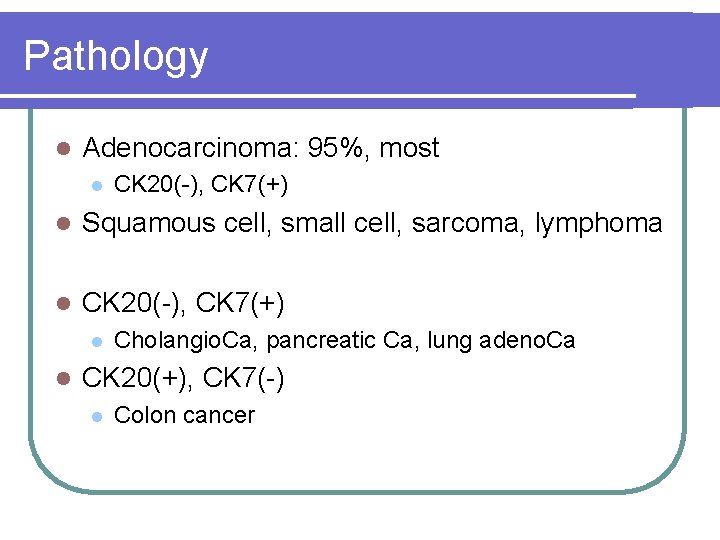
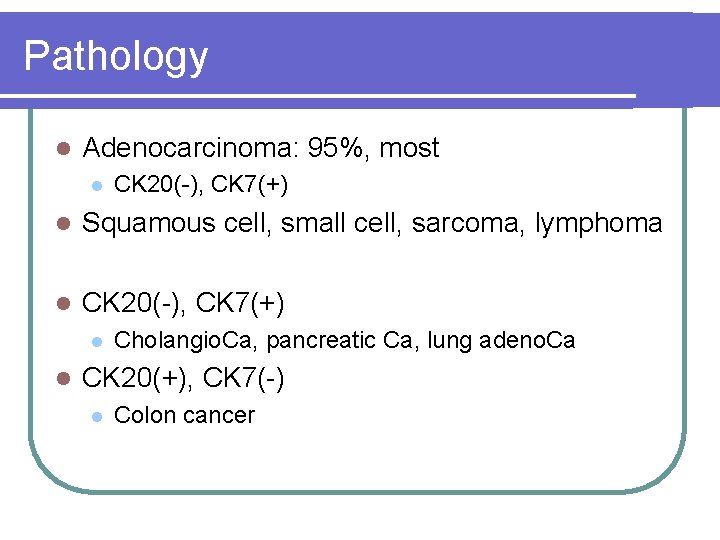
Pathology l Adenocarcinoma: 95%, most l CK 20(-), CK 7(+) l Squamous cell, small cell, sarcoma, lymphoma l CK 20(-), CK 7(+) l l Cholangio. Ca, pancreatic Ca, lung adeno. Ca CK 20(+), CK 7(-) l Colon cancer
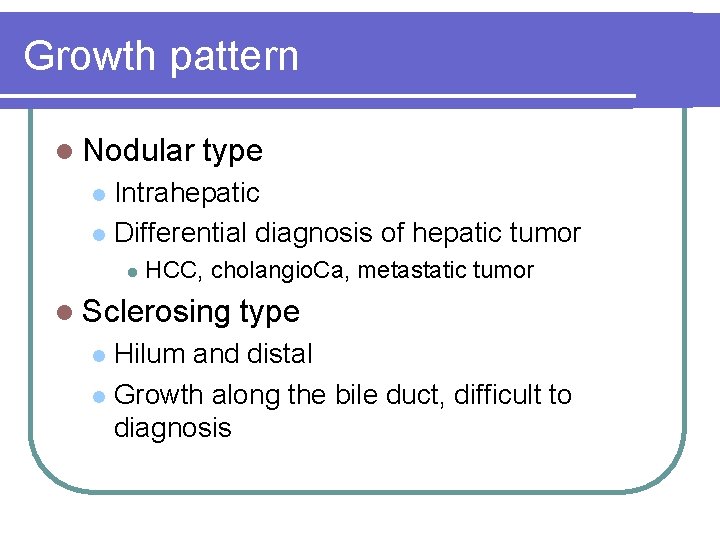
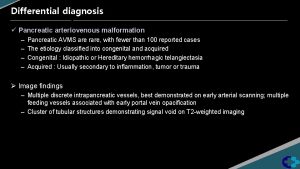
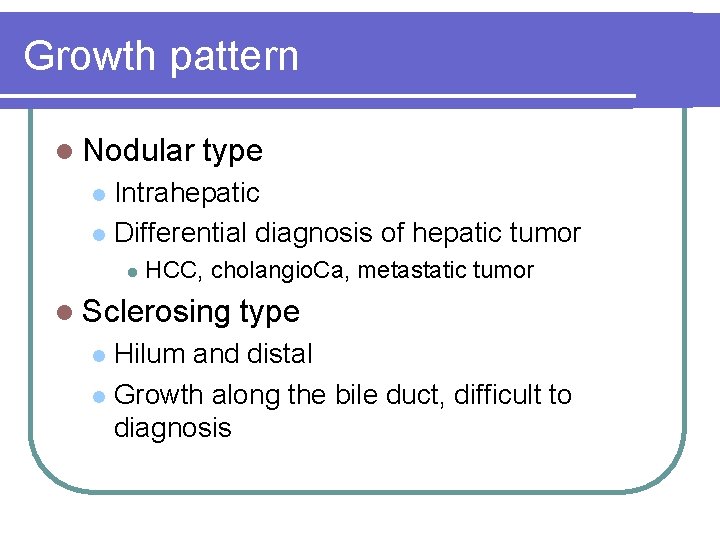
Growth pattern l Nodular type Intrahepatic l Differential diagnosis of hepatic tumor l l HCC, cholangio. Ca, metastatic tumor l Sclerosing type Hilum and distal l Growth along the bile duct, difficult to diagnosis l
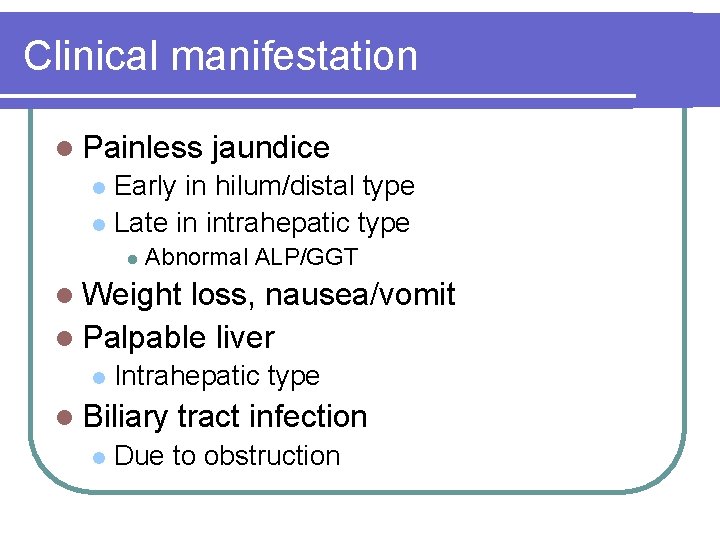
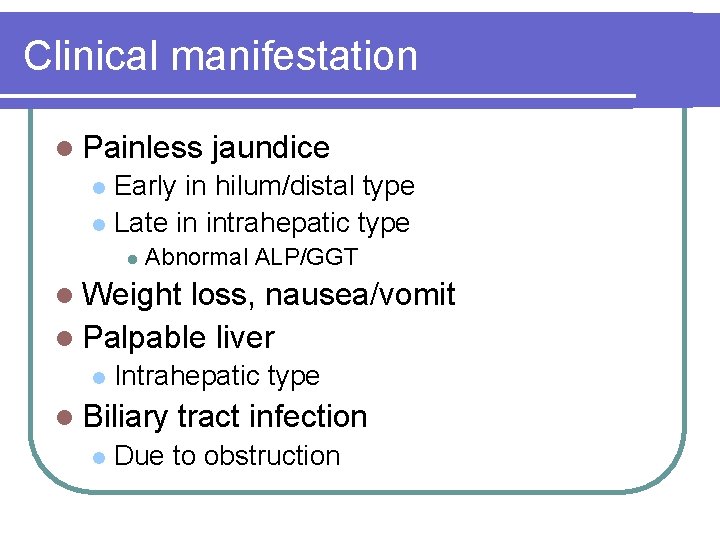
Clinical manifestation l Painless jaundice Early in hilum/distal type l Late in intrahepatic type l l Abnormal ALP/GGT l Weight loss, nausea/vomit l Palpable liver l Intrahepatic type l Biliary l tract infection Due to obstruction
Clinical manifestation l Tumor l markers Elevated serum CEA and CA 19 -9
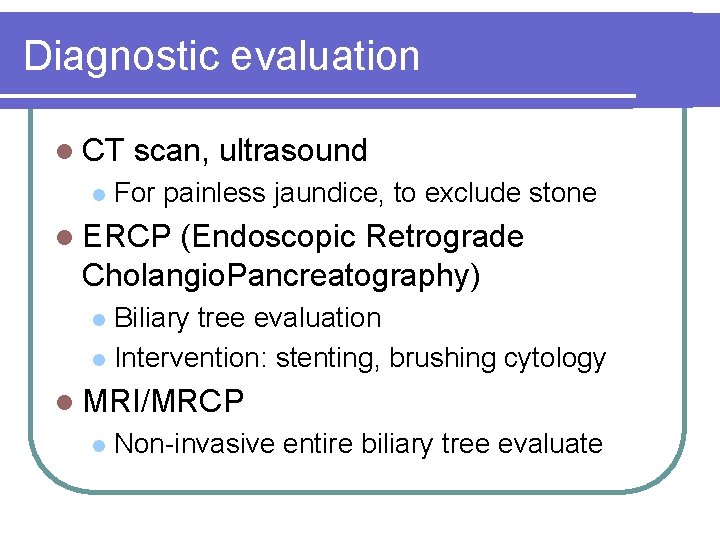
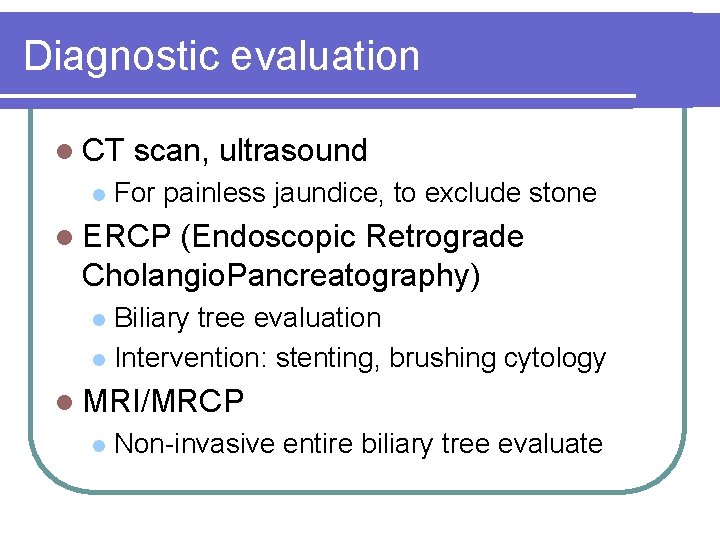
Diagnostic evaluation l CT l scan, ultrasound For painless jaundice, to exclude stone l ERCP (Endoscopic Retrograde Cholangio. Pancreatography) Biliary tree evaluation l Intervention: stenting, brushing cytology l l MRI/MRCP l Non-invasive entire biliary tree evaluate
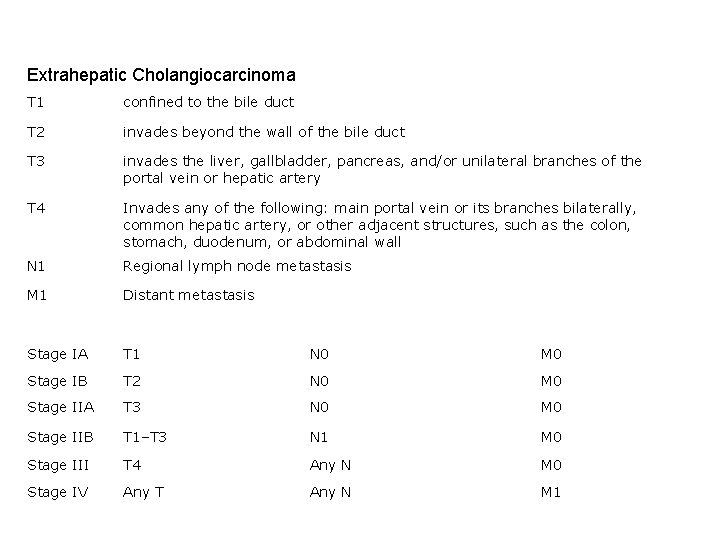
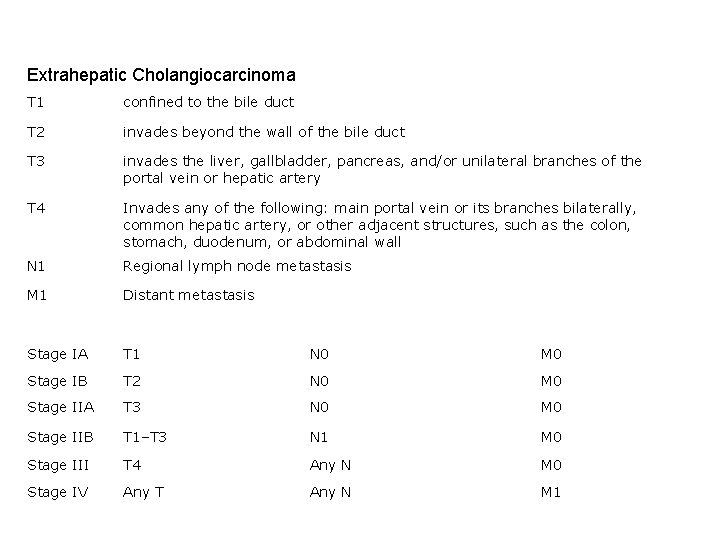
Extrahepatic Cholangiocarcinoma T 1 confined to the bile duct T 2 invades beyond the wall of the bile duct T 3 invades the liver, gallbladder, pancreas, and/or unilateral branches of the portal vein or hepatic artery T 4 Invades any of the following: main portal vein or its branches bilaterally, common hepatic artery, or other adjacent structures, such as the colon, stomach, duodenum, or abdominal wall N 1 Regional lymph node metastasis M 1 Distant metastasis Stage IA T 1 N 0 M 0 Stage IB T 2 N 0 M 0 Stage IIA T 3 N 0 M 0 Stage IIB T 1–T 3 N 1 M 0 Stage III T 4 Any N M 0 Stage IV Any T Any N M 1
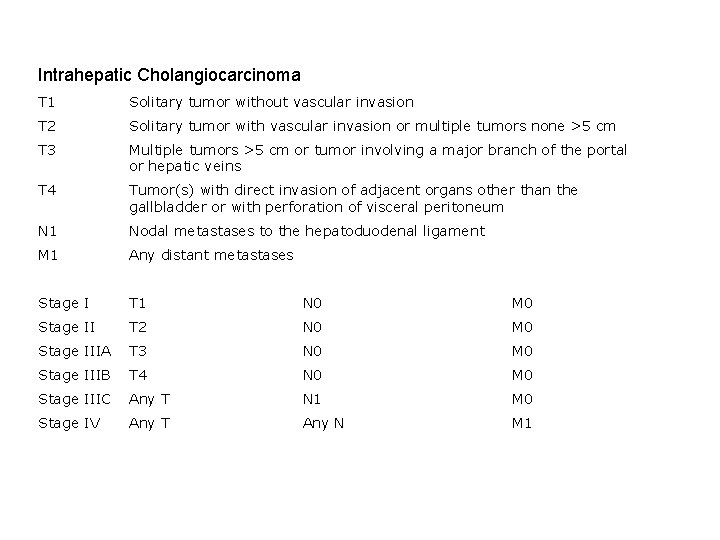
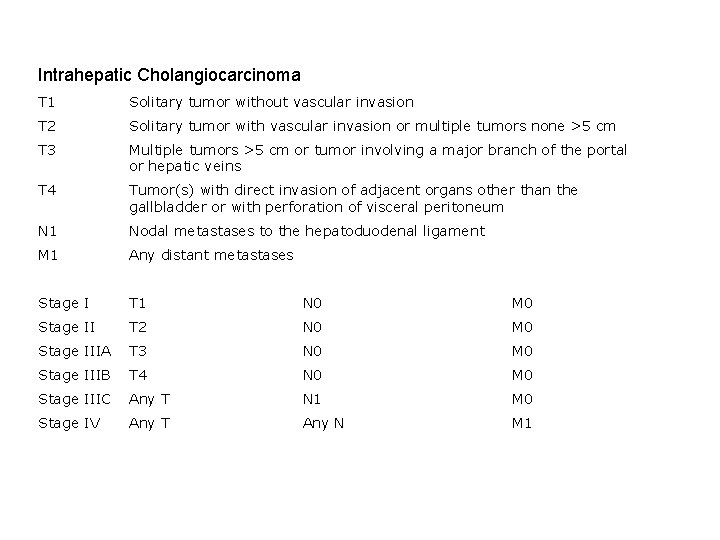
Intrahepatic Cholangiocarcinoma T 1 Solitary tumor without vascular invasion T 2 Solitary tumor with vascular invasion or multiple tumors none >5 cm T 3 Multiple tumors >5 cm or tumor involving a major branch of the portal or hepatic veins T 4 Tumor(s) with direct invasion of adjacent organs other than the gallbladder or with perforation of visceral peritoneum N 1 Nodal metastases to the hepatoduodenal ligament M 1 Any distant metastases Stage I T 1 N 0 M 0 Stage II T 2 N 0 M 0 Stage IIIA T 3 N 0 M 0 Stage IIIB T 4 N 0 M 0 Stage IIIC Any T N 1 M 0 Stage IV Any T Any N M 1
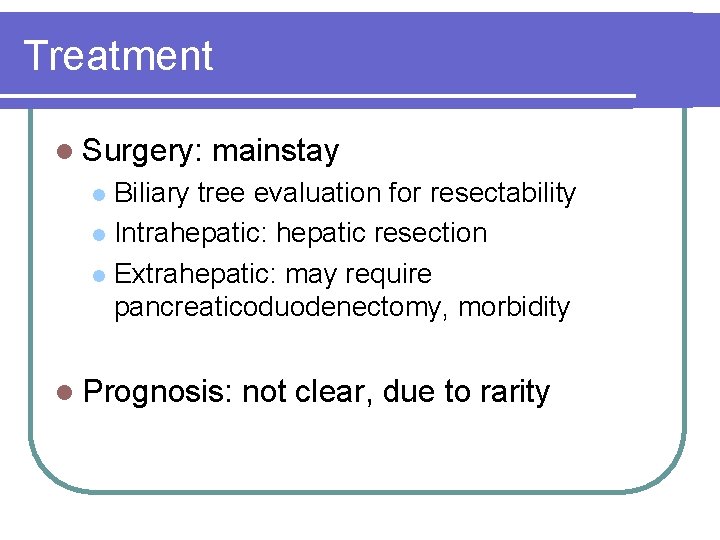
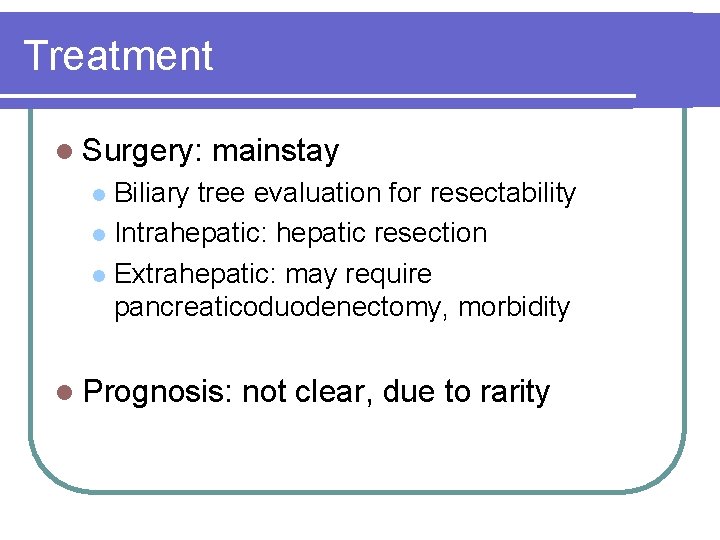
Treatment l Surgery: mainstay Biliary tree evaluation for resectability l Intrahepatic: hepatic resection l Extrahepatic: may require pancreaticoduodenectomy, morbidity l l Prognosis: not clear, due to rarity
Multimodality treatment l Pre-op l neoadjuvant tx RT, C/T, CRT no benefit l Post-op l adjuvant tx RT, C/T, CRT no benefit A trial suggest adjuvant C/T may benefit GB ca l Adjuvant CCRT for locally advance dz? l
Locally advanced disease l CCRT, can be considered 5 FU/LV l Good performance l Liver toxicity, GI toxicity l l Palliative chemotherapy
Palliative chemotherapy l Pooled analysis, extra- and intra-hepatic l 5 FU/LV remained mainstay Infusion, bolus l RR: 20%-30% l Survival 6 -7 m l l Combination: Traditional: cisplatin, mitomycin l Newer agents: gemcitabine, taxane l
Palliative procedure l Biliary stenting, PTCD l Complication of biliary stenting Communicate bile duct and intestine l Bile is sterile l Resultant repeat infection (BTI) l
 Epi 4 dogs
Epi 4 dogs Stage 2b pancreatic cancer
Stage 2b pancreatic cancer Ralph steinman pancreatic cancer
Ralph steinman pancreatic cancer Exocrine cell signaling
Exocrine cell signaling Mérocrine
Mérocrine Cardiac muscle striations
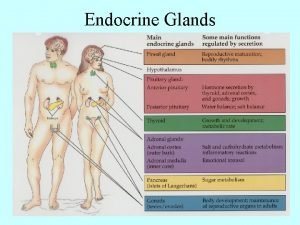
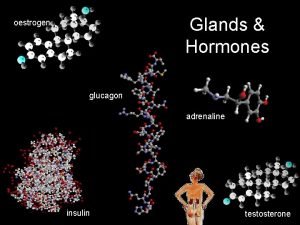
Cardiac muscle striations Endocrine versus exocrine
Endocrine versus exocrine Pancreas exocrine gland
Pancreas exocrine gland Intraductal papillary mucinous neoplasm
Intraductal papillary mucinous neoplasm Endocrine exocrine
Endocrine exocrine Exocrine glands
Exocrine glands Whats the difference between endocrine and exocrine glands
Whats the difference between endocrine and exocrine glands The only example of unicellular exocrine glands are
The only example of unicellular exocrine glands are Difference between endocrine and exocrine glands
Difference between endocrine and exocrine glands Endocrine weight loss
Endocrine weight loss Classification of exocrine glands
Classification of exocrine glands Types of exocrine glands
Types of exocrine glands Exocrine glands
Exocrine glands Glande endocrine exocrine
Glande endocrine exocrine Ap biology chapter 40
Ap biology chapter 40 Are endocrine glands ductless
Are endocrine glands ductless Endocrine vs exocrine
Endocrine vs exocrine Stratum granulosum
Stratum granulosum Exocrine vs endocrine
Exocrine vs endocrine Multicellular exocrine glands can be classified
Multicellular exocrine glands can be classified Characteristics of epithelial tissue
Characteristics of epithelial tissue Hydrohepatosis
Hydrohepatosis Glucagon mechanism of action
Glucagon mechanism of action Pancreas
Pancreas Pancreatic juice
Pancreatic juice Wikipedia
Wikipedia Pancreas divisum surgery
Pancreas divisum surgery Absorption
Absorption Cells
Cells Daughter mother grandmother pancreatic lesions
Daughter mother grandmother pancreatic lesions Pancreatic digestive secretions
Pancreatic digestive secretions Pancreatic calcification
Pancreatic calcification Pancreatic enzymes
Pancreatic enzymes Ransons criteria
Ransons criteria Parotid
Parotid Cck function in digestion
Cck function in digestion Retinol function
Retinol function