Palpitation definition Most probable diagnoses DDX Important and
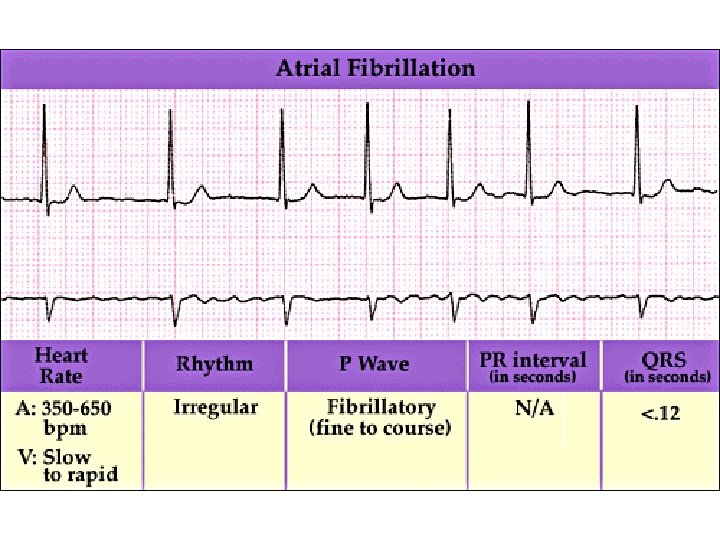
Palpitation - definition ? – Most probable diagnoses & DDX. – Important and serious diagnoses. – Common pitfalls.
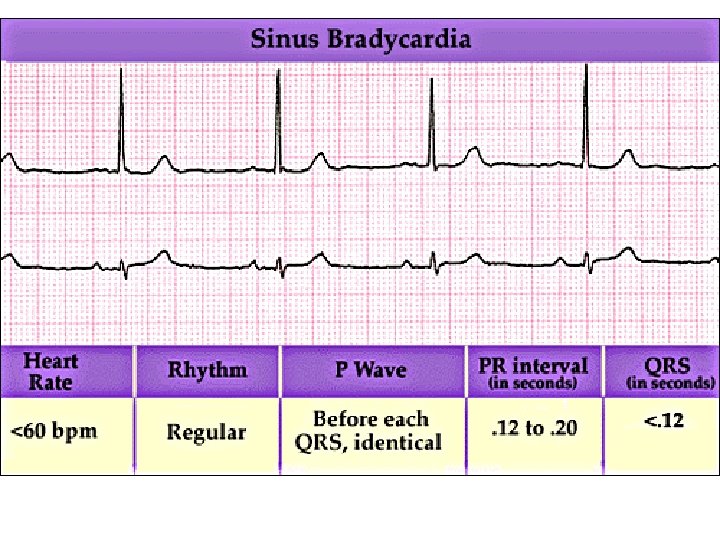
Palpitation definition • A subjective awareness of one’s heartbeat • # Bradycardia • # tachycardia
Spectrum of Patients’ Descriptions • • • Heart flips or flip-flops Skipped beats Strong beats Irregular beats Heart thumping Bubble sensation in heart or chest Racing or rapid heart beats Pounding in neck or chest Heart jumping out of chest Chest or whole body shaking
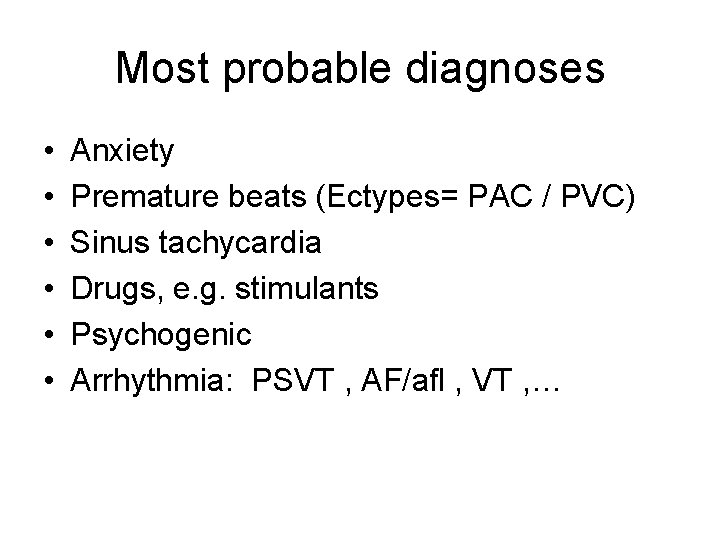
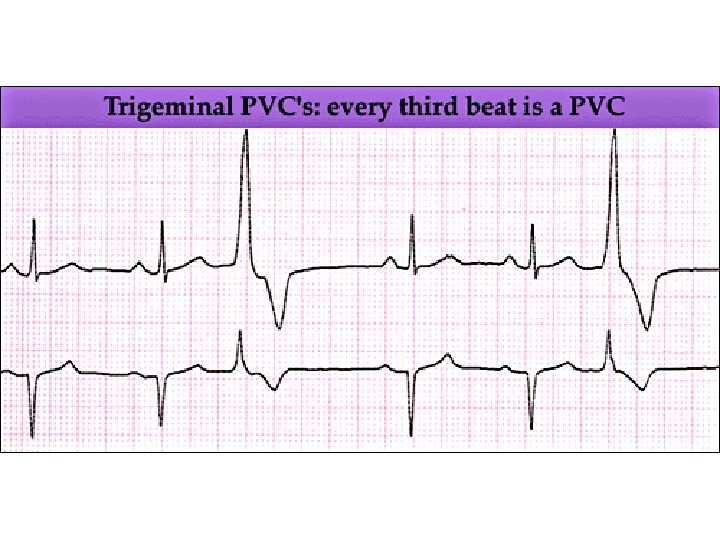
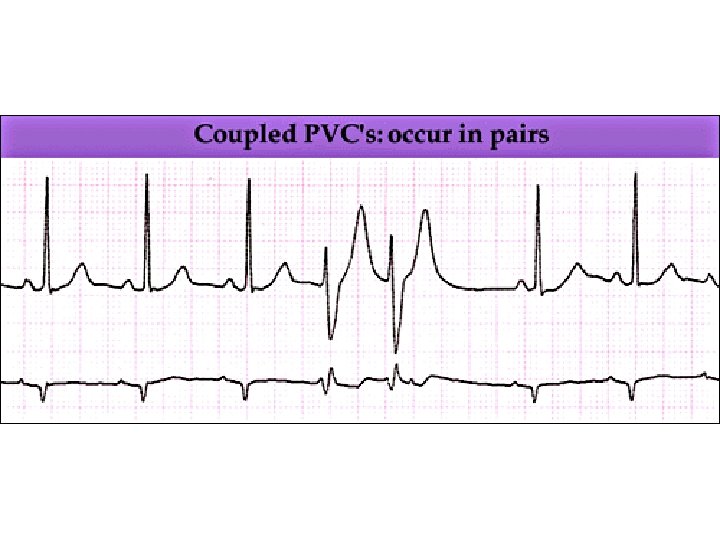
Most probable diagnoses • • • Anxiety Premature beats (Ectypes= PAC / PVC) Sinus tachycardia Drugs, e. g. stimulants Psychogenic Arrhythmia: PSVT , AF/afl , VT , …
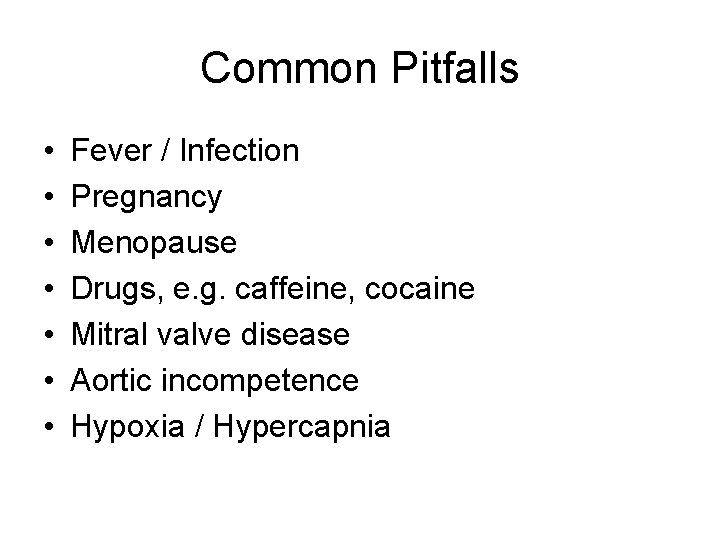
Common Pitfalls • • Fever / Infection Pregnancy Menopause Drugs, e. g. caffeine, cocaine Mitral valve disease Aortic incompetence Hypoxia / Hypercapnia
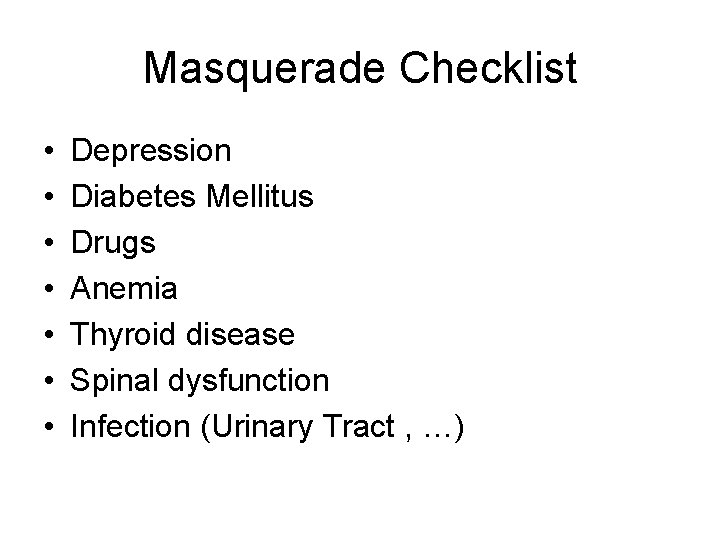
Masquerade Checklist • • Depression Diabetes Mellitus Drugs Anemia Thyroid disease Spinal dysfunction Infection (Urinary Tract , …)
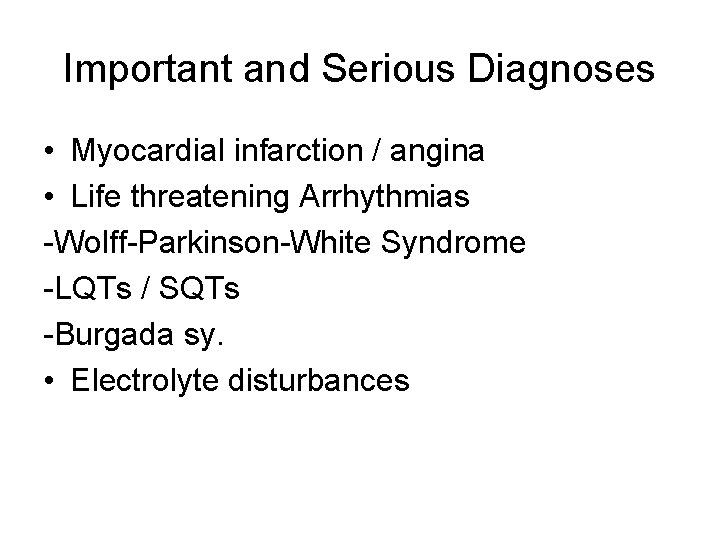
Important and Serious Diagnoses • Myocardial infarction / angina • Life threatening Arrhythmias -Wolff-Parkinson-White Syndrome -LQTs / SQTs -Burgada sy. • Electrolyte disturbances
History Keys: • Characterization of the palpitation • Attendant symptoms • Cardiac history • Arrhythmia history • Family history • Possible systemic & endocrinology disorders • Drug use
1 -Characterization of the Palpitation 1. 2. 3. 4. 5. 6. 7. Circumstances at onset Duration of the problem Mode of onset/offset , Trigger factors Heart rate estimate Rhythm regularity vs. irregularity Episode duration Symptom frequency
2 - Attendant Symptoms • • Symptoms arising from rhythm disorder Symptoms due to CAD or CHF Neurohormonal responses Psychological symptoms: Anxiety disorder , Panic attacks
3 - Cardiac History • • Ischemic heart disease LV dysfunction Valvular heart disease Atrial or ventricular arrhythmias
4 -Arrhythmia History • Recurrence vs. new onset • Recent history of radiofrequency ablation • Pacemaker or ICD implantation
5 - Family History • Long QT syndrome • Brugada’s syndrome • Familial cathecolamine-mediated polymorphic V. tachycardia • Atrial fibrillation
6 - Possible Endocrine and Metabolic Disorders • • Hyper or hypothyroidism Pheochromocytoma Diabetes Renal disorders Anemia Electrolyte imbalance Hypoglycemia Hx of rheumatic fever
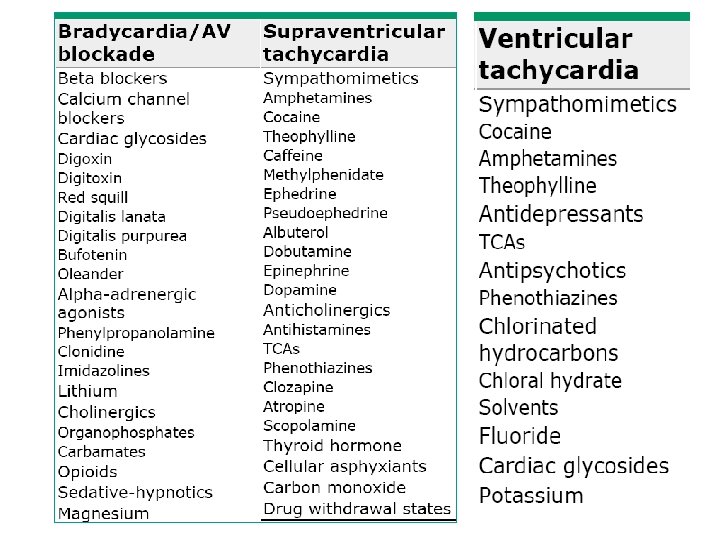
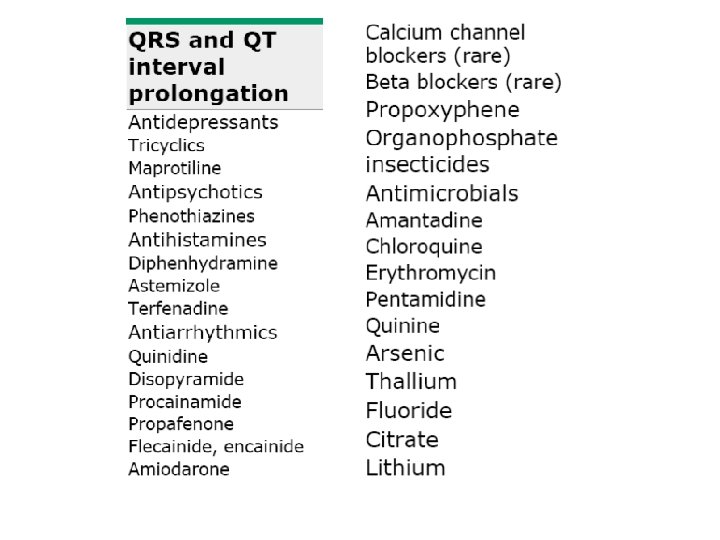
7 - Drug & Dietary Use • • Bronchodilator therapy, beta agonists, Caffeine , alcohol , Chocolate Stimulants / substance abuse: Cocaine OTC sympathomimetic agents QT-prolonging drugs Thyroid replacement medications phenothiazine, isotretinoin, digoxin Tobacco
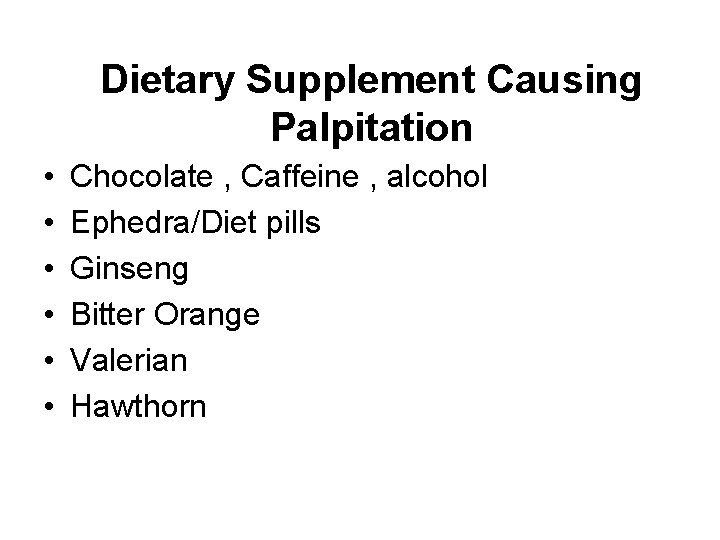
Dietary Supplement Causing Palpitation • • • Chocolate , Caffeine , alcohol Ephedra/Diet pills Ginseng Bitter Orange Valerian Hawthorn
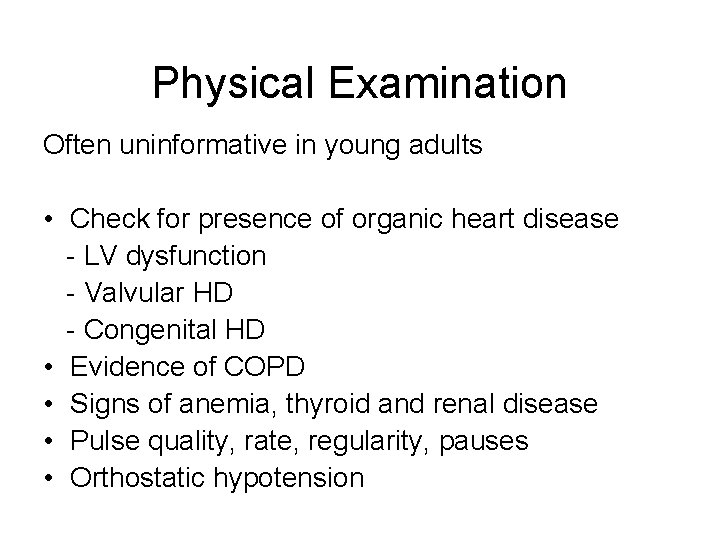
Physical Examination Often uninformative in young adults • Check for presence of organic heart disease - LV dysfunction - Valvular HD - Congenital HD • Evidence of COPD • Signs of anemia, thyroid and renal disease • Pulse quality, rate, regularity, pauses • Orthostatic hypotension
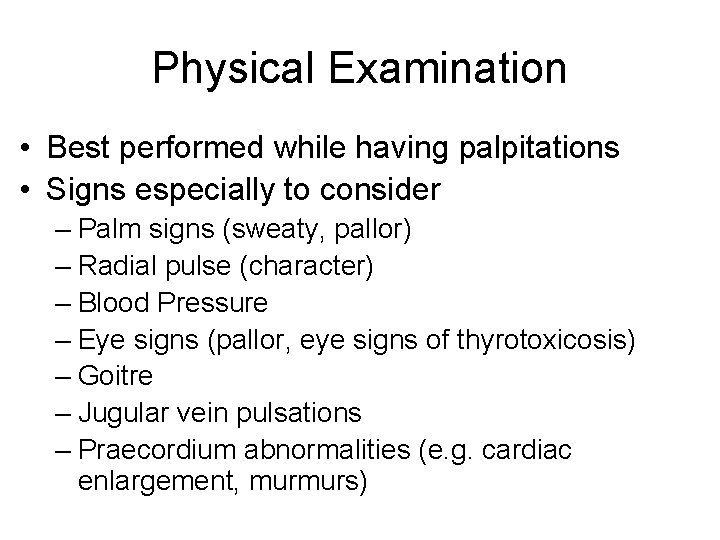
Physical Examination • Best performed while having palpitations • Signs especially to consider – Palm signs (sweaty, pallor) – Radial pulse (character) – Blood Pressure – Eye signs (pallor, eye signs of thyrotoxicosis) – Goitre – Jugular vein pulsations – Praecordium abnormalities (e. g. cardiac enlargement, murmurs)
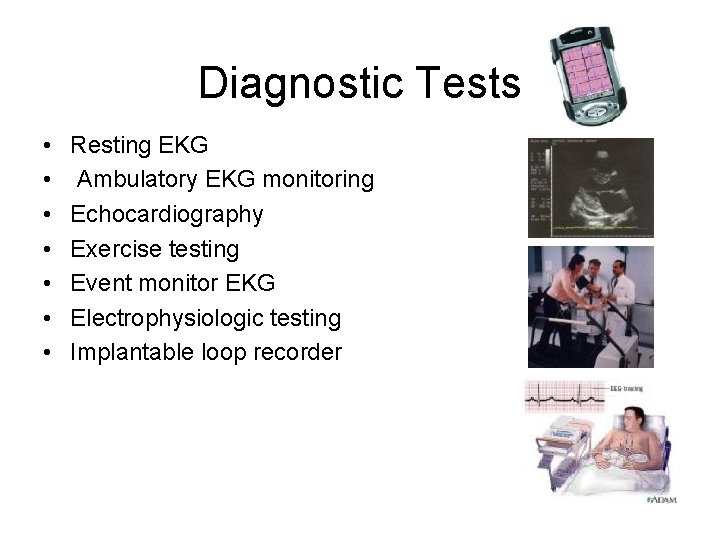
Diagnostic Tests • • Resting EKG Ambulatory EKG monitoring Echocardiography Exercise testing Event monitor EKG Electrophysiologic testing Implantable loop recorder
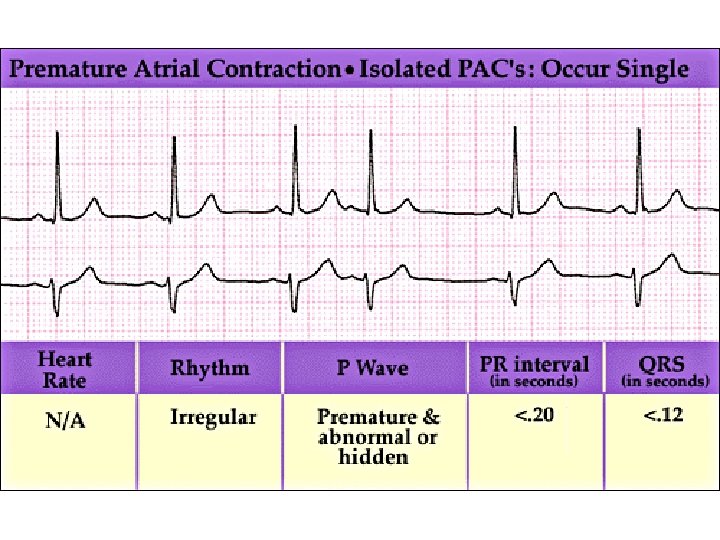
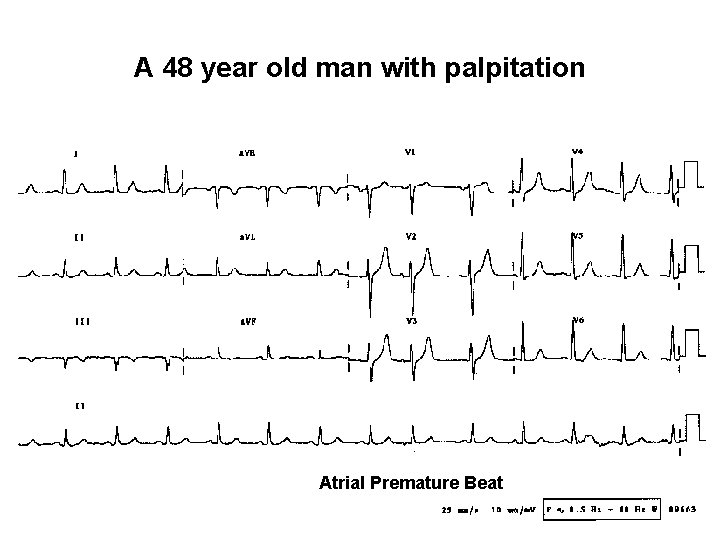
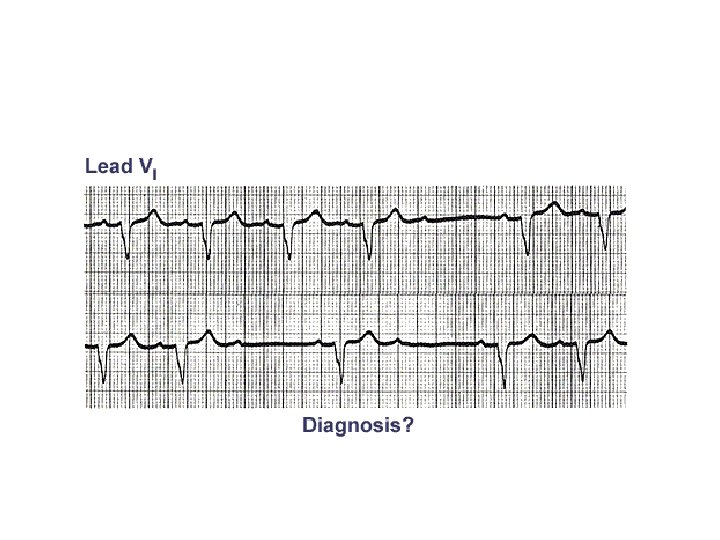
A 48 year old man with palpitation Atrial Premature Beat
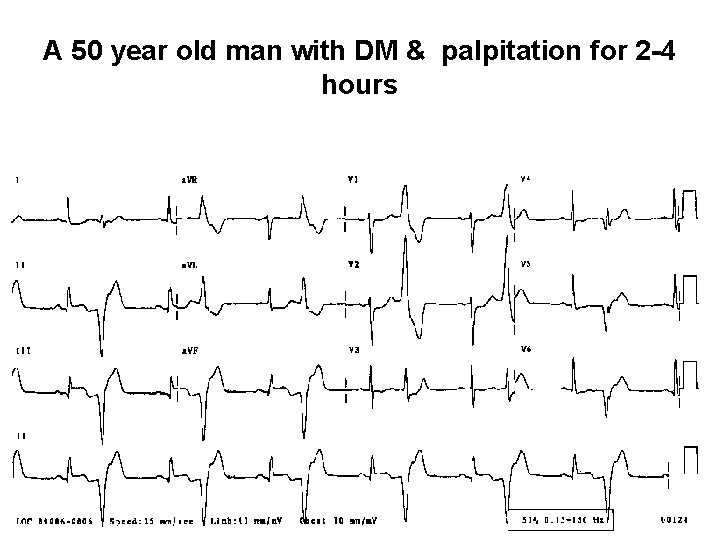
A 50 year old man with DM & palpitation for 2 -4 hours
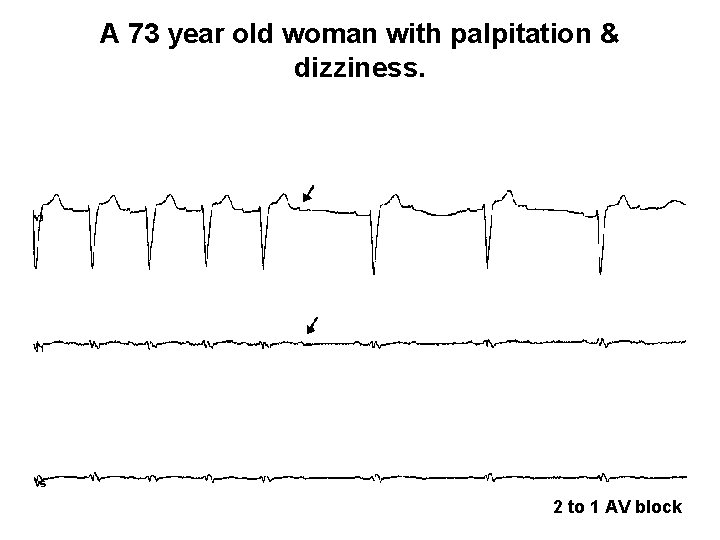
A 73 year old woman with palpitation & dizziness. 2 to 1 AV block
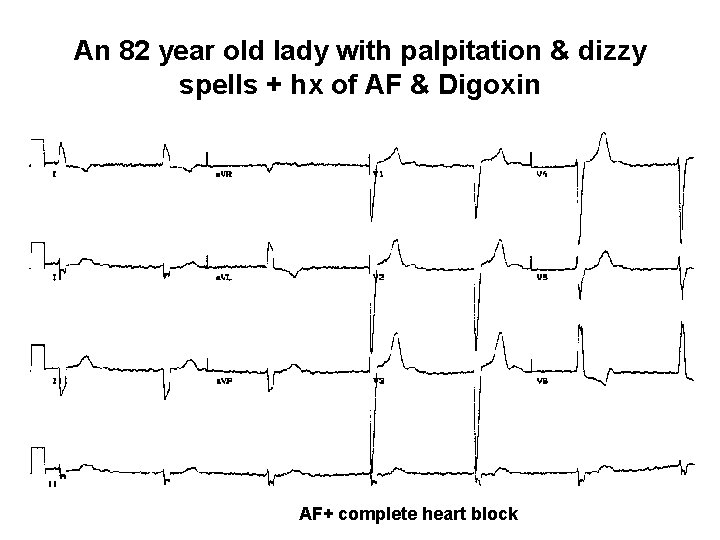
An 82 year old lady with palpitation & dizzy spells + hx of AF & Digoxin AF+ complete heart block
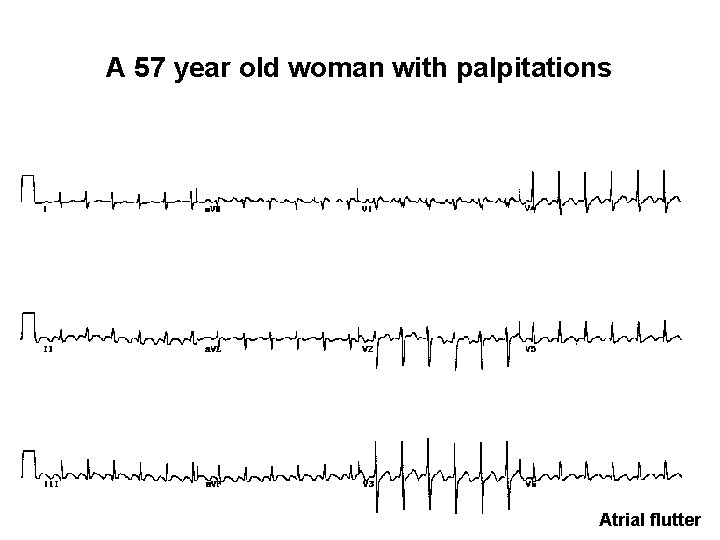
A 57 year old woman with palpitations Atrial flutter
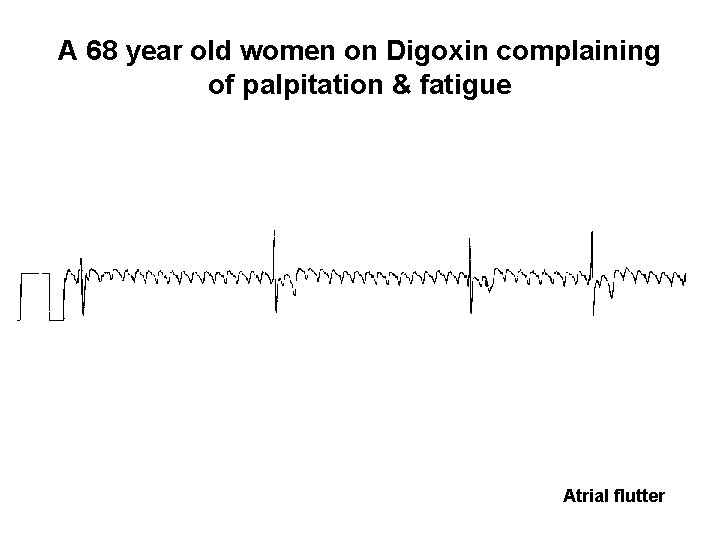
A 68 year old women on Digoxin complaining of palpitation & fatigue Atrial flutter
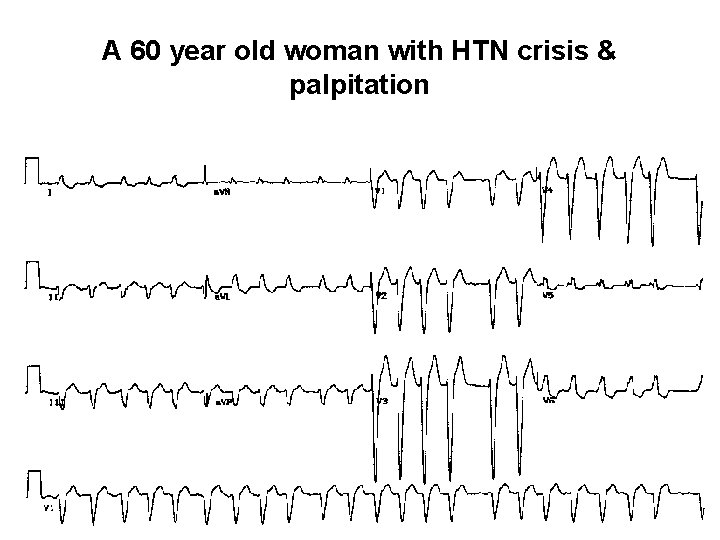
A 60 year old woman with HTN crisis & palpitation
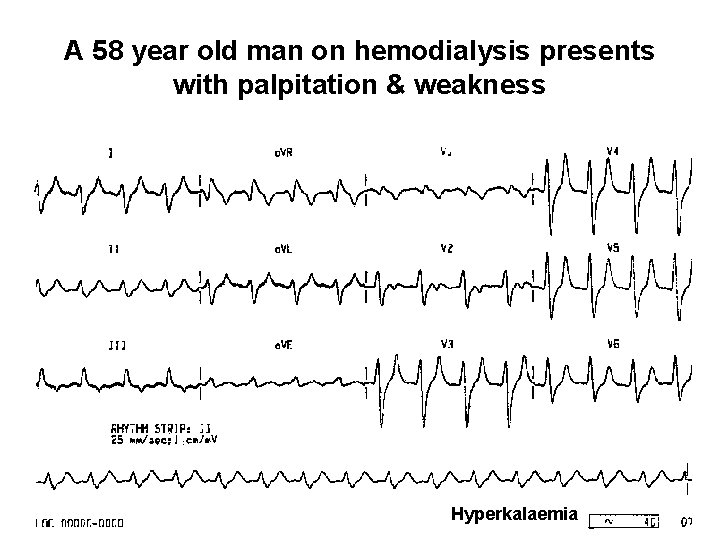
A 58 year old man on hemodialysis presents with palpitation & weakness Hyperkalaemia
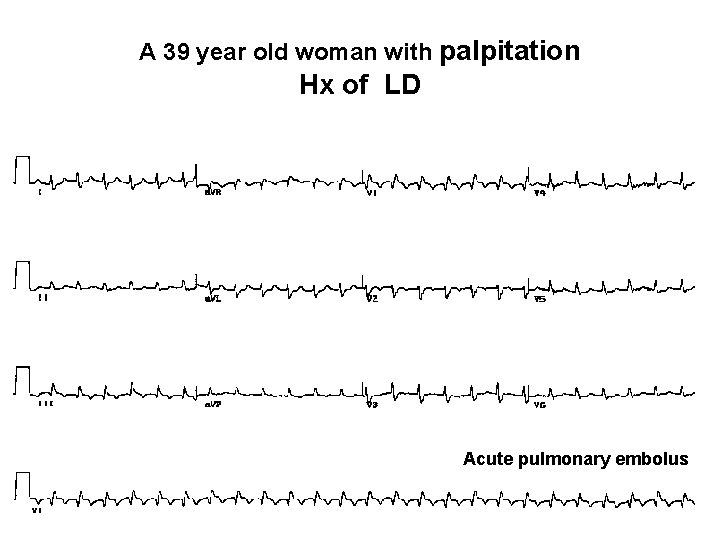
A 39 year old woman with palpitation Hx of LD Acute pulmonary embolus
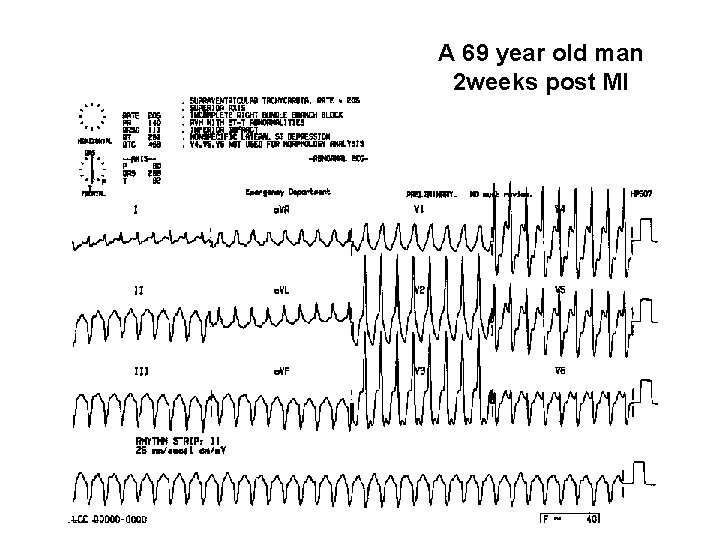
A 69 year old man 2 weeks post MI
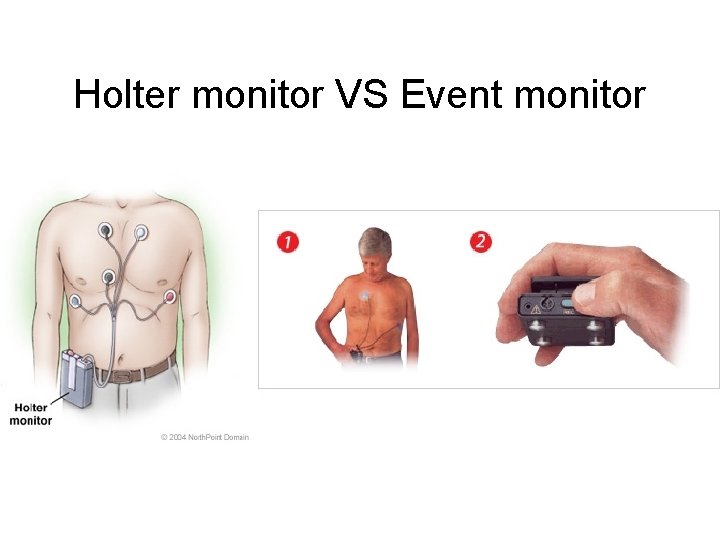
Holter monitor VS Event monitor
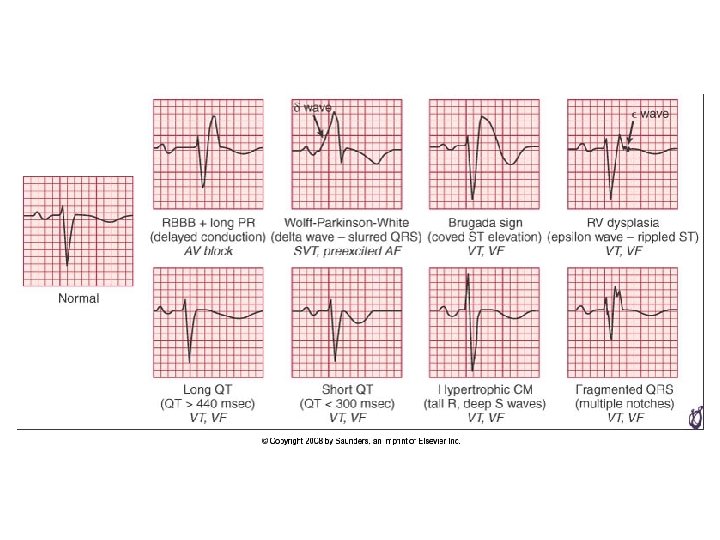
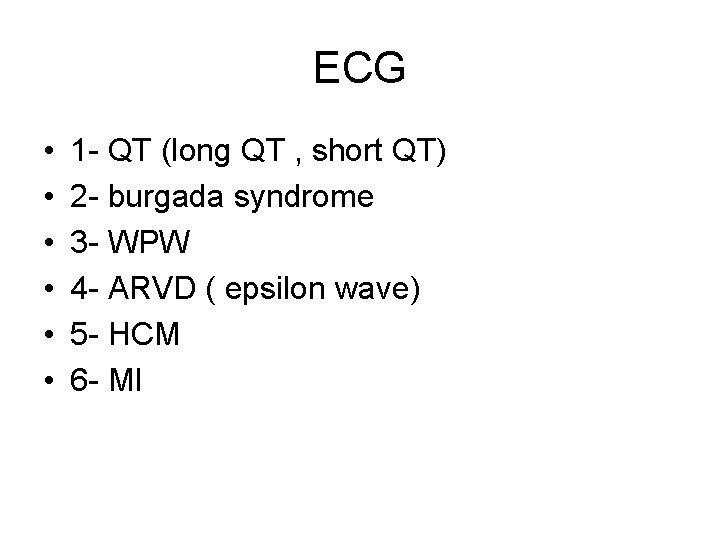
ECG • • • 1 - QT (long QT , short QT) 2 - burgada syndrome 3 - WPW 4 - ARVD ( epsilon wave) 5 - HCM 6 - MI
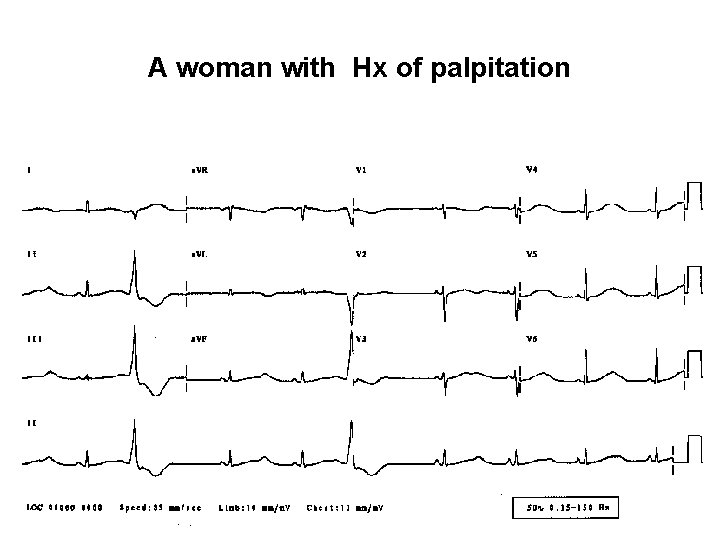
A woman with Hx of palpitation
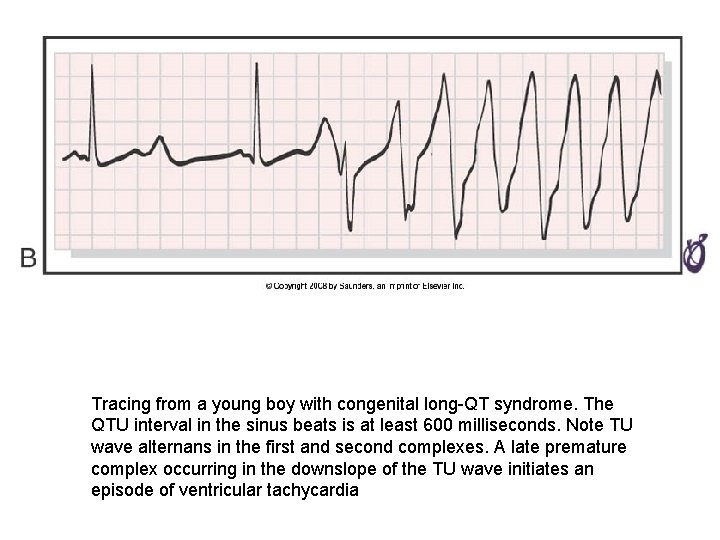
Tracing from a young boy with congenital long-QT syndrome. The QTU interval in the sinus beats is at least 600 milliseconds. Note TU wave alternans in the first and second complexes. A late premature complex occurring in the downslope of the TU wave initiates an episode of ventricular tachycardia
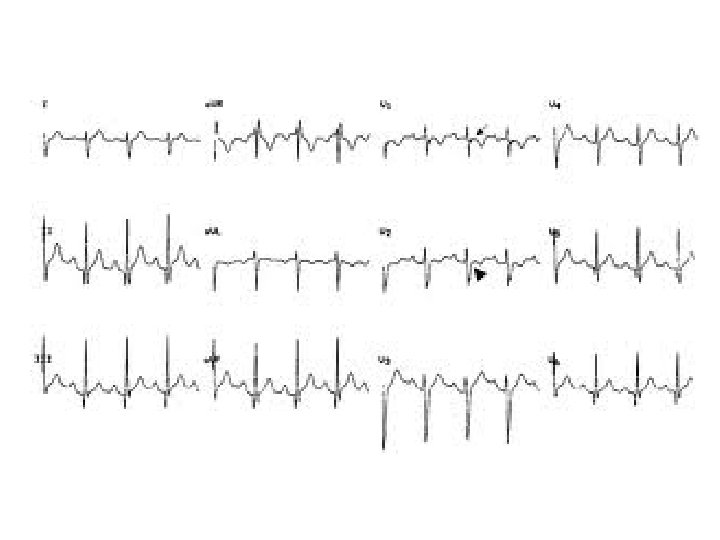
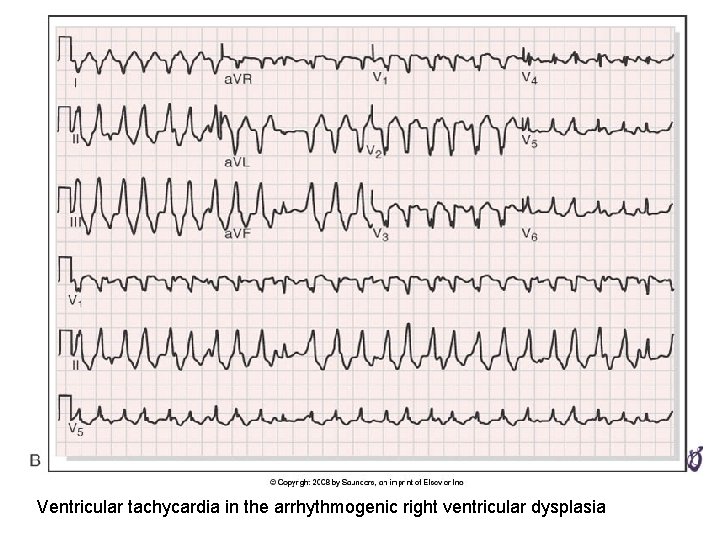
Ventricular tachycardia in the arrhythmogenic right ventricular dysplasia
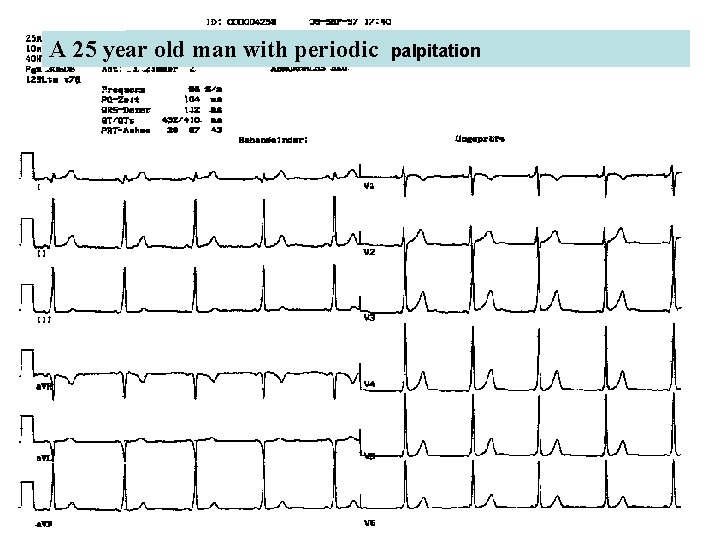
A 25 year old man with periodic palpitation
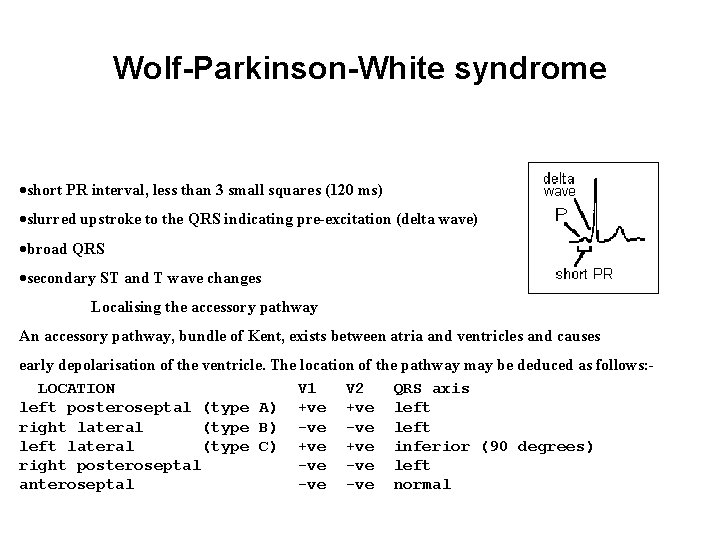
Wolf-Parkinson-White syndrome ·short PR interval, less than 3 small squares (120 ms) ·slurred upstroke to the QRS indicating pre-excitation (delta wave) ·broad QRS ·secondary ST and T wave changes Localising the accessory pathway An accessory pathway, bundle of Kent, exists between atria and ventricles and causes early depolarisation of the ventricle. The location of the pathway may be deduced as follows: LOCATION V 1 V 2 QRS axis left posteroseptal (type A) +ve left right lateral (type B) -ve left lateral (type C) +ve inferior (90 degrees) right posteroseptal -ve left anteroseptal -ve normal
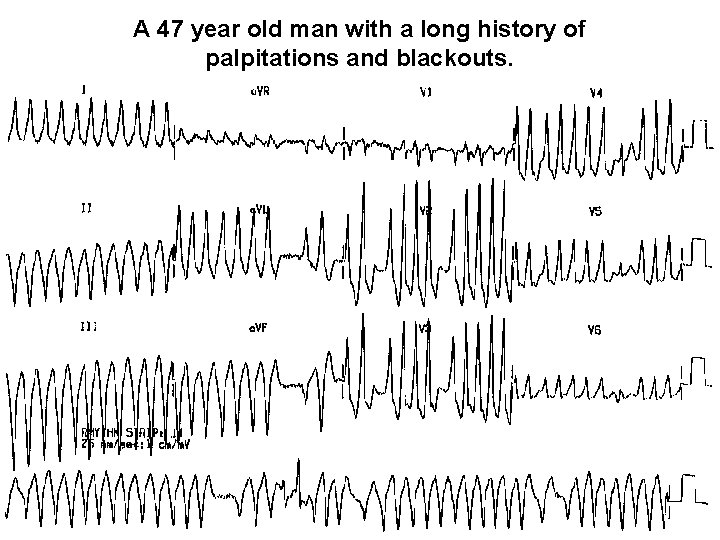
A 47 year old man with a long history of palpitations and blackouts.
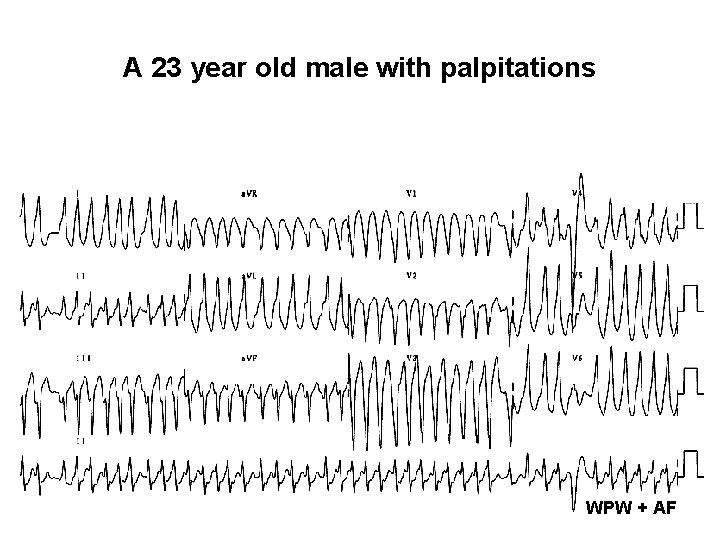
A 23 year old male with palpitations WPW + AF
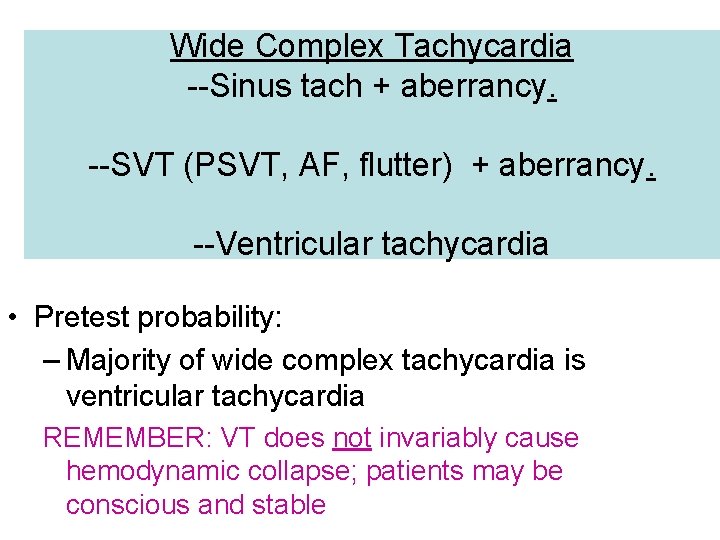
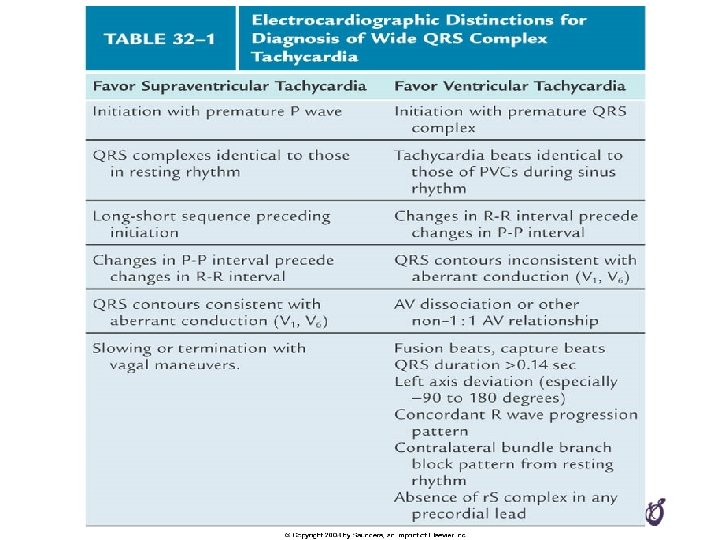
Wide Complex Tachycardia --Sinus tach + aberrancy. --SVT (PSVT, AF, flutter) + aberrancy. --Ventricular tachycardia • Pretest probability: – Majority of wide complex tachycardia is ventricular tachycardia REMEMBER: VT does not invariably cause hemodynamic collapse; patients may be conscious and stable
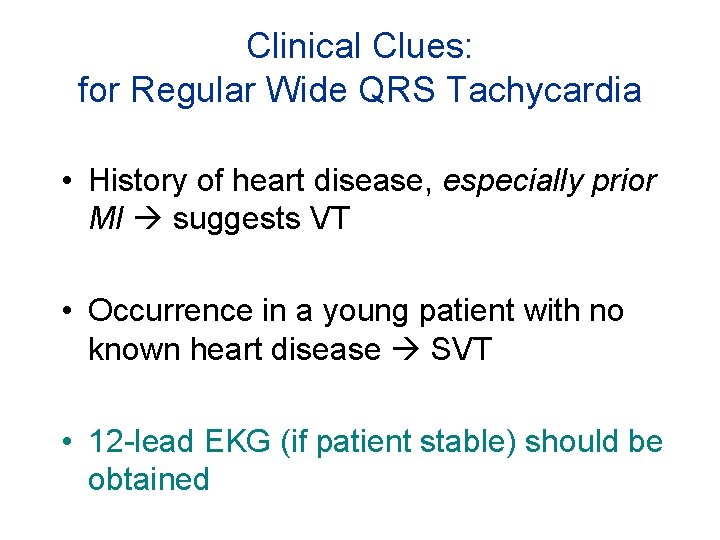
Clinical Clues: for Regular Wide QRS Tachycardia • History of heart disease, especially prior MI suggests VT • Occurrence in a young patient with no known heart disease SVT • 12 -lead EKG (if patient stable) should be obtained
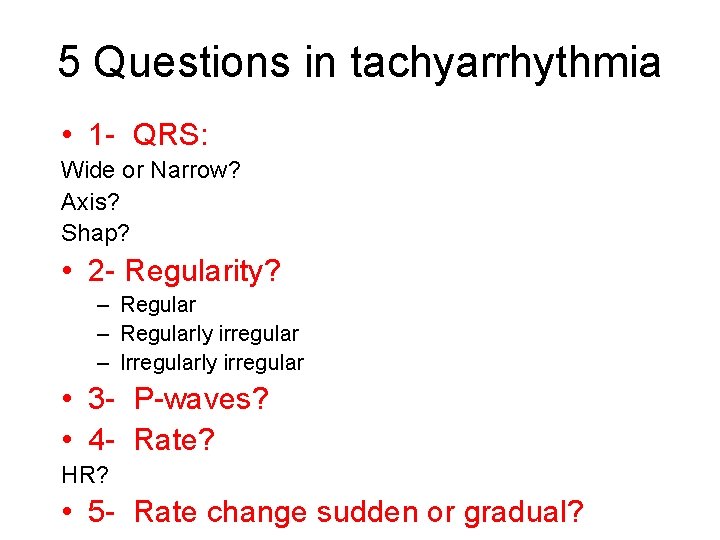
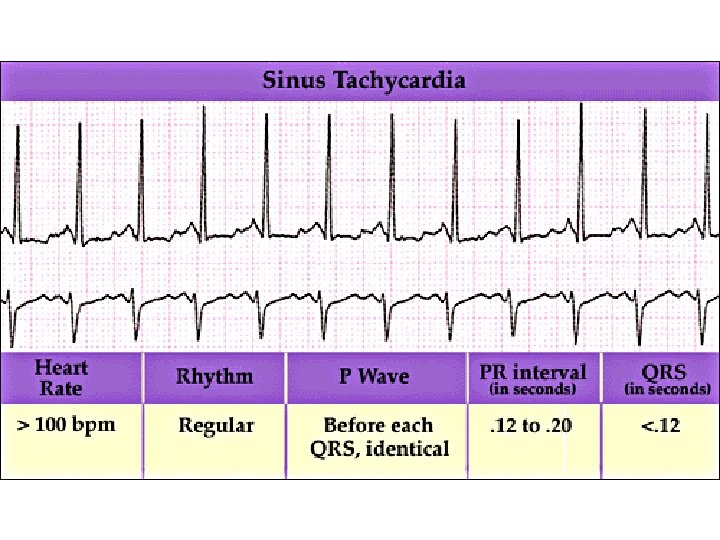
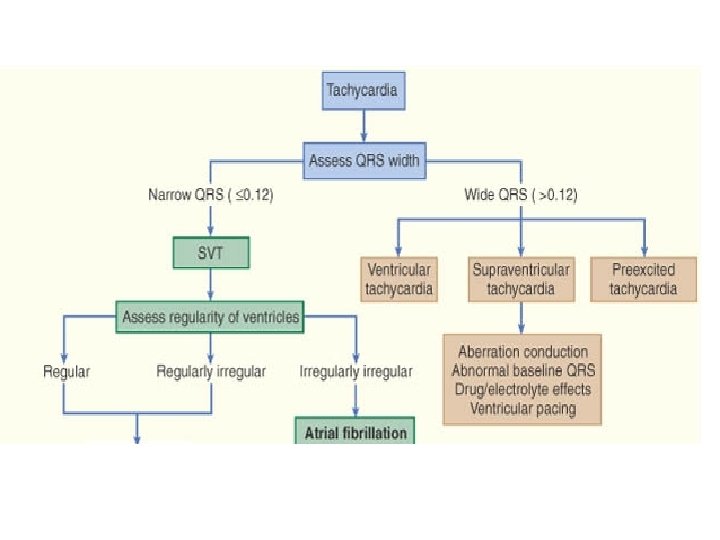
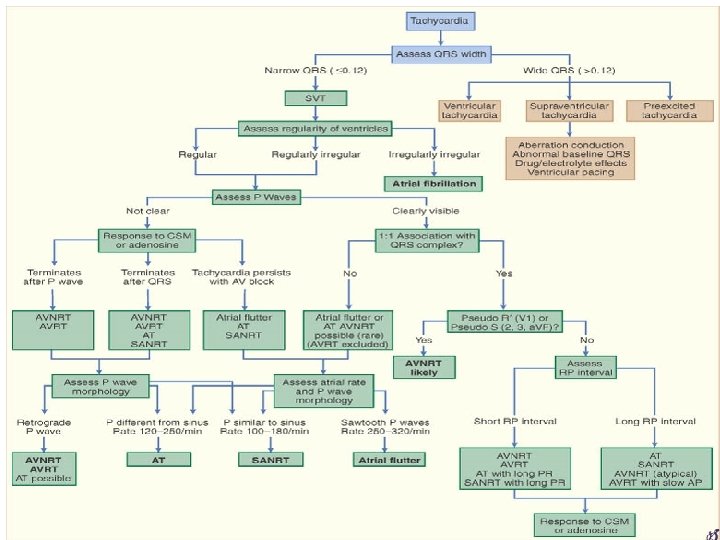
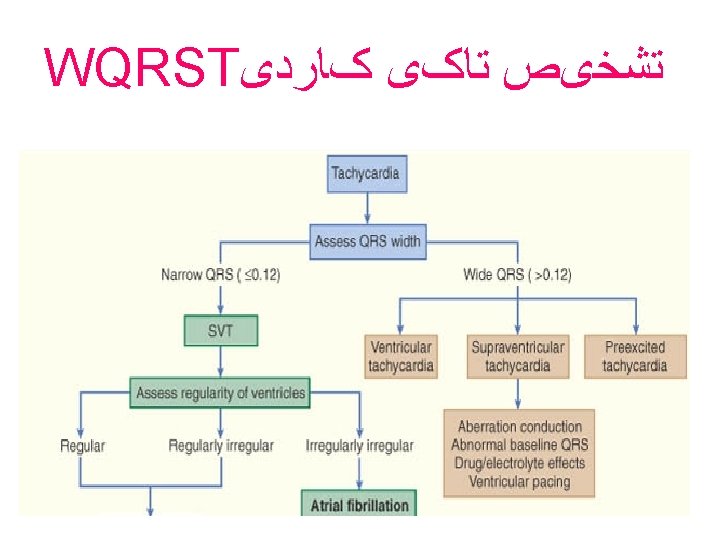
5 Questions in tachyarrhythmia • 1 - QRS: Wide or Narrow? Axis? Shap? • 2 - Regularity? – Regularly irregular – Irregularly irregular • 3 - P-waves? • 4 - Rate? HR? • 5 - Rate change sudden or gradual?
1 - QRS: Wide or Narrow • Narrow – Sinus, PSVT, A flutter, A fib • (All without aberrancy) • Wide – SVT + aberrancy – Ventricular tachycardia
Aberrancy - SVT with wide complex • Abnormal ventricular conduction – Anatomical : RBBB or LBBB – Functional : Rate-related BBB – Antidromic Reciprocating • Goes down through bypass tract
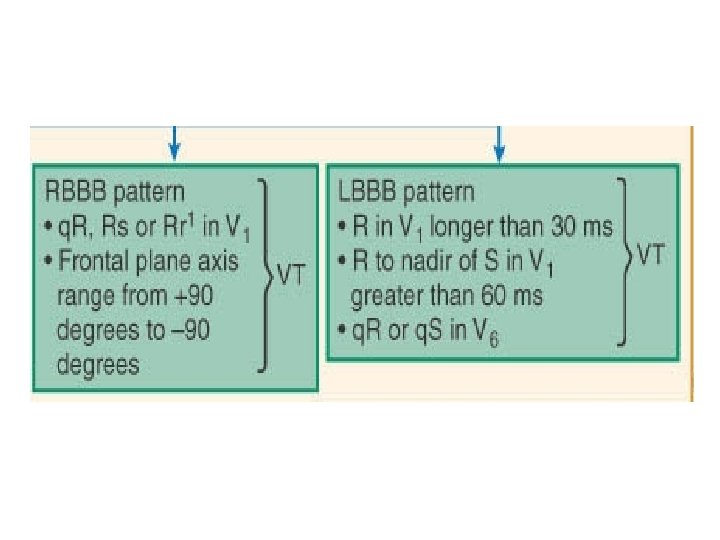
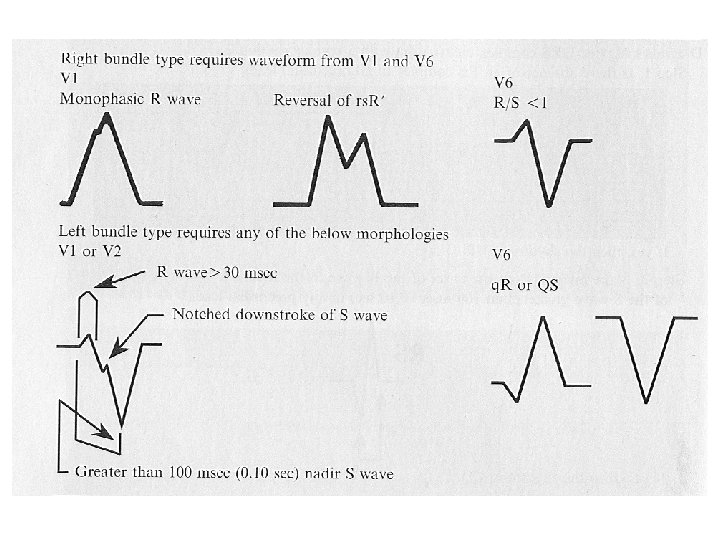
Suggest VT • In RBBB pattern > 140 ms • In LBBB pattern > 160 ms
1 - QRS: Shape? Typical or atypical LBBB/RBBB • true bundle branch block pattern – Right or left (sinus or SVT with aberrancy) • absence of RS complex in all leads V 1 -V 6 (negative Concordance)
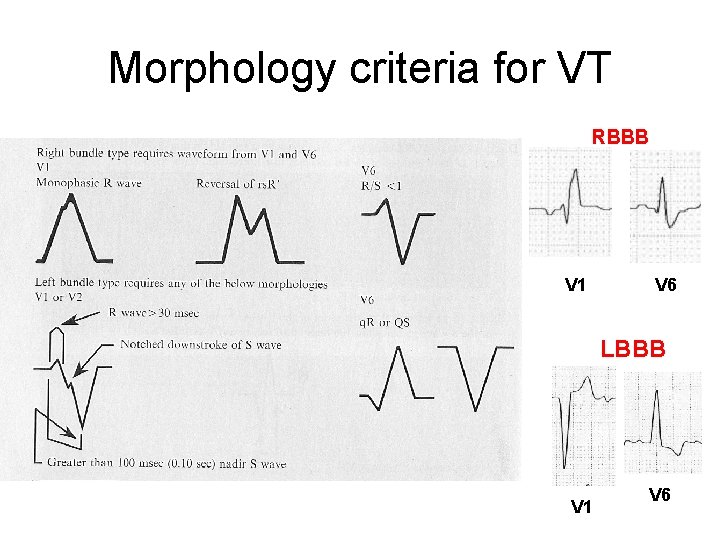
Morphology criteria for VT RBBB V 1 V 6 LBBB V 1 V 6
1 -QRS: Axis • >45 degree R in a. VR
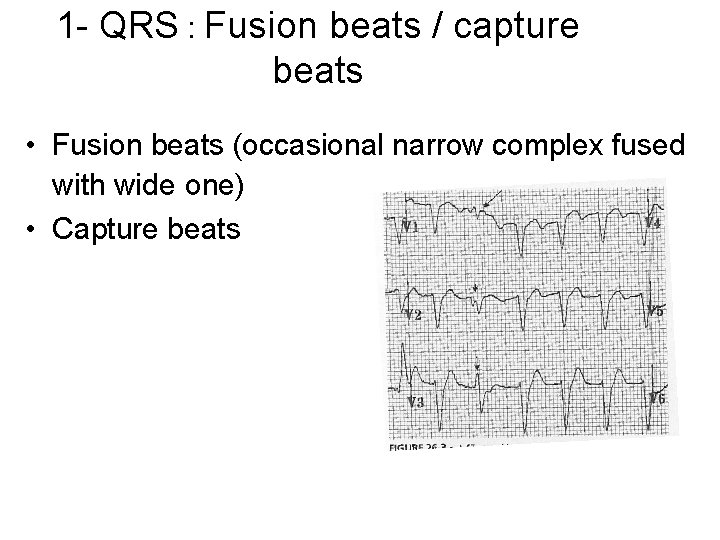
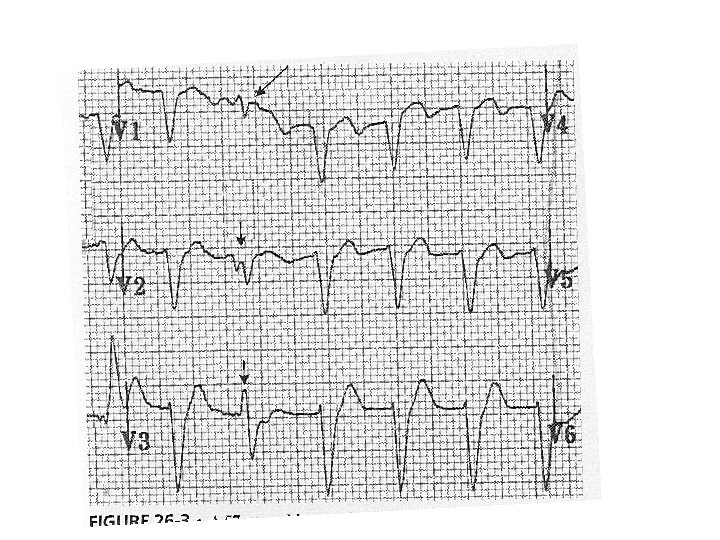
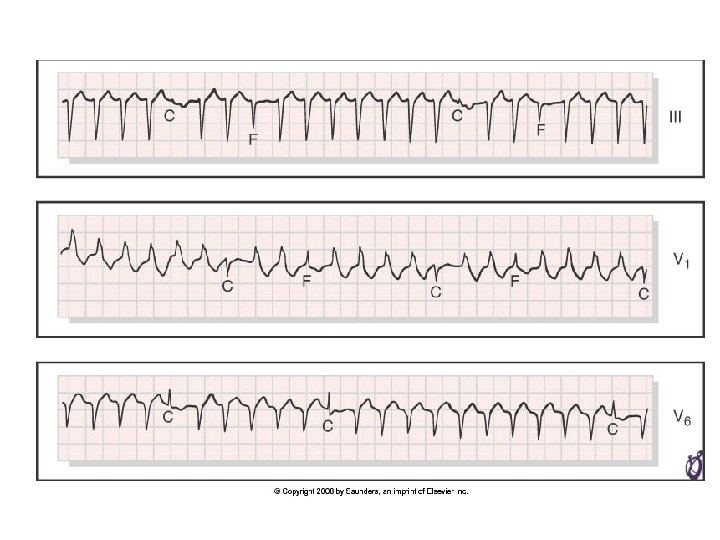
1 - QRS : Fusion beats / capture beats • Fusion beats (occasional narrow complex fused with wide one) • Capture beats
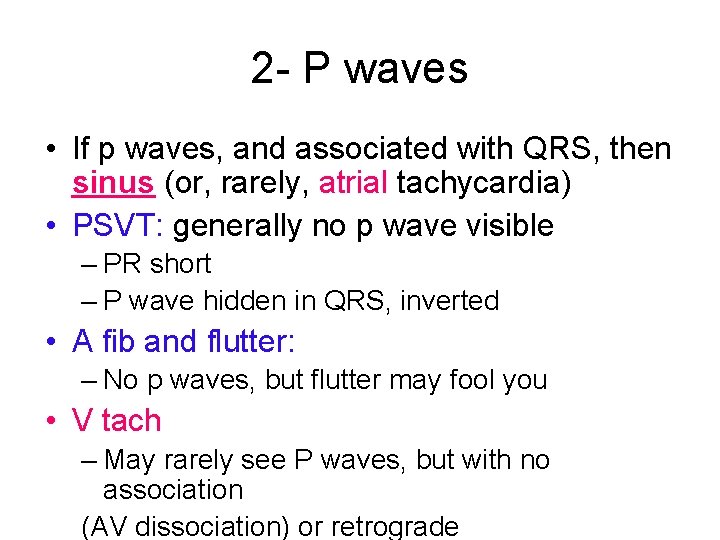
2 - P waves • If p waves, and associated with QRS, then sinus (or, rarely, atrial tachycardia) • PSVT: generally no p wave visible – PR short – P wave hidden in QRS, inverted • A fib and flutter: – No p waves, but flutter may fool you • V tach – May rarely see P waves, but with no association (AV dissociation) or retrograde
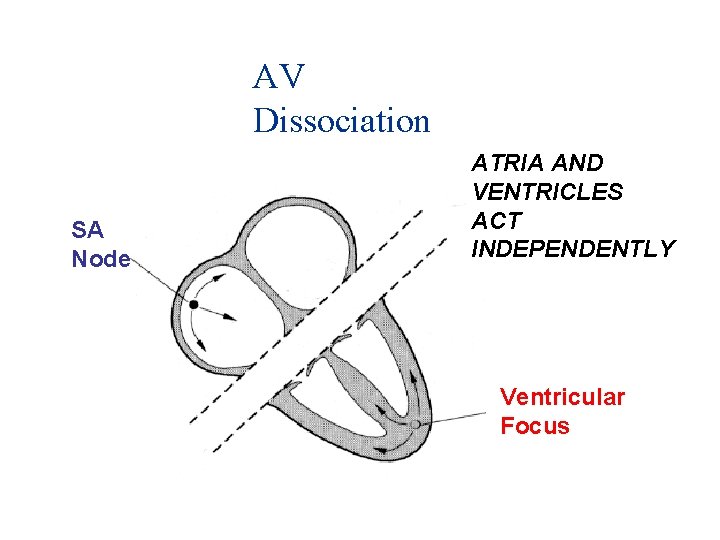
AV Dissociation SA Node ATRIA AND VENTRICLES ACT INDEPENDENTLY Ventricular Focus
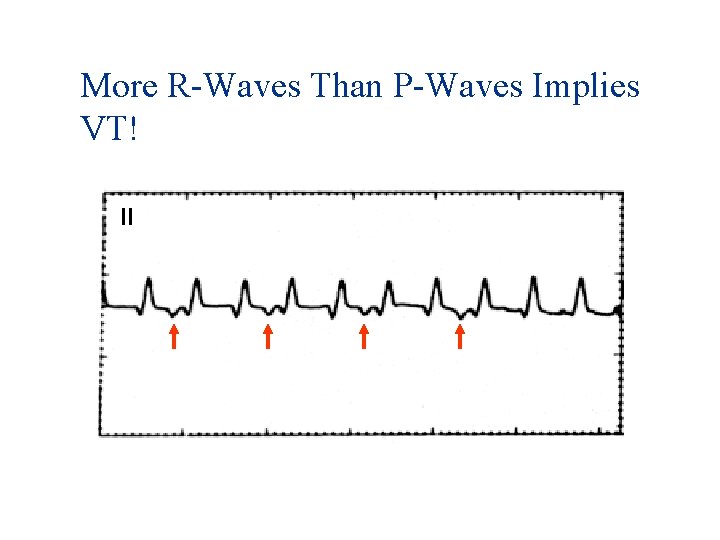
More R-Waves Than P-Waves Implies VT! II
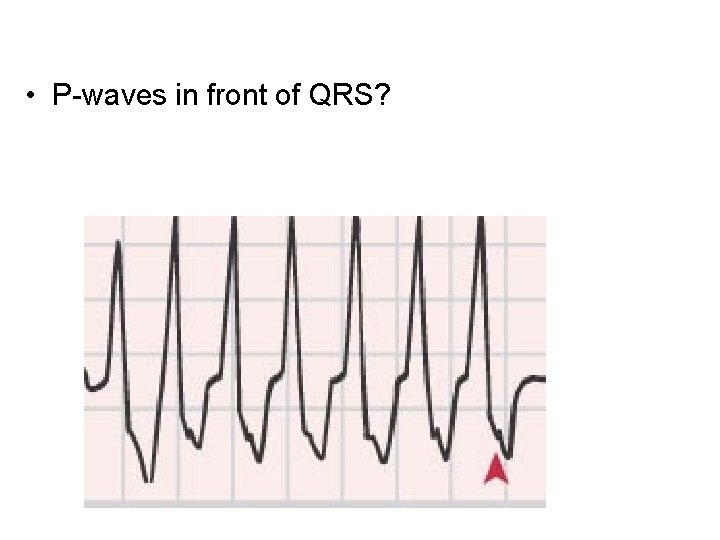
• P-waves in front of QRS?
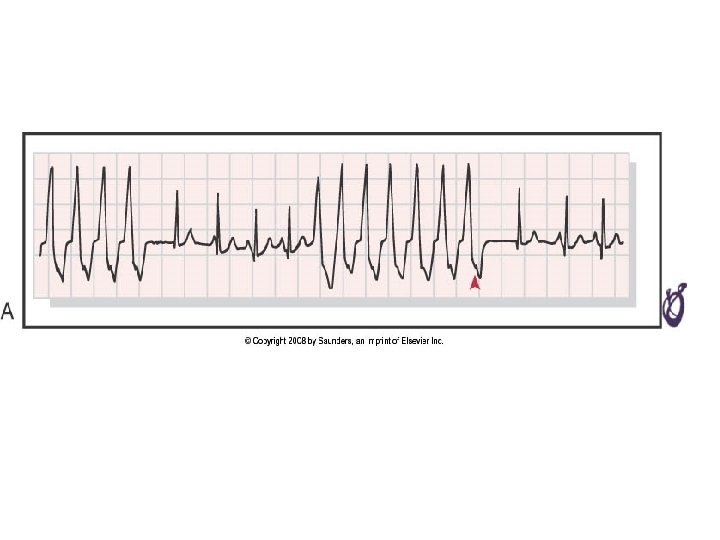
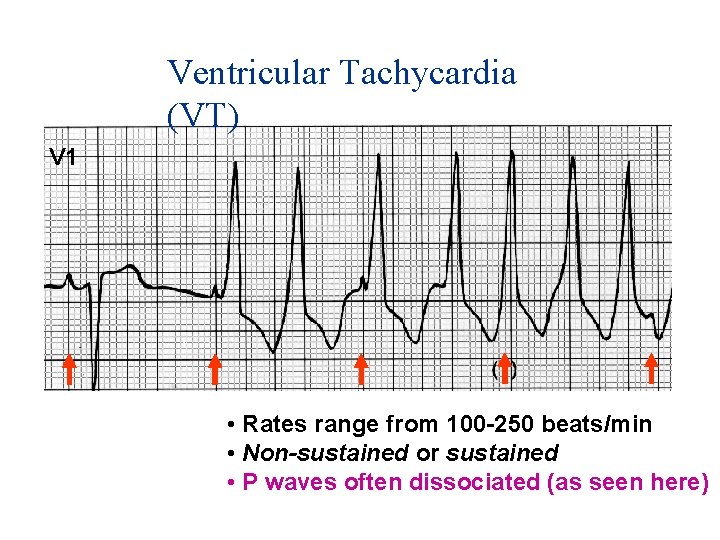
Ventricular Tachycardia (VT) V 1 • Rates range from 100 -250 beats/min • Non-sustained or sustained • P waves often dissociated (as seen here)
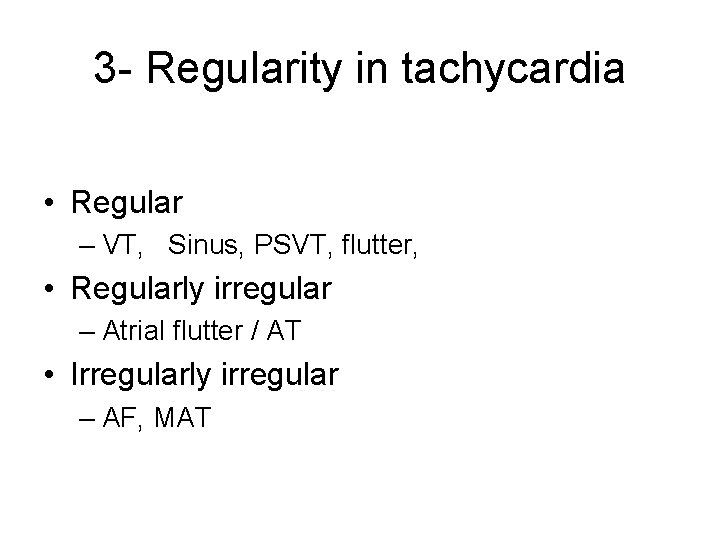
3 - Regularity in tachycardia • Regular – VT, Sinus, PSVT, flutter, • Regularly irregular – Atrial flutter / AT • Irregularly irregular – AF, MAT
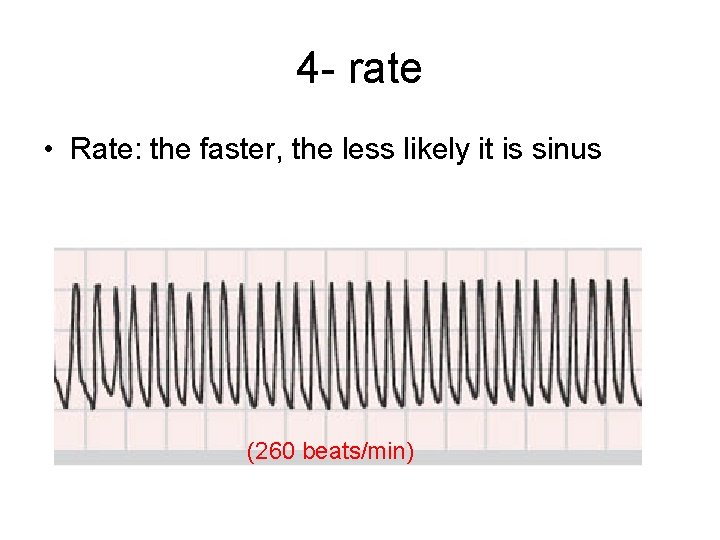
4 - rate • Rate: the faster, the less likely it is sinus (260 beats/min)
5 - Sudden vs. Gradual change (Re-entry vs. automaticity) • • • Sinus: gradual PSVT: sudden Atrial flutter: sudden AF: always changing, but sudden onset Ventricular tachycardia: Sudden
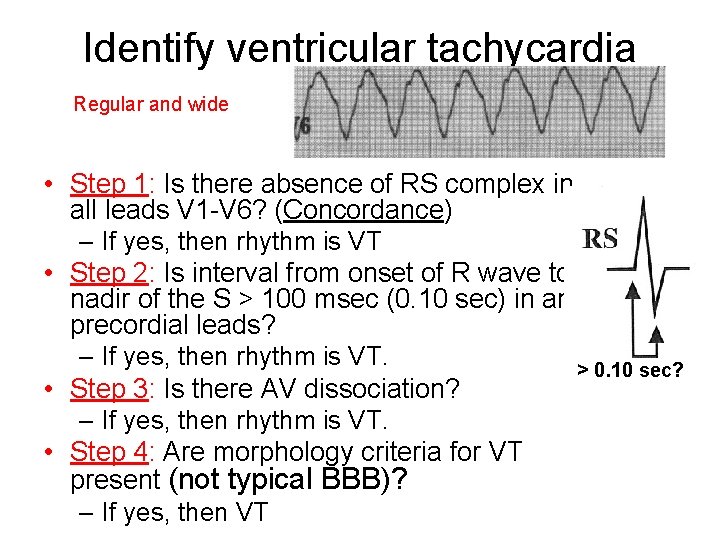
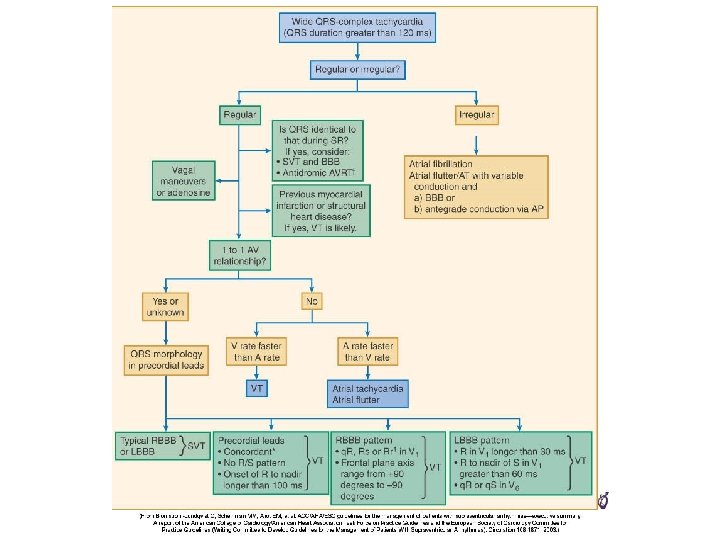
Identify ventricular tachycardia Regular and wide • Step 1: Is there absence of RS complex in all leads V 1 -V 6? (Concordance) – If yes, then rhythm is VT • Step 2: Is interval from onset of R wave to nadir of the S > 100 msec (0. 10 sec) in any precordial leads? – If yes, then rhythm is VT. > 0. 10 sec? • Step 3: Is there AV dissociation? – If yes, then rhythm is VT. • Step 4: Are morphology criteria for VT present (not typical BBB)? – If yes, then VT
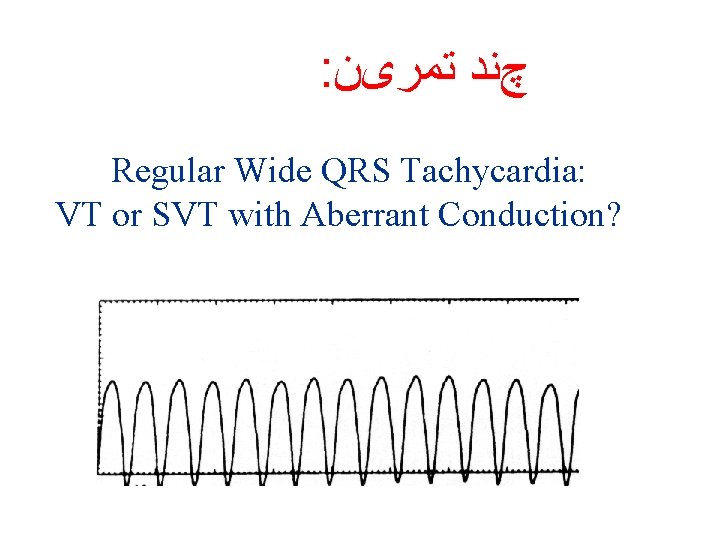
: چﻨﺪ ﺗﻤﺮیﻦ Regular Wide QRS Tachycardia: VT or SVT with Aberrant Conduction?
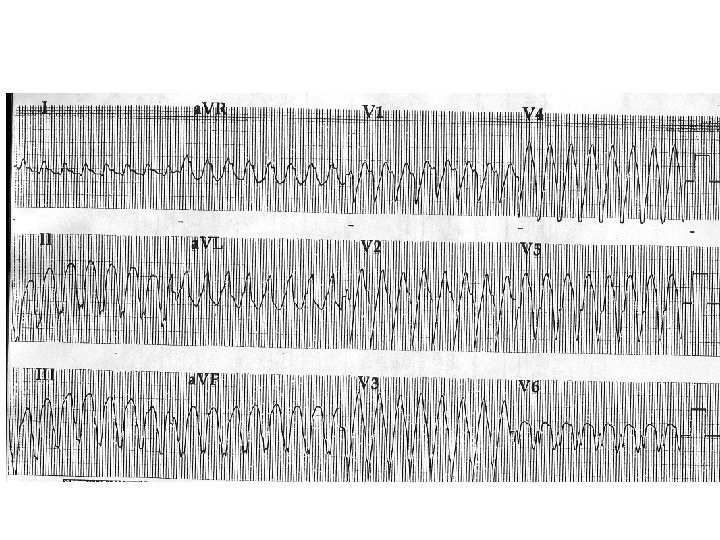
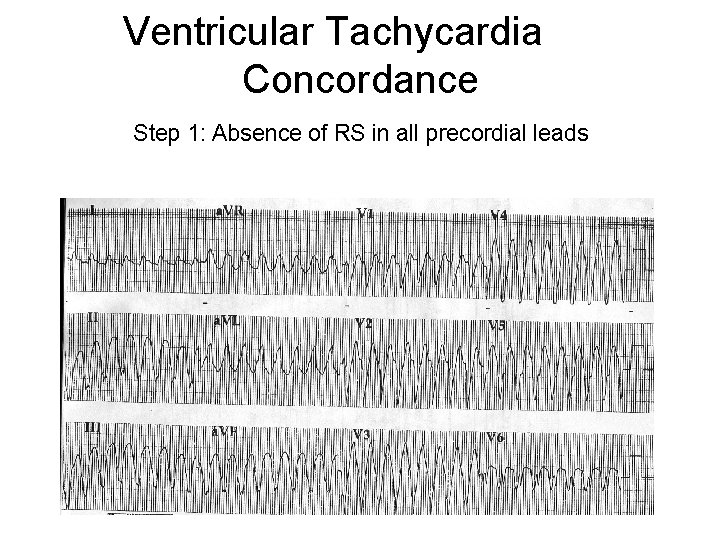
Ventricular Tachycardia Concordance Step 1: Absence of RS in all precordial leads
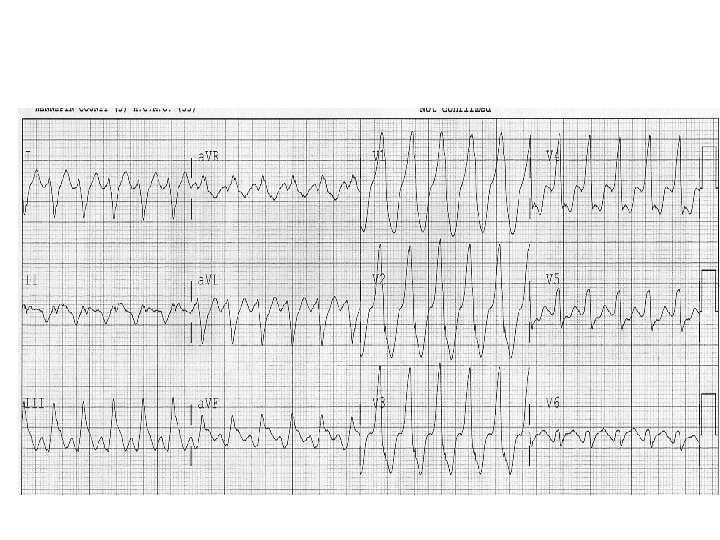
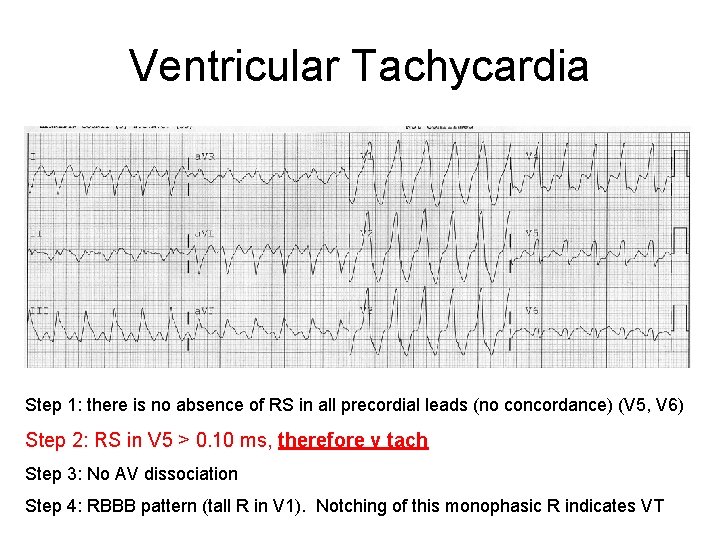
Ventricular Tachycardia Step 1: there is no absence of RS in all precordial leads (no concordance) (V 5, V 6) Step 2: RS in V 5 > 0. 10 ms, therefore v tach Step 3: No AV dissociation Step 4: RBBB pattern (tall R in V 1). Notching of this monophasic R indicates VT
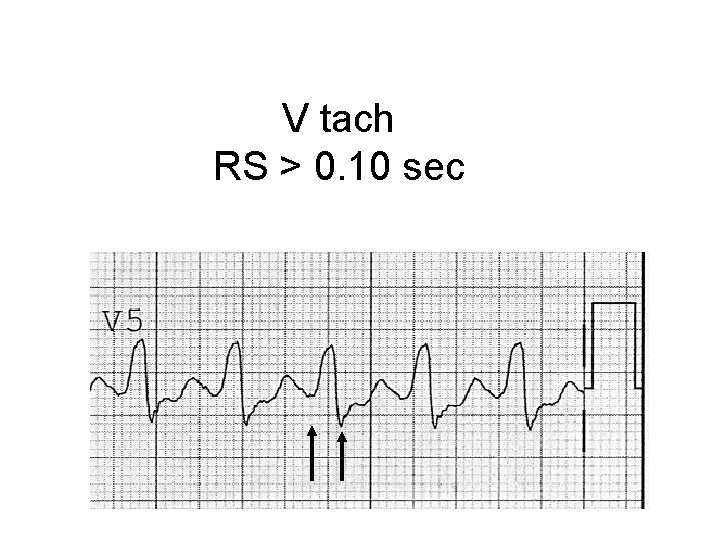
V tach RS > 0. 10 sec
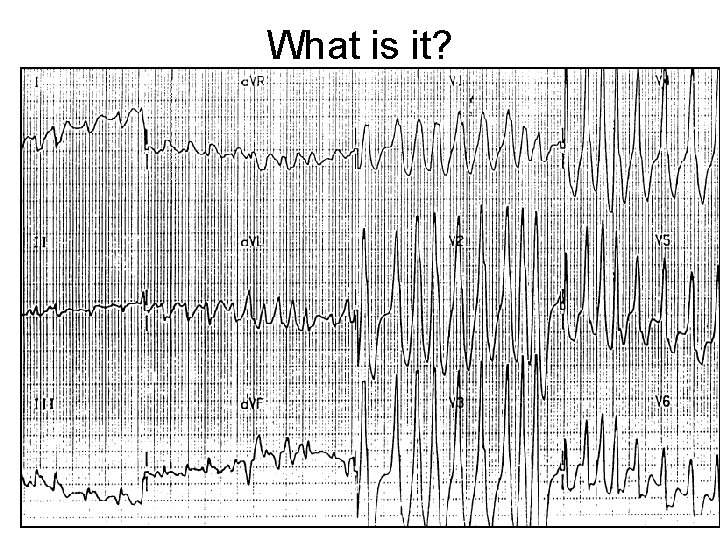
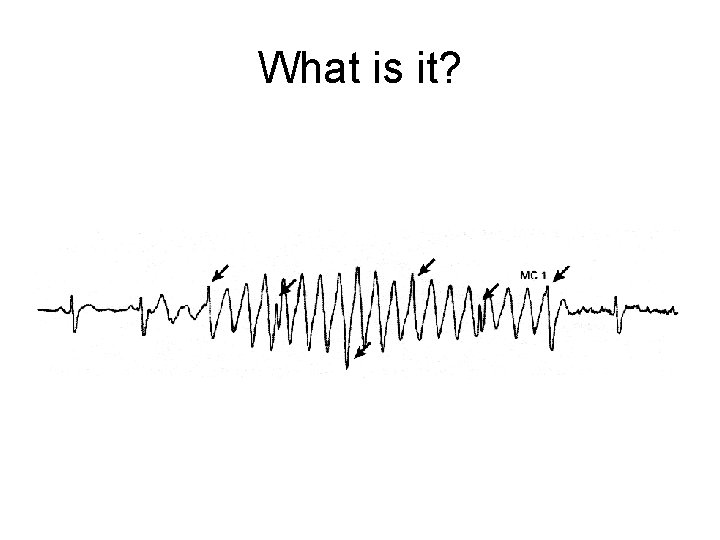
What is it?
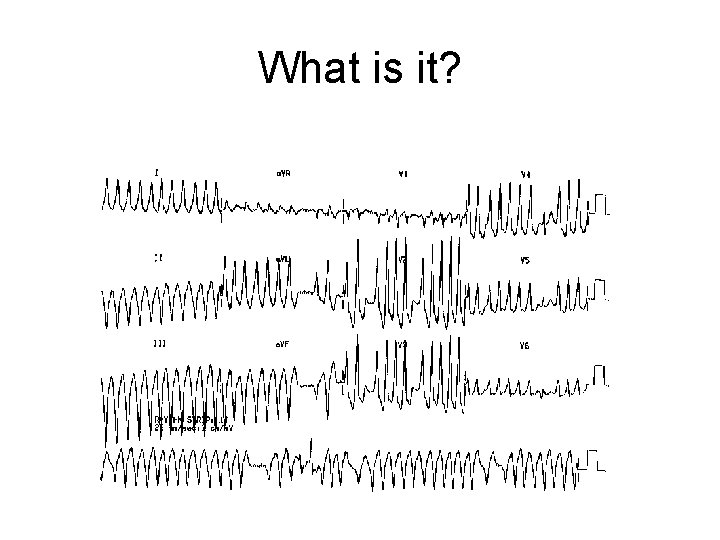
What is it?
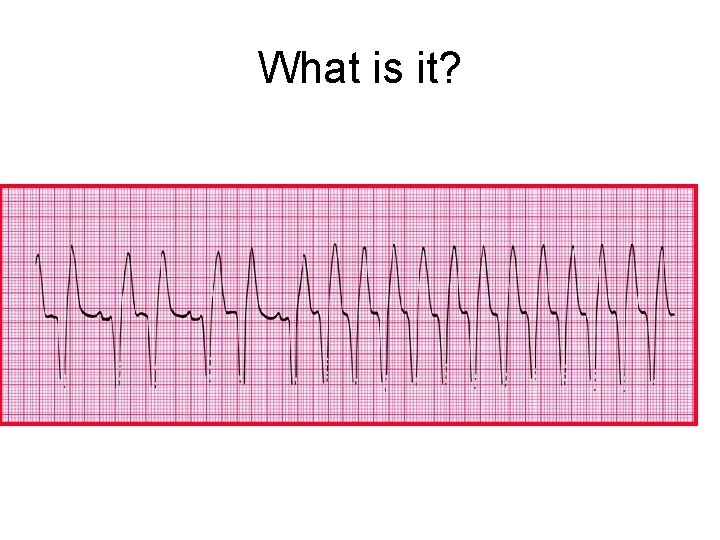
What is it?
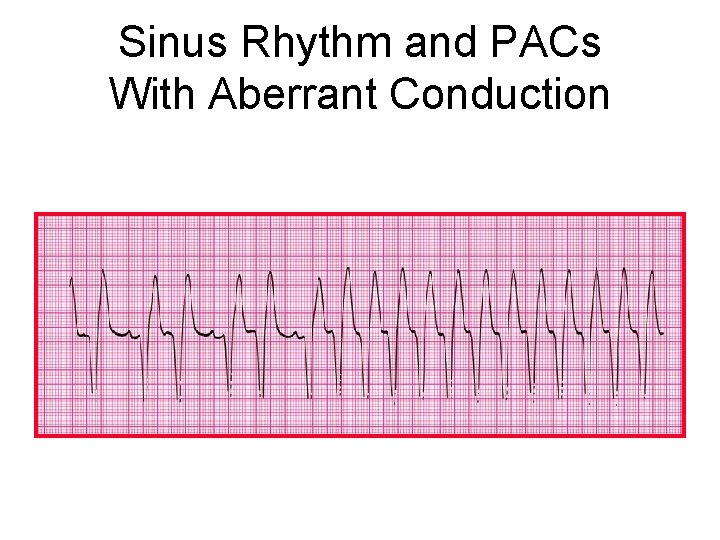
Sinus Rhythm and PACs With Aberrant Conduction
What is it?
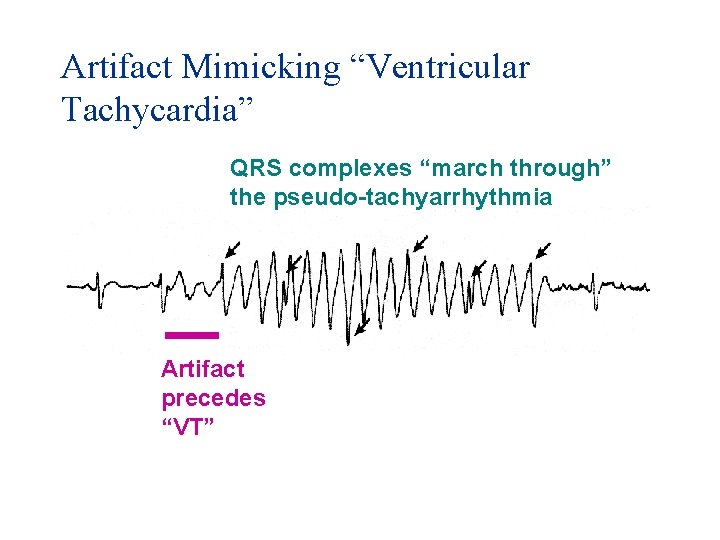
Artifact Mimicking “Ventricular Tachycardia” QRS complexes “march through” the pseudo-tachyarrhythmia Artifact precedes “VT”
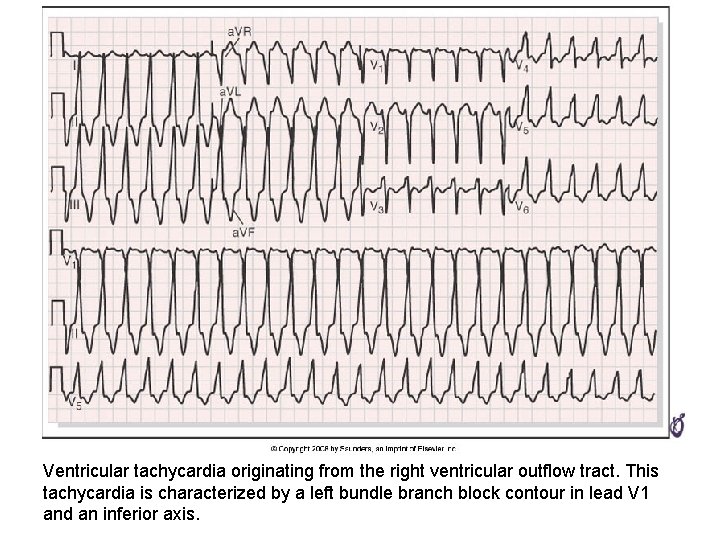
Ventricular tachycardia originating from the right ventricular outflow tract. This tachycardia is characterized by a left bundle branch block contour in lead V 1 and an inferior axis.
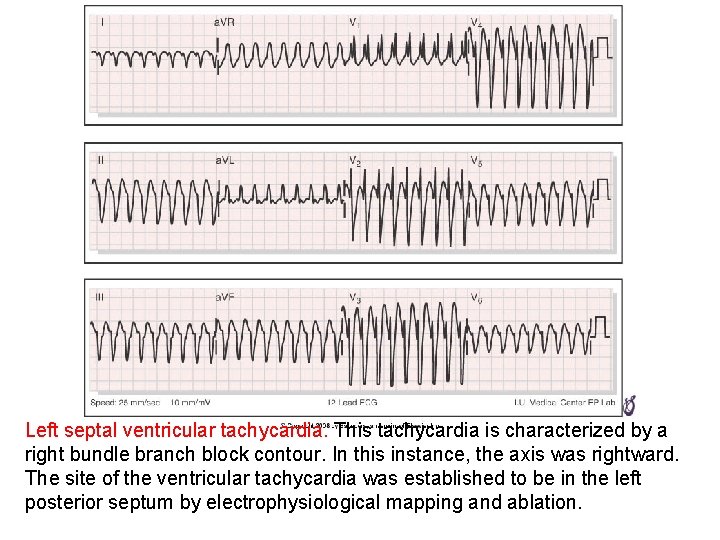
Left septal ventricular tachycardia. This tachycardia is characterized by a right bundle branch block contour. In this instance, the axis was rightward. The site of the ventricular tachycardia was established to be in the left posterior septum by electrophysiological mapping and ablation.
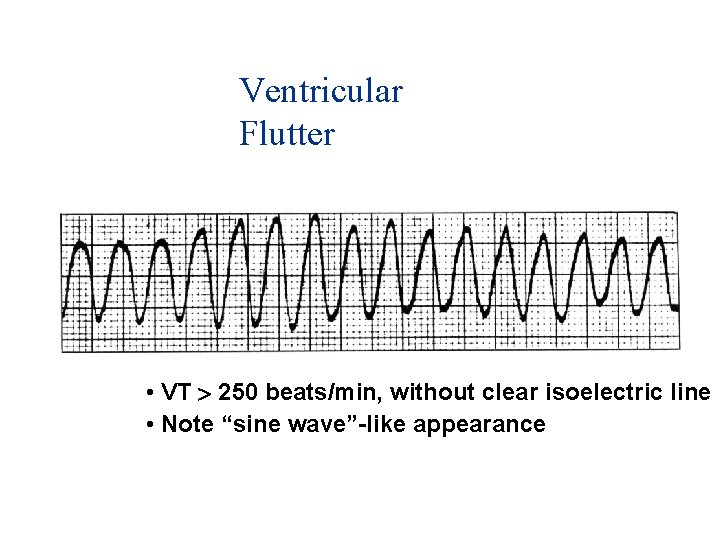
Ventricular Flutter • VT 250 beats/min, without clear isoelectric line • Note “sine wave”-like appearance
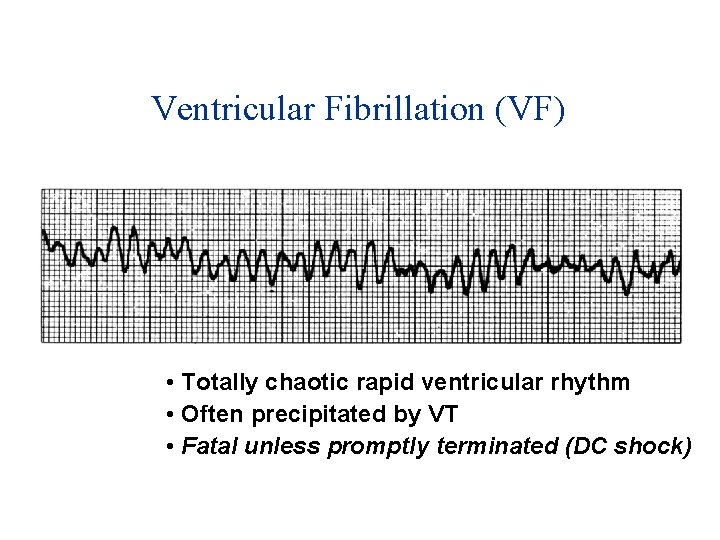
Ventricular Fibrillation (VF) • Totally chaotic rapid ventricular rhythm • Often precipitated by VT • Fatal unless promptly terminated (DC shock)
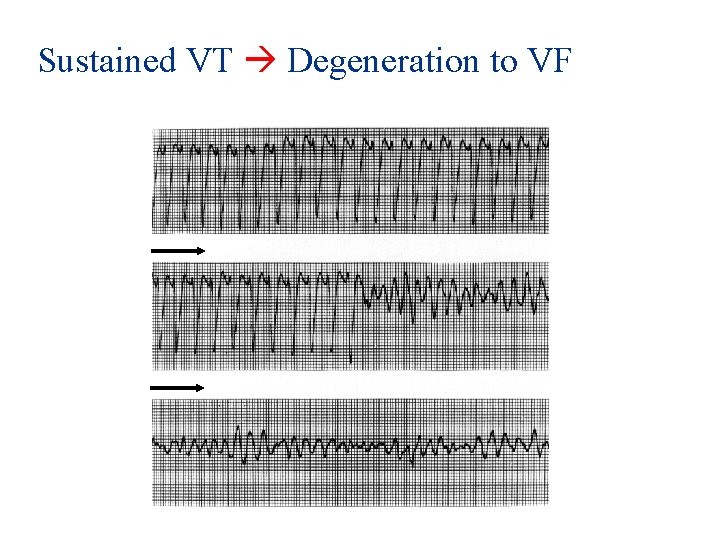
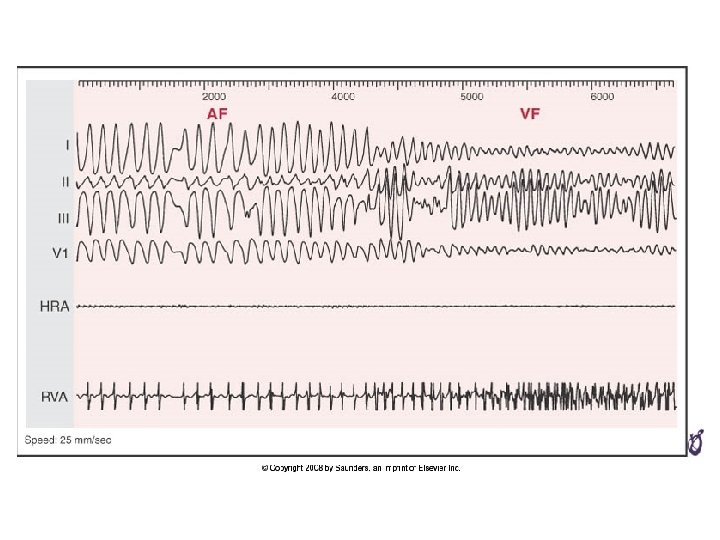
Sustained VT Degeneration to VF
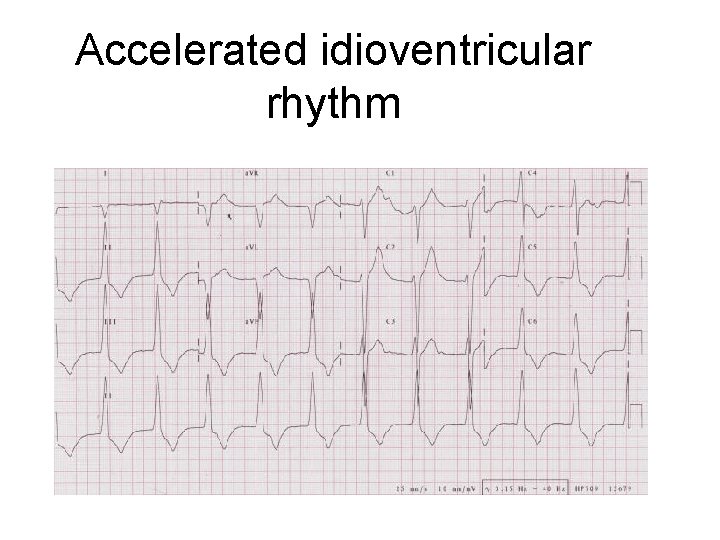
Accelerated idioventricular rhythm
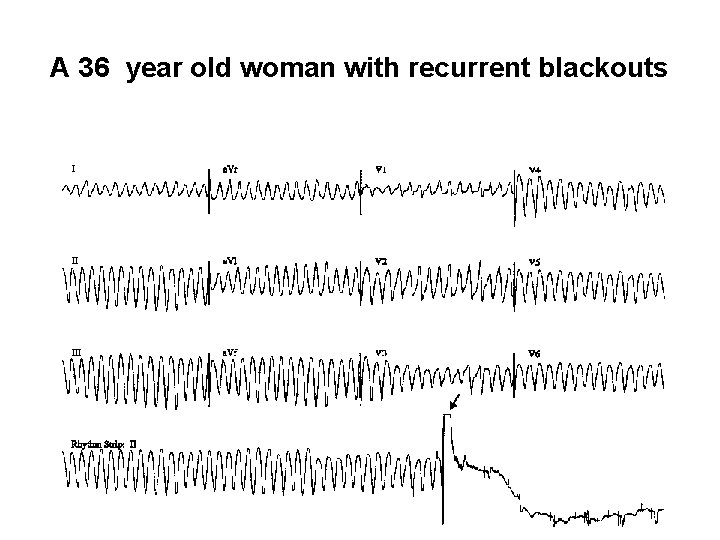
A 36 year old woman with recurrent blackouts

Rx
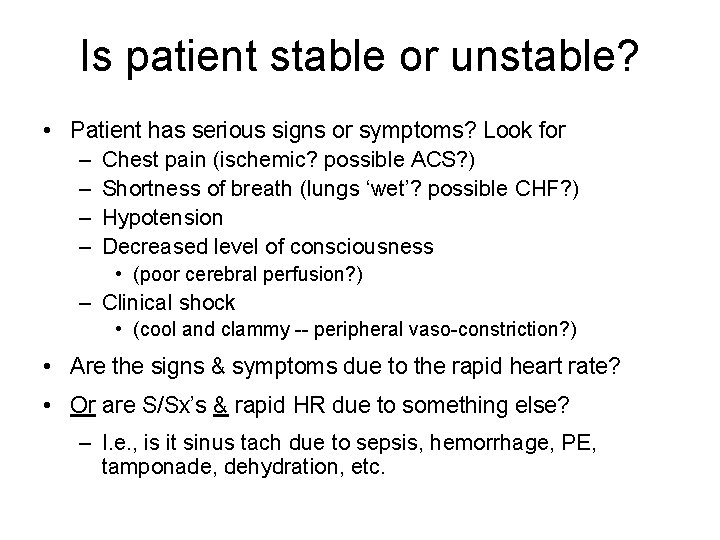
Is patient stable or unstable? • Patient has serious signs or symptoms? Look for – Chest pain (ischemic? possible ACS? ) – Shortness of breath (lungs ‘wet’? possible CHF? ) – Hypotension – Decreased level of consciousness • (poor cerebral perfusion? ) – Clinical shock • (cool and clammy -- peripheral vaso-constriction? ) • Are the signs & symptoms due to the rapid heart rate? • Or are S/Sx’s & rapid HR due to something else? – I. e. , is it sinus tach due to sepsis, hemorrhage, PE, tamponade, dehydration, etc.
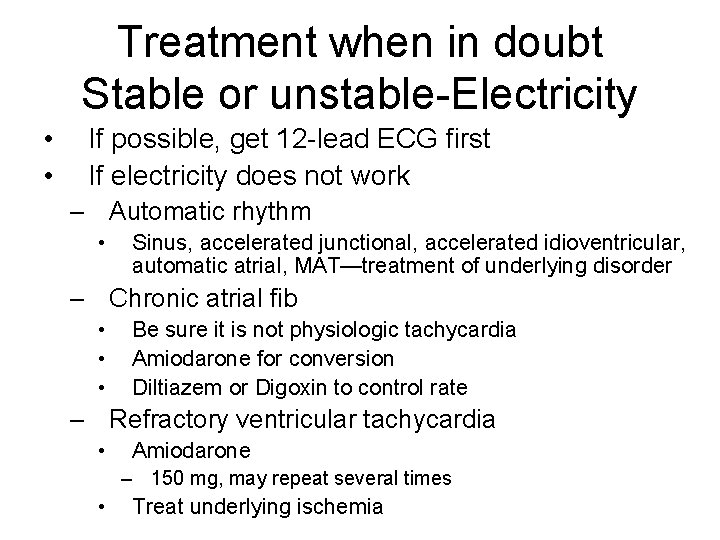
Treatment when in doubt Stable or unstable-Electricity • • If possible, get 12 -lead ECG first If electricity does not work – Automatic rhythm • Sinus, accelerated junctional, accelerated idioventricular, automatic atrial, MAT—treatment of underlying disorder – Chronic atrial fib • • • Be sure it is not physiologic tachycardia Amiodarone for conversion Diltiazem or Digoxin to control rate – Refractory ventricular tachycardia • Amiodarone – 150 mg, may repeat several times • Treat underlying ischemia
Conclusion: When in doubt • Shock a fast rhythm • Pace a slow rhythm • In anterior STEMI – Be certain that transcutaneous pacing will capture if there is high grade block • But don’t shock sinus tachycardia!!
- Slides: 106