Palliative Care in Long Term Care Facilities the





- Slides: 50
Palliative Care in Long Term Care Facilities: the EU PACE Project Professor Katherine Froggatt Elley Sowerby International Observatory on End of Life Care Lancaster University www. eupace. eu @fp 7 PACE

Acknowledgement This project has received funding from the European Union’s Seventh Framework Programme for research, technological development and demonstration under grant agreement no. 603111. 2
What experience and questions do you bring today?
EU FP 7 PACE: Palliative care in care and nursing homes in six EU countries Palliative care in LTCFs PACE study I PACE Steps to Success intervention 4
Palliative care in LTCFs PACE study I PACE Steps to Success intervention 5
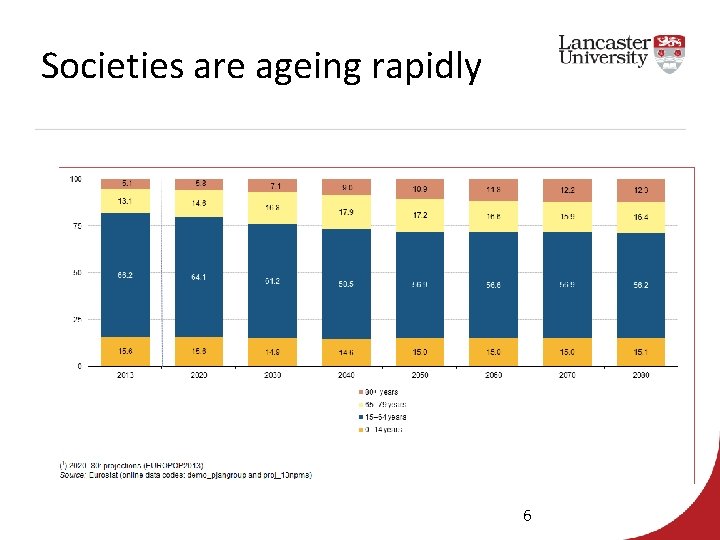
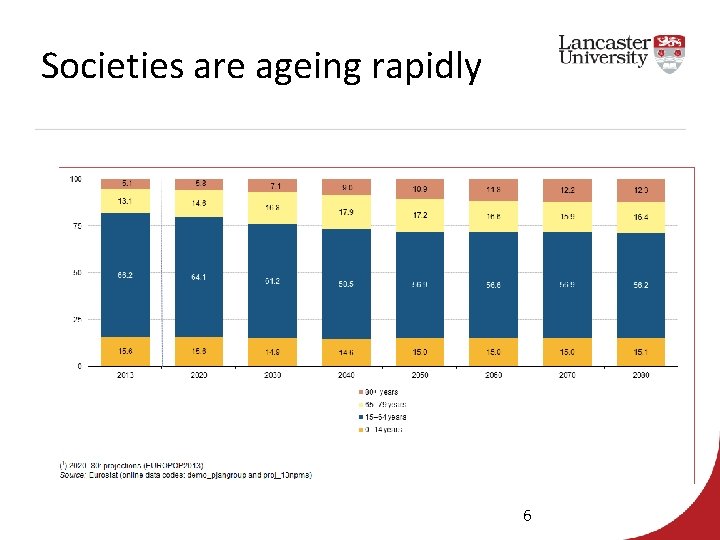
Societies are ageing rapidly 6
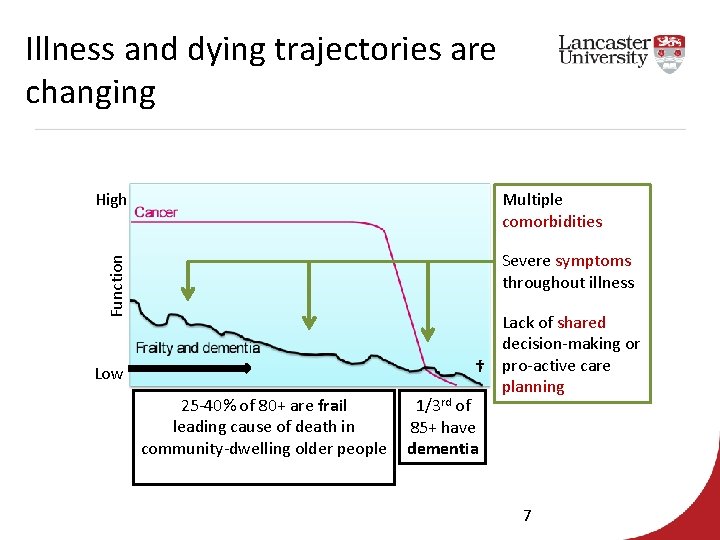
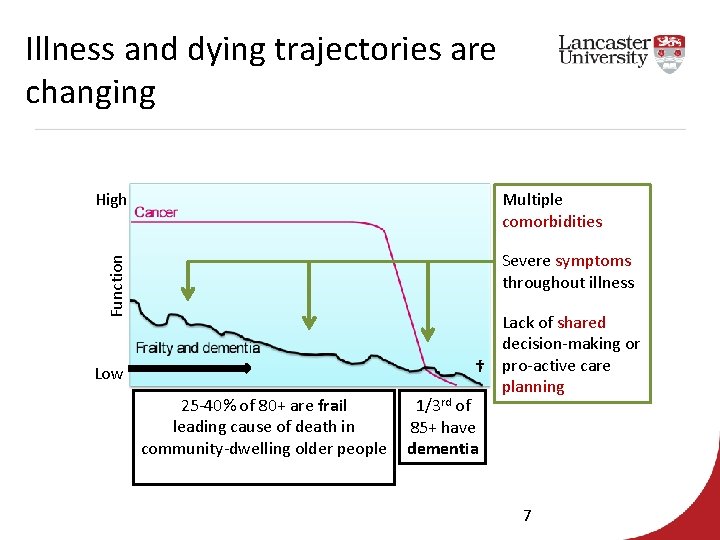
Illness and dying trajectories are changing High Multiple comorbidities Function Severe symptoms throughout illness Low 25 -40% of 80+ are frail leading cause of death in community-dwelling older people Lack of shared decision-making or † pro-active care planning 1/3 rd of 85+ have dementia 7
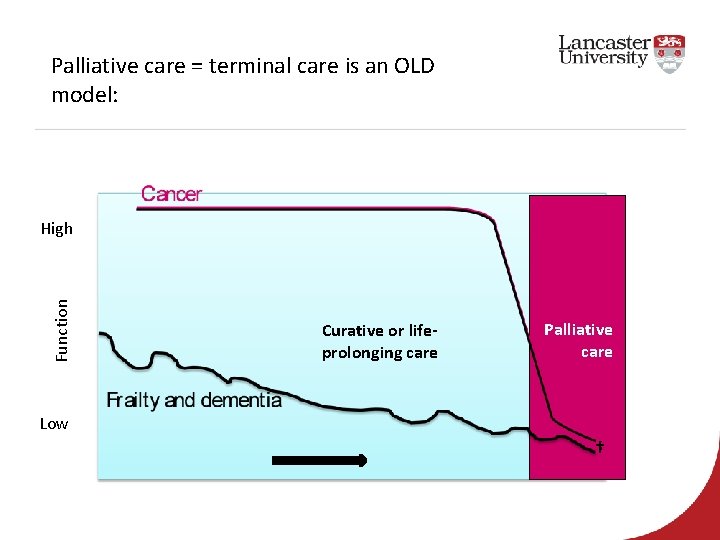
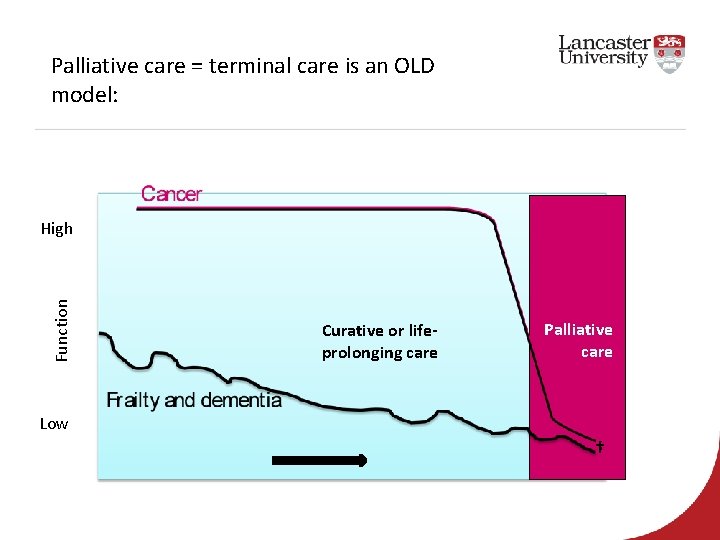
Palliative care = terminal care is an OLD model: Function High Curative or lifeprolonging care Palliative care Low †
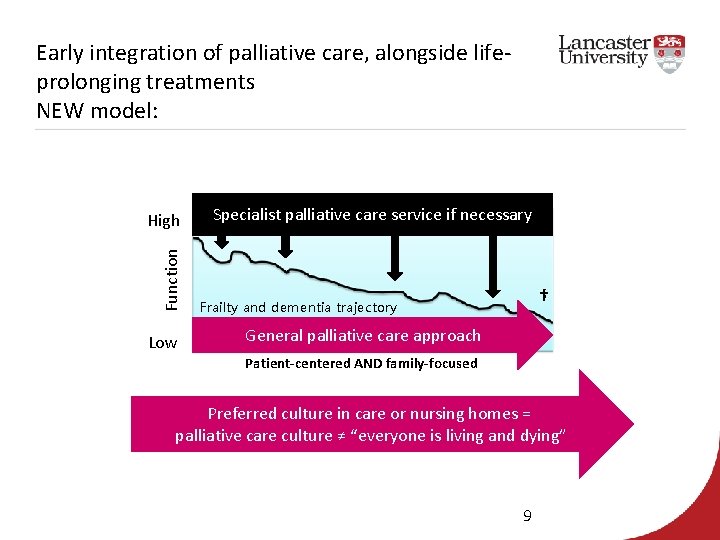
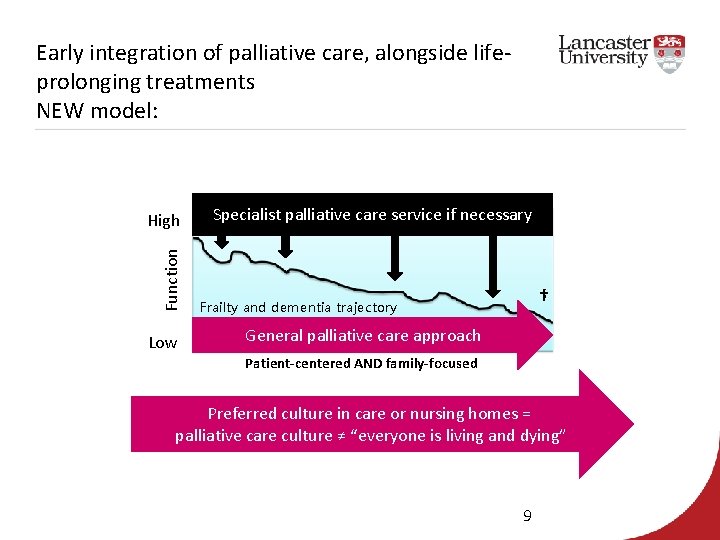
Early integration of palliative care, alongside lifeprolonging treatments NEW model: Function High Low Specialist palliative care service if necessary † Frailty and dementia trajectory General palliative care approach Patient-centered AND family-focused Preferred culture in care or nursing homes = palliative care culture ≠ “everyone is living and dying” 9
Palliative Care Palliative care for frail older people is defined as: • an active, compassionate approach that treats, comforts and supports • older individuals who are living with, or dying from, progressive or chronic life-threatening conditions. Focuses on • personal (physical, psychological), cultural and spiritual domains • encompasses support for families and friends • over time - up to and including the period of bereavement (Fisher et al, 2000)
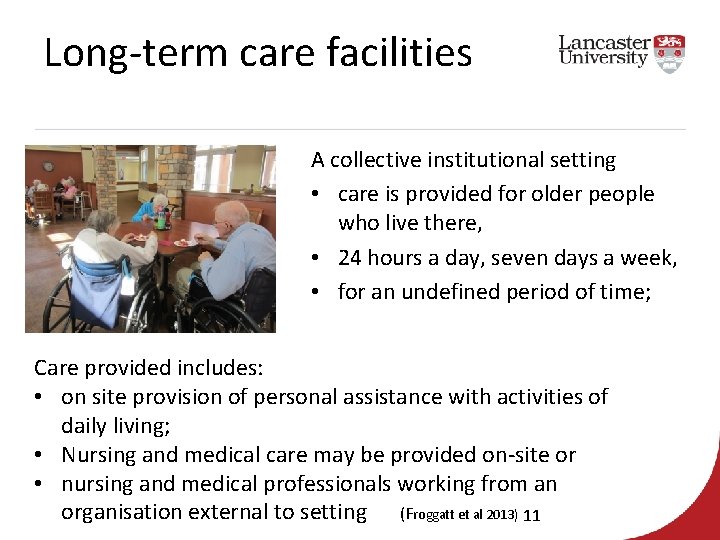
Long-term care facilities A collective institutional setting • care is provided for older people who live there, • 24 hours a day, seven days a week, • for an undefined period of time; Care provided includes: • on site provision of personal assistance with activities of daily living; • Nursing and medical care may be provided on-site or • nursing and medical professionals working from an organisation external to setting (Froggatt et al 2013) 11
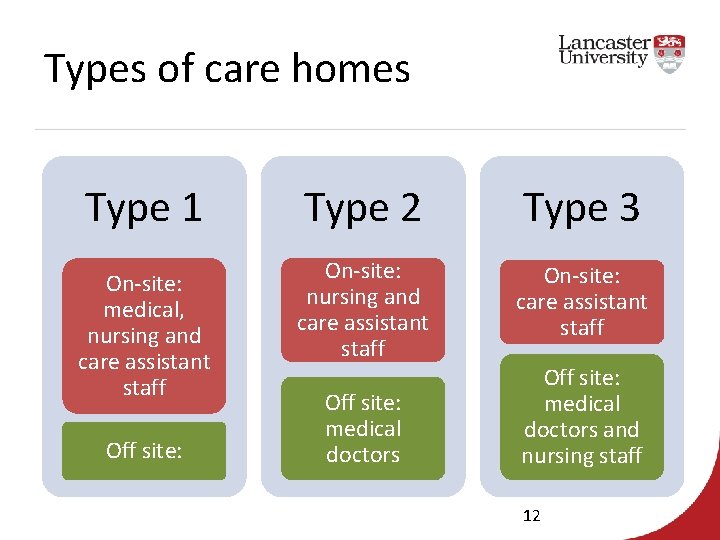
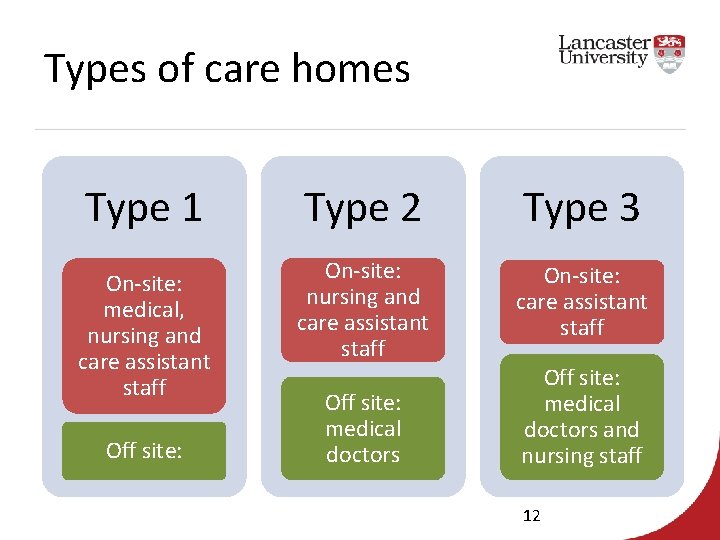
Types of care homes Type 1 On-site: medical, nursing and care assistant staff Off site: Type 2 Type 3 On-site: nursing and care assistant staff On-site: care assistant staff Off site: medical doctors and nursing staff 12
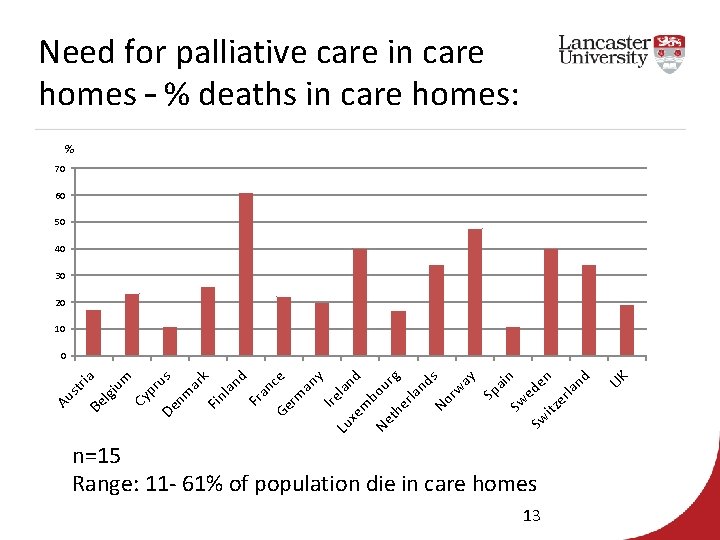
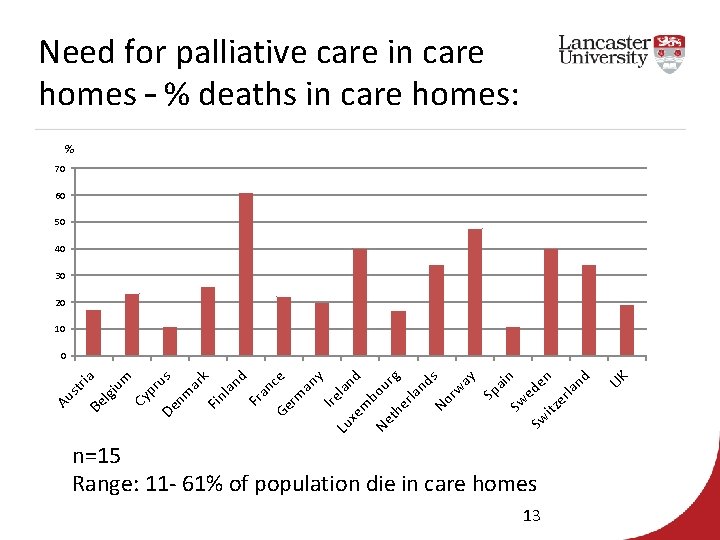
Need for palliative care in care homes – % deaths in care homes: % 70 60 50 40 30 20 10 Au n=15 Range: 11 - 61% of population die in care homes 13 UK st ria Be lgi um Cy pr De us nm ar k Fin la nd Fr an Ge ce rm an y Ire la Lu nd xe m b Ne ou rg th er la nd No s rw ay Sp ai Sw n Sw ede itz n er la nd 0
Palliative care in LTCFs PACE study I PACE Steps to Success intervention 14
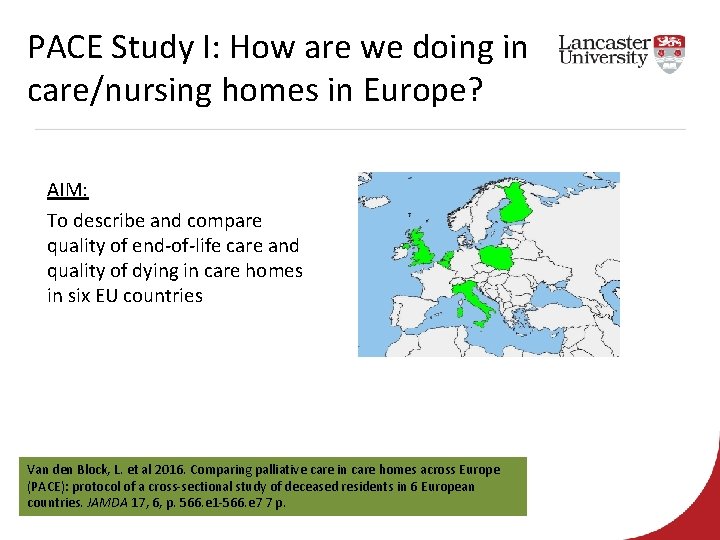
PACE Study I: How are we doing in care/nursing homes in Europe? AIM: To describe and compare quality of end-of-life care and quality of dying in care homes in six EU countries Van den Block, L. et al 2016. Comparing palliative care in care homes across Europe (PACE): protocol of a cross-sectional study of deceased residents in 6 European countries. JAMDA 17, 6, p. 566. e 1 -566. e 7 7 p.
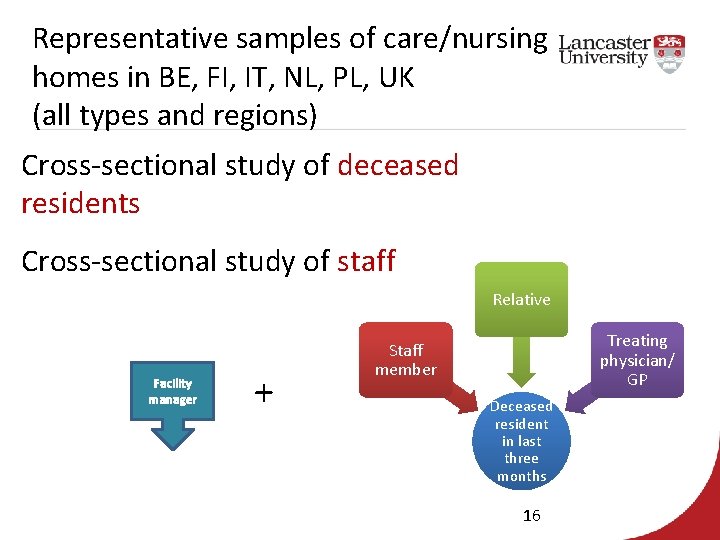
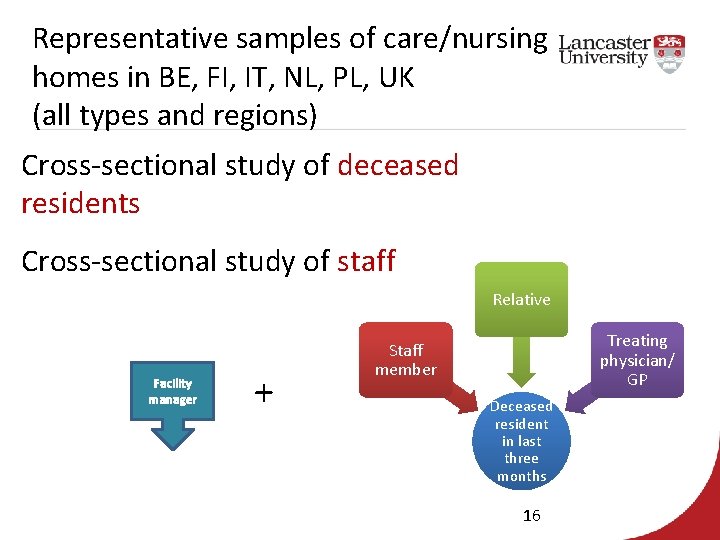
Representative samples of care/nursing homes in BE, FI, IT, NL, PL, UK (all types and regions) Cross-sectional study of deceased residents Cross-sectional study of staff Relative Facility manager + Treating physician/ GP Staff member Deceased resident in last three months 16
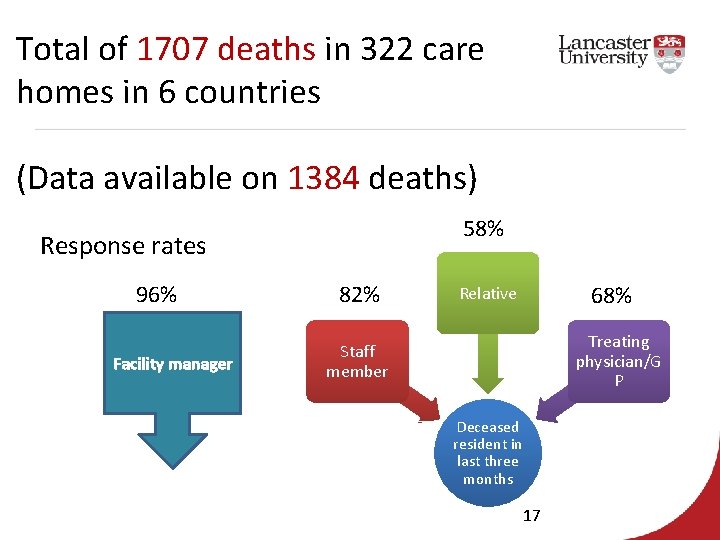
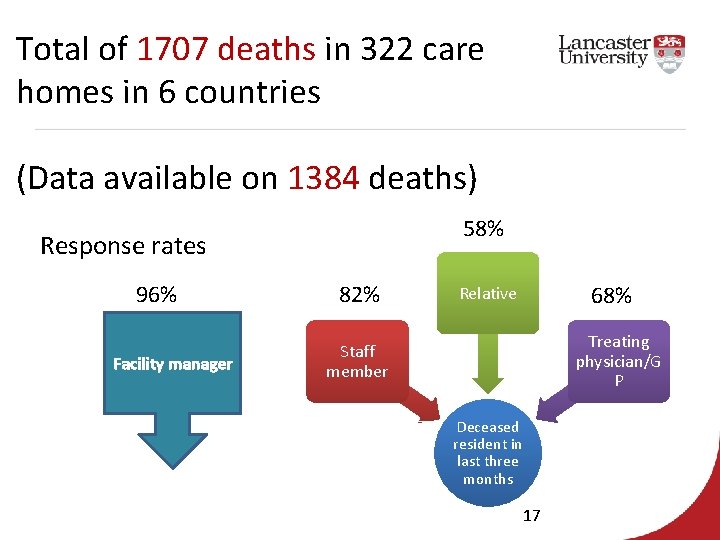
Total of 1707 deaths in 322 care homes in 6 countries (Data available on 1384 deaths) 58% Response rates 96% Facility manager 82% 68% Relative Treating physician/G P Staff member Deceased resident in last three months 17
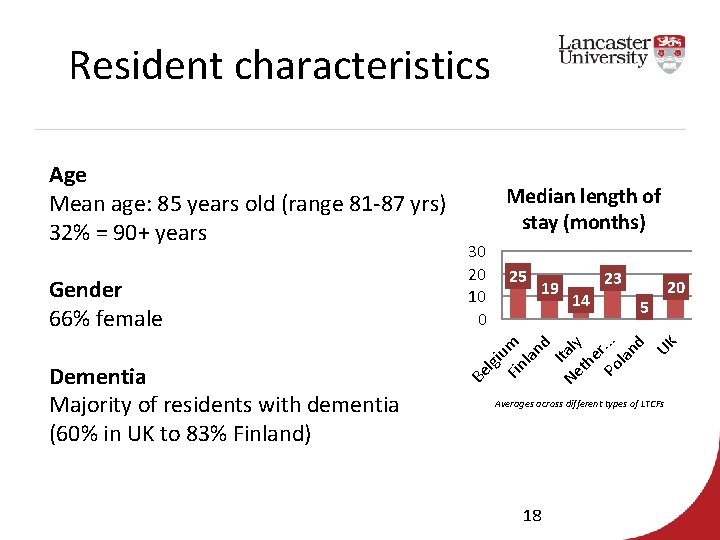
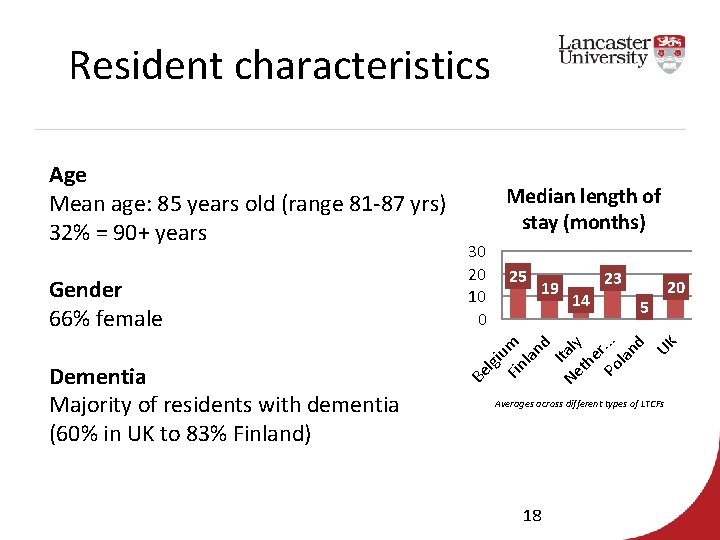
Resident characteristics 25 19 23 14 5 20 u Fin m la nd I Ne taly th er Po. . . la nd UK Dementia Majority of residents with dementia (60% in UK to 83% Finland) 30 20 10 0 lgi Gender 66% female Median length of stay (months) Be Age Mean age: 85 years old (range 81 -87 yrs) 32% = 90+ years Averages across different types of LTCFs 18
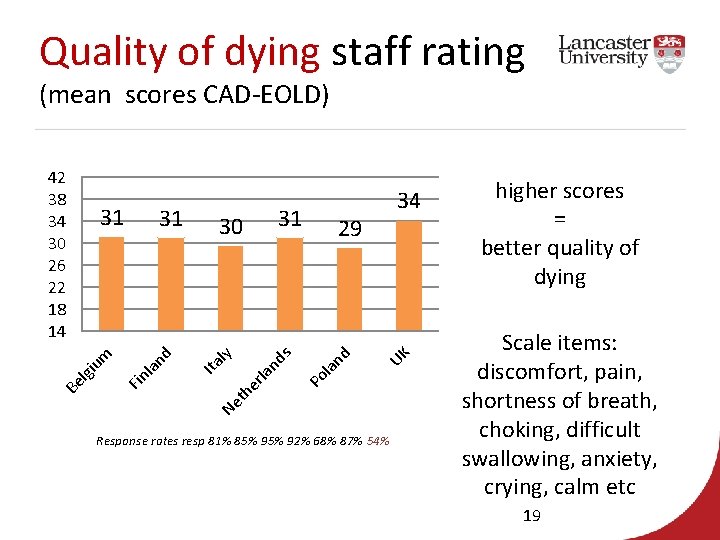
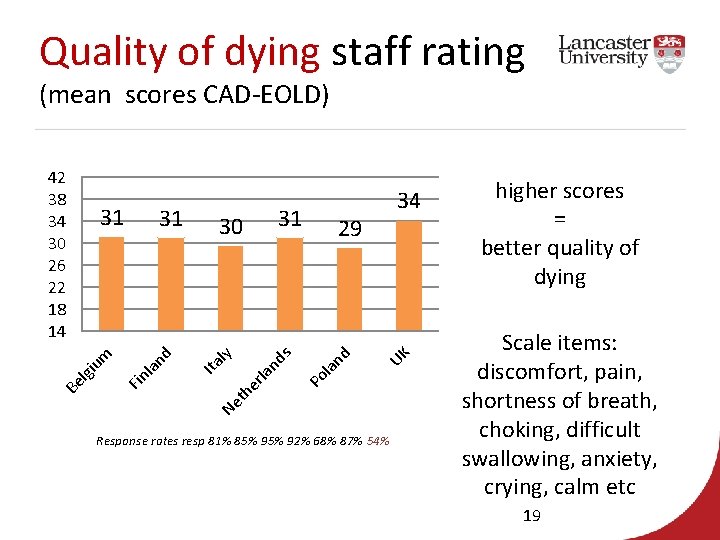
Quality of dying staff rating (mean scores CAD-EOLD) 31 34 UK la nd 29 Ne Po rla nd s 30 th e la nd 31 Fin Be lgi um 31 Ita ly 42 38 34 30 26 22 18 14 Response rates resp 81% 85% 92% 68% 87% 54% higher scores = better quality of dying Scale items: discomfort, pain, shortness of breath, choking, difficult swallowing, anxiety, crying, calm etc 19
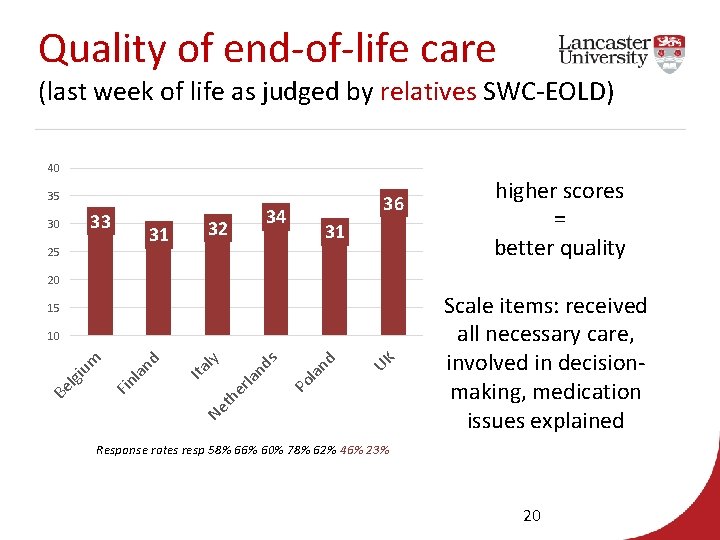
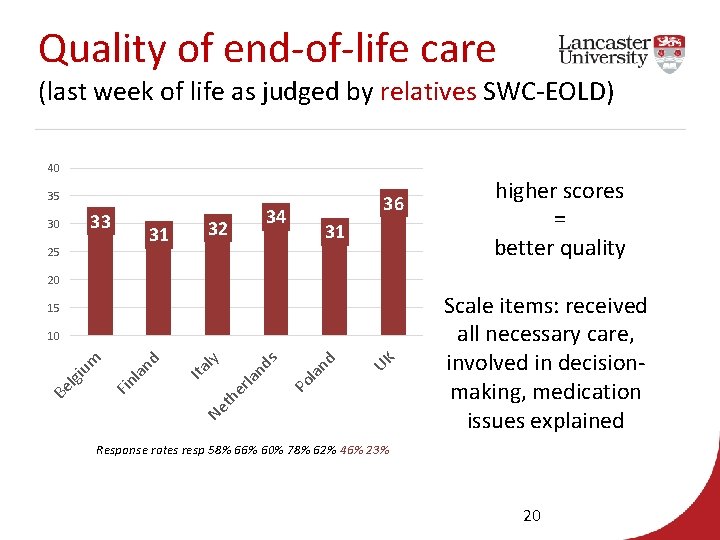
Quality of end-of-life care (last week of life as judged by relatives SWC-EOLD) 40 35 33 30 31 25 36 34 32 31 higher scores = better quality 20 15 UK la nd Po s nd rla Ne th e Ita ly la nd Fin Be lgi um 10 Scale items: received all necessary care, involved in decisionmaking, medication issues explained Response rates resp 58% 66% 60% 78% 62% 46% 23% 20
Primary care involvement? Sample n=1132 GPs/treating physicians (Response rate: 68% - range 23. 8% - 88. 4%) 21
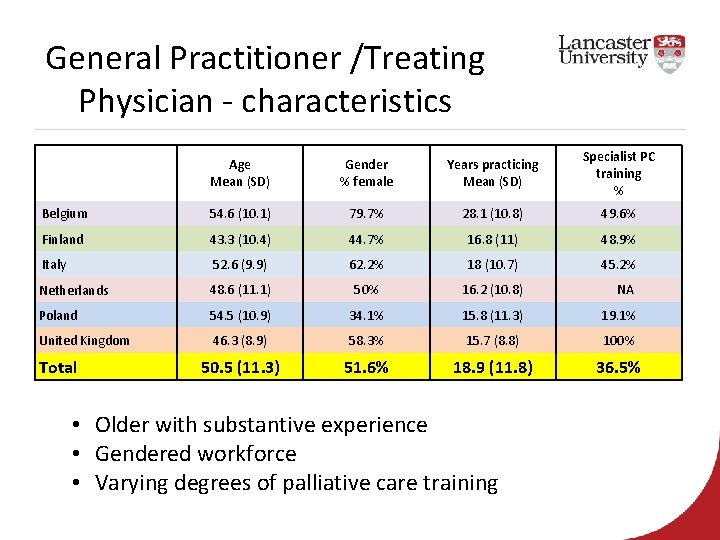
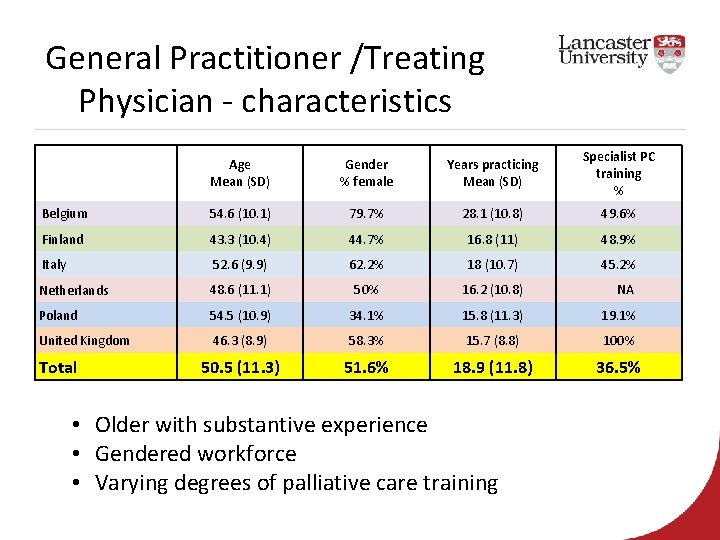
General Practitioner /Treating Physician - characteristics Age Mean (SD) Gender % female Years practicing Mean (SD) Specialist PC training % Belgium 54. 6 (10. 1) 79. 7% 28. 1 (10. 8) 49. 6% Finland 43. 3 (10. 4) 44. 7% 16. 8 (11) 48. 9% Italy 52. 6 (9. 9) 62. 2% 18 (10. 7) 45. 2% Netherlands 48. 6 (11. 1) 50% 16. 2 (10. 8) NA Poland 54. 5 (10. 9) 34. 1% 15. 8 (11. 3) 19. 1% United Kingdom 46. 3 (8. 9) 58. 3% 15. 7 (8. 8) 100% 50. 5 (11. 3) 51. 6% 18. 9 (11. 8) 36. 5% Total • Older with substantive experience • Gendered workforce • Varying degrees of palliative care training
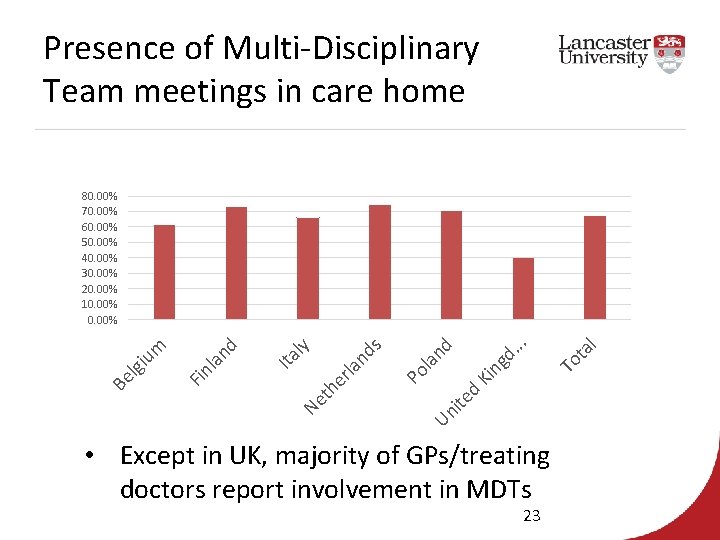
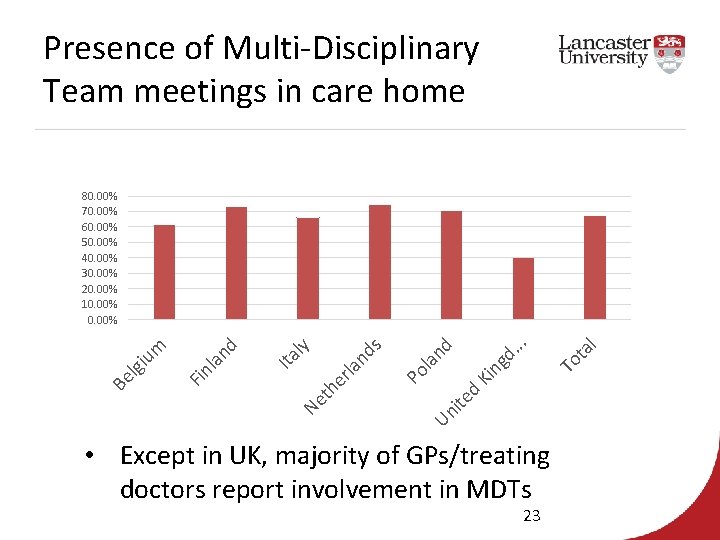
Presence of Multi-Disciplinary Team meetings in care home ot al U ni te d K T in gd. . . ol an d la he r et N P nd s ly Ita nd Fin la Be lgi um 80. 00% 70. 00% 60. 00% 50. 00% 40. 00% 30. 00% 20. 00% 10. 00% • Except in UK, majority of GPs/treating doctors report involvement in MDTs 23
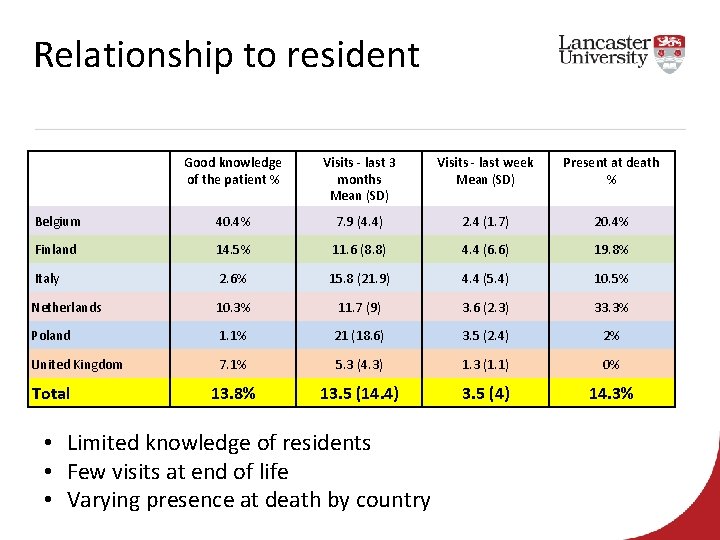
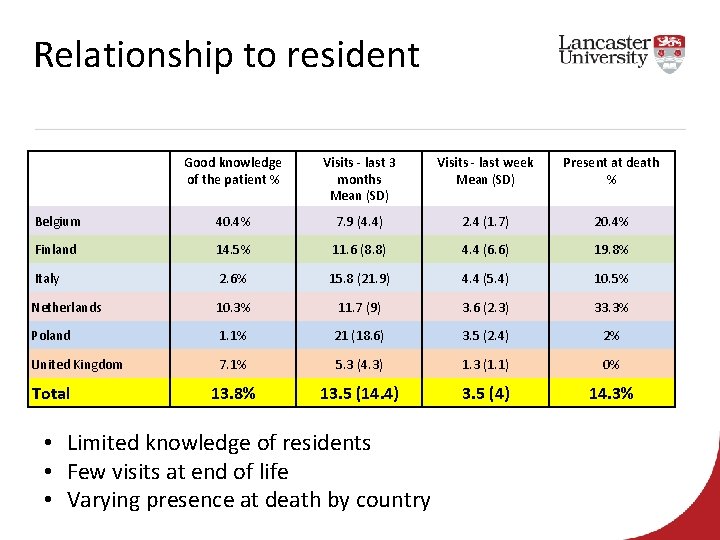
Relationship to resident Good knowledge of the patient % Visits - last 3 months Mean (SD) Visits - last week Mean (SD) Present at death % Belgium 40. 4% 7. 9 (4. 4) 2. 4 (1. 7) 20. 4% Finland 14. 5% 11. 6 (8. 8) 4. 4 (6. 6) 19. 8% Italy 2. 6% 15. 8 (21. 9) 4. 4 (5. 4) 10. 5% Netherlands 10. 3% 11. 7 (9) 3. 6 (2. 3) 33. 3% Poland 1. 1% 21 (18. 6) 3. 5 (2. 4) 2% United Kingdom 7. 1% 5. 3 (4. 3) 1. 3 (1. 1) 0% 13. 8% 13. 5 (14. 4) 3. 5 (4) 14. 3% Total • Limited knowledge of residents • Few visits at end of life • Varying presence at death by country
Any questions?
Palliative care in LTCFs PACE study I PACE Steps to Success intervention 26
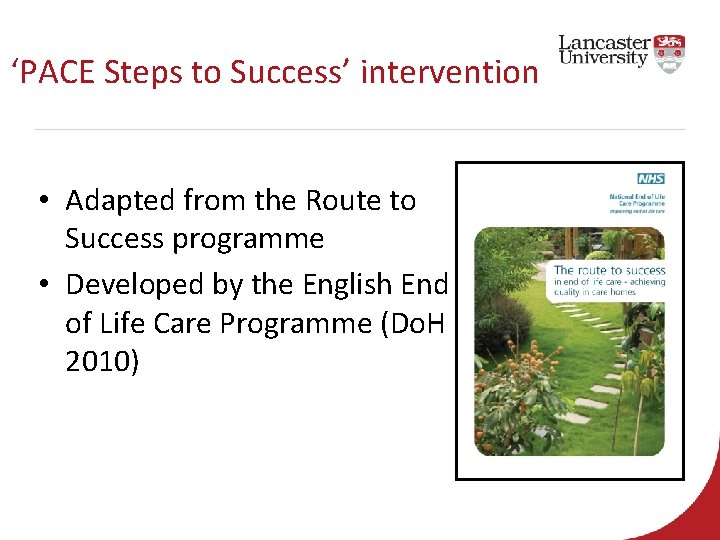
‘PACE Steps to Success’ intervention • Adapted from the Route to Success programme • Developed by the English End of Life Care Programme (Do. H 2010)
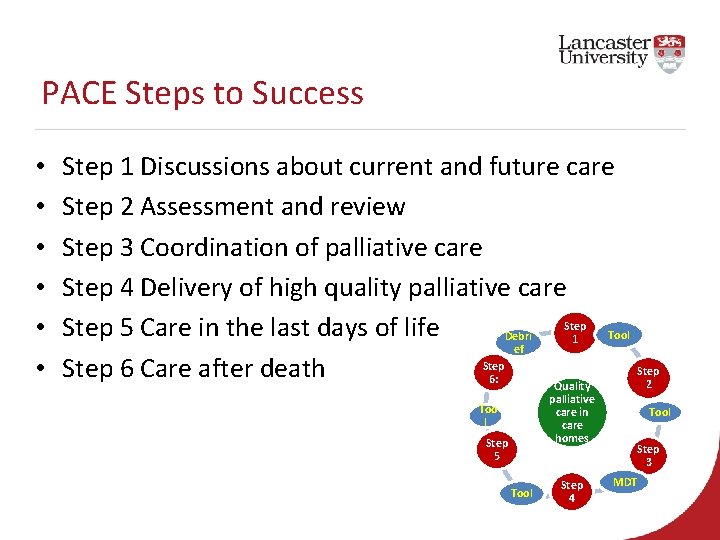
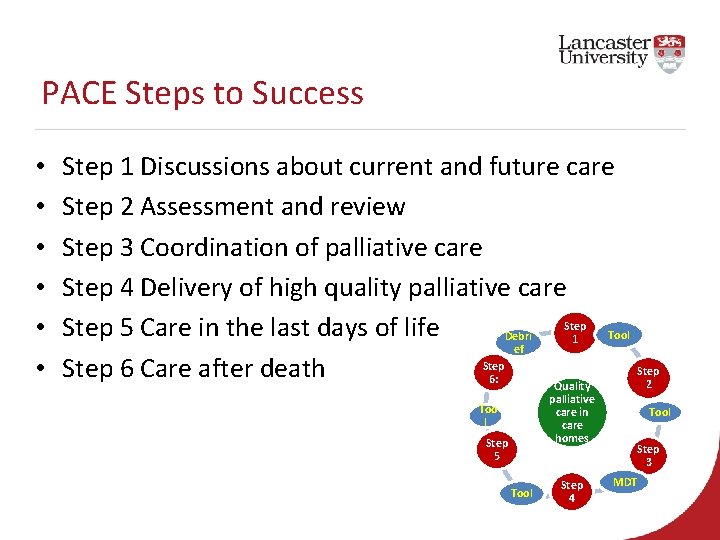
PACE Steps to Success • • • Step 1 Discussions about current and future care Step 2 Assessment and review Step 3 Coordination of palliative care Step 4 Delivery of high quality palliative care Step 5 Care in the last days of life Tool Debri 1 ef Step 6 Care after death 6: 2 Quality palliative care in care homes Too l Step 5 Tool Step 4 Tool Step 3 MDT
Who is involved? • • • Country trainer Facility manager Facility PACE Coordinators Facility care staff GPs Families 29

Country Trainers • 1 -3 trainers per country • Experience in palliative care/ geriatrics/ LTCFs • Nurses, doctors, psychologists • Supported by International Trainer 30
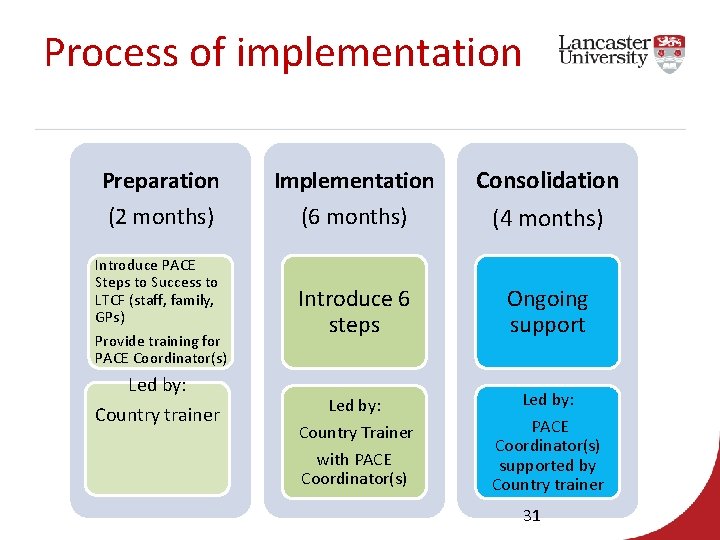
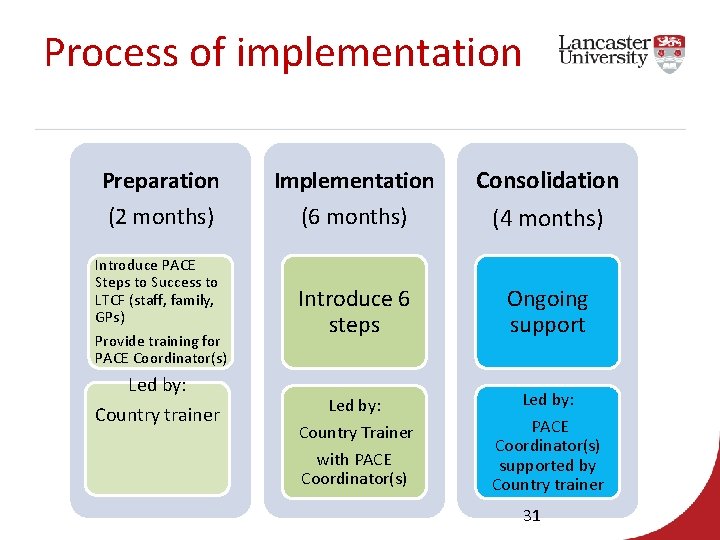
Process of implementation Preparation (2 months) Implementation (6 months) Consolidation (4 months) Introduce PACE Steps to Success to LTCF (staff, family, GPs) Provide training for PACE Coordinator(s) Introduce 6 steps Ongoing support Led by: Country Trainer Led by: Country trainer with PACE Coordinator(s) supported by Country trainer 31

Step 1 – Current and future care Action: Conversations held with residents about their views and preferences for current and future care.
Tool: ‘Looking and thinking ahead’ document
Resource Looking and thinking ahead discussions
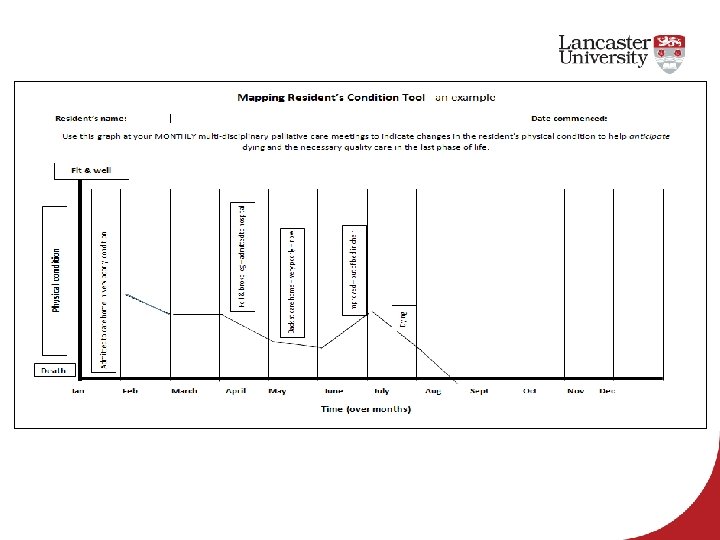
Step 2 – Assessment & Review Action: Review each resident to consider their condition and record any ongoing changes
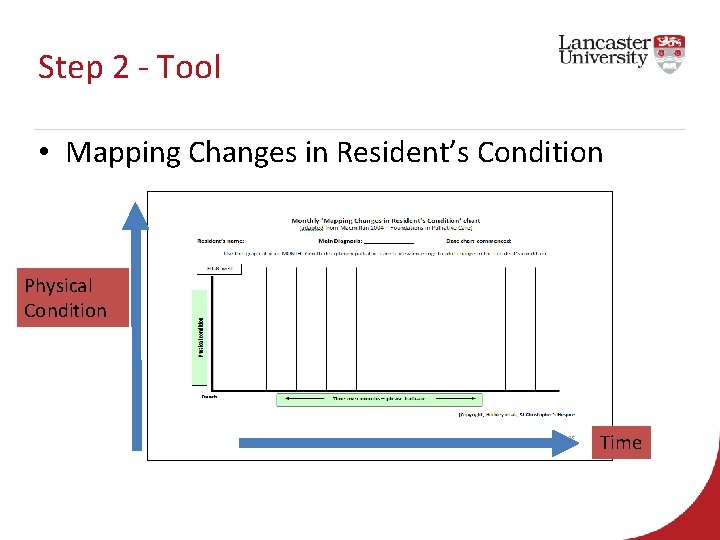
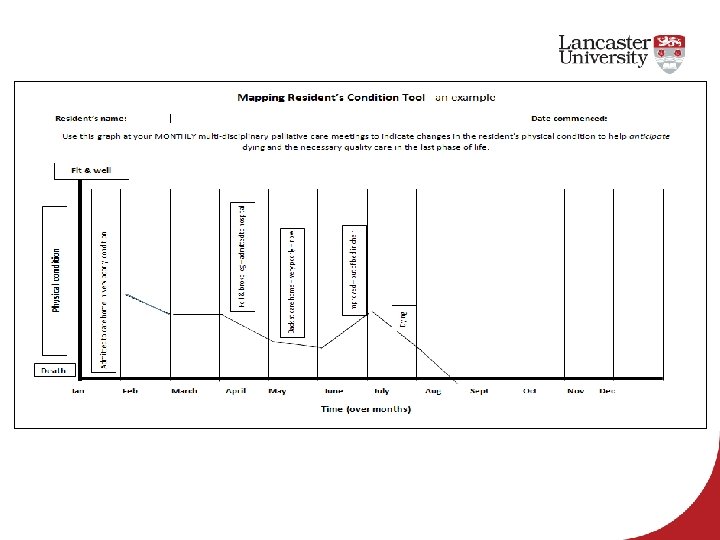
Step 2 - Tool • Mapping Changes in Resident’s Condition Physical Condition Time

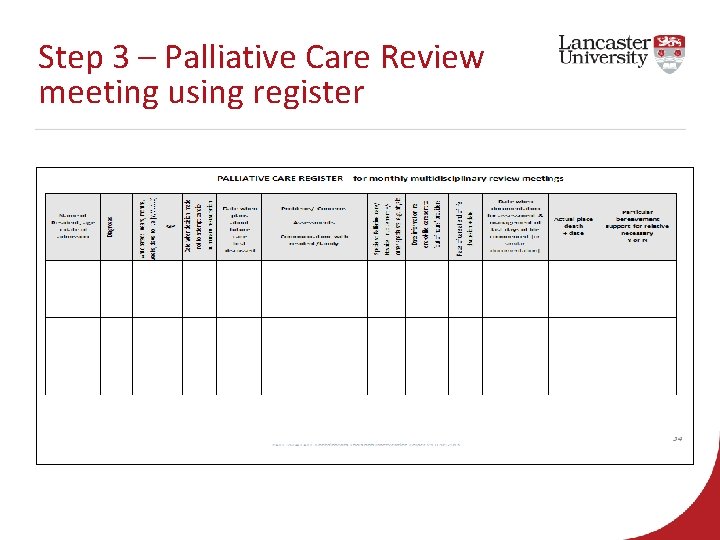
Step 3: Good Coordination of Palliative Care Action: A monthly multi-disciplinary team meeting focusing on the palliative care needs of all residents
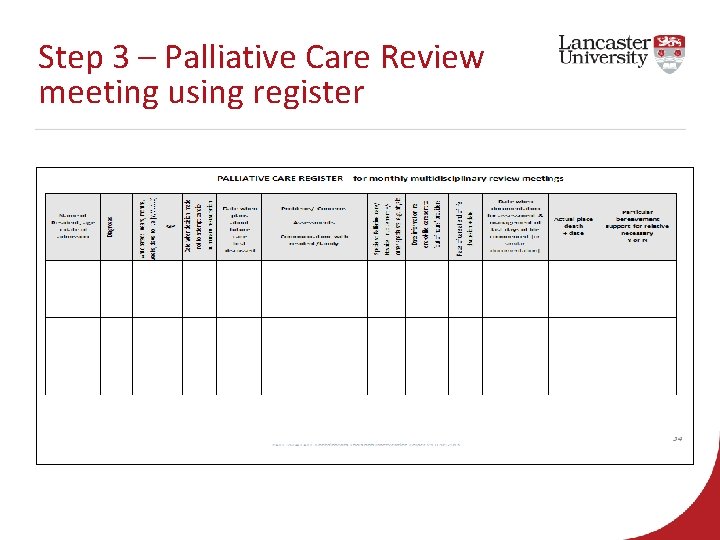
Step 3 – Palliative Care Review meeting using register

Resource: MDT meetings
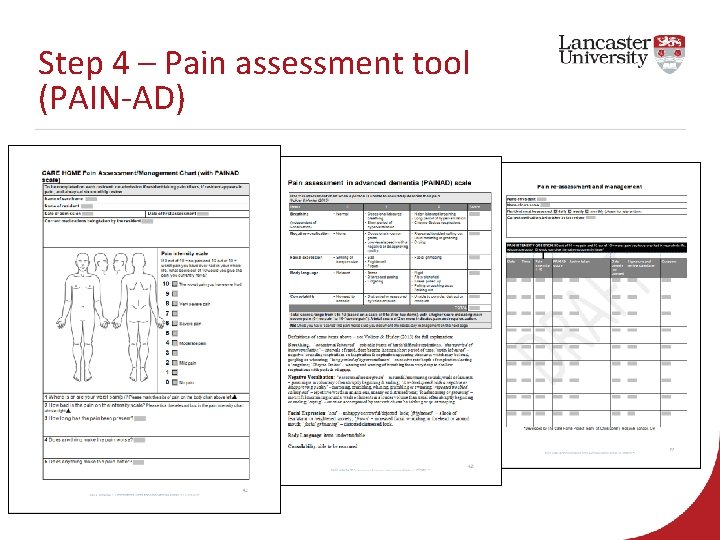
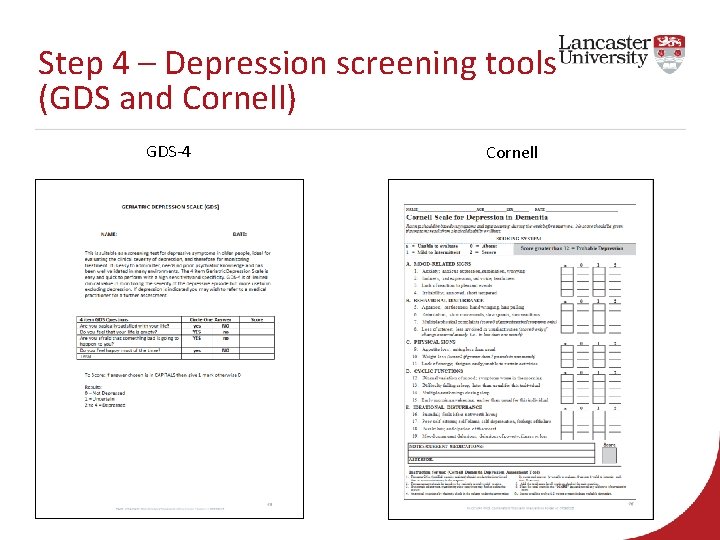
Step 4 – Delivery of high quality palliative care: symptom management Action: Pain Management: • Undertake a pain assessment for all current residents in the care home and on admission for all new residents Depression Screening: • Undertake the assessment once the resident has settled into the care home
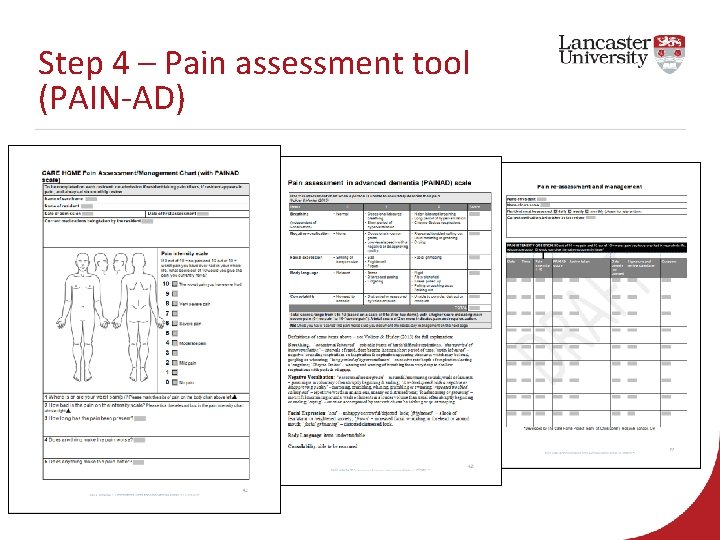
Step 4 – Pain assessment tool (PAIN-AD)
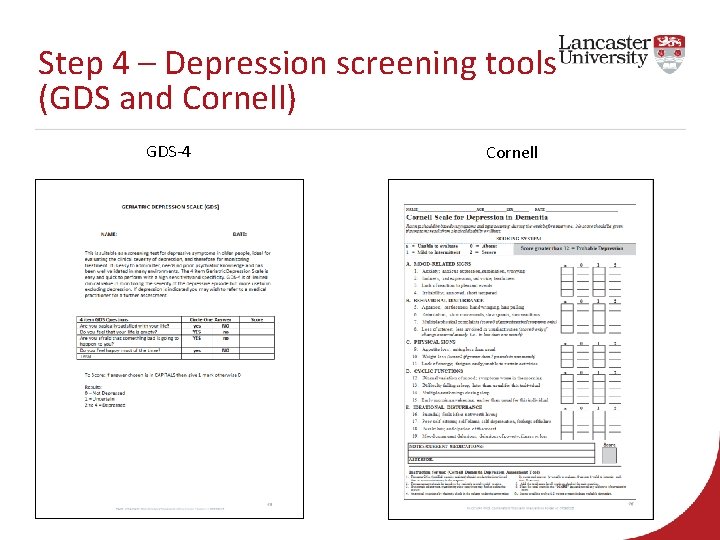
Step 4 – Depression screening tools (GDS and Cornell) GDS-4 Cornell
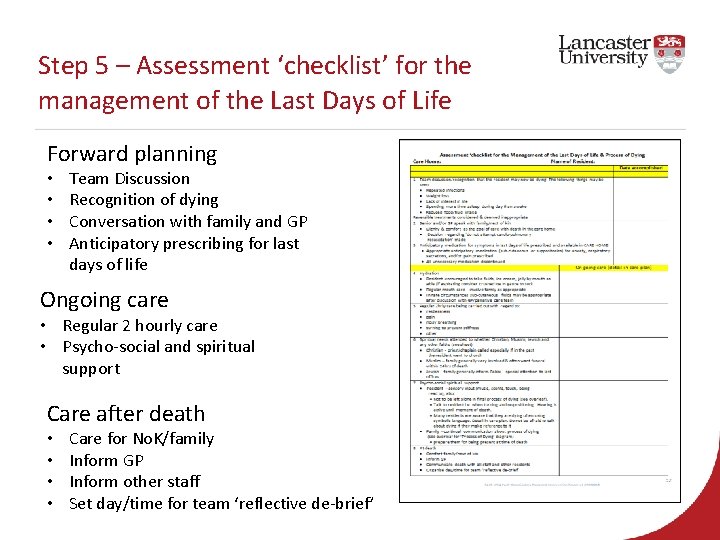
Step 5 – Care in the last days of life Action: Integrate Assessment ‘checklist’ for the Management of the last days of life alongside the residents normal plan of care for with residents who may have only a few days to live. Example image
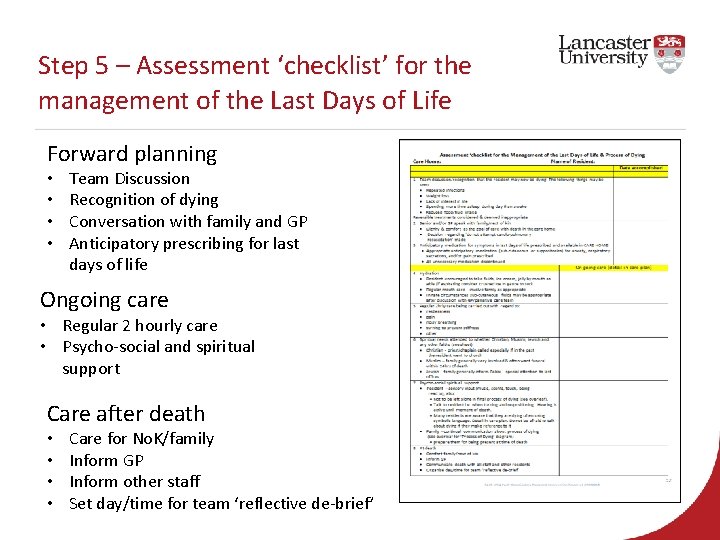
Step 5 – Assessment ‘checklist’ for the management of the Last Days of Life Forward planning • • Team Discussion Recognition of dying Conversation with family and GP Anticipatory prescribing for last days of life Ongoing care • Regular 2 hourly care • Psycho-social and spiritual support Care after death • • Care for No. K/family Inform GP Inform other staff Set day/time for team ‘reflective de-brief’
Step 6 – Care after death Action: Commence monthly reflective debriefing session & death audit tool
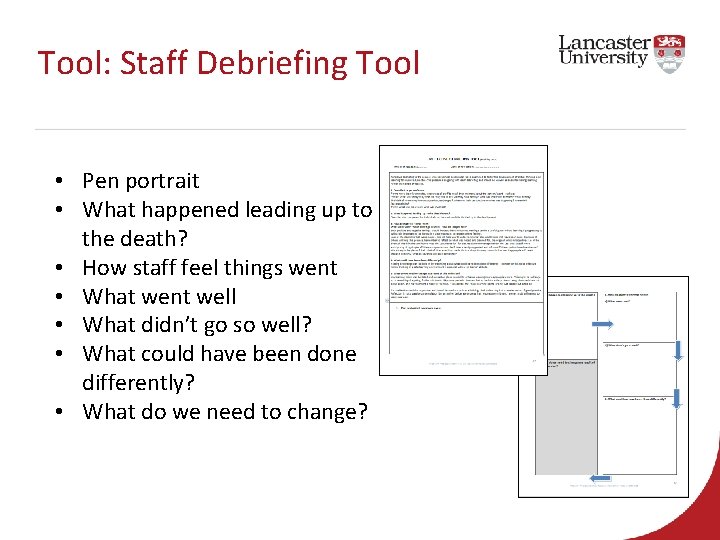
Tool: Staff Debriefing Tool • Pen portrait • What happened leading up to the death? • How staff feel things went • What went well • What didn’t go so well? • What could have been done differently? • What do we need to change?
Resource – Reflective Debriefing
Any questions?
Thank you www. eupace. eu @fp 7 PACE k. froggatt@lancaster. ac. uk e. sowerby@lancaster. ac. uk