PAIN MANAGEMENT IN ELDERLY PERSONS UCLA Multicampus Program




- Slides: 20
PAIN MANAGEMENT IN ELDERLY PERSONS UCLA Multicampus Program of Geriatrics and Gerontology
Physicians Have a Moral Obligation to Provide Comfort and Pain Management Especialy for those near the end of life! l l l Pain is the most feared complication of illness Pain is the second leading complaint in physicians’ offices Often under-diagnosed and under-treated Effects on mood, functional status, and quality of life Associated with increased health service use
18% of Elderly Persons Take Analgesic Medications Regularly (daily or more than 3 times a week) l 71 % take prescription analgesics – 63% for more than 6 months l 72% take OTC analgesics – Median duration more than 5 years l 26% report side-effects – 10% were hospitalized – 41% take medications for side-effects
ELDERLY PATIENTS TAKING PAIN MEDICATIONS FOR CHRONIC PAIN WHO HAD SEEN A DOCTOR IN THE PAST YEAR l l l l 79% had seen a primary care physician 17% had seen a orthopedist 9% had seen a rheumatologist 6% had seen a neurologist 5% had seen a pain specialist 5% had seen a chiropractor 20% had seen more than 5 doctors

Common Causes of Pain In Elderly Persons l Osteoarthritis – back, knee, hip Night-time leg cramps l Claudication l Neuropathies l – idiopathic, traumatic, diabetic, herpetic l Cancer
MISCONCEPTIONS ABOUT PAIN Myth: Pain is expected with aging. Fact: Pain is not normal with aging.

PAIN THRESHOLD WITH AGING
Age Related Differences in Sensory Receptor Function l Encapsulated end organs – 50% reduction in Pacini’s – 10 -30% reduction Meissner’s/Merkels Disks l Free nerve endings – no age change
Age Related Differences in Peripheral Nerve Function n n Myelinated nerves - Reduction in density (all sizes including small) - Increase in abnormal/degenerating fibres - Decrease in action potential/slower conduction velocity Unmyelinated nerves - Reduction in number (1. 2 -1. 6 un) not (. 4 un) - Substance P, CGRP content decreased - Neurogenic inflammation reduced
Age Related Differences in Central Nervous System Function n Loss of dorsal horn spinal neurons - Altered endogenous inhibition, hyperalgesia. n Loss of neurons in cortex, midbrain, brain stem - (18% reduction in thalamus, no change cingulum cortex) - Altered cerebral evoked responses (increased latency, reduced amplitude) - Reduced catecholamines, acetylcholine, GABA, 5 HT, not neuropeptides
MISCONCEPTIONS ABOUT PAIN Myth: If they don’t complain, they don’t have pain Fact: There are many reasons patients may be reluctant to complain, despite pain that significantly effects their functional status and mood.
REASONS PATIENTS MAY NOT REPORT PAIN Fear of diagnostic tests l Fear of medications l Fear meaning of pain l Perceive physicians and nurses too busy l Complaining may effect quality of care l Believe nothing can or will be done l
The most reliable indicator of the existence pain and its intensity is the patient’s description.


There is a lot we can do to relieve pain! Analgesic drugs l Non-drug strategies l Specialized pain treatment centers l Patient and caregiver education and support l
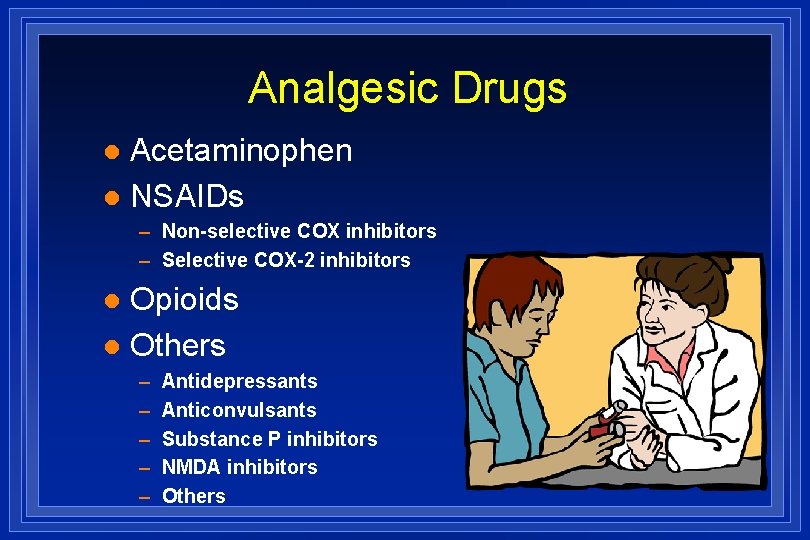
Analgesic Drugs Acetaminophen l NSAIDs l – Non-selective COX inhibitors – Selective COX-2 inhibitors Opioids l Others l – – – Antidepressants Anticonvulsants Substance P inhibitors NMDA inhibitors Others
CAUTION Meperidine (Demerol) l Butorphanol (Stadol) l Pentazocine (Talwin) l Propoxiphene (Darvon) l Methadone (Dolophine) l Transderm Fentanyl (Duragesic) l
Do Not Use Placebos! Unethical in clinical practice l They don’t work l Not helpful in diagnosis l Effect is short lived l Destroys trust l
Non-Drug Strategies l l Exercise – PT, OT, stretching, strengthening – general conditioning l Physical methods l – ice, heat, massage l l Cognitivebehavioral therapy l Chiropracty Acupuncture TENS Alternative therapies – relaxation, imagery – herbals
PATIENT AND CAREGIVER EDUCATION Diagnosis, prognosis, natural history of underlying disease l Communication and assessment of pain l Explanation of drug strategies l Management of potential side-effects l Explanation of non-drug strategies l