Pain Management for Older Adults Miriam B Rodin
Pain Management for Older Adults Miriam B. Rodin, MD, Ph. D Division of Geriatrics and Gerontology St Louis University Medical School Weeks Conference 5/10/2019
No conflicts of interest to declare
OBJECTIVES 1. 2. 3. 4. 5. 6. Describe the different kinds of pain: somatic, visceral, neuropathic Distinguish acute, cancer and chronic noncancer pain. Understand the indications for opioid therapy Describe at least 2 opiate tolerance syndromes. Formulate an approach to chronic pain in older adults Use a guide for titration of opiates.
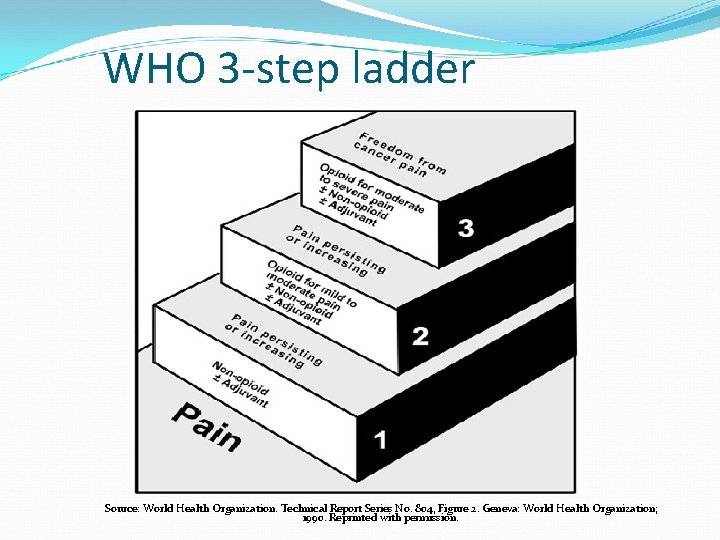
WHO 3 -step ladder Source: World Health Organization. Technical Report Series No. 804, Figure 2. Geneva: World Health Organization; 1990. Reprinted with permission.
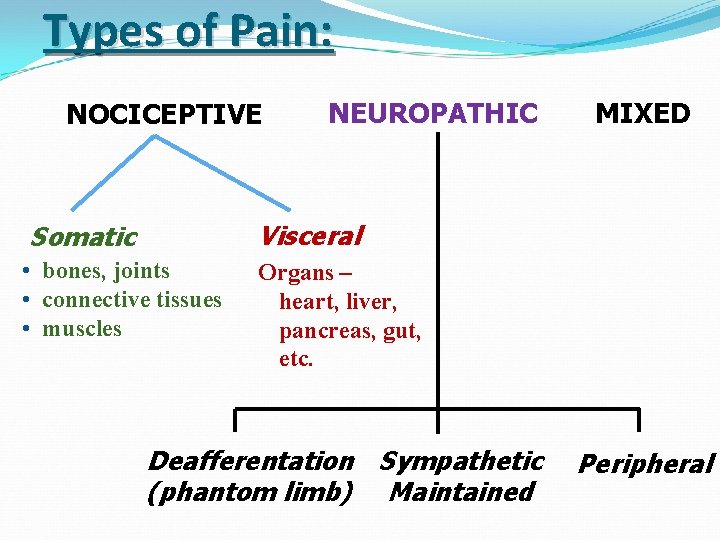
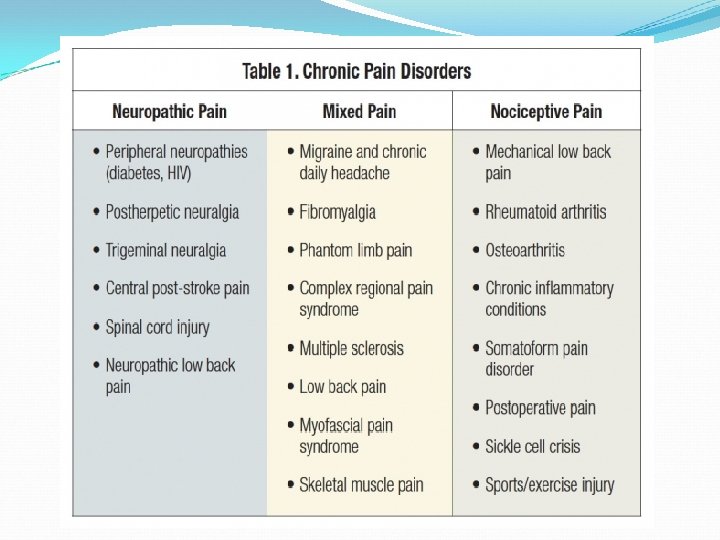
Types of Pain: NOCICEPTIVE NEUROPATHIC MIXED Visceral Somatic • bones, joints • connective tissues • muscles Organs – heart, liver, pancreas, gut, etc. Deafferentation Sympathetic (phantom limb) Maintained Peripheral
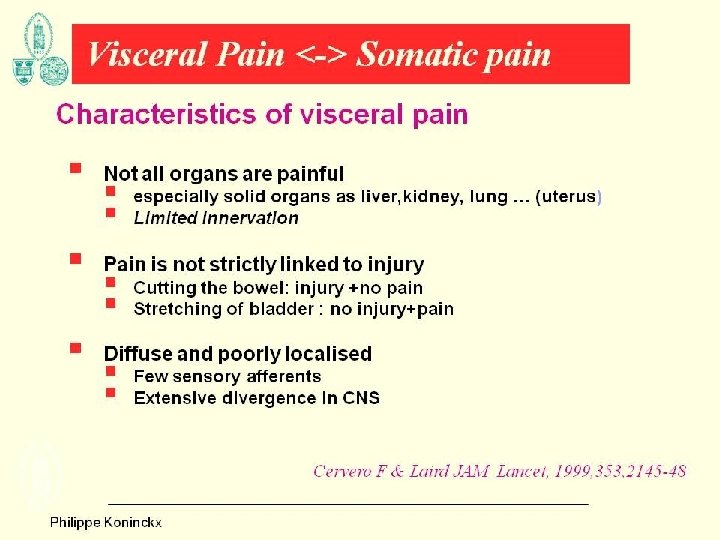
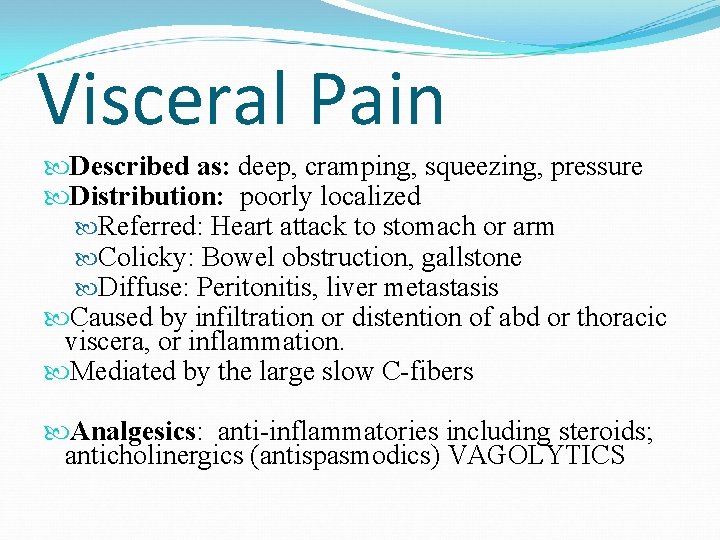
Visceral Pain Described as: deep, cramping, squeezing, pressure Distribution: poorly localized Referred: Heart attack to stomach or arm Colicky: Bowel obstruction, gallstone Diffuse: Peritonitis, liver metastasis Caused by infiltration or distention of abd or thoracic viscera, or inflammation. Mediated by the large slow C-fibers Analgesics: anti-inflammatories including steroids; anticholinergics (antispasmodics) VAGOLYTICS
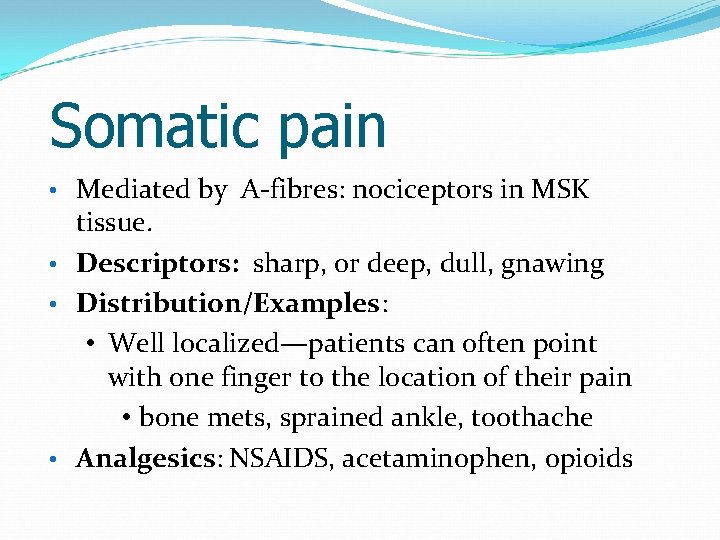
Somatic pain Mediated by A-fibres: nociceptors in MSK tissue. • Descriptors: sharp, or deep, dull, gnawing • Distribution/Examples: • Well localized—patients can often point with one finger to the location of their pain • bone mets, sprained ankle, toothache • Analgesics: NSAIDS, acetaminophen, opioids •
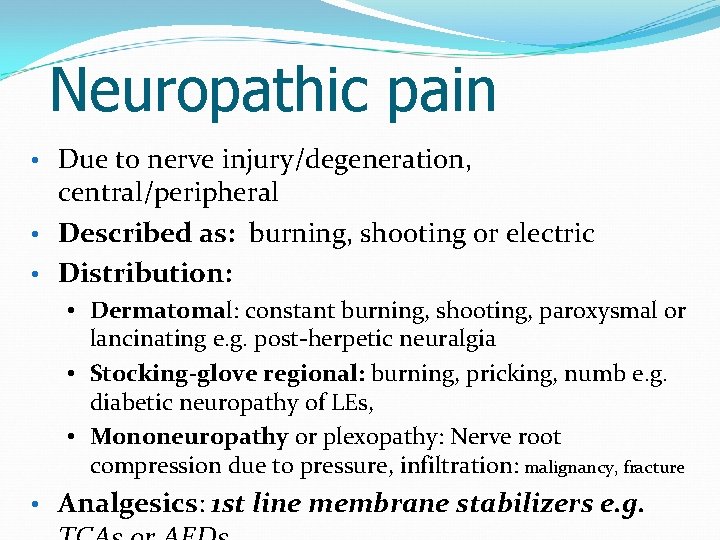
Neuropathic pain Due to nerve injury/degeneration, central/peripheral • Described as: burning, shooting or electric • Distribution: • • Dermatomal: constant burning, shooting, paroxysmal or lancinating e. g. post-herpetic neuralgia • Stocking-glove regional: burning, pricking, numb e. g. diabetic neuropathy of LEs, • Mononeuropathy or plexopathy: Nerve root compression due to pressure, infiltration: malignancy, fracture • Analgesics: 1 st line membrane stabilizers e. g.
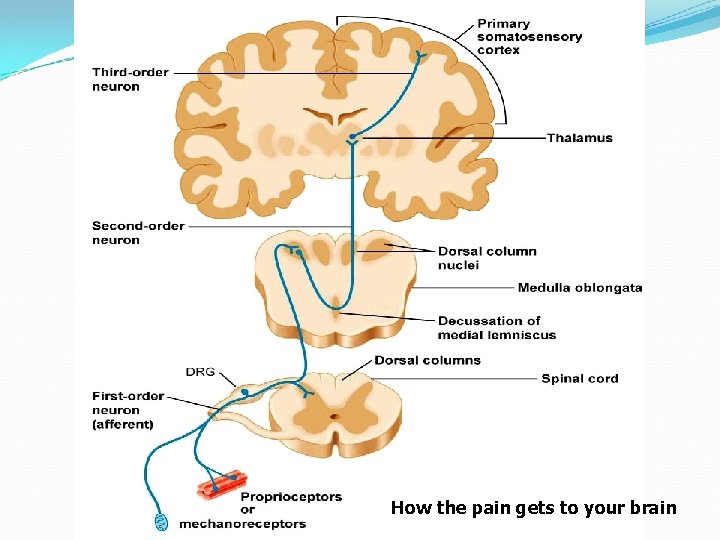
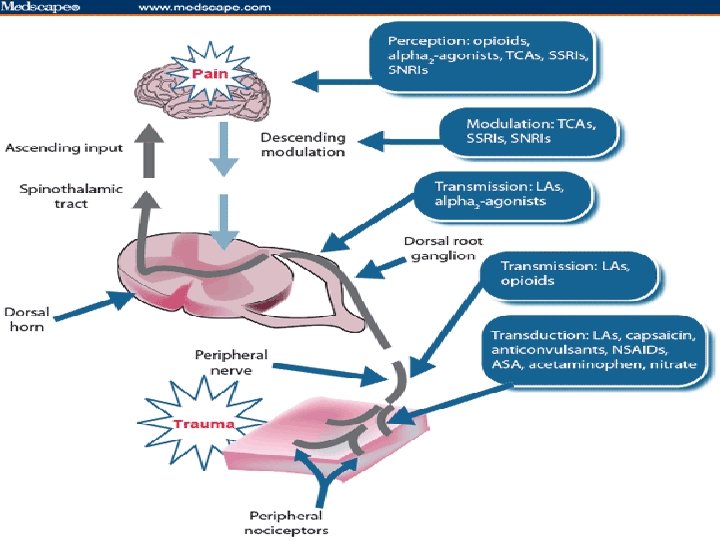
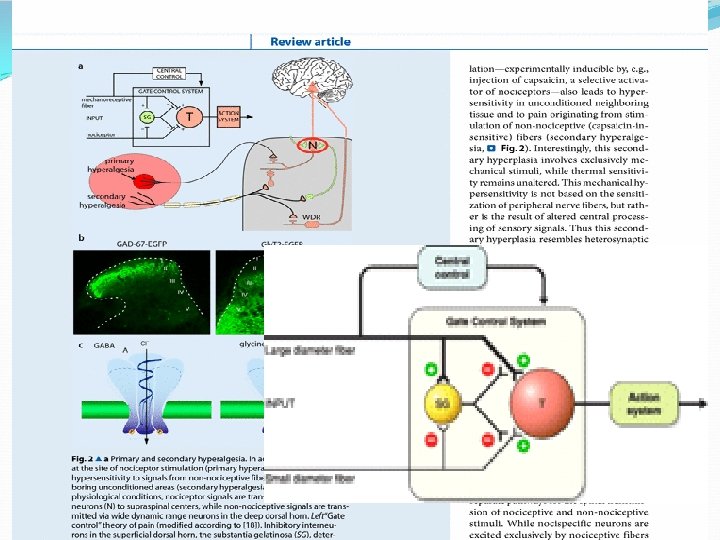
How the pain gets to your brain
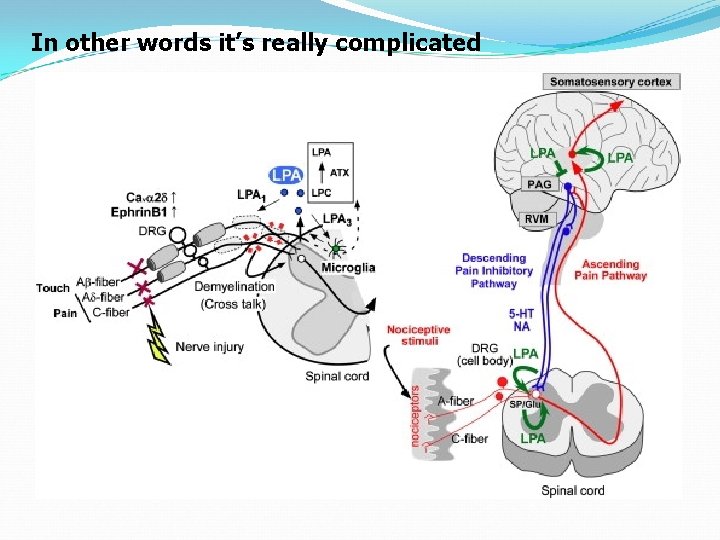
In other words it’s really complicated
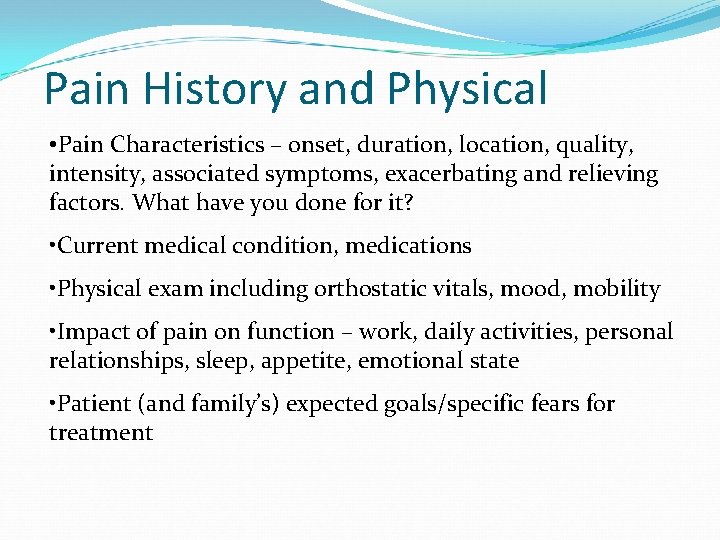
Pain History and Physical • Pain Characteristics – onset, duration, location, quality, intensity, associated symptoms, exacerbating and relieving factors. What have you done for it? • Current medical condition, medications • Physical exam including orthostatic vitals, mood, mobility • Impact of pain on function – work, daily activities, personal relationships, sleep, appetite, emotional state • Patient (and family’s) expected goals/specific fears for treatment
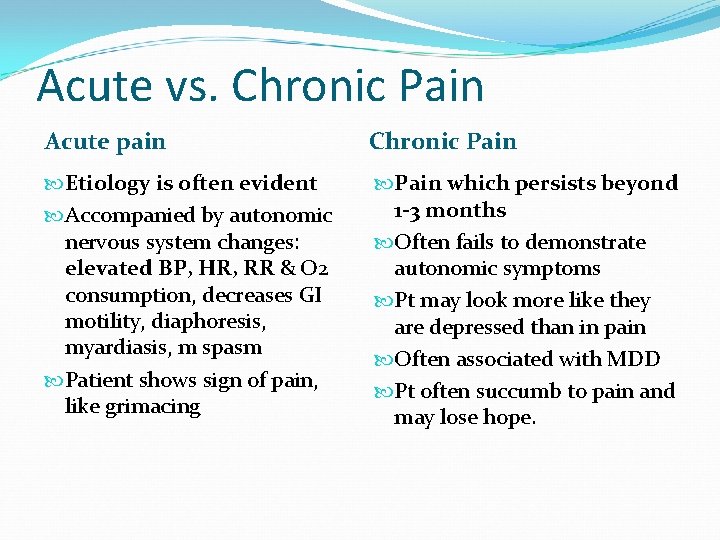
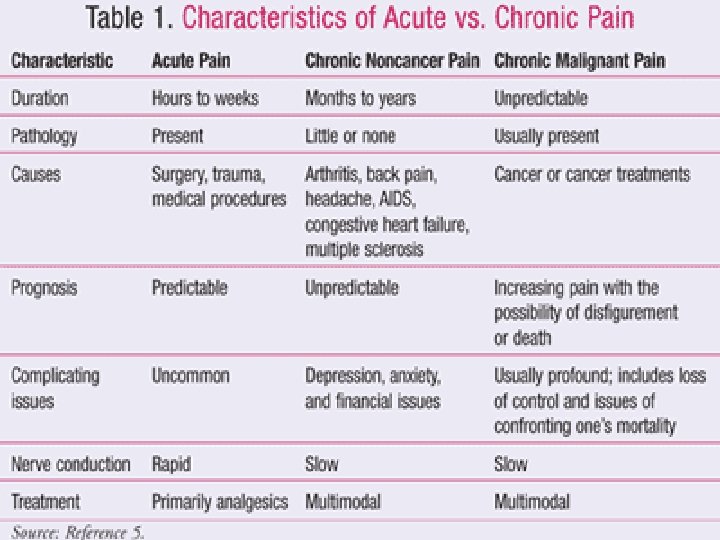
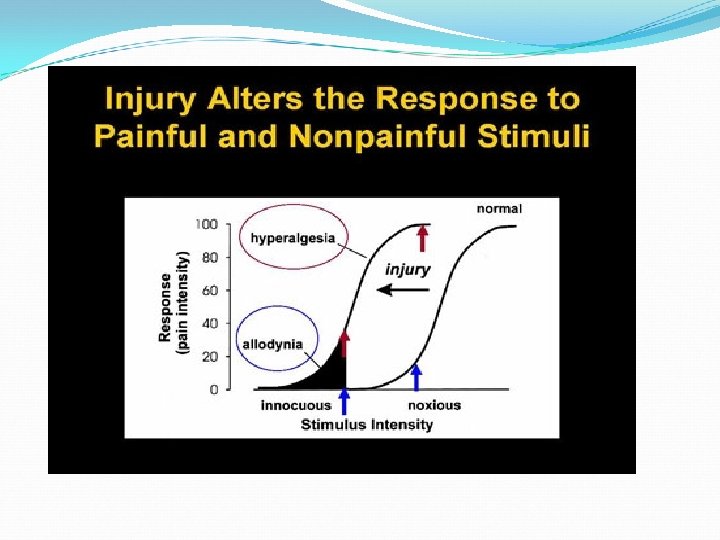
Acute vs. Chronic Pain Acute pain Chronic Pain Etiology is often evident Pain which persists beyond 1 -3 months Accompanied by autonomic nervous system changes: elevated BP, HR, RR & O 2 consumption, decreases GI motility, diaphoresis, myardiasis, m spasm Patient shows sign of pain, like grimacing Often fails to demonstrate autonomic symptoms Pt may look more like they are depressed than in pain Often associated with MDD Pt often succumb to pain and may lose hope.
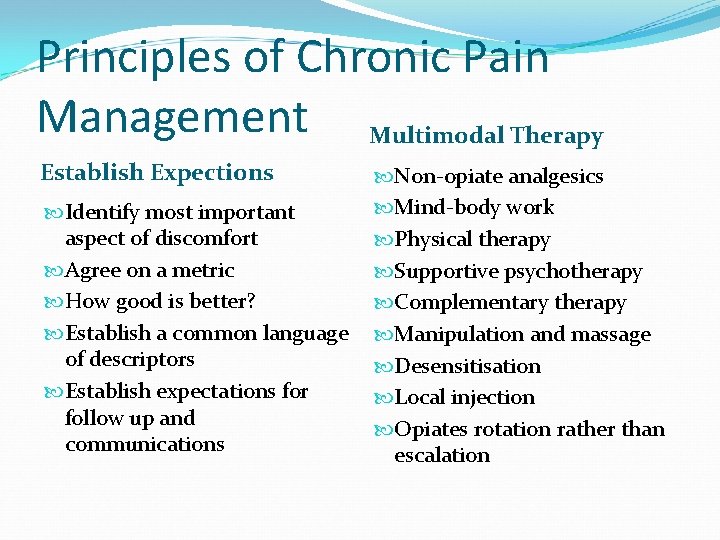
Principles of Chronic Pain Management Multimodal Therapy Establish Expections Identify most important aspect of discomfort Agree on a metric How good is better? Establish a common language of descriptors Establish expectations for follow up and communications Non-opiate analgesics Mind-body work Physical therapy Supportive psychotherapy Complementary therapy Manipulation and massage Desensitisation Local injection Opiates rotation rather than escalation
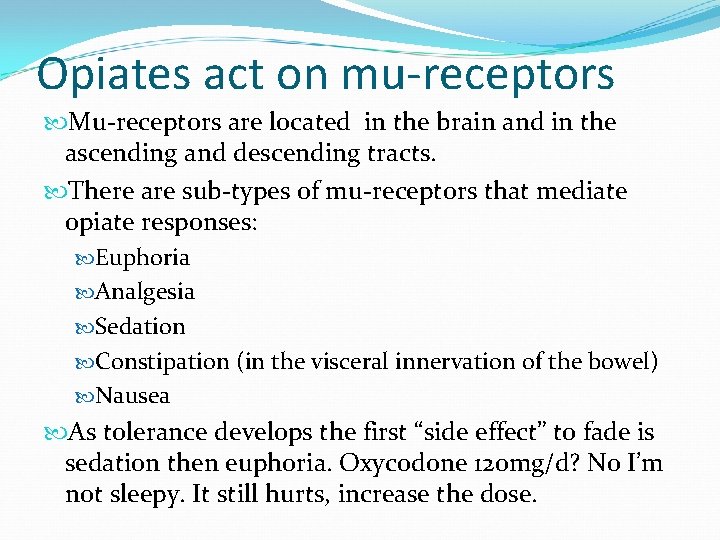
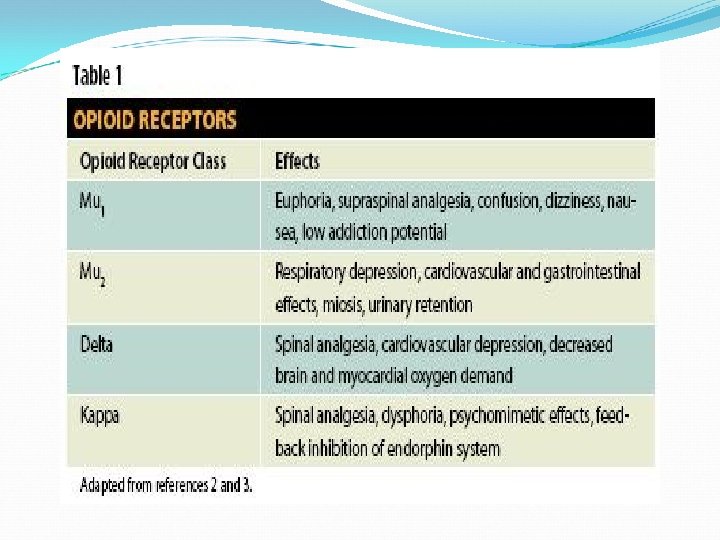
Opiates act on mu-receptors Mu-receptors are located in the brain and in the ascending and descending tracts. There are sub-types of mu-receptors that mediate opiate responses: Euphoria Analgesia Sedation Constipation (in the visceral innervation of the bowel) Nausea As tolerance develops the first “side effect” to fade is sedation then euphoria. Oxycodone 120 mg/d? No I’m not sleepy. It still hurts, increase the dose.
Not all opiates are the same If one “stops working” do not increase it, rotate it. Methadone is messy but it has NMDA (glutamate is an excitatory NT) blockade activity Use a validated conversion calculator and don’t trust yourself to remember where the decimal goes. (Fentanyl) www. globalrph. com Google: narcotic converter
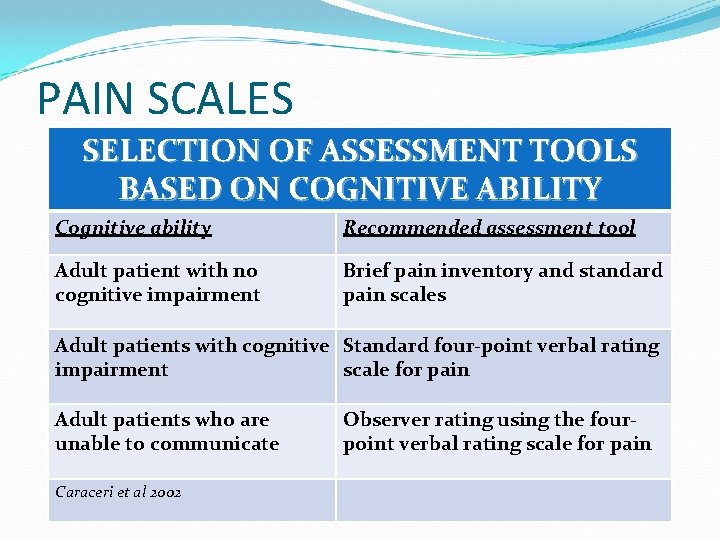
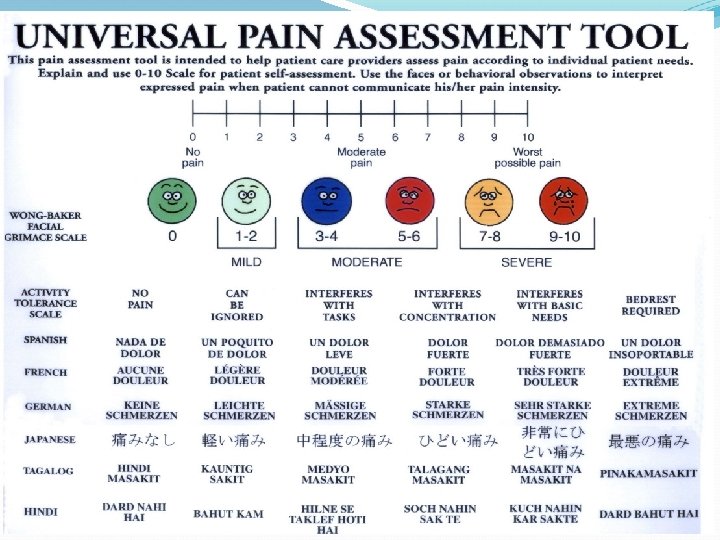
PAIN SCALES SELECTION OF ASSESSMENT TOOLS BASED ON COGNITIVE ABILITY Cognitive ability Recommended assessment tool Adult patient with no cognitive impairment Brief pain inventory and standard pain scales Adult patients with cognitive Standard four-point verbal rating impairment scale for pain Adult patients who are unable to communicate Caraceri et al 2002 Observer rating using the fourpoint verbal rating scale for pain
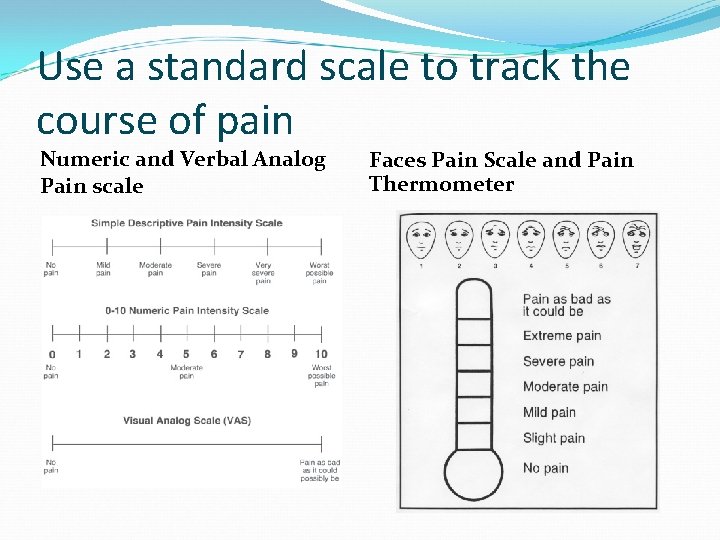
Use a standard scale to track the course of pain Numeric and Verbal Analog Pain scale Faces Pain Scale and Pain Thermometer
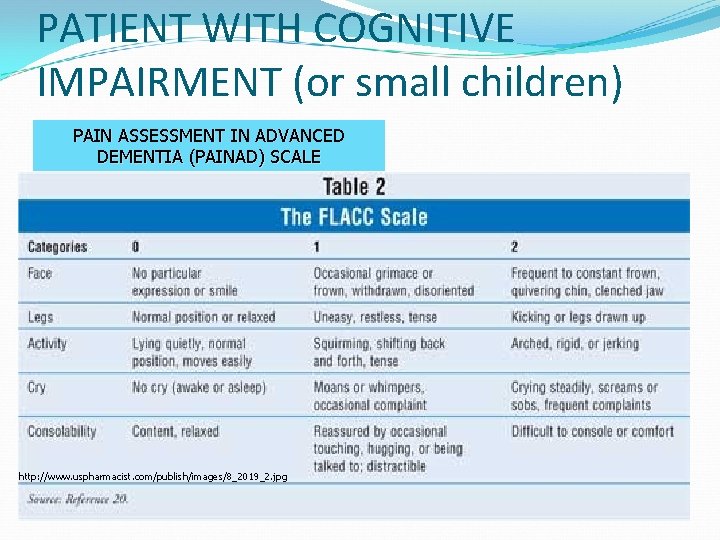
PATIENT WITH COGNITIVE IMPAIRMENT (or small children) PAIN ASSESSMENT IN ADVANCED DEMENTIA (PAINAD) SCALE http: //www. uspharmacist. com/publish/images/8_2019_2. jpg
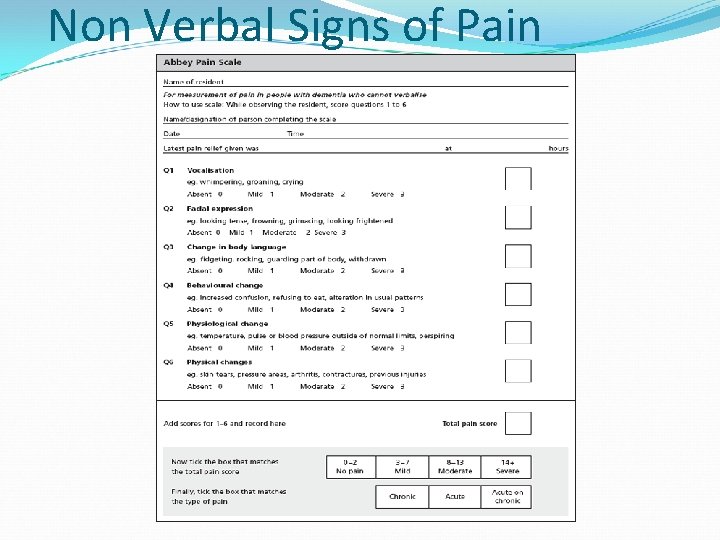
Non Verbal Signs of Pain
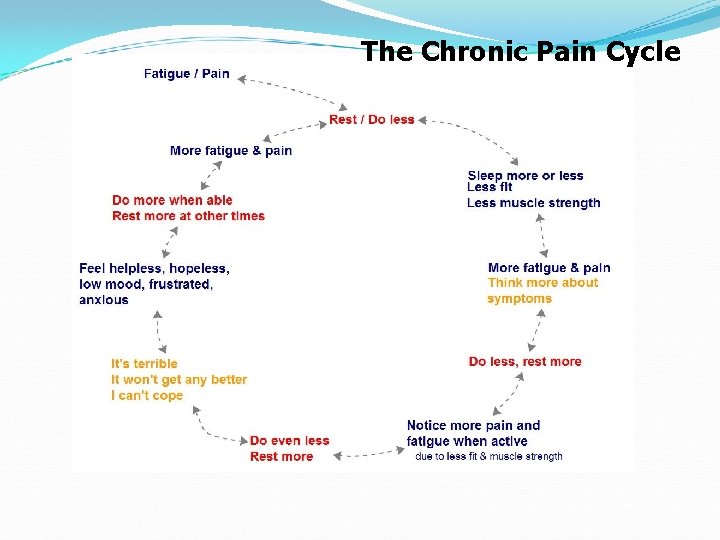
The Chronic Pain Cycle
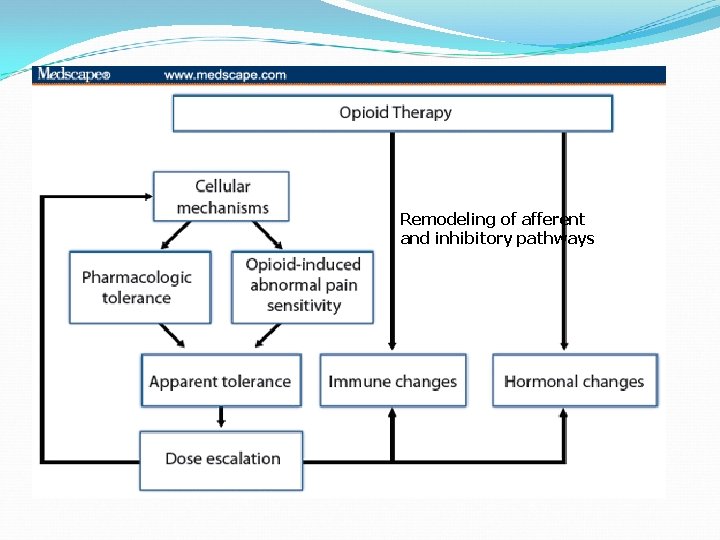
Remodeling of afferent and inhibitory pathways
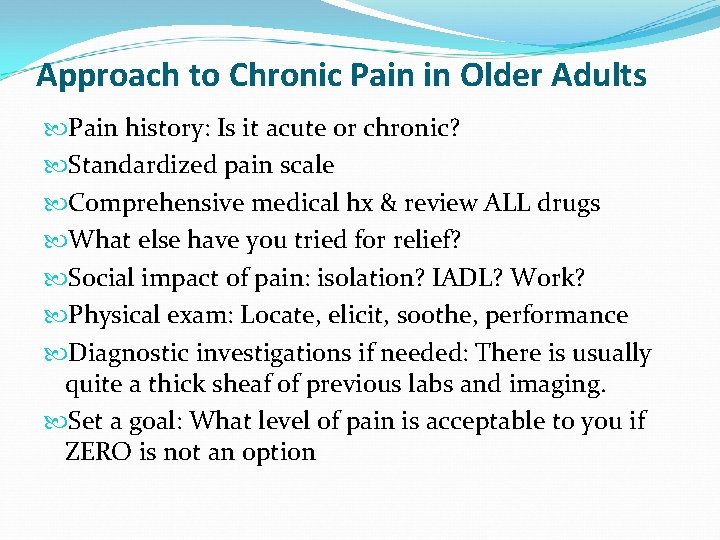
Approach to Chronic Pain in Older Adults Pain history: Is it acute or chronic? Standardized pain scale Comprehensive medical hx & review ALL drugs What else have you tried for relief? Social impact of pain: isolation? IADL? Work? Physical exam: Locate, elicit, soothe, performance Diagnostic investigations if needed: There is usually quite a thick sheaf of previous labs and imaging. Set a goal: What level of pain is acceptable to you if ZERO is not an option
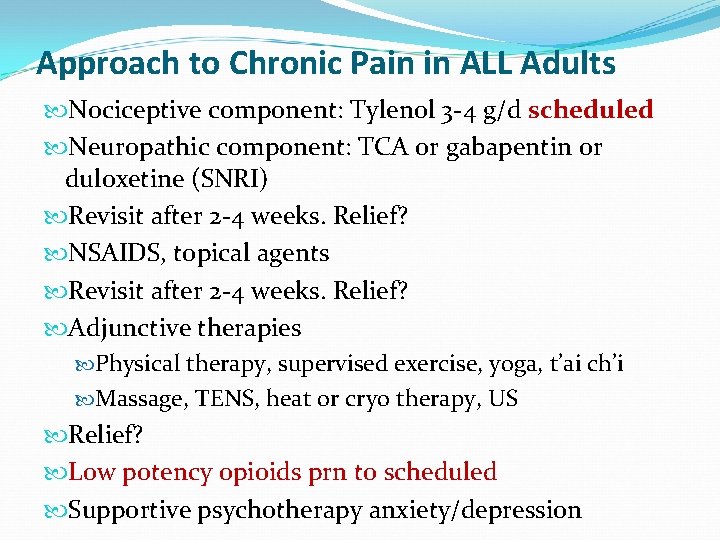
Approach to Chronic Pain in ALL Adults Nociceptive component: Tylenol 3 -4 g/d scheduled Neuropathic component: TCA or gabapentin or duloxetine (SNRI) Revisit after 2 -4 weeks. Relief? NSAIDS, topical agents Revisit after 2 -4 weeks. Relief? Adjunctive therapies Physical therapy, supervised exercise, yoga, t’ai ch’i Massage, TENS, heat or cryo therapy, US Relief? Low potency opioids prn to scheduled Supportive psychotherapy anxiety/depression
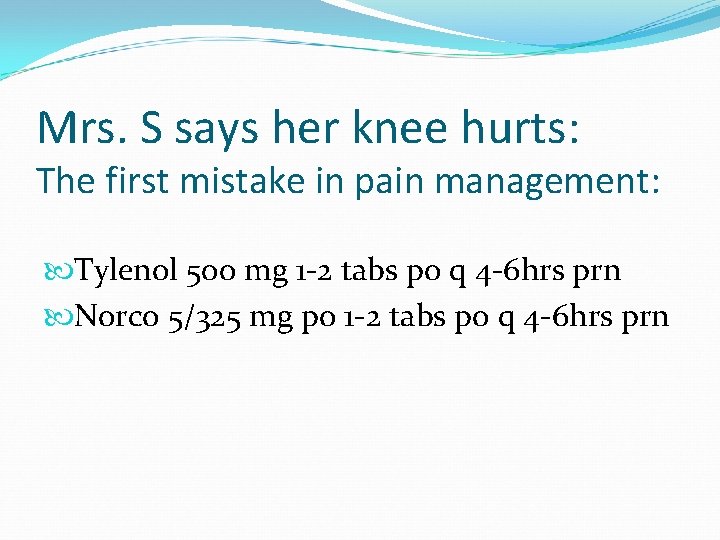
Mrs. S says her knee hurts: The first mistake in pain management: Tylenol 500 mg 1 -2 tabs po q 4 -6 hrs prn Norco 5/325 mg po 1 -2 tabs po q 4 -6 hrs prn
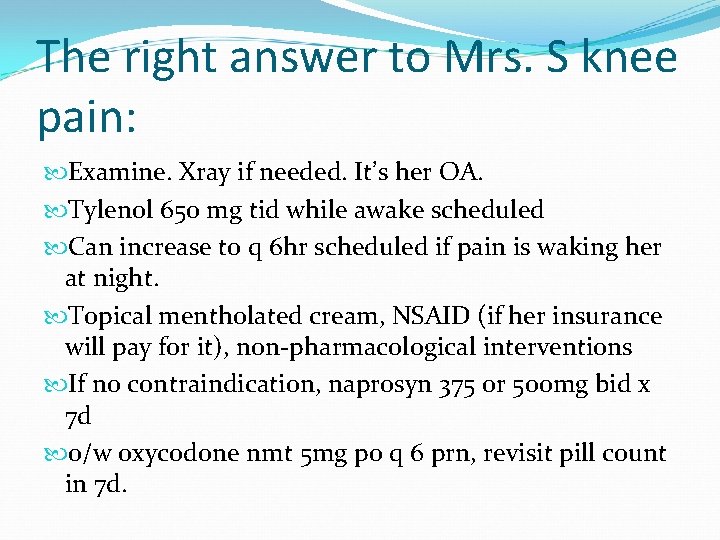
The right answer to Mrs. S knee pain: Examine. Xray if needed. It’s her OA. Tylenol 650 mg tid while awake scheduled Can increase to q 6 hr scheduled if pain is waking her at night. Topical mentholated cream, NSAID (if her insurance will pay for it), non-pharmacological interventions If no contraindication, naprosyn 375 or 500 mg bid x 7 d o/w oxycodone nmt 5 mg po q 6 prn, revisit pill count in 7 d.
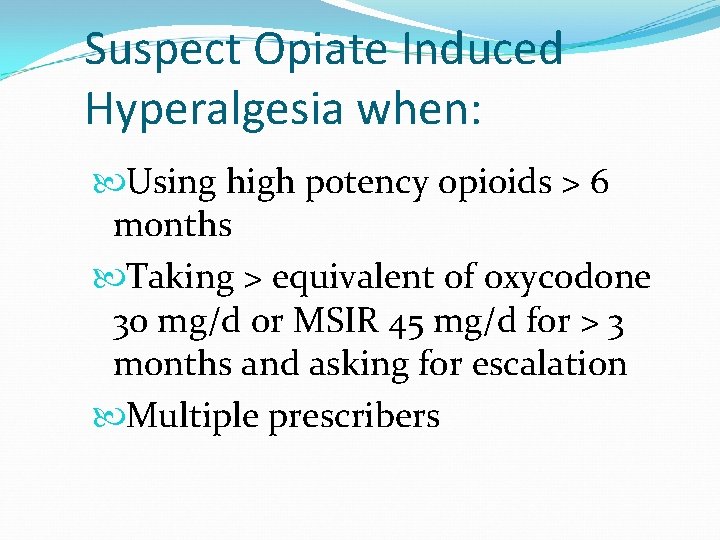
Suspect Opiate Induced Hyperalgesia when: Using high potency opioids > 6 months Taking > equivalent of oxycodone 30 mg/d or MSIR 45 mg/d for > 3 months and asking for escalation Multiple prescribers
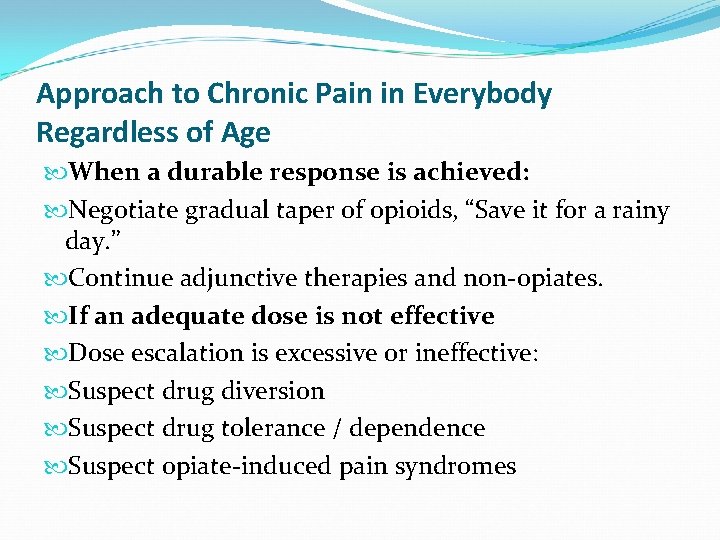
Approach to Chronic Pain in Everybody Regardless of Age When a durable response is achieved: Negotiate gradual taper of opioids, “Save it for a rainy day. ” Continue adjunctive therapies and non-opiates. If an adequate dose is not effective Dose escalation is excessive or ineffective: Suspect drug diversion Suspect drug tolerance / dependence Suspect opiate-induced pain syndromes
Suspect drug diversion if Utox is negative or Elderly patient is always accompanied by a younger person who verbalizes the pain for them Multiple prescribers
Adjuvant Medications: in order Topicals Tylenol NSAIDS, Celecoxib, steroids Anticonvulsants Antidepressants Anticholinergics Anxiolytics Muscle relaxants Antihistamines
Summary Pain is a normal bodily function. Chronic pain indicates that normal pain physiology has changed either by pathway remodeling or drug induced changes. Chronic pain is defined by >3 months duration, no obvious localizable cause Approach to chronic pain should be systematic and step-wise. Approach to chronic pain should be multimodal and multidisciplinary.
Thanks!
- Slides: 40