Pain Management and Documentation What When Where Pain
- Slides: 23
Pain Management and Documentation What When Where
Pain l l Pain is a symptom that signals distress in diverse populations of all ages Pain – “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage” International Association for the Study of Pain
Self Report of Pain l l l Patients who are alert and have the ability to communicate appropriately Adults of all ages Children about 5 years or more
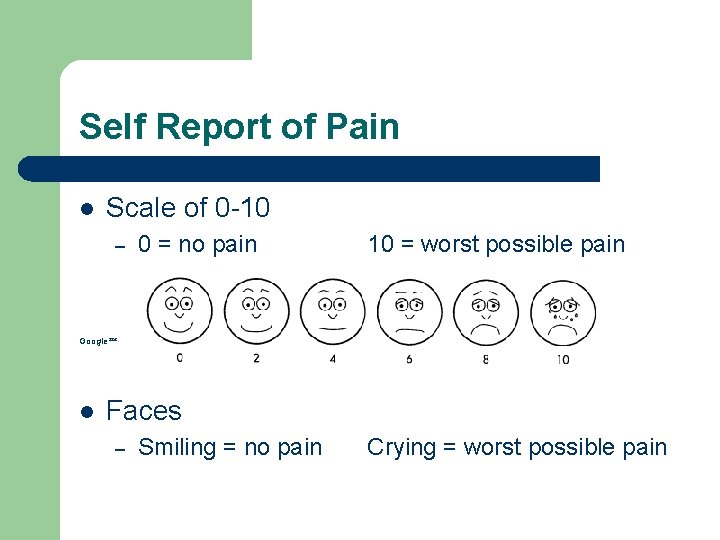
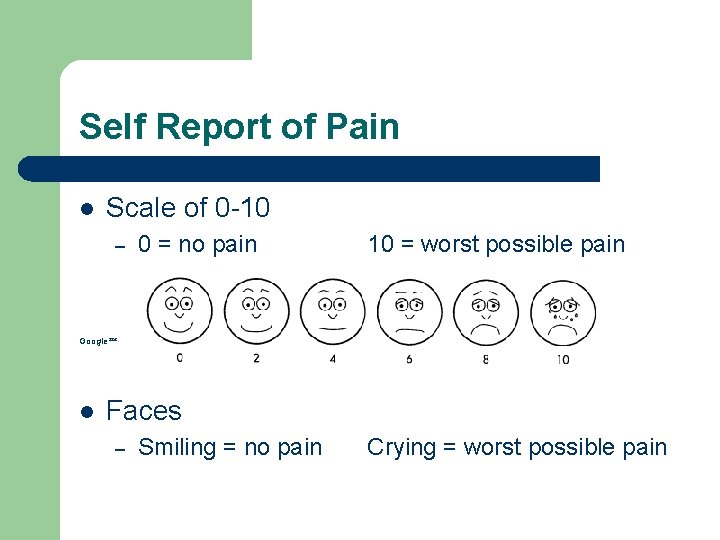
Self Report of Pain l Scale of 0 -10 – 0 = no pain 10 = worst possible pain Google l Faces – Smiling = no pain Crying = worst possible pain
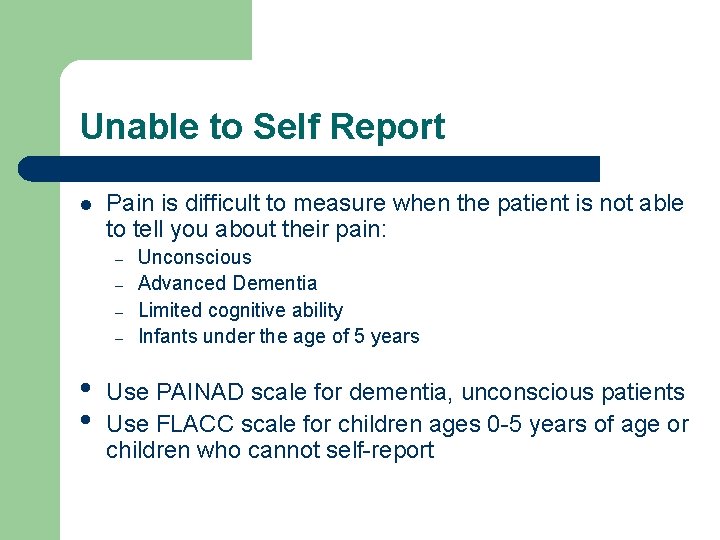
Unable to Self Report l Pain is difficult to measure when the patient is not able to tell you about their pain: – – • • Unconscious Advanced Dementia Limited cognitive ability Infants under the age of 5 years Use PAINAD scale for dementia, unconscious patients Use FLACC scale for children ages 0 -5 years of age or children who cannot self-report
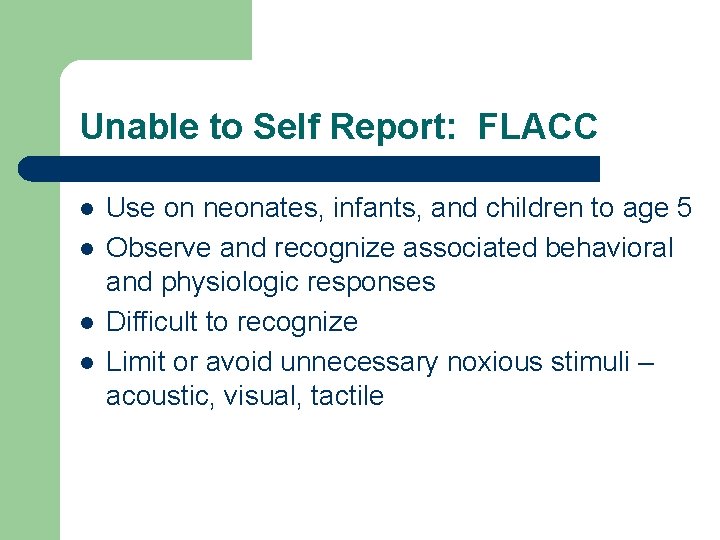
Unable to Self Report: FLACC l l Use on neonates, infants, and children to age 5 Observe and recognize associated behavioral and physiologic responses Difficult to recognize Limit or avoid unnecessary noxious stimuli – acoustic, visual, tactile
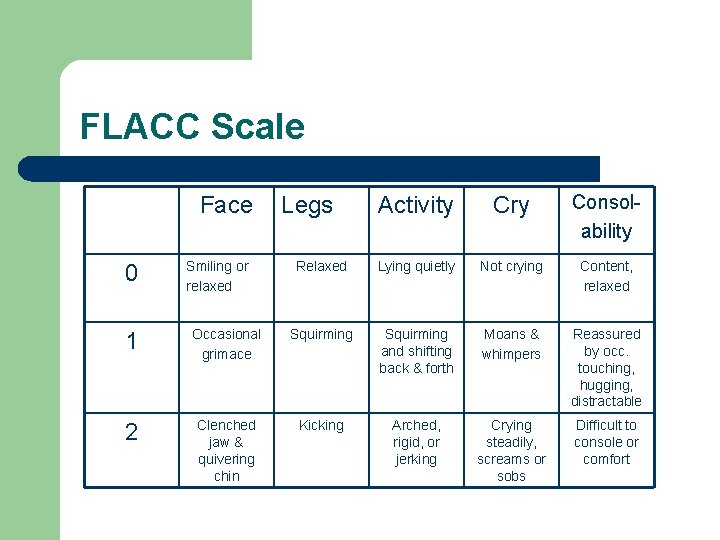
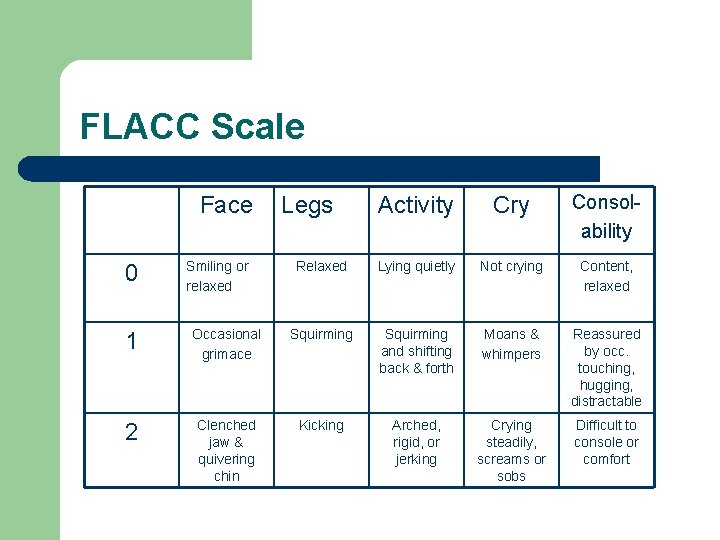
FLACC Scale Face 0 Smiling or relaxed Activity Cry Consolability Relaxed Lying quietly Not crying Content, relaxed Legs 1 Occasional grimace Squirming and shifting back & forth Moans & whimpers Reassured by occ. touching, hugging, distractable 2 Clenched jaw & quivering chin Kicking Arched, rigid, or jerking Crying steadily, screams or sobs Difficult to console or comfort
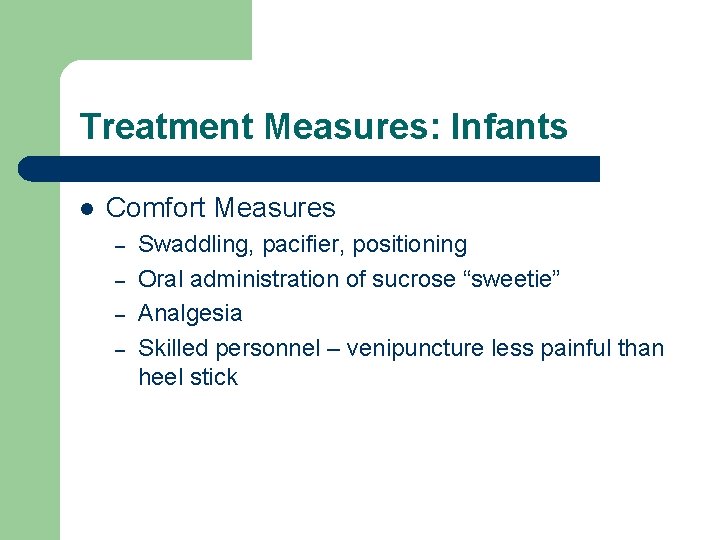
Treatment Measures: Infants l Comfort Measures – – Swaddling, pacifier, positioning Oral administration of sucrose “sweetie” Analgesia Skilled personnel – venipuncture less painful than heel stick
Unable to Self Report: PAINAD l l Lack of ability to self report Cognitive disorder – cerebral palsy, head trauma, dementia, unconscious Requires special consideration during assessment of pain Multiple tools exist, but many have not been validated for reliability in a clinical setting
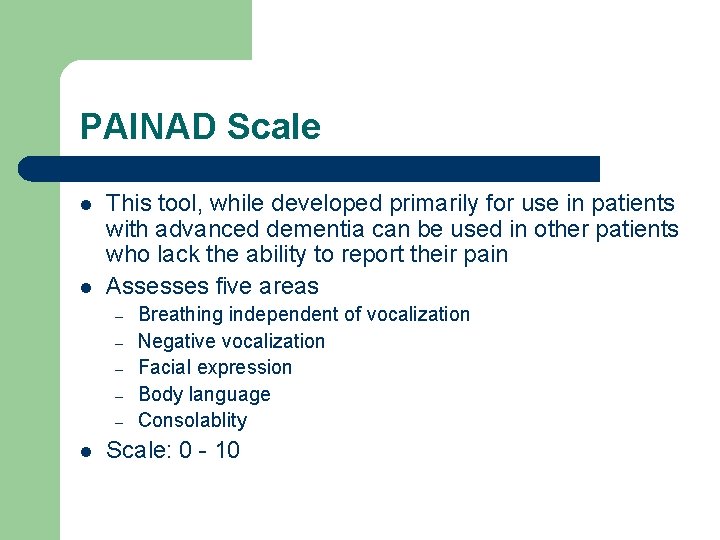
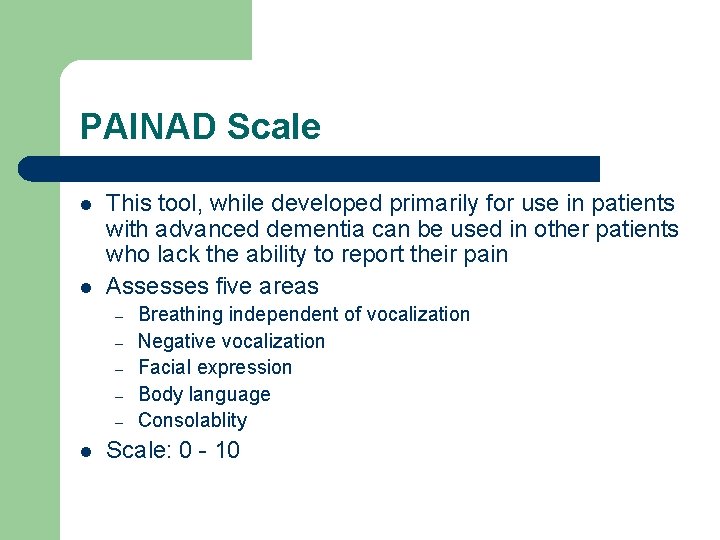
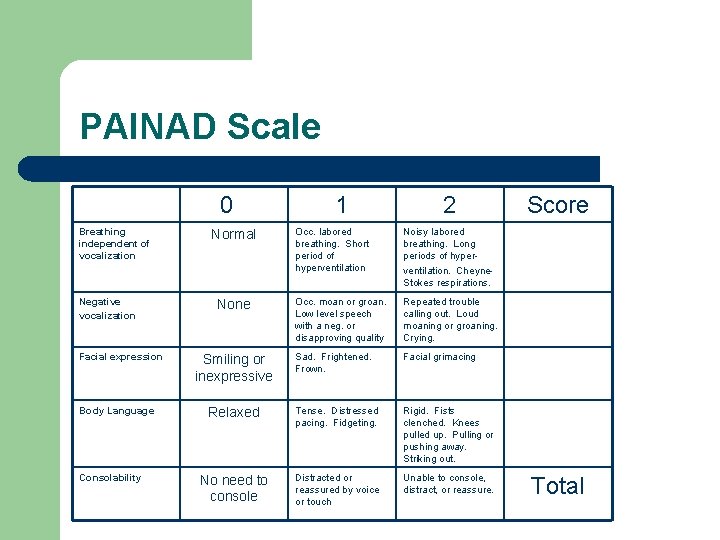
PAINAD Scale l l This tool, while developed primarily for use in patients with advanced dementia can be used in other patients who lack the ability to report their pain Assesses five areas – – – l Breathing independent of vocalization Negative vocalization Facial expression Body language Consolablity Scale: 0 - 10
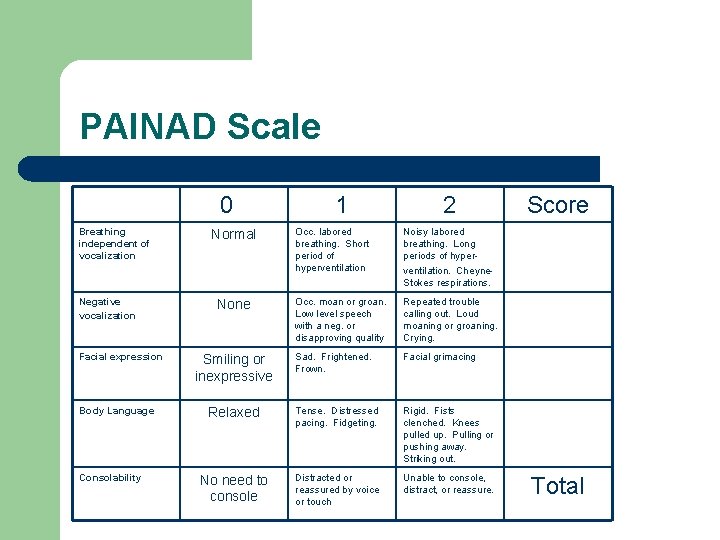
PAINAD Scale 0 Breathing independent of vocalization Negative vocalization Facial expression Body Language Consolability 1 2 Occ. labored breathing. Short period of hyperventilation Noisy labored breathing. Long periods of hyperventilation. Cheyne. Stokes respirations. Occ. moan or groan. Low level speech with a neg. or disapproving quality Repeated trouble calling out. Loud moaning or groaning. Crying. Sad. Frightened. Frown. Facial grimacing Relaxed Tense. Distressed pacing. Fidgeting. Rigid. Fists clenched. Knees pulled up. Pulling or pushing away. Striking out. No need to console Distracted or reassured by voice or touch Unable to console, distract, or reassure. Normal None Smiling or inexpressive Score Total
Surrogate Reporting of Pain l Don’t forget the help that can come from a caregiver who really knows and understands patient’s behavior
When to Assess l All patients regardless of where they enter the healthcare setting should have their pain level assessed on admission – – Triage Admission Inpatient Outpatient
The NEXT Assessment l l Timing of the next assessment varies based on location of care and needs of the patient Inpatients (ICU, 2 East, 3 East) – – – At least q 12 hours 60 minutes post any intervention – medication, repositioning, etc At discharge
l ODA – – – l ED – – l On return from surgery 60 minutes post any intervention At discharge from ODA 60 minutes post any intervention Determined by category and patient condition PACU – – 20 minutes post any intervention Determined by patient condition
Special Circumstances l l ODA and OR - Prior to surgery the nurse will check with anesthesia regarding need for pain relief due to the medication that will be given as sedation or anesthesia during actual procedure MBU – many obstetric patients receive an epidural catheter for pain relief during labor and delivery – – The catheter is placed by anesthesia and medication is delivered by anesthesia initially and placed on a pump for continued pain relief Nurses continue to assess patient’s pain needs at least q 1 hour
Patient Controlled Analgesia l PCA – – l Ordered by physician Consult Anesthesia Document initial pain relief Assess and document pain level at least q 2 hours NOTE – PATIENT CONTROLLED ONLY
Barriers to Pain Management l l Attitudes, biases Misinformation about addiction Fear of legal problems Worries about side effects
Addiction Fewer than 2 in 10, 000 patients with pain will become addicted to an opioid.
Patient Attitudes l l l Afraid of addiction Misinformed “Strong” Remember to consider your patient’s cultural, religious, and social backgrounds
Education l Discuss with patients and document their role in pain relief – – Pain should be reported If no relief, physician to be notified Expected pain Intractable pain
Remember…. If the patient says he/she is in pain…they are in pain.
Pain Management must be a Team Effort!