Pain Assessment and Management Nursing Learning Objectives Upon
Pain Assessment and Management Nursing
Learning Objectives Upon completion of this module, you will • Verbalize the definition of pain • States who is responsible for the management pain • Utilizes appropriate pain scale for the type of patient being assessed • Understands methods to relieve pain • Discuss the assessment procedure • Discuss the appropriate documentation procedure • Discuss the importance of patient/family teaching 2
Definition of Pain is defined as the unpleasant sensory or /or emotional experience. Pain is subjective ‐ stated by the patient. Hence, all employees will accept the patients report of pain as stated. CHSB policy states “It is the responsibility of all staff to follow the established guidelines for effective pain management and promote comfort for the patient. 3
Staff Responsibility CHSB will aggressively respond to the patients complaint of pain All patients pain will be managed utilizing a variety of treatment modalities The individual pain will be assessed/reassessed utilizing the appropriate scale Upon admission, an established goal will be identify an acceptable level of pain. 4
Let’s get started on assessment of pain… 5
Pain Assessment Obtain any significant history upon admission or pre/post procedure • Previous/Ongoing pain and the effects on the patient • Previous method for pain control that was effective/non effective • Patient/family attitude toward the use of pain medications • Any history of substance abuse • Patient typical coping style • Expectation/beliefs concerning pain and identification of pain goal • Describe how the patient demonstrate pain • Inventory the current medications – Over the counter – Prescription – Herbal. /Vitamins 6
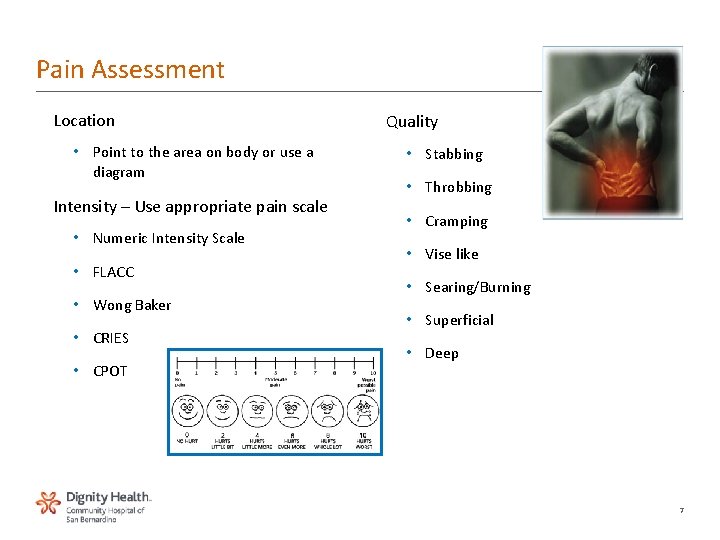
Pain Assessment Location • Point to the area on body or use a diagram Intensity – Use appropriate pain scale • Numeric Intensity Scale • FLACC • Wong Baker • CRIES • CPOT Quality • Stabbing • Throbbing • Cramping • Vise like • Searing/Burning • Superficial • Deep 7
Pain Assessment Precipitating Factors • Motion/Position changes • Fear and emotional distress • Fatigue • Environmental stressors • Inadequate pain relief measure Factors Associated with Pain • Nausea/Vomiting • Bradycardia/Tachycardia • Hypertension/Hypotension • Perspiration • Apprehension/Anxiety Non verbal indicators of pain • Withdrawal • Grimacing • Crying • Inactivity • Family/Significant other/ Caregivers alert of clues from patient 8
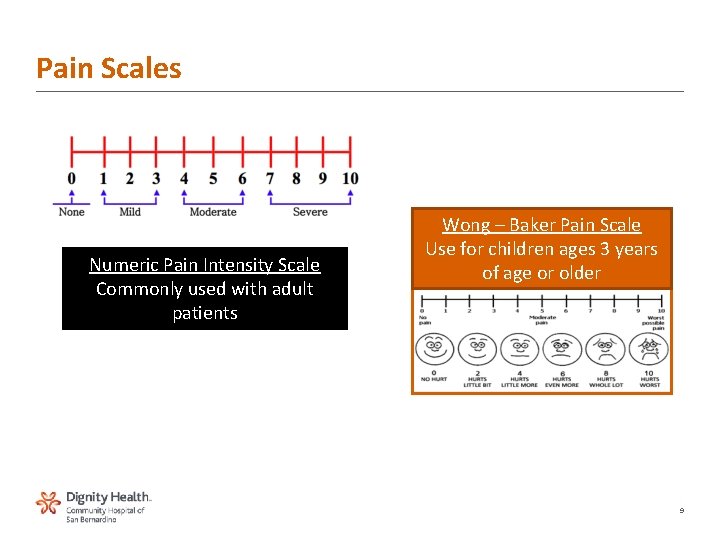
Pain Scales Numeric Pain Intensity Scale Commonly used with adult patients Wong – Baker Pain Scale Use for children ages 3 years of age or older 9
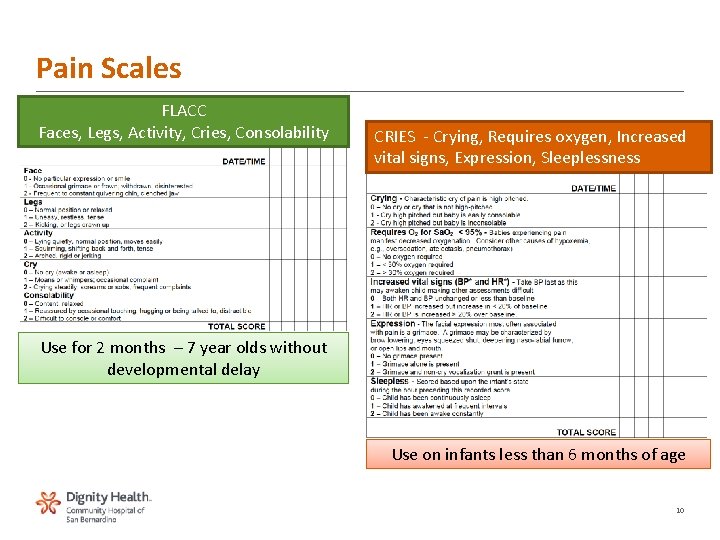
Pain Scales FLACC Faces, Legs, Activity, Cries, Consolability CRIES ‐ Crying, Requires oxygen, Increased vital signs, Expression, Sleeplessness Use for 2 months – 7 year olds without developmental delay Use on infants less than 6 months of age 10
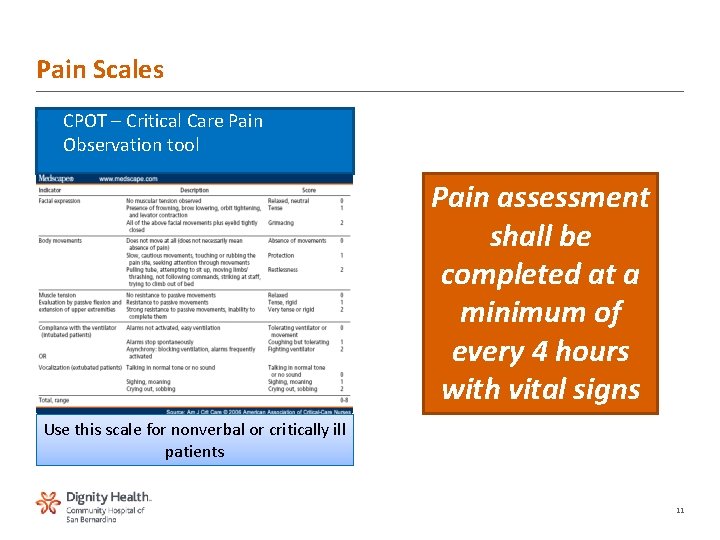
Pain Scales • CPOT – Critical Care Pain Observation tool Pain assessment shall be completed at a minimum of every 4 hours with vital signs Use this scale for nonverbal or critically ill patients 11
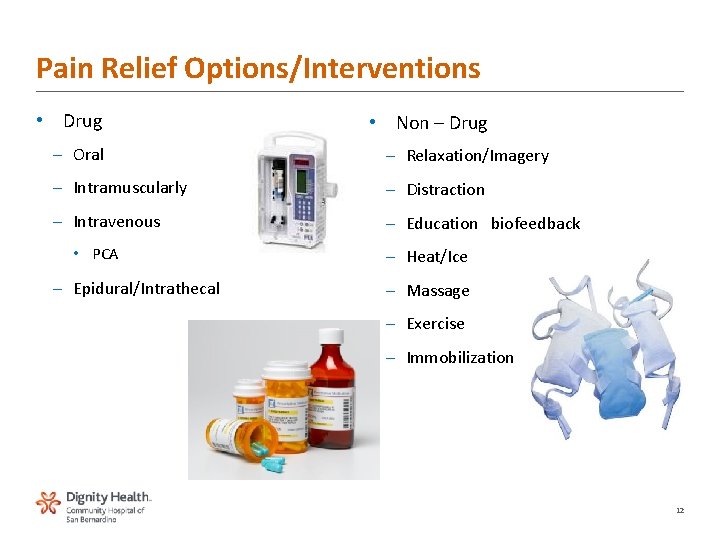
Pain Relief Options/Interventions • Drug • Non – Drug – Oral – Relaxation/Imagery – Intramuscularly – Distraction – Intravenous – Education biofeedback • PCA – Epidural/Intrathecal – Heat/Ice – Massage – Exercise – Immobilization 12
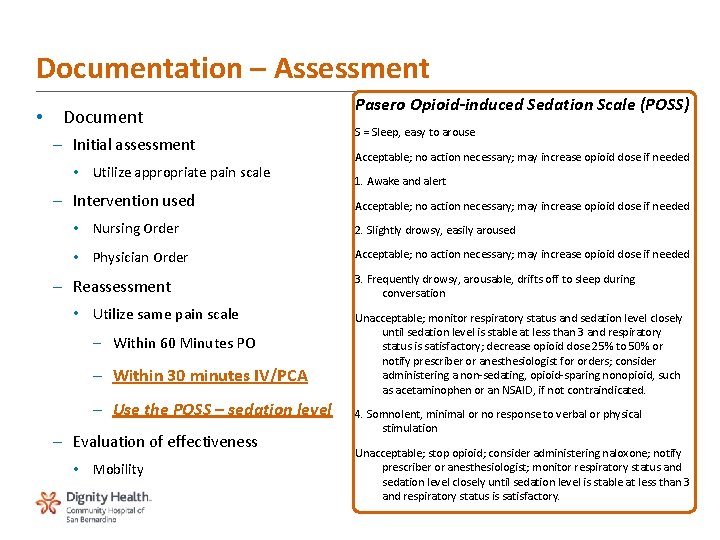
Documentation – Assessment • Document – Initial assessment • Utilize appropriate pain scale – Intervention used Pasero Opioid‐induced Sedation Scale (POSS) S = Sleep, easy to arouse Acceptable; no action necessary; may increase opioid dose if needed 1. Awake and alert Acceptable; no action necessary; may increase opioid dose if needed • Nursing Order 2. Slightly drowsy, easily aroused • Physician Order Acceptable; no action necessary; may increase opioid dose if needed – Reassessment • Utilize same pain scale – Within 60 Minutes PO – Within 30 minutes IV/PCA – Use the POSS – sedation level – Evaluation of effectiveness • Mobility 3. Frequently drowsy, arousable, drifts off to sleep during conversation Unacceptable; monitor respiratory status and sedation level closely until sedation level is stable at less than 3 and respiratory status is satisfactory; decrease opioid dose 25% to 50% or notify prescriber or anesthesiologist for orders; consider administering a non‐sedating, opioid‐sparing nonopioid, such as acetaminophen or an NSAID, if not contraindicated. 4. Somnolent, minimal or no response to verbal or physical stimulation Unacceptable; stop opioid; consider administering naloxone; notify prescriber or anesthesiologist; monitor respiratory status and sedation level closely until sedation level is stable at less than 3 and respiratory status is satisfactory. 13
Documentation – Patient/Family Teaching • Patient/Family should have active involvement in pain prevention and treatment. • Teach the use of the pain scale appropriate for their age and condition. • Educate with respect their beliefs: – Personal – Cultural – Spiritual – Ethnic • Include demonstration and/or discussion of the options available – Non – Drug • Review/Reassess pain management plan 14
Special Considerations Infants/Children Use appropriate pain scale for age and development Use toys/stuffed animal for location of pain Elderly Differentiate between acute and chronic type pain Observe for interaction response due to OTC medications observe for signs of dementia, cognitive impairment, or delirium observe for signs of over/under medication response Substance Abusers History may predispose them to re abusive behavior May require high doses due to past tolerance of substance abuse End of life/palliative Care Ensure a dignified, peaceful, and comfortable death Consult the Palliative Coordinator Complicated pain management related to multiple disease processes 15
Congrats you have completed the pain module. . . Now take the test 16

Thank You
- Slides: 17