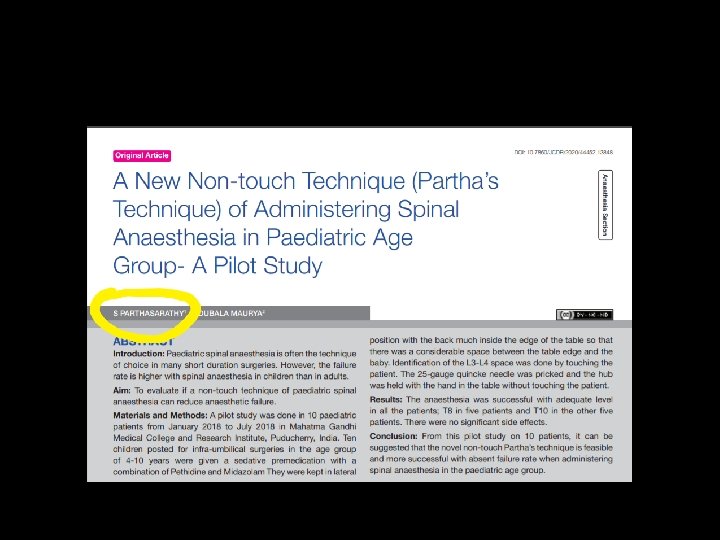
Paediatric spinal anaesthesia clinical pearls Dr S Parthasarathy






- Slides: 38
Paediatric spinal anaesthesia clinical pearls Dr. S. Parthasarathy MD. , DA. , DNB, MD (Acu), Dip. Diab. Dip. Software based statistics. Ph. D(Physiology) FICA, IDRA , CUGRA. Professor MGMCRI www. painfreepartha. com
My salute !! Legendary teacher of two centuries
History • Spinal anesthesia was probably the earliest form of regional anesthesia that was considered a useful practice for children • ( Bainbridge, 1901 ; Tyrell-Gray, 1909 ). • Popularized in 1990 s
Why it came to lime light ? ? • Premature infants – possible hernia • Muscular and neuromuscular disease for lower abdominal and lower limb surgery
Other indications • The safety and success of spinal • such as pyloromyotomy, gastrostomy placement, • myelomeningocele repair, • cardiac surgery, and genitourinary procedures. • Moreover, spinal anesthesia has been successfully used in high-risk infants and • for cardiac catheterization,
To consider spinal in ? ? • • • facial dysmorphia difficult intubation, muscular dystrophy, family history of malignant hyperthermia or a full stomach with aspiration risk
Contraindications • Coagulation abnormalities • Systemic sepsis or local infection at the puncture point • Uncorrected hypovolaemia • Parental refusal or an uncooperative child • Neurological abnormalities such as spina bifida, • increased intracranial pressure • Procedures lasting more than 90 minutes

• Are there any differences ? ?
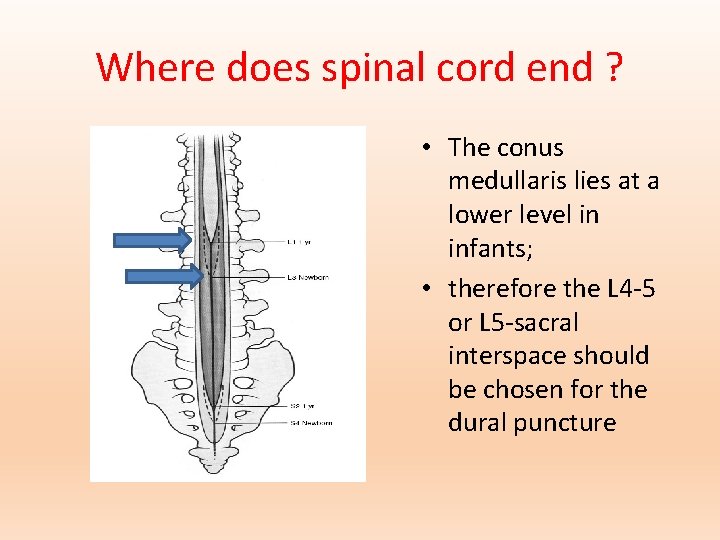
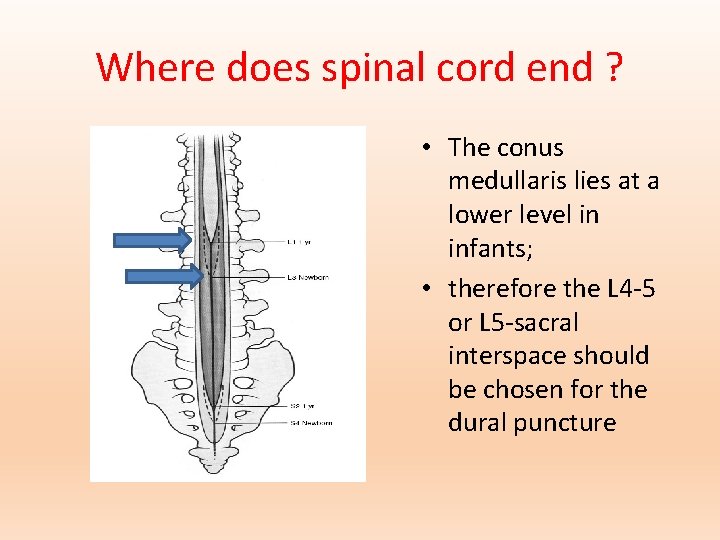
Where does spinal cord end ? • The conus medullaris lies at a lower level in infants; • therefore the L 4 -5 or L 5 -sacral interspace should be chosen for the dural puncture
Intercristal line ? ? • Tuffiers line !! • The intercristal line crosses the midline at the S 1 interspace in neonates, and at the L 5 interspace in older children
Differences • The approach to the subarachnoid space requires a straighter trajectory of the needle than in older children. • The distance to the subarachnoid space is small, • cerebral spinal fluid (CSF) flow may be slow, • ligamentum flavum is thin • Laminae are cartilaginous - no to paramedian approach
Difference • CSF volume - 4 m. L/kg (2 m. L/kg in adults) with 50% being in the spinal canal compared with 25% in adults • Higher doses • More vascular -- Duration – short Even bupivacaine maximum 90 minutes Usually 45 minutes…
Characters of nerve fibres • Small nerve fibres • Nonmyelinated • Small distances between nodes of ranvier • Lumbar lordosis - Absent but in two years it may be present
Differences • fibrous sheaths around nerves are not well developed and myelination is not complete until about 2 years of age. • This makes immature nerves more sensitive to local anaesthetics and less concentrated solutions than are used in adults usually result in a dense block.
Not only CSF volume • In term babies the length of the spinal cord is about 20 cm (in adults 65– 70 cm). • This means that the length to weight ratio is four or five times higher in newborns than in adults. • so -- Dose differences
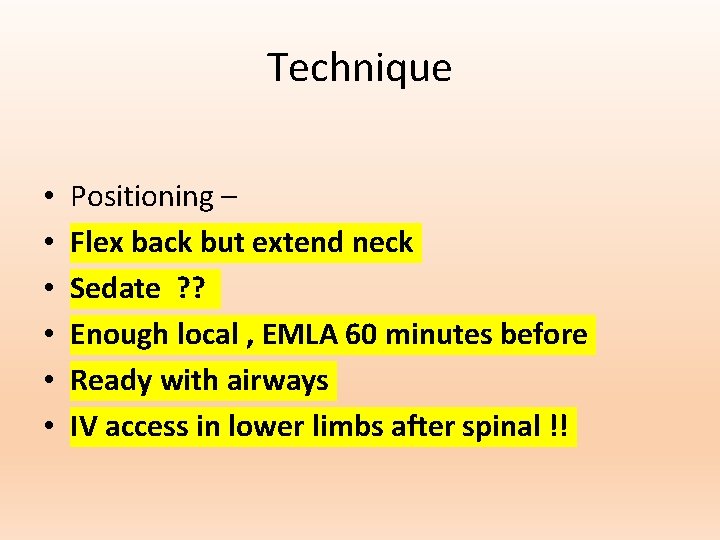
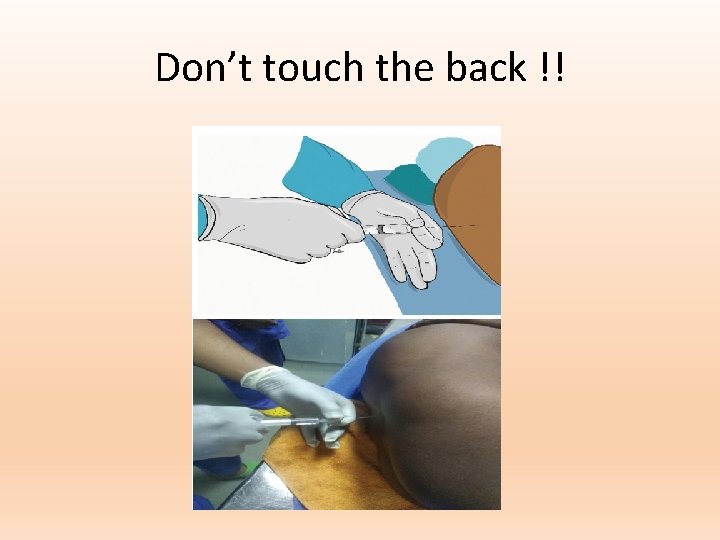
Technique • • • Positioning – Flex back but extend neck Sedate ? ? Enough local , EMLA 60 minutes before Ready with airways IV access in lower limbs after spinal !!

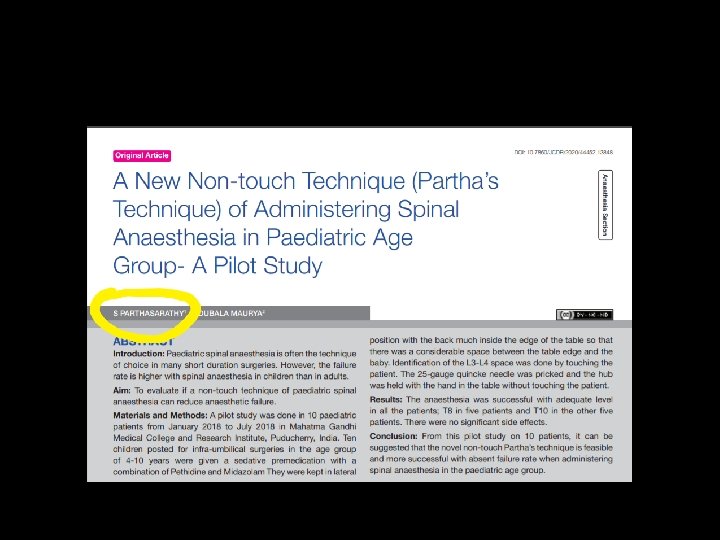
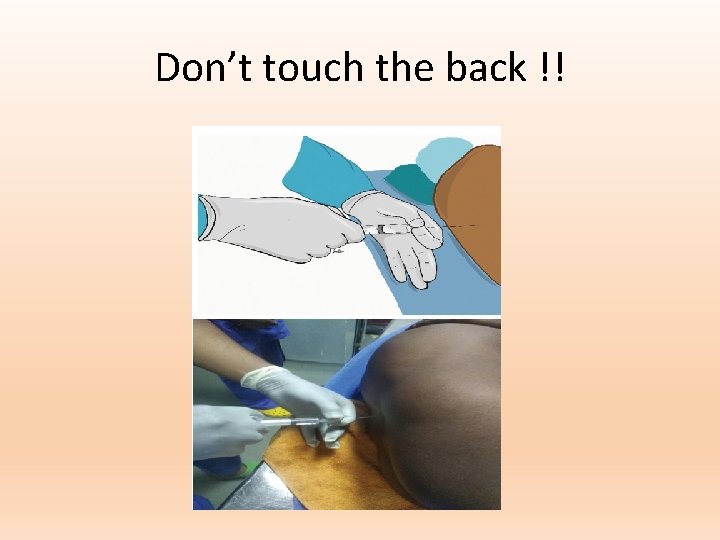
Don’t touch the back !!
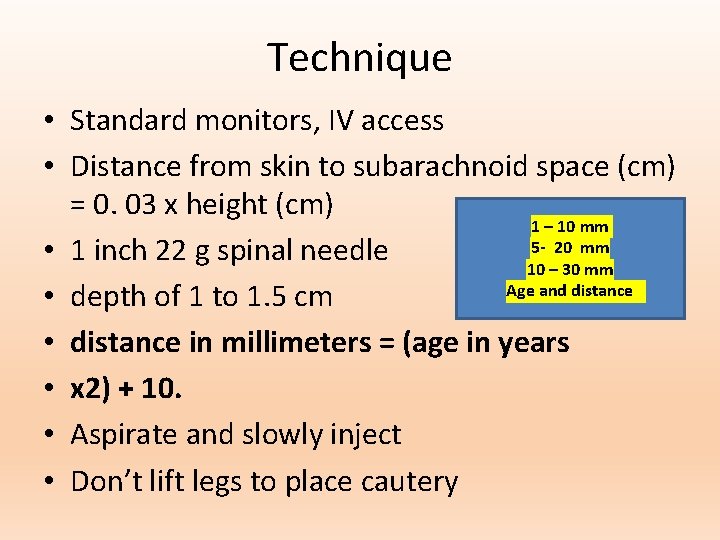
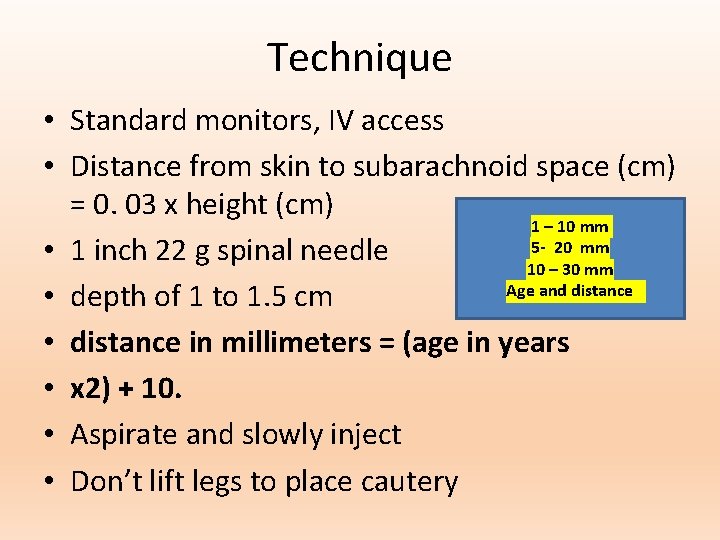
Technique • Standard monitors, IV access • Distance from skin to subarachnoid space (cm) = 0. 03 x height (cm) 1 – 10 mm 5 - 20 mm • 1 inch 22 g spinal needle 10 – 30 mm Age and distance • depth of 1 to 1. 5 cm • distance in millimeters = (age in years • x 2) + 10. • Aspirate and slowly inject • Don’t lift legs to place cautery
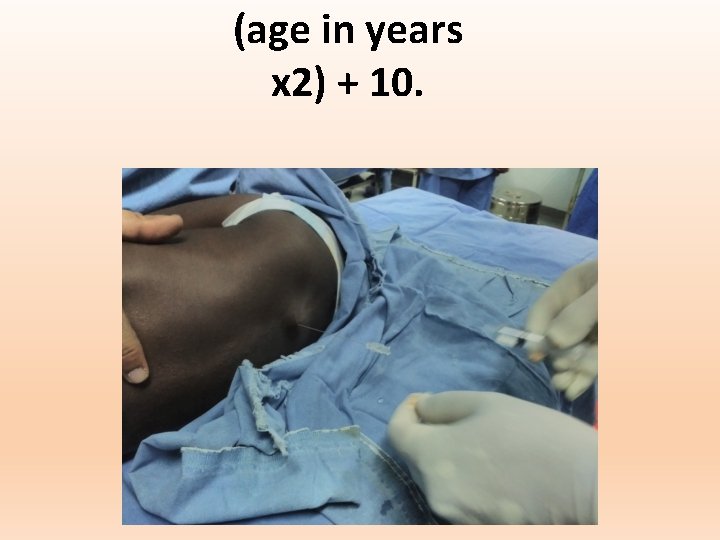
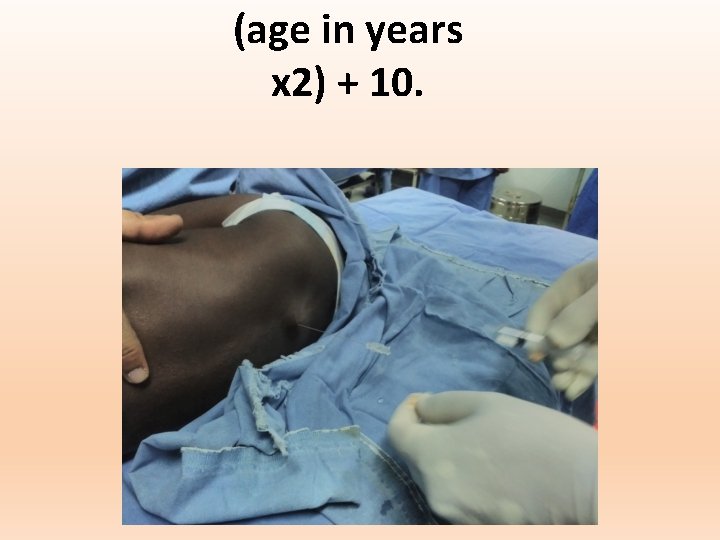
(age in years x 2) + 10.
This is my midazolam
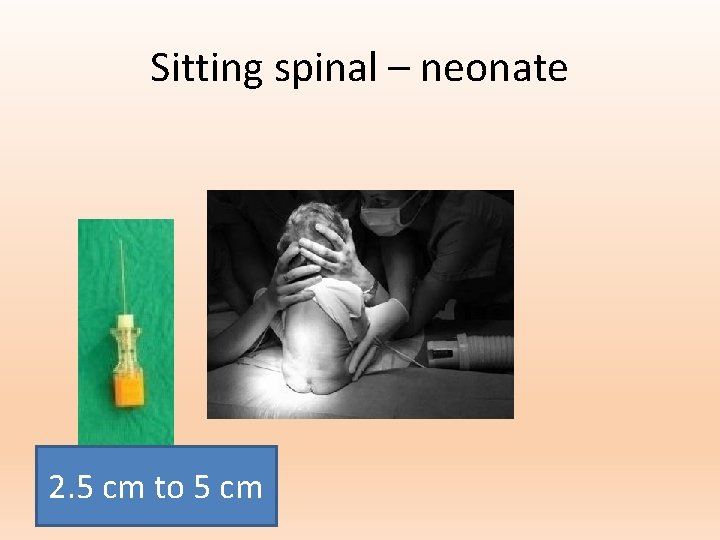
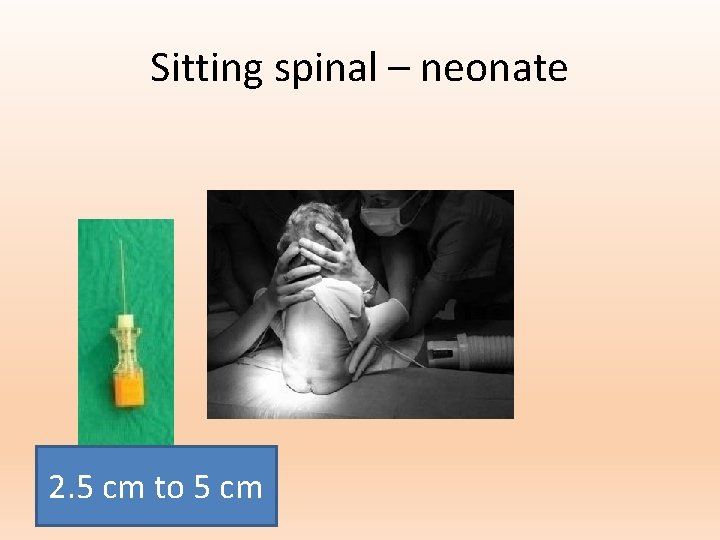
Sitting spinal – neonate 2. 5 cm to 5 cm
Technique • The ligamentum flavum is very soft in children and a distinctive “pop” may not be perceived when the dura is penetrated. • Be gentle and slow • Inject the dose and give 0. 2 ml or 0. 1 ml of air later

Straight – 1 ml syringe www. painfreepartha. com
Assessing the block is difficult. • The response to cold spray can be useful, • observation of paradoxical respiratory muscle movement • loss of response to a low amperage tetanic stimulus.
Level ? ? • • Pacifier nipple Spread of the block is less predictable High level means – no BP fall but apnea !! • Monitor 24 hours
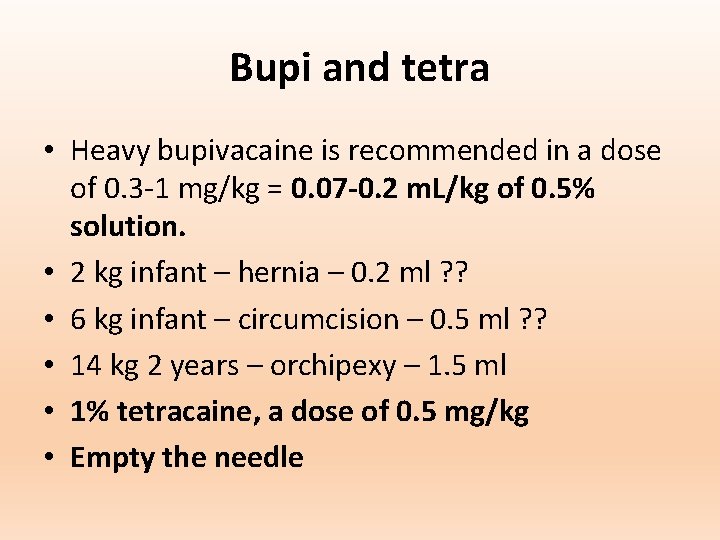
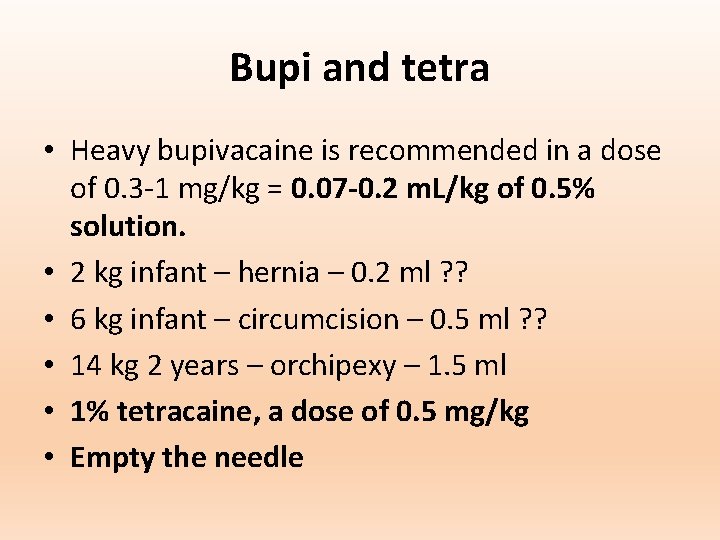
Bupi and tetra • Heavy bupivacaine is recommended in a dose of 0. 3 -1 mg/kg = 0. 07 -0. 2 m. L/kg of 0. 5% solution. • 2 kg infant – hernia – 0. 2 ml ? ? • 6 kg infant – circumcision – 0. 5 ml ? ? • 14 kg 2 years – orchipexy – 1. 5 ml • 1% tetracaine, a dose of 0. 5 mg/kg • Empty the needle
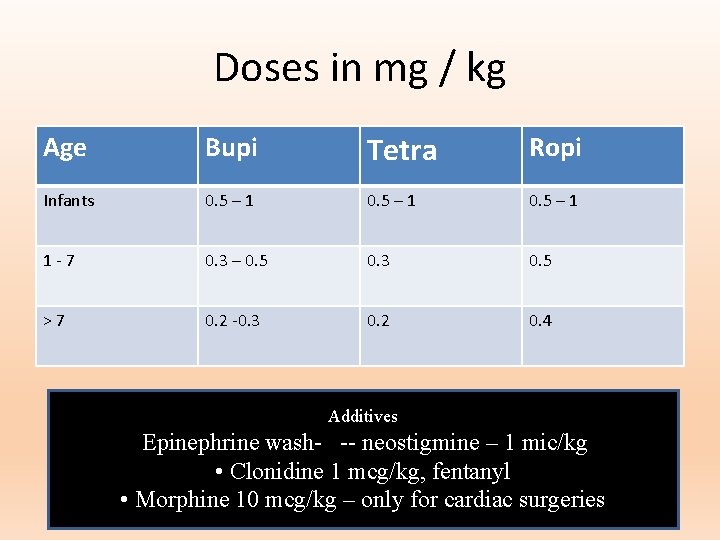
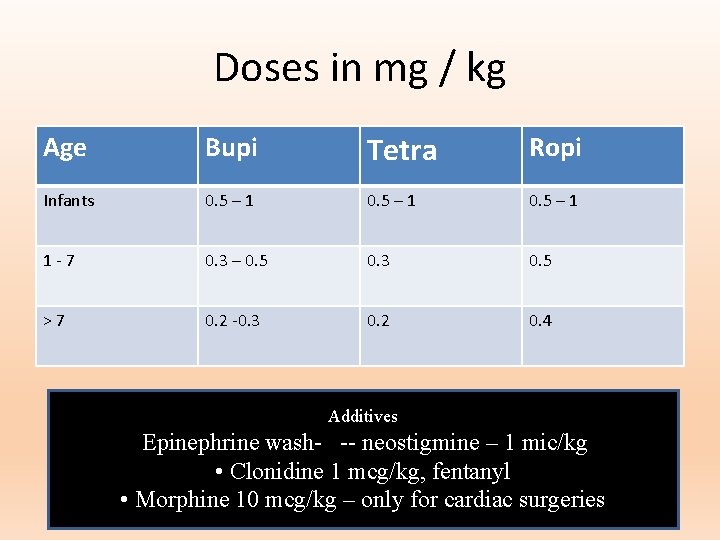
Doses in mg / kg Age Bupi Tetra Ropi Infants 0. 5 – 1 1 -7 0. 3 – 0. 5 0. 3 0. 5 >7 0. 2 -0. 3 0. 2 0. 4 Additives Epinephrine wash- -- neostigmine – 1 mic/kg • Clonidine 1 mcg/kg, fentanyl • Morphine 10 mcg/kg – only for cardiac surgeries
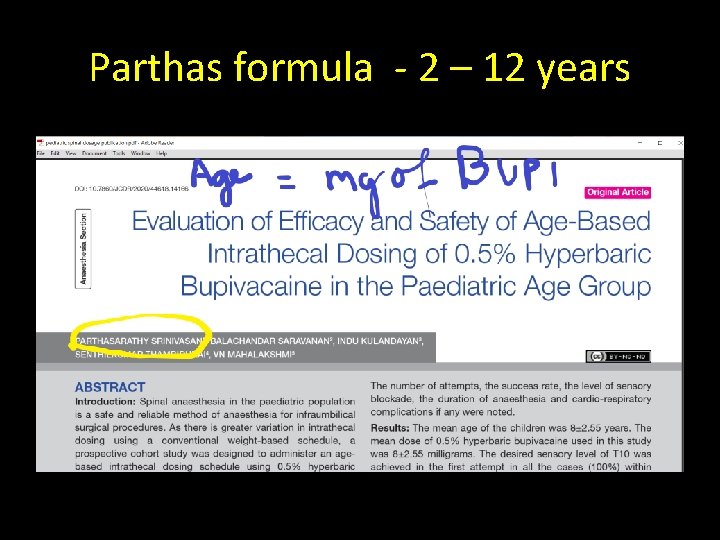
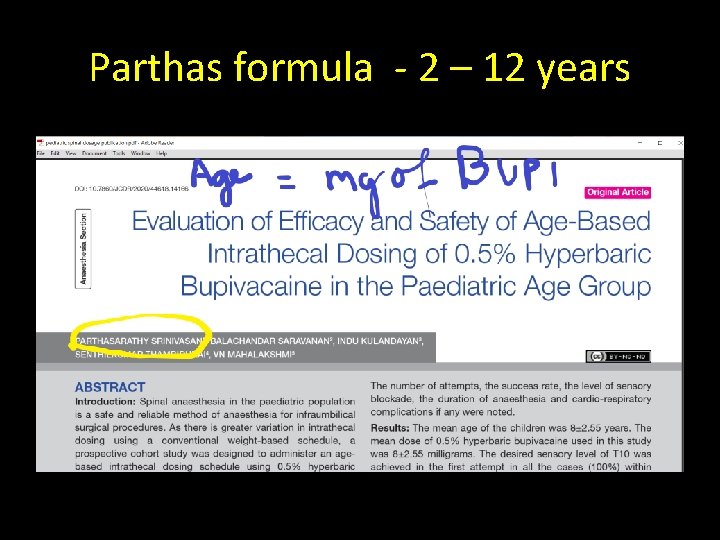
Parthas formula - 2 – 12 years
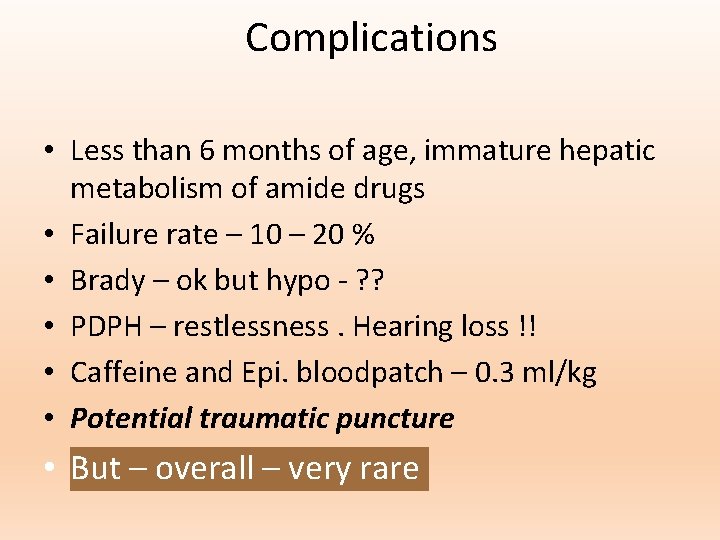
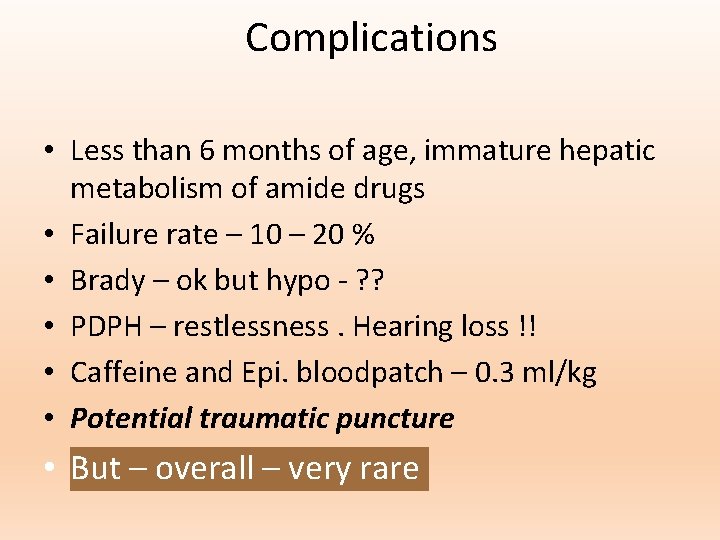
Complications • Less than 6 months of age, immature hepatic metabolism of amide drugs • Failure rate – 10 – 20 % • Brady – ok but hypo - ? ? • PDPH – restlessness. Hearing loss !! • Caffeine and Epi. bloodpatch – 0. 3 ml/kg • Potential traumatic puncture • But – overall – very rare
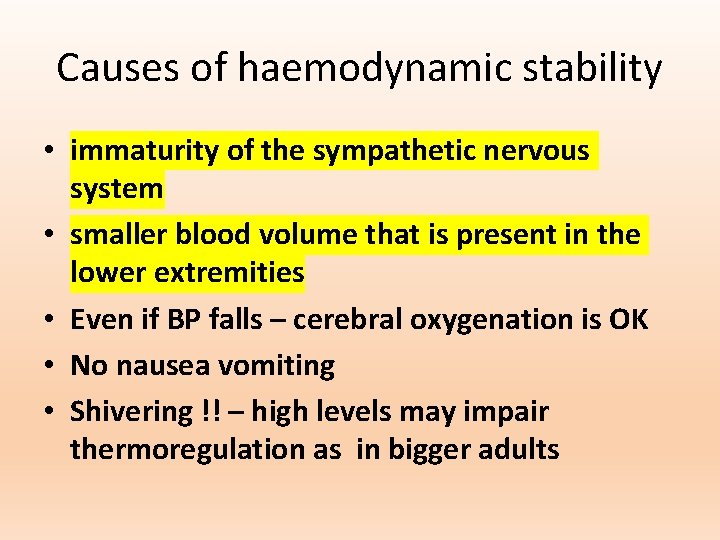
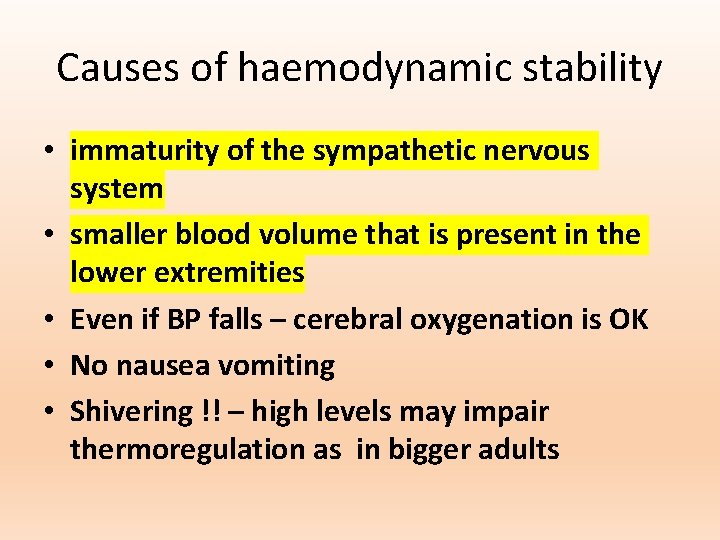
Causes of haemodynamic stability • immaturity of the sympathetic nervous system • smaller blood volume that is present in the lower extremities • Even if BP falls – cerebral oxygenation is OK • No nausea vomiting • Shivering !! – high levels may impair thermoregulation as in bigger adults
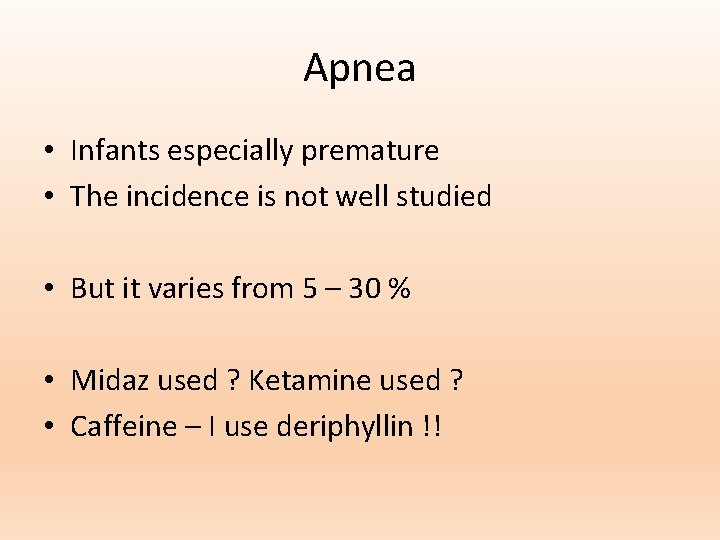
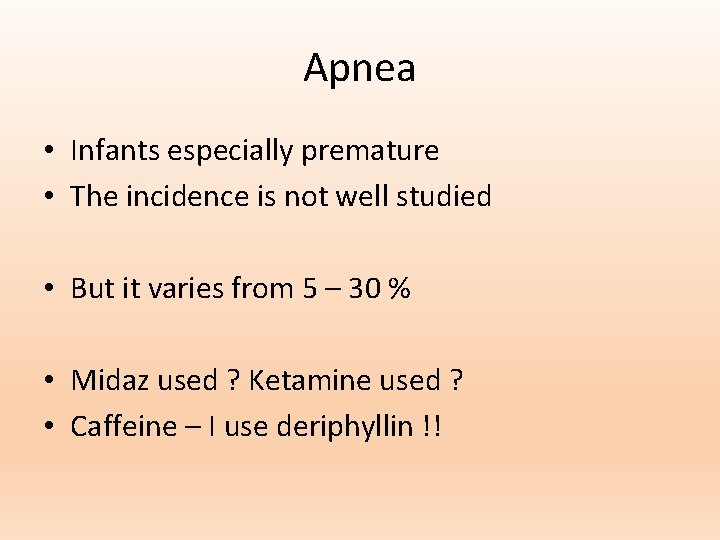
Apnea • Infants especially premature • The incidence is not well studied • But it varies from 5 – 30 % • Midaz used ? Ketamine used ? • Caffeine – I use deriphyllin !!

www. painfreepartha. com

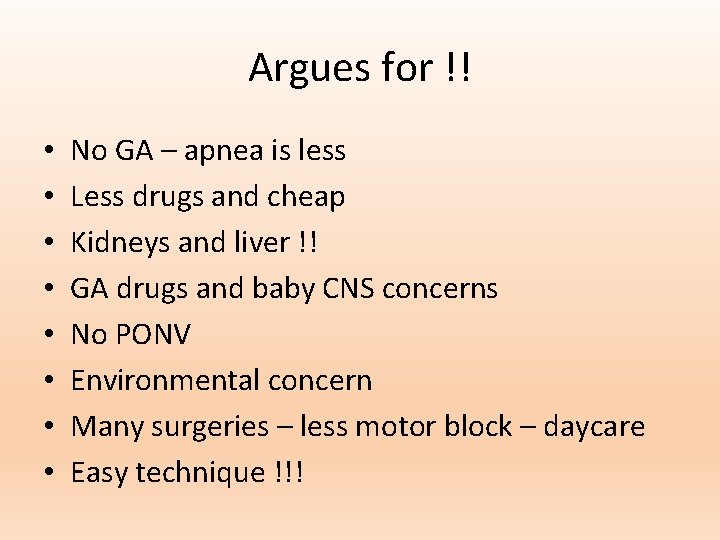
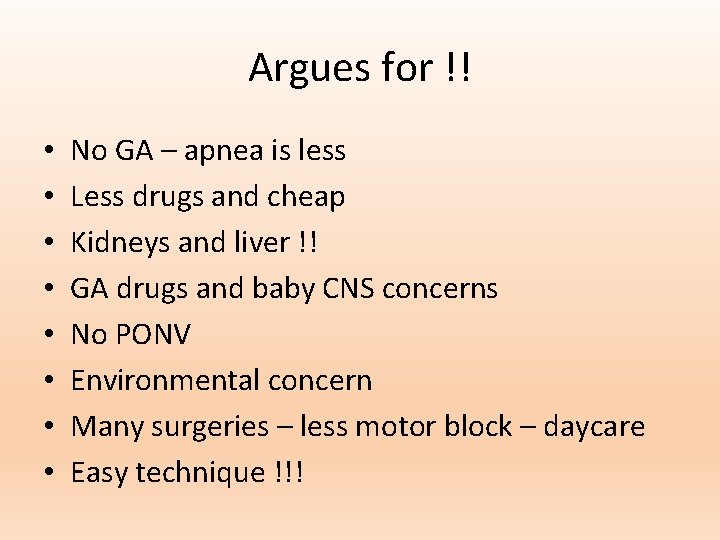
Argues for !! • • No GA – apnea is less Less drugs and cheap Kidneys and liver !! GA drugs and baby CNS concerns No PONV Environmental concern Many surgeries – less motor block – daycare Easy technique !!!
Against • Duration of action – limited • Mental inhibition among anaesthesiologists • Awake unsettled infants and kids

Summary Indications Differences Dose and drugs Position Dexterity Complications For and against Thank you all