PAEDIATRIC LUMBAR PUNCTURE THINGS TO CONSIDER Indications Contraindications
PAEDIATRIC LUMBAR PUNCTURE
THINGS TO CONSIDER • Indications • Contraindications • What stuff do you need? • Anaesthesia and positioning • Sample collection • Interpretation of results • Potential complications
INDICATIONS • Suspected sub-arachnoid haemorrhage with a normal CT • Suspected meningitis or encephalitis • Do not do a lumbar puncture if the child is so sick that you will give antibiotics for meningitis even if the CSF is normal on microscopy
CONTRAINDICATIONS • The clinical findings that suggest you should give dexamethasone and antibiotics immediately, and delay lumbar puncture for 1 -2 days until the child is improving are: • Coma • Signs of raised intracranial pressure • bulging fontanelle in the absence of other signs of raised ICP, is not a contraindication • Cardiovascular compromise/ shock • Respiratory compromise • Focal neurological signs or seizures • Recent seizures (within 30 minutes or not regained normal conscious level afterwards)
MORE CONTRAINDICATIONS • Coagulopathy/thrombocytopenia • Local infection (in the area where an LP would be performed) • The febrile child with purpura where meningococcal infection is suspected. When to scan? • Do a CT scan if the child has focal neurological signs • A normal CT scan does not rule out raised ICP • CT scans are not helpful in most children with meningitis • Don’t delay antibiotics whilst waiting for a scan
WHAT STUFF DO YOU NEED? • At least one trained assistant to hold the child • Sterile gloves • Sterile drapes and procedure tray • Skin preparation: Betadine or chlorhexidine • Topical anaesthetic + local anaesthetic • CSF tubes x 2 • Spinal needle (next slide)
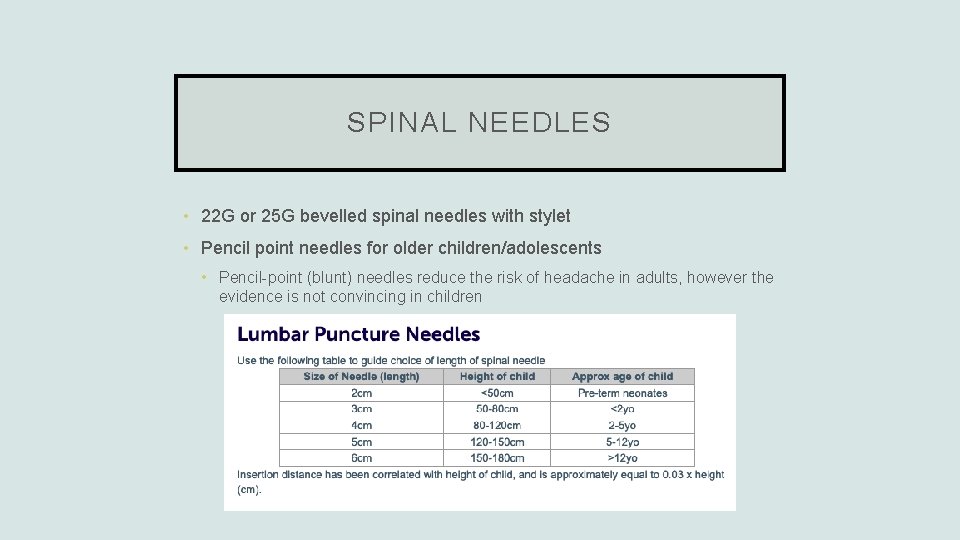
SPINAL NEEDLES • 22 G or 25 G bevelled spinal needles with stylet • Pencil point needles for older children/adolescents • Pencil-point (blunt) needles reduce the risk of headache in adults, however the evidence is not convincing in children
ANAESTHESIA + POSITIONING • Non-pharmacological techniques should be used where possible, including explanation (in an older child), distraction, and the presence of a parent • Topical anaesthetic cream (Emla) except where specimens are required urgently • Subcutaneous lignocaine should be used in addition to topical anaesthetic. • Up to 0. 4 ml/kg of 1% (4 mg/kg) • Oral sucrose should be used for infants <3 months • Sedation, including nitrous, should be considered for children older than 6 months with normal conscious state. • Monitor all sedated or seriously ill children with continuous pulse oximetry +/ECG leads
HOW DO YOU ACTUALLY DO IT? • Position the child either sitting or in the left lateral position, try not to flex the neck • Have a helper firmly holding the child in position • Hold the needle with the stylet in place and the bevel facing skywards (if the child is decubitus), or to the side (if they are sitting) – helps to prevent post-LP headache • Aim for the L 4/L 5 intervertebral space (L 3/L 4 will also do) • Aim the needle towards the umbilicus • Opening pressures are not routinely measured in children • Feel resistance as you meet the spinous ligament, and this will fall as you pass it • Obtain your sample • Replace the stylet before removing the needle – helps to reduce post-LP headache • Apply pressure to the skin for a minute, and then apply a dressing
SAMPLE COLLECTION • Try to collect 2 numbered tubes, each with 5 -10 drops of CSF • Send urgently to the lab for: • Microscopy • Protein • Glucose • Culture • Suspect encephalitis? Send for HSV PCR • Suspect meningitis? Send for enterovirus PCR, Neisseria PCR – and meningococcal PCR if the child has already received antibiotics
COMPLICATIONS • Failure to obtain a specimen / need to repeat LP / traumatic tap (common) • Post-dural puncture headache in up to 5 -15% (fairly common) • Transient/persistent paresthesiae/numbness (very uncommon) • Respiratory arrest from positioning (rare) • Spinal haematoma or abscess (very rare) • Tonsillar herniation (extremely rare in the absence of contraindications)

RESOURCES • Royal Children’s Hospital Clinical Practice Guidelines – Lumbar Puncture https: //www. rch. org. au/clinicalguide/guideline_index/Lumbar_puncture/
- Slides: 13