PAEDIATRIC DEFIBRILLATION A guide to an essential therapy
PAEDIATRIC DEFIBRILLATION A guide to an essential therapy June 2013 Dr David Cloete
Introduction � Why this lecture? Critical link in the chain of survival. Epidemiology of VF & Pulseless VT � 19% out-of-hospital � 27% in-hospital; 10 -15% as initial arrythmia. Survival VF > asystole. Survival ≈ minimizing time to shock. Clinical importance - Knowledge is power.

Agenda: � � � Introduction ✔ A brief note on CPR Definitions & Arrhythmias Electrophysiology CPR & Defibrillation Types of Defibrillator Some Physics Procedure AEDS Safety & Complications Reversible/Complicating Factors Conclusion
A brief note on CPR � Early CPR saves lives. Compressions AND ventilations. � AHA vs. UK Resuscitation Council � � Paediatric arrests mostly respiratory � ↑ likelihood of bystander CPR, compressions easy, no equipment, negligible delay. � Chest compressions: high quality!! � Important for defibrillation.
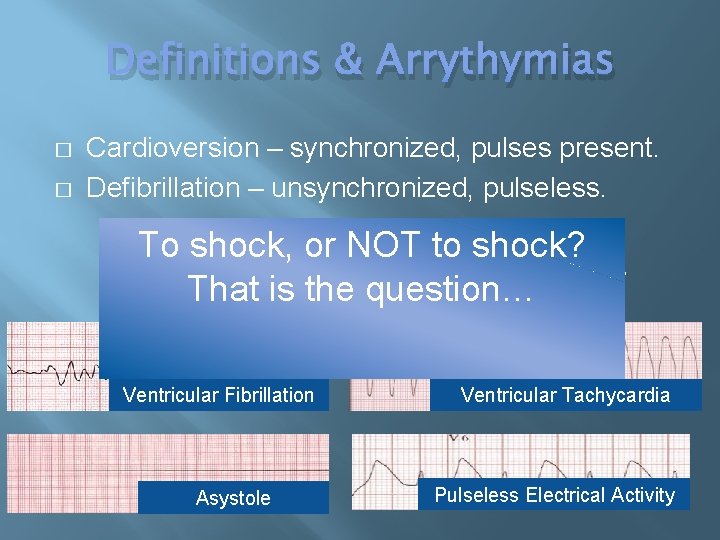
Definitions & Arrythymias � � Cardioversion – synchronized, pulses present. Defibrillation – unsynchronized, pulseless. To shock, or NOT to shock? Eber’s Papyrus: “Heart diseased…vessels That is the question… inactive… death is near. ” Ventricular Fibrillation Asystole Ventricular Tachycardia Pulseless Electrical Activity
Electrophysiology � Cardioversion � Depolarization; tissue rendered refractory. � Defibrillation � Controversy exists. � Stuns the heart. Pacemaker cells resume. � Critical mass hypothesis. � Upper limit of vulnerability hypothesis.
CPR & Defibrillation � Defibrillation Success: � State of myocardium. � Amount of myocardial damage. � Prior functional state. � Cause of VF. � VF duration ≈ ATP stores ≈ pacemaker recovery � Definition of successful shock
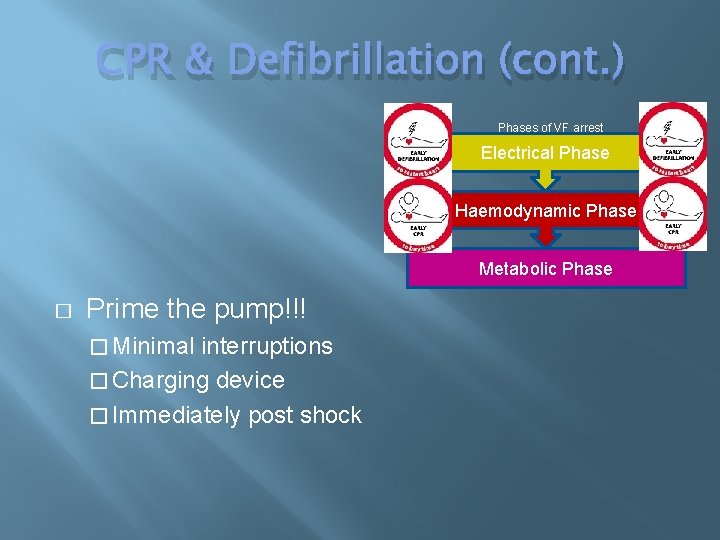
CPR & Defibrillation (cont. ) Phases of VF arrest Electrical Phase Haemodynamic Phase Metabolic Phase � Prime the pump!!! � Minimal interruptions � Charging device � Immediately post shock
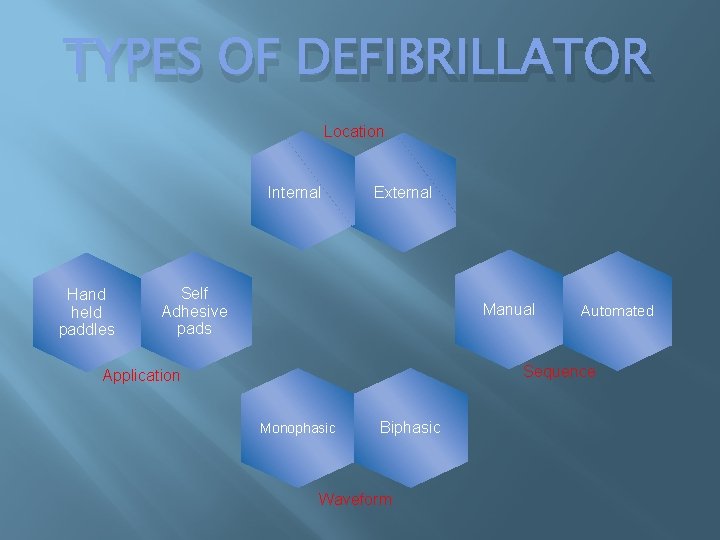
TYPES OF DEFIBRILLATOR Location Internal Hand held paddles External Self Adhesive pads Manual Automated Sequence Application Monophasic Biphasic Waveform
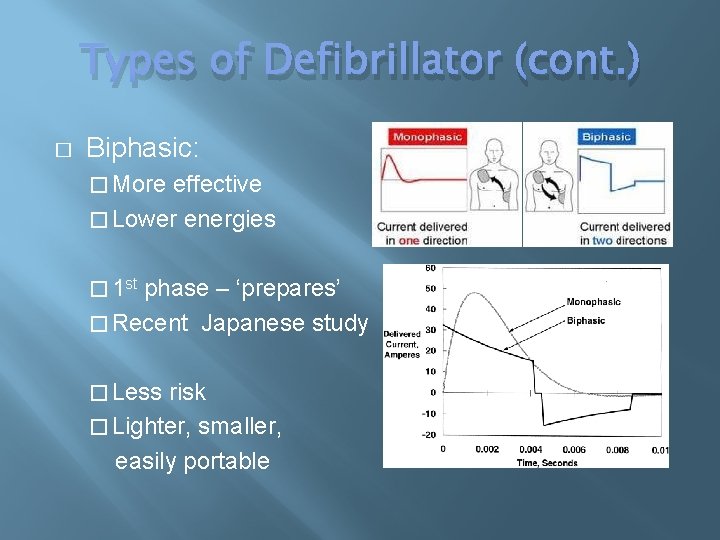
Types of Defibrillator (cont. ) � Biphasic: � More effective � Lower energies � 1 st phase – ‘prepares’ � Recent Japanese study � Less risk � Lighter, smaller, easily portable
Some physics… � Current flow → defibrillates � Current density → ratio of current magnitude with area perpendicular to current flow Fractional transmyocardial current
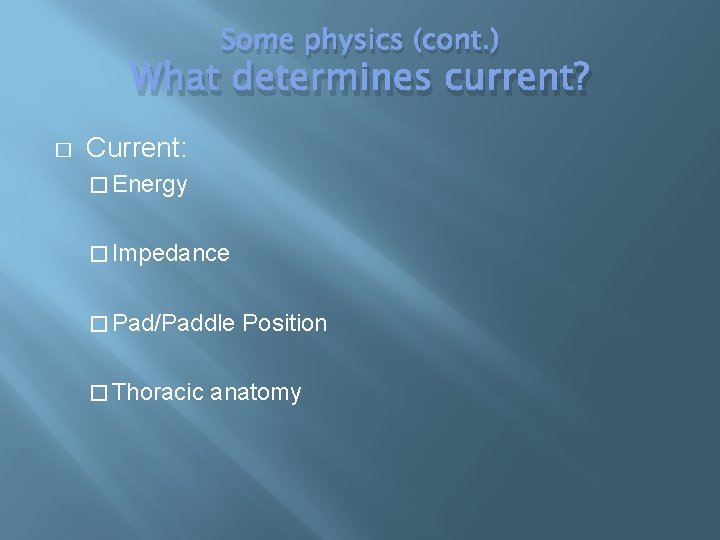
Some physics (cont. ) What determines current? � Current: � Energy � Impedance � Pad/Paddle Position � Thoracic anatomy
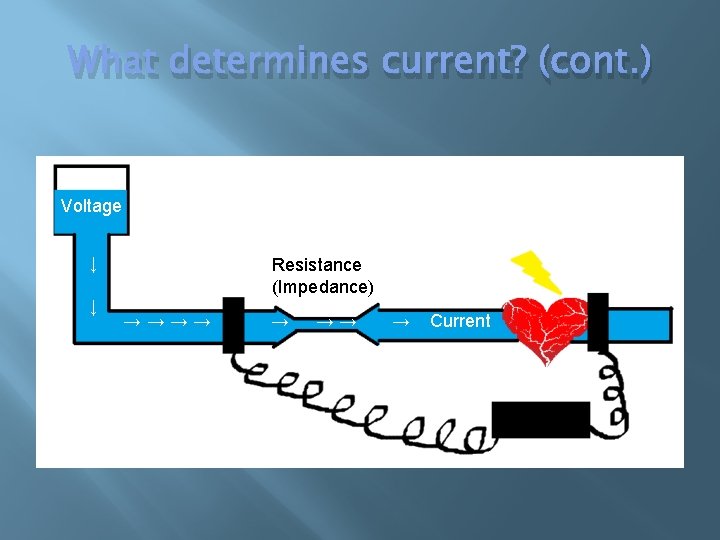
What determines current? (cont. ) Voltage ↓ ↓ Resistance (Impedance) → → → → Current
Some Physics… (cont. ) Impedance � Ohm’s Law: Current = Voltage / Impedance � Energy dissipation → lungs, thoracic cage, chest � Impedance too high: defibrillation not successful.
Impedance (cont. ) � Energy Selected → unsuccessful shock? Higher energy. � Electrode size & Interelectrode distance → Largest without touching. → 3 cm between → Paddles = Pads; other benefits → >10 kg: adult → <10 kg: infant
Impedance (cont. ) Electrode-Skin Interface → appropriate gel/paste for paddles � � Electrode pressure: firm paddles � Time Interval � Phase of ventilation: expiration � Tissue properties
Any questions thus far?
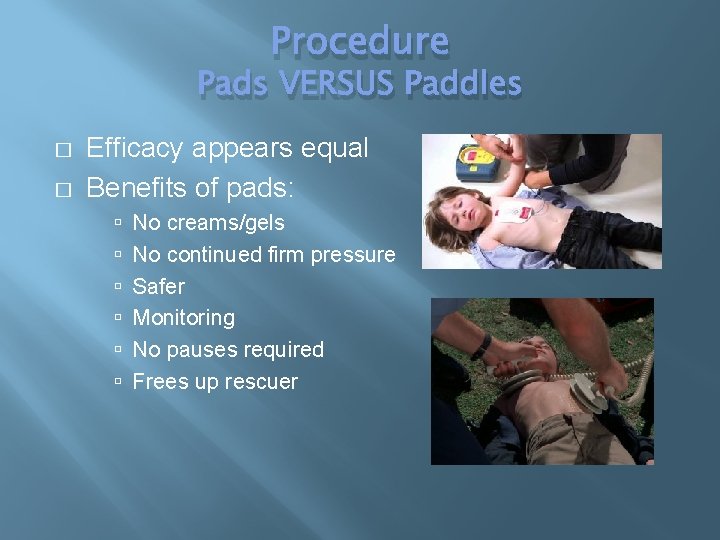
Procedure Pads VERSUS Paddles � � Efficacy appears equal Benefits of pads: No creams/gels No continued firm pressure Safer Monitoring No pauses required Frees up rescuer
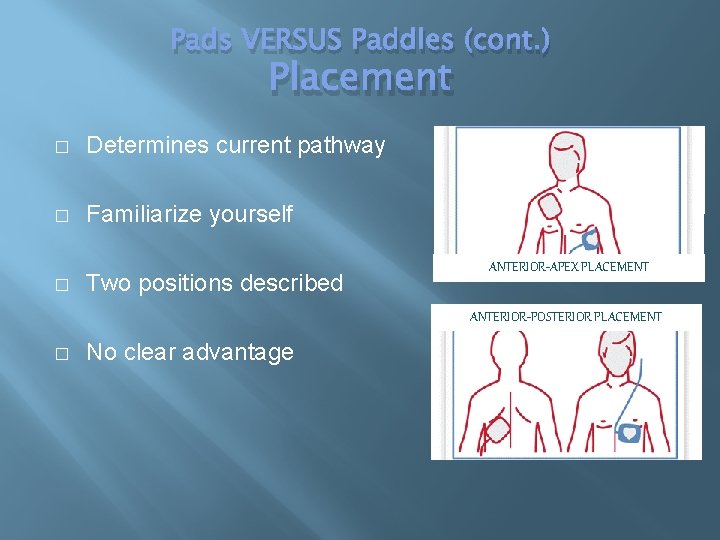
Pads VERSUS Paddles (cont. ) Placement � Determines current pathway � Familiarize yourself � Two positions described ANTERIOR-APEX PLACEMENT ANTERIOR-POSTERIOR PLACEMENT � No clear advantage
Procedure (cont. ) Selecting Energy Dose � Optimal dose? Upper limit for safety? UNKNOWN � AHA � 1 st shock 2 J/kg � 2 nd shock 4 J/kg � Subsequent shocks ≥ 4 J/kg (max 10 J/kg or adult dose)
Selecting Energy Dose (cont. ) � UK resuscitation council � Single 4 J/kg shock strategy � � Negligible effects with higher doses Initial dose 2 J/kg low success rate
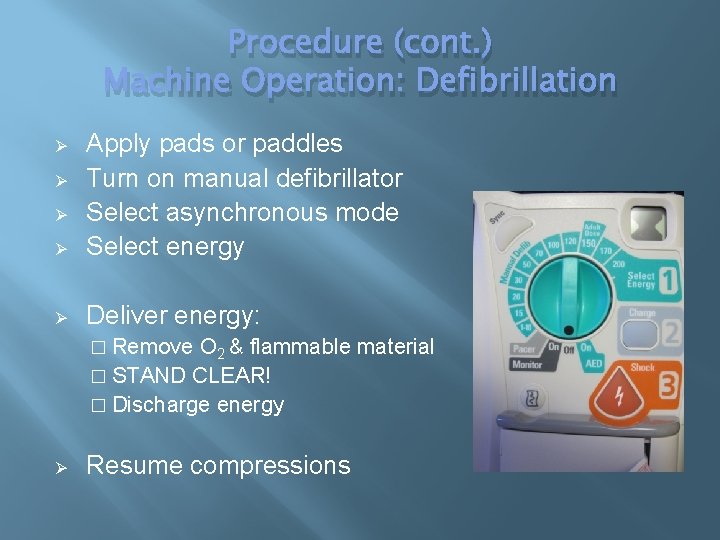
Procedure (cont. ) Machine Operation: Defibrillation Ø Apply pads or paddles Turn on manual defibrillator Select asynchronous mode Select energy Ø Deliver energy: Ø Ø Ø � Remove O 2 & flammable material � STAND CLEAR! � Discharge energy Ø Resume compressions
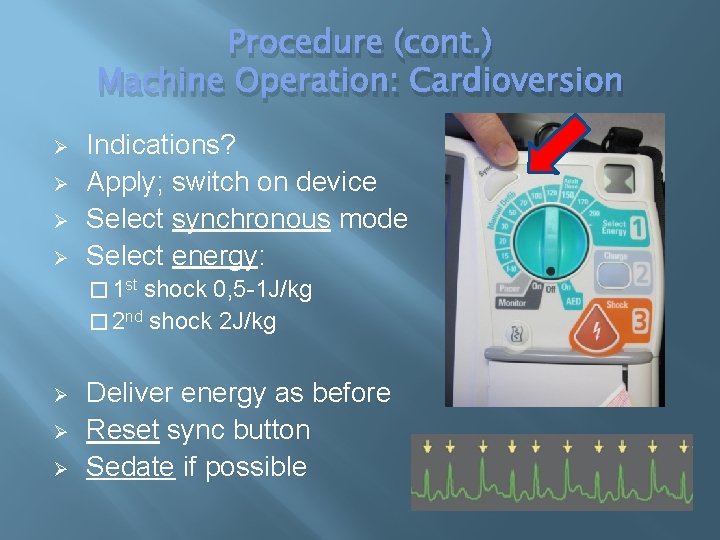
Procedure (cont. ) Machine Operation: Cardioversion Ø Ø Indications? Apply; switch on device Select synchronous mode Select energy: � 1 st shock 0, 5 -1 J/kg � 2 nd shock 2 J/kg Ø Ø Ø Deliver energy as before Reset sync button Sedate if possible
AEDs � Reliable � Voice & Visual prompts � Accurately differentiate � Safe � No previous training � Universal availability important
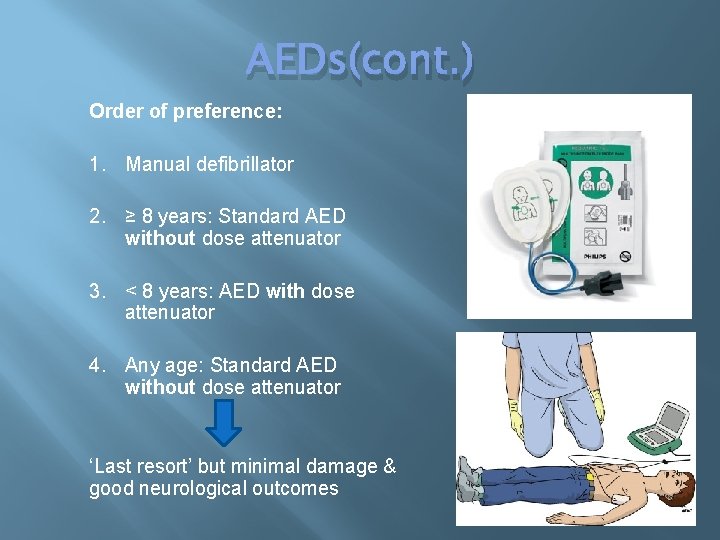
AEDs(cont. ) Order of preference: 1. Manual defibrillator 2. ≥ 8 years: Standard AED without dose attenuator 3. < 8 years: AED with dose attenuator 4. Any age: Standard AED without dose attenuator ‘Last resort’ but minimal damage & good neurological outcomes
Safety & Complications � Defibrillate when indicated! � Oxygen ≥ 1 m away � STAND CLEAR! � Arrythmias Myocardial injury Skin burns � � Use appropriate energy & reduce impedance
Reversible/Complicating Factors Always consider these! � � � H –ypovalaemia H – ypoxia H – ydrogen ion (acidosis) H – ypoglycaemia H – ypo/per. K+ H –ypothermia � � � T – ension pneumo T – amponade (cardiac) T – oxins T – hrombosis (pulmonary) T –hrombosis (coronary) T –rauma
Conclusion � Children do experience VF & pulseless VT � VF survival better than asystole � Early CPR & early defibrillation saves lives � High quality chest compressions AND ventilations crucial
Conclusion (cont. ) � Foundation of good ALS = good BLS! � Know the difference between defibrillation & cardioversion � Always consider: � Impedance � Hs & Ts � Be familiar with your resources!
YOU MEAN TO TELL ME Questions? ? THAT I CAN’T ‘PLAY’ WITH ELECTRICITY, BUT NOW YOU CAN? !
- Slides: 30